Define fetal monitoring
Fetal Heart Monitoring | Johns Hopkins Medicine
What is fetal heart monitoring?
Fetal heart rate monitoring measures the heart rate and rhythm of your baby (fetus). This lets your healthcare provider see how your baby is doing.
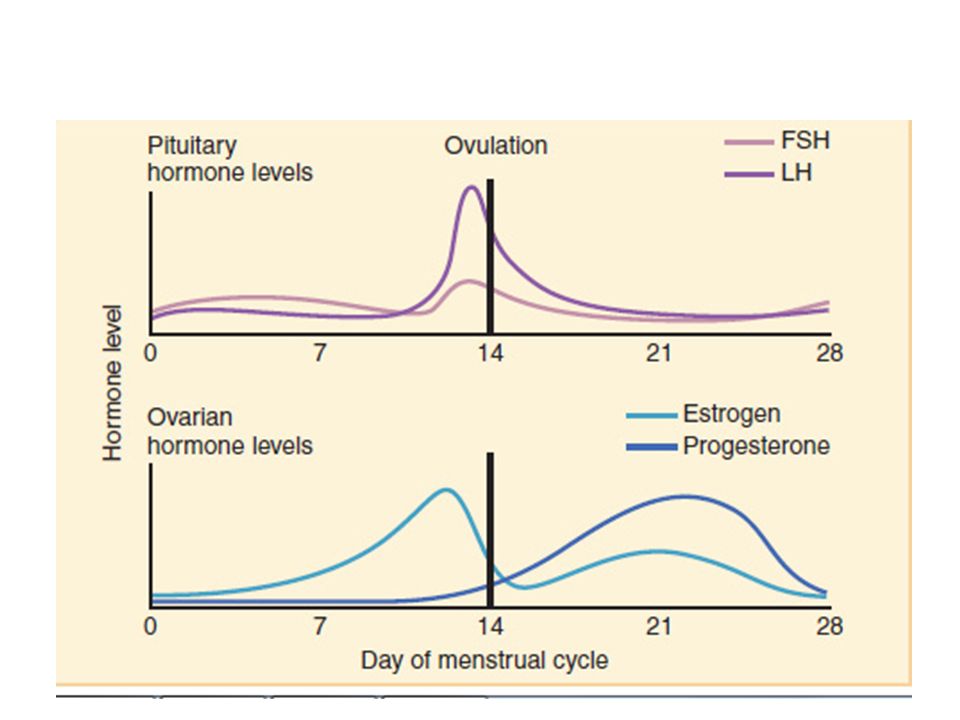
Your healthcare provider may do fetal heart monitoring during late pregnancy and labor. The average fetal heart rate is between 110 and 160 beats per minute. It can vary by 5 to 25 beats per minute. The fetal heart rate may change as your baby responds to conditions in your uterus. An abnormal fetal heart rate may mean that your baby is not getting enough oxygen or that there are other problems.
There are 2 ways to do fetal heart monitoring, external and internal:
External fetal heart monitoring
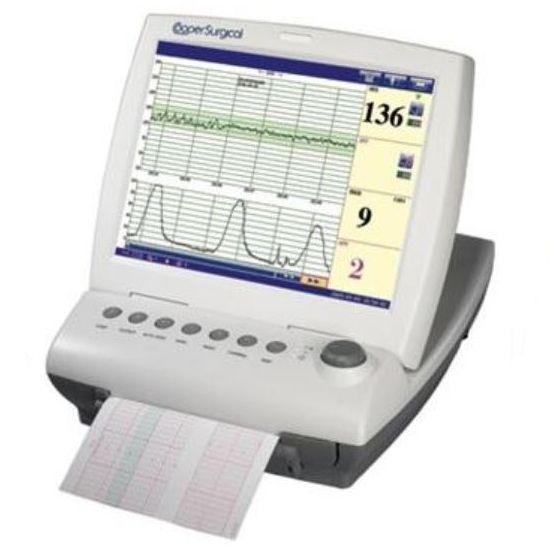
This method uses a device to listen to and record your baby’s heartbeat through your belly (abdomen). One type of monitor is a Doppler ultrasound device. It’s often used during prenatal visits to count the baby’s heart rate. It may also be used to check the fetal heart rate during labor. The healthcare provider may also check your baby’s heart rate continuously during labor and birth. To do this, the ultrasound probe (transducer) is fastened to your belly. It sends the sounds of your baby’s heart to a computer. The rate and pattern of your baby’s heart rate are shown on a screen and printed on paper.
Internal fetal heart monitoring
This method uses a thin wire (electrode) put on your baby’s scalp. The wire runs from the baby through your cervix. It is connected to the monitor. This method gives better readings because things like movement don’t affect it. But it can only be done if the fluid-filled sac that surrounds the baby during pregnancy (amniotic sac) has broken and the cervix is opened. Your provider may use internal monitoring when external monitoring is not giving a good reading. Or your provider may use this method to watch your baby more closely during labor.
During labor, your healthcare provider will watch your uterine contractions and your baby’s heart rate. Your provider will note how often you are having contractions and how long each lasts. Because the fetal heart rate and contractions are recorded at the same time, these results can be looked at together and compared.
Your provider will note how often you are having contractions and how long each lasts. Because the fetal heart rate and contractions are recorded at the same time, these results can be looked at together and compared.
Your provider may check the pressure inside your uterus while doing internal fetal heart monitoring. To do this, he or she will put a thin tube (catheter) through your cervix and into your uterus. The catheter will send uterine pressure readings to a monitor.
Why might I need fetal heart monitoring?
Fetal heart rate monitoring is especially helpful if you have a high-risk pregnancy. Your pregnancy is high risk if you have diabetes or high blood pressure. It is also high risk if your baby is not developing or growing as it should.
Fetal heart rate monitoring may be used to check how preterm labor medicines are affecting your baby. These are medicines are used to help keep labor from starting too early.
Fetal heart rate monitoring may be used in other tests, including:
- Nonstress test.
 This measures the fetal heart rate as your baby moves.
This measures the fetal heart rate as your baby moves. - Contraction stress test. This measures fetal heart rate along with uterine contractions. Contractions are started with medicine or other methods.
- A biophysical profile (BPP). This test combines a nonstress test with ultrasound.
Things that may affect the fetal heart rate during labor:
- Uterine contractions
- Pain medicines or anesthesia given to you during labor
- Tests done during labor
- Pushing during the second stage of labor
Your healthcare provider may have other reasons to use fetal heart rate monitoring.
What are the risks of fetal heart monitoring?
Radiation is not used for this test. The transducer usually causes no discomfort.
You may find the elastic belts that hold the transducers in place slightly uncomfortable. These can be readjusted as needed.
These can be readjusted as needed.
You must lie still during some types of fetal heart rate monitoring. You may need to stay in bed during labor.
With internal monitoring, you may have some slight discomfort when the electrode is put in your uterus.
Risks of internal monitoring include infection and bruising of your baby’s scalp or other body part.
Note: You should not have internal fetal heart rate monitoring if you are HIV positive. This is because you may pass the infection on to your baby.
You may have other risks depending on your specific health condition. Be sure to talk with your provider about any concerns you have before the procedure.
Certain things may make the results of fetal heart rate monitoring less accurate. These include:
- Obesity of the mother
- Position of the baby or mother
- Too much amniotic fluid (polyhydramnios)
- Cervix is not dilated or the amniotic sac is not broken.
 Both of these need to happen to do internal monitoring
Both of these need to happen to do internal monitoring
How do I get ready for fetal heart monitoring?
- Your healthcare provider will explain the procedure to you. Ask him or her any questions you have about the procedure.
- You may be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if anything is not clear.
- The consent form for fetal heart monitoring may be included as part of the general consent for labor and birth.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, or anesthesia.
- If fetal heart rate monitoring is done along with another monitoring test, you may be asked to eat a meal before the test. This can help make your baby more active.
- The amniotic sac must be broken and your cervix must be dilated several centimeters before the internal device can be put in place.
- Follow any other instructions your provider gives you to get ready.
What happens during fetal heart monitoring?
You may have fetal heart rate monitoring in your healthcare provider's office or as part of a hospital stay. The way the test is done may vary depending on your condition and your healthcare provider's practices.
Generally, fetal heart rate monitoring follows this process:
External fetal heart monitoring
- Depending on the type of procedure, you may be asked to undress from the waist down. Or you may need to remove all of your clothes and wear a hospital gown.
- You will lie on your back on an exam table.
- The healthcare provider will put a clear gel on your abdomen.
- The provider will press the transducer against your skin. The provider will move it around until he or she finds the fetal heartbeat. You will be able to hear the sound of the fetal heart rate with Doppler or an electronic monitor.

- During labor, the provider may check the fetal heart rate at intervals or nonstop, based on your condition and the condition of your baby.
- For continuous electronic monitoring, the provider will connect the transducer to the monitor with a cable. A wide elastic belt will be put around you to hold the transducer in place.
- The provider will record the fetal heart rate. With continuous monitoring, the fetal heart pattern will be displayed on a computer screen and printed on paper.
- You may not be able to get out of bed with nonstop external fetal heart rate monitoring.
- Once the procedure is done, the provider will wipe off the gel.
Internal fetal heart monitoring
- You will be asked to remove your clothes and put on a hospital gown.
- You will lie on a labor bed. Your feet and legs will be supported as for a pelvic exam.

- Your healthcare provider will do a vaginal exam with a gloved hand to see how far you are dilated. This may be slightly uncomfortable.
- If the amniotic sac is still intact, your healthcare provider may break open the membranes with a tool. You will feel warm fluid coming out of your vagina.
- Your healthcare provider will feel the part of the baby at the cervical opening with gloved fingers. This is usually the baby’s head.
- The provider will put a thin tube (catheter) into your vagina. He or she will put a small wire at the end of the catheter on the baby’s scalp. He or she will gently turn it on the baby’s skin.
- The provider will remove the catheter and leave the wire in place on the baby’s scalp.
- The provider will connect the wire to a monitor cable. He or she will keep it in place with a band around your thigh.
- You may not be able to get out of bed with nonstop internal fetal heart rate monitoring.
- Once the baby is born, the provider will remove the wire.
What happens after fetal heart rate monitoring?
You do not need any special care after external fetal heart monitoring. You may go back to your normal diet and activity unless your healthcare provider tells you otherwise.
After internal fetal heart rate monitoring, your healthcare provider will check your baby’s scalp for infection, bruising, or a cut. The provider will clean the site with an antiseptic.
Your healthcare provider may give you other instructions, based on your situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure
Electronic Fetal Heart Rate Monitoring Test: Procedure & Results
Written by Lisa Fields
In this Article
- What Is Fetal Heart Rate Monitoring?
- Reasons for Fetal Heart Rate Monitoring
- Types of Fetal Heart Rate Monitoring
- Fetal Heart Rate Monitoring Risks
- Fetal Heart Rate Monitoring Procedure
- Fetal Heart Rate Monitoring Results
- Abnormal Fetal Heart Rate Treatments
What Is Fetal Heart Rate Monitoring?
Fetal heart rate monitoring is a process that lets your doctor see how fast your baby’s heart is beating. If you’re pregnant, your doctor will want to make sure your baby is healthy and growing as they should. One of the ways they do that is to check the rate and rhythm of your baby’s heartbeat.
If you’re pregnant, your doctor will want to make sure your baby is healthy and growing as they should. One of the ways they do that is to check the rate and rhythm of your baby’s heartbeat.
The doctor is most likely to do this later in your pregnancy and when you’re in labor. They may combine it with other tests for a closer look if you have diabetes, high blood pressure, or any condition that could cause problems for you and your baby.
Reasons for Fetal Heart Rate Monitoring
The doctor is more likely to use fetal heart rate monitoring when your pregnancy is high-risk. You may need fetal heart rate monitoring when:
- You have diabetes.
- You have high blood pressure.
- You’re taking medicine for preterm labor.
- Your baby isn’t growing or developing normally.
The doctor might also use fetal heart rate monitoring to make sure your baby is OK when you’re in labor or if there are other reasons to check your baby’s heart rate.
Types of Fetal Heart Rate Monitoring
The doctor can monitor your baby’s heartbeat in a couple of ways. They can listen for or electronically record the beats from outside your belly. Or once your water has broken and you’re in labor, they can thread a thin wire through your cervix and attach it to your baby’s head.
External monitoring (auscultation): If your pregnancy is going normally, the doctor likely will check your baby’s heart rate from time to time with a special stethoscope or a hand-held device called a Doppler ultrasound. Doctors sometimes call this type of fetal heart rate monitoring auscultation.
If you need it, the doctor might do a special test called a nonstress test, usually starting around week 32 of your pregnancy. It counts the number of times your baby’s heart speeds up during a 20-minute period.
For the test, you'll lie down with an electronic sensor belt around your belly that continuously records the baby's heartbeat.
The doctor also may wrap an electronic sensor belt around you to measure the baby’s heart rate during labor and delivery. This lets them know if the contractions are stressing your baby. If so, you might have to have your baby as soon as possible.
This lets them know if the contractions are stressing your baby. If so, you might have to have your baby as soon as possible.
Internal monitoring: Once your water breaks and your cervix opens to prepare for birth, the doctor can run a wire called an electrode through it and into your womb. The wire attaches to your baby’s head and connects to a monitor. This gives a better reading than listening to your baby’s heartbeat from the outside.
Fetal Heart Rate Monitoring Risks
External monitoring isn’t risky. It doesn’t hurt or use radiation. If your doctor uses a belt, it might be a little uncomfortable. It also might mean you have to stay in bed during labor.
Internal monitoring risks include:
- Slight discomfort
- Infection
- Bruising or scratching your baby’s scalp
If you’re HIV-positive, you shouldn’t have internal fetal heart rate monitoring. That’s because there’s a risk of passing the infection to your baby. If you have other health conditions, ask your doctor if there are any special risks.
Fetal Heart Rate Monitoring Procedure
Fetal heart rate monitoring could happen in your doctor’s office or at the hospital. The procedure will depend on what type of monitoring you’ll have.
External fetal heart rate monitoring procedure
- Your doctor will ask you to undress and lie down on an exam table or labor bed.
- You’ll get clear gel on your belly.
- Your doctor will press a gadget called Doppler transducer to your belly and move it around.
- You’ll hear the sound of your baby’s heartbeat.
- If your doctor wants to measure the heartbeat continuously, they’ll use a wide belt to hold the transducer in place.
- Your doctor will record the fetal heart rate. You may see it on a computer screen.
Internal fetal heart rate monitoring procedure
- You’ll be asked to undress and lie down.
- You’ll put your feet and legs in supports, like you’re getting a vaginal exam.

- The doctor will check to see if your cervix is dilated.
- If your water hasn’t broken, the doctor may break it.
- The doctor will feel for your baby’s head.
- The doctor will put a thin tube (catheter) with a small wire at the end into your vagina.
- The doctor will put the wire on your baby’s scalp and remove the catheter.
- Once it’s connected to a cable, the wire will record your baby’s heartbeat until a doctor removes it or your baby is born.
Fetal Heart Rate Monitoring Results
A healthy baby’s heart usually beats 110-160 times a minute in the womb. It speeds up when the baby moves. Signs of possible problems include:
- Heart beats slower than 110 beats a minute
- Heart beats faster than 160 beats a minute
- A heartbeat pattern that isn’t normal
- The heartbeat doesn’t go up when the baby moves or during contractions
Lack of a normal heartbeat doesn’t always mean something is wrong with your baby. But it can be a sign that the baby isn’t getting enough oxygen.
But it can be a sign that the baby isn’t getting enough oxygen.
Your results also may be less accurate if:
- You’re obese.
- You or your baby is in the wrong position.
- You have too much amniotic fluid.
Abnormal Fetal Heart Rate Treatments
If your baby’s heart rate isn't what it should be, the doctor may try:
- Changing your positions to move the baby
- Giving you fluids through an IV
- Having you breathe extra oxygen
- Relaxing your uterus with medicine to slow contractions
- Giving you other drugs
If these steps don’t return your baby’s heart rate to normal, you may need to deliver them right away. If your cervix is completely open, the doctor may use a tool called forceps or a special vacuum to help you push the baby out. Otherwise, you’ll have the baby by emergency cesarean section.
Fetal monitoring | Rumex
Fetal monitoring is an important process by which abnormalities in the development of the child can be detected. It is carried out on the basis of traditional and innovative methods. Periodic examinations are the guarantor of a successful pregnancy. If the expectant mother wants to give birth to a healthy baby, she must visit the clinic and follow the recommendations of doctors.
It is carried out on the basis of traditional and innovative methods. Periodic examinations are the guarantor of a successful pregnancy. If the expectant mother wants to give birth to a healthy baby, she must visit the clinic and follow the recommendations of doctors.
What methods of fetal monitoring are available? Let's consider this point in more detail.
Auscultation
This is a physical diagnostic method that has been used for many years. It means listening to the fetal heartbeat. A stethoscope is used for auscultation. The instrument is applied to the abdomen of a pregnant woman lying on a couch.
The heartbeat is determined from the 20th week. As the fetus grows, heart rhythms are heard more clearly. During the examination, the specialist finds the point of the best listening to tones. It determines the rhythm and nature of the contractions of the heart. If the tones are clear and clean, everything is fine. Deafness of tones indicates the presence of intrauterine hypoxia.
Auscultation is a simple and affordable method. This is the advantage due to which this method of listening to the fetal heart is used to this day. But it also has a significant drawback: the difficulty in localizing sounds.
Fetal phonocardiography
This is an outdated technique that assesses the general condition of the heart. It was popular in the last century. To record the phonocardiogram, special sensors were used that convert vibrations into signals. The study was characterized by absolute safety, but there was no need to talk about high accuracy. Today, fetal phonocardiography is not used, since it has been superseded by modern techniques. For example, fetal monitoring of the fetus.
Doppler
This is a type of ultrasound. With its help, the state of the child's cardiac activity is determined and the patency of the umbilical cord vessels is assessed. This method of diagnosis gives significant results. A qualified specialist determines the presence of hypoxia, detects the entanglement of the fetus with the umbilical cord and detects abnormalities in the work of the placenta.
No preparation is required for the study. Most ultrasound machines are equipped with a Doppler function. The procedure is absolutely painless. It takes place over 15 minutes. The study is prescribed for women who are in the third semester of pregnancy.
Doppler ultrasound is 70% accurate in detecting abnormalities. The absence of problems in a specific period of time does not exclude the development of complications in the later stages.
Amnioscopy
This is a visual method that examines the amniotic fluid. It is carried out in several cases: re-carrying of pregnancy, suspicion of intrauterine death of the child and prolonged labor, in which the fetal bladder did not burst.
Amnioscopy performed at gestational age greater than 36 weeks. During the study, the doctor evaluates the amount and color of amniotic fluid. The presence of foreign impurities is also determined. The results obtained are sent to the obstetrician-gynecologist.
Fetal monitoring with an amnioscope can detect serious abnormalities. Research requires advance preparation. Amnioscopy is carried out with the consent of a woman informed of possible complications. There is a 0.5% chance of miscarriage or preterm labor after the study.
Research requires advance preparation. Amnioscopy is carried out with the consent of a woman informed of possible complications. There is a 0.5% chance of miscarriage or preterm labor after the study.
Echocardiography
This is an ultrasound examination of the fetus that focuses on the heart. The study is scheduled between 18-28 weeks of pregnancy. Echocardiography is a complex technique in which one-dimensional ultrasound and Doppler mode are used. With its help, the structure of the heart and large vessels is determined.
Fetal echocardiography is performed as indicated. These include the presence of diabetes in a woman, age (over 38 years), intrauterine growth retardation of the child. Other criteria are also important: the transfer of infectious diseases, alcohol abuse, as well as the birth of children who have heart problems.
Echocardiography is a safe way to examine the heart. It does not cause discomfort. The doctor receives comprehensive information about the work of the heart. There are no significant drawbacks to this technique.
There are no significant drawbacks to this technique.
Ultrasound
This is a common method of diagnosis during pregnancy. Fetal monitoring is carried out using modern equipment. The number of scheduled ultrasound examinations does not exceed five times. For the first time, a woman comes to a medical facility to determine pregnancy. Subsequent ultrasounds are performed for different purposes:
- 11-13 weeks - assessment of fetal development and placental condition
- 19-21 weeks - the size of the fetus and the sex of the child are determined, the condition of the amniotic fluid is assessed
- 32-34 weeks - the weight of the child and the condition of the umbilical cord are determined. The commensurability of the size of the baby's head and the birth canal is also evaluated
- Ultrasound before childbirth - possible complications are identified
Transabdominal and transvaginal examinations are carried out in medical institutions. In the first case, the sensor is placed on the abdomen. In the second case, a special device is used, which is inserted inside.
In the first case, the sensor is placed on the abdomen. In the second case, a special device is used, which is inserted inside.
Ultrasound is a painless method of fetal monitoring. Its advantages include information content, a high level of security, and no need for preliminary preparation. Ultrasound examinations have been used for 40 years. During this time, no adverse effects on fetal development were identified. For this reason, the technique is successfully used in clinics. But development does not stand still. Traditional methods are being replaced by innovative solutions.
Electronic fetal monitoring
This is an advanced technique that detects serious complications: cerebral palsy, fetal death, cardiac abnormalities. Fetal monitoring is carried out as follows: a woman in labor, lying on her back, has belts with sensors placed on her stomach. One device records the fetal heartbeat, and the second - the duration and intensity of uterine contractions. The sensors are connected to the monitor.
In some cases (eg serious hazard to the fetus) an internal examination is used. Its essence is as follows: the electrode is inserted through the cervix and is located on the baby's head. With such an examination, the doctor receives the exact data necessary to assess the current situation. Internal monitoring is used after rupture of membranes. The cervix must also be dilated (at least 1 cm).
External electronic monitoring takes about half an hour. The clinics use innovative devices. For example, it can be Avalon fetal monitors. This is a technologically advanced equipment with the best characteristics. It is characterized by functionality, long service life, ease of use.
Fetal monitoring is an advanced technology used in state-of-the-art medical facilities. Therefore, it is necessary to consider in more detail its features and benefits.
Fetal monitoring of the fetus - an advanced solution
Cardiotocography is a technique that implies a comprehensive diagnosis of the state of the fetus and the body of a pregnant woman.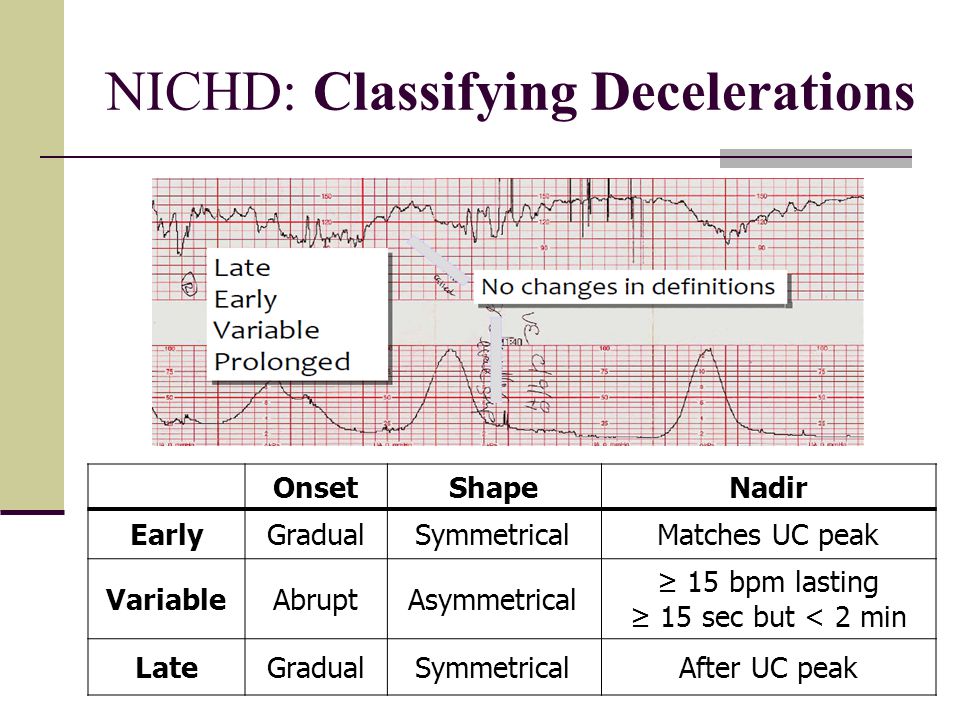 When conducting research, fetal monitors developed on the basis of advanced technologies are used. With their help, vital signs are determined, on which the normal development of the child depends.
When conducting research, fetal monitors developed on the basis of advanced technologies are used. With their help, vital signs are determined, on which the normal development of the child depends.
Cardiotocography has been used successfully for a long period. This is a technique, the key purpose of which is the early diagnosis of fetal disorders. Studies are conducted twice (in the third semester). In some cases, additional testing is recommended. These include:
- delayed pregnancy
- unexpected decrease in the child's motor activity
- suspected congenital malformations
- multiple pregnancy
- premature aging of the placenta
In difficult cases, fetal monitors are used just before delivery. Research helps the doctor decide on the tactics of future childbirth. Qualified specialists decide what to do next: to stimulate, to perform an emergency caesarean section, or to wait for the intensification of labor. During childbirth, cardiotocography provides complete information about how the child tolerates the load.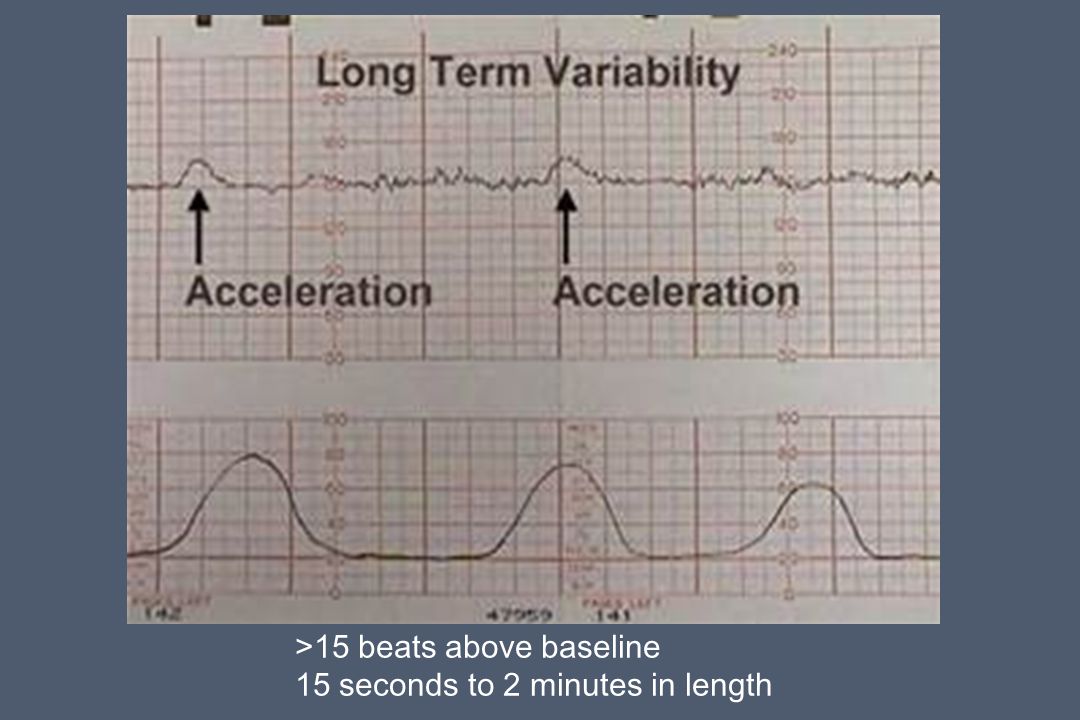 Therefore, fetal monitors perform an important function.
Therefore, fetal monitors perform an important function.
Cardiotocography is a unique technique that reduces perinatal morbidity and mortality by half. When conducting examinations, advanced devices are used to identify risks and possible complications. CTG is performed in the position that is most convenient for a pregnant woman. The results obtained are deciphered by experienced specialists. In the absence of deviations, the heart rate is 110-160 beats per minute. When the fetus moves, the indicators change - 130-190 hits.
When evaluating the results, a special system is used:
- 9-10 points - satisfactory condition
- 6-8 points - fetal hypoxia
- less than five points - severe oxygen starvation
Cardiotocography is a procedure that helps to assess the condition of the fetus and determine the tone of the uterus. When diagnosing, important information is analyzed: the number of heartbeats per minute, a change in rhythm over a certain period of time, an increase in the number of contractions when the baby moves in the womb.
Fetal monitoring is a test with numerous advantages:
- painless - sensors are placed on the abdomen. The woman does not feel discomfort
- no special training required
- safety - fetal monitoring does not cause complications
- information content - during the diagnosis, important parameters necessary for the successful management of pregnancy are determined. In the process of studying the heartbeat, the doctor assesses the condition of the fetus and, in the presence of deviations, correctly plans further actions
Fetal monitors are devices that meet strict quality standards. Brand manufacturers offer advanced devices that solve the tasks as accurately as possible. Fetal monitors from the Dutch company Philips deserve close attention.
Philips medical equipment is in demand in many countries. Avalon fetal monitors provide high-precision measurement of the required parameters. The devices are easy to use because they are equipped with color touch screens. The equipment is equipped with soft-touch sensors that are easy to use.
The equipment is equipped with soft-touch sensors that are easy to use.
Fetal monitors from a Dutch company are smart devices that collect all the important information. With their help, doctors measure the heart rate of the fetus and intrauterine pressure, and also determine the motor activity of the baby. Systems analyze parameters even for several fetuses. This is a significant advantage, thanks to which the devices are widely used in medical institutions.
Equipment from a leading brand ideal for use in outpatient, inpatient, pregnancy and childbirth settings. The devices are used for a long time and perfectly cope with their functions!
What is pregnancy monitoring and why is it needed?
Preparation for the birth of a healthy, full-fledged child is a long and responsible process. There are 9 whole months between conception and birth, during which the female body faces many dangers - infections and diseases that can harm not only the woman, but also her unborn child. Therefore, the duty of every expectant mother is to monitor during pregnancy not only her own lifestyle and health, but also the condition of the fetus. This will help monitoring pregnancy - a set of tests, during which the main biochemical markers of the state of the fetus and the female body are recorded.
Therefore, the duty of every expectant mother is to monitor during pregnancy not only her own lifestyle and health, but also the condition of the fetus. This will help monitoring pregnancy - a set of tests, during which the main biochemical markers of the state of the fetus and the female body are recorded.
First of all, a general blood test is prescribed for a woman. As a rule, if the pregnancy proceeds without complications, the analysis is repeated three times for 9 months. It is thanks to this simple procedure that the doctor can determine the presence of diseases in the body.
Another mandatory set of tests during pregnancy is isoserological. With the help of this study, specialists determine the blood type, as well as the Rh factor of the pregnant woman and the fetus, and assess the likelihood of a conflict that occurs if they are incompatible in the woman in labor and the fetus.
A blood test for "biochemistry" reflects the work of the main internal organs and metabolic processes. In a pregnancy that proceeds without pathology, a biochemical blood test is given in the first trimester. But if necessary, it can be re-appointed for a period of 30 weeks. In parallel, hemosyndrome is also determined - the body's tendency to bleed, caused by various blood clotting disorders.
In a pregnancy that proceeds without pathology, a biochemical blood test is given in the first trimester. But if necessary, it can be re-appointed for a period of 30 weeks. In parallel, hemosyndrome is also determined - the body's tendency to bleed, caused by various blood clotting disorders.
The presence of viral diseases in the body will help to identify the analysis for infection. If special treatment is not carried out, viruses can provoke miscarriage and death, both of the fetus and the woman. In addition, the occurrence of infections can be a direct indication for termination of pregnancy. For 9months, tests for infections are taken three times after the first appointment, as well as in the third trimester.
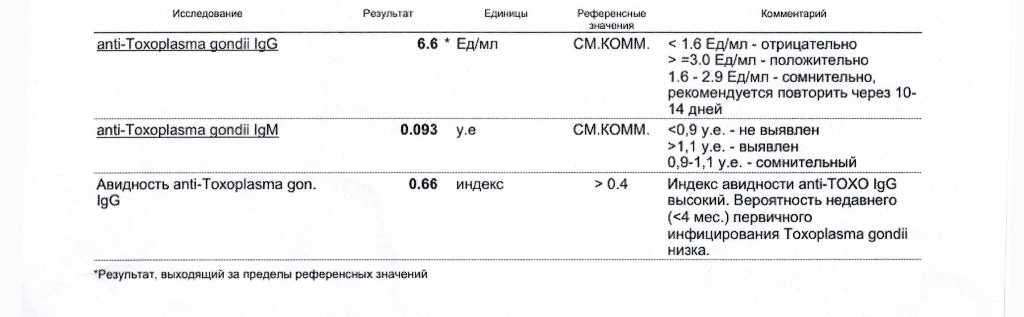
PCR method or polymerase chain reaction - an analysis that is today considered the most sensitive and accurate diagnostic method. It is effective even when other tests are powerless, because it allows you to identify the presence of the causative agent of the disease, even if only a few bacterial or viral DNA molecules are present in the sample. During pregnancy, the diagnosis of infections is of particular importance, since there is a risk of infection of the fetus. Tests for cytomegalovirus, toxoplasma, herpes virus, rubella virus, mycoplasma and chlamydia form the so-called TORCH complex. PCR is a mandatory diagnostic step for every woman who wants to give birth to a healthy baby.
During pregnancy, the diagnosis of infections is of particular importance, since there is a risk of infection of the fetus. Tests for cytomegalovirus, toxoplasma, herpes virus, rubella virus, mycoplasma and chlamydia form the so-called TORCH complex. PCR is a mandatory diagnostic step for every woman who wants to give birth to a healthy baby.
Urinalysis is also important, thanks to which the function of the kidneys and the presence of a whole range of diseases in the body are determined. Unlike other tests, this one is often given - once a month until 28 weeks, then - 2 times a month.
Diabetes mellitus, even if it is latent, can be detected with a blood sugar test. Blood "for sugar" is given after the first visit to the doctor. But, as in the case of biochemical analysis, the procedure can be repeated at the 30th week of pregnancy.
Ultrasound, one of the most important types of research, makes it possible to determine the uterine or ectopic pregnancy, as well as to determine whether the fetus has developmental defects. The attending physician prescribes an ultrasound at the first visit, after which the procedure is performed three times. From 12 to 14 weeks, then from 22 to 24, and finally between 32 and 34 weeks.
The attending physician prescribes an ultrasound at the first visit, after which the procedure is performed three times. From 12 to 14 weeks, then from 22 to 24, and finally between 32 and 34 weeks.
Bakposev - an analysis that allows you to obtain data on the state of the microflora of a future woman in labor, as well as determine whether opportunistic flora is present in the body, and whether there are inflammatory processes. The analysis is carried out twice - at the beginning of observation by a doctor and at 9month of pregnancy.
Finally, one of the most important tests is prenatal trisomy screening. This is a blood test, thanks to which it is possible to determine the likelihood of chromosomal abnormalities in the fetus. For example, even before birth, identify Down syndrome or Edwards syndrome. This analysis can be carried out even at the planning stage of pregnancy, and, as a result, the transmission of genetic diseases can be minimized. For women over 35, this procedure is mandatory.