Chickenpox treatment in pregnancy
Chickenpox during pregnancy | March of Dimes
Chickenpox is an infection caused by a virus. If you get it during pregnancy, it can cause problems for you and your baby.
You’re probably safe from chickenpox if you’ve had it before or if you’ve had the vaccine. Both of these help make you immune to chickenpox.
Talk to your health care provider to make sure you’re immune to chickenpox before you get pregnant or early in pregnancy.
What is chickenpox?
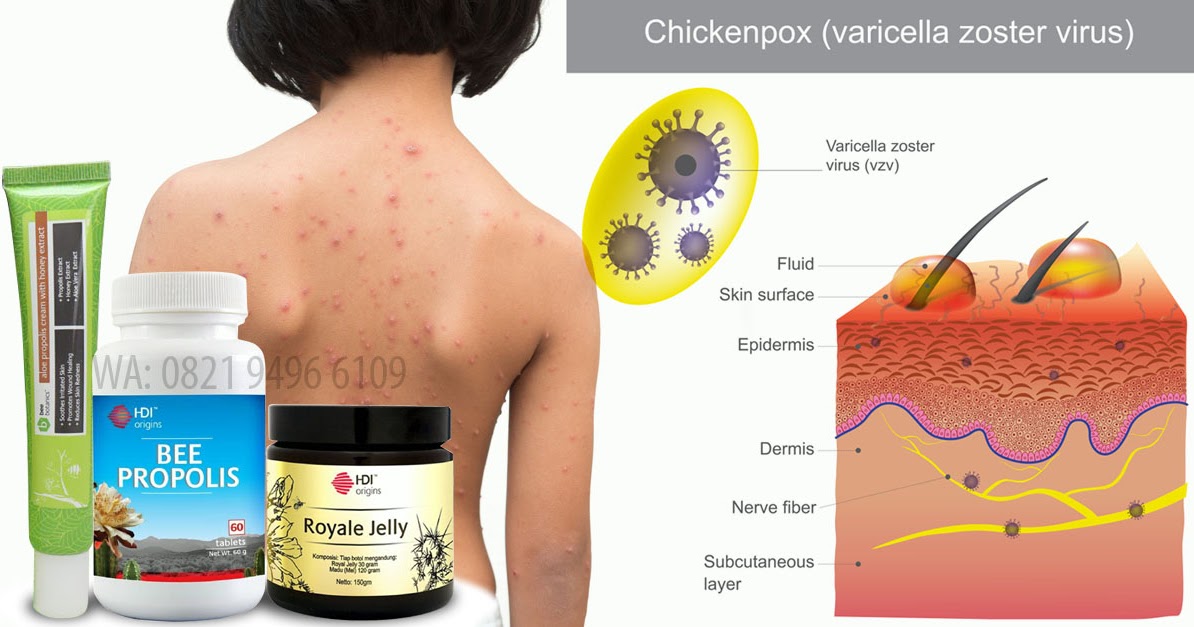
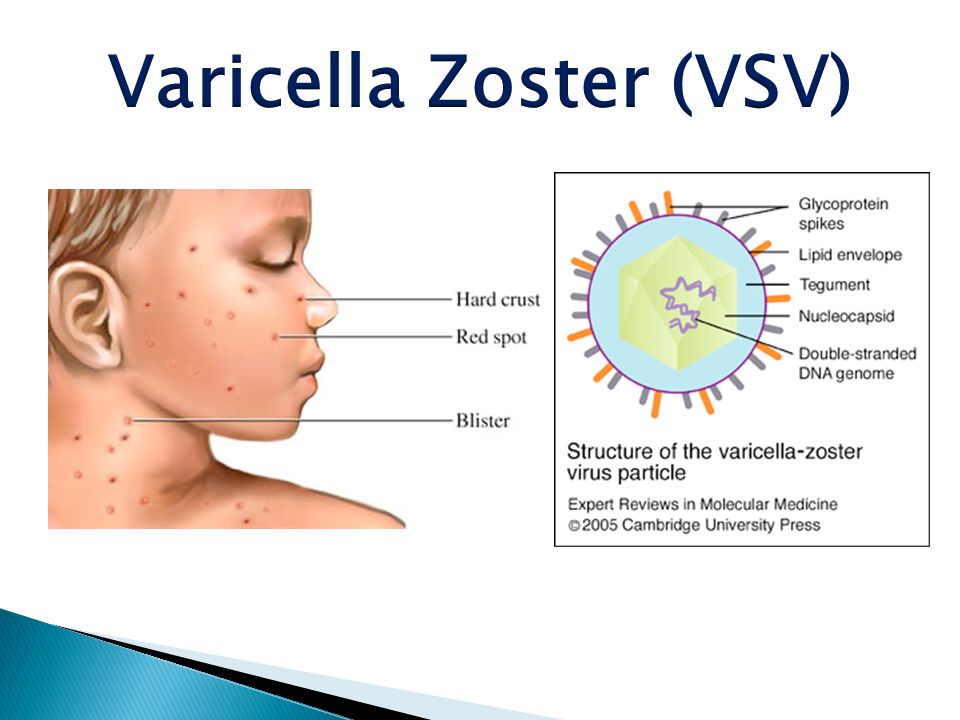
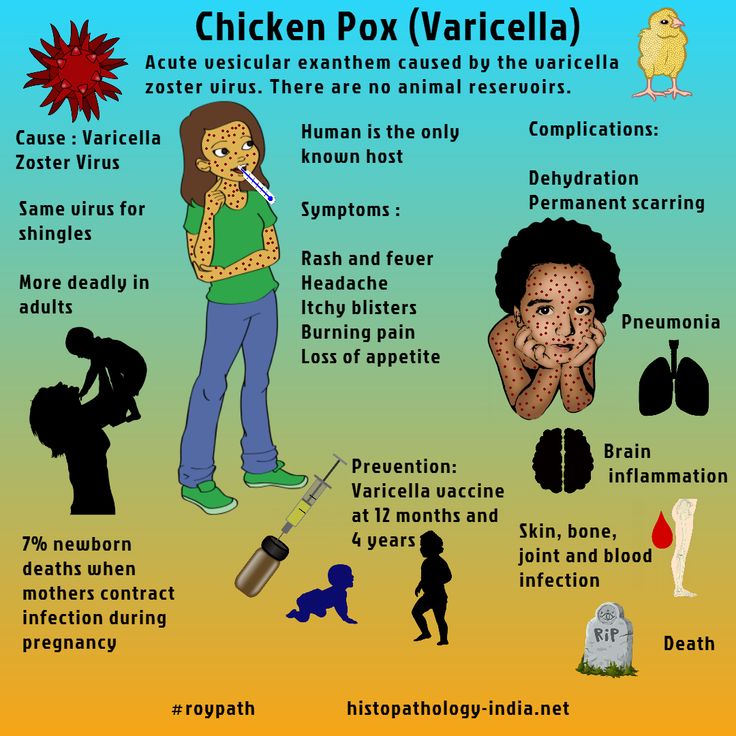
Chickenpox is an infection caused by a virus called the varicella-zoster virus. Chickenpox used to be a common infection, especially in children under age 12. It’s less common now because a vaccine is available to help prevent it. A vaccine is medicine that makes you immune to certain diseases.
Chickenpox usually isn’t dangerous in children. But some people are at higher risk for complications from chickenpox, including pregnant people and newborns.
The chances of getting chickenpox during pregnancy are low. Most pregnant people are immune to chickenpox because they’ve had the infection before or they’ve been vaccinated against it. Talk with your health care provider to make sure you’re immune to chickenpox before you get pregnant or early in pregnancy.
What are the symptoms of chickenpox?
Chickenpox causes an itchy rash that turns into blisters and then scabs. The rash usually starts on the chest, back, and face and spreads all over the body. The rash appears about 10 to 21 days after you’re infected and can last 5 to 10 days.
Other symptoms can include fever, headache, being tired and not being hungry. These symptoms may appear 1 to 2 days before the rash.
How does chickenpox spread?
If you’re not immune to chickenpox, you can get it easily by being in contact with someone who has the infection. A person with chickenpox can spread the infection starting about 2 days before the rash appears and until all the blisters are covered by scabs. It can spread through:
It can spread through:
- Droplets in the air when someone with chickenpox coughs or sneezes
- The saliva (spit) or mucus of someone with chickenpox
- Touching a chickenpox rash
If you’re not immune to chickenpox, you can also get it through close contact with someone who has shingles. Shingles is an infection caused by the same virus that causes chickenpox. If you’ve had chickenpox before, the virus stays in your body and can come back later as shingles. Shingles causes a painful rash on one side of the face or body. People with shingles can spread chickenpox to other people, but they can’t spread shingles to other people.
Can chickenpox during pregnancy cause problems for you and your baby?
Yes. Having chickenpox during pregnancy can increase your risk of getting pneumonia and can even be life-threatening. Pneumonia is a lung infection that can be very serious. The symptoms of pneumonia include cough, chest pain when you breathe or cough, fever, fatigue (being very tired) and shortness of breath.
Chickenpox during pregnancy can cause these problems for your baby:
If you get chickenpox during the first 20 weeks of pregnancy, your baby may have an increased risk for congenital varicella syndrome. This is a rare group of serious birth defects that can cause:
- Scars on the skin
- Problems with the arms, legs, brain and eyes
- Gastrointestinal complications
- Low birthweight. This is when a baby is born weighing less than 5 pounds, 8 ounces.
If you get chickenpox between 2 weeks before birth to 2 weeks after birth, you can pass the infection to your baby. If this happens, the infection in your baby usually is mild.
If you get chickenpox immediately before or right after birth (5 days before birth to 2 days after birth), your baby may have an increased risk for a serious infection called neonatal varicella. This infection can be life-threatening, but treatment is helping more babies survive.
If you have a preterm birth, your newborn may be at higher risk of complications from chickenpox. Preterm birth is birth that happens before 37 weeks of pregnancy.
Can you prevent chickenpox?
Yes. The varicella vaccine can protect you from chickenpox. In fact, this vaccine prevents more than 3.5 million cases of chickenpox each year. But the vaccine is not safe to get during pregnancy.
Talk to your provider if you’re pregnant or planning a pregnancy and you’re not sure if you've had the vaccine or had chickenpox before. Your provider can do a blood test to find out if you’re immune.
If you aren’t immune, how can you protect yourself from chickenpox during pregnancy?
If you’re planning a pregnancy and the blood test shows you’re not immune, get vaccinated. You get the vaccine in two doses. It’s best to wait 3 months after the second dose before getting pregnant.
If you’re already pregnant, don’t get the vaccine until after you give birth.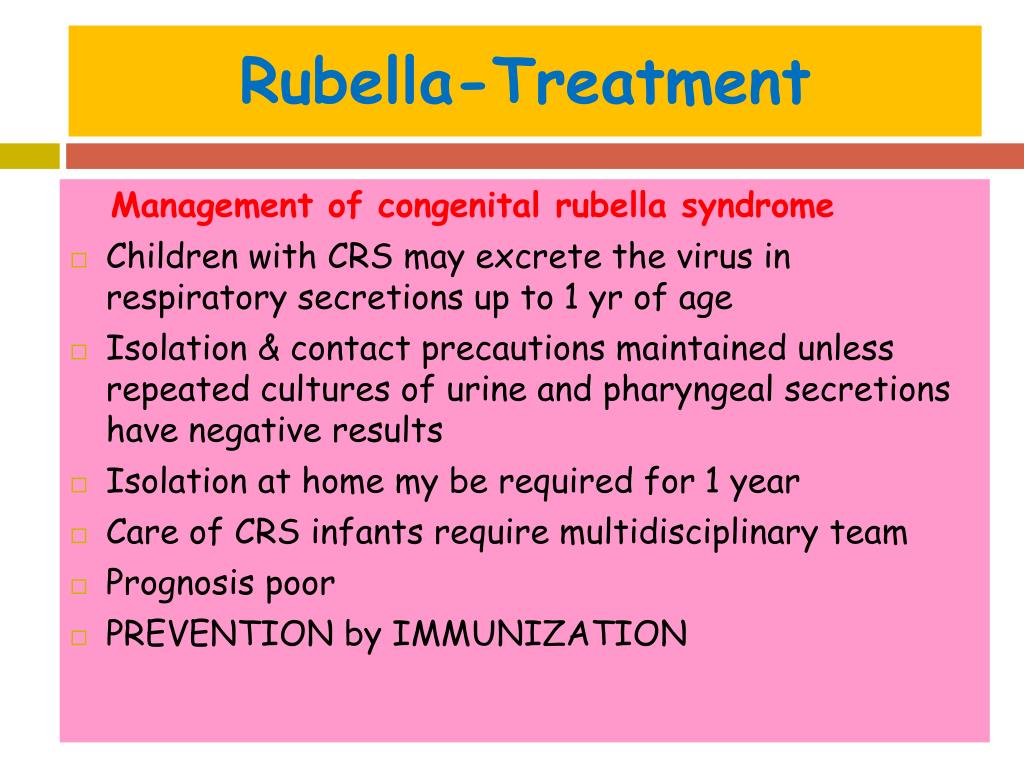 In the meantime, stay away from anyone who has chickenpox or shingles.
In the meantime, stay away from anyone who has chickenpox or shingles.
Tell your provider right away if you’re pregnant and you come into contact with someone who has chickenpox. Your provider can treat you with medicine that has chickenpox antibodies. Antibodies help the body fight infections. It’s important to get treatment within 10 days after you’ve come into contact with chickenpox to help prevent the infection or make it less serious. And tell your provider if you come in contact with a person who has shingles. Your provider can decide if you need treatment to help prevent you from getting infected.
How is chickenpox diagnosed?
Your provider can tell you if you have chickenpox by doing a physical exam. Your provider may do a blood test or take a swab of the rash and send it to a laboratory for testing to be sure it’s chickenpox.
How is chickenpox treated during pregnancy?
If you get chickenpox during pregnancy, your provider may give you an antiviral medicine such as acyclovir or valacyclovir. An antiviral is a medicine to treat infections caused by viruses. These medicines are safe to use during pregnancy. They work best when given within 24 hours of the chickenpox rash appearing.
An antiviral is a medicine to treat infections caused by viruses. These medicines are safe to use during pregnancy. They work best when given within 24 hours of the chickenpox rash appearing.
If you have chickenpox and develop signs or symptoms of pneumonia, your provider may want you to stay in the hospital and be treated with acyclovir through an IV (through a needle into a vein).
If you get chickenpox during pregnancy, how is your baby treated after birth?
If you have chickenpox during pregnancy, your baby’s provider may treat your baby right after birth with medicine that has chickenpox antibodies. The medicine can help prevent chickenpox in your baby or make it less dangerous. If your baby gets chickenpox in the 2 weeks after birth, your baby may also be treated with antiviral medicine.
Can you get chickenpox from someone who has gotten the vaccine?
Yes, but it’s rare. If a vaccinated person gets chickenpox, they can still spread it to others. But the vaccine is more than 90 percent effective at preventing chickenpox. Providers recommend that children get their first dose of the varicella vaccine at 12 to 15 months of age and the second dose at age 4 to 6.
But the vaccine is more than 90 percent effective at preventing chickenpox. Providers recommend that children get their first dose of the varicella vaccine at 12 to 15 months of age and the second dose at age 4 to 6.
Last reviewed: May 2021
Management of varicella infection (chickenpox) in pregnancy
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Elsevier Science
Full text links
Review
. 2012 Mar;34(3):287-292.
2012 Mar;34(3):287-292.
doi: 10.1016/S1701-2163(16)35190-8.
Alon Shrim 1 , Gideon Koren 2 , Mark H Yudin 2 , Dan Farine 2 , MATERNAL FETAL MEDICINE COMMITTEE
Collaborators, Affiliations
Collaborators
- MATERNAL FETAL MEDICINE COMMITTEE:
Robert Gagnon 3 , Lynda Hudon 1 , Melanie Basso 4 , Hayley Bos 5 , Joan Crane 6 , Gregory Davies 7 , Marie-France Delisle 4 , Savas Menticoglou 8 , William Mundle 9 , Annie Ouellet 10 , Tracy Pressey 4 , Christy Pylypjuk 11 , Anne Roggensack 12 , Frank Sanderson 13 , Vyta Senikas 14
Affiliations
- 1 Montreal QC.
- 2 Toronto ON.
- 3 Verdun QC.
- 4 Vancouver BC.
- 5 London ON.
- 6 St. John's NL.
- 7 Kingston ON.
- 8 Winnipeg MB.
- 9 Windsor ON.
- 10 Sherbrooke QC.
- 11 Saskatoon SK.
- 12 Calgary AB.

- 13 Saint John NB.
- 14 Ottawa ON.
- PMID: 22385673
- DOI: 10.1016/S1701-2163(16)35190-8
Review
Alon Shrim et al. J Obstet Gynaecol Can. 2012 Mar.
. 2012 Mar;34(3):287-292.
doi: 10.1016/S1701-2163(16)35190-8.
Authors
Alon Shrim 1 , Gideon Koren 2 , Mark H Yudin 2 , Dan Farine 2 , MATERNAL FETAL MEDICINE COMMITTEE
Collaborators
- MATERNAL FETAL MEDICINE COMMITTEE:
Robert Gagnon 3 , Lynda Hudon 1 , Melanie Basso 4 , Hayley Bos 5 , Joan Crane 6 , Gregory Davies 7 , Marie-France Delisle 4 , Savas Menticoglou 8 , William Mundle 9 , Annie Ouellet 10 , Tracy Pressey 4 , Christy Pylypjuk 11 , Anne Roggensack 12 , Frank Sanderson 13 , Vyta Senikas 14
Affiliations
- 1 Montreal QC.

- 2 Toronto ON.
- 3 Verdun QC.
- 4 Vancouver BC.
- 5 London ON.
- 6 St. John's NL.
- 7 Kingston ON.
- 8 Winnipeg MB.
- 9 Windsor ON.
- 10 Sherbrooke QC.
- 11 Saskatoon SK.
- 12 Calgary AB.
- 13 Saint John NB.
- 14 Ottawa ON.
- PMID: 22385673
- DOI: 10.1016/S1701-2163(16)35190-8
Abstract
Objective: To review the existing data regarding varicella zoster virus infection (chickenpox) in pregnancy, interventions to reduce maternal complications and fetal infection, and antepartum and peripartum management.
Methods: The maternal and fetal outcomes in varicella zoster infection were reviewed, as well as the benefit of the different treatment modalities in altering maternal and fetal sequelae.
Evidence: Medline was searched for articles and clinical guidelines published in English between January 1970 and November 2010.
Values: The quality of evidence was rated using the criteria described in the Report of the Canadian Task Force on Preventive Health Care. Recommendations for practice were ranked according to the method described in that report (Table).
Recommendations: 1. Varicella immunization is recommended for all non-immune women as part of pre-pregnancy and postpartum care. (II-3B) 2. Varicella vaccination should not be administered in pregnancy. However, termination of pregnancy should not be advised because of inadvertent vaccination during pregnancy. (II-3D) 3. The antenatal varicella immunity status of all pregnant women should be documented by history of previous infection, varicella vaccination, or varicella zoster immunoglobulin G serology.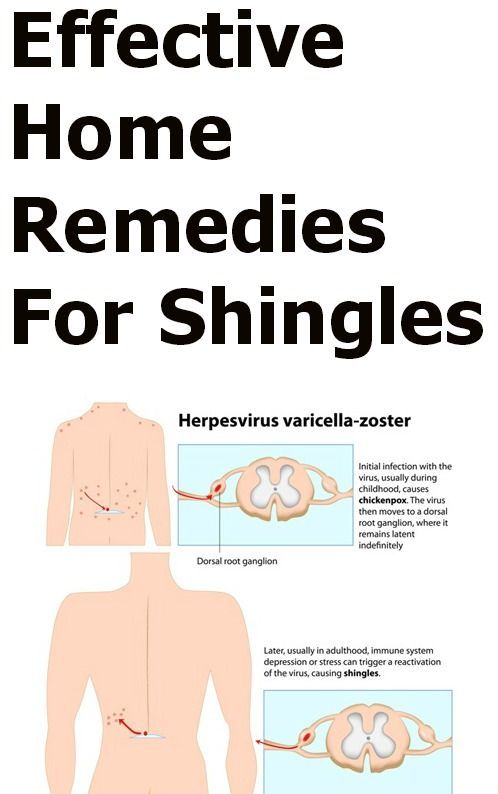 (III-C) 4. All non-immune pregnant women should be informed of the risk of varicella infection to themselves and their fetuses. They should be instructed to seek medical help following any contact with a person who may have been contagious. (II-3B) 5. In the case of a possible exposure to varicella in a pregnant woman with unknown immune status, serum testing should be performed. If the serum results are negative or unavailable within 96 hours from exposure, varicella zoster immunoglobulin should be administered. (III-C) 6. Women who develop varicella infection in pregnancy need to be made aware of the potential adverse maternal and fetal sequelae, the risk of transmission to the fetus, and the options available for prenatal diagnosis. (II-3C) 7. Detailed ultrasound and appropriate follow-up is recommended for all women who develop varicella in pregnancy to screen for fetal consequences of infection. (III-B) 8. Women with significant (e.g., pneumonitis) varicella infection in pregnancy should be treated with oral antiviral agents (e.
(III-C) 4. All non-immune pregnant women should be informed of the risk of varicella infection to themselves and their fetuses. They should be instructed to seek medical help following any contact with a person who may have been contagious. (II-3B) 5. In the case of a possible exposure to varicella in a pregnant woman with unknown immune status, serum testing should be performed. If the serum results are negative or unavailable within 96 hours from exposure, varicella zoster immunoglobulin should be administered. (III-C) 6. Women who develop varicella infection in pregnancy need to be made aware of the potential adverse maternal and fetal sequelae, the risk of transmission to the fetus, and the options available for prenatal diagnosis. (II-3C) 7. Detailed ultrasound and appropriate follow-up is recommended for all women who develop varicella in pregnancy to screen for fetal consequences of infection. (III-B) 8. Women with significant (e.g., pneumonitis) varicella infection in pregnancy should be treated with oral antiviral agents (e. g., acyclovir 800 mg 5 times daily). In cases of progression to varicella pneumonitis, maternal admission to hospital should be seriously considered. Intravenous acyclovir can be considered for severe complications in pregnancy (oral forms have poor bioavailability). The dose is usually 10 to 15 mg/kg of BW or 500 mg/m² IV every 8 h for 5 to 10 days for varicella pneumonitis, and it should be started within 24 to 72 h of the onset of rash. (III-C) 9. Neonatal health care providers should be informed of peripartum varicella exposure in order to optimize early neonatal care with varicella zoster immunoglobulin and immunization. (III-C) Varicella zoster immunoglobulin should be administered to neonates whenever the onset of maternal disease is between 5 days before and 2 days after delivery. (III-C).
g., acyclovir 800 mg 5 times daily). In cases of progression to varicella pneumonitis, maternal admission to hospital should be seriously considered. Intravenous acyclovir can be considered for severe complications in pregnancy (oral forms have poor bioavailability). The dose is usually 10 to 15 mg/kg of BW or 500 mg/m² IV every 8 h for 5 to 10 days for varicella pneumonitis, and it should be started within 24 to 72 h of the onset of rash. (III-C) 9. Neonatal health care providers should be informed of peripartum varicella exposure in order to optimize early neonatal care with varicella zoster immunoglobulin and immunization. (III-C) Varicella zoster immunoglobulin should be administered to neonates whenever the onset of maternal disease is between 5 days before and 2 days after delivery. (III-C).
Similar articles
-
No. 274-Management of Varicella Infection (Chickenpox) in Pregnancy.
Shrim A, Koren G, Yudin MH, Farine D. Shrim A, et al. J Obstet Gynaecol Can. 2018 Aug;40(8):e652-e657. doi: 10.1016/j.jogc.2018.05.034. J Obstet Gynaecol Can. 2018. PMID: 30103889
-
Prenatal screening for fetal aneuploidy in singleton pregnancies.
Chitayat D, Langlois S, Douglas Wilson R; SOGC GENETICS COMMITTEE; CCMG PRENATAL DIAGNOSIS COMMITTEE. Chitayat D, et al. J Obstet Gynaecol Can. 2011 Jul;33(7):736-750. doi: 10.1016/S1701-2163(16)34961-1. J Obstet Gynaecol Can. 2011. PMID: 21749752
-
Guidelines for the Management of a Pregnant Trauma Patient.
Jain V, Chari R, Maslovitz S, Farine D; Maternal Fetal Medicine Committee, Bujold E, Gagnon R, Basso M, Bos H, Brown R, Cooper S, Gouin K, McLeod NL, Menticoglou S, Mundle W, Pylypjuk C, Roggensack A, Sanderson F.
 Jain V, et al. J Obstet Gynaecol Can. 2015 Jun;37(6):553-74. doi: 10.1016/s1701-2163(15)30232-2. J Obstet Gynaecol Can. 2015. PMID: 26334607 English, French.
Jain V, et al. J Obstet Gynaecol Can. 2015 Jun;37(6):553-74. doi: 10.1016/s1701-2163(15)30232-2. J Obstet Gynaecol Can. 2015. PMID: 26334607 English, French. -
Varicella and the pregnant woman: prevention and management.
Daley AJ, Thorpe S, Garland SM. Daley AJ, et al. Aust N Z J Obstet Gynaecol. 2008 Feb;48(1):26-33. doi: 10.1111/j.1479-828X.2007.00797.x. Aust N Z J Obstet Gynaecol. 2008. PMID: 18275568 Review.
-
Antiviral prophylaxis and treatment in chickenpox. A review prepared for the UK Advisory Group on Chickenpox on behalf of the British Society for the Study of Infection.
Ogilvie MM. Ogilvie MM. J Infect. 1998 Jan;36 Suppl 1:31-8. doi: 10.1016/s0163-4453(98)80153-9. J Infect.
 1998. PMID: 9514106 Review.
1998. PMID: 9514106 Review.
See all similar articles
Cited by
-
The Misattributed and Silent Causes of Poor COVID-19 Outcomes Among Pregnant Women.
Machluf Y, Rosenfeld S, Ben Shlomo I, Chaiter Y, Dekel Y. Machluf Y, et al. Front Med (Lausanne). 2021 Oct 26;8:745797. doi: 10.3389/fmed.2021.745797. eCollection 2021. Front Med (Lausanne). 2021. PMID: 34765620 Free PMC article.
-
Immunity to varicella zoster virus among pregnant women in the Norwegian Mother and Child Cohort Study.
Mirinaviciute G, Barlinn R, Gjeruldsen Dudman S, Flem E. Mirinaviciute G, et al. PLoS One. 2019 Aug 13;14(8):e0221084. doi: 10.1371/journal.pone.0221084. eCollection 2019. PLoS One.
 2019. PMID: 31408478 Free PMC article. Clinical Trial.
2019. PMID: 31408478 Free PMC article. Clinical Trial. -
Susceptibility for varicella and factors associated with immunity among pregnant women in a tertiary care hospital in Sri Lanka- a cross-sectional study.
Premathilake IP, Aluthbaduge P, Senanayake CP, Jayalatharachchi R, Gamage S, Jayamaha J. Premathilake IP, et al. BMC Infect Dis. 2019 Apr 29;19(1):356. doi: 10.1186/s12879-019-3996-1. BMC Infect Dis. 2019. PMID: 31035950 Free PMC article.
-
Implementation of Hospital Policy for Healthcare Workers and Patients Exposed to Varicella-Zoster Virus.
Kim SH, Park SH, Choi SM, Lee DG. Kim SH, et al. J Korean Med Sci. 2018 Aug 27;33(36):e252. doi: 10.3346/jkms.2018.33.e252. eCollection 2018 Sep 3. J Korean Med Sci.
 2018. PMID: 30181734 Free PMC article. Review.
2018. PMID: 30181734 Free PMC article. Review. -
Microbiology laboratory and the management of mother-child varicella-zoster virus infection.
De Paschale M, Clerici P. De Paschale M, et al. World J Virol. 2016 Aug 12;5(3):97-124. doi: 10.5501/wjv.v5.i3.97. World J Virol. 2016. PMID: 27563537 Free PMC article. Review.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Full text links
Elsevier Science
Cite
Format: AMA APA MLA NLM
Send To
Chickenpox ("chickenpox"): why is this "childhood" infection dangerous for pregnant women?
| Attention, chicken pox! How to protect a pregnant woman from infection if someone in the family gets sick |
after the last rash appeared) If someone in your family had contact with a sick person and could potentially be infected.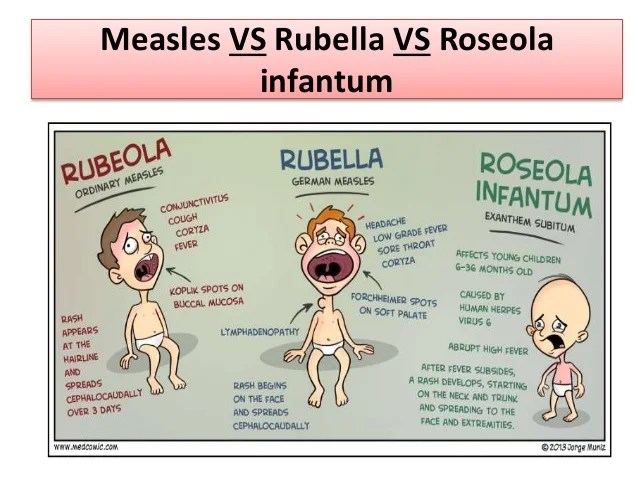 It may manifest the first manifestations of the disease in the period from 7 to 21 days from the moment of contact with the patient. According to such a person, it is also not advisable to communicate with a pregnant woman during this period, because in case of illness, there is a risk of infection. |
Varicella (chickenpox)
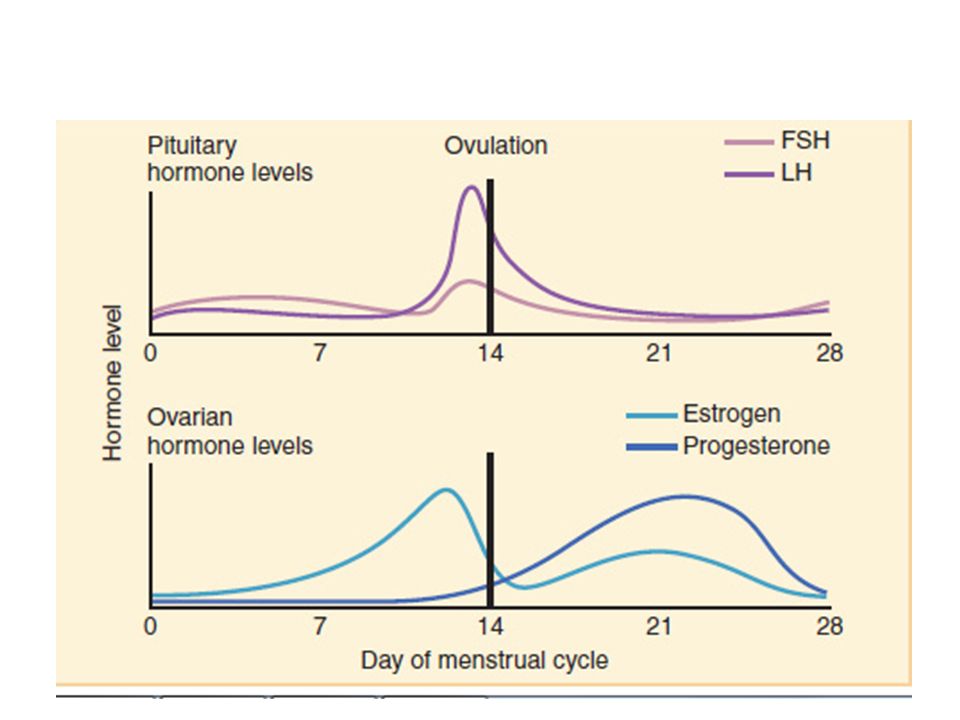
Pathogen - DNA-containing herpes virus type 3 Varicella-Zoster
Incubation period - from 7 to 17 days
Rash - appears simultaneously with an increase in temperature or several hours later. First, small spots form, which quickly turn into papules and vesicles. Vesicles are usually unicameral. Rashes are located on the skin of the trunk, face, limbs, scalp, less often on the mucous membranes of the mouth, respiratory tract, eyes, and external genital organs.
Rash may be accompanied by itching. On the mucous membranes, the elements of the rash quickly macerate with the formation of superficial erosions that heal within 1-2 days.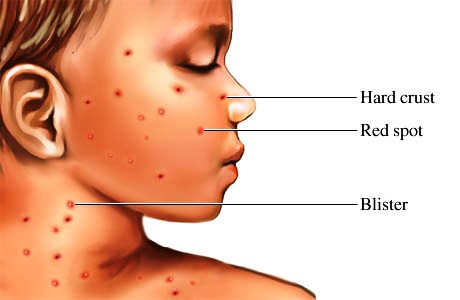 On the skin, the bubbles gradually dry out and become covered with crusts. After exfoliation of the crusts, light pigmentation remains in their place for a long time, in rare cases - scars. The process of rash occurs in jolts, with an interval of 1-2 days for 2-4 days, in rare cases up to 7 days or more.
On the skin, the bubbles gradually dry out and become covered with crusts. After exfoliation of the crusts, light pigmentation remains in their place for a long time, in rare cases - scars. The process of rash occurs in jolts, with an interval of 1-2 days for 2-4 days, in rare cases up to 7 days or more.
There is a false polymorphism of the rash.
Infectiousness period - 10-12 days 1-2 days before the appearance of the rash, the entire period of the rash, up to 5 days after the
appearance of the last rash (blister - vesicles).
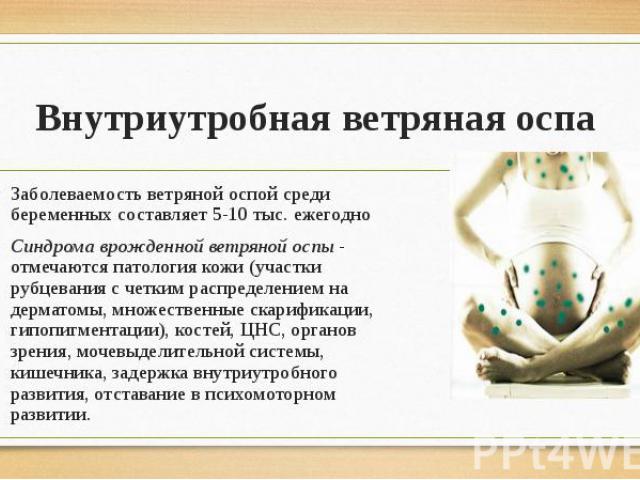
Danger for pregnant women - the most unfavorable first trimester and the last week before delivery. Fetal risk is lowest between 20 and 35 weeks. Infection of a pregnant woman in the 1st trimester may result in the death of the embryo. When infected before the 20th week of pregnancy, there is a danger of the formation of congenital vitrine syndrome. This pathology is characterized by: a violation of the normal development of the limbs, brain, organs of vision, the formation of scars on the skin, as well as a general delay in intrauterine development. A pregnant woman, who fell ill on the eve of childbirth, may have a child with chickenpox of a newborn.
A pregnant woman, who fell ill on the eve of childbirth, may have a child with chickenpox of a newborn.
In general, the pathology of pregnancy is not common, so the disease is not a direct indication for termination of pregnancy. Pregnant women must undergo prenatal screening (double and triple tests), ultrasound (especially for a period of 20-22 weeks). In some cases, a study of amniotic fluid by PCR for the presence of virus DNA in them.
Prevention - isolation of the patient up to 5 days after the last rash. Contacts up to 3 years old, not sick, are isolated from 11 to 21 days from the moment of contact. Isolation of patients for 4 days from the onset of the disease, newborns with congenital rubella ─ up to 1 year. Contacts are not allowed in children's groups for 21 days (from the moment of isolation of the patient), monitoring of contacts.
Prophylactic vaccination available. The virus persists in the body for life, but recurrence after an illness is very rare. When the virus is activated, another form of infection develops - herpes zoster (zoster).
When the virus is activated, another form of infection develops - herpes zoster (zoster).
Emergency prophylaxis on contact (if the patient has not previously been ill and has no vaccination data) - passive immunization: donor immunoglobulin 0.2-0.5 ml / kg in the first 2 days.
Conclusion: If you have a family member with chickenpox, they need to be isolated for 10 to 12 days: 12 days before the rash appears and up to 5 days after the rash appears. To avoid infecting others, especially pregnant women, stay at home and avoid contact with anyone for six days after the rash begins to appear.
Patient Memo
| Infectious Diseases, Power agent | |
| Characteristic manifestations of the disease | 1.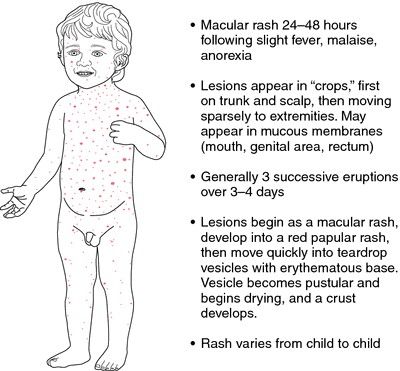 Visip appears simultaneously with fever and is accompanied by itching. Visip appears simultaneously with fever and is accompanied by itching. 2. Spots appear on the spot which then turn into bubbles. Gradually, the bubbles dry up and become covered with crusts. 3. Visipans are located on the trunk, face, limbs, less often on the mucous membranes of the mouth, eyes, and respiratory tract. |
| Disease risk for pregnant women! | The most unfavorable 1st trimester, which may end with the death of the embryo and the last week before delivery (possibly the birth of a child with chickenpox of the newborn). Pregnant women must undergo prenatal screening (double and triple tests) and ultrasound (especially at 20-22 weeks). |
| Prophylaxis | 1. Prophylactic vaccination is possible. 2. Emergency prophylaxis by contact (if the patient has not been ill before and has no data on vaccinations) - passive immunization: donor immunoglobulin in the first 2 days. |
| Attention! How to protect a pregnant woman from infection if someone in the family gets sick | If someone in your family gets sick with chickenpox, he needs to be isolated for 10-12 days (the entire period of the rash, and 5 days after the onset last rash).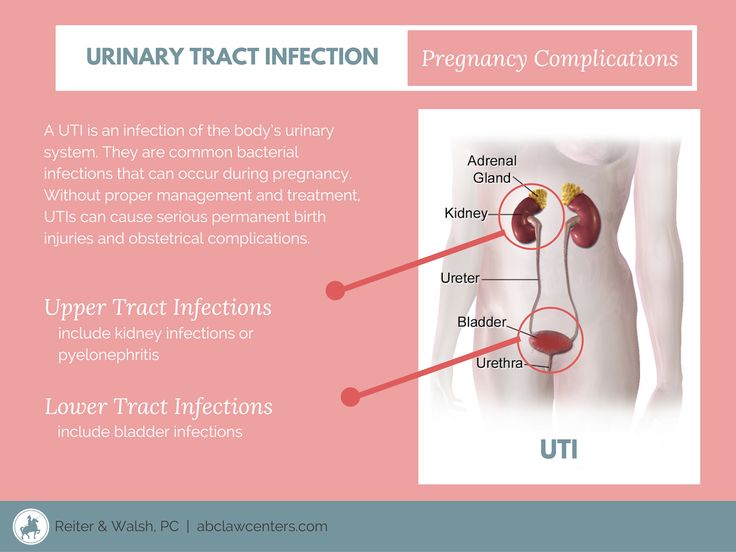 If someone in your family had contact with a sick person and could potentially be infected. |
Chickenpox in pregnant women
08/05/2022
What is chickenpox?
Chicken pox or varicella is an acute respiratory disease, and the infection is transmitted by airborne droplets, but this disease is always considered to be a childhood disease, but there are cases when a person has not been ill in childhood and has not acquired immunity against this disease , which leads to disease in adulthood.
Pregnant women can also get chickenpox, in which case the chickenpox is more severe, and there may be various complications, both in the pregnant woman and in the unborn child. Such a disease in pregnant women is very rare, but there are still coincidences when chickenpox coincides with pregnancy , but this should not be a reason for terminating pregnancy . This is due to the fact that the chickenpox virus rarely causes a complication in a child, and in the case when a pregnant woman becomes infected with chickenpox in the third trimester, the disease does not pose a danger to the fetus at all.
However, every woman should remember that the risk of severe damage to the baby is quite high and after the birth of the child, there may be negative consequences. This may be due to growth retardation, mental retardation, there may be atrophy of the cerebral cortex brain , scars on the skin or the baby may be stillborn or there will be a premature miscarriage. The percentage of such pathological phenomena is not high, however, there are such cases, therefore doctors are always attentive to such women and do everything so that the fetus does not suffer.
The percentage of such pathological phenomena is not high, however, there are such cases, therefore doctors are always attentive to such women and do everything so that the fetus does not suffer.
Symptoms of chickenpox in a pregnant woman
Symptoms of chickenpox in pregnant women are no different from the usual course of the disease, but the temperature may rise at this time, headaches begin to torment, and this is accompanied by chills and a rash on the body. Of course, first of all, a woman should turn to doctors and they assess her condition and immediately prescribe drugs to increase immunity , it can be immunoglobulin, and these dosage forms greatly soften the course of the disease.
Chickenpox is dangerous in the early stages of pregnancy , in the first trimester, it can end in miscarriage or abortion, and then the disease does not cause any harm, but it must be remembered that the most dangerous days are ten days before pregnancy , and also a few days after the birth of the child, it may end in the death of the baby. Therefore, to prevent this from happening, usually with chickenpox in the last 9 days0057 pregnancy , a pregnant woman should delay the onset of labor and at the same time introduce antibodies to the virus, which reduces the possibility of death.
Therefore, to prevent this from happening, usually with chickenpox in the last 9 days0057 pregnancy , a pregnant woman should delay the onset of labor and at the same time introduce antibodies to the virus, which reduces the possibility of death.
Treatment of chicken pox
In the event that a woman develops unbearable itching, antihistamines can be prescribed, but the woman should not scratch the crusts that have appeared, due to the fact that scars can remain on the body or on the face for life. Secondly, you can bring the infection into the wounds, which further aggravate the disease and toxins getting into blood will adversely affect the development of the fetus.
All blistering should be constantly treated with a solution of potassium permanganate or brilliant green. Every woman in the period of this disease should monitor her nails, underwear and the cleanliness of her pastels. During this period, a woman should observe bed rest, ventilate the room well, in addition, she should drink more and best of all tinctures of wild rose and sea buckthorn berries, and also eat, mainly vegetable and dairy foods.