Different types of placenta previa
Placenta Previa | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is placenta previa?
Bleeding can happen at any time during pregnancy. Placenta previa can cause bleeding late in pregnancy. This means after about 20 weeks.
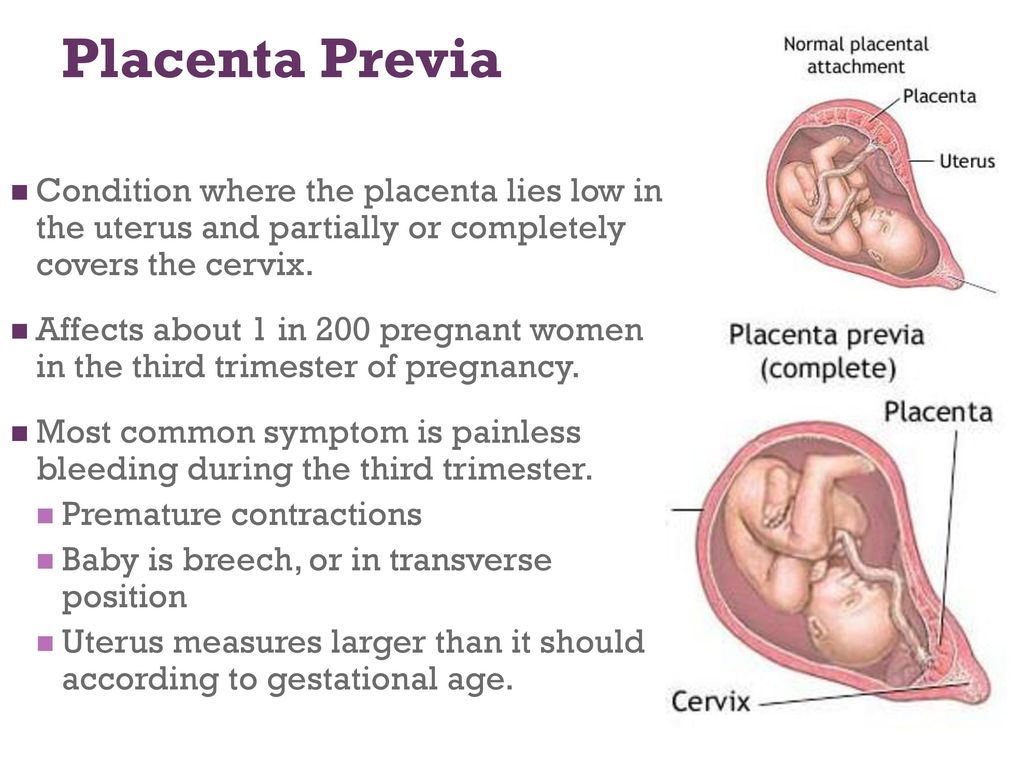
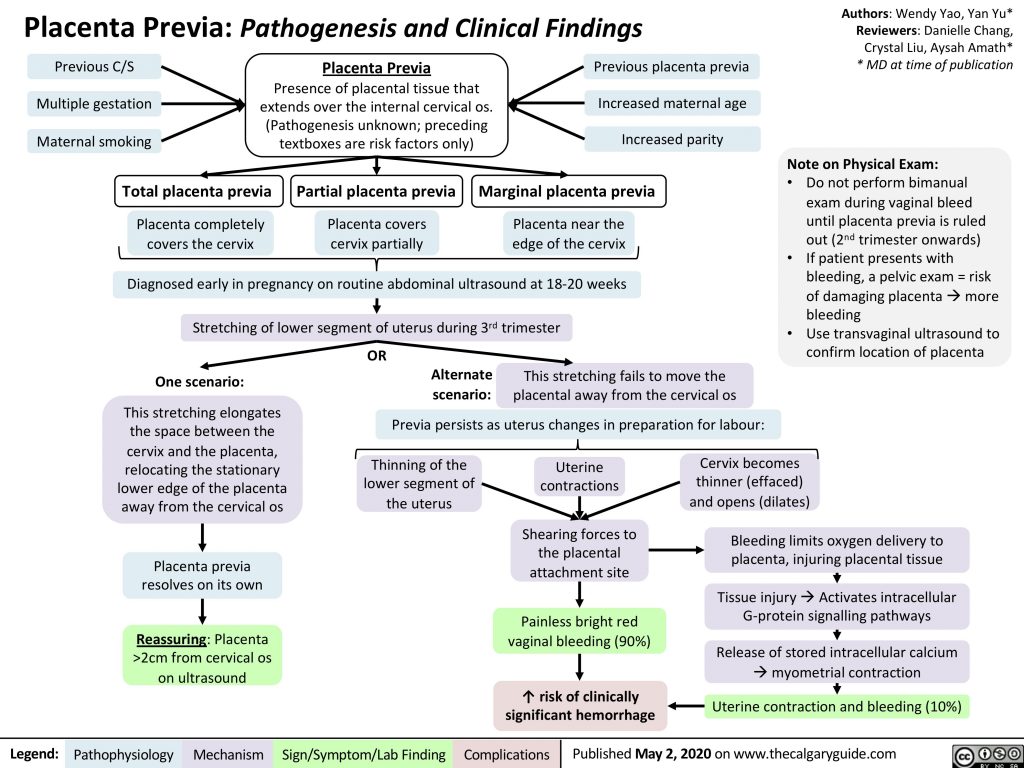
When the placenta is attached close to the opening of the uterus (cervix) or covers the cervix, it is called placenta previa. There are 3 types of placenta previa:
- Complete placenta previa. The placenta completely covers the cervix.
- Partial placenta previa. The placenta is partly over the cervix.
- Marginal placenta previa.
The placenta is near the edge of the cervix.
What causes placenta previa?
Researchers don't know what causes placenta previa. It is more likely to happen with certain conditions. These include:
- Past pregnancies
- Tumors (fibroids) in the uterus. These are not cancer.
- Past uterine surgeries or cesarean deliveries
- Woman who is older than 35
- Woman who is African American or of another nonwhite ethnic background
- Cigarette smoking
- Placenta previa in a past pregnancy
- Being pregnant with a boy
What are the symptoms of placenta previa?
The most common symptom of placenta previa is bright red, painless bleeding from the vagina. This is most common in the third trimester of pregnancy.
This is most common in the third trimester of pregnancy.
The symptoms of placenta previa may look like other health conditions. Make sure to see your healthcare provider for a diagnosis.
How is placenta previa diagnosed?
Your healthcare provider will ask about your health history. He or she will do a physical exam. The provider will also do an ultrasound. An ultrasound uses sound waves to make a picture of the organs. It can show where the placenta is and how much is covering the cervix. You may have a transvaginal ultrasound instead.
An ultrasound may show that a placenta is near the cervix in early pregnancy. But only a few women will develop true placenta previa. It is common for the placenta to move away from the cervix as the uterus grows.
How is placenta previa treated?
There is no treatment to change the position of the placenta. You may need:
- More ultrasounds to track where the placenta is
- Bed rest or hospital stay
- Early delivery of the baby. This will be based on how much bleeding you have, how far along your baby is, and how healthy the baby is.
- Cesarean section delivery
- Blood transfusion for severe blood loss
What are possible complications of placenta previa?
The greatest risk of placenta previa is too much bleeding (hemorrhage). Bleeding often happens as the lower part of the uterus thins during the third trimester of pregnancy. This causes the area of the placenta over the cervix to bleed.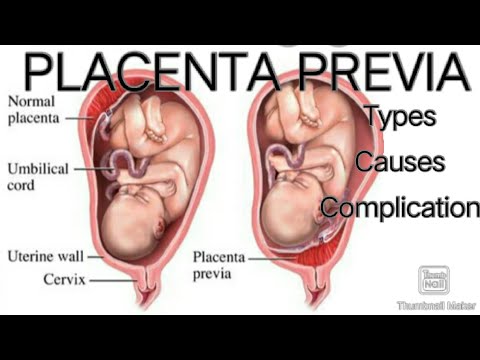 The risk of bleeding is higher if a lot of the placenta covers the cervix. Other complications include:
The risk of bleeding is higher if a lot of the placenta covers the cervix. Other complications include:
- Placenta doesn't attach to the uterus as it should
- Slowed growth of your baby in the uterus
- Preterm birth (before 37 weeks of pregnancy)
- Birth defects
When should I call my healthcare provider?
Call your healthcare provider about any bleeding you have while pregnant. Bleeding during pregnancy may not be serious. If the bleeding is moderate to severe, or you have pain, contact your healthcare provider right away.
Key points about placenta previa
- Placenta previa is a cause of bleeding late in pregnancy. This is after about 20 weeks.
- It causes bleeding because the placenta is close to or covers the cervix.
- Bleeding with placenta previa is painless.
- You may need bed rest or early delivery of your baby.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you.
 Also know what the side effects are.
Also know what the side effects are. - Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Medical Reviewer: Daniel N Sacks MD
Medical Reviewer: Donna Freeborn PhD CNM FNP
Medical Reviewer: Heather Trevino
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care.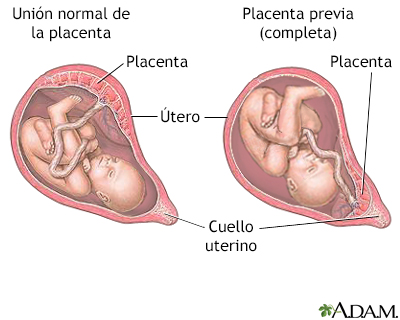 Always follow your healthcare professional's instructions.
Always follow your healthcare professional's instructions.
Placenta Previa
Ontology: Placenta Previa (C0032046)
| Definition (SNOMEDCT_US) | A condition in which the placenta is located over or near the internal os of the cervix, increasing the risk of hemorrhage. |
| Definition (SCTSPA) | Trastorno en el cual la placenta está ubicada sobre o en la proximidad del orificio interno del cuello uterino, con aumento del riesgo de hemorragia. |
| Definition (NCI) |
A condition in which the placenta covers or is within 1 cm of the cervical os. (NICHD) (NICHD)
|
| Definition (MSH) | Abnormal placentation in which the PLACENTA implants in the lower segment of the UTERUS (the zone of dilation) and may cover part or all of the opening of the CERVIX. It is often associated with serious antepartum bleeding and PREMATURE LABOR. |
| Concepts | Pathologic Function (T046) |
| MSH | D010923 |
| ICD10 | O44 |
| SnomedCT | 157059004, 198930005, 36813001 |
| French | PLACENTA PRAEVIA, Placenta praevia, Placenta previa |
| Portuguese | PLACENTA PREVIA, Placenta prévia, Placenta Prévia |
| Swedish | Placenta previa |
| English | PLACENTA PRAEVIA, placenta previa (diagnosis), placenta previa, placenta previa was observed, placenta previa (physical finding), Placenta Previa [Disease/Finding], previa placenta, placenta praevia, Placenta praevia (disorder), Placenta praevia, Placenta previa, PP - Placenta praevia, PP - Placenta previa, Placenta previa (disorder), placenta; previa, previa; placenta, Placenta previa, NOS, Placenta Praevia, Placenta Previa |
| Japanese | ゼンチタイバン, 前置胎盤, 胎盤-前置 |
| Czech | placenta praevia, Placenta praevia |
| Finnish | Etisistukka |
| Russian | PLATSENTY PREDLEZHANIE, ПЛАЦЕНТЫ ПРЕДЛЕЖАНИЕ |
| Italian | Placenta praevia, Placenta previa |
| Korean | 전치 태반 |
| Polish | Łożysko przodujące |
| Hungarian | Elölfekvő lepény, Placenta praevia |
| Norwegian | Placenta praevia, Forliggende morkake |
| Dutch | placenta; praevia, praevia; placenta, placenta praevia, Placenta praevia |
| Spanish | placenta previa (trastorno), placenta previa, Placenta previa, Placenta Previa |
| German | Plazenta praevia, Placenta praevia |
Placenta previa - symptoms, treatment, causes of the disease, first signs
Placenta previa - symptoms, treatment, causes of the disease, first signsHome
Directory of diseases
Placenta previa
Description
- Description
- Who treats
- Where to treat
Published: November 2, 2017
Photo: medaboutme.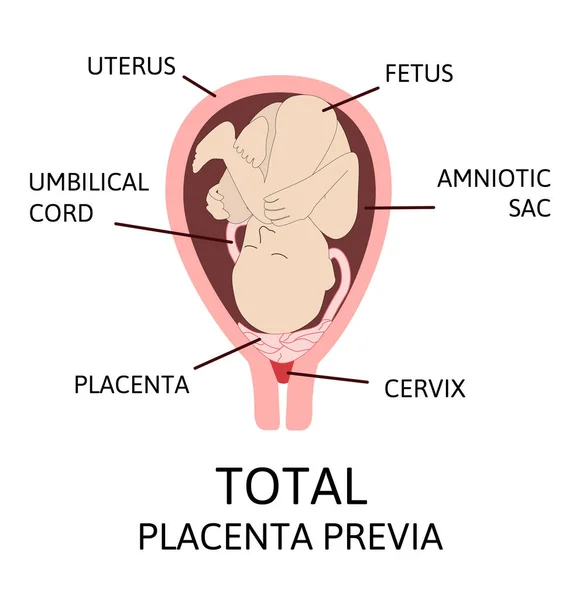 ru
ru
Description
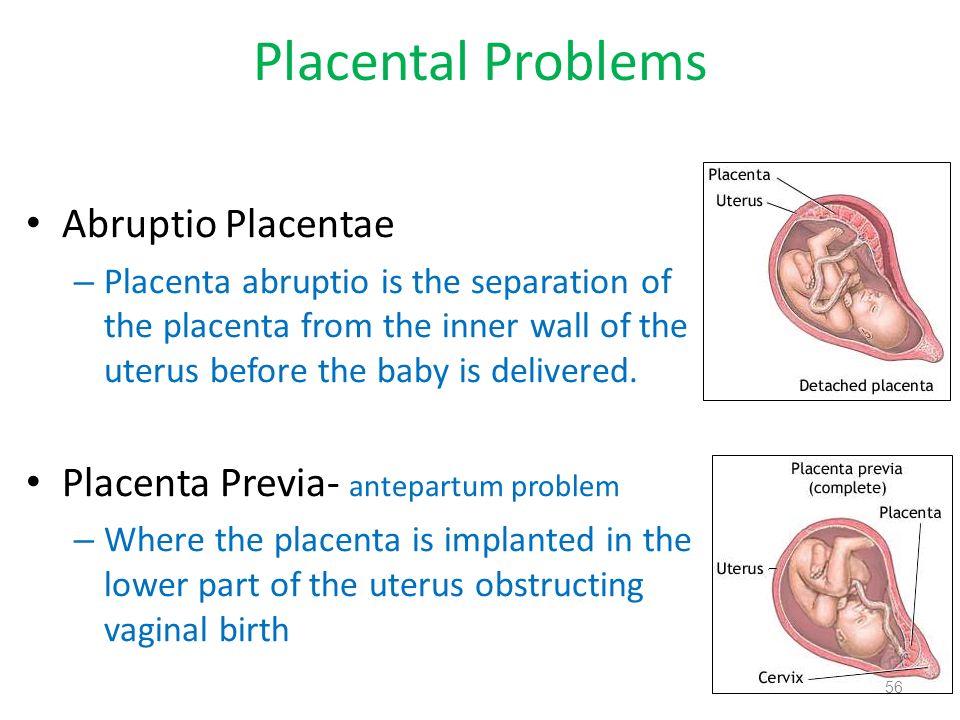
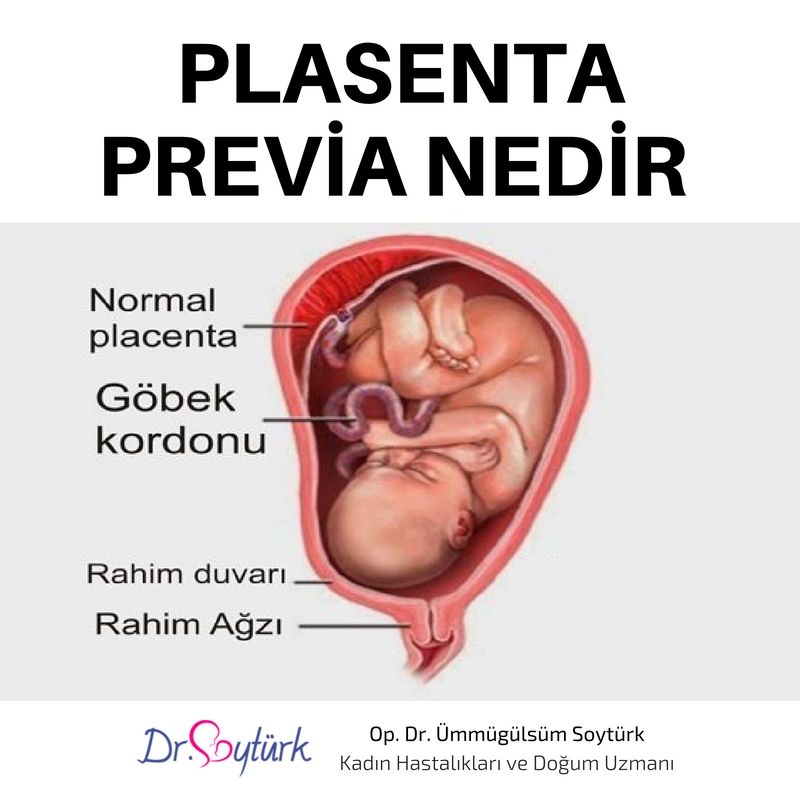
The placenta is part of the female body, thanks to which the normal course of pregnancy is possible. The successful bearing of a child and timely delivery depend on the correctness of its functioning and structure. With an incorrect location of this organ, a pathological placenta previa is diagnosed.
Structure and function
The structure of the placenta resembles a fleecy cloth. Within each villus are blood vessels. With each day of pregnancy, the number of villi increases, the vascular network expands. The fetus is connected to the placenta by the umbilical cord, with the help of which the exchange of substances between the body of the mother and the child takes place.
The placental layer forms with the onset of pregnancy and is considered fully formed at 16 weeks. It performs the following functions:
- provides the body of the fetus with the necessary nutrients, oxygen;
- displays the products of exchange;
- produces hormones necessary for normal development, fetal growth, and successful pregnancy.

Therefore, placenta previa and childbirth are closely related. Pathology can not only contribute to the deterioration of the fetus, but also cause complications during childbirth.
Types of placenta previa
Depending on the location, there are:
- Low presentation. The lower edge of the organ is located less than 6 cm from the exit from the uterus. The diagnosis established during the second trimester is not final. Since by the beginning of the third trimester, the placenta, as a rule, takes the right place due to stretching and pulling the tissues upward.
- Placenta previa proper. The diagnosis means that the organ is actually located in the way the baby exits the mother's pelvis.
Types of placenta previa are distinguished depending on the location. Exists:
- complete (central) placenta previa. The organ completely blocks the way to the exit from the uterus. Being in the lower part of the bottom, it covers the inner hole;
- partial.
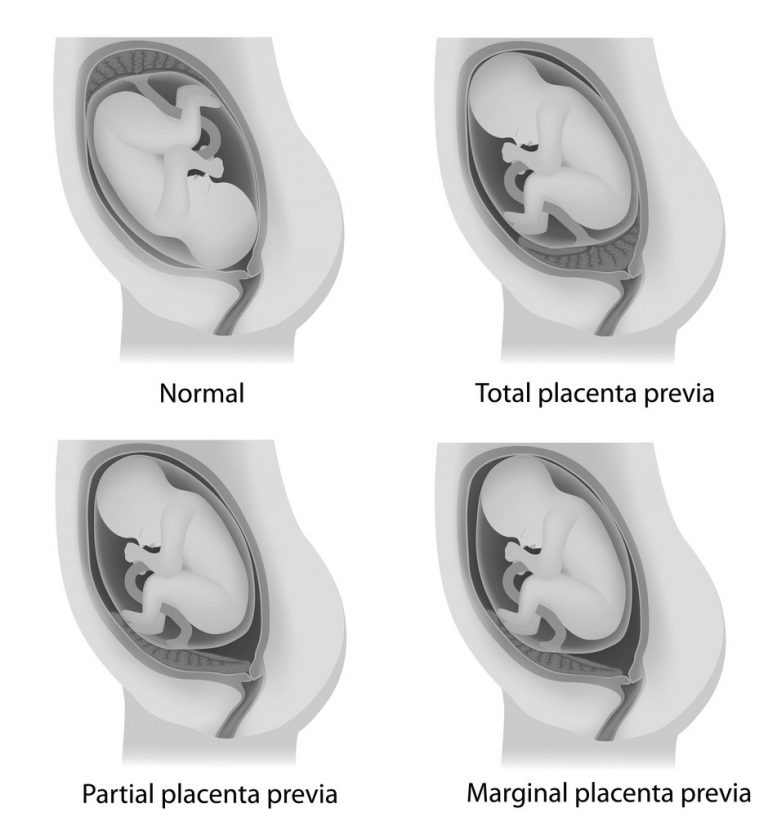 The placental tissue does not completely close the outlet. There are marginal (a third of the internal opening is closed by placental tissue) and lateral (2/3 of the exit is blocked) placenta previa.
The placental tissue does not completely close the outlet. There are marginal (a third of the internal opening is closed by placental tissue) and lateral (2/3 of the exit is blocked) placenta previa.
It is possible to diagnose a pathology and determine its type on ultrasound.
Causes of placenta previa
The main factor contributing to the development of pathology is a structural change in the inner wall of the uterus.
There are the following causes of placenta previa:
- Inflammatory processes of the female genital organs, in particular the uterus (changes in tissue structure as a result of abortion, medical curettage, the presence of genital infections, congenital anomalies of the structure, acquired defects due to surgical intervention, the growth of benign tumors).
- Diseases of the cardiovascular system, congestion in the small pelvis, impaired blood circulation lead to the fact that different parts of the walls of the uterus function differently.
- Second birth. According to statistics, multiparous people experience placenta previa more often than those who give birth for the first time. By the time of the second birth, a woman may have accumulated a list of gynecological diseases, which complicates the course of a subsequent pregnancy.
The cause of the pathology may be too low attachment of the fetal egg.
Placenta previa and childbirth
If the diagnosis is confirmed in the third trimester, there is a complete placenta previa, then, as a rule, a caesarean section is planned at 38 weeks of gestation. At an earlier stage, the operation is performed in the presence of profuse bleeding, recurring blood loss with the development of anemia, hypotension, deterioration of the mother and fetus.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
If you notice a mistake in the text, please highlight it and press Ctrl+Enter
Found error
Makarov I.
 O. • Placenta previa
O. • Placenta previa Ultrasound scanner HS70
Accurate and confident diagnosis. Multifunctional ultrasound system for examinations with expert diagnostic accuracy.
In the normal course of pregnancy, the placenta is usually located in the fundus or body of the uterus, along the back wall, with the transition to the side walls, i.e. in those areas where the walls of the uterus are best supplied with blood. On the anterior wall, the placenta is located somewhat less frequently, since the anterior wall of the uterus undergoes significantly more changes than the posterior one. In addition, the location of the placenta on the back wall protects it from accidental injury.
Placenta previa is a pathology in which the placenta is located in the lower parts of the uterus along any wall, partially or completely blocking the area of the internal os. The incidence of placenta previa averages from 0.1% to 1% of the total number of births.
If the placenta only partially covers the area of the internal pharynx, then it is an incomplete presentation, which occurs with a frequency of 70-80% of the total number of presentations. If the placenta completely covers the area of the internal os, then this is a complete placenta previa. This option occurs with a frequency of 20-30%.
If the placenta completely covers the area of the internal os, then this is a complete placenta previa. This option occurs with a frequency of 20-30%.
There is also a low location of the placenta, when its edge is at a lower level than it should be in the norm, but does not cover the area of the internal os.
Causes of low or low placenta
There are several reasons for low or low placenta. The most common causes are pathological changes in the inner layer of the uterus (endometrium) due to inflammation, surgical interventions (curettage, caesarean section, removal of myomatous nodes, etc.), multiple complicated births. In addition, violations of the attachment of the placenta can be caused by uterine fibroids, endometriosis, underdevelopment of the uterus, isthmicocervical insufficiency, inflammation of the cervix, multiple pregnancy. It should be noted that placenta previa is more common in re-pregnant women than in primiparas. Due to these factors, the fetal egg that enters the uterine cavity after fertilization cannot be implanted in the upper sections of the uterus in a timely manner, and this process is carried out only when the fetal egg has already descended into its lower sections.
The most common manifestation in placenta previa is recurrent bleeding from the genital tract. Bleeding can occur during various periods of pregnancy, starting from its earliest terms. However, most often they are observed already in the second half of pregnancy due to the formation of the lower segment of the uterus. In the last weeks of pregnancy, when uterine contractions become more intense, bleeding may increase.
Bleeding is caused by repeated abruption of the placenta, which is unable to stretch following the stretching of the uterine wall as pregnancy progresses or labor begins. In this case, the placenta partially exfoliates, and bleeding occurs from the vessels of the uterus. The fetus does not shed blood. However, he is threatened by oxygen starvation, since the exfoliated part of the placenta is not involved in gas exchange.
Provoking factors for bleeding during pregnancy can be: physical activity, sudden coughing, vaginal examination, sexual intercourse, increased intra-abdominal pressure with constipation, thermal procedures (hot bath, sauna).
With complete placenta previa, bleeding often occurs suddenly, without pain, and can be very heavy. Bleeding may stop, but reappear after some time, or may continue in the form of scanty discharge. In the last weeks of pregnancy, bleeding resumes and / or increases.
With incomplete placenta previa, bleeding may begin at the very end of pregnancy. However, more often it occurs at the beginning of labor. The amount of bleeding depends on the size of the placenta previa. The more placental tissue is present, the earlier and more bleeding begins.
Recurrent bleeding during pregnancy complicated by placenta previa in most cases leads to the development of anemia.
Pregnancy with placenta previa is often complicated by the threat of miscarriage, which is due to the same reasons as the occurrence of an incorrect location of the placenta. Preterm labor most often occurs in patients with complete placenta previa.
Pregnant women with placenta previa are characterized by low blood pressure, which occurs in 25%-34% of cases.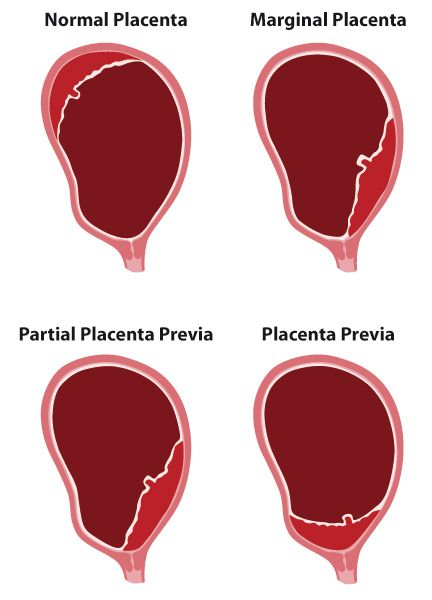
Preeclampsia (nephropathy, late toxicosis) is also no exception for pregnant women with placenta previa. This complication, which occurs against the background of dysfunction of a number of organs and systems, as well as with symptoms of blood clotting disorders, significantly worsens the nature of recurrent bleeding.
Placenta previa is often accompanied by fetal placental insufficiency, lack of oxygen for the fetus and delayed development. The exfoliated part of the placenta is switched off from the general system of the uteroplacental circulation and does not participate in gas exchange. With placenta previa, an incorrect position of the fetus (oblique, transverse) or breech presentation is often formed, which in turn are accompanied by certain complications.
In obstetric practice, the term "migration of the placenta" is widely rooted, which, in fact, does not reflect the real essence of what is happening. The change in the location of the placenta is carried out due to a change in the structure of the lower segment of the uterus during pregnancy and the direction of growth of the placenta towards a better blood supply to the sections of the uterine wall (towards the bottom of the uterus) compared to its lower sections. A more favorable prognosis in terms of placental migration is noted when it is located on the anterior wall of the uterus. Usually the process of "migration of the placenta occurs within 6-10 weeks and is completed by the middle of 33-34 weeks of pregnancy.
A more favorable prognosis in terms of placental migration is noted when it is located on the anterior wall of the uterus. Usually the process of "migration of the placenta occurs within 6-10 weeks and is completed by the middle of 33-34 weeks of pregnancy.
Diagnosis of placenta previa
Placenta previa is not difficult to detect. The presence of placenta previa may be indicated by complaints of a pregnant woman about bleeding. In this case, recurrent bleeding from the second half of pregnancy, as a rule, is associated with complete placenta previa. Bleeding at the end of pregnancy or at the beginning of labor is more often associated with incomplete placenta previa.
In the presence of bleeding, carefully examine the walls of the vagina and cervix using speculums to exclude trauma or pathology of the cervix, which may also be accompanied by the presence of bloody discharge.
A vaginal examination of a pregnant woman also easily reveals clear diagnostic signs indicating an abnormal location of the placenta. However, such a study must be performed as carefully as possible, in compliance with all the necessary rules to prevent possible bleeding.
However, such a study must be performed as carefully as possible, in compliance with all the necessary rules to prevent possible bleeding.
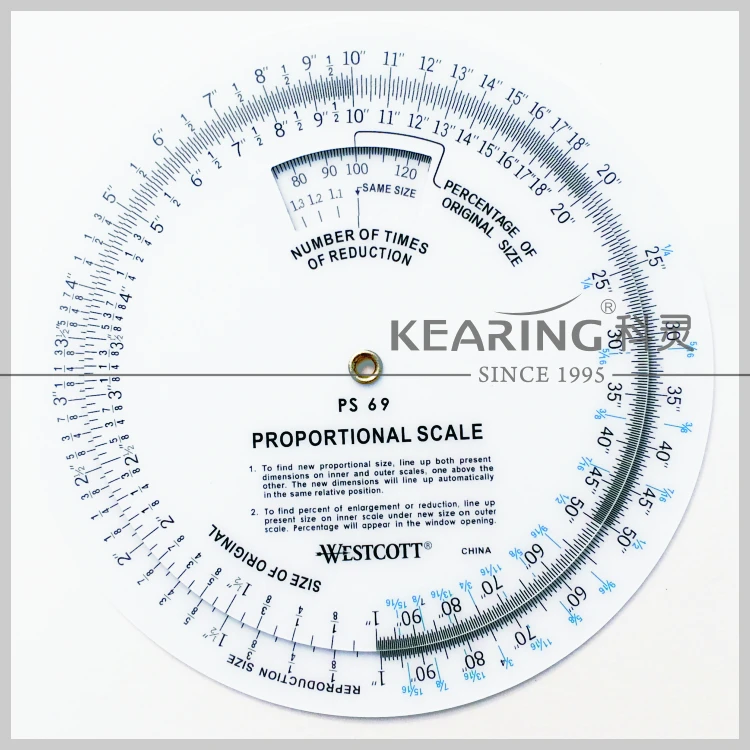
Currently, the most objective and safest method for diagnosing placenta previa is ultrasound, which allows you to establish the fact of placenta previa and the variant of placenta previa (complete, incomplete), determine the size, structure and area of the placenta, assess the degree of detachment, as well as get an accurate picture of the migration of the placenta.
If the ultrasound revealed a complete placenta previa, then a vaginal examination should not be performed at all. The criterion for the low location of the placenta in the III trimester of pregnancy (28 - 40 weeks) is the distance from the edge of the placenta to the area of the internal os 5 cm or less. Placenta previa is indicated by the presence of placental tissue in the area of the internal os.
The nature of the localization of the placenta in the II and III trimesters of pregnancy (up to 27 weeks) is judged by the ratio of the distance from the edge of the placenta to the area of the internal os, with the diameter value (BDP) of the fetal head.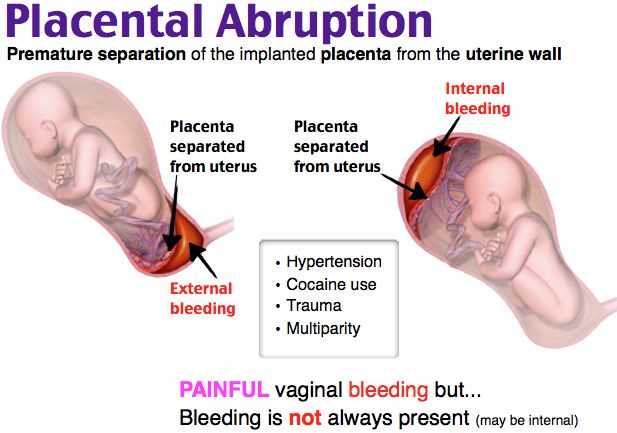
If an abnormal location of the placenta is detected, a dynamic study should be carried out to monitor its "migration". For these purposes, it is advisable to perform at least three echographic controls during pregnancy at 16, 24-26 and 34-36 weeks.
Ultrasound should be done when the bladder is moderately full. With the help of ultrasound, it is also possible to determine the presence of an accumulation of blood (hematoma) between the placenta and the wall of the uterus during placental abruption (in the event that there was no outflow of blood from the uterine cavity). If the site of placental abruption occupies no more than 1/4 of the area of the placenta, then the prognosis for the fetus is relatively favorable. In the event that the hematoma occupies more than 1/3 of the area of the placenta, then most often this leads to the death of the fetus.
Medical support for pregnant women with placenta previa
The nature of management and treatment of pregnant women with placenta previa depends on the severity of bleeding and the amount of blood loss.
In the first half of pregnancy, if there are no blood discharges, then the pregnant woman can be at home under outpatient control in compliance with the regime that excludes the action of provoking factors that can cause bleeding (restriction of physical activity, sexual activity, stressful situations, etc.)
Observation and treatment for more than 24 weeks of pregnancy is carried out only in an obstetric hospital.
Treatment aimed at continuing the pregnancy up to 37-38 weeks is possible if the bleeding is not heavy, and the general condition of the pregnant woman and the fetus is satisfactory. Even despite the cessation of bloody discharge from the genital tract, pregnant women with placenta previa can under no circumstances be discharged from the hospital before delivery.
Management of pregnant women in an obstetric hospital provides for: observance of strict bed rest; the use of drugs that ensure the optimization of the normalization of contractile activity; treatment of anemia and fetal placental insufficiency.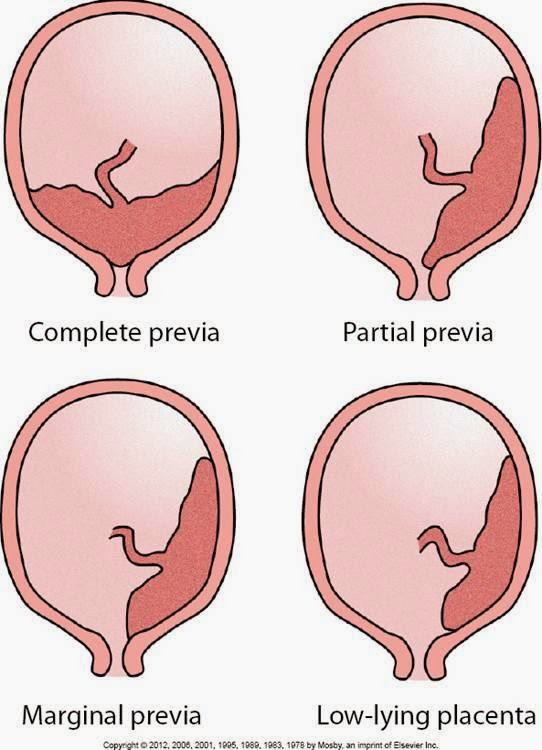
Emergency caesarean section, regardless of gestational age, is indicated for: recurrent bleeding; a combination of small blood loss with anemia and a decrease in blood pressure; simultaneous profuse blood loss; complete placenta previa and bleeding.
The operation is performed according to vital indications on the part of the mother, regardless of the duration of pregnancy and the condition of the fetus.
In the event that the pregnancy has been carried to 37-38 weeks and placenta previa persists, depending on the situation, the most optimal method of delivery is chosen on an individual basis.
The absolute indication for elective caesarean section is placenta previa. Childbirth through the natural birth canal in this situation is impossible, since the placenta that covers the internal os does not allow the presenting part of the fetus (fetal head or pelvic end) to be inserted into the pelvic inlet. In addition, in the process of increasing uterine contractions, the placenta will exfoliate more and more, and the bleeding will increase significantly.
In case of incomplete placenta previa and in the presence of concomitant complications (breech presentation, incorrect position of the fetus, scar on the uterus, multiple pregnancy, severe polyhydramnios, narrow pelvis, age of the primiparous over 30 years, etc.), a caesarean section should also be performed in a planned manner.
If the above associated complications are absent and there is no blood discharge, then you can wait until the onset of spontaneous labor activity, followed by early opening of the fetal bladder. In the event that after opening the fetal bladder, bleeding nevertheless began, then it is necessary to resolve the issue of performing a caesarean section.
If, with incomplete placenta previa, bleeding occurs before the onset of labor, then the fetal bladder is opened. The necessity and expediency of this procedure is due to the fact that when the membranes are opened, the fetal head is inserted into the entrance to the pelvis and presses the exfoliated part of the placenta against the wall of the uterus and pelvis, which helps to stop further placental abruption and stop bleeding. If bleeding after opening the fetal bladder continues and / or the cervix is immature, then a caesarean section is performed. In the case of stopping bleeding, it is possible to conduct labor through the natural birth canal (with a favorable obstetric situation).
Bleeding can also begin in the early stages of labor, from the moment of the first contractions. In this case, early opening of the fetal bladder is also shown.
Thus, the management of childbirth with incomplete placenta previa through the natural birth canal is possible if: the bleeding stopped after opening the fetal bladder; mature cervix; labor activity is good; there is a cephalic presentation of the fetus.
However, caesarean section is one of the most frequently chosen methods of delivery by obstetricians in placenta previa and is performed with a frequency of 70% -80% in this pathology.
Other typical complications in childbirth with incomplete placenta previa are weakness of labor and insufficient oxygen supply to the fetus (fetal hypoxia).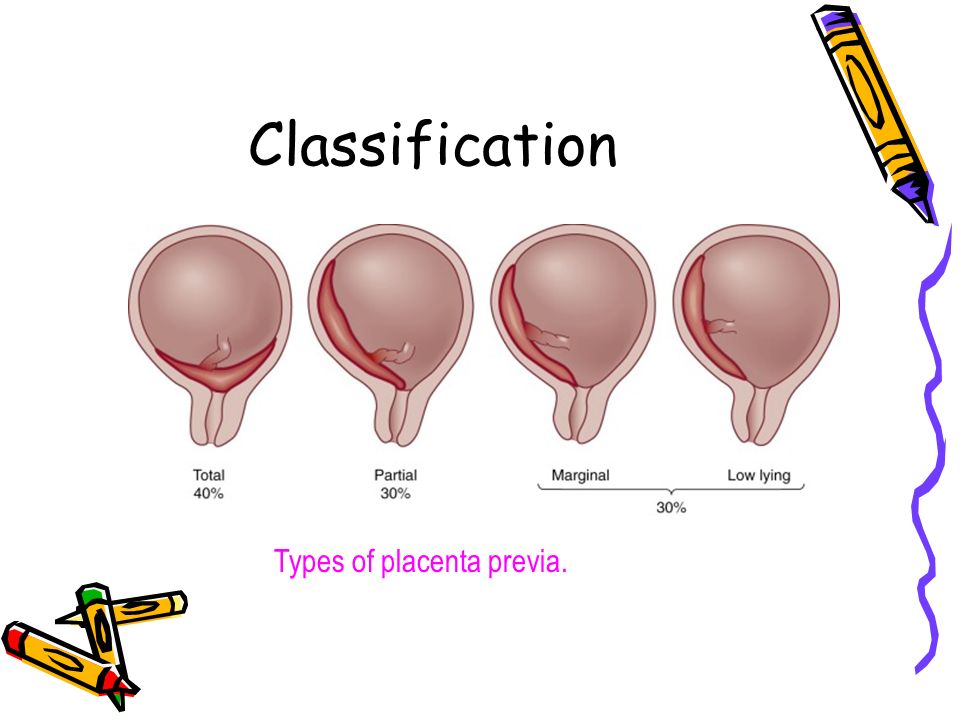
_c53bbd6a-f309-45f6-b20e-2eb8914f5c67-eeeb18.jpg)



.jpg)




