Dichorionic twin pregnancy
What are Dichorionic Diamniotic twins? Are there risks involved in multiple births? Cloudnine BlogWhat are Dichorionic Diamniotic twins?
A 2004 study showed that there is a chance of 1 multiple births in every 67 pregnancies. When it comes to multiple births, twin seems to be the easiest, but is it?
Well, the world of twins is undoubtedly fascinating, and it is understandable if you feel desperate to have twins. But do you know the complications related to twin pregnancies or even the type of twin pregnancies? Let us explain it to you!
Book an appointment online to consult with Dr. Shweta Bansal Wazir for gynecological issues.
What are the main types of twins?
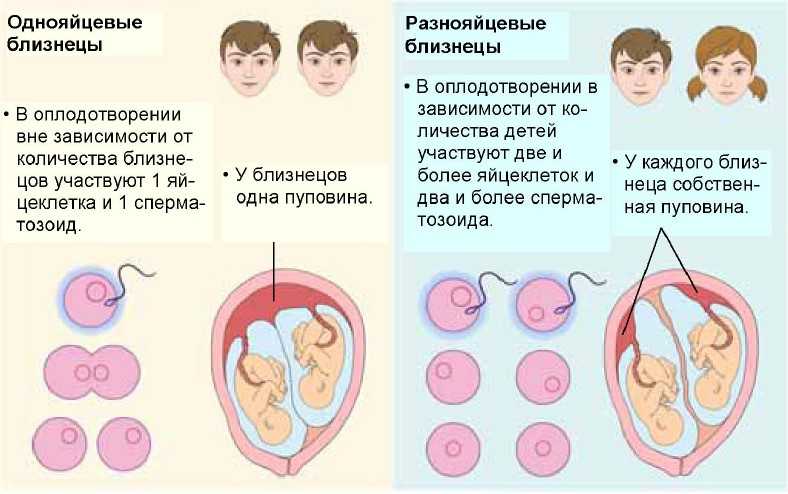
There are three main different types of twins:
- Dizygotic Twins
- Polar Body Twins
- Monozygotic Twins (dichorionic or monochorionic)
Book Online Consultation with Doctor, consult the best Gynecologist in India
What are Dichorionic Diamniotic Twins?
Diamniotic dichorionic pregnancy means that both the babies are growing in separate sacs.
Some twins develop when two different sperms fertilize the two different eggs. This results in the formation of two separate zygotes in the womb where each of the zygotes only shares about 50% of the genes. This makes them genetically like a sibling.
Now, each of the foetus lies within its membranes called the chorion and amnion (they have their own chorionic and amniotic sacs). They are termed as dichorionic diamniotic twins.
Must Read: Twin Pregnancy Symptoms and Early Signs
What is Chorion?
It is the outermost layer of the fluid-filled amniotic sac which surrounds the growing fetus inside the womb. When two foet uses are growing separately in separate sacs, it is surrounded by two separate chorions, and they are termed as dichorionic. The prefix "di" is used to indicate two.
All dizygotic or fraternal twins are dichorionic in nature whereas some monozygotic (identical) twins can be dichorionic at times.
When it comes to the placenta, the dichorionic twins have two individual placentas, but sometimes the placentas are seen to fuse. The placenta is an organ through which the blood from the mother passes to the baby for supplying nutrients.
Must Read: Supermom Harshita Dabbiru, with Twin Superpowers!
Dichorionic twins are also defined as diamniotic twins since each of them have amniotic sac as its outer membrane. That is why dichorionic twins are described as dichorionic-diamniotic twins.
Are there any risks involved in multiple births?
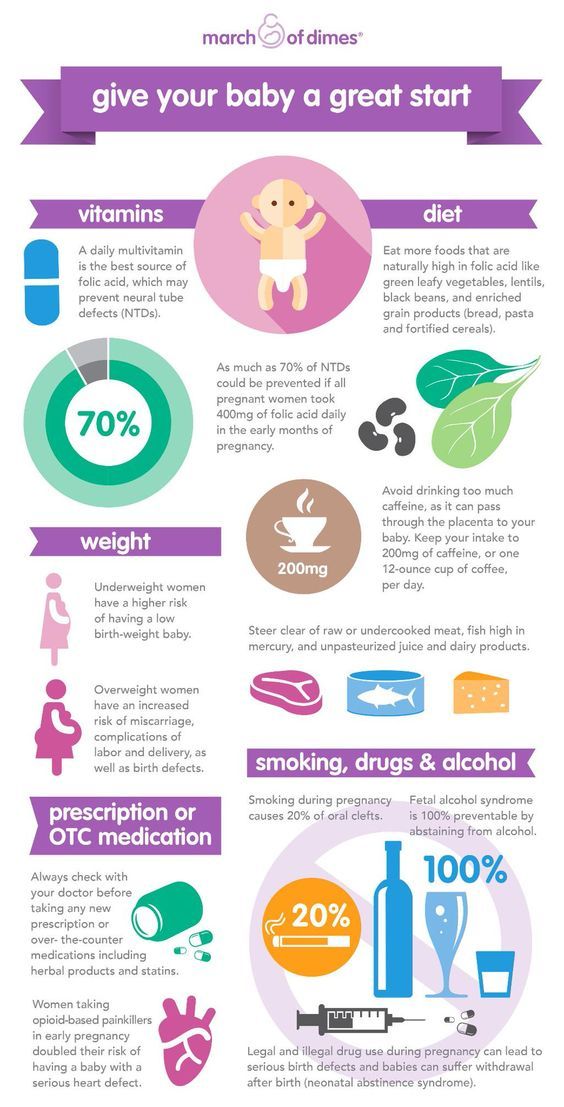
When it comes to twins and triplets the health risks for twins and triplets are greatly more when compared to singletons. This is because multiples have a greater chance of malformations and malnutrition which results in premature birth, underweight child, and early and late miscarriage risks. That is why you should have an excellent medical team around you to guide and support you during your incredible journey.
This is because multiples have a greater chance of malformations and malnutrition which results in premature birth, underweight child, and early and late miscarriage risks. That is why you should have an excellent medical team around you to guide and support you during your incredible journey.
Join our Cloudnine Community to discuss further regarding - Moms of Twins, Foetal Growth, High Risk Pregnancy and Labour and Delivery.
Explore Cloudnine Momeaze for all your shopping needs with wide range of products.
Our customers had a few questions regarding this blog, check them out now!
When are twins detected?
Remedies for back and leg pain?
Have Similar Questions?
Get answers from our Experts, browse through hundreds of Q&A, attend live sessions, and much more
Ask your question!
Want to consult the best gynecologists in India? Please find the links below.
- Best Gynecologists in Bangalore
- Best Gynecologists in Chennai
- Best Gynecologists in Mumbai
- Best Gynecologists in Pune
- Best Gynecologists in Chandigarh
- Best Gynecologists in Gurgaon
- Best Gynecologists in Noida
Want to consult the best Maternity Packages in India? Please find the links below.
- Best Maternity Packages in Bangalore
- Best Maternity Packages in Chennai
- Best Maternity Packages in Mumbai
- Best Maternity Packages in Pune
- Best Maternity Packages in Chandigarh
- Best Maternity packages in Gurgaon
- Best Maternity Packages in Noida
Di/Di Twins: Definition, Risks, and More
It may seem in recent years like the possibility of twins is becoming more and more of an everyday reality. If you’ve found out you’re having twins (or just recently met a family with a pair of twins), you may wonder, how did this happen?
If you’ve found out you’re having twins (or just recently met a family with a pair of twins), you may wonder, how did this happen?
How did two babies come to be and how genetically identical are they? They may share the same birthday, but did they share the same placenta? Do they share the exact same genes?
Unless you are a twin or have given birth to twins, you may be confused about the different types of twins and what their genetic makeups are. (Completely understandable!) Perhaps your doctor or friend mentioned that the twins in question are di/di. What does this mean? Please allow us to explain…
When someone talks about twins they are referring to two babies that develop during the same pregnancy, but this can happen in many different ways. Believe it or not, the term twins is pretty broad!
Two major categories twins are typically divided into are identical and fraternal.
Identical twins are also sometimes called monozygotic twins, because they came from the same fertilized egg.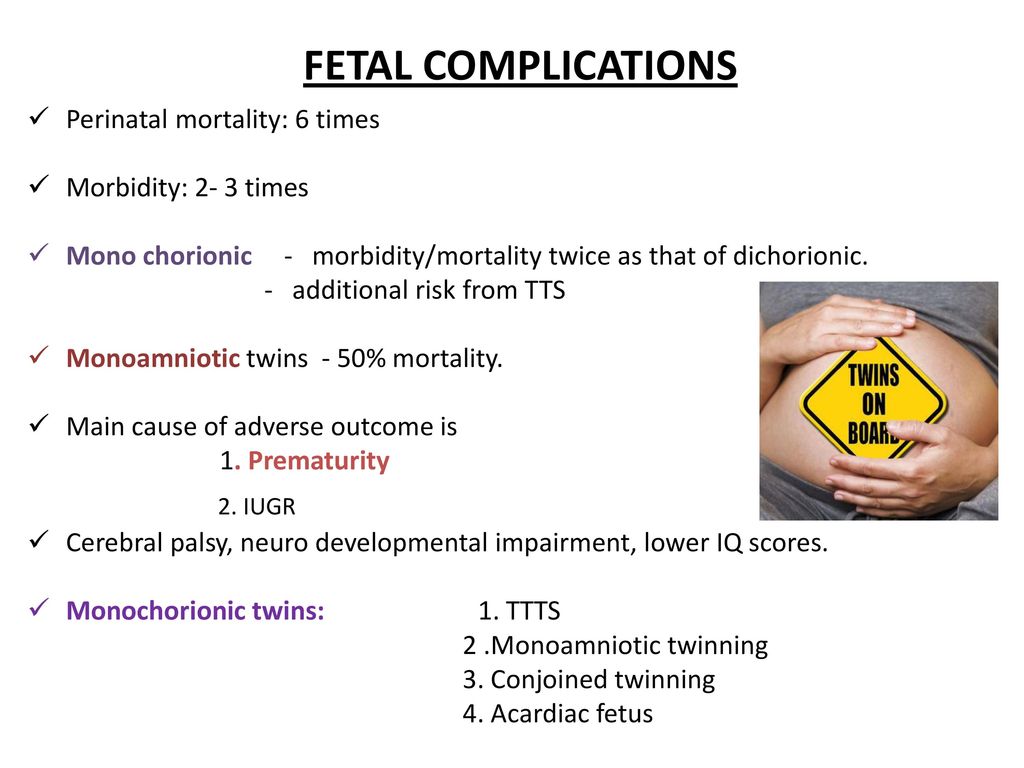 (Identical twins are created when one egg and sperm meet like normal. The single egg splits in two shortly after fertilization.)
(Identical twins are created when one egg and sperm meet like normal. The single egg splits in two shortly after fertilization.)
Because identical twins come from the same egg/sperm, their chromosomes will be identical, which means they will be the same sex and have the same genetic characteristics (e.g., hair and eye color).
On the other hand, fraternal twins only share about 50 percent of their chromosomes, as other siblings do. This means they can appear nearly identical or completely different. They can be different sexes with different hair and eye colors or the same sex and look very similar.
Fraternal twins are also called dizygotic twins, because they come from two different eggs. (The mother releases two eggs at around the same time, which are fertilized by two different sperm.)
Still with us? Well, there’s even more to it than whether they are identical and fraternal if you want to know how a set of twins developed. The type of twins (fraternal or identical) and the timing of their development affects whether the babies shared or had their own separate chorionic and amniotic sacs.
We know what you’re thinking… what is a chorion? (And while we’re at it, what’s amnion/an amniotic sac?) And why do they matter?
The chorion is the outermost fetal membrane. The chorion connects the amnion, amniotic fluid, and the fetus to the placenta. It also contributes to placenta development.
Why is this important? Well, if two twins share a chorion, they’ll share one placenta. If twins have separate chorion, they will have two separate placentas.
The amnion on the other hand is the innermost fetal membrane. It protects the fetus and includes amniotic fluid. Like the chorion, twins can either share an amnion or have one all of their own.
Since this is the inner layer, the options here depend on the chorion. One chorion that is shared can contain one or two amnions. So even though two babies may share the same placenta, they can each still be swimming in their own amniotic fluid if they have their own amniotic sac. On the other hand, two chorions mean two separate amnions.
Got all that? Don’t worry, we know it’s a lot to take in, so here’s a quick view of the different ways this can all come together…
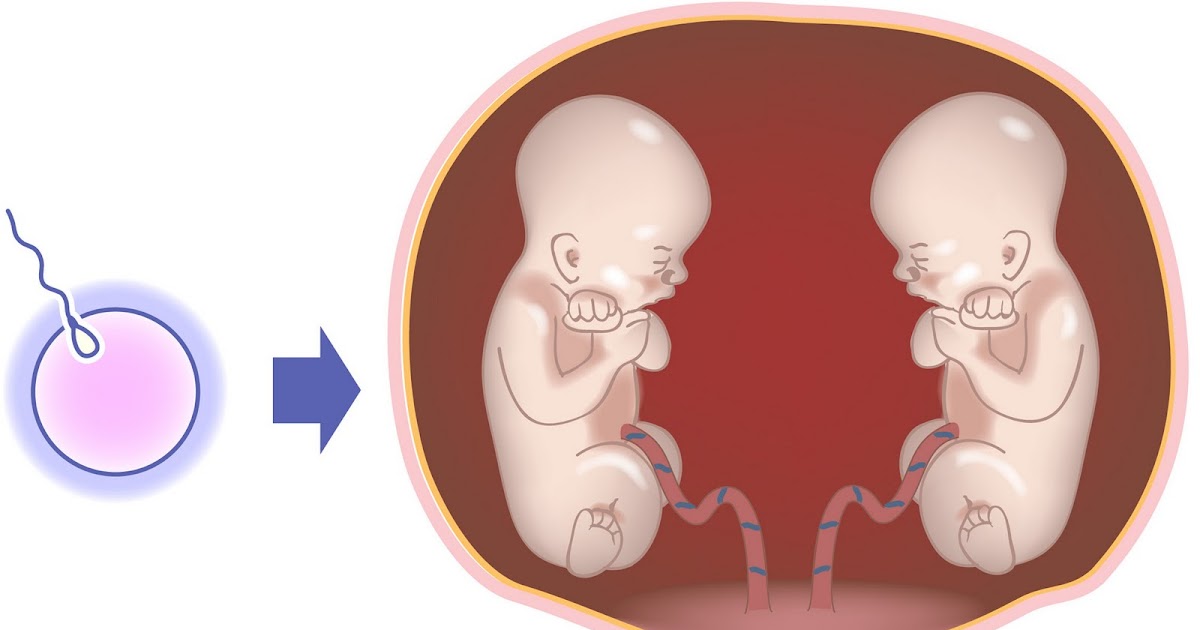
Di/di
In a di/di pregnancy (more scientifically referred to as a dichorionic diamniotic pregnancy) the twins each have their own chorionic and amniotic sacs. Essentially, each of the babies is growing like they would as a singleton, but just a little more cramped, because they’re sharing the same womb.
Mo/di
In a mo/di pregnancy (more scientifically referred to as a monochorionic diamniotic pregnancy) the twins share a chorionic sac, but have different amniotic sacs. Simply put, the difference between a di/di and a mo/di pregnancy is that a mo/di pregnancy only involves one placenta.
Mo/mo
In a mo/mo pregnancy (more scientifically referred to as a monochorionic monoamniotic pregnancy) the twins share both the chorionic and amniotic sacs. This means one placenta and one amniotic sac for both babies. Because the babies are sharing so much, mo/mo pregnancies can be tricky and require lots of monitoring!
While it may seem like an ultrasound should be able to offer all the answers, the truth is that it has its limitations when it comes to determining di/di, mo/di, and mo/mo pregnancies.
Ultrasounds are most accurate at determining chorionicity in the first trimester. Signs that may indicate a di/di pregnancy on an ultrasound done in the first trimester are:
- two gestational sacs with a thick echogenic chorion around each embryo
- a thick inter-twin membrane
- the twin peak sign (it looks like an upside-down letter Y)
- two yolk sacs (This won’t tell whether it’s a mo/di or a di/di pregnancy though!)
Even if some of these signs are spotted, further testing may be necessary to confirm.
Di/di pregnancies account for the majority of all twin pregnancies and can produce identical or fraternal twins.
All fraternal twins are di/di, but identical twins can also be di/di. How is this possible?
With a fraternal twin pregnancy, separate eggs are individually fertilized by two different sperm cells creating two individual zygotes. Each zygote will have its own placenta and amniotic sac.
On the other hand, an identical pregnancy begins with the combination of one egg and one sperm cell, but at some point that single egg splits. When that happens affects the development of the placenta and amniotic sac.
When that happens affects the development of the placenta and amniotic sac.
If there is a separation of the zygotes approximately 1 to 4 days after the fertilization it’s more likely to lead to a di/di twin set-up.
Since the combinations aren’t solely determined by whether the pregnancy is fraternal or identical, it can be difficult to determine via ultrasound if the twins you’re carrying are fraternal or identical.
Obviously, if ultrasound reveals you’re carrying one of each sex, it’s clear that the twins are fraternal. However, if the twins share the same sex, it’s less clear whether or not they’re identical.
A study from 2012 found that close to 15 percent of parents who were told their twins’ zygosity based on ultrasound were misinformed. For parents who want to know for sure, genetic testing performed after birth will give the clearest answers.
Being pregnant with twins does come with some additional risks. While a di/di pregnancy carries with it the lowest rate of complications among twin pregnancies, any woman carrying twins has an added risk of issues with the placenta and intrauterine growth restriction (i. e. babies outgrowing the real estate available!).
e. babies outgrowing the real estate available!).
Some complications that may be more likely with a twin birth include:
- Placenta previa. A larger or heavier placenta from having twins may be more likely to hang low and cover the cervix making normal delivery dangerous.
- Placental abruption. A larger or heavier placenta from having twins may also be more likely to tear away from the uterine wall.
- Placenta accreta. This occurs when the placenta attaches itself too deeply into the uterine wall.
- Prematurity. Because of uterine space restrictions and the potential for other complications indicating an earlier birth would be beneficial, twins have a higher likelihood of being born premature (before 37 weeks gestation).
- Low birth weight. Since twin babies develop sharing space in the uterus and may need to be born a little earlier than what is considered full term, they are at a higher likelihood of having a low birth weight.
 (A baby is considered to have low birth weight if it is born weighing less than 5 pounds, 8 ounces.)
(A baby is considered to have low birth weight if it is born weighing less than 5 pounds, 8 ounces.) - Gestational diabetes. This can occur when blood sugar levels are too high.
- Gestational hypertension. This is high blood pressure during pregnancy.
- Postpartum hemorrhage. One potential reason for a hemorrhage after giving birth is that a large placenta from having twins has caused the uterus to stretch more than normal.
Of course, knowing which type of twin combination is present during pregnancy is important to understand the level of risk involved. As noted earlier, a di/di combination comes with a lower level of risk, since each baby is enclosed in their own amniotic bubble and they’re sharing space in the womb, but not other elements.
If the babies are sharing a placenta, there is a risk that one baby may receive more of the nutrients and oxygen needed for development. This issue occurs in approximately one-third of mo/di twin pregnancies.
This unequal division can lead to issues such as twin to twin transfusion syndrome (TTTS), twin anemia polycythemia sequence (TAPS), or selective intrauterine growth restriction (SIUGR). As such, mo/di pregnancies should be more closely monitored.
The highest risk occurs when twins are sharing both the amnion and chorion in a mo/mo pregnancy. Because there is nothing to separate the babies from one another in the womb there is a risk of cord entanglement.
These pregnancies are very rare — they account for less than 1 percent of twin pregnancies — but the risks mean you’ll be monitored very closely.
Whether inside or outside the womb, twin development can be confusing and offer some extra complications. (Don’t worry though, they can also bring double the joy!)
If you’re about to be a twin parent, you likely have a lot of questions about their genetics and how they came to be. Some questions can be answered via ultrasound, but others can only be discovered through genetic testing.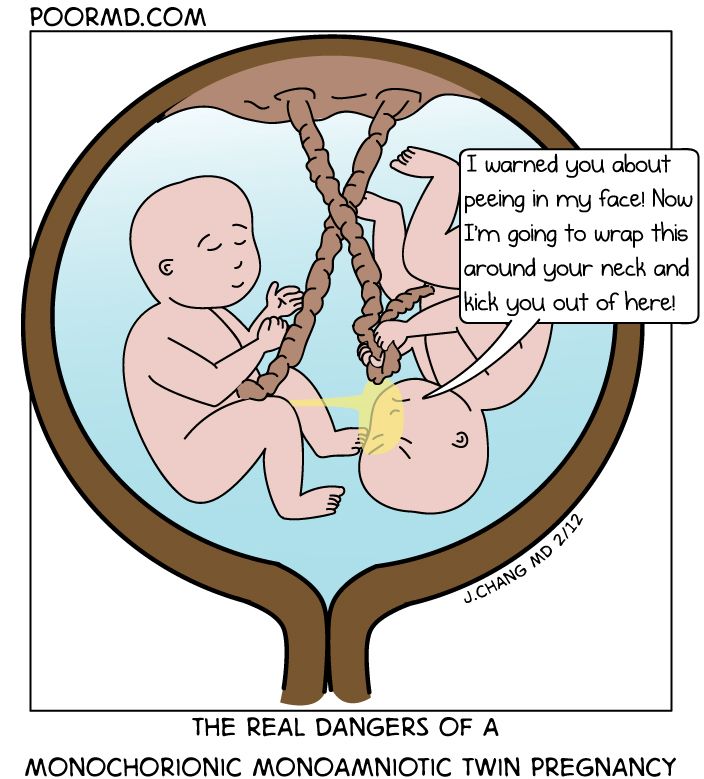
Armed with a little more background information, you’ll be better prepared to ask the questions you need to get the information you want!
articles from the specialists of the clinic "Mother and Child"
Arifullina Claudia Viktorovna
Gastroenterologist
Clinical Hospital "AVICENNA" GC "Mother and Child"
There is data on the frequency of twins in case of anomalies in the development of the uterus, characterized by its bifurcation (bicornuate uterus, having a septum in the cavity, etc.). The cause of polyembryony may be the separation of blastomeres (in the early stages of crushing), resulting from hypoxia, cooling, acidity and ionic composition of the medium, exposure to toxic and other factors. Multiple pregnancy can occur: as a result of the fertilization of two or more simultaneously mature eggs, as well as the development of two or more embryos from one fertilized egg. nine0003
Twins formed from two (three, etc. ) eggs are called dizygotic (polyzygotic), those arising from one are called identical. The origin of fraternal twins (polyzygotic twins): the simultaneous maturation (and ovulation) of two or more follicles in one ovary is possible. There may be maturation of two or more follicles and ovulation in both ovaries.
) eggs are called dizygotic (polyzygotic), those arising from one are called identical. The origin of fraternal twins (polyzygotic twins): the simultaneous maturation (and ovulation) of two or more follicles in one ovary is possible. There may be maturation of two or more follicles and ovulation in both ovaries.
A third way of the origin of fraternal (multi-ovular) twins is possible - the fertilization of two or more eggs that have matured in one follicle. The origin of identical twins: most often, the occurrence of identical twins is associated with the fertilization of an egg that has two or more nuclei. a single embryonic germ in the stage of crushing is divided into two parts; from each part an embryo (fruit) is formed. Twin twin. Fertilized eggs develop on their own. After penetration into the mucous membrane, each embryo develops its own aqueous and fleecy membranes; in the future, each twin forms its own placenta with an independent network of vessels, each fetal egg, except for the chorion and amnion, has an independent capsular membrane (decidua capsularis). In some cases, anastomoses are formed between the vessels of independent placentas. Twins can be same-sex (both boys or both girls) or different-sex (boy and girl). Their blood type can be the same or different. Identical twin. Identical twins have a common capsular and fleecy membrane and a common placenta; the vessels (both arterial and venous) of both twins in the placenta communicate with the help of numerous anastomoses. The water membrane of each twin is separate, the septum between the fetal sacs consists of two water membranes (biamniotic twins). nine0003
In some cases, anastomoses are formed between the vessels of independent placentas. Twins can be same-sex (both boys or both girls) or different-sex (boy and girl). Their blood type can be the same or different. Identical twin. Identical twins have a common capsular and fleecy membrane and a common placenta; the vessels (both arterial and venous) of both twins in the placenta communicate with the help of numerous anastomoses. The water membrane of each twin is separate, the septum between the fetal sacs consists of two water membranes (biamniotic twins). nine0003
Identical twins always belong to the same sex (both boys or both girls), look alike, have the same blood type.
In fraternal twins, the membranes in the septum are arranged as follows: amnion - chorion, chorion - amnion; with monozygotic amnion-amnion.
Important signs for the diagnosis are: blood type (and other blood factors), eye color, hair color, skin texture of the fingertips, shape and location of teeth. In identical twins, these signs are completely the same. Fraternal twins share the same similarities as normal siblings. nine0017
In identical twins, these signs are completely the same. Fraternal twins share the same similarities as normal siblings. nine0017
MULTIPLE PREGNANCY
With multiple pregnancy, increased demands are made on the woman's body: the cardiovascular system, lungs, liver, nights and other organs function with great stress. In this regard, multiple pregnancies are more difficult than single pregnancies.
- Pregnant women often complain of fatigue and shortness of breath, which increases towards the end of pregnancy. The cause of shortness of breath is a difficulty in the activity of the heart due to a significant displacement of the diaphragm by the bottom of the uterus, the size of which is larger in multiple pregnancy than in singleton. nine0031
- Often there is a dilation of the veins of the lower extremities. By the end of pregnancy, there is often an increase in the urge to urinate due to the pressure of a large fetus on the bladder.

- Pregnant women often complain of heartburn and constipation.
- In multiple pregnancies, toxicosis occurs more often than in singleton pregnancies: vomiting, salivation, edema, nephropathy, eclampsia.
- With twins, polyhydramnios of one of the fetuses is often found, which leads to a sharp increase and hyperextension of the uterus, shortness of breath, tachycardia and other disorders. Polyhydramnios is more common in one of the identical twins. In some cases, the polyhydramnios of one twin is accompanied by an oligohydramnios of the other fetus. nine0031
- Premature termination of multiple pregnancies often occurs.
- With twins, preterm birth occurs in at least 25% of women.
- Prematurity is more common in triplets than in twins. The greater the number of gestated fetuses, the more often preterm births are observed.
- Development of term twins is normal in most cases. However, their body weight is usually less than that of single fetuses.
 Often there is a difference in body weight of twins by 200-300 g, and sometimes more. nine0031
Often there is a difference in body weight of twins by 200-300 g, and sometimes more. nine0031 - Uneven development of twins is associated with unequal intake of nutrients from a single placental circulation.
- Often there is a difference not only in weight, but also in the length of the body of the twins. In connection with this, the theory of supergenesis (superfoetatio) was put forward. Proponents of this hypothesis believe that fertilization of eggs of different ovulation periods is possible, i.e., the onset of a new pregnancy in the presence of an already existing, previously occurring, pregnancy. nine0031
- Due to the uneven delivery of nutrients and oxygen, a significant developmental disorder and even death of one of the twins can occur. This is more commonly seen in identical twins. The dead fetus is squeezed by the second, well-growing fetus, the amniotic fluid is absorbed, the placenta undergoes regression. The compressed mummified fetus ("paper fetus") is released from the uterus along with the placenta after the birth of a live twin.
 Polyhydramnios of one fetus, which occurs during multiple pregnancies, often also prevents the other twin from developing correctly. With pronounced polyhydramnios, certain anomalies in the development of the fetus, which grows with an excess of amniotic fluid, are often observed. Rarely, fused twins are born (fusion can be in the head, chest, abdomen, pelvis) and twins with other malformations. nine0031
Polyhydramnios of one fetus, which occurs during multiple pregnancies, often also prevents the other twin from developing correctly. With pronounced polyhydramnios, certain anomalies in the development of the fetus, which grows with an excess of amniotic fluid, are often observed. Rarely, fused twins are born (fusion can be in the head, chest, abdomen, pelvis) and twins with other malformations. nine0031 - The position of the fetus in the uterine cavity in most cases (about 90%) is normal. In the longitudinal position, different presentation options are observed: both fetuses are presented with the head, both with the pelvic end, one with the head, and the other with the pelvic end. With longitudinal presentation, one fetus may be behind the other, which makes diagnosis difficult. Less commonly observed is the longitudinal position of one fetus and the transverse position of the other. The most rare is the transverse position of both twins. nine0031
- Position of the twins in the uterus, both fetuses are presented with the head, one fetus is presented with the head, the second - with the pelvic end, both fetuses are in the transverse position
- In case of multiple pregnancies, women are taken to a special account and carefully monitored.
 When the earliest signs of complications appear, the pregnant woman is sent to the pregnancy pathology department of the maternity hospital. Given the frequent occurrence of preterm birth, it is recommended that a pregnant woman with twins be sent to the maternity hospital 2 to 3 weeks before delivery, even in the absence of complications. nine0031
When the earliest signs of complications appear, the pregnant woman is sent to the pregnancy pathology department of the maternity hospital. Given the frequent occurrence of preterm birth, it is recommended that a pregnant woman with twins be sent to the maternity hospital 2 to 3 weeks before delivery, even in the absence of complications. nine0031
RECOGNITION OF MULTIPLE PREGNANCY
Diagnosis of multiple pregnancy often presents significant difficulties, especially in its first half. In the second half, towards the end of pregnancy, the recognition of twins (triplets) is facilitated. However, diagnostic errors occur during the study at the end of pregnancy and even during childbirth.
When recognizing a multiple pregnancy, the following signs are taken into account: nine0017
- The enlargement of the uterus in multiple pregnancy occurs faster than in pregnancy with one fetus, so the size of the uterus does not correspond to the gestational age.
 The bottom of the uterus is usually high, especially at the end of pregnancy, the circumference of the abdomen during this period reaches 100-110 cm or more.
The bottom of the uterus is usually high, especially at the end of pregnancy, the circumference of the abdomen during this period reaches 100-110 cm or more. - The following signs are unstable and not sufficiently reliable: a) deepening of the uterine fundus (saddle uterus), the formation of which is associated with protrusion of the corners of the uterus with large parts of the fetus; b) the presence of a longitudinal depression on the anterior wall of the uterus, which is formed as a result of the fruits that are in a longitudinal position adjacent to each other; c) the presence of a horizontal groove on the anterior wall of the uterus with the transverse position of the fetus. nine0031
- The small size of the presenting head with a significant volume of the pregnant uterus and the high standing of its bottom also make it possible to suspect a multiple pregnancy. The presence of this sign is explained by the fact that the study determines the head of one and the pelvic end (in the bottom of the uterus) of another fetus, which lies slightly higher.
- Feeling the movement of the fetus in different places and probing the parts of the fetus in different parts of the abdomen (both on the right and on the left) also indicate multiple pregnancies. nine0031
Make an appointment
to the doctor - Arifullina Claudia Viktorovna
Clinical Hospital "AVICENNA" GC "Mother and Child"
GastroenterologyPediatric Gastroenterology
By clicking on the submit button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
nine0002 Clinical Hospital "AVICENNA" GC "Mother and Child"Novosibirsk Center for Reproductive MedicineAll directionsGynecological proceduresSpecialist consultations (adults)Specialist consultations (children)Laboratory of molecular geneticsGeneral clinical studiesProcedure roomTherapeutic studiesUltrasound examinations for adults
nine0002 01.
Gynecological procedures
02.
Consultations of specialists (adults)
03.
Consultations of specialists (children's)
04.
Laboratory of molecular genetics
05.
General clinical studies
06 06.
Treatment Room
07.
Therapeutic Research
08.
Adult Ultrasound
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of tests by calling
Multiple pregnancy: a modern view on the problem of pregnancy and childbirth (literature review) | Tsivtsivadze E.B., Novikova S.V.
The problem of the appearance of twins has been worrying the minds since the existence of mankind, has ethnic, cultural, social and economic implications. Traditions associated with the birth of twins have appeared in all ages. Hippocrates believed that twins were the result of the division of the seed into two parts, Democritus considered twins as the result of an excess of the seed, Aristotle explained the appearance of twins by the splitting of one germ into two. But even so far there is no unambiguous hypothesis explaining the formation of monozygotic twins. nine0003
Hippocrates believed that twins were the result of the division of the seed into two parts, Democritus considered twins as the result of an excess of the seed, Aristotle explained the appearance of twins by the splitting of one germ into two. But even so far there is no unambiguous hypothesis explaining the formation of monozygotic twins. nine0003
The relevance of the problem of multiple pregnancy lies in a significant number of complications during pregnancy and childbirth, an increase in the proportion of cesarean section, postpartum complications, an increased level of antenatal losses at various gestational periods, and a high incidence of neurological disorders in surviving children [44].
Multiple pregnancies occur in 1.5–2.5% of cases, more often in families where the mother or father, or both spouses, were born as a result of a multiple pregnancy [1]. In this case, the genotype of the mother plays the most significant role. It is impossible not to recall the well-known formula, according to which multiple pregnancies occur with a frequency of geometric progression, which is formed when the number is raised to the power of 80: one twin occurs in 80 births, triplets - in 80 births in a square (6400), quadruple - in 80 births in a cube ( 512,000), five - for 80 births in the fourth degree (40 960,000).
The interest in multiple pregnancies that has existed since ancient times has increased in the last 15–20 years due to the avalanche-like increase in multiple pregnancies associated with the introduction of assisted reproductive technologies.
Patients with multiple pregnancies remain at a high risk of perinatal complications. Even with the modern development of medicine, perinatal mortality during twin pregnancy is 5 times higher than in singleton pregnancy, intrauterine fetal death is 4 times higher, neonatal - 6 times, perinatal - 10 times. The frequency of cerebral palsy in children from twins is 3-7 times higher, with triplets - 10 times. The level of ante- and intranatal complications on the part of the mother is 2-10 times higher than that in patients with singleton pregnancies [7, 14, 17, 19, 35, 40, 60].
Perinatal morbidity and mortality in twins depend on chorionicity. According to Sebire studies, the perinatal mortality rate, mainly due to severe prematurity at birth, is higher in monochorionic twins than in dichorionic twins (5 and 2%, respectively).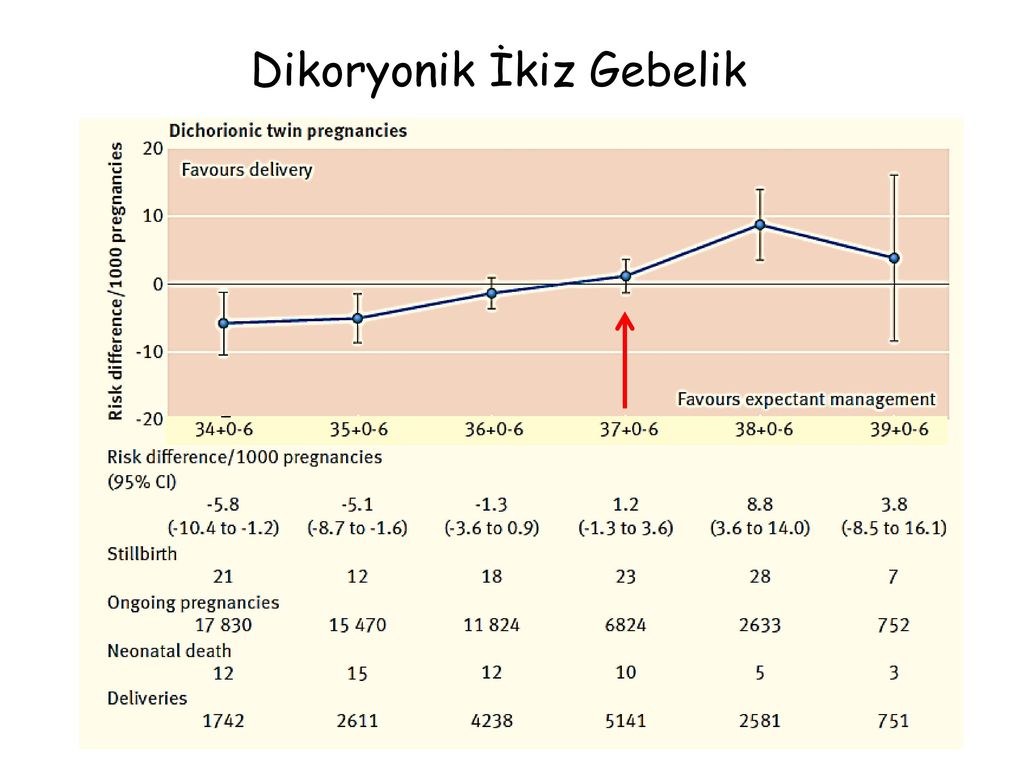 The frequency of preterm birth up to 32 weeks. in monochorionic pregnancy is 10% compared to 5% in dichorionic twins. The frequency of spontaneous abortion in the period from the 11th to the 24th week. in dichorionic twins it is 2%, in monochorionic twins it is about 10% [1, 33, 50, 64, 65]. nine0003
The frequency of preterm birth up to 32 weeks. in monochorionic pregnancy is 10% compared to 5% in dichorionic twins. The frequency of spontaneous abortion in the period from the 11th to the 24th week. in dichorionic twins it is 2%, in monochorionic twins it is about 10% [1, 33, 50, 64, 65]. nine0003
Interesting data were obtained by a group of authors who studied sex-associated differences in perinatal complications in 16,045 pregnant women with twins. Women with female twins have been found to have an increased risk of preeclampsia, but after birth, these twins had lower rates of neonatal and infant mortality, as well as a lower risk of respiratory disease than male twins [66].
Determination of zygosity before delivery is possible only when examining DNA in fetuses obtained as a result of amniocentesis, chorionic biopsy or cordocentesis. However, on the basis of zygosity, one cannot judge the type of placentation. Monozygotic twins can be either monochorionic or bichorionic [56].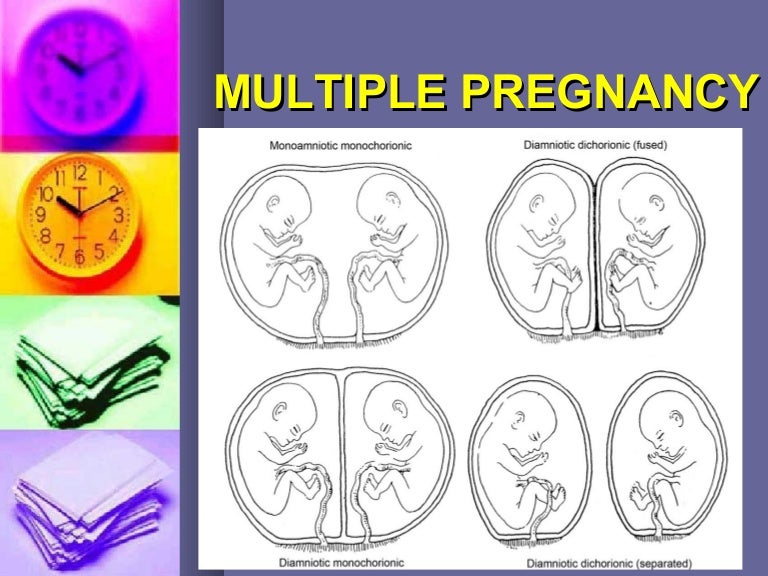 nine0003
nine0003
Determination of the chorionicity of the fetuses is possible during an ultrasound scan, during which the number of placentas, the sex of the fetuses, and the presence of an amniotic septum are determined. The optimal time for the diagnosis of chorionicity is 6–9 weeks. pregnancy. In the presence of dichorionic twins, two fetal eggs are determined, separated by a thickened septum of 2 mm or more. The use of this criterion makes it possible to diagnose mono- and bichorionic twins with an accuracy of up to 85% and 92.3%, respectively [71]. nine0003
Multiple pregnancy may be complicated by growth retardation of one or both fetuses, feto-fetal transfusion syndrome (FFTS), intrauterine death of one or both fetuses.
FFTS, first described by Schatz in 1982, occurs in 1 out of 5 monochorionic twins [47, 48]. Its morphological substrate is the anastomosing vessels between the two fetal circulatory systems [28]. This is a specific complication for monozygotic twins with a monochorionic type of placentation.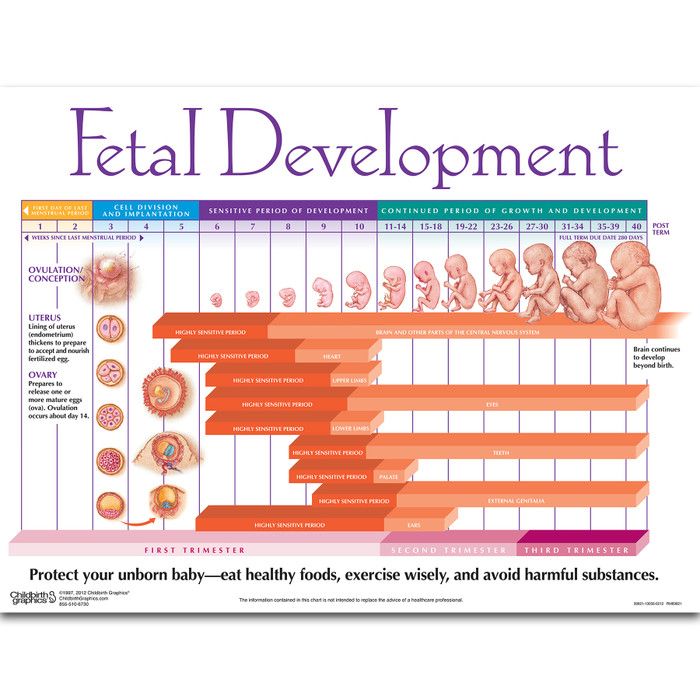 Of particular difficulty are monochorionic monoamniotic twins, when pregnancy is complicated not only by FTTS, but also by problems with the umbilical cords of the fetuses (Fig. 1). nine0003
Of particular difficulty are monochorionic monoamniotic twins, when pregnancy is complicated not only by FTTS, but also by problems with the umbilical cords of the fetuses (Fig. 1). nine0003
The criteria for FFTS are an intra-pair difference in weight of more than 20% and different concentrations of hemoglobin in fetuses [23]. For many years, the diagnosis of TTTS was established retrospectively in the neonatal period. Based on the data of ultrasound diagnostics, FFTS criteria were developed, which are used in practice to determine the management of pregnancy [63].
The most common factor associated with ante- and neonatal mortality and morbidity in twin pregnancies is low birth weight. In the vast majority of cases, low body weight of children is due to preterm birth. Various hypotheses of threatened miscarriage in multiple pregnancies are discussed in the literature. According to one of them (premature birth is a natural consequence of twin pregnancy), the main cause of premature development of labor is the overstretching of the muscle fibers of the uterus, the release of prostaglandins and reduced uteroplacental blood flow. Another hypothesis is based on the data of the Joint Perinatology Project [4], indicating that infection of the amniotic membranes contributes to their premature rupture, which most often leads to preterm birth. nine0003
Another hypothesis is based on the data of the Joint Perinatology Project [4], indicating that infection of the amniotic membranes contributes to their premature rupture, which most often leads to preterm birth. nine0003
A systematic review of randomized controlled trials that evaluated the effectiveness of antenatal screening for the presence of lower genital tract infections, as well as their treatment to reduce the incidence of preterm birth and associated morbidity, demonstrated the high effectiveness of such screening programs. Thus, in the intervention group (2058 women) screening and treatment of bacterial vaginosis, trichomoniasis and candidiasis were performed, in the control group (2097 women) were not screened, they were examined only in the presence of complaints or clinical manifestations. Preterm birth before 37 weeks. were observed significantly less frequently in the intervention group (3% vs. 5% in the control group) with a relative risk (BP) of 0.55 (95% CI 0.41 to 0.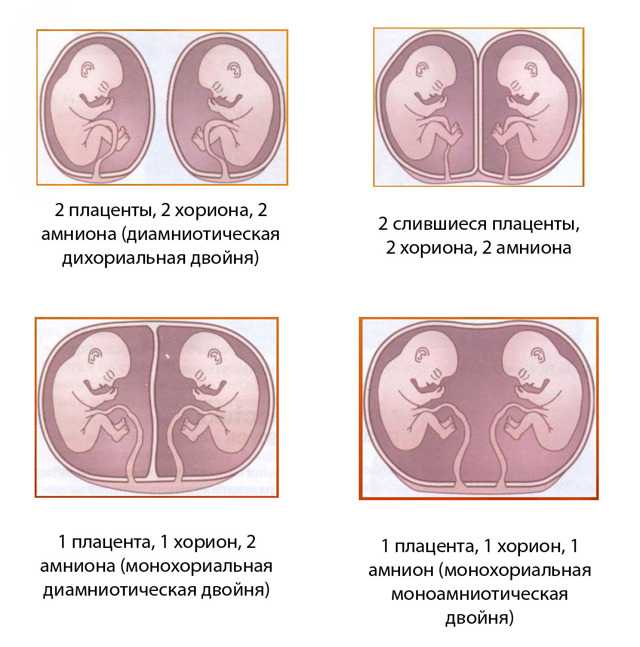 75). The frequency of birth of children with low body weight (weighing 2500 g or less) was 52% lower in the intervention group (BP 0.48, 95% CI 0.34 to 0.66), and very low birth weight children (weighing 1500 g or less) - 6% lower in the intervention group than in the control group (BP 0.34, 95% CI 0.15 to 0.75) [53].
75). The frequency of birth of children with low body weight (weighing 2500 g or less) was 52% lower in the intervention group (BP 0.48, 95% CI 0.34 to 0.66), and very low birth weight children (weighing 1500 g or less) - 6% lower in the intervention group than in the control group (BP 0.34, 95% CI 0.15 to 0.75) [53].
Thus, there is high-certainty evidence that screening and treatment programs for vaginal infections in pregnant women reduce preterm and low birth weight preterm births.
The high-risk group for complications during pregnancy and perinatal outcomes should include women with congenital anomalies in the development of the uterus. The results of numerous studies have shown that the outcome of pregnancy is largely due to the nature and severity of the malformation of the uterus. Relatively favorable outcomes were observed with a saddle uterus, unfavorable - with a bicornuate uterus and intrauterine septum [2, 9, 11, 38]. So, in the literature available to us, only 7 cases of multiple pregnancy in a bicornuate uterus were found. A. Bongain et al. (1994) suggest that the possibility of fertilization of two eggs in a pregnant woman with a congenital anomaly of the uterus (bicornuate, complete doubling) is 1:1,000,000.
A. Bongain et al. (1994) suggest that the possibility of fertilization of two eggs in a pregnant woman with a congenital anomaly of the uterus (bicornuate, complete doubling) is 1:1,000,000.
Based on the foregoing, our clinical case of multiple pregnancy with complete duplication of the uterus is of scientific and practical interest.
Pregnant S., 1988 years of age, was observed under the conditions of MONIIAG in 2010 due to the presence of an anomaly in the development of the genitourinary system - complete doubling of the uterus and pregnancy with twins. The pregnancy proceeded with the phenomena of the threat of termination, for which inpatient treatment was repeatedly carried out. On December 28, 2010, emergency delivery was performed at a gestational age of 35 weeks. due to premature rupture of amniotic fluid. A Pfannenstiel transection was performed, caesarean sections were performed in the lower uterine segments of both uterus with Derfler incisions (Fig. 2). The children were born weighing 2320 and 2000, are currently healthy. nine0003
The children were born weighing 2320 and 2000, are currently healthy. nine0003
Neurological complications are a significant problem in multiple pregnancies [6, 44]. The greatest number of neurological complications is observed in premature babies and in children with malnutrition, as well as in the presence of FTTS.
Stillbirth and neonatal mortality in multiple pregnancies are recorded 3 times more often than in singleton pregnancies, and are respectively 14.9 and 19.8 per 1000 live births. The financial costs of providing medical care to each child from twins with multiple pregnancies during the first 5 years of life are 2 times higher than those for children born with a single pregnancy. nine0003
Prematurity is considered as the main cause of neonatal mortality in multiple pregnancies. Preterm birth is the leading cause of neonatal death, as well as early and delayed disability. The rate of preterm birth varies from 6% to 12% in developed countries, and this figure is usually higher in developing countries. About 40% of all preterm births occur before 34 weeks. and 20% - up to 32 weeks. The contribution of these preterm births to the total perinatal morbidity and mortality is more than 50% [38, 46]. nine0003
About 40% of all preterm births occur before 34 weeks. and 20% - up to 32 weeks. The contribution of these preterm births to the total perinatal morbidity and mortality is more than 50% [38, 46]. nine0003
Despite a significant arsenal of tocolytic agents, the frequency of preterm births in the world is not decreasing, and the decrease in perinatal mortality is mainly due to the success of neonatologists in nursing premature babies. In connection with the foregoing, the tactics of managing and treating the threat of preterm labor should take into account the possible causes of their development, and not consist only in the appointment of symptomatic agents aimed at reducing the contractile activity of the uterus. nine0003
At present, some progress has been made in the treatment of threatened preterm labor due to drugs that suppress the contractile activity of the uterus.
In practical obstetrics, magnesium sulfate is often used. The mechanism of action of Mg2+ ions on smooth muscles has not been finally established.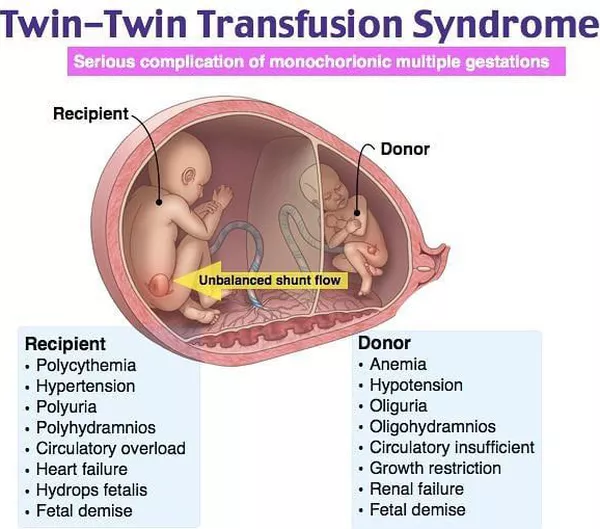 An important aspect of the use of magnesium sulfate in obstetric practice is the presence of an anticonvulsant effect in the drug, which allows it to be used to treat preeclampsia and eclampsia. With the threat of preterm birth, the prophylactic use of magnesium sulfate as a monotherapy has a less pronounced effect. nine0003
An important aspect of the use of magnesium sulfate in obstetric practice is the presence of an anticonvulsant effect in the drug, which allows it to be used to treat preeclampsia and eclampsia. With the threat of preterm birth, the prophylactic use of magnesium sulfate as a monotherapy has a less pronounced effect. nine0003
There is evidence of a relationship between the use of magnesium sulfate in the prenatal period in preterm labor or preeclampsia and a subsequent decrease in the risk of developing cerebral palsy in premature newborns with low birth weight. It should be emphasized that a neuroprotective effect was demonstrated for low total doses of magnesium sulfate (4 and 12 g), while for high total doses (>30 g) a toxic effect was demonstrated, which was accompanied by an increase in infant mortality. Incidence statistics were assessed using electronic databases and journal publications [25]. nine0003
The Committee on Obstetrics of the American College of Obstetricians and Gynecologists (ACOG, March 2010), based on multicenter data on the neuroprotective effect of magnesium sulfate and the reduction in the incidence of cerebral palsy in preterm infants, recommends that the use of this drug be added to protocols for impending PR <30 weeks: bolus 4-6 g of magnesium sulfate, then infusion of 1-2 g/h for 12 hours [27, 32, 33].
In recent decades, both foreign and domestic researchers have accumulated considerable experience in the use of calcium channel blockers in obstetric practice, primarily in diseases accompanied by an increase in blood pressure. However, the use of calcium channel blockers as tocolytic agents in case of threatened miscarriage is often accompanied by undesirable effects. It should also be remembered that in Russia nifedipine is not registered as a tocolytic agent, therefore, before using it, it is necessary to obtain the written informed consent of the patient for its use [10, 22, 55]. nine0003
As you know, the decisive role in the regulation of the contractile function of the uterus during childbirth is assigned to biologically active substances of a lipid nature - prostaglandins (especially PGF2a). The tocolytic effect of prostaglandin synthesis inhibitors has been proven experimentally and as a result of clinical observations. However, without selective properties, prostaglandin synthesis inhibitors cause undesirable effects on the fetus and newborn.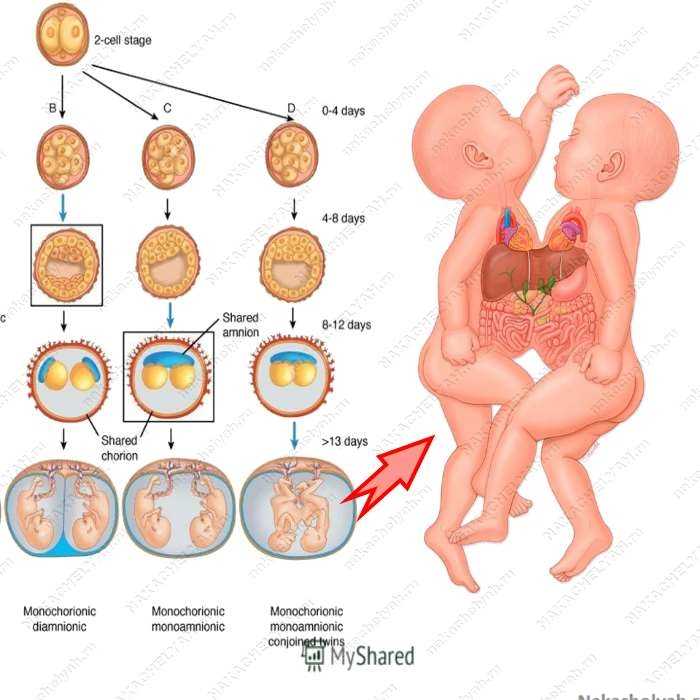 The most severe complications are manifested in premature closure of the arterial duct and a pronounced increase in pulmonary arterial pressure [59, 71].
The most severe complications are manifested in premature closure of the arterial duct and a pronounced increase in pulmonary arterial pressure [59, 71].
Progesterone, although not a tocolytic in the true sense of the word, is increasingly being used in the protocols of tocolytic therapy for preterm birth. There is no effective way to prevent preterm birth during twin pregnancy. At the same time, three large randomized trials have demonstrated that progesterone is effective in preventing preterm birth in high-risk singleton pregnancies. In recent years, the main (primarily immune) mechanisms for the implementation by gestagens of their protective function in relation to the fetus have been revealed [19, 35, 40, 74].
In patients belonging to the high-risk group (history of preterm birth or shortening of the cervix), the use of progesterone in the prenatal period led to a decrease in the frequency of early termination of pregnancy by 35% [28, 30, 52, 53, 63, 68].
It is noteworthy that the reduction in the incidence of preterm birth with the use of progesterone is not accompanied by a significant improvement in neonatal outcomes and a decrease in perinatal mortality. However, antenatal use of progesterone in singleton pregnancies has been found to be associated with a reduced risk of neonatal sepsis. nine0003
However, antenatal use of progesterone in singleton pregnancies has been found to be associated with a reduced risk of neonatal sepsis. nine0003
British experts conducted a study to evaluate the value of progesterone in the prevention of preterm birth in twins (STOPPIT - STudy Of Progesterone for the Prevention of Preterm Birth In Twins). It was concluded that the use of progesterone in twins does not reduce the incidence of preterm birth or intrauterine fetal death up to 34 weeks. pregnancy [21]. Perhaps this is due to the insufficient dosage of progesterone preparations [3].
Differences in the biological effectiveness of progesterone in multiple and singleton pregnancies should be the subject of further research. According to the authors, such differences are associated with the predominance in the pathogenesis of preterm labor with twin overstretching of muscle fibers, while in singleton pregnancy, infectious and inflammatory processes play the main role [58]. nine0003
When prescribing progesterone preparations, the informed consent of the woman is required, since the manufacturing companies, when registering these medicines in the Russian Federation, in the indications for the use of progesterone do not indicate threatening preterm labor and the possibility of using the drugs in the second and third trimesters of pregnancy.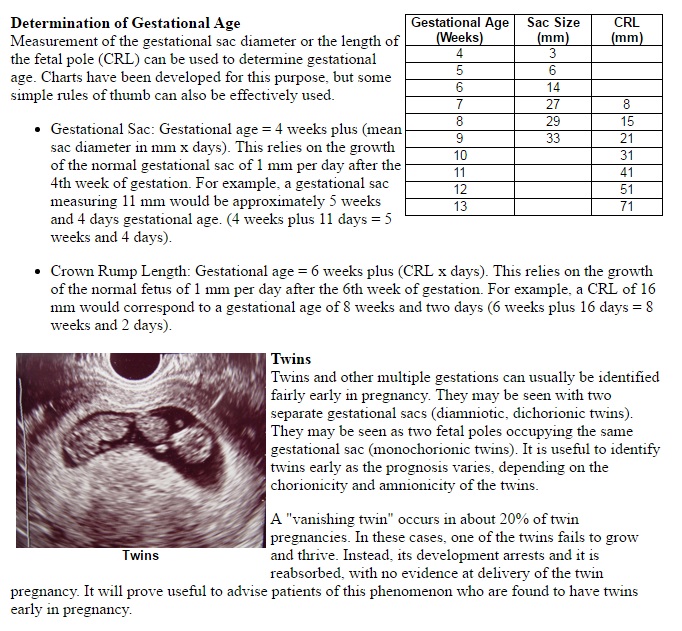
In recent years, in Russia, the most common and frequently used drug from the group of β-mimetic agents is hexoprenaline, a selective β2-sympathomimetic that relaxes the muscles of the uterus. However, according to the results of systematic reviews of randomized controlled trials, the effect of tocolytics alone on reducing the incidence of preterm birth has not been proven. The main goal of prescribing tocolysis is to delay delivery by 48 hours in order to transport the pregnant woman to the perinatal center and conduct a full course of antenatal steroids [31, 43, 56, 73]. nine0003
Risk of preterm birth: diagnostic criteria
Diagnosis of preterm labor is associated with certain difficulties, since there are no specific symptoms. The diagnosis of the onset of preterm labor can be clarified using transvaginal ultrasound with the measurement of the length of the cervix or the determination of fetal fibronectin in the cervico-vaginal secret [1, 70].
In 2010, Conde-Agudelo et al. summarized the available data on the accuracy of predicting spontaneous preterm birth in twins by measuring the length of the cervix. They conducted a systematic review and meta-analysis of 21 non-randomized studies (16 studies of pregnant women with clinical signs of possible preterm birth and 5 studies of pregnant women without symptoms of threatened miscarriage, a total of 3523 women). It was concluded that vaginal echocervicometry is a good diagnostic criterion for spontaneous preterm birth in the absence of clinical symptoms in pregnant women with twins at 20–24 weeks of gestation. [26]. nine0003
summarized the available data on the accuracy of predicting spontaneous preterm birth in twins by measuring the length of the cervix. They conducted a systematic review and meta-analysis of 21 non-randomized studies (16 studies of pregnant women with clinical signs of possible preterm birth and 5 studies of pregnant women without symptoms of threatened miscarriage, a total of 3523 women). It was concluded that vaginal echocervicometry is a good diagnostic criterion for spontaneous preterm birth in the absence of clinical symptoms in pregnant women with twins at 20–24 weeks of gestation. [26]. nine0003
In twin pregnancy, suturing the shortened cervix increases the risk of preterm birth [17].
At the same time, a number of authors describe the positive experience of applying U-shaped and circular sutures, which contribute to the prolongation of pregnancy until the birth of viable children with twins, triplets and even quadruplets [42].
In order to determine the risk of preterm birth, available express test systems are used to determine phosphorylated protein-1 that binds insulin-like growth factor (PSIFR-1) in cervical secretion [12].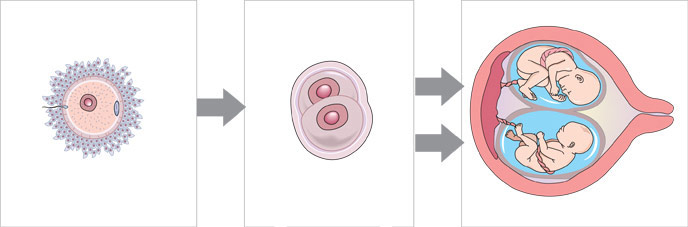 These methods increase diagnostic accuracy and reduce the risk of iatrogenic complications, as they prevent overdiagnosis of preterm labor. nine0003
These methods increase diagnostic accuracy and reduce the risk of iatrogenic complications, as they prevent overdiagnosis of preterm labor. nine0003
Two indicators are important for the diagnosis of active preterm labor: regular contractions and dynamic changes in the cervix. The degree of cervical dilation is an indicator of the prognosis of the effectiveness of tocolysis. If the opening of the pharynx is more than 3 cm, tocolysis is likely to be ineffective. Changes in the cervix are a more objective indicator than the assessment of labor activity. With a cervical length of more than 3 cm, the probability of labor onset within the next week is about 1%, which does not require hospitalization of the patient [48]. nine0003
The algorithm of actions of a doctor in case of a threat of preterm birth depends on the clinical picture, gestational age, integrity of the membranes and consists of the following main areas: risk assessment of preterm birth, prevention of RDS of the newborn, prolongation of pregnancy to transfer the mother to the perinatal center, prevention and treatment of infectious complications, in including with premature rupture of the membranes.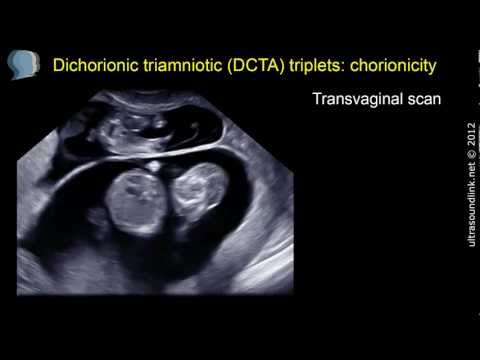
At present, the most accurate marker of preterm labor should be considered the detection of fibronectin in the cervico-vaginal secretion at gestational age up to 35 weeks, which indicates an increased risk of preterm labor, especially within 2 weeks. since the test. It is very important for clinical practice that this test has a high predictive value of a negative result - in the absence of fibronectin in the vaginal secretion, the probability that a woman will give birth within 1 week is about 1% [37]. nine0003
The appointment of antenatal steroids significantly reduces the incidence and mortality of children from RDS, IVH, NEC, and patent ductus arteriosus.
Roberts et al. in a recent meta-analysis of 21 randomized trials, a single antenatal course of steroids (betamethasone 24 mg or dexamethasone 24 mg over 48 hours) significantly reduced neonatal mortality by 31%, RDS by 34%, and early sepsis within the first 48 hours life - by 44% and the need for artificial lung ventilation - by 20%.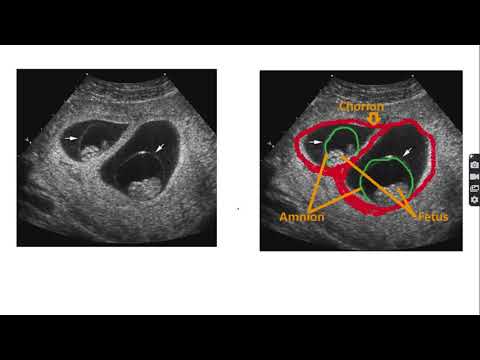 A repeated antenatal course of corticosteroids may be useful in the case when more than 7 days have passed from the previous course and symptoms of threatened preterm labor continue or reappear. nine0003
A repeated antenatal course of corticosteroids may be useful in the case when more than 7 days have passed from the previous course and symptoms of threatened preterm labor continue or reappear. nine0003
Laswell et al. in 2010, a meta-analysis was conducted of 41 publications that examined neonatal mortality among infants weighing <1500 g or <32 weeks gestation in perinatal centers compared with infants born in lower-level hospitals. The results of the meta-analysis showed that timely transportation of a pregnant woman with a high risk of preterm birth to a perinatal center is an event that significantly increases the chances of survival of a premature baby. nine0003
Antibiotic therapy for premature rupture of membranes
The effect of prescribing antibiotics in reducing the incidence of chorioamnionitis and neonatal morbidity in cases of premature rupture of membranes has been confirmed in qualitative studies.
A systematic review of 22 randomized controlled trials showed that the use of antibiotics for preterm rupture of the membranes and preterm pregnancy significantly reduces the incidence of chorioamnionitis and the number of children born within 48 hours after rupture of the membranes. In addition, the use of antibiotics in this clinical situation can reduce the incidence of neonatal infection, the need for surfactants, the use of oxygen therapy in the newborn, and the incidence of pathological symptoms in neurosonography. nine0003
In addition, the use of antibiotics in this clinical situation can reduce the incidence of neonatal infection, the need for surfactants, the use of oxygen therapy in the newborn, and the incidence of pathological symptoms in neurosonography. nine0003
All of the above suggests that those carrying multiple pregnancies are a special contingent that needs careful monitoring at all stages of pregnancy.
It is necessary to say a few words about childbirth. Undoubtedly, this group of pregnant women represents women whose caesarean section rate is much higher than in the population [13].
According to MONIIAG, in spontaneous multiple pregnancies, the percentage of spontaneous births and caesarean sections is 46.4 and 44.9, respectively.%. Delivery operations used at the birth of the second fetus account for 8.7%. Nevertheless, we do not deny the possibility of conducting childbirth through the natural birth canal. It should be noted that the course of the second stage of labor with twins is often unpredictable and uncontrollable, and much is determined by the skill of the obstetrician-gynecologist. If the doctor has the necessary skill, then both the application of a vacuum extractor to the head of the second fetus and the extraction of the second fetus by the pelvic end will be common obstetric operations that do not affect the child's condition at birth and during the period of neonatal adaptation. nine0003
If the doctor has the necessary skill, then both the application of a vacuum extractor to the head of the second fetus and the extraction of the second fetus by the pelvic end will be common obstetric operations that do not affect the child's condition at birth and during the period of neonatal adaptation. nine0003
As for multiple pregnancies that occurred as a result of IVF, in many obstetric institutions, planned abdominal delivery is carried out. Under the conditions of MORIAG, 30% of pregnant women with multiple pregnancies resulting from IVF were delivered through the natural birth canal.
It should be emphasized that in general there can be no standards in obstetrics, and clinical success is possible only with an individual, balanced and thoughtful medical approach. nine0003
Thus, patients with multiple pregnancies constitute a high-risk group for the development of maternal and perinatal complications. This is directly related to the fact that, evolutionarily, the body of a pregnant woman is adapted for bearing one fetus.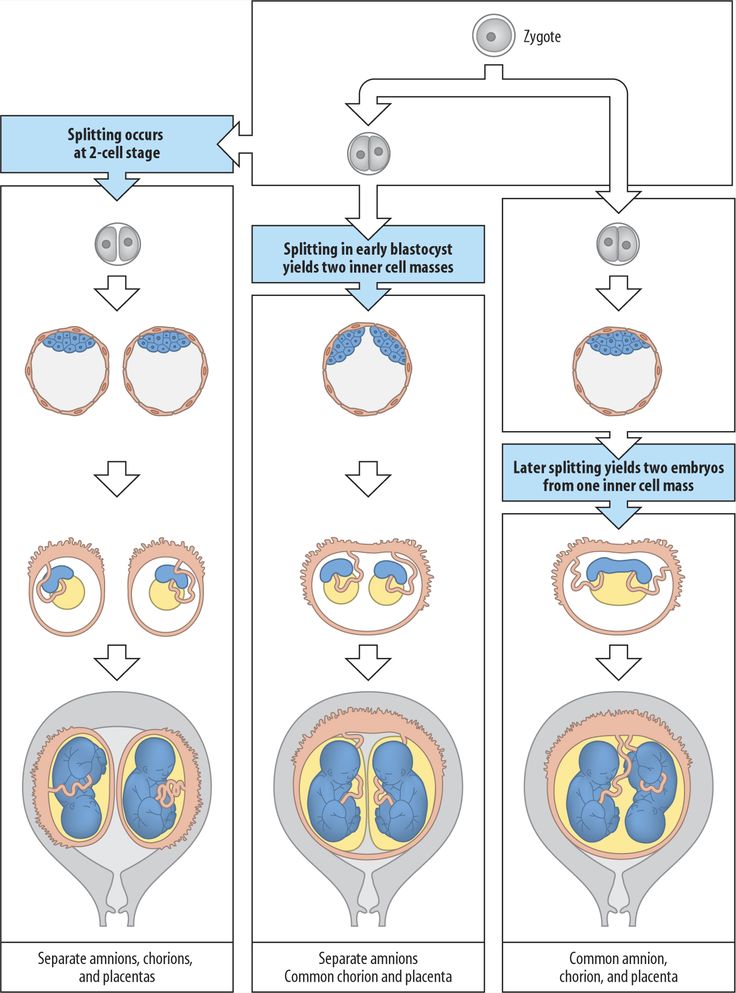



:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/674814/chart_01_large.0.png)