What stimulates breast milk
Causes & How It Works
Overview
Lactation is the process of making human milk. It's driven by hormones and results in milk coming from your nipple.What is lactation?
Lactation is the process of producing and releasing milk from the mammary glands in your breasts. Lactation begins in pregnancy when hormonal changes signal the mammary glands to make milk in preparation for the birth of your baby. It’s also possible to induce lactation without a pregnancy using the same hormones that your body makes during pregnancy. Lactation ends once your body stops producing milk.
Feeding your baby directly from your breasts is called breastfeeding (or sometimes chestfeeding) or nursing. You can also feed your baby milk that you have expressed or pumped from your breast and saved in a bottle.
Where does human milk come from?
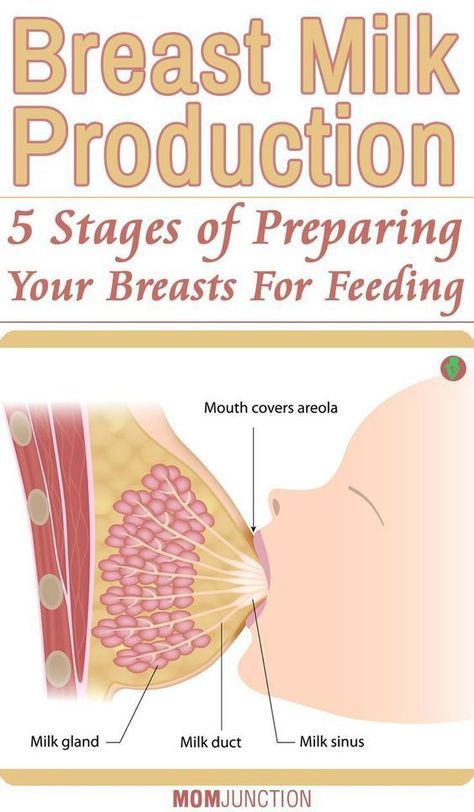
Human milk comes from your mammary glands inside your breasts. These glands have several parts that work together to produce and secrete milk:
- Alveoli: These tiny, grape-like sacs produce and store milk.
A cluster of alveoli is called lobules, and each lobule connects to a lobe.
- Milk ducts: Each lobe connects to a milk duct. You can have up to 20 lobes, with one milk duct for every lobe. Milk ducts carry milk from the lobules of alveoli to your nipples.
- Areola: The dark area surrounding your nipple, which has sensitive nerve endings that lets your body know when to release milk. To release milk, the entire areola needs stimulation.
- Nipple: Your nipple contains several tiny pores (up to about 20) that secrete milk. Nerves on your nipple respond to suckling (either by a baby, your hands or a breast pump). This stimulation tells your brain to release milk from the alveoli through the milk ducts and out of your nipple.
It helps to think of the lactation system as a large tree. Your nipple is the trunk of the tree. The milk ducts are the branches. The leaves are the alveoli.
Why do people lactate?
The primary reason people lactate is to feed a baby. Lactation is a biological, hormonal response that occurs during and after pregnancy to feed a newborn baby. Your body triggers specific hormones to initiate milk production and ejection (releasing of milk). All mammals lactate for this purpose and it’s possible to induce lactation in men and in non-pregnant women using the right hormone medications.
Lactation is a biological, hormonal response that occurs during and after pregnancy to feed a newborn baby. Your body triggers specific hormones to initiate milk production and ejection (releasing of milk). All mammals lactate for this purpose and it’s possible to induce lactation in men and in non-pregnant women using the right hormone medications.
Function
What triggers lactation?
A series of hormonal events, which begin when you’re pregnant, trigger the lactation process. That process is called lactogenesis.
Stage one lactogenesis: This begins around the 16th week of pregnancy and lasts until a few days after you give birth.
- Estrogen and progesterone rise and cause your milk ducts to grow in number and size. This causes your breasts to become fuller. Your mammary glands begin to prepare for milk production.
- Your nipples darken and your areolas become larger.
- Your Montgomery glands (small bumps on the areola) secrete oil to lubricate your nipple.
- Your body begins making colostrum. It’s highly nutritious and filling and serves as your baby’s first milk.
Stage two lactogenesis: This stage starts about two or three days postpartum (after giving birth). It’s when milk production intensifies.
- Once your baby and placenta are delivered, a sudden drop in your estrogen and progesterone causes the hormone prolactin to take over.
- Prolactin is the hormone that produces milk.
- You’ll notice your milk production increases dramatically at this stage. It’s often referred to as milk “coming in.”
- Your breasts are often engorged (or overly full of milk) to the point where they feel sore, painful or tender.
Stage three lactogenesis: This describes the rest of the time you lactate.
- Lactation generally continues as long as milk is removed from your breast.
- The more milk that’s removed, the more milk your body makes to replace it. Frequent feeding or pumping will cause your body to make more milk.
Hormones for lactation
The hormone prolactin controls the amount of milk you produce, and your body begins producing prolactin early in pregnancy. At first, the high levels of estrogen, progesterone and other pregnancy hormones suppress prolactin. Once you deliver the placenta, those pregnancy hormones drop and prolactin takes charge.
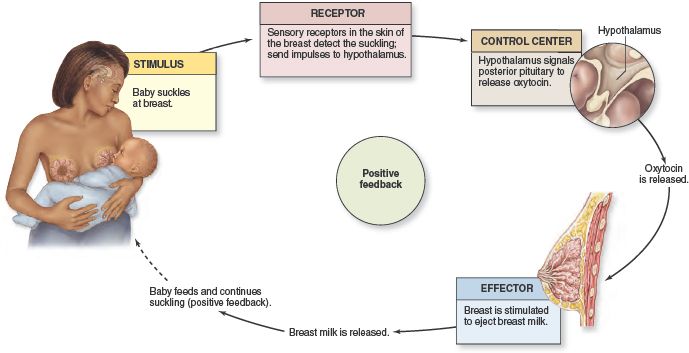
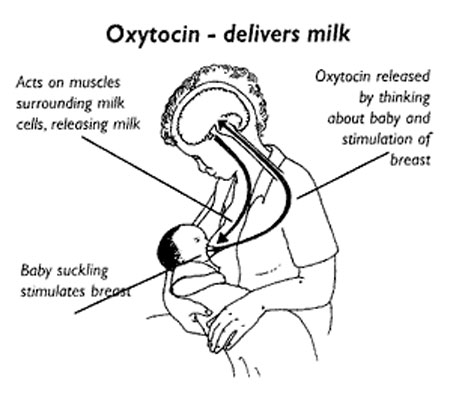
When your baby suckles, it stimulates nerves that tell your body to release prolactin and oxytocin. Prolactin causes the alveoli to make milk and oxytocin causes muscle contractions that push out of the alveoli and through the milk ducts.
When milk is released, it’s called a “letdown,” and it takes about 30 seconds of suckling before the letdown occurs. Because you can’t control which breast receives the hormones, the letdown can cause milk to drip from both nipples.
Inducing lactation in people who aren’t pregnant requires medication that mimics hormones your body makes during pregnancy. Suckling from the nipple can initiate lactation, either with a breast pump or by a baby. This is a complex process that involves working closely with a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
This is a complex process that involves working closely with a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
When do you lactate during pregnancy?
Lactation begins as early as a few weeks into the second trimester of your pregnancy. As estrogen and progesterone levels rise, your body prepares for lactation by increasing the number of milk ducts in your breasts, and those milk ducts will transport milk from the alveoli to your nipples. About midway through pregnancy, your body creates colostrum, which is your baby’s first milk.
Can you lactate when you’re not pregnant?
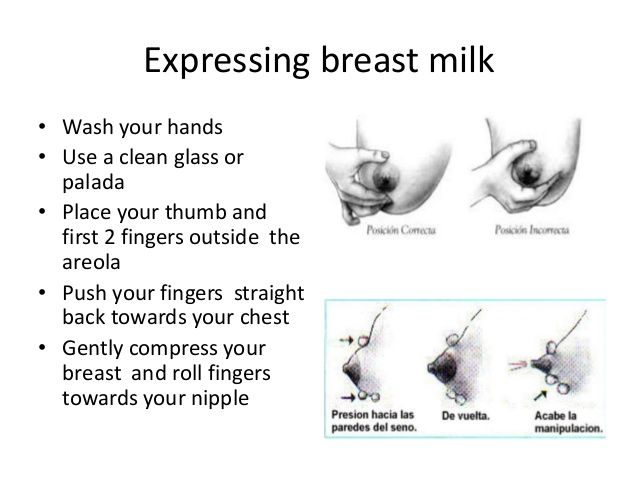
Yes, it’s possible to lactate if you’re not pregnant. Inducing lactation is a complex process that usually involves using hormone-mimicking drugs for several months to produce milk. The second part of lactation is expressing the milk through your nipple. Stimulation from infant suckling, pumping with a breast pump or hand-expressing signals the brain to release the milk.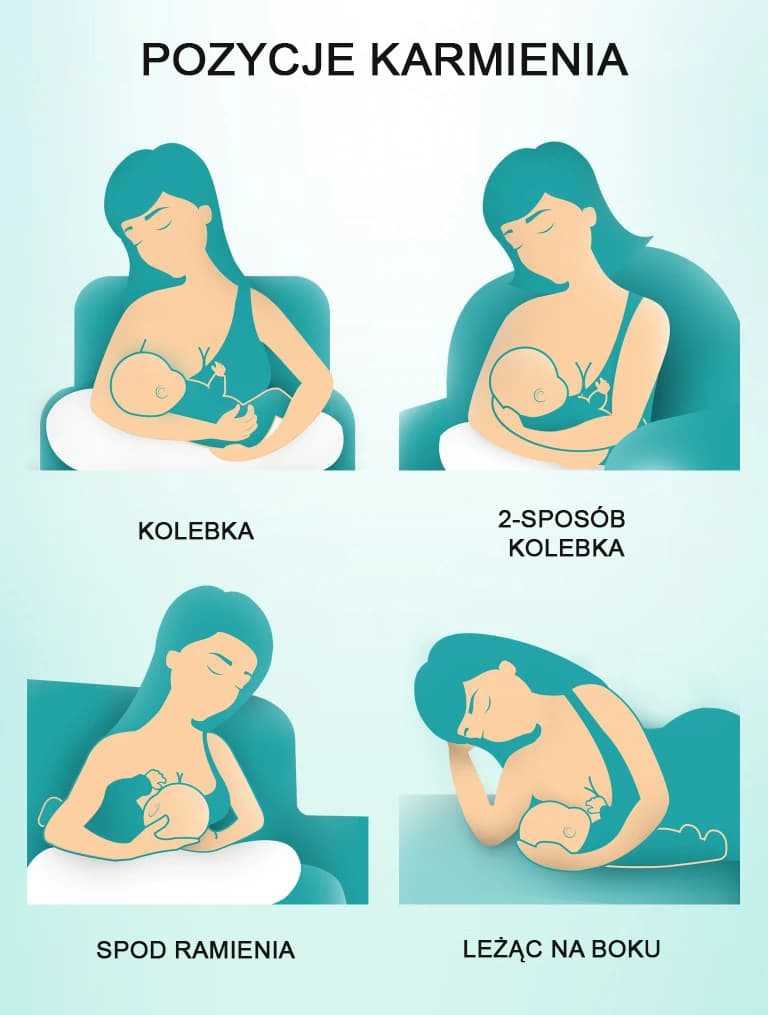 It’s common for people in this situation to receive assistance from a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
It’s common for people in this situation to receive assistance from a healthcare provider who understands the needs of non-pregnant people and has experience initiating lactation.
How do you stop lactation?
There are many reasons why you might need to stop producing milk, and you can stop lactating either naturally or with the help of hormonal drugs.
Natural milk suppression
Lactation is a supply-and-demand process. Your milk supply gradually goes down as your baby relies less on breast milk, or as you reduce the number of times you nurse or pump. Generally, if you decrease the volume of milk removed from your breasts, your body will slow milk production.
Suppressing your milk can feel uncomfortable and most people will become engorged (the term for overfilled breasts). You may also leak milk or develop a clogged milk duct. However, you can treat that pain by taking an over-the-counter pain reliever, wearing a firm bra or using an ice pack on your breasts.
Medication suppression
Medications can also be an option if you need to stop producing milk. Your healthcare provider can explain more about lactation-suppressing drugs, as well as the benefits and possible side effects.
Anatomy
Where are the mammary glands located?
Mammary glands are commonly called breasts and both genders have them. They are located on your chest and are composed of connective tissue, fat and special glandular tissue that makes milk. A woman’s glandular tissue is slightly different because it contains the alveoli and lobules necessary for producing milk. Women also have much more glandular tissue.
Conditions and Disorders
What are common conditions that affect your ability to lactate?
The ability to lactate and the length of time you’re able to produce milk varies. Some can produce milk for years, while others have trouble producing enough milk for their baby.
Some common factors that can impact lactation or breastfeeding are:
- Hormonal levels and conditions.

- Medications.
- Undergoing radiation therapy in the past.
- Trauma to your breast or nipples.
- Breast augmentation, reconstruction or other breast surgeries.
- Other medical conditions like HIV infection.
- Use of drugs and alcohol.
If you’re nursing or pumping your milk to bottle-feed your baby, you should always consult with your healthcare provider before starting any new medications or treatments. Many medications can pass to your baby through breast milk, which may have dangerous effects on your baby.
What is lactational amenorrhea?
Lactation amenorrhea (ah-men-oh-re-uh) means you aren’t menstruating (getting a period) due to lactation. When you’re lactating, your body produces prolactin, the hormone that produces milk. Prolactin reduces the amount of luteinizing hormone (LH) in your body, which helps trigger the release of an egg during ovulation. If you aren’t producing enough LH, you can’t ovulate or get your period. The length of time you can be amenorrheic due to lactation varies from a few months or until you’re completely done lactating.
The length of time you can be amenorrheic due to lactation varies from a few months or until you’re completely done lactating.
Does lactation reduce my risk of any diseases?
Studies have shown that breastfeeding reduces a woman’s risk of ovarian and breast cancers. It can also lower your risk for Type 2 diabetes and high blood pressure.
Care
How do you maintain milk production?
Maintaining lactation is mostly based on supply and demand. The more your baby breastfeeds or the more milk you express with a breast pump, the more your body will make. There are ways to suppress lactation with hormones or oral contraceptives. If you wish to maintain lactation, some things you should do are:
- Continue nursing on-demand or pump milk frequently (approximately every four hours).
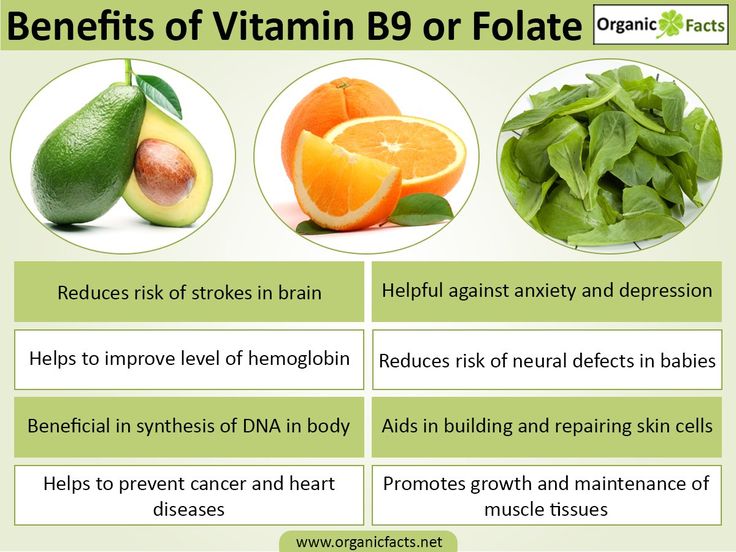
- Eat a healthy diet with enough calories. Low-calorie diets can decrease milk supply.
- Drink plenty of water to stay hydrated. Human milk is primarily water.
- Avoid smoking, drugs or alcohol.
 These can reduce your supply and transfer to your milk.
These can reduce your supply and transfer to your milk.
Frequently Asked Questions
What is the difference between lactation and colostrum?
Lactation describes the process of making and secreting milk from your breast. Colostrum is the first milk your breasts create during lactation and the first milk your baby drinks. It’s thick, yellow and commonly called “liquid gold.” Colostrum is high in protein, minerals, vitamins and antibodies.
What is hormone therapy for inducing lactation?
Couples or families who wish to induce lactation, maybe because of adoption, surrogacy or other reasons, can try hormone therapy. Induced lactation means you’re creating a milk supply without being pregnant. It’s a process that involves taking estrogen and progesterone for several months to make your body believe it’s pregnant. This helps prepare your breasts for lactation. Some medications and herbs are believed to help establish a milk supply, too.
Several weeks before your baby arrives, begin pumping your breasts with a breast pump. This encourages your body to release prolactin, which produces milk. Ideally, you express your milk several times a day, just like you would if you had a baby. This helps establish a supply. You can also freeze any milk you produce for use once your baby arrives.
This encourages your body to release prolactin, which produces milk. Ideally, you express your milk several times a day, just like you would if you had a baby. This helps establish a supply. You can also freeze any milk you produce for use once your baby arrives.
If you’re considering this as an option, you should talk to your healthcare provider about your desire to feed your baby with human milk. Induced lactation works for many people, but not all.
A note from Cleveland Clinic
If you want to feed your baby human milk, it’s helpful to understand the process of lactation so you know what to expect. Talk to your healthcare provider about how to best prepare for nursing or expressing milk. Remember, lactation can look different for everyone depending on your circumstances and health history. If you struggle with lactation at any point, you may feel embarrassed or even ashamed. But struggling with lactation is very common, and lactation specialists and other healthcare providers can help you as you try to overcome these difficulties.
How to Increase Breast Milk: Home Remedies, Diet, Supplements
Medically reviewed by Valinda Riggins Nwadike, MD, MPH — By Adrienne Santos-Longhurst on May 7, 2018
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Can you increase breast milk production?
If you’re worried that you’re not producing enough breast milk for your baby, you’re not alone.
Data from the Centers for Disease Control and Prevention shows that approximately 75 percent of new mothers start off breastfeeding their babies, but many stop either partially or completely within the first few months. One of the most common reasons for this is worry about insufficient milk production.
For many women, your milk supply is just fine. However, if you do need to increase your breast milk production, there are ways to do it.
Read on to learn how to increase your breast milk production using several evidence-based methods and some practices mothers have sworn by for centuries.
How to increase breast milk production
The following are things that you can do to increase breast milk production. How long it’ll take to boost your milk supply depends on how low your supply is to begin with and what’s contributing to your low breast milk production. Most of these methods, if they’re going to work for you, should begin working within a few days.
Most of these methods, if they’re going to work for you, should begin working within a few days.
1. Breastfeed more often
Breastfeed often and let your baby decide when to stop feeding.
When your baby suckles your breast, hormones that trigger your breasts to produce milk are released. That’s the “let-down” reflex. The let-down reflex is when muscles in your breasts contract and move the milk through the ducts, which happens shortly after your baby begins breastfeeding. The more you breastfeed, the more milk your breasts make.
Breastfeeding your new baby 8 to 12 times a day can help establish and maintain milk production. But this doesn’t mean that more or fewer feedings indicates a problem.
2. Pump between feedings
Pumping between feedings can also help you increase milk production. Warming your breasts before pumping can help make you more comfortable and pump easier, too.
Try pumping whenever:
- You have milk left over after a feeding.
- Your baby has missed a feeding.
- Your baby gets a bottle of breast milk or formula
3. Breastfeed from both sides
Have your baby feed from both breasts at each feeding. Let your baby feed from the first breast until they slow down or stop feeding before offering the second breast. The stimulation of having both breasts breastfed from can help increase milk production. Pumping milk from both breasts simultaneously has also been found to increase milk production and result in a higher fat content in the milk.
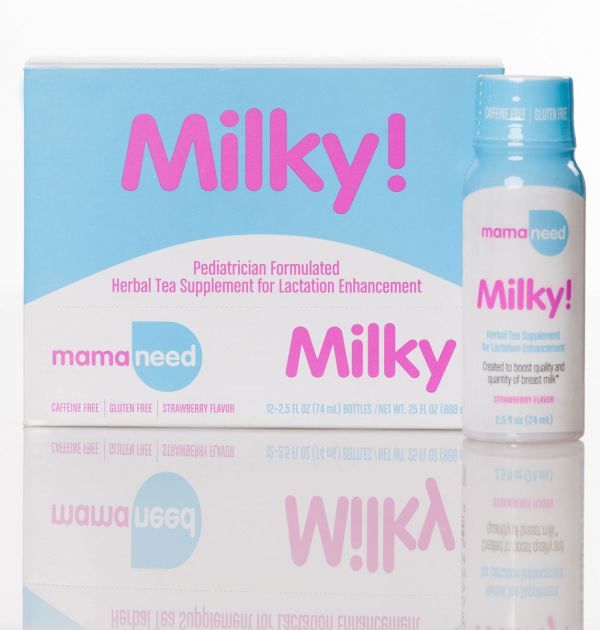
4. Lactation cookies
You can find lactation cookies in stores and online on Amazon or you can make your own. While there’s no research available on lactation cookies specifically, some of the ingredients have been linked to an increase in breast milk. These foods and herbs contain galactagogues, which may promote lactation. More research is needed, though.
Some of these include:
- whole oats
- wheat germ
- brewer’s yeast
- flaxseed meal
Easy lactation cookie recipe
Ingredients
- 2 cups white flour
- 2 cups oats
- 1 tbsp.
 wheat germ
wheat germ - 1/4 cup brewers’ yeast
- 2 tbsp. flaxseed meal
- 1 cup butter, softened
- 3 egg yolks
- 1/2 cup white sugar
- 1/2 cup brown sugar
- 1/4 cup water
- 1 1/2 teaspoons pure vanilla extract
- 1 tsp. baking soda
- 1/2 tsp. salt
Directions
- Preheat oven to 350°F (175°C).
- Mix the flaxseed meal with water in small bowl and let soak for at least 5 minutes.
- Cream the butter and white and brown sugar in a large mixing bowl. Add egg yolks and vanilla extract. Beat on low for 30 seconds or until ingredients are combined. Stir in flaxseed meal and water.
- In a separate bowl, mix flour, baking soda, brewer’s yeast, wheat germ, and salt. Add to butter mixture, and stir just until combined. Fold in the oats.
- Roll dough into 2-inch balls and place 2 inches apart onto a baking sheet.
- Bake for 10 to 12 minutes or until edges start to golden. Let the cookies stand on the baking sheet for 1 minute.
 Cool on a wire rack.
Cool on a wire rack.
You also can add dried fruit, chocolate chips, or nuts for some variety.
5. Other foods, herbs, and supplements
There are other foods and herbs that may increase breast milk production, according to the Canadian Breastfeeding Foundation. Some, such as fenugreek, have been found to take effect in as little as seven days. These foods and herbs include:
- garlic
- ginger
- fenugreek
- fennel
- brewer’s yeast
- blessed thistle
- alfalfa
- spirulina
Always talk to your doctor before taking a new supplement, especially when breastfeeding. Even natural remedies can cause side effects.
Potential causes for low milk supply
There are several factors that can interfere with the let-down reflex and cause low milk supply, including:
Emotional factors
Anxiety, stress, and even embarrassment can interfere with the let-down reflex and cause you to produce less milk. Creating a private and relaxing environment for breastfeeding and making the experience enjoyable and free of stress can help increase breast milk production. Try one of these 10 ways to relieve stress.
Creating a private and relaxing environment for breastfeeding and making the experience enjoyable and free of stress can help increase breast milk production. Try one of these 10 ways to relieve stress.
Medical conditions
Some medical conditions may interfere with milk production. These conditions include:
- pregnancy-induced high blood pressure
- diabetes
- polycystic ovarian syndrome (PCOS)
Certain medications
Medications that contain pseudoephedrine, such as sinus and allergy medications, and certain types of hormonal birth control may lower breast milk production.
Smoking and alcohol
Smoking and drinking moderate to heavy amounts of alcohol can lower your milk production.
Previous breast surgery
Not having enough glandular tissue because of breast surgery, such as breast reduction, cyst removal, or mastectomy, can interfere with lactation. Breast surgery and nipple piercings can damage the nerves that are connected to breast milk production.
Is your supply low?
You may be worried that your milk supply is low, but low breast milk production is rare. Most women make more than one-third more milk than their babies need, according to the Mayo Clinic.
There are many reasons your baby may cry, fuss, or seem distracted while breastfeeding, but it’s unlikely to be due to your milk supply. Teething, gas pains, or even just being tired can lead to fussiness. Babies are also more easily distracted as they age. This can interfere with feedings and cause them to pull away when you’re trying to breastfeed.
Every baby’s needs are different. Most newborns need 8 to 12 feedings in 24 hours, some even more. As your baby gets older, they’ll feed more efficiently. This means that even though feedings are much shorter, they may be getting more milk in less time. Other babies like to linger and suck longer, often until the flow of milk has almost stopped. Either way is fine. Take your cue from your baby and feed until they stop.
As long as your baby is gaining weight as expected and needing regular diaper changes, then you’re probably producing enough milk.
When your baby is getting enough milk, they will:
- gain weight as expected, which is 5.5 to 8.5 ounces each week until 4 months
- have three or four stools every day by 4 days of age
- have two wet diapers over 24 hours by the 2nd day after birth, and six or more wet diapers after day 5
Regular checkups with your child’s pediatrician will help determine if your milk supply may be low or if your child is undernourished. Tracking feedings and diaper changes can also help your doctor determine whether or not your milk supply is lower than it should be.
If your milk supply is low, supplementing with formula may be an option. Speak to your doctor or a lactation specialist before supplementing feedings with formula to avoid accidental early weaning.
A lactation specialist can create a supplementation plan for you to follow so that you can increase your milk production and gradually decrease supplementation.
When to seek help
If you’re worried that your baby isn’t getting enough milk or feel that your baby isn’t thriving, speak to your doctor or consult a lactation specialist. If low milk production is the problem, correcting it may be as simple as making a few changes to your routine or feeding technique, or adjusting a medication you’re on.
If you’re supply is low or you’re having other trouble with breastfeeding, try to remember the motto “Fed is best.” As long as your baby is well-fed and getting the nourishment they need, breast milk or formula are both fine.
Last medically reviewed on May 7, 2018
- Parenthood
- Postpartum Care
- Post Delivery
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Amount of milk. (n.d.).
llli.org/breastfeeding-info/amount/ - Breastfeeding report card –– United States, 2010. (2010).
cdc.gov/breastfeeding/pdf/breastfeedingreportcard2010.pdf - Increasing supply. (2018).
breastfeeding.asn.au/bf-info/common-concerns–mum/supply - Kent JC, et al. (2012). Principles for maintaining or increasing breast milk production. DOI:
- LaFleur E. (2015). What causes a low milk supply during breast-feeding?
mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/expert-answers/low-milk-supply/faq-20058148 - Lee HC, et al. (2012). A quality improvement project to increase breast milk use in very low birth weight infants. DOI:
10.1542/peds.2012-0547 - Newman J, et al. (2009). Herbs for increasing milk supply.
canadianbreastfeedingfoundation.org/induced/herbs.shtml - Pitman T. (n.d.). Losing your milk: What seems like dwindling milk can actually be normal changes in baby and you.

breastfeedingusa.org/content/article/losing-your-milk-what-seems-dwindling-milk-can-actually-be-normal-changes-baby-and-y - Prime DK, et al. (2012). Simultaneous breast expression in breastfeeding women is more effective than sequential breast expression. DOI:
10.1089/bfm.2011.0139 - Your guide to breastfeeding. (n.d.).
womenshealth.gov/files/documents/your-guide-to-breastfeeding.pdf
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
May 7, 2018
Written By
Adrienne Santos-Longhurst
Edited By
Frank Crooks
Medically Reviewed By
Valinda Riggins Nwadike, MD, MPH
Share this article
Pumping when mom needs to go away | Philips Avent
Search Support iconKeywords for searching
Home ›› Milk Expression of Mom from the Baby
Home Milk During Temporary Out of Mom from the Baby
↑ Verkh.
9000
Even if you don't have the opportunity to be near your baby, you can be sure that by pumping, he will receive all the necessary nutrients from breast milk. Perhaps you are already using a breast pump to continue breastfeeding when you go to work, or you just want to have more free time between feedings. nine0003
3 Philips Avent products to help you pump and store your milk comfortably:
Not sure when to start pumping or when to use a pump? Don't worry, we've put together a quick guide to help you learn how to express milk and learn about the benefits of using a breast pump. We'll also give you tips on how to express your milk when you're away from home, how to keep it adequate, and how to store it safely. nine0003
When should I start expressing milk?
Most women begin to express milk after six months, but there are circumstances that force them to do so sooner.
If you intend to express milk as early as possible, the answer to the question “When can I start expressing milk?” will be: "A few hours after birth. " Some mothers find that expressing milk is effective at a very early stage, especially if the baby has latch-on problems, as pumping improves the flow of milk to the breast. nine0015
" Some mothers find that expressing milk is effective at a very early stage, especially if the baby has latch-on problems, as pumping improves the flow of milk to the breast. nine0015
Other mothers start pumping after breastfeeding is established because they want someone in the household to help with feeds while they are away or with feeds after they go to work.
There are no specific rules about when to start pumping, so you can do whatever works best for you. Whatever your needs, you can pump to make your schedule less dependent on feedings.
How to express breast milk: general questions
How long should I express milk? How much milk do I need to express? What equipment do I need for this? Every mother has questions about this topic, however, once she starts expressing milk, she easily adapts to this process.
Most moms find a breast pump to be the easiest way to express breast milk. The principle of operation of different breast pumps may vary slightly, so read the instructions for use before using the device. Remember that it can take 1-2 minutes for milk to come out of your breast during pumping, so don't worry if you don't see it right away! nine0003
Remember that it can take 1-2 minutes for milk to come out of your breast during pumping, so don't worry if you don't see it right away! nine0003
Not sure how long to express milk? If you are not in a hurry, try to express milk until you feel that your chest is empty. Due to the individual characteristics of each woman, the pumping time will be different.
The amount of milk expressed will depend on when you last breastfed and how long you have been using the pump and are accustomed to using it. Even your internal state and time of day can affect the amount of milk. If you have problems with lactation, check out our tips for increasing your milk supply. Generally, the best time to express is in the morning. During sleep, there is an increase in the level of hormones responsible for the production of milk. nine0003
Should breastfeeding be combined with pumping? Wait about an hour between pumping and the next feeding. So you will be sure that the baby will have enough milk! Feed your baby as much as it takes to keep him full and happy. Use a breast pump to fully express milk from your breasts and save excess milk.
Use a breast pump to fully express milk from your breasts and save excess milk.
How to Express Breast Milk: Practical Tips
Whether you are expressing milk at home (for a night feed) or at work, there are a few key points to keep in mind to help you. nine0003
1. Plan ahead. If you have to leave your baby, start using a breast pump a few weeks in advance. This way you will store enough milk for your baby and get used to using a breast pump.
2. Be ready. You may be aware of the so-called "oxytocin reflex", which stimulates the flow of milk due to the release of the hormone oxytocin. Oxytocin increases the secretion of breast milk that can be expressed. The production of the hormone can be caused in many ways, even just by looking at the child. Therefore, many mothers find it effective to look at a photo of their baby while pumping while away from home. After you finish pumping, you can also use bra pads to keep your breasts dry and protect your clothes from milk stains. nine0015
nine0015
3. Get comfortable. The more comfortable you feel, the easier it will be to express milk. Find a quiet, private place and feel free to change the lighting and music to your liking. It is helpful to find a seat with good support so that you can sit comfortably with the pump in front of you.
4. Express as many times as you would like to breastfeed your baby. To maintain the required supply of milk, express it as often as you normally feed your baby.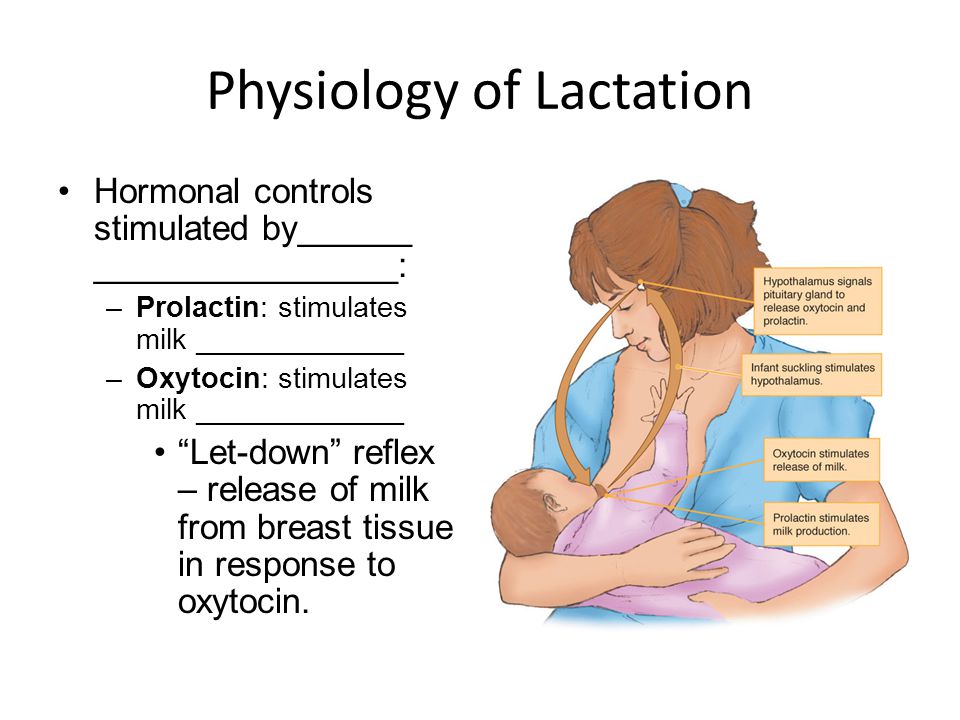 Thus, if the baby usually has three feedings during your absence, then you need to express milk at least three times. nine0003
Thus, if the baby usually has three feedings during your absence, then you need to express milk at least three times. nine0003
How to choose the best breast pump for expressing milk
There are several different types of breast pumps, each with its own advantages. Choose the one that will help you feel comfortable in your daily life. Perhaps you prefer to have a device that is designed to be used on the go? Or do you need a breast pump that will allow you to express milk quickly?
Storage and preparation of milk after pumping
After you have expressed your milk, remember to freeze or refrigerate it. Then, before feeding the baby, it must be thawed and warmed up. Here are some tips on how to store breast milk:
- Use sterile milk storage containers or freezer bags to collect and store milk.
- Do not fill the container to the upper limit, because. when frozen, breast milk "expands", the optimal portion for storage is 60-120 ml.
 nine0088
nine0088 - Label the container with the pumping date or write the pumping date on the container with a permanent marker.
- Store milk in the refrigerator at 2-4°C for up to 24 hours.
- After cooling the expressed milk in the refrigerator for 0.5 hours, the milk can be frozen in the freezer and stored there for 3 months.
- Place the milk closer to the back of the refrigerator or freezer than in the door to keep the milk at a constant temperature. nine0088
- Thawed milk placed in the refrigerator should be used within 24 hours.
- Do not refreeze defrosted milk.
- Transport milk in an insulated container with an ice pack.
Use these tips to prepare your expressed milk for nursing:
- Thaw or warm breast milk under running warm water, in a bain-marie, or with a bottle warmer. nine0088
- Do not use a microwave oven to heat milk.
- Do not heat milk to boiling point.
- Shake the milk bottle before feeding until smooth.
- Check milk temperature before feeding. The most optimal temperature is the average between body temperature and room temperature. To check the temperature of milk, you can drop it on your skin.
Advice for first-time moms
If you are just starting to express milk, remember that this process may not be entirely comfortable. The more relaxed you are, the easier it will be to express milk. Sometimes this will be difficult to do, for example if you are trying to express milk during a busy work day or in an unfamiliar place; therefore, it is necessary to practice well at home and show patience. You will soon learn how to express breast milk. In the next article, you will learn how to store breast milk! nine0003
Philips Avent articles & tips
Baby+ app
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.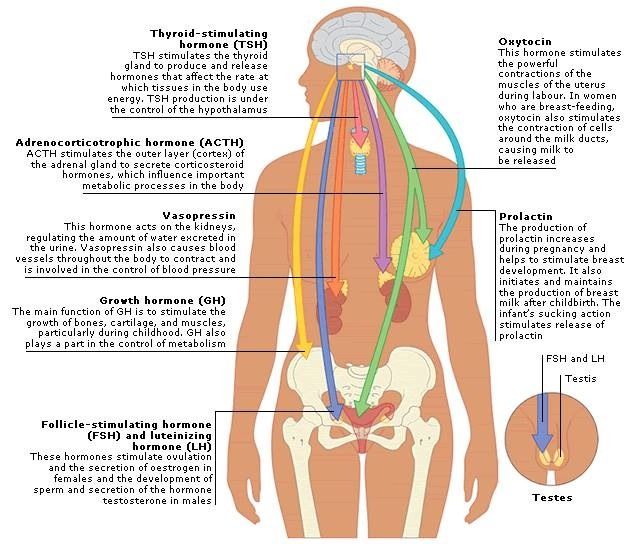 nine0003
nine0003
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
How much should a newborn baby eat
search support iconSearch Keywords
Home ›› How much milk should a newborn baby drink?
Home ›› How much milk should a newborn baby drink?
↑ Top
Like every new mom, you're probably wondering, "How often should a newborn eat?" and “How many milliliters does a newborn baby drink at a time?”.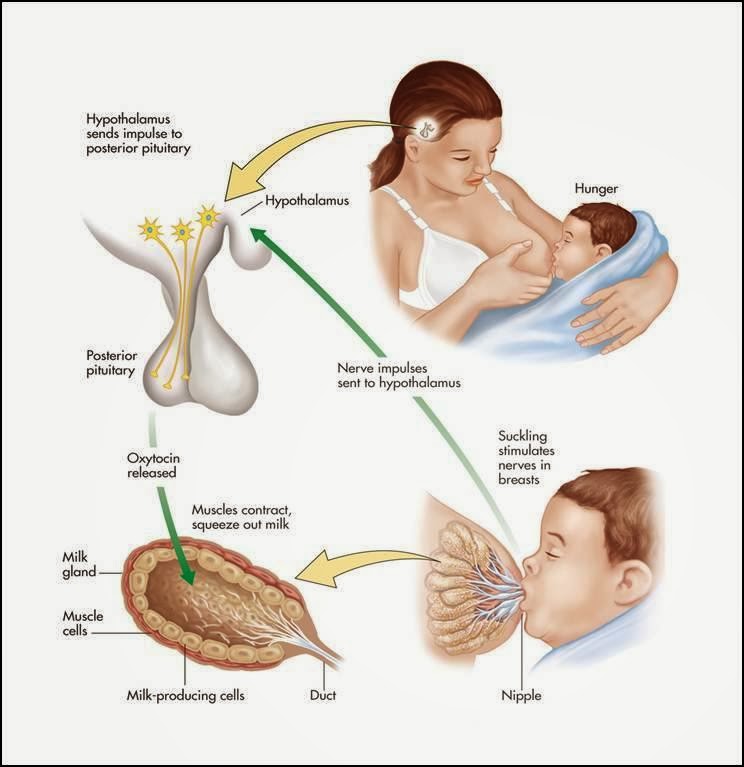 A mother's body is designed to provide her baby with all the nutrients she needs, but every mom needs practical advice and confidence when it comes to how much milk a newborn should drink. nine0003
A mother's body is designed to provide her baby with all the nutrients she needs, but every mom needs practical advice and confidence when it comes to how much milk a newborn should drink. nine0003
Whether you are breastfeeding, bottle feeding or a combination, here you will find all the information you need to know about how much food your baby needs to grow and develop properly.
Signs indicating that the child is hungry
Every mother has a wonderful maternal instinct, but we cannot guess the child's desires the first time. Over time, you will learn your child's unique gestures and body movements, as well as signs that he is hungry. In the meantime, here are some of the most common signs that a child is hungry:
- turns head towards your breast or bottle;
- clenches;
- puts pens in mouth;
- pouts, smacks or licks lips.
If your child is showing any of these signs, they may be trying to tell you it's time to eat. Ideally, your baby should be fed on demand when he is hungry. If you're breastfeeding, on-demand feeding is a good way to keep your milk supply going as your body will naturally respond to your baby's needs and continue to produce the required amount of milk. Bottle-feeding on demand can also be beneficial for your baby, as it allows him to self-regulate his feeding needs. nine0003
Ideally, your baby should be fed on demand when he is hungry. If you're breastfeeding, on-demand feeding is a good way to keep your milk supply going as your body will naturally respond to your baby's needs and continue to produce the required amount of milk. Bottle-feeding on demand can also be beneficial for your baby, as it allows him to self-regulate his feeding needs. nine0003
How much breast milk should a newborn drink?
So, how much should a newborn baby eat? A remarkable feature of each child is its uniqueness, so it would be wrong to feed the baby strictly according to the instructions. Don't panic if the recommendations below don't fit your own feeding schedule, but please contact your healthcare provider or pediatrician if you have any questions.
Although every baby is different, newborns typically eat every two to three hours, for a total of 8 to 12 meals a day. nine0003
How many milliliters does a newborn baby drink? At the very beginning, your body will only produce a small amount of yellowish and thick breast milk called colostrum.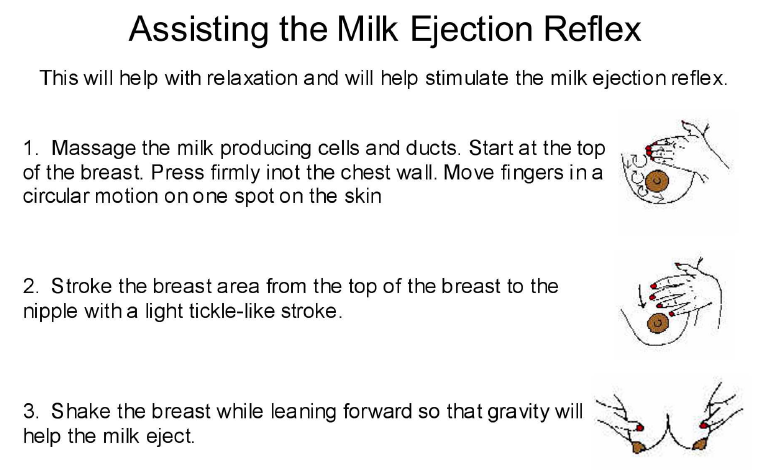 This milk is an ideal source of nutrients that your newborn needs, in addition, it has many immunological components. 1
This milk is an ideal source of nutrients that your newborn needs, in addition, it has many immunological components. 1
How much milk does a newborn baby drink? Infants drink 30-60 ml per feeding, while this volume increases to 60-90 ml by two weeks of age. So don't worry if you don't feel like your body is producing much milk in those first few days after your baby is born! Feeding times will also vary, ranging from 10 to 30 minutes at the very beginning and then gradually increasing as your baby grows.
How much bottle-feeding breast milk does your baby take
If you choose to bottle-feed your baby from time to time, do so at the same intervals and for the same period of time as if you were breastfeeding. Pumping is a great option for breastfeeding your baby. It will allow you to separate from the baby if necessary and at the same time retain all the benefits of breastfeeding. nine0015
It's also important to get a bottle that helps make bottle feeding more natural for both you and your baby.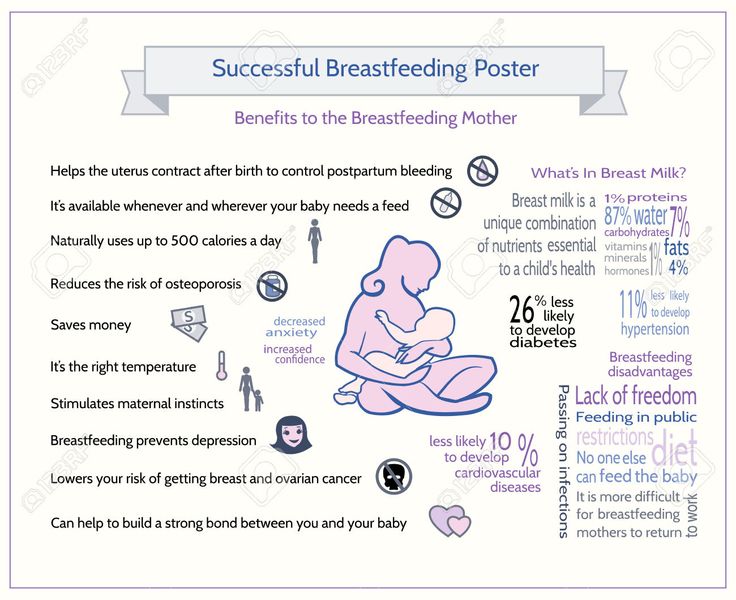
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/674814/chart_01_large.0.png)