Anatomy of fetus in womb
Anatomy of pregnancy and birth - uterus
Anatomy of pregnancy and birth - uterus | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What does the uterus look like?
One of the most recognised changes in a pregnant woman’s body is the appearance of the ‘baby bump’, which forms to accommodate the baby growing in the uterus. The primary function of the uterus during pregnancy is to house and nurture your growing baby, so it is important to understand its structure and function, and what changes you can expect the uterus to undergo during pregnancy.
The uterus (also known as the ‘womb’) has a thick muscular wall and is pear shaped. It is made up of the fundus (at the top of the uterus), the main body (called the corpus), and the cervix (the lower part of the uterus ). Ligaments – which are tough, flexible tissue – hold it in position in the middle of the pelvis, behind the bladder, and in front of the rectum.
The uterus wall is made up of 3 layers. The inside is a thin layer called the endometrium, which responds to hormones – the shedding of this layer causes menstrual bleeding. The middle layer is a muscular wall. The outside layer of the uterus is a thin layer of cells.
Illustration showing the female reproductive system.The size of a non-pregnant woman's uterus can vary. In a woman who has never been pregnant, the average length of the uterus is about 7 centimetres. This increases in size to approximately 9 centimetres in a woman who is not pregnant but has been pregnant before. The size and shape of the uterus can change with the number of pregnancies and with age.
How does the uterus change during pregnancy?
During pregnancy, as the baby grows, the size of a woman’s uterus will dramatically increase. One measure to estimate growth is the fundal height, the distance from the pubic bone to the top of the uterus. Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Fundal height can vary from person to person, and many factors can affect the size of a pregnant woman’s uterus. For instance, the fundal height may be different in women who are carrying more than one baby, who are overweight or obese, or who have certain medical conditions. A full bladder will also affect fundal height measurement, so it’s important to empty your bladder before each measurement. A smaller than expected fundal height could be a sign that the baby is growing slowly or that there is too little amniotic fluid. If so, this will be monitored carefully by your doctor. In contrast, a larger than expected fundal height could mean that the baby is larger than average and this may also need monitoring.
As the uterus grows, it can put pressure on the other organs of the pregnant woman's body. For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
How does the uterus prepare for labour and birth?
Braxton Hicks contractions, also known as 'false labour' or 'practice contractions', prepare your uterus for the birth and may start as early as mid-way through your pregnancy, and continuing right through to the birth. Braxton Hicks contractions tend to be irregular and while they are not generally painful, they can be uncomfortable and get progressively stronger through the pregnancy.
During true labour, the muscles of the uterus contract to help your baby move down into the birth canal. Labour contractions start like a wave and build in intensity, moving from the top of the uterus right down to the cervix. Your uterus will feel tight during the contraction, but between contractions, the pain will ease off and allow you to rest before the next one builds. Unlike Braxton Hicks, labour contractions become stronger, more regular and more frequent in the lead up to the birth.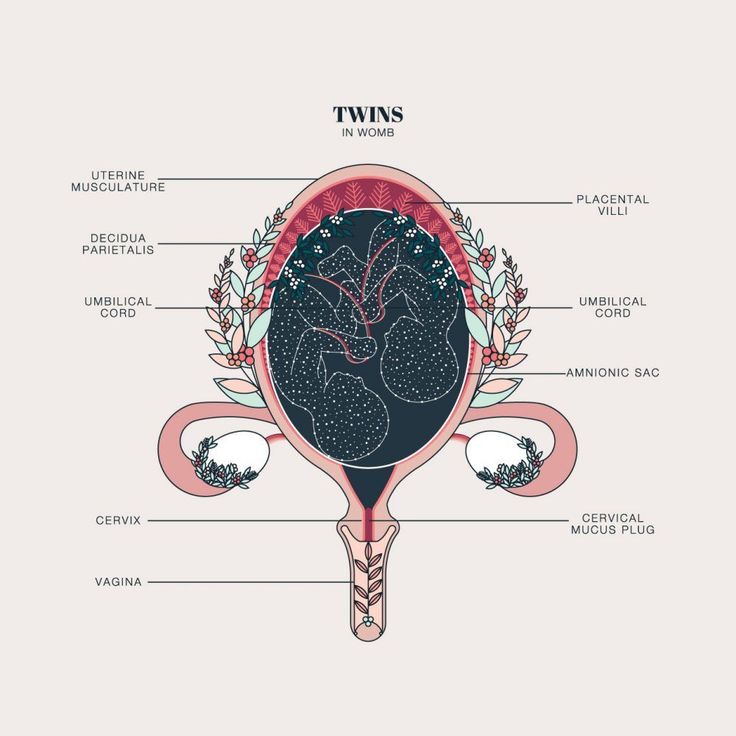
How does the uterus change after birth?
After the baby is born, the uterus will contract again to allow the placenta, which feeds the baby during pregnancy, to leave the woman’s body. This is sometimes called the ‘after birth’. These contractions are milder than the contractions felt during labour. Once the placenta is delivered, the uterus remains contracted to help prevent heavy bleeding known as ‘postpartum haemorrhage‘.
The uterus will also continue to have contractions after the birth is completed, particularly during breastfeeding. This contracting and tightening of the uterus will feel a little like period cramps and is also known as 'afterbirth pains'.
Read more here about the first few days after giving birth.
Sources:
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), StatPearls Publishing (Anatomy, Abdomen and Pelvis), Department of Health (Clinical practice guidelines: Pregnancy care), Better Health Channel Victoria (Pregnancy stages and changes), Mater Mother's Hospital (Labour and birth information), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (The First Few Weeks Following Birth), Queensland Health (Queensland Clinical Guidelines – maternity and neonatal), King Edward Memorial Hospital (Fundal height: Measuring with a tape measure), Royal Hospital for Women (Fetal growth assessment (clinical) in pregnancy), MSD Manual (Female internal genital organs)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Anatomy of pregnancy and birth - perineum and pelvic floor
- Anatomy of pregnancy and birth - pelvis
- Anatomy of pregnancy and birth - cervix
- Anatomy of pregnancy and birth - abdominal muscles
- Anatomy of pregnancy and birth
Need more information?
Prolapsed uterus - Better Health Channel
The pelvic floor and associated supporting ligaments can be weakened or damaged in many ways, causing uterine prolapse.
Read more on Better Health Channel website
Uterus, cervix & ovaries - fact sheet | Jean Hailes
This fact sheet discusses some of the health conditions that may affect a woman's uterus, cervix and ovaries.
Read more on Jean Hailes for Women's Health website
Dilatation and curettage (D&C)
A D&C is an operation to lightly scrape the inside of the uterus (womb).
Read more on WA Health website
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilised egg implants outside the uterus (womb)
Read more on WA Health website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Pelvic Floor | Family Planning NSW
The pelvic floor is a group of muscles in the pelvic area that support the bladder, bowel and uterus (womb).
Read more on Family Planning NSW website
Mirena IUD | Hormonal IUD Mirena | IUD Mirena insertion | IUD Mirena cost | Mirena IUD Melbourne - Sexual Health Victoria
The hormonal intrauterine device (IUD) is a small contraceptive device that is put into the uterus (womb) to prevent pregnancy.
Read more on Sexual Health Victoria website
Endometriosis | Your Fertility
Endometriosis is a condition where the tissue that lines the uterus also grows in other areas of the body
Read more on Your Fertility website
Pelvic Floor Muscle Damage - Birth Trauma
The pelvic floor muscles are a supportive basin of muscle attached to the pelvic bones by connective tissue to support the vagina, uterus, bladder and bowel.
Read more on Australasian Birth Trauma Association website
What is Ectopic Pregnancy? | Ectopic Pregnancy Symptoms | How do I know if I have had an Ectopic Pregnancy? | Ectopic Pregnancy Treatment - Sexual Health Victoria
Ectopic pregnancy is a pregnancy that develops outside the uterus, usually in one of the fallopian tubes. In almost all cases, the embryo dies.
Read more on Sexual Health Victoria website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.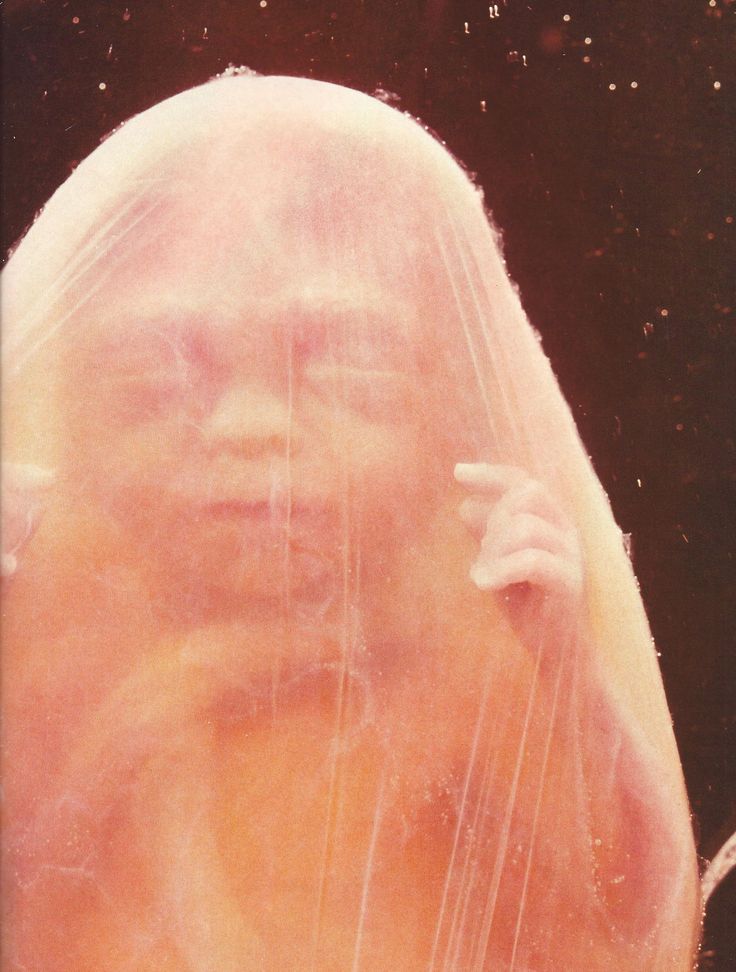
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.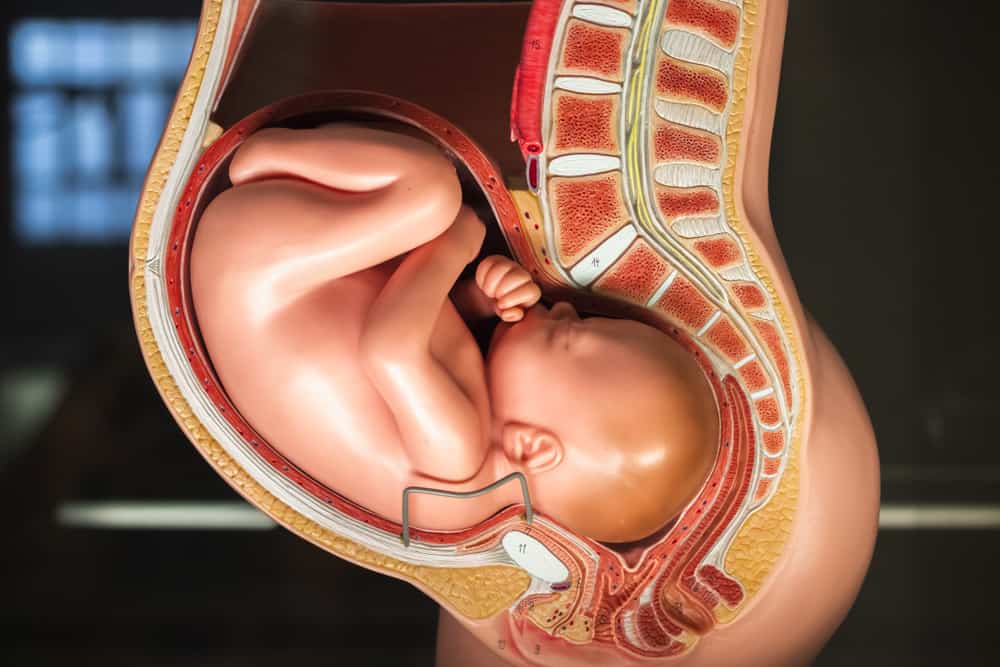
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
The Anatomy Ultrasound: Everything You Should Know
Halfway through your pregnancy, you will experience one of my favorite parts of pregnancy: the anatomy scan. The anatomy scan is a level 2 ultrasound, which is typically performed between 18 and 22 weeks. Other than finding out the sex of your baby (if you want to know), the ultrasound technician will be taking many measurements of your baby.
Since the technician will be concentrating on the screen, they may or may not talk you through the examination. Don’t be afraid to ask questions, though. I find that it’s best to go in with an idea of what the technician will be looking for specifically and a written list of questions.
Brain
The technician will be assessing the fluid-filled spaces inside the brain and the shape of the cerebellum, which is in the back of the brain. He or she will also be able to identify if any cysts are in the choroid plexus, which is a tissue in the brain that produces cerebrospinal fluid. Fetal cysts may indicate an increased risk for a chromosome abnormality; however, the majority of these cysts disappear by the 28th week of pregnancy with no effect on the baby.
Face
Depending on the positioning of your baby, the technician may or may not be able to detect if your baby has a cleft lip. Rarely are they able to detect if there is a cleft of the palate.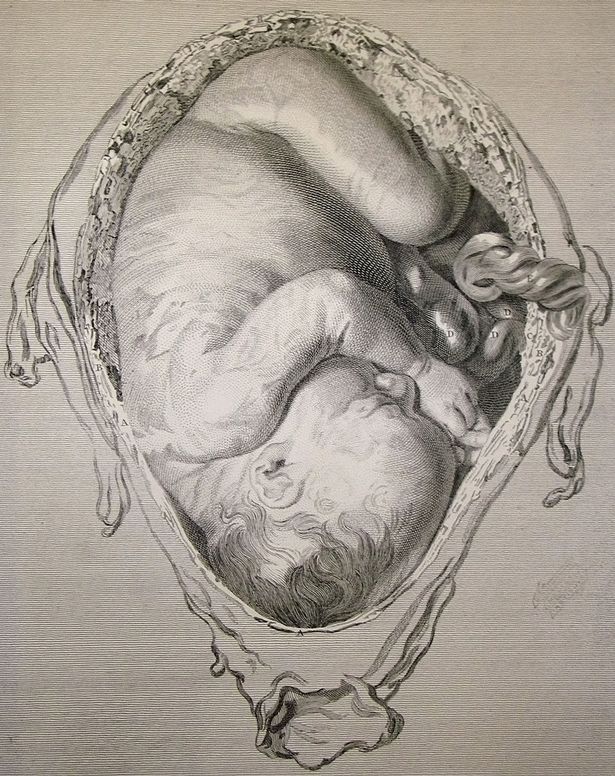 According to The Cleft Palate Foundation, clefts of the lip and palate are the fourth most common birth defect, affecting 1 out of every 600 newborns in the US.
According to The Cleft Palate Foundation, clefts of the lip and palate are the fourth most common birth defect, affecting 1 out of every 600 newborns in the US.
Due to the number of oral health and medical problems associated with a cleft lip or palate, a team of doctors and other specialists will be involved in the care of your baby after birth. If it is determined that your baby does have a cleft lip during the ultrasound, it is helpful to research facilities that can provide the medical treatment your baby will need prior to birth.
Heart
Congenital Heart Defects are one of the leading causes of birth defects and infant death. A prenatal diagnosis can prepare you and your medical team to provide your infant with the best medical care possible throughout your pregnancy and after birth. Here are the important questions you will want to ask your technician:
- Do you see four chambers?
- Do you look at the arteries or outflow tracts as part of your scan?
- Are the heart and stomach in correct positions? Both organs should lay on the left side of the fetus.
- Is the heart rate normal? A normal heart rate range for a fetus is 120-180 beats per minute.
- Is the heart function normal?
- Does the muscle work normally?
- Is everything hooked-up correctly?
Spine
Your baby’s spine will be evaluated in the long view and in a cross section. The technician will be looking to make sure that the vertebrae are in alignment and that the skin covers the spine at the back.
Other Major Organs
The scan will also evaluate your baby’s stomach, abdominal wall, and diaphragm. The scan will determine if your baby has two kidneys and if his or her bladder is functioning properly.
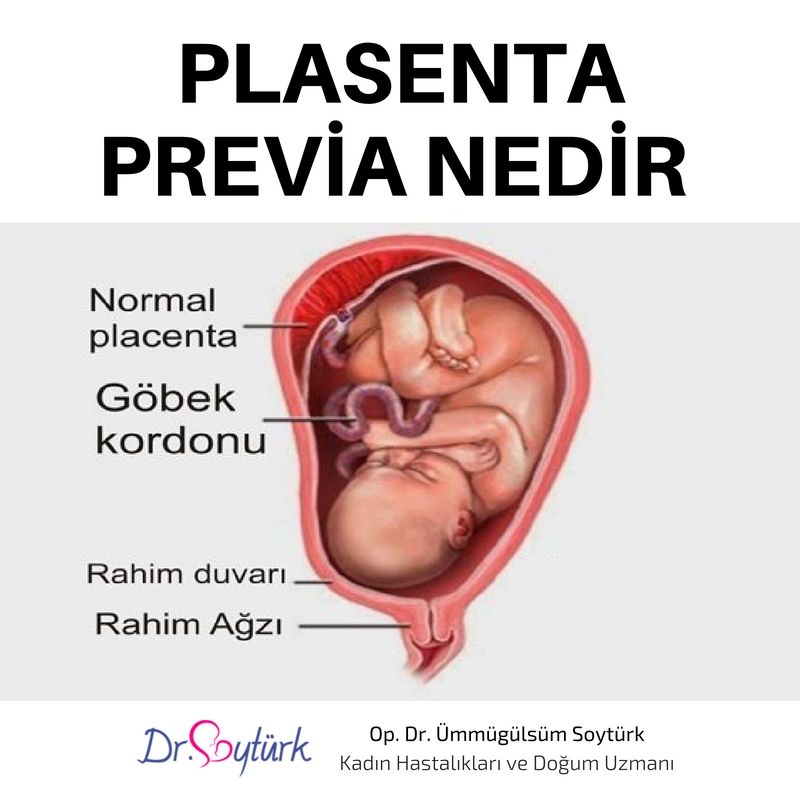
Mom’s Anatomy
The technician will look at the positioning of your placenta, specifically looking for placenta previa. The umbilical cord will be checked to determine if it enters the abdomen normally and that it has three vessels. The technician will also look to see if there is enough amniotic fluid surrounding the baby to allow it to move freely at this stage.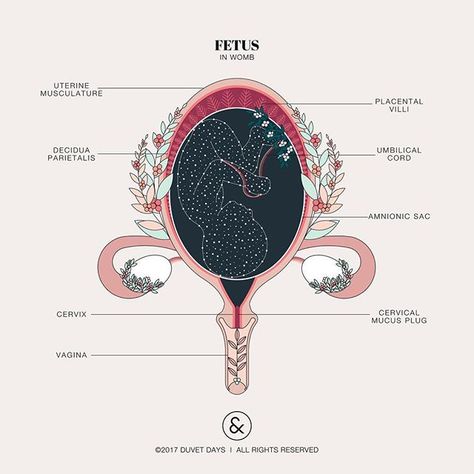
This may seem like a lot of scary information, but it is better to be informed and involved in the examination instead of completely unprepared. The anatomy scan really is an exciting examination, where you are able to get a close-up glimpse of your little one moving around. Enjoy the special moment!
Fetal anatomy screening
Fetal anatomy screening is one of the most important ultrasound examinations during pregnancy. This study is carried out using a transabdominal probe at the 20-21st week of pregnancy. By this time, all organs have developed in the fetus and the period of growth and maturation begins. At the 20th week of pregnancy, almost half of the pregnancy is over and half is still ahead. At this time, the fetus weighs 300-350 g, its length is 21-22 cm.
The fetus already looks like a baby, but does not yet know how to smile, because the mimic muscles of the face are not yet developed. The fetus already opens its mouth , swallows and inhales amniotic fluid, smells and tastes it.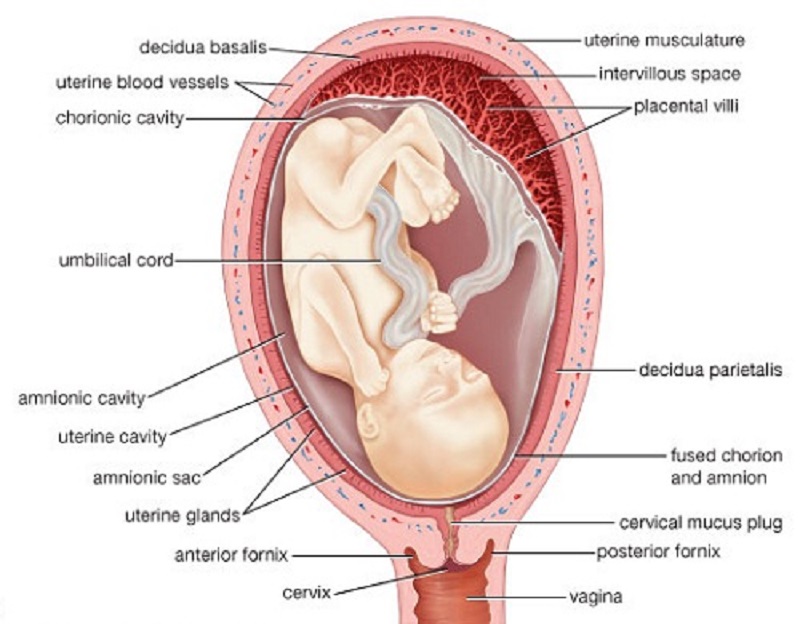 The inner ear has already developed so that it hears the sounds coming from the womb - the beating of the mother's heart, breath sounds in the lungs, bowel movements. However, he is not yet able to distinguish sounds coming from outside: for example, the voice of his father. The baby's skin is covered with fluff and fetal lubrication, which protect it from the macerating action of amniotic fluid. The fetus already has eyebrows and formed eyelids, but the eyes are still covered with embryonic film, so he cannot open them yet. The fetus does not have hair and eyelashes, but nails are already beginning to form on the fingers and toes.
The inner ear has already developed so that it hears the sounds coming from the womb - the beating of the mother's heart, breath sounds in the lungs, bowel movements. However, he is not yet able to distinguish sounds coming from outside: for example, the voice of his father. The baby's skin is covered with fluff and fetal lubrication, which protect it from the macerating action of amniotic fluid. The fetus already has eyebrows and formed eyelids, but the eyes are still covered with embryonic film, so he cannot open them yet. The fetus does not have hair and eyelashes, but nails are already beginning to form on the fingers and toes.
The fetal heart is already the size of a one euro coin and beats at a frequency of 120-160 times per minute - twice as fast as the mother's heart, or in other words, like the mother's and father's hearts combined.
Fetal ultrasound evaluates the size and structure of the placenta, attachment of the umbilical cord to the placenta.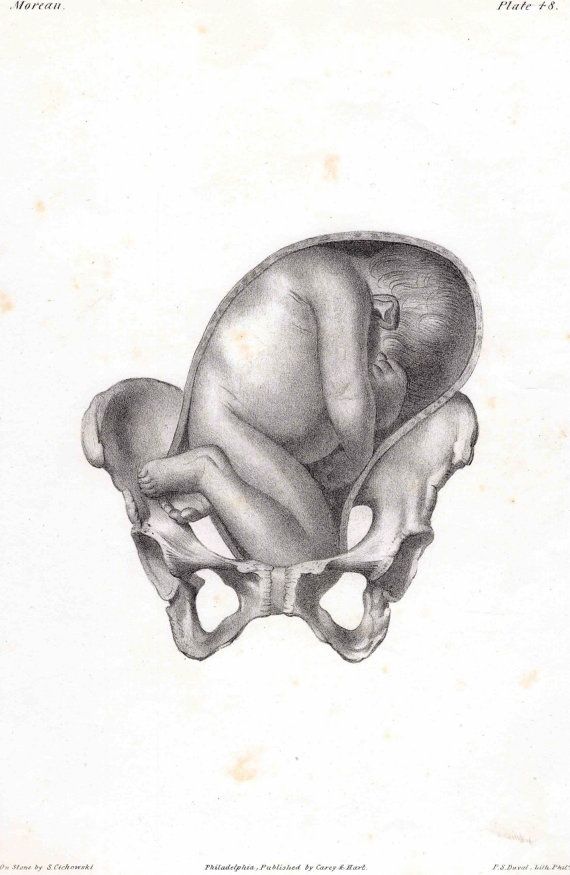 It is important to assess whether the lower part of the placenta overlaps the cervix, which in the future may
It is important to assess whether the lower part of the placenta overlaps the cervix, which in the future may
interfere with the birth of a child.
The amount of amniotic fluid is assessed, whether it is too little or too much. Measuring the size of the skull, the girth of the abdomen and the length of the femur allows you to estimate the size of the child and clarify the date of birth.
It is very important to examine and evaluate the structure of the fetal organs in detail: the skull must be intact, the sutures and fontanelles of the skull bones must be open so that the fetal brain tissue can grow unhindered. Brain structures and their correspondence to the gestational age are assessed.
Pay attention to the fetal eyes and interocular distance. The integrity of the child's upper lip is assessed so that in the future he has a beautiful smile. The lower jaw of the fetus is examined to assess whether the baby will be able to suckle later.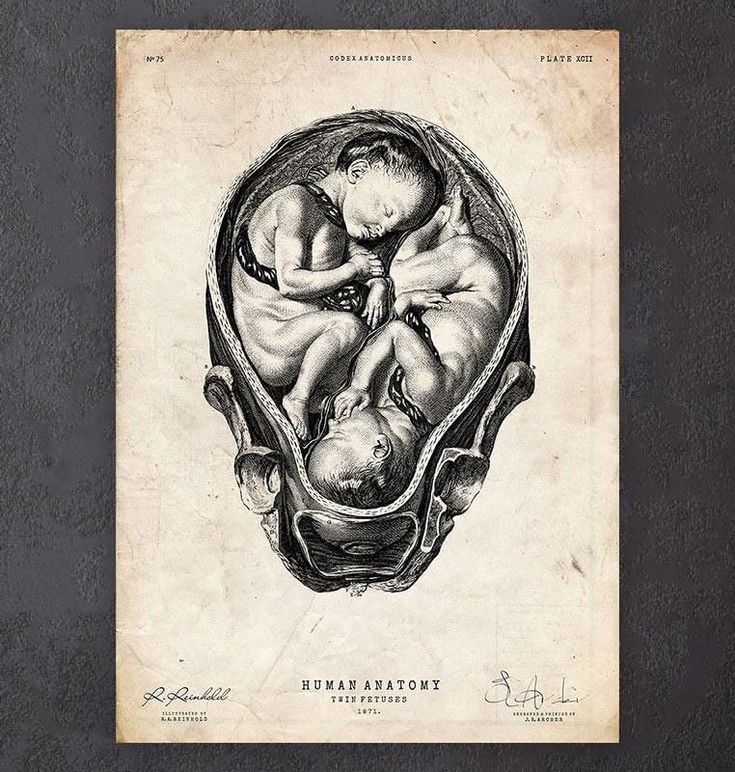
Look for ultrasound abnormalities characteristic of chromosomal disorders. Pay attention to the integrity of the spine and the anterior abdominal wall of the fetus, as well as to the umbilical cord coming from the abdomen.
The integrity of the fetal arms and legs, their position and movement are assessed. The fetus bends and stretches the arms and legs, already knows how to compress and unclench the fists. Pay attention to the presence of kidneys and their structure, their function is assessed, as well as the fullness of the bladder and the presence of umbilical arteries surrounding the bladder. Pay attention to whether the fetus swallows, whether the stomach is located on the same side as the heart (left), and whether it is full.
Particular attention is paid to the structure of the fetal heart: the heart must have four chambers from which the corresponding large vessels originate, the fetal cardiac activity must be regular.
If there is an increased risk of preterm birth (twin pregnancy, uterine anomalies, previous preterm birth, cervical surgery), the transvaginal probe can measure the length of the cervix and, based on this, assess the risk of preterm birth.
In the second trimester, fetal anatomy screening may reassess the risk of preeclampsia obtained from OSCAR or recommend screening for preeclampsia in women who were not assessed for risk by OSCAR.
At the request of the family, the sex of the child can also be determined during this ultrasound examination.
At the end of the ultrasound examination, the family is introduced to its results and explained in detail the nature and causes of possible deviations and their prognosis for the fetus.
It is important to know that most children develop and are born healthy.
Video: Fetal anatomy screening. Dr. Marek Scheus
Child development by week | Regional Perinatal Center
Expectant mothers are always curious about how the fetus develops at a time when it is awaited with such impatience.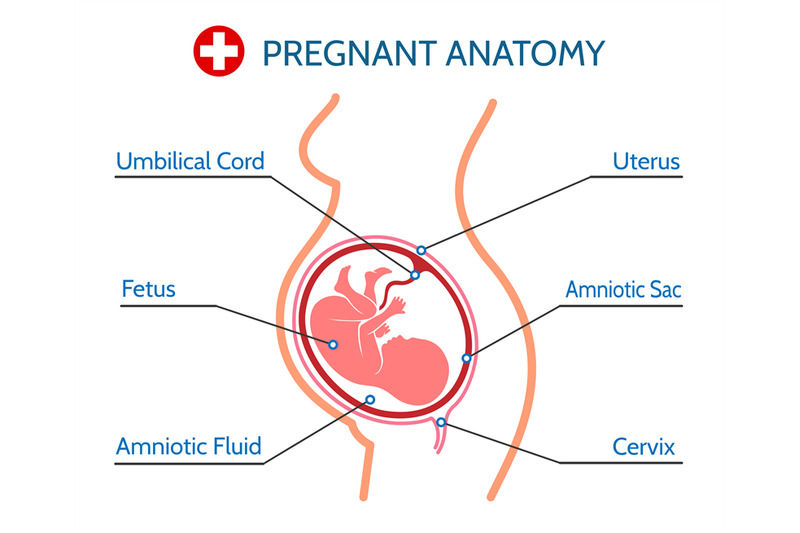 Let's talk and look at the photos and pictures of how the fetus grows and develops week by week.
Let's talk and look at the photos and pictures of how the fetus grows and develops week by week.
What does the puffer do for 9 whole months in mom's tummy? What does he feel, see and hear?
Let's start the story about the development of the fetus by weeks from the very beginning - from the moment of fertilization. A fetus up to 8 weeks old is called embryo , this occurs before the formation of all organ systems.
Embryo development: 1st week
The egg is fertilized and begins to actively split. The ovum travels to the uterus, freeing itself from the membrane along the way.
On the 6th-8th days, implantation of eggs is carried out - introduction into the uterus. The egg settles on the surface of the uterine mucosa and, using the chorionic villi, attaches to the uterine mucosa.
Embryo development: 2-3 weeks
Picture of embryo development at 3 weeks.
The embryo is actively developing, starting to separate from the membranes. At this stage, the beginnings of the muscular, skeletal and nervous systems are formed. Therefore, this period of pregnancy is considered important.
At this stage, the beginnings of the muscular, skeletal and nervous systems are formed. Therefore, this period of pregnancy is considered important.
Embryo development: 4–7 weeks
Fetal development by week in pictures: week 4
Fetal development by week photo: week 4
Photo of an embryo before the 6th week of pregnancy.
The heart, head, arms, legs and tail are formed in the embryo :) . Gill slit is defined. The length of the embryo at the fifth week reaches 6 mm.
Development of the fetus by weeks photo: week 5
At the 7th week, the rudiments of the eyes, stomach and chest are determined, and fingers appear on the handles. The baby already has a sense organ - the vestibular apparatus. The length of the embryo is up to 12 mm.
Fetal development: 8th week
Fetal development by weeks photo: weeks 7-8
The face of the fetus can be identified, the mouth, nose, and auricles can be distinguished. The head of the embryo is large and its length corresponds to the length of the body; the fetal body is formed. All significant, but not yet fully formed, elements of the baby's body already exist. The nervous system, muscles, skeleton continue to improve.
The head of the embryo is large and its length corresponds to the length of the body; the fetal body is formed. All significant, but not yet fully formed, elements of the baby's body already exist. The nervous system, muscles, skeleton continue to improve.
Fetal development in the photo already sensitive arms and legs: week 8
The fetus developed skin sensitivity in the mouth area (preparation for the sucking reflex), and later in the face and palms.
At this stage of pregnancy, the genitals are already visible. Gill slits die. The fruit reaches 20 mm in length.
Fetal development: 9–10 weeks
Fetal development by week photo: week 9
Fingers and toes already with nails. The fetus begins to move in the pregnant woman's stomach, but the mother does not feel it yet. With a special stethoscope, you can hear the baby's heartbeat. Muscles continue to develop.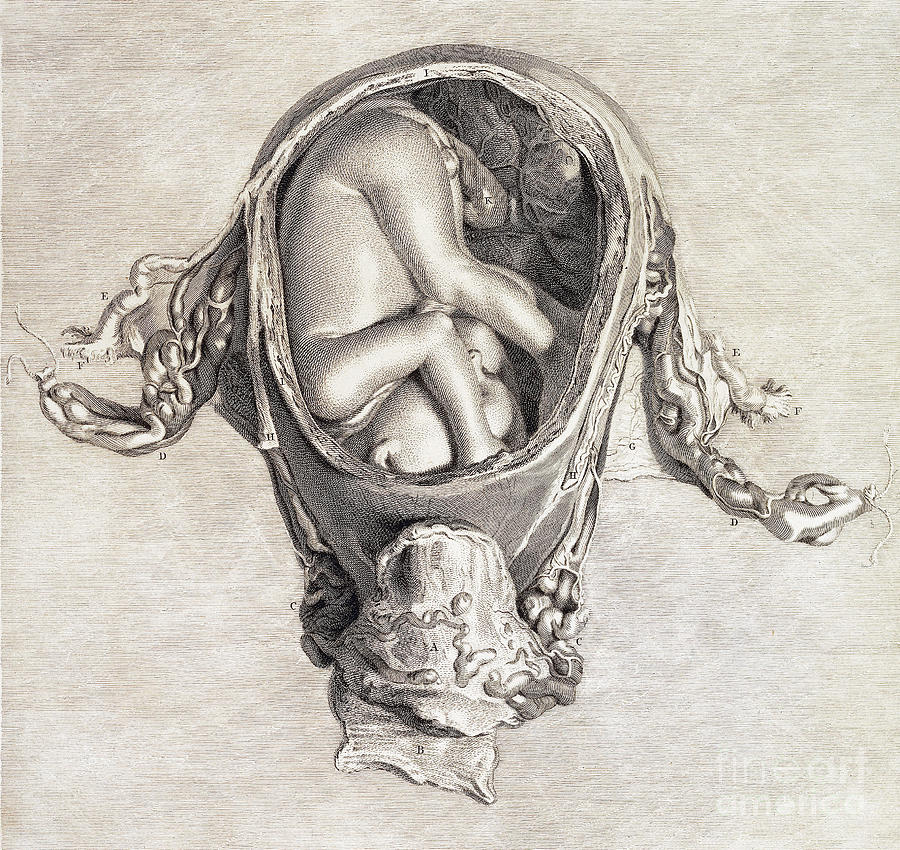
Fetal development by weeks photo: week 10
The entire surface of the fetal body is sensitive and the baby develops tactile sensations with pleasure, touching his own body, the walls of the fetal bladder and the umbilical cord. It is very curious to observe this on ultrasound. By the way, the baby first moves away from the ultrasound sensor (of course, because it is cold and unusual!), And then puts his hands and heels trying to touch the sensor.
It's amazing when a mother puts her hand to her stomach, the baby tries to master the world and tries to touch with his pen "from the back".
The development of the fetus: 11–14 weeks
Development of the fetus in the photo of the legs: weeks 11
In the baby, the legs, legs and eyelids are formed, and the genitals become distinguishable (you can find out the gender (you can find out the gender child). The fetus begins to swallow, and if something is not to its taste, for example, if something bitter got into the amniotic fluid (mother ate something), then the baby will begin to frown and stick out his tongue, making less swallowing movements.
The fetus begins to swallow, and if something is not to its taste, for example, if something bitter got into the amniotic fluid (mother ate something), then the baby will begin to frown and stick out his tongue, making less swallowing movements.
Fruit skin appears translucent.
Fruit development: Week 12
Photo of the fetus 12 weeks at 3D ultrasound
DEVELOPMENT OF RELATIONS photo: Week 14
9000
9000
urine. Blood forms inside the bones. And hairs begin to grow on the head. Moves more coordinated.
Fetal development: 15-18 weeks
Fetal development by week photo: week 15
The skin turns pink, the ears and other parts of the body, including the face, are already visible. Imagine, a child can already open his mouth and blink, as well as make grasping movements. The fetus begins to actively push in the mother's tummy. The sex of the fetus can be determined by ultrasound.
The sex of the fetus can be determined by ultrasound.
Fetal development: 19-23 weeks
Fetal development by week photo: week 19
Baby sucks his thumb, becomes more energetic. Pseudo-feces are formed in the intestines of the fetus - meconium , kidneys begin to work. During this period, the brain develops very actively.
Fetal development by weeks photo: week 20
The auditory ossicles become stiff and now they are able to conduct sounds, the baby hears his mother - heartbeat, breathing, voice. The fetus intensively gains weight, fat deposits are formed. The weight of the fetus reaches 650 g, and the length is 300 mm.
The lungs at this stage of fetal development are so developed that the baby can survive in the artificial conditions of the intensive care unit.
Fetal development: 24-27 weeks
Lungs continue to develop. Now the baby is already falling asleep and waking up.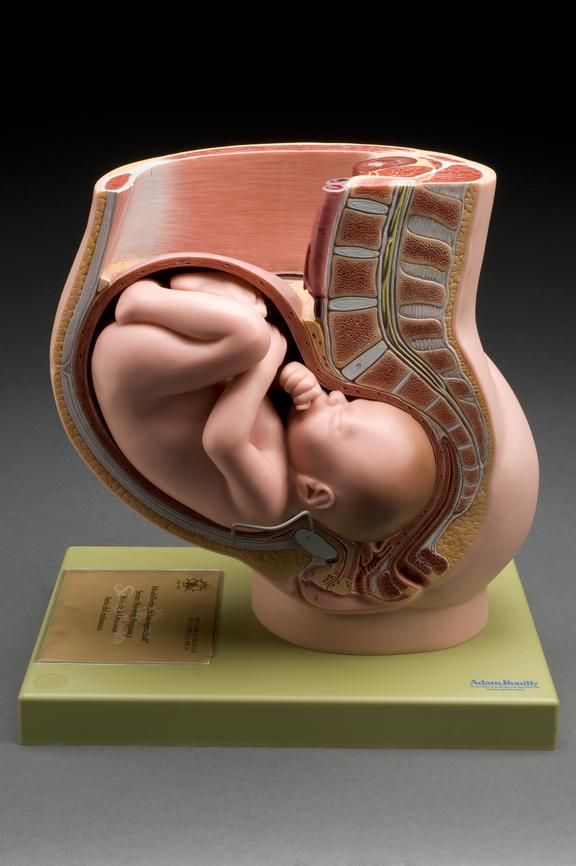 Downy hairs appear on the skin, the skin becomes wrinkled and covered with grease. The cartilage of the ears and nose is still soft.
Downy hairs appear on the skin, the skin becomes wrinkled and covered with grease. The cartilage of the ears and nose is still soft.
Fetal development by week photo: week 27
Lips and mouth become more sensitive. The eyes develop, open slightly and can perceive light and squint from direct sunlight. In girls, the labia majora do not yet cover the small ones, and in boys, the testicles have not yet descended into the scrotum. Fetal weight reaches 900–1200 g, and the length is 350 mm.
9 out of 10 children born at this term survive.
Fetal development: 28-32 weeks
The lungs are now adapted to breathe normal air. Breathing is rhythmic and body temperature is controlled by the CNS. The baby can cry and responds to external sounds.
Child opens eyes while awake and closes during sleep.
The skin becomes thicker, smoother and pinkish. Starting from this period, the fetus will actively gain weight and grow rapidly.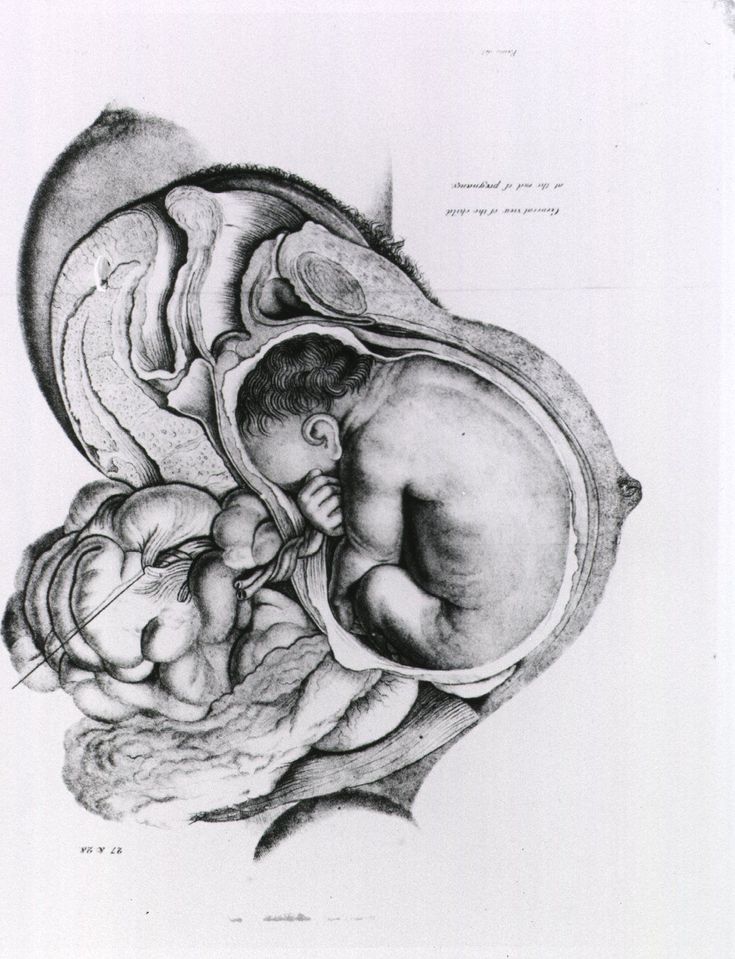 Almost all babies born prematurely at this time are viable. The weight of the fetus reaches 2500 g, and the length is 450 mm.
Almost all babies born prematurely at this time are viable. The weight of the fetus reaches 2500 g, and the length is 450 mm.
Fetal development: 33–37 weeks
Fetal development by week photo: week 36
The fetus reacts to a light source. Muscle tone increases and the baby can turn and raise his head. On which, the hairs become silky. The child develops a grasping reflex. The lungs are fully developed.
Fetal development: 38-42 weeks
The fetus is quite developed, prepared for birth and considered mature. The baby has mastered over 70 different reflex movements. Due to the subcutaneous fatty tissue, the baby's skin is pale pink. The head is covered with hairs up to 3 cm.
Fetal development by weeks photo: week 40
The baby perfectly mastered the movements of his mother , knows when she is calm, excited, upset and reacts to this with her movements. During the intrauterine period, the fetus gets used to moving in space, which is why babies love it so much when they are carried in their arms or rolled in a stroller.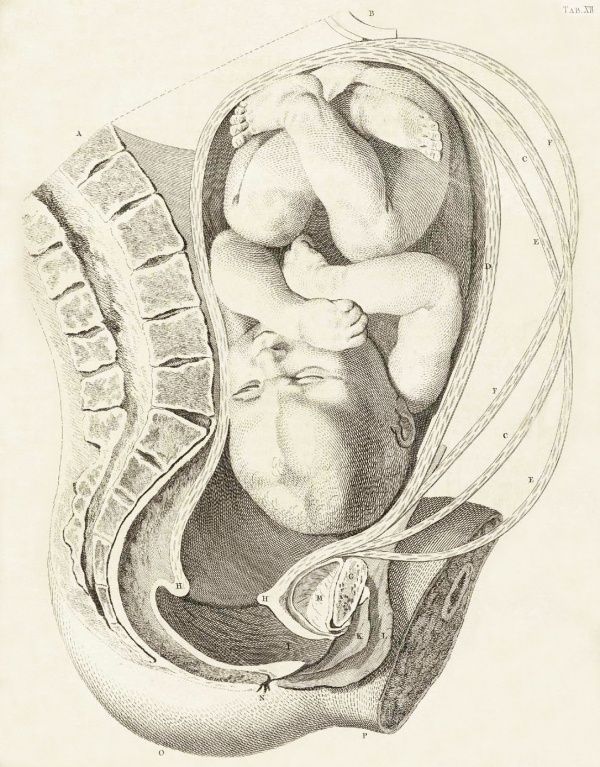 For a baby, this is a completely natural state, so he will calm down and fall asleep when he is rocked.
For a baby, this is a completely natural state, so he will calm down and fall asleep when he is rocked.
The nails protrude beyond the tips of the fingers, the cartilages of the ears and nose are elastic. In boys, the testicles have descended into the scrotum, and in girls, the large labia cover the small ones. The weight of the fetus reaches 3200-3600 g, and the length is 480-520 mm.
After the birth, the baby longs for touching his body, because at first he cannot feel himself - the arms and legs do not obey the child as confidently as it was in the amniotic fluid. Therefore, so that your baby does not feel lonely, it is advisable to carry him in your arms, press him to you while stroking his body.
And one more thing, the baby remembers the rhythm and sound of your heart very well . Therefore, you can comfort the baby in this way - take him in your arms, put him on the left side and your miracle will calm down, stop crying and fall asleep.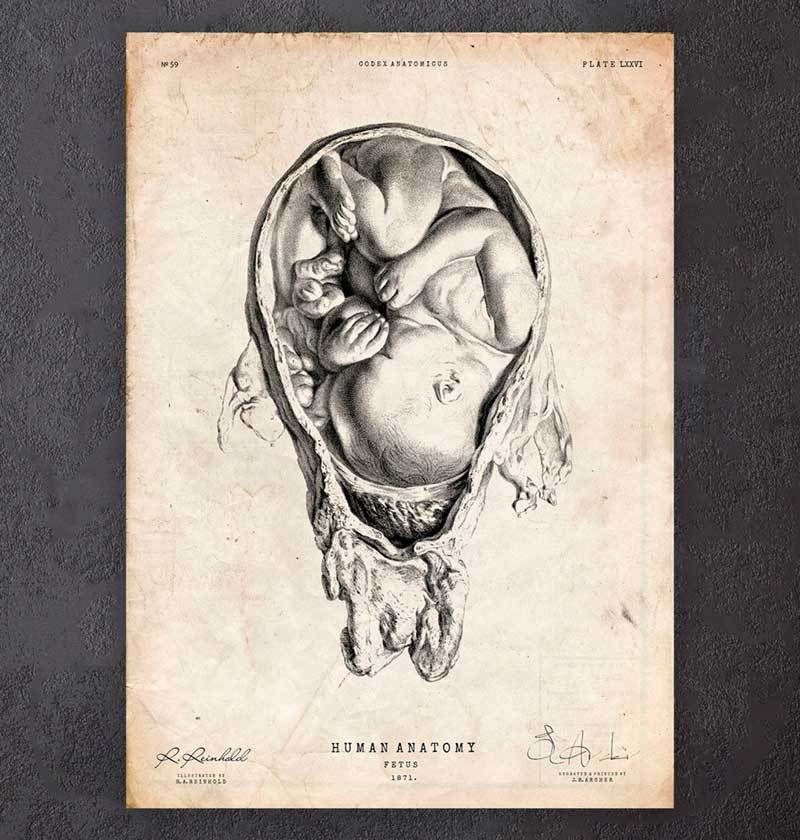



.jpg)






