Skin turns white when pressed
Why Skin Turns White When Pressed
Published: 2011-06-22 - Updated: 2022-02-28
Author: Disabled World | Contact: Disabled World (Disabled-World.com)
Peer-Reviewed Publication: N/A
Additional References: Skin Conditions Publications
Synopsis: Intravascular Volume Depletion and what causes your skin to turn white in color or blanched when pressed with a finger and released. When you press on the skin, you force the blood out of the capillaries and the skin turns white. This is called blanching, blanched skin, skin blanches, or simply skin turns white. When skin is blanched, it takes on a whitish appearance as blood flow to the region is prevented. A test for blanch-ability is called Diascopy and is performed by applying pressure with a finger or glass slide and observing color changes on the skin.
advertisements
What causes your skin to turn white in color, or blanched, when pressed with a finger and released?
Related Publications:
- List of Skin Diseases and Conditions
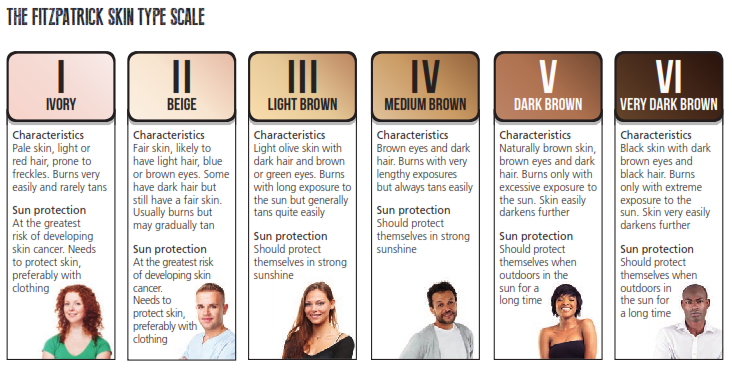
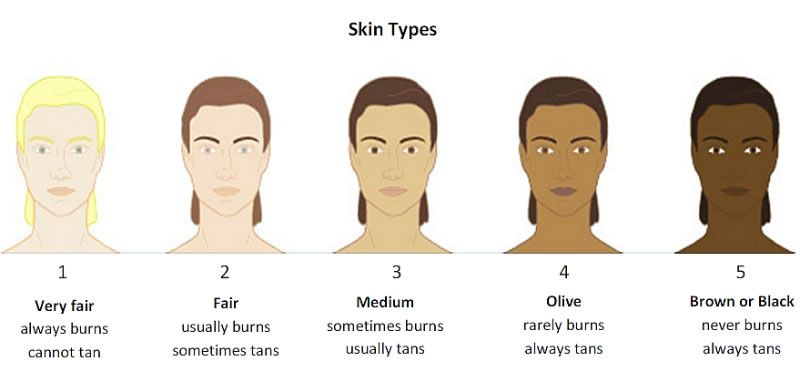
- Fitzpatrick Scale Skin Type Test and Results
- Leucoderma: White Spots or Patches on Skin
I'm sure everyone has experienced it, especially on a red spot on your skin, like a sunburn, but it can happen to people with a dark suntan as well. After applying pressure (like a poke) the skin turns white, very briefly, in the area that received the pressure.
What Causes This?
When you press on the skin, you force the blood out of the capillaries and the skin turns white. This is called blanching, blanched skin, skin blanches, or simply skin turns white.
When skin is blanched, it takes on a whitish appearance as blood flow to the region is prevented. If circulation is normal, the capillary blood comes back instantly and skin color returns. But if the blood return is sluggish, the skin stays white for several seconds and can indicate poor blood circulation. Blanching of the skin is usually a localized reaction and may be a sign that the skin tissue is not receiving its usual blood supply - poor circulation - due to swelling, cold, or other problems, such as insufficient blood flow through the vessels.
Blanching of the skin is usually a localized reaction and may be a sign that the skin tissue is not receiving its usual blood supply - poor circulation - due to swelling, cold, or other problems, such as insufficient blood flow through the vessels.
A test for blanch-ability is called Diascopy and is performed by applying pressure with a finger or glass slide and observing color changes on the skin.
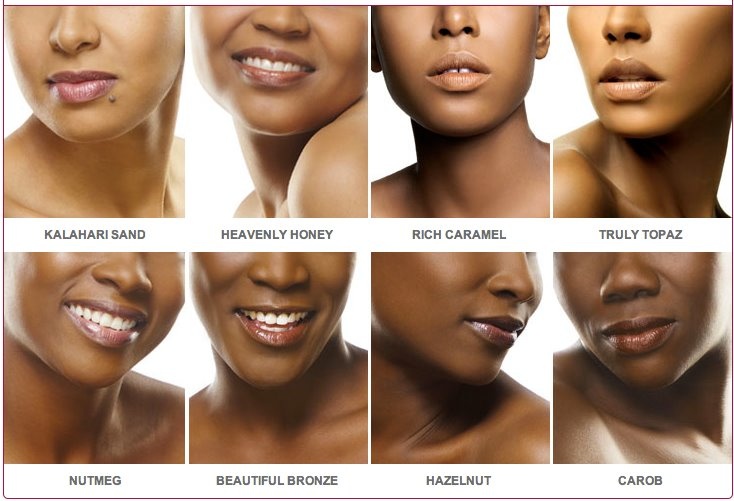
Doctors are continually developing tools for effectively measuring skin blanching in individuals with varying amounts of melanin pigment in the skin. Although a subtle symptom, blanching of the skin remains an important indicator of overall health. A comprehensive examination, history and physical are required and diagnostic studies such as laboratory tests may be necessary. Treatment will depend on the underlying condition.
Detecting changes in skin color is challenging because there is such a wide range of skin coloration in all individuals. Subtle changes like skin blanching may occur gradually over time, or there may be a sudden onset. Call 911 if Blanching of the skin is accompanied by:
Call 911 if Blanching of the skin is accompanied by:
- Chest pain.
- Sweating profusely.
- Dizziness or fainting.
- Air hunger or gasping for breath.
- Shortness of breath or breathing difficulties.
Intravascular Volume
In medicine, intravascular volume status refers to the volume of blood in a patient's circulatory system, and is essentially the blood plasma component of the overall volume status of the body, which otherwise includes both intracellular fluid and extracellular fluid. Intravascular volume depletion can exist in an adequately hydrated person if there is loss of water into interstitial tissue (e.g. due to hyponatremia or liver failure).
Intravascular Volume Depletion
Volume contraction of intravascular fluid (blood plasma) is termed hypovolemia, and its signs include:
- A fast pulse.
- A weak pulse.
- Cool extremities (e.g. cool fingers).
- Infrequent and low volume urination.
- Dry mucous membranes (e.g. a dry tongue).
- Decreased skin turgor (e.g. the skin remains "tented" when it is pinched).
- Orthostatic hypotension (dizziness upon standing up from a seated or reclining position, due to a drop in cerebral blood pressure).
- Poor capillary refill (e.g. when the patient's fingertip is pressed, the skin turns white, but upon release, the skin does not return to pink as fast as it should).
Post to Twitter Add to Facebook
advertisements
Disabled World is an independent disability community established in 2004 to provide disability news and information to people with disabilities, seniors, their family and/or carers. See our homepage for informative news, reviews, sports, stories and how-tos. You can also connect with us on Twitter and Facebook or learn more about Disabled World on our about us page.
Disabled World provides general information only. The materials presented are never meant to substitute for professional medical care by a qualified practitioner, nor should they be construed as such.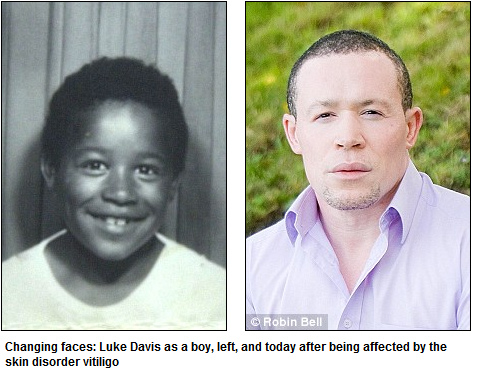 Financial support is derived from advertisements or referral programs, where indicated. Any 3rd party offering or advertising does not constitute an endorsement.
Financial support is derived from advertisements or referral programs, where indicated. Any 3rd party offering or advertising does not constitute an endorsement.
• Cite This Page (APA): Disabled World. (2011, June 22). Why Skin Turns White When Pressed. Disabled World. Retrieved January 15, 2023 from www.disabled-world.com/health/dermatology/skin/blanched-skin.php
• Permalink: <a href="https://www.disabled-world.com/health/dermatology/skin/blanched-skin.php">Why Skin Turns White When Pressed</a>
Causes and When to Seek Help
Overview
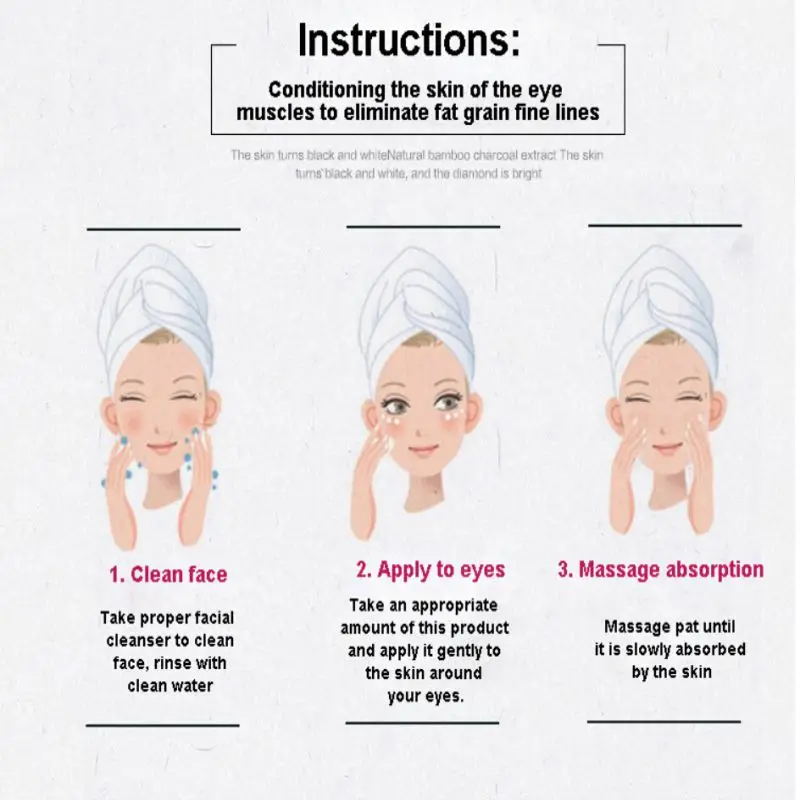
In the French language, “blanc” translates to “white.” Blanching of the skin occurs when the skin becomes white or pale in appearance.
Blanching of the skin is typically used by doctors to describe findings on the skin. For example, blood vessels, such as spider veins, on the skin can be identified easily if they are blanchable, meaning that you can make them go away by pressing on them.
Dermatologists often use a procedure called diascopy to do this.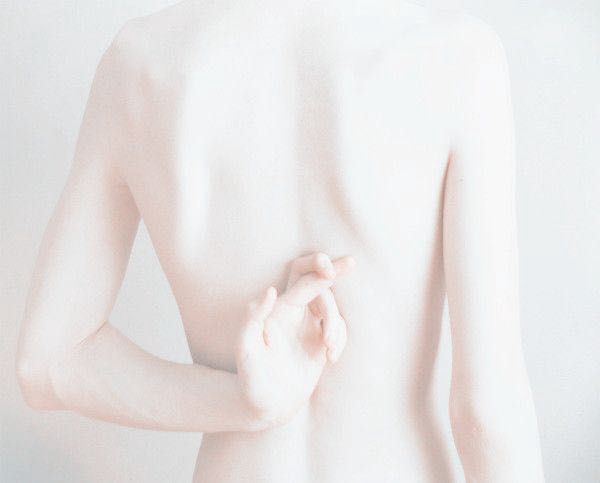 It involves pressing a glass slide on the lesion to see if it blanches or “goes away.”
It involves pressing a glass slide on the lesion to see if it blanches or “goes away.”
Blanching is also a characteristic finding in erythema, blanching redness on the skin, which essentially represents inflammation on the skin and can be present in a variety of different disorders.
When something blanches, it typically indicates a temporary obstruction of blood flow to that area. This causes the color of that area to become pale relative to the surrounding skin.
You can test this on yourself if you press gently on an area of your skin, it likely turns lighter before resuming its natural color.
Raynaud’s phenomenon
Raynaud’s phenomenon and Raynaud’s disease are associated with blanching of the skin. These conditions are marked by spasmodic constriction of the arterial blood vessels, which can cause:
- blanching of the skin
- numbness
- pain
According to the National Institutes of Health, 5 percent of Americans have Raynaud’s. The condition most commonly affects:
The condition most commonly affects:
- the fingers
- toes
However, rarely some people have symptoms on their:
- nose
- lips
- ears
Skin conditions
Several skin conditions can cause blanching of the skin:
- Frostbite is when the skin’s tissues become frozen, resulting in loss of blood flow.
- Pressure sores may be discovered in their early formation due to blanching of skin which can indicate impaired blood flow. Blanching is usually the primary indicator of an impending ulcer formation.
- Erythema represents redness on the skin that can be blanched. It can be seen in a variety of inflammatory skin disorders.
- Blood vessels on the skin, such as vascular lesions like spider veins, are blanchable. These can be seen in a variety of disorders such as rosacea, sun-damaged skin, or in liver disease. Pregnant women’s skin may also display this condition.
Blanching of the skin causes the skin to appear white or paler than usual, depending on your skin tone. The skin may feel cool to the touch if blood flow is affected.
Seek immediate medical attention if you or a loved one experiences any of the following symptoms in addition to blanching of skin:
- ulcers forming on the areas of blanched skin, such as the fingertips
- severe pain
A doctor diagnoses blanching of skin by conducting a physical examination to determine potential causes. They’ll examine how the skin looks around the blanched area and request your medical history to determine any conditions that may contribute to the blanching of skin.
Treatments for blanching of skin depend upon the underlying cause. For example, in Raynaud’s phenomenon, lifestyle changes, such as avoiding the cold can be a treatment method. Amlodipine is a blood pressure pill used off-label to help treat the condition.
For Raynaud’s phenomenon, keep the skin warm through:
- layering
- wearing mittens or warm socks
- refraining from staying in the cold too long
For pressure ulcers, people who have to remain in bed due to a health condition require frequent turning to keep excess pressure from causing bedsores.
Pressure points such as the buttocks, elbows, and the heels are vulnerable to pressure that can cause wounds known as decubitus ulcers.
Blanching of the skin is typically a sign of restricted blood flow to an area of the skin causing it to become paler than the surrounding area. See your doctor if you believe that you may have a condition causing blanching of the skin.
Dermographic urticaria: modern ideas about the diagnosis and treatment of the disease | #04/16
Chronic urticaria is accompanied by the appearance of itchy blisters and / or angioedema for more than 6 weeks. It can be spontaneous or induced. The latter includes symptomatic/urticarial dermographism (syn. urticaria factitia , mechanical urticaria, dermographic urticaria (DK)), cold, pressure-delayed, solar, heat, cholinergic, contact urticaria, and vibratory angioedema. nine0005
In a broad sense, dermographism is a local reaction of skin vessels in the form of bands of different (usually red or white) colors at the site of dashed mechanical skin irritation. A change in skin color at the site of mechanical action in dermographism is due to a reaction (spasm or expansion) of the arterial and venous vessels of the skin.
A change in skin color at the site of mechanical action in dermographism is due to a reaction (spasm or expansion) of the arterial and venous vessels of the skin.
When talking about dermographism in relation to urticaria, it refers to a condition in which itching and blisters occur within a few minutes after mechanical irritation of the skin, for example, with a blunt object or clothing. It is customary to divide dermographism into urticarial, that is, symptomatic with the development of a blister-erythema-itch reaction in the area of skin irritation, and non-urticarial (white, red and black). nine0005
Separately, simple dermographism is considered, which occurs in 2-5% of healthy individuals in response to significant (medium and strong) mechanical irritation of the skin in the form of erythema and blisters in the contact area. Despite the absence of itching (an important diagnostic sign of the condition), the reaction can be quite noticeable. It is believed that this response is associated with a physiological overreaction of the skin. Treatment in this case, as a rule, is not required.
Treatment in this case, as a rule, is not required.
In contrast to simple dermographism, DC almost always presents with both pruritus and blistering and erythema, and mild skin irritation is often required for a reaction to occur. nine0005
DC is considered the most common form of induced urticaria, with a prevalence of 4.2–17% and a median duration of about 6 years. DC is most common at a young age, can coexist with other types of disease, such as chronic spontaneous urticaria, and can lead to a significant reduction in quality of life.
As with other types of urticaria, the pathogenesis of DC is associated with degranulation of mast cells and the release of biologically active substances, primarily histamine, which leads to symptoms of the disease. Currently, it is assumed that the formation of an antigen (“self-allergen”), which is released during mechanical stimulation of the skin, leads to the degranulation of mast cells, which causes the formation of specific IgE antibodies directed against this antigen. The role of IgG/IgM antibodies is discussed. nine0005
The role of IgG/IgM antibodies is discussed. nine0005
DC is usually idiopathic. In other cases, the disease may occur in a transient short form after taking certain drugs, such as penicillin and famotidine, with scabies, mastocytosis, dermatomyositis, injuries, such as coral reef, insect bites / stings.
DC manifests itself in the form of typical blisters and itching, repeating the trace of an irritating object. Manifestations of the reaction increase within 5–10 min after exposure to the stimulus and resolve in 30–60 min (Fig. 1). Sometimes the patient may complain of severe itching even in the absence of visible rashes and swelling on the skin. Blisters can be of various shapes: oblong, linear, square, diamond-shaped, etc. Rashes often appear in places of friction, compression by clothing (for example, underwear), when wearing watches, socks, and also around the belt and sometimes when swimming in the shower or when drying with a towel afterwards. Touching the face, scratching, or rubbing slightly itchy eyelids or lips can lead to dermographic angioedema. nine0005
nine0005
Diagnostics
To confirm the diagnosis, it is necessary to conduct a provocative test. It is advisable that the patient stop taking antihistamines (AHP) at least 2-3 days before the study.
A calibrated instrument, a dermographometer, is used to accurately diagnose dermographism. It looks like a pen with a steel smooth tip 0.9 mm in diameter (Fig. 2). The pressure at the tip can be changed by turning the screw on the top of the instrument. Scale values from 0 to 15 are equal to the corresponding tip pressure values from 20 to 160 g/mm 2 .
With the help of a dermographometer, dashed skin irritation is performed in the region of the upper back in the form of three parallel lines (up to 10 cm long) with a pressure of 20, 35 and 60 g/mm2, respectively. A positive result in the case of DC will appear in the area of provocation within 10 to 15 minutes as linear pruritic blistering and erythema at pressures of 36 g/mm 2 (353 kPa) or less. An urticarial reaction without itching on provocation of 60 g/mm 2 (589 kPa) or more is indicative of simple dermographism. The result is evaluated 10 minutes after testing. nine0005
An urticarial reaction without itching on provocation of 60 g/mm 2 (589 kPa) or more is indicative of simple dermographism. The result is evaluated 10 minutes after testing. nine0005
When a dermographometer is not available, the test can be performed using any smooth, blunt object such as a ballpoint pen or wooden spatula (Figure 3). The combination of pruritus, blistering, and erythema confirms the diagnosis. A new provocative testing device, the FricTest®, has recently been developed. This simple and inexpensive tool can reliably confirm the diagnosis of DC.
Overview of modern treatments
After establishing the diagnosis, it is necessary to explain to the patient the mechanism of the development of the disease, recommend the exclusion of provoking factors, such as mechanical irritation of the skin, and clarify the possibility of reducing the severity of stress and anxiety. nine0005
Histamine is the main mediator that is involved in the development of symptoms of DC, so the disease usually responds well to antihistamine therapy (AHP), as well as other forms of urticaria. The goal of treatment is to reduce the severity of itching and rashes as much as possible, although even with therapy, slight erythema and itching may persist.
The goal of treatment is to reduce the severity of itching and rashes as much as possible, although even with therapy, slight erythema and itching may persist.
It is advisable to start therapy with standard daily doses of non-sedating 2nd generation antihistamines (drugs of choice), from the use of which in most cases a good effect is observed. Schoepke et al. noted an improvement in the course of DC in more than 49% of patients receiving antihistamines. Drugs can be prescribed for several months if the disease flows for a long time, or as needed for episodic symptoms. Since itching tends to increase at certain times of the day, more often in the evening, an antihistamine may be recommended 1 hour before its peak, including 1st generation antihistamines with a sedative effect, such as hydroxyzine. In a more severe course of the disease, it is possible to use off-label high daily doses of antihistamines (in this case, drugs are prescribed with an interval of 12, not 24 hours). A combination of two or more antihistamines may be required. nine0005
A combination of two or more antihistamines may be required. nine0005
An additional effect may appear when histamine H2 receptor blockers, such as ranitidine, famotidine, or cimetidine, are added to the treatment. However, this treatment has not been shown to be effective in all studies.
Omalizumab, a monoclonal anti-IgE antibody, has been successfully used to treat patients with induced urticaria, including DC, at a dose of 150–300 mg. Many patients noted a complete resolution of the symptoms of the disease within a few days after the first injection. No significant side effects were identified. nine0005
There is a positive experience with the use of ketotifen. In separate studies, scientists have noted the effectiveness of ultraviolet radiation and PUVA therapy. However, in most patients, improvement was transient and DC symptoms recurred 2–3 days after phototherapy was discontinued.
Lawlor et al. did not note a significant improvement in the course of DC in the treatment of calcium channel blocker nifedipine.
The effectiveness of antileukotriene drugs, cyclosporine, and IV immunoglobulin, which are used in other types of urticaria, is not yet known. nine0005
Conclusion
Thus, DC can lead to a decrease in the quality of life, but is not a life-threatening disease and has a favorable prognosis. The diagnosis of the disease is made on the basis of the clinical picture and the results of provocative tests. In the absence of an apparent cause of DC, it is important to choose and continue adequate therapy until spontaneous remission occurs. The drugs of choice are 2nd generation antihistamines with a possible increase in their dose and / or the appointment of alternative treatment (eg, omalizumab, histamine H2 receptor blockers) in resistant and severe cases. Further research is needed to develop pathogenetically sound treatments for DC. nine0005
Literature
- Zuberbier T., Aberer W., Asero R., Bindslev-Jensen C., Brzoza Z.
 , Canonica G. W., Church M. K., Ensina L. F., Gimenez-Arnau A., Godse K., Goncalo M., Grattan C., Hebert J., Hide M., Kaplan A., Kapp A., Abdul Latiff A. H., Mathelier-Fusade P., Metz M., Nast A., Saini S. S., Sanchez-Borges M., Schmid-Grendelmeier P., Simons F. E., Staubach P., Sussman G., Toubi E., Vena G. A., Wedi B., Zhu X. J., Maurer M. The EAACI/GA (2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update // Allergy. 2014; 69: 868–887.
, Canonica G. W., Church M. K., Ensina L. F., Gimenez-Arnau A., Godse K., Goncalo M., Grattan C., Hebert J., Hide M., Kaplan A., Kapp A., Abdul Latiff A. H., Mathelier-Fusade P., Metz M., Nast A., Saini S. S., Sanchez-Borges M., Schmid-Grendelmeier P., Simons F. E., Staubach P., Sussman G., Toubi E., Vena G. A., Wedi B., Zhu X. J., Maurer M. The EAACI/GA (2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update // Allergy. 2014; 69: 868–887. - Dontsov R. G., Uryvaev Yu. V. Dermography in healthy people: dependence of types of reactions of skin vessels on the strength of irritation // Ros. physiol. magazine 2006: 232–237.
- Taskapan O., Harmanyeri Y. Evaluation of patients with symptomatic dermographism // J Eur Acad Dermatol Venereol. 2006; 20:58–62.
- Breathnach S. M., Allen R., Ward A. M., Greaves M. W. Symptomatic dermographism: natural history, clinical features laboratory investigations and response to therapy // Clin Exp Dermatol.
 nineteen83; 8:463–476.
nineteen83; 8:463–476. - Silpa-archa N., Kulthanan K., Pinkaew S. Physical urticaria: prevalence, type and natural course in a tropical country // J Eur Acad Dermatol Venereol. 2011; 25:1194–1199.
- Humphreys F., Hunter J. A. The characteristics of urticaria in 390 patients // Br J Dermatol. 1998; 138:635–668.
- Kozel M. M., Mekkes J. R., Bossuyt P. M., Bos J. D. The effectiveness of a history-based diagnostic approach in chronic urticaria and angioedema // Arch Dermatol. nineteen98; 134: 1575–1580.
- Schoepke N., Mlynek A., Weller K., Church M. K., Maurer M. Symptomatic dermographism: an inadequately described disease // J Eur Acad Dermatol Venereol. 2015; 29:708–712.
- Zuberbier T., Grattan C., Maurer M. Urticaria and Angioedema // Dordrecht: Springer. 2010: 1 online resource (156 p.).
- Horiko T., Aoki T. Dermographism (mechanical urticaria) mediated by IgM // Br J Dermatol.
 nineteen84; 111:545–550.
nineteen84; 111:545–550. - Grimm V., Mempel M., Ring J., Abeck D. Congenital symptomatic dermographism as the first symptom of mastocytosis // Br J Dermatol. 2000; 143:1109.
- Rahim K. F., Dawe R. S. Dermatomyositis presenting with symptomatic dermographism and raised troponin T: a case report // J Med Case Rep. 2009; 3: 7319.
- Colhir P. V. Urticaria and angioedema. M.: Practical medicine, 2012. nine0069 James J., Warin R. P. Factitious wealing at the site of previous cutaneous response // Br J Dermatol. 1969; 81:882–884.
- Borzova E., Rutherford A., Konstantinou G. N., Leslie K. S., Grattan C. E. Narrowband ultraviolet B phototherapy is beneficial in antihistamine-resistant symptomatic dermographism: a pilot study // J Am Acad Dermatol. 2008; 59:752–757.
- Schoepke N., Abajian M., Church M. K., Magerl M. Validation of a simplified provocation instrument for diagnosis and threshold testing of symptomatic dermographism // Clin Exp Dermatol.
 2015; 40:399–403.
2015; 40:399–403. - Kolkhir P. V., Kochergin N. G., Kosoukhova O. A. Antihistamines in the treatment of chronic urticaria: a review of the literature // Treating Physician. 2014: 25.
- Boyle J., Marks P., Gibson J. R. Acrivastine versus terfenadine in the treatment of symptomatic dermographism — a double-blind, placebo-controlled study // J Int Med Res. 1989; 17 Suppl 2: 9B-13B.
- Matthews C. N., Boss J. M., Warin R. P., Storari F. The effect of h2 and h3 histamine antagonists on symptomatic dermographism // Br J Dermatol. 1979; 101:57–61.
- Sharpe G. R., Shuster S. In dermographic urticaria h3 receptor antagonists have a small but therapeutically irrelevant additional effect compared with h2 antagonists alone // Br J Dermatol. 1993; 129:575–579.
- Metz M., Altrichter S., Ardelean E., Kessler B., Krause K., Magerl M., Siebenhaar F., Weller K., Zuberbier T.
 , Maurer M. Anti-immunoglobulin E treatment of patients with recalcitrant physical urticaria // Int Arch Allergy Immunol. 2011; 154:177–180.
, Maurer M. Anti-immunoglobulin E treatment of patients with recalcitrant physical urticaria // Int Arch Allergy Immunol. 2011; 154:177–180. - Vieira Dos Santos R., Locks Bidese B., Rabello de Souza J., Maurer M. Effects of omalizumab in a patient with three types of chronic urticaria // Br J Dermatol. 2014; 170:469–471.
- Metz M., Ohanyan T., Church M. K., Maurer M. Retreatment with omalizumab results in rapid remission in chronic spontaneous and inducible urticaria // JAMA Dermatol. 2014; 150:288–290.
- Cap J. P., Schwanitz H. J., Czarnetzki B. M. Effect of ketotifen in urticaria factitia and urticaria cholinergica in a crossover double-blind trial // Hautarzt. 1985; 36:509–511.
- Logan R. A., O’Brien T. J., Greaves M. W. The effect of psoralen photochemotherapy (PUVA) on symptomatic dermographism // Clin Exp Dermatol. 1989; 14:25–28.
- Lawlor F., Ormerod A.
 D., Greaves M. W. Calcium antagonist in the treatment of symptomatic dermographism. Low-dose and high-dose studies with nifedipine // Dermatologica. nineteen88; 177:287–291.
D., Greaves M. W. Calcium antagonist in the treatment of symptomatic dermographism. Low-dose and high-dose studies with nifedipine // Dermatologica. nineteen88; 177:287–291.
O. Yu. Candidate of Medical Sciences
First Moscow State Medical University named after I. M. Sechenov Ministry of Health of the Russian Federation, Moscow
1 Contact information: [email protected]
13 Symptoms of internal diseases - KP.ru
Komsomolskaya Pravda
Health Healthcard Pavlova
Oleg Kolesov
March 20, 2017 0:06
Leather - an important indicator of your health, do not miss the signals that your own gives you their own organism!
The skin is an important indicator. Photo: EAST NEWS
Jerome K was right after all. Jerome: sometimes you can diagnose yourself, even without going to the doctor. And for this it is not at all necessary to read a medical encyclopedia.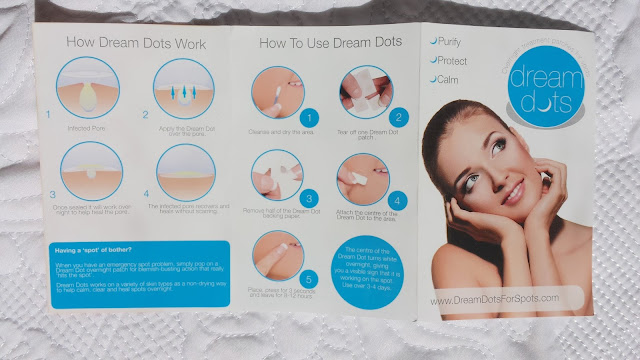 You just need to go to the mirror and take a closer look at yourself. Scientists at Washington University in St. Louis say that the skin is an indicator of a person's overall health. And often just a glance at the face is enough to determine what diseases this or that person suffers from. nine0005
You just need to go to the mirror and take a closer look at yourself. Scientists at Washington University in St. Louis say that the skin is an indicator of a person's overall health. And often just a glance at the face is enough to determine what diseases this or that person suffers from. nine0005
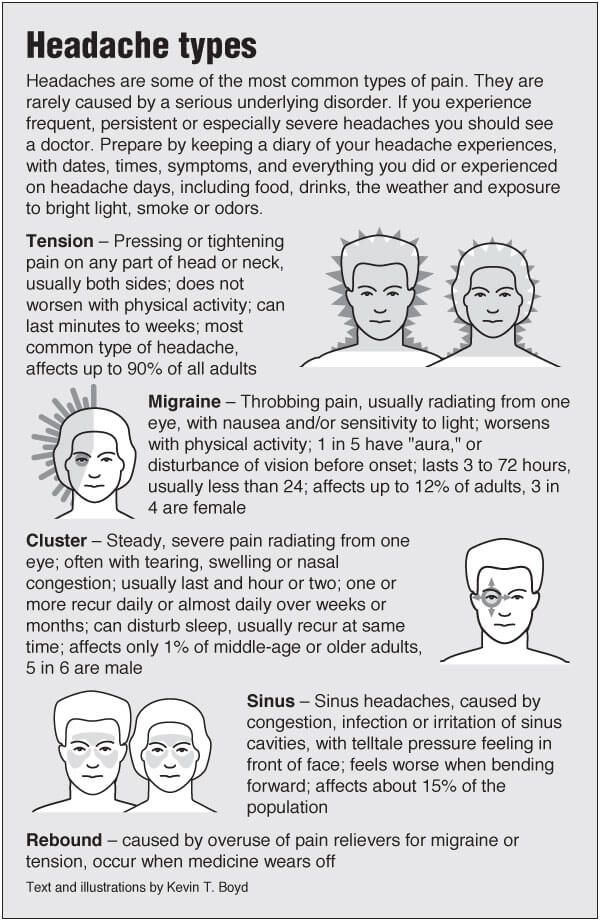
A NETWORK OF SMALL PREMATURE WRINKLES ALL OVER THE FACE
The first sign of body dehydration is probably known to everyone. However, sometimes such a symptom can indicate a more serious problem. For hypothyroidism. Or, in other words, insufficient levels of thyroid hormones. This disease is often accompanied by a constant feeling of cold, weight gain, frequent fatigue.
“ Diabetes also has a network of microwrinkles ,” warns MD, Associate Professor at NYU School of Medicine Roshini Raj .
EXCESS FACIAL HAIR
Unwanted hair, especially along the jaw line and upper lip, as well as in the sideburn area, is the first sign that a woman is not all right with her hormones (so-called hirsutism).
It can also be a symptom of polycystic ovary syndrome.
YELLOW BUCKLES AROUND THE EYES
Xanthelasma, as they are scientifically called, are signs of high cholesterol levels in the body. And, therefore, a harbinger of cardiovascular disease and heart attack. nine0005
As proof, the University of Washington cites a 2011 Danish study of 13,000 patients who had similar yellow patches around the eyes. Tests of volunteers showed that 70 percent of them were at high risk of developing arteriosclerosis (hardening of the arteries), and almost half of them were at risk of a heart attack in the next decade.
ASYMMETRY OF THE FACE
« This may be one of the first signs of a nervous disease and even a stroke ,” says Liana Wen , MD, emergency physician at George Washington University, and adds:
- Some of my patients often describe it like this: “I looked in the mirror and saw another person in the reflection. ” And someone just starts to feel that one side of the face is numb. Still others cannot smile in full force. Four have speech problems. If you, God forbid, encounter one of these symptoms, immediately call an ambulance - the first four hours after a stroke are the most important for saving a person. nine0004
” And someone just starts to feel that one side of the face is numb. Still others cannot smile in full force. Four have speech problems. If you, God forbid, encounter one of these symptoms, immediately call an ambulance - the first four hours after a stroke are the most important for saving a person. nine0004
COLOR CHANGES
Constant pallor often indicates that a person has anemia.
Yellowness indicates problems with the liver, most likely, it ceases to properly process red blood cells, which can threaten hepatitis, cirrhosis or liver cancer.
By the way, the yellowed sclera of the eyes can also speak about this.
But bluish skin and blueness on the lips or near the nail bed can indicate heart problems or lung disease, says Dr. Mallika Marshall, an internist and pediatrician at Massachusetts General Hospital.
Pale lips indicate a lack of iron in the body.
RED SPOTS
Often similar to impact marks, they cause not only aesthetic inconvenience, but also physical, because they cause itching. This indicates certain problems with digestion, and very serious ones. We can talk about celiac disease, an autoimmune disease in which the body reacts incorrectly to gluten. nine0005
CLUSTER OF EXTENDED CAPILLARIES
At some point there are so many of them that from the "constellation" it becomes like a spot, or even several. They are on the same level with the skin and are not palpable. The medical name for this phenomenon is erythema.
May be due to capillary dilation due to increased blood flow. But sometimes it becomes a symptom of several inflammations at once, including the intestines, sarcoidosis, and various infections.
BROWN SPOTS OR PAPULES
This is most likely a manifestation of seborrheic keratosis. And he, in turn, can indicate not only age-related changes in the skin (the main symptom), but also a serious problem in the body - cancer.
" These papules are especially associated with adenocarcinoma ," warns MD, MD, Harvard Medical School Elizabeth H. Page .
Of course, most often these "senile warts" are an age-related manifestation, but still, if they appear, you should check with a doctor just in case. nine0005
STRONG PIGMENTATION
Moreover, pigmentation is not just spots - the skin begins to darken in whole areas. Perhaps this suggests that the mechanisms of the development of Addison's disease have started in the body. It is accompanied by a malfunction of the adrenal cortex or pituitary gland.
ACNE IN ADULTY
Acne in adolescence is a common and understandable phenomenon. Another thing is if such a “nuisance” jumps up in a woman over 30 years old. This may be a sign of both strong hormonal changes and, second, problems in the gastrointestinal tract, explains Dr. Derick, co-author of the study at the University of Washington. nine0005
nine0005
He also says that women with acne should definitely get checked out by a gynecologist because PCOS or some other reproductive system problem could also be the cause.
RED SPOT "BUTTERFLY"
Symmetrical spots on the cheeks or cheekbones, which are connected on the bridge of the nose in the form of a butterfly, often speak of rosacea, that is, circulatory disorders.
But this type is also characteristic of discoid and disseminated lupus erythematosus, an autoimmune disease with a violation of the DNA of healthy cells. It's worth checking out just in case! nine0005
DARK CIRCLES AROUND THE EYES
Most often this is, of course, the cause of lack of sleep, poor lifestyle or simply a genetic factor. However, dark circles can also accompany diseases of the kidneys and adrenal glands. Such pathologies require accurate diagnosis and treatment.
SLOW CHIN
Together with such features as a thick neck and a small jaw, it can speak of sleep apnea, a disorder in which a person's breathing stops for several seconds and repeatedly during sleep.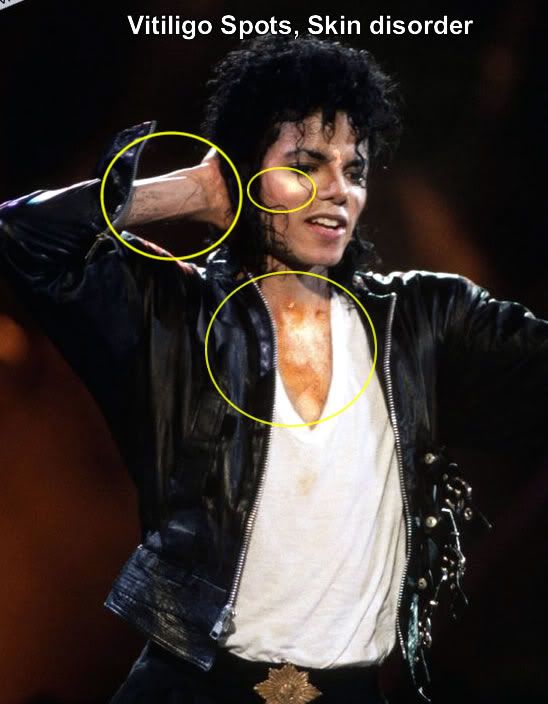 nine0005
nine0005
OPINION OF SPECIALISTS
Dermatologist, Ph.D. Marina BOGARAZ:
“Human skin is the largest organ of the body, constantly growing and renewing. At the same time, the skin is connected with almost all organs of the body, if not directly, then with vessels and blood circulation, which is why the epidermis gives an idea of what is happening in the body - from stress levels and your addictions to serious diseases.
However, skin diagnosis can only be primary. Only a doctor can make a final diagnosis, especially since one symptom may be associated with more than one disease, and making a diagnosis will require not only a medical examination, but also tests. nine0005
Zukhra PAVLOVA, PhD, endocrinologist Systemic Medicine Clinic:
It's true, the skin is an indicator of human health. But to make a final diagnosis without a doctor is really not worth it. And to the symptoms mentioned above, I would also add that premature wrinkles can also be a manifestation of a decrease in the level of sex hormones, which largely determine the beautiful, elastic, healthy skin of a person in his youth.
Excess facial hair - a signal of congenital dysfunction of the adrenal cortex.
Facial asymmetry, of course, first of all suggests a neurological problem, but sometimes it can also be a consequence of injuries. So do not jump to conclusions when talking to a stranger.
As for the change in complexion, here you can add changes in the skin around the eyes with a characteristic brown tint - often this accompanies Jellinek's symptom, diffuse toxic goiter. Or this still happens with the syndrome of "fatigue" of the adrenal glands, the so-called Adrenal Fatigue. nine0005
Red spots on the face can be a manifestation of mycoses or, in other words, a fungal infection of the skin, which is often disguised as other diseases, such as eczema or acne, and therefore is not properly treated.
As for age-related acne , in the case of hormonal disorders, an imbalance of steroid and androgenic hormones comes to the fore.
Age category of the site 18+
Online publication (website) registered by Roskomnadzor, certificate El No. FS77-80505 dated March 15, 2021
CHIEF EDITOR OLESIA VYACHESLAVOVNA NOSOVA.
EDITOR-IN-CHIEF OF THE SITE - KANSK VICTOR FYODOROVICH.
THE AUTHOR OF THE MODERN VERSION OF THE EDITION IS SUNGORKIN VLADIMIR NIKOLAEVICH.
Messages and comments from site readers are posted without preliminary editing. The editors reserve the right to remove them from the site or edit them if the specified messages and comments are an abuse of freedom mass media or violation of other requirements of the law. nine0005
JSC "Publishing House "Komsomolskaya Pravda". TIN: 7714037217 PSRN: 1027739295781 127015, Moscow, Novodmitrovskaya d. 2B, Tel. +7 (495) 777-02-82.
Exclusive rights to materials posted on the website www.kp.ru, in accordance with the legislation of the Russian Federation for the Protection of the Results of Intellectual Activity belong to JSC Publishing House Komsomolskaya Pravda, and do not be used by others in any way form without the written permission of the copyright holder.


:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/674814/chart_01_large.0.png)