Contraction pain in stomach
Ouch! Managing Labor Pains
We’ve all seen those movie scenes when a woman in a wheelchair is being rushed through the hospital doors after her water breaks. Cut to the mother-to-be screaming at the top of her lungs while pushing the baby out. Then, the money shot of the new parents staring adoringly at their newborn. But in real life, childbirth can take a lot longer than a few minutes of edited screen time, and there are a variety of ways to manage the pain that comes with bringing a baby into the world.
Erica Vu, certified nurse midwife at UC San Diego Health, talks about the stages of labor, the pain associated with the process and the interventions — both medicated and non-medicated — that are available.
How does a pregnant woman know when she is in labor?
Labor is very mysterious and one can never exactly know when it will start. Most women start to have various labor signs a few hours or weeks even before labor officially begins. These may include:
- Increased vaginal discharge — brown, pink or increased mucous discharge in general is a good sign the cervix is starting to ripen and the mucous plug, the sealed entrance to the uterus, is released.
- Many women notice more pelvis pressure as the baby’s head descends in her pelvis. Some call this “lightening” and it can happen weeks before or just as labor is starting.
- Some women start to have more nausea and loose stools or even diarrhea as the body is preparing for labor.
- The most common sign of labor is the increase in cramping associated with abdomen tightening or Braxton hicks. These early contractions usually start in the lower abdomen/pubic area and radiate towards the lower back. The frequency and duration of these start to increase and become more regular and rhythmic. At times, these contractions can start and increase rapidly, but for most, this can take several hours or even several days. We time the contractions from the start of one to the start of the next contraction. When they are still irregular and more than five minutes apart, most women are still in the cervical ripening/very early labor stage. These irregular contractions may even slow down or stop to give the mom’s a break.
 When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
What are the stages of labor and the pain associated with each stage?
The first stage of labor is cervical dilation, or the opening of the cervix, from 0 to 10 centimeters. Early labor is when the cervix starts to dilate from closed to five centimeters with regular contractions. Early labor contractions tend to be a bit shorter in duration (60 seconds or less) and more menstrual like-cramping in the lower abdomen and back. Early labor can take several hours or even a day or more.
When the contractions intensify, include the upper abdomen and are around two to three minutes apart, active labor is most likely starting, which is the stage from 6 to 10 centimeters. Active labor contractions are a lot stronger, longer (one to two minutes in duration) and almost always necessitate more focus, breathing and position changes/labor support. Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Once women get to 10 centimeters, the second stage of labor starts and pushing begins until the baby is delivered. This can take minutes to hours depending on the baby’s position, maternal effort and anesthesia interventions.
The third stage of labor is when the baby is out and the placenta is delivered.
What type of non-medicated interventions does UC San Diego Health provide for labor pain?
Still of Katherine Heigl and Seth Rogen from Universal Picture's Knocked Up.
Multiple position changes: Walking, lunges, squats, birthing balls, birthing stools and using Rebozos (a fabric shawl originally from Mexico that when placed appropriately can help to lift lower abdomen weight off the pubic bone, squeeze hips with back labor or help during the pushing stage by pulling on the fabric in different positions both sitting, squatting or standing).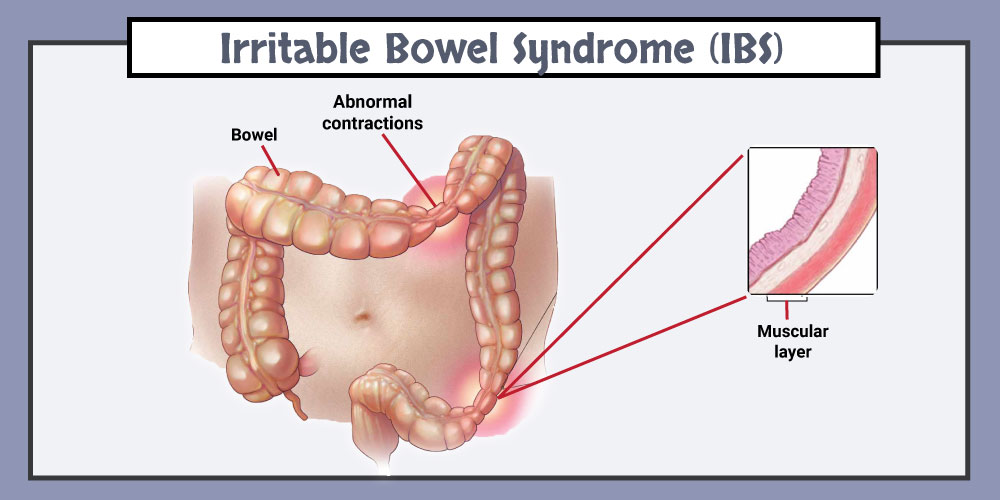 All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
Doulas: Women can hire private doulas or ask for one of our volunteer Hearts & Hands Program. Doulas are beneficial in so many ways, but specifically they give continuous non-medical labor support, including help with breathing techniques, counter pressure, position changes and massage and can be an advocate for your preference of labor process and birth.
Hydrotherapy (Labor tubs): Buoyancy can help with freedom of movement during contractions. Warm water helps to relax between contractions, eases body aches, including back aces, improves circulation and is a safe and effective form of pain relief.
Showers: Warm water helps with relaxation and decreases maternal tension during the peak of the contractions. Partners are invited to join to help with support.
Partners are invited to join to help with support.
Waterproof Wireless Monitors: These allow laboring women to be in the shower for pain relief while still allowing the benefits of hydrotherapy and close monitoring of the baby. The wireless monitors also allow women to change positions easily and walk freely about in their rooms or down the hallways if they so desire.
What type of medicated interventions does UC San Diego Health provide for labor pain?
Nitrous Oxide: Nitrous is a gas women breathe in through a mask during contractions. Women are still aware of the contractions, but the nitrous helps to decrease anxiety during them. Some women may experience nausea or dizziness initially but that usually resolves in a few minutes. This intervention allows freedom of movement, such as standing or sitting on a birthing ball, to help the baby descend down the birthing canal. Women can use nitrous as the only form of pain relief or it can also be used as a bridge to other forms of pain relief as labor progresses. It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
Intravenous Pain Relief: Narcotics or opioids help to relax the mind and body during the peak of the contractions. These help to decrease the sensations of pain, and depending on the stage of labor, may even allow the woman to rest and sleep a bit. It does cross over to the baby through the placenta but in time, just like the mother, it wears off and has little side effects. Some women feel initial dizziness and nausea as well but that often resolves with time. We often combine the narcotic with an anti-emetic (anti-nausea) medication to help but also to prolong the duration of the pain relief. There are different types of narcotics used for different stages of labor to decrease side effects in the newborn in case of a quick delivery.
Regional Anesthesia (Epidurals): This is a pain relief method that decreases pain sensations from the abdomen and below by placing a small tube into in an area surrounding the spinal cord in the lower back and is connected to a pump. The medicine is continuously infusing during the course of labor while women remain awake and alert. Most women do not feel the majority of the pain sensations of contractions, but some will feel the pressure of the baby descending in the pelvis, which helps women to push when ready. Women are not allowed to walk with epidurals but are able to change positions in bed.
Learn more about labor pain management options at UC San Diego Health.
About UC San Diego Health Midwives
To learn more about the featured medical specialties, please visit:
- Pregnancy and Birth Care
How to Tell the Difference?
What are Braxton Hicks contractions?
Braxton Hicks contractions, also known as false contractions, are the sensations your uterus produces in order to prepare for the labor.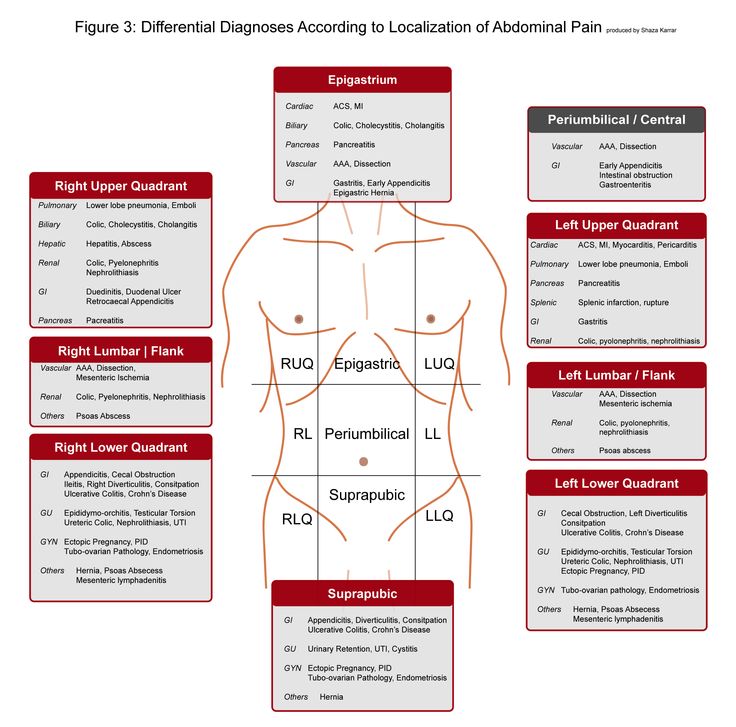 Your doctor will most likely inform you of Braxton Hicks and let you know to not concern over it.
Your doctor will most likely inform you of Braxton Hicks and let you know to not concern over it.
Still, women who are at risk of premature labor, and women with other health risk factors affecting the pregnancy often worry about being unable to distinguish real contractions from Braxton Hicks.
You can picture Braxton Hicks contractions as a way for your uterus to get in shape, to exercise, in order to prepare for childbirth.
Unlike real contractions, Braxton Hicks are weaker and last up to 30 seconds.
Typically, Braxton Hicks are the localized contractions of the sides of the uterus, rather than the front. However, as the belly already feels tight, it might be hard for you to distinguish whether your belly is tightening from the top downwards, or only on the sides.
Take a quiz
Find out what you can do with our Health Assistant
Braxton Hicks contractions can be repetitive but are not rhythmic, they do not get stronger. They appear randomly, or sporadically.
Most women get used to having Braxton Hicks in certain times of the day or in certain situations. For most women, the false contractions intensify when they're more active or get tired. Long sitting can also intensify Braxton Hicks, and they're frequent in late evenings.
Since every woman has a different level of sensitivity to contractions and other sensations that occur inside the belly (gas, bloating, under-rib pains and stretching), Braxton Hicks will feel differently.
In general, you'll feel false contractions as a type of painless, numb pressure in your upper abdomen. If you're sensitive enough to distinguish that the cramping is happening at the sides of the uterus, good for you! If not, don't get alarmed. There are still plenty of ways and strategies for you to distinguish false from real contractions.
What are real labor contractions?
A real contraction, on its own, happens when a uterus cramps from its top, creating a pressure on the cervix.
This causes the cervix to shorten and then, and eventually start to dilate. When it comes to a timely, full-term labor, most women prefer for the process to go as fast as possible.
However, if there's a risk from premature labor, you should learn more about real contraction to be able to recognize them. Here are some of the real contraction characteristics:
Pain
Real contractions are painful, but the intensity of pain varies among women.
Low-pelvic pressure
False contractions normally don't cause the pressuring feeling in the low abdomen and pelvic area. However, if you start feeling like there's something pressuring your pelvis from the inside out, it's possible that the contractions are real.
Rhythmic repetition
More frequent than 5 or 6 per hour. Real contractions most often repeat every 9-11 minutes and get progressively closer (every 8 and five minutes) with time.
Effect on the cervix
Real labor contractions do have an effect on the cervix opening.
Bleeding/other labor symptoms
If the contractions are accompanied by other labor symptoms, you can consider them to be real.
Persistence
Real contractions persist as the time passes, regardless if you change positions or rest. If your contractions persist regardless of rest, it’s time to grab your newborn essentials and head to the hospital!
How can I tell the difference between true and false labor?
There are a couple of ways to track your contractions and distinguish real from false. Here are a couple of guidelines:
Timing
Are contractions regular and repetitive? Braxton Hicks contractions are random, and you won't notice them repeating after 20 or 15 minutes. However, if the real contractions start, they will most certainly repeat every 15-20 minutes.
Consistency
False contractions will stop if you lie down and get some rest, most often after 20-30 minutes. They will also ease if you empty your bladder and drink some water. Real contractions will progress even if you get some rest.
Real contractions will progress even if you get some rest.
Low abdomen pain
Real contractions are followed with low abdomen pains, which vary from light, period-like cramping, to severe pain. Braxton Hicks can cause discomfort, especially if you're already feeling pains under your ribs or in your back (which is normal during pregnancy).
Lower back pain
Some women experience sharp, lower back pain during real contractions. If you already suffer from lower back pain, the contraction pains will be distinguishable as they'll feel sharper and more intense.
Duration
Braxton Hicks mainly last shorter than 30 seconds, while real contraction pains extend to 60 seconds or longer. The same goes for the pain sensation, regardless of the pain intensity.
Contraction course
With different levels of sensitivity to pain, and particularly with other typical pregnancy aches, you might be unable to distinguish the real contraction experience. In general, a real contraction will feel like a constant, lasting (60 seconds or longer) pain or pressure that starts either in your lower back (you might not feel this pain) and extend to your abdomen, resulting in low abdomen (pelvic) pressure.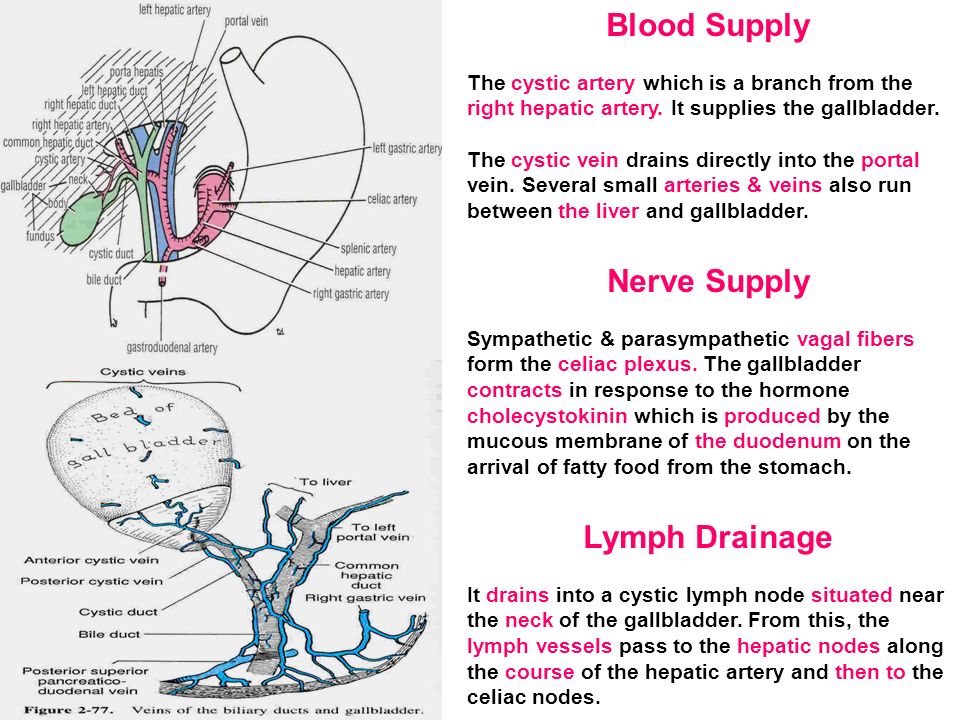 Unlike this, a false contraction will be a localized cramping in your upper abdomen lasting anywhere from a couple to 30 seconds.
Unlike this, a false contraction will be a localized cramping in your upper abdomen lasting anywhere from a couple to 30 seconds.
When should I call my doctor, doula, birth partner?
If you're full term, your Braxton Hicks will become more frequent and intense. Still, there are a couple of guidelines for distinguishing real contractions from Braxton Hicks.
Although these guidelines are general, every doctor practices their own protocols and tailors them to every individual pregnancy.
For example, if your pregnancy was regular and with no risk factors from the start, your doctor will instruct you differently than if it was a high-risk pregnancy.
Here's when you should grab your hospital bag and go to the doctor:
- Contractions are rhythmic and repeat every 15 minutes.
One of the base differences between real and Braxton Hicks contractions is the pace in which contractions re-occur. Braxton Hicks is random, which means that you can have 2-3 contractions one hour, and then none at all for the rest of the day.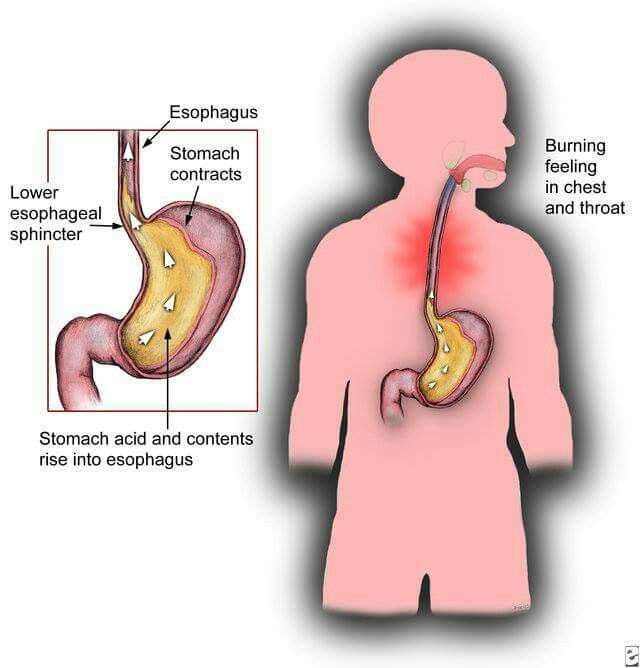
In the case of real contractions, the cramping doesn't stop after 2-3 hours. Instead, it intensifies. If you feel like your contractions are becoming regular or more intense past 2 hours, make sure to get medical help.
- You feel contractions in your lower abdomen. Braxton Hicks is typical to the upper abdomen area (above your hips). Low abdomen contractions, however, are most likely real, especially if accompanied by sharp pain.
- Contractions are painful. Braxton Hicks contractions are rarely painful. When they happen, you'll most likely feel a low-intense pain in your back or upper abdomen. If the contractions you are feeling are painful and focused in your lower abdomen, there's a good chance they're real.
- Presence of other symptoms. Nausea, vomiting, increased temperature, and blood pressure – are all signs that you need some sort of medical help. Contractions accompanied with these symptoms don't always have to signal labor, but they do in most cases.

Summing up
If you're not yet to go into labor, and you fear to miss the initial signs of a premature labor, your concerns are even greater. On a humorous side, most women realize that the intensity of Braxton Hicks contractions is nowhere near the intensity of real contractions. Rest assured that you will be able to distinguish real from false contractions. If you’re still worried, don’t hesitate to give your midwife or doctor a call and ask any questions.
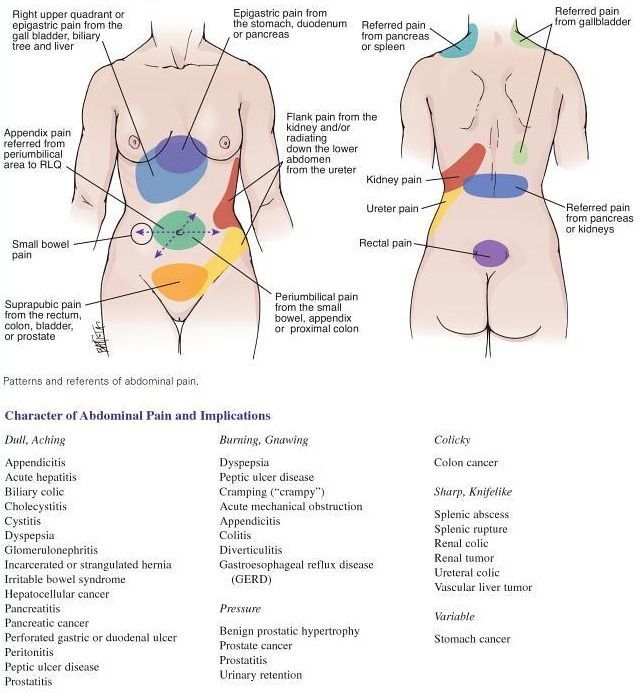
Cramping pains in the abdomen - causes
Cramping pains in the abdomen - unpleasant acute, sudden pain in various parts of the abdomen, which can be associated with a large number of diseases, not only of the gastrointestinal tract, but also of other organ systems.
Most often, this condition is associated with spasms in the biliary system, stomach, and intestines.
"Symptoms of anxiety": if the cramping pain in the abdomen is of high intensity, accompanied by fever, chills, nausea, vomiting, severe bloating in the abdomen, constipation or diarrhea, blood in the stool, tension in the anterior abdominal wall, sharp pain when lightly touching the abdomen or pushing the bed - you should immediately consult a doctor, as an examination of the abdomen, blood tests, ultrasound examination (ultrasound) of the abdominal cavity and, possibly, other studies to rule out acute surgical and other serious pathology.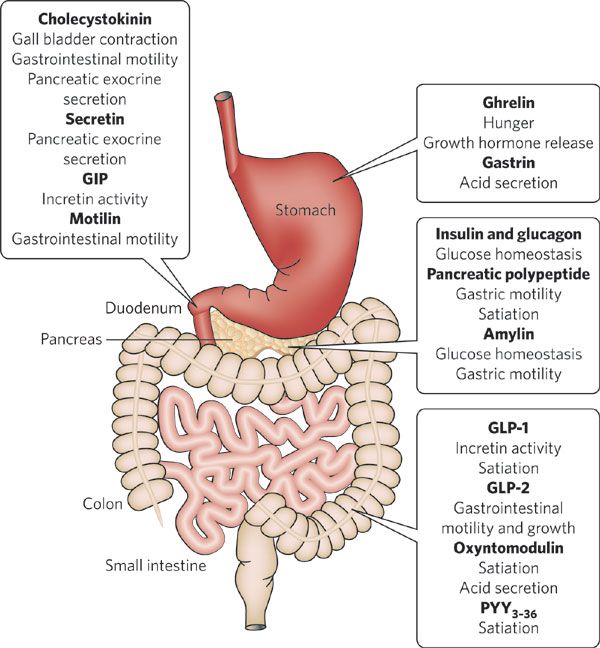 nine0005
nine0005
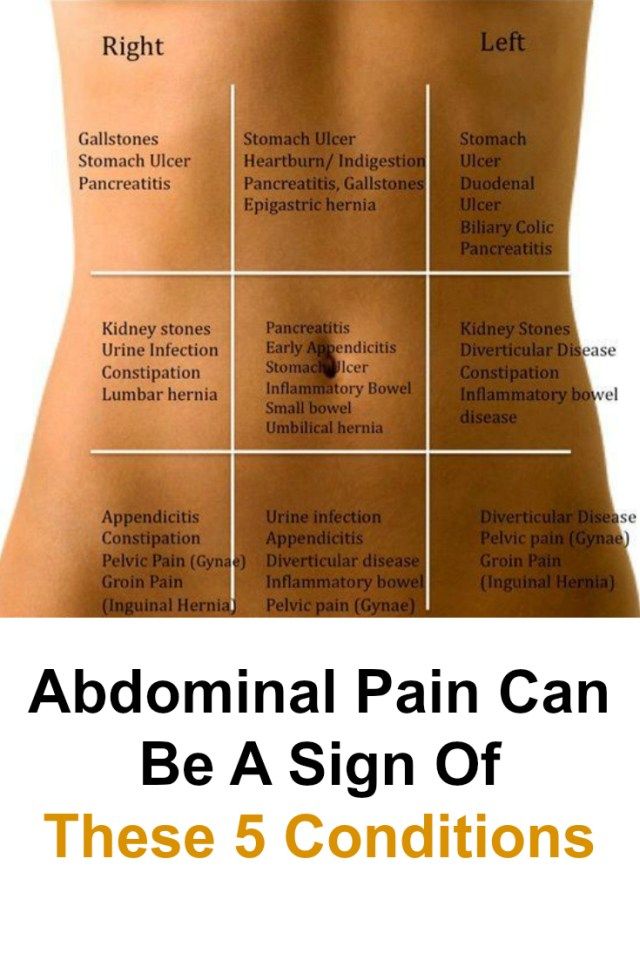
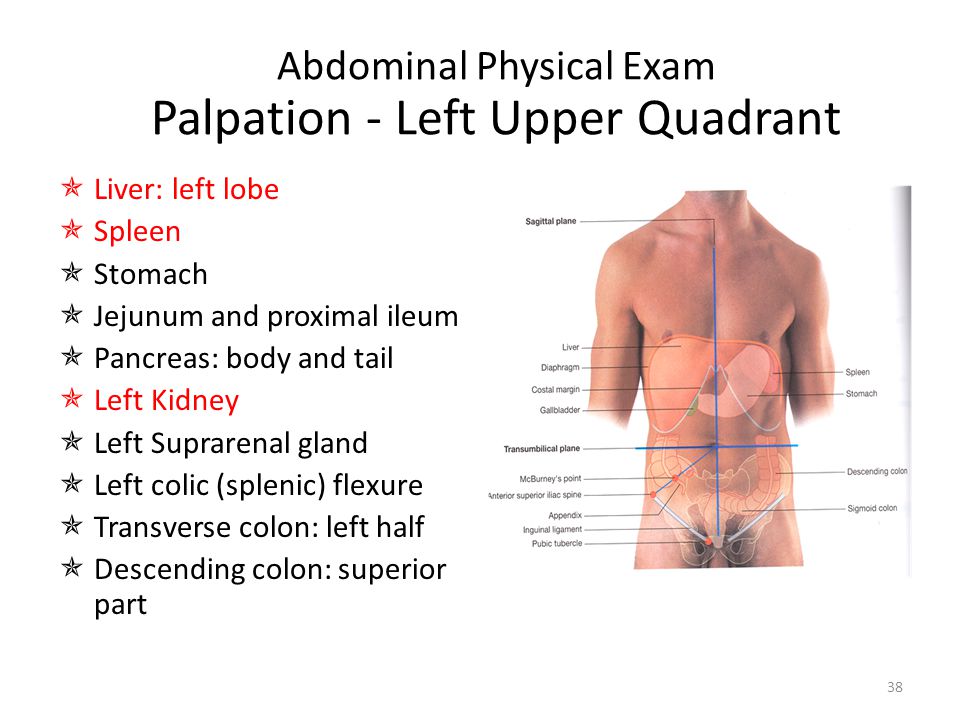
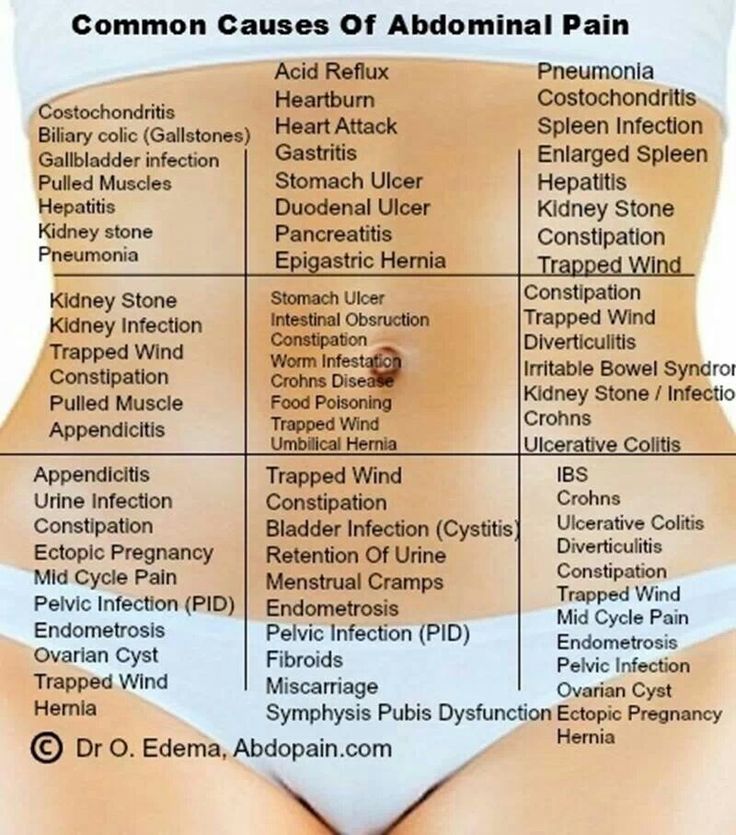
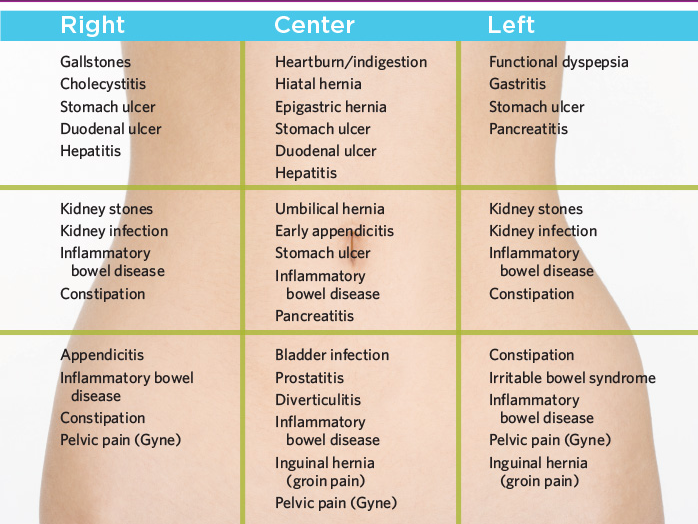
Causes of cramping pain in the right side of the abdomen:
- acute appendicitis
-
diseases of the stomach and duodenum (acute erosive gastroduodenitis, peptic ulcer, stomach cancer)
-
diseases of the liver and biliary system (acute cholecystitis, cholelithiasis and biliary colic, biliary dyskinesia with spasm of the gallbladder and bile duct sphincters, abscess, liver cancer)
-
bowel diseases (acute infectious enterocolitis, intestinal obstruction, strangulated hernia of the anterior abdominal wall, Crohn's disease, ulcerative colitis, diverticulitis, intestinal cancer)
-
damage to the vessels of the abdominal cavity (dissecting aortic aneurysm, thrombosis and embolism of intestinal vessels, hepatic veins, portal vein, thrombosis of the right renal artery)
-
diseases of the urinary system (urolithiasis and renal colic, cancer of the right kidney)
-
diseases of the genital organs (acute right-sided adnexitis, ovarian cyst, ectopic pregnancy, dysmenorrhea, acute prostatitis)
-
diseases of the nervous system (shingles (herpes zoster), damage to the solar plexus)
-
diseases of the chest organs (lower lobe right-sided pneumonia, pleurisy, pneumothorax, acute myocardial infarction, pulmonary embolism)
-
diseases of the endocrine system (diabetic ketoacidosis)
-
rare diseases (acute intermittent porphyria, lead colic, periodic illness)
Causes of cramping pain in the left side of the abdomen:
- diseases of the pancreas (acute pancreatitis, cancer)
-
diseases of the stomach (acute erosive gastritis, peptic ulcer, stomach cancer)
-
bowel diseases (acute infectious enterocolitis, intestinal obstruction, strangulated hernia of the anterior abdominal wall, Crohn's disease, ulcerative colitis, diverticulitis, intestinal cancer, Makelia-Dvorkin-Biehl syndrome (splenic flexure syndrome of the large intestine with severe accumulation of gases)
-
diseases of the spleen (splenomegaly in blood diseases, infectious diseases, cirrhosis of the liver; cysts, tumors, abscess, rupture, perisplenitis, impaired blood supply - spleen infarction)
-
damage to the vessels of the abdominal cavity (dissecting aneurysm of the aorta, thrombosis and embolism of the intestinal vessels, thrombosis of the splenic vein, left renal artery)
-
diseases of the urinary system (urolithiasis and renal colic, cancer of the left kidney)
-
diseases of the genital organs (acute left-sided adnexitis, ovarian cyst, ectopic pregnancy, dysmenorrhea, acute prostatitis)
-
diseases of the nervous system (shingles (herpes zoster), damage to the solar plexus)
Causes of epigastric cramping pain:
- acute appendicitis (at the beginning of the disease)
-
diseases of the stomach (acute gastritis, gastric ulcer, cancer)
-
hiatal hernia (strangulation)
nine0019 -
diseases of the biliary system (acute cholecystitis, cholelithiasis and biliary colic, biliary dyskinesia with gallbladder spasm)
-
bowel diseases (irritable bowel syndrome)
-
abdominal vascular disease (dissecting aortic aneurysm, thrombosis and embolism)
-
diseases of the nervous system (shingles (herpes zoster), damage to the solar plexus)
-
heart disease (acute myocardial infarction)
diseases of the pancreas (acute pancreatitis, cysts, cancer)
In our center we are engaged in determining the cause of cramping pain in the abdomen, conducting an examination and differential diagnosis of this condition. Experienced medical specialists (gastroenterologist, surgeon, neurologist, endocrinologist, psychotherapist), as well as the opportunity to be examined using expert-class equipment (ultrasound, videogastroduodenoscopy, colonoscopy) will help to deal with this problem. nine0005
Experienced medical specialists (gastroenterologist, surgeon, neurologist, endocrinologist, psychotherapist), as well as the opportunity to be examined using expert-class equipment (ultrasound, videogastroduodenoscopy, colonoscopy) will help to deal with this problem. nine0005
causes, symptoms, treatment, what to do with acute pain
If a person says: “I have abdominal pain”, then it is important to understand that abdominal pain can hide problems of any organs of the abdominal cavity, retroperitoneal space, small pelvis.
If a person says: “I have abdominal pain”, then it is important to understand that abdominal pain can hide problems of any organs of the abdominal cavity, retroperitoneal space, and small pelvis. The intestines (ileal, lean, thick, sigmoid, colon, transverse intestine), appendix, stomach, liver, duodenum, spleen, ureters, kidneys, mesenteric (mesenteric) intestinal vessels can give painful sensations to the stomach. Therefore, pathologies can be of a gastroenterological, surgical, gynecological, urological nature. nine0005
nine0005
Types of pain
Abdominal pain is very different:
- Acute and chronic . Acute pains occur suddenly, chronic ones develop gradually, their intensity increases step by step - sometimes over several weeks. In this case, a special variety is formed by chronically recurrent abdominal pain. They can suddenly make themselves felt, and then also suddenly disappear and resume after a certain period of time.
- Tonic and clonic . With tonic pain, the muscles are very tense, compacted areas appear on the abdomen, uncontrolled muscle contraction is observed. Tonic pains are accompanied by rather rhythmic spastic spasms.
- Burning (cutting) and aching - reminiscent of hunger.
Pain can be localized in the abdominal cavity, hypochondrium, areas above or below them.
Symptoms
A person who complains of abdominal pain may have different symptoms.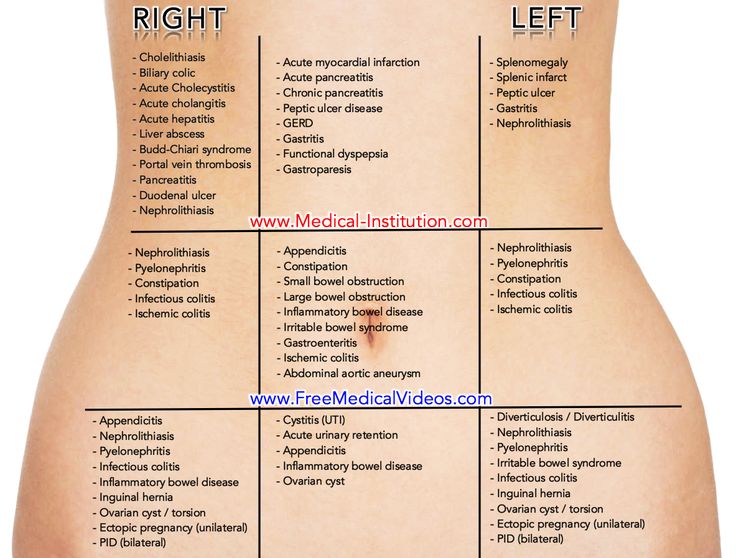 Most often, it manifests itself in the form of spasms, colic. nine0005
Most often, it manifests itself in the form of spasms, colic. nine0005
- Colic - attacks, primarily of stabbing (hence the name) pain. With colitis, a person has colitis in both sides, with appendicitis or inflammation of the ovaries - in the lower abdomen, with poisoning, the localization of colic can be in different parts of the abdomen and most often there is an additional symptom (vomiting, diarrhea).
- Spasms - pain accompanied by involuntary muscle contraction. In this case, the skin turns pale. Because of the pain, a person can lose consciousness. If spasms - with inflammatory diseases of the intestines, stomach, they are accompanied by fever. Gynecological problems are indicated by spasms accompanied by bleeding.,
- Anginal pain - an unpleasant sensation with a strong burning sensation.
- Sharp pain in the area above the navel is a common symptom of appendicitis.
- Feeling of "fullness" in the lower back may indicate problems with the large intestine
- Cyclic pain (sometimes intensify, then subside) - characteristic symptoms in diseases of the bladder, intestines.
- Pain with severe gas indicates a malfunction of the colon.
- Pain in the background of itching of the anus - symptoms of damage to the rectum.
- Unpleasant sensations in the abdomen that worsen at rest and disappear with movement are the result of circulatory problems.
Causes
What are the causes of abdominal pain, disorders of the abdominal cavity and retroperitoneal space?
Colic can be caused by appendicitis, inflammation of the ovaries (in these cases, colic in the lower abdomen), poisoning, colitis. With colitis, a person has colitis in both sides. If the colic is cramping and at the same time localized both in the abdomen and in the lower back, the pain is more intense, the cause is most often in urolithiasis, kidney injuries or pyelonephritis. Colic in the navel may be a response to irritants of the sensitive mesenteric plexus of the intestine. nine0005
Among the common causes of paroxysmal spasms are intestinal obstruction, gastroduodenitis.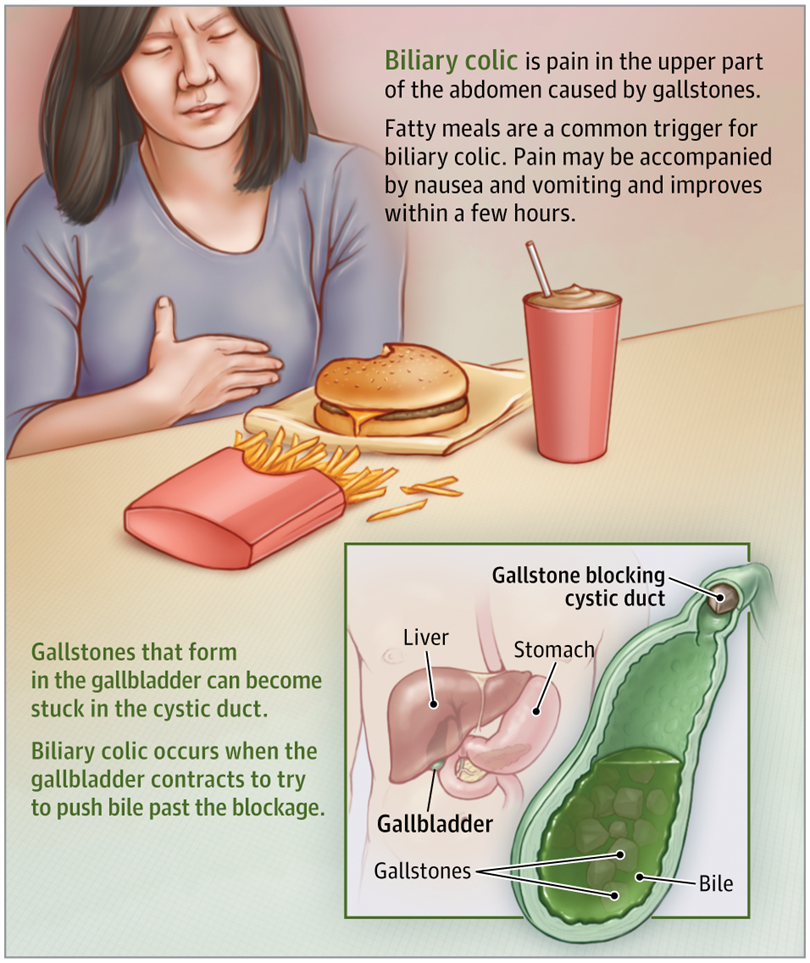 And for spasms during urination in women, most often there is endometriosis of the uterus.
And for spasms during urination in women, most often there is endometriosis of the uterus.
If abdominal pain is accompanied by increased gas formation, frequent urge to defecate, then the cause will most often be associated with diseases of the colon.
If the pain in the abdomen is anginal, and the patient is disturbed by an expressive burning sensation - the cause is most often gastritis (inflammation of the gastric mucosa) or pancreatitis (inflammation of the pancreas). If pain and burning sensation are accompanied by strong tension in the muscles of the abdominal wall, and a person complains that he is pressing in his chest, the cause may be related to heart pathologies: in particular, such pain is typical for 60% of patients with myocardial infarction. nine0005
Abdominal pain accompanied by subfebrile temperature (for a long time the temperature stays at 37.1-37.5 °C ) is most often caused by inflammatory bowel disease.
Diseases
Most often, abdominal pain is caused by diseases of the intestines, stomach, pancreas, problems with the gallbladder, as well as hernias.
Bowel disease
- Ulcerative colitis - diffuse inflammation. The mucous membrane of the rectum is affected. In the initial forms of ulcerative colitis, inflammation affects only the proximal section (entrance to the intestines), when neglected, the problems affect the entire colon. With the progression, exacerbation of the disease, the patient feels a sharp deterioration in well-being, he begins to become intoxicated, the pulse quickens, and blood appears in the feces in most cases. If the disease is not treated, then the body can poison itself, peritonitis can develop - a lesion of the abdominal cavity that poses a threat to life. nine0020
- Enteritis . The small intestine becomes inflamed. At first, the disease “masquerades” as a departure, and often is an accompaniment to this problem. If the disease is not treated in time, then the functions of the small intestine are disturbed. Food begins to be poorly absorbed by the intestinal walls.
 Digestion processes are disturbed.
Digestion processes are disturbed. - Crohn's disease . Both one and several sections of the intestine can become inflamed. But at the same time, almost always, the entire inflammation affects the junction of the large and small intestines. One of the most unpleasant moments is that inflammation affects the entire thickness of the wall, and a complication of the disease is intestinal obstruction syndrome, the treatment of which requires the adoption of a set of measures related to the simulation of motility and the restoration of bowel function. nine0020
- Dysbacteriosis – violation of the intestinal microflora. In the intestines, the number of beneficial bacteria is reduced, and pathogenic microflora develops. As a result, gas formation occurs, a person cannot digest food, and stool is disturbed. Very often, the development of dysbacteriosis is a consequence of incorrect antibiotic therapy or a reaction to stress.
Diseases of the pancreas
- Pancreatitis .
 The most common disease affecting the pancreas is pancreatitis. With inflammation of the pancreas, a person feels severe discomfort in the upper abdomen, it becomes difficult for the body to digest proteins and fats. Often in everyday life in this case they say: "Not enough enzymes." And it really reflects the real picture. In the affected pancreas, the production of lipase, chymotrypsin, and trypsin is significantly reduced. nine0020
The most common disease affecting the pancreas is pancreatitis. With inflammation of the pancreas, a person feels severe discomfort in the upper abdomen, it becomes difficult for the body to digest proteins and fats. Often in everyday life in this case they say: "Not enough enzymes." And it really reflects the real picture. In the affected pancreas, the production of lipase, chymotrypsin, and trypsin is significantly reduced. nine0020 - Cystic fibrosis is a disease that disrupts the functioning of the pancreas and respiratory organs. It is a non-inflammatory pathology. The reason is hereditary factors. A complication of the disease can be the formation of a duodenal ulcer.
Diseases of the stomach
One of the most common diseases that affect people of all ages, accompanied by pain in the abdomen is the pathology of the stomach, especially its mucous membrane. Leaders are gastritis, ulcers, gastroesophageal reflux disease. nine0005
- Gastritis .
 It is an inflammation of the gastric mucosa. The entire stomach or its individual sections can become inflamed. With gastritis, burning pains and spasms predominate. The patient is concerned about discomfort after eating, a feeling of a full stomach, or, on the contrary, "sucking" and a constant feeling of hunger. Companions of the disease in the acute stage - vomiting and nausea.
It is an inflammation of the gastric mucosa. The entire stomach or its individual sections can become inflamed. With gastritis, burning pains and spasms predominate. The patient is concerned about discomfort after eating, a feeling of a full stomach, or, on the contrary, "sucking" and a constant feeling of hunger. Companions of the disease in the acute stage - vomiting and nausea. - Gastric ulcer . Pain occurs against the background of characteristic ulcerative lesions of the gastric mucosa. Dyspeptic phenomena are expressed: heaviness in the stomach, a feeling of oversaturation of the stomach, cramps in the epigastric region. nine0020
- Gastroesophageal reflux disease (popularly known as “reflux”). The disease is associated with a weakening of the valve between the stomach and esophagus. The result of this weakening is pain, accompanied by heartburn. Very often, gastroesophageal reflux disease appears in patients who have already experienced gastritis or stomach ulcers.
Hernias
Abdominal pains are often caused by abdominal hernias. They can be umbilical, inguinal, diaphragmatic. Umbilical hernias are more often formed during pregnancy or in the postpartum period, inguinal hernias - with excessive loads, diaphragmatic hernias - abdominal wall defects that form as a reaction to improper bowel function, an incorrectly selected corset, weight lifting. The insidiousness of diaphragmatic hernias is that at the initial stage of the disease, a person believes that he has a typical gastritis - with heartburn and belching, but traditional therapy does not provide treatment, and ultrasound shows that the reason is not in inflammation of the stomach, but in the presence of a hernia. In toga, to combat pathology, it is not necessary to relieve inflammation, eliminate spasms, but surgical treatment, which is aimed at strengthening the abdominal wall. nine0005
Diseases of the gallbladder and bile ducts
Diseases associated with the gallbladder and bile duct constitute a special group.
- Cholangitis . Inflammation of the bile ducts. The pain is unbearable. Mostly on the right side. It is difficult because it requires not only the rapid removal of an attack of the pains themselves, but also the normalization of blood pressure.
- Cholecystitis . Acute pain on the background of fatty foods. Often, the pain itself is followed by vomiting with an admixture of bile. Flatulence (gas formation) and vomiting may disturb. nine0020
- Cholelithiasis – formation of solid structures in bile – stones. Pain during the disease is paroxysmal. Especially if the stones move along the gallbladder and ducts.
Contraindications
Incorrect diagnosis is fraught with the fact that the treatment will not only be useless, but will provoke serious complications. After all, many medicines, physiotherapeutic methods, effective in some diseases, accompanied by pain in the abdomen - are strict contraindications for other diseases with similar symptoms.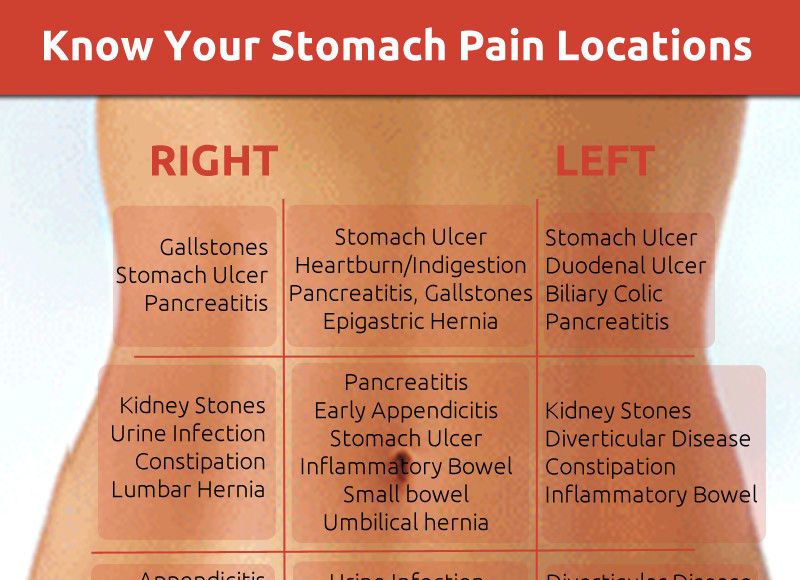
For example, if a number of drugs prescribed for pancreatitis are given to patients with hepatic colic, the response may be unpredictable. And the treatment of a number of diseases of the stomach with an antibiotic can cause serious dysbacteriosis.
And absolute contraindications in the event of pain in the abdomen, stomach is self-treatment - especially the independent decision to take an anesthetic or antispasmodic. If, for example, such drugs are used by a person whose appendix has become inflamed, then relief will follow for a while. But this will not be help, but false help to oneself. It is not uncommon for patients who did not get to the surgeon in time to remove appendicitis, necrosis of the tissues of neighboring organs began. nine0005
In no case, without making a diagnosis, one should not grab even seemingly “harmless” means to combat hyperacidity. What seems to be just a release of excess hydrochloric acid and inflammation of the stomach may be a symptom of a completely different disease, such as a heart attack.
Also, for pain in the abdomen with an unexplained diagnosis, do not apply a heating pad with hot water. In a number of pathologies, heat only accelerates the inflammatory process, activates bleeding. nine0005
Examinations
An effective examination of a patient who suffers from abdominal pain consists of a survey, palpation of the abdomen, laboratory and functional diagnostics.
Even the smallest details are important for the doctor to make a diagnosis. For example, even an elementary assessment of feces can clarify a lot in case of pain in the abdomen.
- Hard lumps ("sheep" feces) are a frequent companion of colitis, lengthening of the sigmoid colon, stomach ulcers.
- Watery stool often accompanies poisoning, infectious diseases. nine0020
- With a parasitic disease (the presence of worms in the intestines), dysbacteriosis, stool particles are usually very loose.
Oral questioning of the patient is also important for the choice of instrument, diagnostic technology. The doctor asks the patient how long the pain lasts, whether there are attacks, what exactly causes pain - physical movements, going to the toilet, eating, taking a certain position.
The doctor asks the patient how long the pain lasts, whether there are attacks, what exactly causes pain - physical movements, going to the toilet, eating, taking a certain position.
Diagnosis
The following examinations are especially valuable for identifying the cause of the disease and finding methods of treatment for pathologies of the abdominal cavity:
- Abdominal ultrasound . One of the most prompt measures in diagnosing diseases of the abdominal cavity and small pelvis, identifying the cause of abdominal pain is ultrasound diagnostics. With the help of ultrasound, pathologies of the liver, gallbladder, spleen, kidneys, uterus, and ovaries can be detected. Many people wonder: is the stomach and intestines visible on ultrasound. The stomach cannot be examined by ultrasound, the intestines - partially. If the equipment has a good resolution, for example, volumetric formations in this area are visible on it. nine0020
- FGDS (gastroscopy, probing, swallowing the “intestine”) is a diagnostic method that can be used to obtain an objective picture of the state of the stomach, duodenum, esophagus.
 If necessary, you can immediately conduct a rapid test for Helicobacter pylori (Helicobacter pylori) (which is the cause of the development of an ulcer), do cytology and biopsy - to exclude the oncological nature of the disease, determine the "acidity".
If necessary, you can immediately conduct a rapid test for Helicobacter pylori (Helicobacter pylori) (which is the cause of the development of an ulcer), do cytology and biopsy - to exclude the oncological nature of the disease, determine the "acidity". - X-ray. An old, but still practiced method of diagnosis. It can be used as an emergency measure for examining the stomach, if for some reason it is impossible to do an EGD. In addition, X-ray is informative in identifying diseases accompanied by symptoms of intestinal obstruction. Depending on the nature of the pain and complaints of the patient, a traditional X-ray or an X-ray with contrast enhancement (irrigoscopy) can be used. nine0020
- MRI is a progressive diagnostic method for abdominal injuries, liver enlargement, and an uninformative picture of the abdominal cavity during ultrasound (for example, due to severe flatulence).
- Colonoscopy. One of the most accurate methods for examining the intestines.
 It is carried out using a fibrocolonoscope. With the help of the device, you can explore everything - even the most difficult areas, including the inner surface of the colon.
It is carried out using a fibrocolonoscope. With the help of the device, you can explore everything - even the most difficult areas, including the inner surface of the colon. - Cholescintigraphy . Isotopic research. It is carried out using a radio pharmacological preparation. Informative for problems with the gallbladder and bile ducts. nine0020
- Blood, urine and canal testing . In the analysis of blood, special emphasis is placed on ESR (inflammation can be determined by the erythrocyte sedimentation rate), biochemical parameters, and stool, with many types of examinations for abdominal pain, is examined for occult blood.
What to do?
So, the main thing in case of pain in the abdomen is not to self-medicate, not to delay the visit to the doctor and diagnosis.
At the same time, in some cases, it is important not just to sign up for a clinic, but to immediately call an ambulance. In what cases is an ambulance required? nine0005
- Pain in the abdomen is very intense.
- Cold sweat breaks out.
- Severe vomiting with blood begins.
If the pain is not acute, there is no blood in the vomit, the temperature differs from the temperature of a healthy person, but there is no fever, consultation with a general practitioner, gastroenterologist and diagnostics is recommended.
Timely diagnosis is a guarantee that the most gentle methods will be used to combat the disease. Even when it comes to surgery. nine0005
- Laparoscopy is used to remove gallstones and appendicitis (if the situation is not advanced).
- Laparoscopic funduplication is used to treat astroesophageal reflux disease.
- Surgical hernioplasty is used to effectively solve hernia problems and strengthen the abdominal wall.
If there are no indications for surgical treatment, the therapeutic effect in many diseases of the intestines and stomach provides an integrated approach based on diet therapy, physiotherapy and drug therapy - antibiotics, antiparasitics, corticosteroids, prokinetics to improve intestinal motility.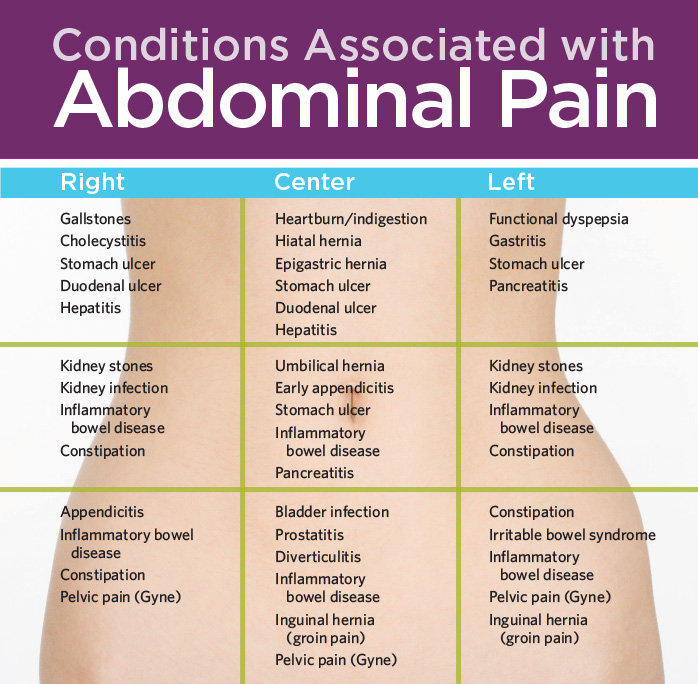 nine0005
nine0005
Where to contact?
Vast experience in laparoscopic surgery, hernioplasty in Minsk - the doctors of the 5th Clinical Hospital.
In addition to accepting patients who are citizens of Belarus, the 5th City Hospital of Minsk also accepts foreign citizens (for a fee). Each of them can undergo complex diagnostics and treatment on the basis of the surgical, therapeutic department.
The hospital has its own clinical diagnostic laboratory, X-ray department, CT and MRI rooms. The physiotherapy department has all conditions for rehabilitation programs. nine0005
Prevention
Doctors of the 5th Hospital will not only select the best option for diagnosis and treatment for each patient, but also advise on preventing relapses.
Diet occupies a special place among measures for the prevention of diseases of the intestines and stomach. In nutrition, it is important to learn how to maintain a balance. You can not overeat, chew food should be carefully and slowly.