Diabetes in newborn symptoms
Neonatal Diabetes
Nationwide Children’s Hospital
Overview
Signs & Symptoms
Causes
Diagnosis
Treatment
Seeking Help
What Is Neonatal Diabetes?
Neonatal diabetes mellitus is a rare form of diabetes that occurs within the first 6 months of life. Our bodies need insulin to help our cells make energy. Infants with this condition do not produce enough insulin, which increases blood glucose levels.
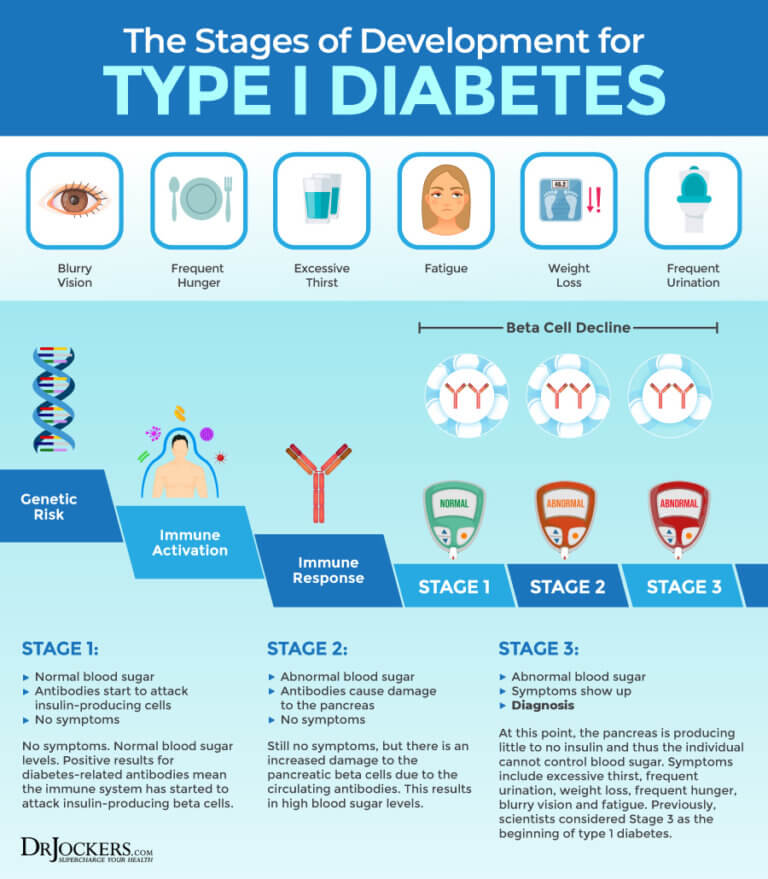
Neonatal diabetes is often mistaken as type 1 diabetes, which is much more common. But type 1 diabetes usually occurs in children older than 6 months.
- Half of babies diagnosed with neonatal diabetes have a lifelong condition.
This is called permanent neonatal diabetes mellitus. It occurs in 1 in 260,000 babies in some areas of the world.
- For the other half, the condition disappears within the first twelve weeks of life: but it can reoccur later. This is called transient neonatal diabetes mellitus.
Fetuses with neonatal diabetes do not grow as well in the womb, and these newborns may be small for their gestational age. This is called intrauterine growth restriction.
What Are the Symptoms of Neonatal Diabetes?
When blood glucose levels become high, some glucose leaves the body through urine. This causes many of the initial symptoms, which may include:
- Increased numbers of wet diapers
- Increased appetite
- Dehydration
What Causes Neonatal Diabetes?
Neonatal diabetes is a “monogenetic” disease. This means it is caused by mutations in a single gene.
In most cases, the gene mutation is inherited.
How Is Neonatal Diabetes Diagnosed?
Neonatal diabetes is diagnosed when your doctor finds elevated levels of glucose in the infant’s blood or urine.
Neonatal diabetes can sometimes be confused with type 1 diabetes. Since neonatal diabetes is caused by a genetic mutation, genetic testing can help properly diagnose it.
How Is Neonatal Diabetes Treated?
Neonatal diabetes is often treated with insulin. In some cases, once specific genetic mutations are known, oral medications may be used for treatment.
Can Neonatal Diabetes Be Prevented or Cured?
Neonatal diabetes is caused by a genetic mutation. There’s currently no way to prevent or cure it, but it can be managed.
In approximately half of infants diagnosed with neonatal diabetes, the condition disappears in infancy but can reoccur later in life.
When to Seek Help for Your Child?
If you suspect your infant has neonatal diabetes, talk to his or her health care provider as soon as possible.
You Might Also Be Interested In
Article
Resources for Parents and Schools
Access logs, management plans, diabetes care tips and more.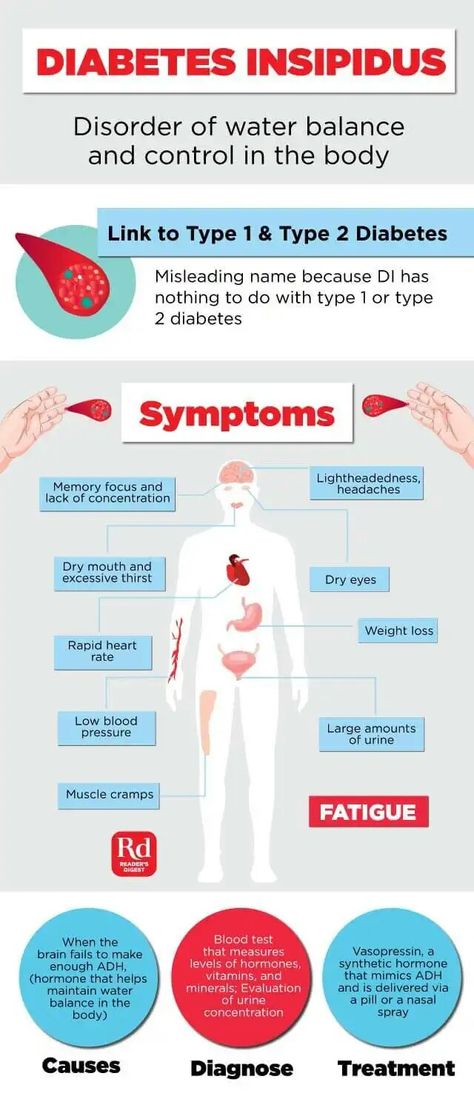
Blog
Why Does My Child Have Stinky Pee?
Most people know what “normal” pee smells like, but what happens if your child goes pee and it doesn’t smell normal to you? This is not as uncommon as you may think. Below are the most common reasons for abnormal urine odors.
Blog
Benefits of Massage Therapy for Children
Your young ones are more active than ever, in mind and in body. Teaching them to manage stress and body awareness while they are young can help prevent a lifetime of chronic pain and poor habits.
Neonatal Diabetes - Types, Symptoms, Treatment and Complications
Neonatal diabetes is a rare form of diabetes that is usually diagnosed in children under 6 months of age.
This early occurring type of diabetes is caused by one of a number of genetic mutations and is therefore described as a monogenic form of diabetes.
Neonatal diabetes is treatable and may or may not require insulin so a diagnosis by genetic testing is recommended.
Types of neonatal diabetes
There are two main types of neonatal diabetes:
- Transient Neonatal Diabetes Mellitus
- Permanent Neonatal Diabetes Mellitus
Transient neonatal diabetes is so called because it usually disappears within a year of birth but can come back again typically during adolescence
Permanent neonatal diabetes, once diagnosed, stays for the rest of life.
How common is neonatal diabetes?
Neonatal diabetes is very rare, occurring in around 1 in 300,000 to 1 in 400,000 births
Out of the two types of neonatal diabetes, the transient type is slightly more common affecting 50-60% of cases of neonatal diabetes.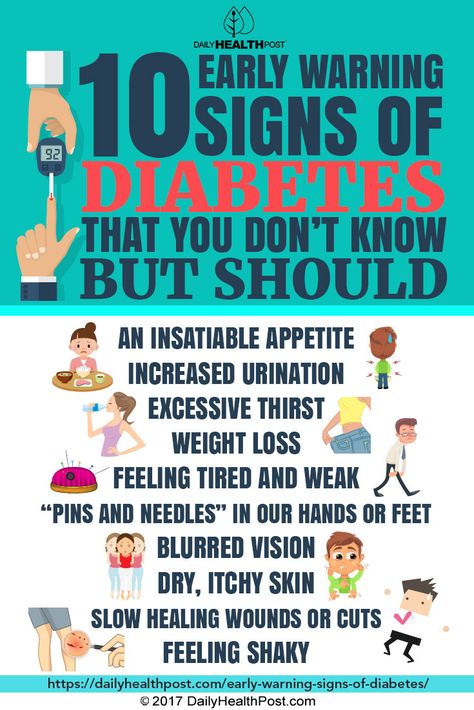 [105]
[105]
Symptoms and diagnosis
The symptoms of neonatal diabetes include persistent thirst, frequent urination and dehydration. [103]
Presence of diabetes mellitus can be diagnosed with a blood glucose test. A diagnosis of diabetes before 6 months should suggest neonatal diabetes, as opposed to type 1 diabetes
In some cases, neonatal diabetes may be diagnosed after 6 months however.
Genetic testing is advised for children diagnosed with diabetes under the age of 9 months to asses which form of diabetes is present and to guide the best form of treatment. [104]
Treatment
Neonatal diabetes will usually either be treated with a drug called glibenclamide or with insulin.
Around 50% of people with neonatal diabetes can be treated with glibenclamide, a drug which causes the pancreas to release more insulin. Glibenclamide is in a class of diabetes drugs called sulfonylureas If glibenclamide is not effective enough, insulin will need to be taken.
If neonatal diabetes is transient, it won’t require treatment during the years in which it is resolved. However, the condition should be monitored for reappearance of diabetes in adolescence and later years.
Complications
A number of health complications can occur in people with neonatal diabetes, depending on which gene is affected. The following complications are relatively common in children with neonatal diabetes:
- Developmental delay such as muscle weakness and learning disabilities
- Diabetic ketoacidosis
- Low birth weight
- Muscle weakness
- Epilepsy
- Macroglossia – a larger than normal tongue
Treatment with glibenclamide has been shown to help reduce the effects of developmental delay.
Prevention
Neonatal diabetes is genetic disorder for which, unfortunately, there is no known prevention.
Childhood diabetes | Prevention | GBUZ "City Polyclinic No. 6 of Novorossiysk" MH KK
Diabetes in children: causes, symptoms and signs, diagnosis, treatment.
) in the blood. Diabetes mellitus ranks first among all endocrine diseases in children. Diabetes mellitus in children is relatively acute and without appropriate treatment, as a rule, acquires a severe, progressive course. This development of diabetes in children is due to the intensive growth of the child's body and, accordingly, increased metabolism
Diagnosis of diabetes in children is based on identifying the symptoms of the disease and determining the concentration of glucose and insulin in the blood. Treatment of diabetes mellitus in children includes diet, dosed exercise, treatment with insulin preparations.
Forms of diabetes in children. There are two main types of diabetes mellitus:
- Insulin-dependent diabetes (type 1 diabetes).
- Non-insulin dependent diabetes (type 2 diabetes).
While type 2 diabetes mellitus predominates among adults, type 1 diabetes mellitus (insulin-dependent) predominates among children.
Type 1 diabetes mellitus is characterized by very low levels of insulin in the blood, as a result of which the diabetic child is dependent on insulin treatment.
Features of the development of diabetes in children
A child's pancreas (an organ that produces the hormone insulin) is very small. By the age of 10, the mass of the child's pancreas doubles, reaching a size of 12 cm and a weight of just over 50 g. The production of insulin by the pancreas is one of its most important functions, which is finally formed by the fifth year of a child's life. It is from this age and up to about 11 years that children are especially susceptible to diabetes. All metabolic processes in a child's body proceed much faster than in an adult. Carbohydrate metabolism (assimilation of sugars) is no exception. Accordingly, a child needs to consume 10 g of carbohydrates per 1 kg of weight per day. Therefore, all children are very fond of sweets - this is a natural need of their body.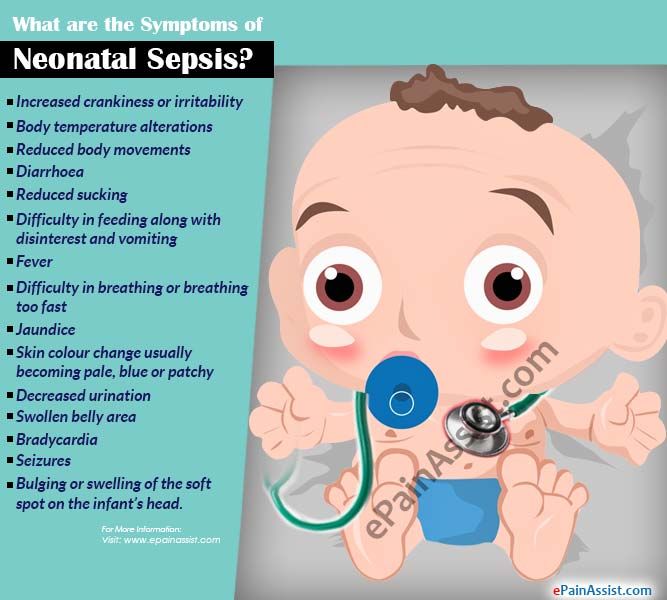 The metabolism of carbohydrates is also affected by the nervous system of the child, which is not yet fully formed, therefore it can malfunction and also affect blood sugar levels. Contrary to popular belief, even the consumption of significant amounts of sweets in childhood does not lead to the development of diabetes.
The metabolism of carbohydrates is also affected by the nervous system of the child, which is not yet fully formed, therefore it can malfunction and also affect blood sugar levels. Contrary to popular belief, even the consumption of significant amounts of sweets in childhood does not lead to the development of diabetes.
In general, the risk of developing diabetes is higher in premature, underdeveloped children, or adolescents during puberty. Also, the risk of developing diabetes is higher in children subject to significant physical exertion (for example, in pupils of sports schools).
The main cause of diabetes in children is a viral infection that destroys insulin-producing cells in the pancreas. Among childhood infections, many can cause the development of diabetes (mumps, rubella, measles, etc.). In this regard, one of the most important measures to prevent the development of diabetes in children is the timely vaccination of the child.
The course of diabetes mellitus in children also depends on the age of the child at which the disease began.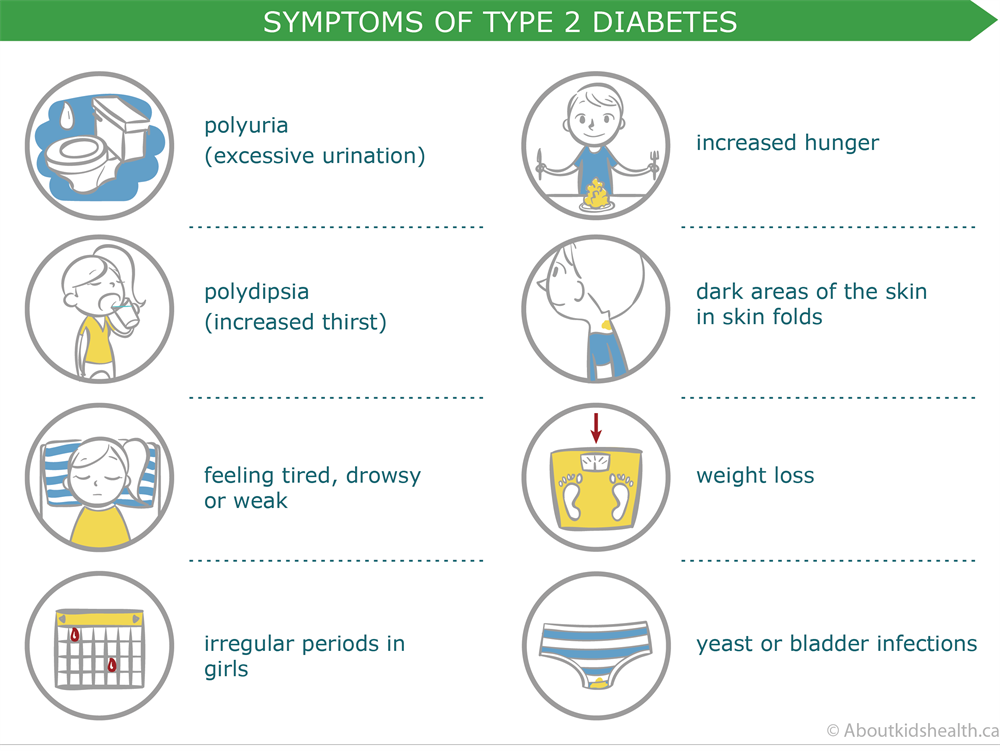 The younger the child with diabetes, the more severe it is and the greater the risk of various complications. As a rule, once having arisen, diabetes in a child never goes away. A child with diabetes will need supportive care throughout his life.
The younger the child with diabetes, the more severe it is and the greater the risk of various complications. As a rule, once having arisen, diabetes in a child never goes away. A child with diabetes will need supportive care throughout his life.
Risk factors for diabetes in children
There are a number of risk factors that contribute to the development of diabetes in children. The presence of one or more risk factors greatly increases a child's chances of developing diabetes. Risk factors for diabetes in children:
- children born to diabetic mothers
- both parents of the child have diabetes mellitus
- frequent acute viral diseases
- birth weight exceeded 4.5 kg
- other metabolic disorders (hypothyroidism, obesity)
- immunosuppression
Symptoms of diabetes in children are almost the same as in adults:
- thirst
- weight loss
- excessive urine output (more than 2-3 liters per day)
- severe infections
- fatigue, inability to concentrate
Parents do not always notice these symptoms, which makes it difficult to detect diabetes in children.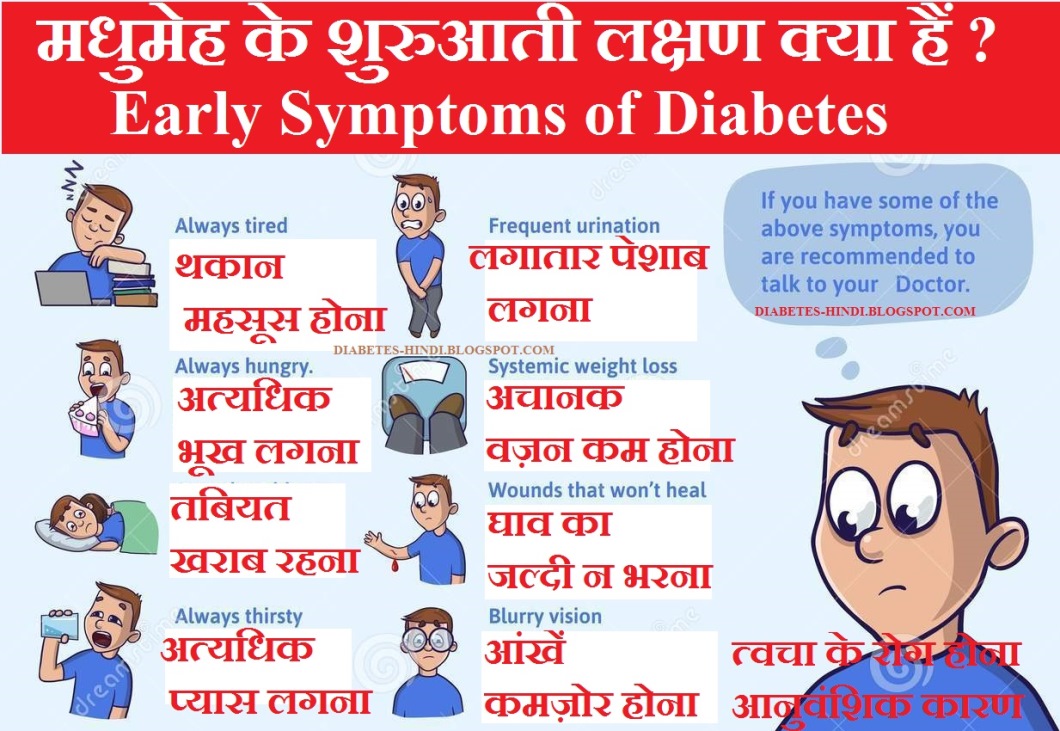 Despite the difficulty in identifying the symptoms of diabetes in a child, there are characteristic signs of diabetes in children that make it easier to identify the disease. So, for example, an important symptom of diabetes is bedwetting. Children with diabetes produce 2-4 times more urine than healthy children. Also, in children with diabetes, skin lesions (furunculosis), itching of the skin, etc. often occur. In infants, diabetes mellitus is accompanied by indigestion (diarrhea, constipation, vomiting), anxiety. A diabetic child suckles a lot and greedily at the breast or drinks water. From sweet urine, linen and diapers become hard, crispy. These symptoms are often observed in moderate or severe diabetes mellitus. In mild diabetes mellitus, sick children may have little to no complaints or signs of illness, and the diagnosis is based on blood and urine sugar levels.
Despite the difficulty in identifying the symptoms of diabetes in a child, there are characteristic signs of diabetes in children that make it easier to identify the disease. So, for example, an important symptom of diabetes is bedwetting. Children with diabetes produce 2-4 times more urine than healthy children. Also, in children with diabetes, skin lesions (furunculosis), itching of the skin, etc. often occur. In infants, diabetes mellitus is accompanied by indigestion (diarrhea, constipation, vomiting), anxiety. A diabetic child suckles a lot and greedily at the breast or drinks water. From sweet urine, linen and diapers become hard, crispy. These symptoms are often observed in moderate or severe diabetes mellitus. In mild diabetes mellitus, sick children may have little to no complaints or signs of illness, and the diagnosis is based on blood and urine sugar levels.
Treatment of diabetes in children.
Treatment of diabetes in a child includes: exercise, diet, medication.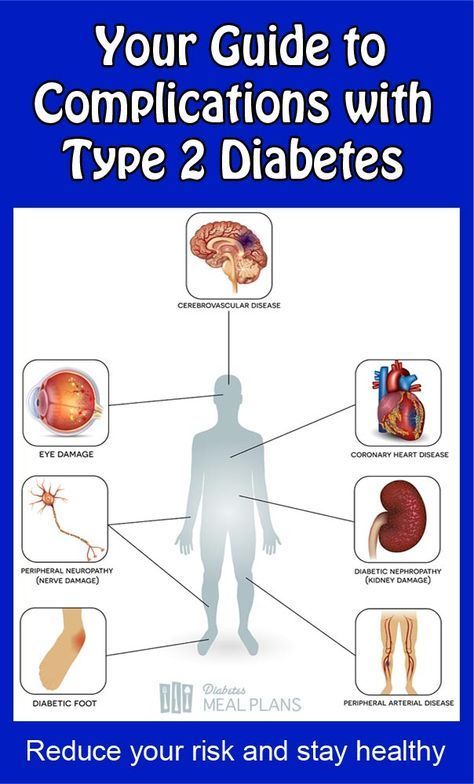
Exercise for children with diabetes
Exercise increases the sensitivity of body tissues to insulin and lowers blood sugar levels. In this regard, dosed physical activity is an important part of the treatment of children with diabetes. It should be emphasized that only dosed physical activity is useful in diabetes, while uncontrolled physical activity in patients with diabetes mellitus contributes to the development of hypoglycemic conditions.
Proper exercise management in diabetic children necessarily includes the use of additional carbohydrates before, during and after exercise in accordance with the recommendations given by your doctor, as well as periodic monitoring of blood glucose levels.
It is important to measure blood glucose before, during and after exercise in order to correctly dose insulin with a short or intermediate duration of action.
Nutrition of a sick child plays an important role in the treatment of diabetes mellitus. The nutrition of a child with diabetes should meet all the requirements that are currently imposed on the nutrition of a healthy child: the diet should be as balanced as possible in all the most important ingredients (proteins, fats, carbohydrates and vitamins).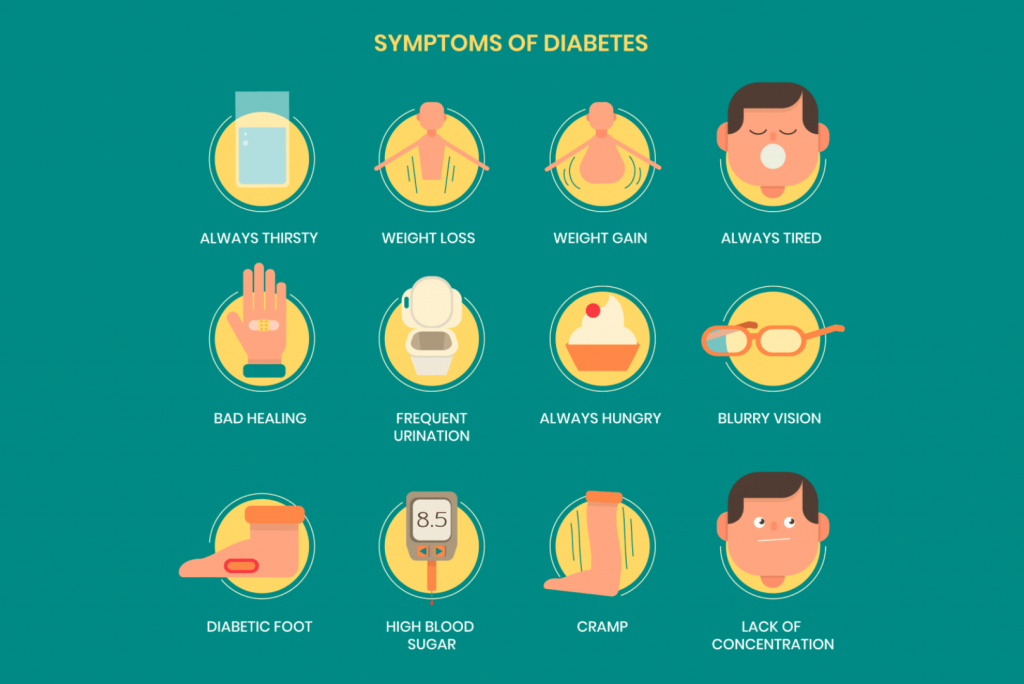 Compliance with this condition allows children with diabetes to grow and develop normally. At the same time, a special diet eliminates the carbohydrate load and thus facilitates the course and treatment of diabetes.
Compliance with this condition allows children with diabetes to grow and develop normally. At the same time, a special diet eliminates the carbohydrate load and thus facilitates the course and treatment of diabetes.
In diabetes mellitus, they limit the use of such foods and dishes as bakery products made from wheat flour, potatoes, cereals (semolina, rice). Porridge is given to the child no more than once a day, using coarse grinding cereals (buckwheat, oatmeal, corn) for their preparation.
Rice, semolina and pasta should be used in limited quantities. The consumption of bread should not exceed 100g per day. Vegetables (everything except potatoes) can be offered to the child without restrictions. Moreover, dishes from various vegetables should make up a significant part of the daily diet of children.
Fruits and berries – unsweetened varieties of apples, black currants, cherries, etc. – are also widely included in the diet for diabetes. Occasionally, you can give your child citrus fruits (oranges, tangerines), strawberries, wild strawberries, raspberries. A child can eat fruits raw and in the form of compotes prepared with sugar substitutes.
A child can eat fruits raw and in the form of compotes prepared with sugar substitutes.
Fatty, spicy and salty sauces, sweet sauces are excluded from the menu. If the child does not have liver diseases associated with diabetes, it is allowed to add a small amount of onion to food as a seasoning.
It is necessary to feed a child with diabetes 6 times a day and more often. The greatest satisfaction for the child, as a rule, brings his usual food. In view of this, when compiling a diet, the features of the family nutrition stereotype should be taken into account: the hours and volume of each meal, the child's eating habits. The composition of the child's diet should be agreed with the doctor observing the child.
Drug treatment of diabetes in children.
Almost all children with diabetes receive insulin. Thanks to the introduction of long-acting insulin preparations into medical practice, as a rule, one injection of insulin per day is sufficient.
The choice of insulin preparation, its dosage and administration schedule are also determined by the attending physician. Tablets for diabetes (Maninil, Glipizide, etc.) are quite effective in treating diabetes in adults, but very rarely give good results in children. They are used in mild forms of the disease or prescribed as an adjuvant to reduce the number of injections or the dose of insulin.
Children and adolescents who are regularly treated, adhere to the diet exactly, develop well physically and mentally.
Properly selected and organized therapy with insulin preparations and constant monitoring of the child's condition greatly alleviate the course of the disease and allow children with diabetes to lead a full life.
Material taken from the site: Cherepovets City Maternity Hospital
Diabetes mellitus in children and adolescents
Category: Useful information.
Type 1 diabetes mellitus (insulin-dependent) predominates among children.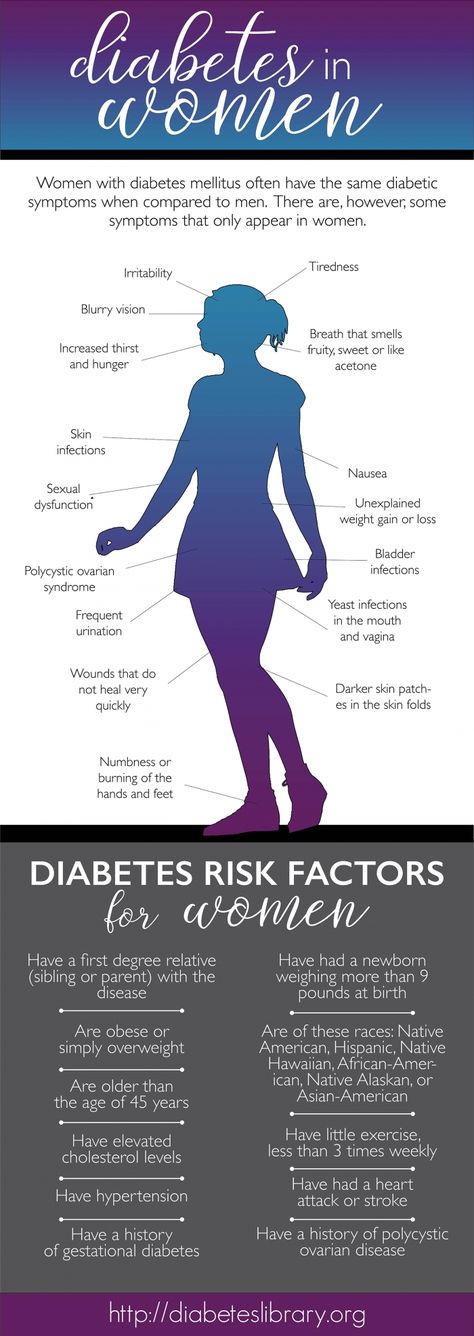 Although in recent years, type 2 diabetes occurs in obese children older than 8 years. A child can get sick at any age, often diabetes develops in children under 5 years of age.
Although in recent years, type 2 diabetes occurs in obese children older than 8 years. A child can get sick at any age, often diabetes develops in children under 5 years of age.
What contributes to the development of diabetes in children?
- genetic predisposition.
- Early refusal of breastfeeding, improper introduction of complementary foods,
- Overweight.
- Infectious diseases transferred in early childhood.
- Stress.
The symptoms of diabetes mellitus in children are almost the same as in adults: severe thirst, bedwetting appears, the child loses weight, fatigue, poor performance at school, skin infections (boils, barley) often recur, and vaginal candidiasis in girls.
Diabetes in children of the first year of life is rare, but it still happens sometimes. An infant cannot complain. If the baby is in a diaper, then parents are unlikely to notice that he has begun to excrete much more urine. Diabetes can be suspected if the child is not gaining or losing weight; greedily drinks water; frequent diaper rash; after the urine dries, the diapers become as if starched; if urine gets on the floor, then sticky spots remain there. Acute symptoms of diabetes in children: vomiting, intoxication, severe dehydration.
Diabetes can be suspected if the child is not gaining or losing weight; greedily drinks water; frequent diaper rash; after the urine dries, the diapers become as if starched; if urine gets on the floor, then sticky spots remain there. Acute symptoms of diabetes in children: vomiting, intoxication, severe dehydration.
The diagnosis is usually quickly confirmed by detecting an increase in blood glucose (greater than 11.1 mmol/L). If ketone bodies are detected in the blood or urine, urgent therapy is indicated. Waiting the next day to confirm hyperglycemia can be life-threatening. Children with diabetes need lifelong hormone replacement therapy. Diabetes never goes away. A child with diabetes will need maintenance treatment with insulin for the rest of his life.
Prevention of diabetes.
- Control of blood glucose levels, if among close relatives there are patients with diabetes mellitus.
- Breastfeeding up to 12 months, timely introduction of complementary foods.