Clotrimazole cream while pregnant
Clotrimazole topical Use During Pregnancy
Print SaveMedically reviewed by Drugs.com. Last updated on Feb 28, 2023.
Clotrimazole topical is also known as: Abtrim, Abtrim Pessaries, Canesten, Canesten 1, Canesten 3, Canesten 6 Day Pessary, Clotrimazole-3, Clotrimazole-7, Desenex Antifungal Cream, Femcare, FungiCURE Pump Spray, Gyne-Lotrimin, Gyne-Lotrimin 3 Day, Gyne-Lotrimin Inserts, Lotrimin AF Athlete's Foot Cream, Lotrimin AF For Her Athlete's Foot Cream, Lotrimin AF Jock Itch Cream, Lotrimin AF Ringworm Cream, Mycelex, Mycelex OTC, Trivagizole 3
Clotrimazole topical Pregnancy Warnings
Clotrimazole topical has been assigned to pregnancy category B by the FDA. Systemic absorption is minimal following topical or vaginal administration. Animals given high doses intravaginally have not revealed evidence of teratogenicity. High oral doses resulted in embryotoxicity and maternal toxicity. In clinical trials involving women in their second and third trimester, clotrimazole treatment of vaginal candidiasis was not associated with fetal harm. Clotrimazole use has not been well studied during the first trimester. Clotrimazole should only be used during the first trimester when need has been clearly established.
See references
Clotrimazole topical Breastfeeding Warnings
There are no data on the excretion of clotrimazole into human milk. However, systemic absorption is minimal after topical and vaginal administration. The manufacturer recommends that caution be used when administering clotrimazole topical to nursing women.
See references
See also
- Clotrimazole use while Breastfeeding (in more detail)
- clotrimazole topical Consumer Information
- Pregnancy Support Group
- FDA Pregnancy Categories
- Medicine use during Pregnancy
- Medicine use while Breastfeeding
- Safe Medications during Breastfeeding
References for pregnancy information
- Haram K, Digranes A "Vulvovaginal candidiasis in pregnancy treated with clotrimazole.
 " Acta Obstet Gynecol Scand 57 (1978): 453-5
" Acta Obstet Gynecol Scand 57 (1978): 453-5 - Tan CG, Good CS, Milne LJ, Loudon JD "A comparative trial of six day therapy with clotrimazole and nystatin in pregnant patients with vaginal candidiasis." Postgrad Med J 50 Suppl 1 (1974): 102-5
- Lindeque BG, van Niekerk WA "Treatment of vaginal candidiasis in pregnancy with a single clotrimazole 500 mg vaginal pessary." S Afr Med J 65 (1984): 123-4
- Frerich W, Gad A "The frequency of Candida infections in pregnancy and their treatment with clotrimazole." Curr Med Res Opin 4 (1977): 640-4
- "Product Information. Mycelex (clotrimazole)." Bayer (2001):
- "Product Information. Lotrimin (clotrimazole topical)." Schering-Plough Corporation (2003):
References for breastfeeding information
- "Product Information. Lotrimin (clotrimazole topical)." Schering-Plough Corporation (2003):
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Medical Disclaimer
Is Antifungal Medication Safe During Pregnancy?
Pregnancy
Is it ok to take an antifungal while pregnant or breastfeeding?
Megha Trivedi, MD
AUTHOR
Jenny Murase, MD
EDITOR
Is it ok to take an antifungal while pregnant or breastfeeding?
From nail infections to itchy scalp to yeast infections, skin fungal infections are very common in the general population. Unfortunately, pregnancy is not immune to these conditions and many women who face skin fungus in pregnancy require treatment. However, not all antifungals are safe to use during pregnancy. Many antifungals are available over the counter and the safety of antifungal medications during pregnancy applied directly to the skin (topical) and those taken in oral form (systemic) will be reviewed.
It is worthwhile to note that fungi that infect humans come in two major forms: candida (yeast) and tinea (dermatophytes/mold). Candida or yeast often grow in moist environments such as the folds of the skin, oral cavity, and vaginal and anal areas. Infection with Candida is usually red and itchy. Tinea infections include a group of mold/dermatophyte infections, which include Trichophyton, Epidermophyton, and Microsporum species. These infections can take place anywhere on the skin including the nails and hair. The symptoms vary by type of infection but often times the skin can get discolored and appear white, brown, tan, or pink. Medication used to treat fungal infections is often different for these two classes of critters.[1]
Candida or yeast often grow in moist environments such as the folds of the skin, oral cavity, and vaginal and anal areas. Infection with Candida is usually red and itchy. Tinea infections include a group of mold/dermatophyte infections, which include Trichophyton, Epidermophyton, and Microsporum species. These infections can take place anywhere on the skin including the nails and hair. The symptoms vary by type of infection but often times the skin can get discolored and appear white, brown, tan, or pink. Medication used to treat fungal infections is often different for these two classes of critters.[1]
Topical Antifungals: Safe Medications in Pregnancy
Topical antifungals include nystatin, clotrimazole, miconazole, terbinafine, ciclopirox, and selenium sulfide. Table 1 briefly summarizes the information we will discuss.
The topical form of nystatin is often used to treat superficial fungal infections, most commonly known as candida. This medication is rarely used in oral form because it does not absorb well into the bloodstream when taken orally.[2] It is categorized as pregnancy category A when used as an intravaginal tablet for fungal infections in that area, such as vulvovaginal yeast infections. Its topical form (ointment, powder, cream) has been labeled pregnancy category C, simply because there are no good human or animal studies verifying its safety in pregnancy. However, there are no reports in the literature about negative effects to the fetus when used in pregnancy. It has a lactation category of L1 and is safe to use while breastfeeding.[3]
This medication is rarely used in oral form because it does not absorb well into the bloodstream when taken orally.[2] It is categorized as pregnancy category A when used as an intravaginal tablet for fungal infections in that area, such as vulvovaginal yeast infections. Its topical form (ointment, powder, cream) has been labeled pregnancy category C, simply because there are no good human or animal studies verifying its safety in pregnancy. However, there are no reports in the literature about negative effects to the fetus when used in pregnancy. It has a lactation category of L1 and is safe to use while breastfeeding.[3]
Clotrimazole is another antifungal commonly used to treat vulvovaginal yeast infection. It has been commonly used to treat these infections in pregnancy and is considered generally safe. A single case was published about its potential association with spontaneous abortion in a patient. However, it was never confirmed to be the cause and there have been no reports since then of negative effects on the fetus when used in pregnant women. [4] In 1999, a large study with more than 18,000 patients concluded that clotrimazole use during pregnancy does not significantly correlate with abnormalities in the fetus.[5] It is pregnancy category B and lactation category L1 and safe to use while breastfeeding.[3] Some clinicians prefer to use this first to treat vulvovaginal yeast infection before trying nystatin in pregnant women.[4] A related topical agent, miconazole, has also been used safely in many pregnancies and there have been no birth defects in babies reported. It is labeled as pregnancy category C. It has an L2 lactation rating and is most likely safe to use during breastfeeding.[6]
[4] In 1999, a large study with more than 18,000 patients concluded that clotrimazole use during pregnancy does not significantly correlate with abnormalities in the fetus.[5] It is pregnancy category B and lactation category L1 and safe to use while breastfeeding.[3] Some clinicians prefer to use this first to treat vulvovaginal yeast infection before trying nystatin in pregnant women.[4] A related topical agent, miconazole, has also been used safely in many pregnancies and there have been no birth defects in babies reported. It is labeled as pregnancy category C. It has an L2 lactation rating and is most likely safe to use during breastfeeding.[6]
Topical terbinafine is often used to treat athlete’s foot, jock itch, ringworm, and a variety of other fungal infections. It is assigned pregnancy category B as animal studies with the use of this agent have not demonstrated any adverse effects to the fetus. Also, topical terbinafine is not greatly absorbed through the skin. It is generally regarded as safe to prescribe during pregnancy.[3,4] It has a lactation category L2 and is not thought to affect breastfeeding.[4]
It is generally regarded as safe to prescribe during pregnancy.[3,4] It has a lactation category L2 and is not thought to affect breastfeeding.[4]
Ciclopirox is a medication used to treat many of the above-listed conditions. It is usually only used topically and is pregnancy category B. In animal studies, this medication has not been shown to harm the growing fetus when administered either topically or orally to rats, mice, monkeys, and rabbits. Therefore, it can be used topically safely during pregnancy but is not often chosen as a first-line agent. Its effects on breastfeeding are less well known, and it is labeled L3. It should not be chosen as the first-line medication for breastfeeding moms as there are other medications (such as the ones listed above) with more safety data/reports available.[3]
Selenium sulfide is commonly found in shampoos and is used to treat conditions like seborrheic dermatitis (itchy, flaky scalp, aka. dandruff). We would like to focus on this agent since it is so common in over the counter products. It is important to note that it has been labeled pregnancy category C. There have been no animal or human studies conducted to assess the safety of this agent in pregnant women. The current recommendations state that it is safe to use in very local areas for limited amounts of time.[3] It has a lactation rating of L3. It is generally considered safe to use during lactation, but there is one reported case of breast milk production suppression in a woman using selenium disulfide to treat a condition called tinea versicolor, but this is the only known reported case of such an effect.[7]
dandruff). We would like to focus on this agent since it is so common in over the counter products. It is important to note that it has been labeled pregnancy category C. There have been no animal or human studies conducted to assess the safety of this agent in pregnant women. The current recommendations state that it is safe to use in very local areas for limited amounts of time.[3] It has a lactation rating of L3. It is generally considered safe to use during lactation, but there is one reported case of breast milk production suppression in a woman using selenium disulfide to treat a condition called tinea versicolor, but this is the only known reported case of such an effect.[7]
Table 1.Topical Antifungals and Pregnancy and Lactation Categories
|
Topical Antifungal |
Pregnancy Category |
Lactation Category |
|
Nystatin |
A (vaginal)- safe to use B (topical)- safe to use |
L1- safe to use |
|
Clotrimazole |
B- safe to use |
L1- safe to use |
|
Miconazole |
C-Physicians generally consider safe to use |
L2- Most likely safe during breastfeeding |
|
Terbinafine |
B- safe to use |
L2- generally safe to use |
|
Ciclopirox |
B- safe to use, but not first-line, try something else first. |
L3- Avoid if possible, very little data. |
|
Selenium Sulfide |
C- use in local areas for short time |
L3- One report of milk production suppression, therefore, L3 rating, but physicians believe it is most likely safe during breastfeeding. |
Oral Antifungals: Safe Medications in Pregnancy
Five commonly used oral antifungal agents include griseofulvin, terbinafine, and three antifungals in the “azole” category including fluconazole, ketoconazole, and itraconazole. Table 2 provides a summary of the safety categories and general recommendations.
Griseofulvin is an oral antifungal used to treat fungal infections, such as ringworm of the scalp known as tinea capitis. It is categorized as pregnancy category C and is generally not recommended during pregnancy due to very limited data. There was one reported case of conjoined twins with the use of this agent as well.[8] It has a lactation category of L2, but due to minimal data, most clinicians recommend avoiding the agent while breastfeeding. [3]
There was one reported case of conjoined twins with the use of this agent as well.[8] It has a lactation category of L2, but due to minimal data, most clinicians recommend avoiding the agent while breastfeeding. [3]
The “azole” class of antifungals are used to treat mold and yeast infections, including oral or vulvovaginal yeast infections.[9] However, these are all pregnancy category C, and human studies and reports have demonstrated a risk to the fetus. Specifically, exposure to these agents in the first trimester can result in neurologic, cardiac, bone, and facial defects in the baby. These should be avoided during pregnancy. All of these agents are lactation category L2. Fluconazole has the most data on lactation and is likely safe to use while breastfeeding. Itraconazole has been shown to reach high concentrations in breast milk and may be best to avoid while breastfeeding. There is very limited data on lactation and ketoconazole—experts say that it is likely safe, but more data is needed to confirm this. [3]
[3]
Oral terbinafine is often used to treat fungal infections of the finger and toenails, and sometimes fungal infections of the scalp in older children and adults. It does not treat yeast infections such as vaginal or oral candida. Although there have not been any published reports of harmful effects to the fetus in pregnant women who have taken this medication, there is very limited data on its pregnancy safety. It is currently labeled pregnancy category B. Since the medication is used to treat non-life threatening conditions (nail and scalp fungal infections), it is recommended that oral terbinafine be avoided during pregnancy. It has a lactation category of L2. For breastfeeding mothers, the current recommendation states that oral terbinafine should only be used for short time periods.[3]
Table 2. Oral (Systemic) Antifungals and Pregnancy and Lactation Categories
|
Oral Antifungal |
Pregnancy Category |
Lactation Category |
|
Griseofulvin |
C- limited data, do not use in pregnant women if it can be avoided |
L2- but limited data, so again, avoid if possible |
|
Fluconazole |
C- avoid in pregnancy, birth defects reported |
L2- most data out of all the “azole” drugs, likely safe to use |
|
Ketoconazole |
C- avoid in pregnancy, birth defects reported |
L2-likely safe, but limited data, more data needed to confirm safety |
|
Itraconazole |
C- avoid in pregnancy, birth defects reported |
L2- reaches high concentrations in breast milk, avoid and try other drugs first |
|
Terbinafine |
B - wait to treat with this medication after pregnancy |
L2- use only for short period of time |
For any drugs discussed here, please consult the drug package insert for complete prescribing information and for complete information regarding side effects.
* This Website is for general skin beauty, wellness, and health information only. This Website is not to be used as a substitute for medical advice, diagnosis or treatment of any health condition or problem. The information provided on this Website should never be used to disregard, delay, or refuse treatment or advice from a physician or a qualified health provider.
References
- Habif TP. Clinical dermatology. (2015). Elsevier Health Sciences.
- Pilmis B, Jullien V, Sobel J, et al. Antifungal drugs during pregnancy: an updated review. J Antimicrob Chemother.2015;70(1):14-22; PMID: 25204341 Link to Research
- Murase JE, Heller MM, Butler DC. Safety of dermatologic medications in pregnancy and lactation: Part I. Pregnancy. J Am Acad Dermatol.2014;70(3):401 e401-414; quiz 415; PMID: 24528911 Link to Research
- Mullegger RR, Haring NS, Glatz M. Skin infections in pregnancy. Clin Dermatol.2016;34(3):368-377; PMID: 27265075 Link to Research
- Czeizel AE, Toth M, Rockenbauer M.
 No teratogenic effect after clotrimazole therapy during pregnancy. 1999;10(4):437-440; PMID: 10401880 Link to Research
No teratogenic effect after clotrimazole therapy during pregnancy. 1999;10(4):437-440; PMID: 10401880 Link to Research - Hale EK, Pomeranz MK. Dermatologic agents during pregnancy and lactation: an update and clinical review. Int J Dermatol.2002;41(4):197-203; PMID: 12031026 Link to Research
- Sugathan P, Riyaz N. Suppression of lactation by selenium disulfide. Int J Dermatol.1990;29(3):232-233; PMID: 2335423 Link to Research
- Rosa FW, Hernandez C, Carlo WA. Griseofulvin teratology, including two thoracopagus conjoined twins. 1987;1(8525):171; PMID: 2880014 Link to Research
- Cottreau JM, Barr VO. A Review of Antiviral and Antifungal Use and Safety during Pregnancy. 2016;36(6):668-678; PMID: 27139037 Link to Research
Share
DISCUSSIONSsmart choice » Obstetrics and Gynecology
Pharmacotherapy during pregnancy is not an easy task, in which the assessment of the expected benefits and risks to the mother and fetus is of particular importance. Meanwhile, there are a number of diseases, the likelihood of which during this period is especially high. One of them is vulvovaginal candidiasis (CVV).
Meanwhile, there are a number of diseases, the likelihood of which during this period is especially high. One of them is vulvovaginal candidiasis (CVV).
Facts and figures
Pregnancy rates are much higher in pregnant women than in non-pregnant women. It can reach 60.8%. The frequency of detection increases with increasing gestational age. Some authors point to a particularly high prevalence of CVC in the III trimester compared to the II and I trimesters - 90, 38 and 25% respectively 1 .
Such a high incidence of CVV during pregnancy is due, firstly, to a change in hormonal balance - an increase in the level of a number of hormones, against which the adhesive properties of vaginal epitheliocytes increase, cell proliferation and glycogen content increase in them. When it is broken down, glucose is formed - an excellent nutrient medium for fungi 2 .
An equally important factor is the functional decrease in immunity. During pregnancy, the cytokine balance shifts towards some immunosuppression to prevent rejection of the semi-foreign fetus 3 .
Meanwhile, ECV poses a risk to mother and fetus. For example, it increases the risk of abortion, premature birth, fetal hypoxia, wound infection of the birth canal, postpartum endometritis, and intrauterine and postnatal infection of newborns 2 .
Difficult task…
It is obvious that close attention should be paid to the treatment of CVC during pregnancy. But the possibilities of pharmacotherapy during this period are limited. Currently, a large amount of data has been accumulated on the negative effects of certain drugs on the fetus. Thus, pharmacotherapy in the first trimester is associated with a high risk of affecting the fetus during the laying of the neural tube, organs and systems. Treatment in the II and III trimesters can be complicated by various disorders in the functioning of the organs of the fetus, as well as the mental and physical status of the newborn 4 .
Drugs for the treatment of CVC during pregnancy must meet two important criteria: have a high safety profile in terms of effects on the fetus, as well as provide relief of symptoms of the disease and sanitation of the vagina from fungi 1 .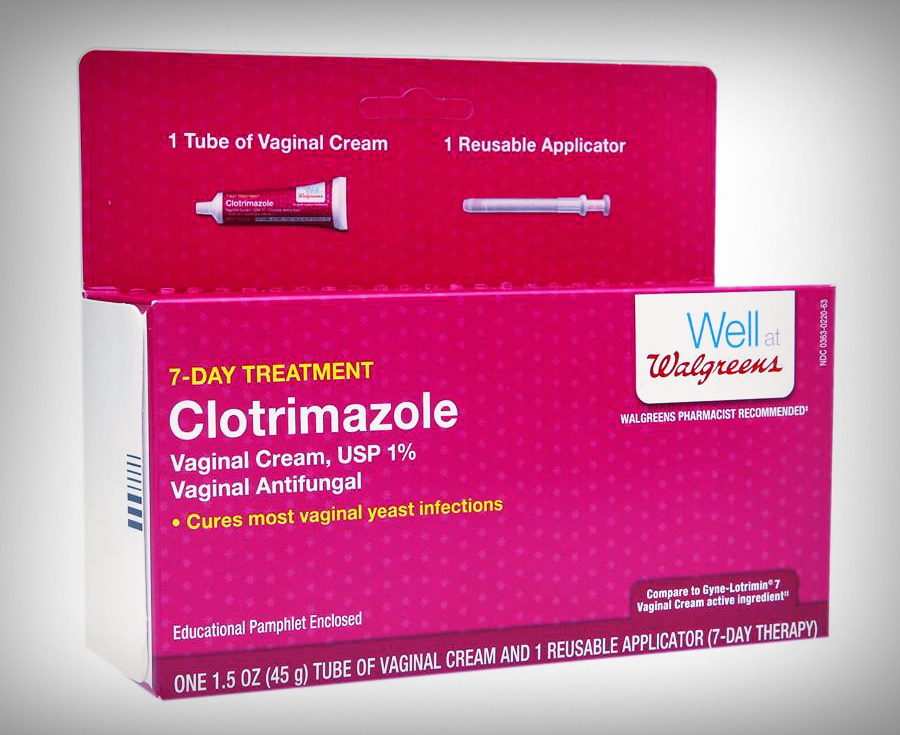
- Vaginal cream Clotrimazole 2% can be used in the second and third trimesters of pregnancy for the treatment of genital infections caused by yeast-like fungi of the genus Candida 5 .
- During pregnancy, the use of the vaginal applicator is not recommended 5 .
- The decision on the appropriateness of the use is made by the doctor.
…and possible solution
In this regard, the possibilities of intravaginal therapy are of particular interest. In the II and III trimesters of pregnancy, the vaginal cream Clotrimazole 2% may become the drug of choice for the treatment of VVC. The OTC drug has a wide spectrum of activity in dermatophytes, yeast-like and mold fungi, as well as gram-positive bacteria (Streptococcus spp., Staphylococcus spp.), anaerobes (Bacteroides spp., Gardnerella vaginalis) and protozoa (T. vaginalis) 1.5 . This makes it possible to use the drug for the treatment of infections of mixed etiology. However, the cream does not inhibit the growth of lactobacilli 1.5 .
However, the cream does not inhibit the growth of lactobacilli 1.5 .
WHO added clotrimazole to the list of essential medicines for the treatment of fungal infections, revised in 2017 1 . The list of contraindications for the use of 2% clotrimazole cream is minimal: it includes the first trimester of pregnancy, hypersensitivity to the components of the drug 5 .
__________
1 Bebneva T.N., Dicke G.B. Modern features of vulvovaginal candidiasis and the choice of rational therapy outside and during pregnancy // BC. Mother and child. 2018. V. 1. No. 1. S. 49–56.
2 Peresada O.A., Kirdik V.E., Grinets L.V., Korsak E.N., Bugrov V.Yu. Vulvovaginal candidiasis during pregnancy // Medical News. 2004. No. 6. pp. 91-93.
3 Allan S.E. et al. // Immunol Rev. 2008. No. 223. P. 391–421.
4 Medicines. Adverse side effects and safety control // Safety of drugs and pharmacovigilance. 2009. No. 2, pp. 3–22.
5 Instruction LP-004092 dated 01/23/2017
| 📜 Instructions for use Clotrimazole 💊 Ingredients of the drug Clotrimazole ✅ Use of the drug Clotrimazole 📅 Storage conditions Clotrimazole ⏳ Expiration date Clotrimazole Search for analogues Product description clotrimazole (Clotrimazole) Based on the official label for the drug, approved by the manufacturer and prepared for the electronic edition of the Vidal Handbook 2014 year, update date: 2018.12.24 Marketing authorization holder:GlaxoSmithKline Trading JSC (Russia)
Manufactured:GlaxoSmithKline Pharmaceuticals, S.  A. (Poland) A. (Poland)
Contacts for inquiries:GlaxoSmithKline Trading JSC (Russia) ATX code: G01AF02 (Clotrimazole) Active substance: clotrimazole (clotrimazole) Rec.INN registered by WHO Dosage form
Release form, packaging and composition drug ClotrimazoleVaginal tablets white, oblong, biconvex, smooth surface, rounded at one end and flat at the other. Excipients : lactose monohydrate - 1122.2 mg, potato starch - 180 mg, adipic acid - 140 mg, sodium bicarbonate - 110 mg, magnesium stearate - 31.3 mg, colloidal silicon dioxide - 12.3 mg, sodium lauryl sulfate - 4.2 mg. 6 pcs. - blisters (1) - packs of cardboard. Clinical and pharmacological group: Drug with antifungal action for local use in gynecology Pharmacotherapeutic group: Antifungal agent Pharmacological action Clotrimazole inhibits the growth and division of microorganisms and, depending on the concentration, may have a fungistatic or fungicidal effect. Clotrimazole has a broad spectrum of antifungal and antibacterial activity . It is active against: dermatophytes (Epidermophyton floccosum, Microsporum canis, Trichophyton mentagrophytes, Trichophyton rubrum), yeasts (Candida spp. Clotrimazole is also active against certain Gram-positive bacteria. In vitro, clotrimazole has a broad spectrum of fungistatic and fungicidal activity. It affects the mycelium of dermatophytes (Trichophyton, Microsporum, Epidermophyton) similarly to griseofulvin, its effect on budding yeast-like fungi (Candida) is similar to that of polyenes (amphotericin B and nystatin). At concentrations less than 1 μg / ml, clotrimazole inhibits the development of most strains of pathogenic fungi related to Trichophyton rubrum, Trichophyton mentagrophytes, Epidermophyton floccosum, Microsporum canis. At a concentration of 3 μg / ml, clotrimazole inhibits the development of most other bacteria: Pityrosporum orbiculare, Aspergillus fumigatus, Candida genus, incl. Candida albicans, some strains of Staphylococcus aureus, Streptococcus pyogenes, and some strains of Proteus vulgaris and Salmonella. At concentrations greater than 100 µg/ml it is effective against Trichomonas vaginalis. Clotrimazole-resistant fungi are extremely rare; there are data only for individual strains of Candida guilliermondii. No resistance has been reported in clotrimazole-sensitive fungi after passage of Candida albicans and Trichophyton mentagrophytes. No cases of development of resistance to clotrimazole in strains of Candida albicans resistant to polyene antibiotics due to a chemical mutation have been described. PharmacokineticsAbsorption and distribution Pharmacokinetic studies of clotrimazole with intravaginal use have shown that absorption is 3-10% of the administered dose. In the liver, clotrimazole is metabolized to pharmacologically inactive metabolites; therefore, its plasma concentration when intravaginally administered at a dosage of 500 mg is less than 10 ng / ml, confirming the fact that clotrimazole when administered intravaginally does not lead to significant systemic effects or side effects. Metabolism Clotrimazole is primarily metabolized in the liver to metabolites excreted via the kidneys and intestines. Indications of the drug clotrimazole
Open list of ICD-10 codes
Dosing regimen For intravaginal use. If there is no effect within 3 days, confirm the diagnosis. If symptoms persist for more than 7 days, follow up with a physician. Treatment may be repeated if necessary, but recurrent infections may be indicative of an underlying pathology, including diabetes mellitus or HIV infection. If symptoms recur within 2 months, the patient should consult a doctor. In case of simultaneous infection of the vulva and adjacent areas, external treatment with a cream is necessary. For complete dissolution of vaginal tablets, normal moisture of the vaginal mucosa is required. In women with dryness of the vaginal mucosa, undissolved parts of the tablet may be excreted. To prevent this, it is necessary to inject the tablet as deep as possible into the vagina before going to bed. Treatment during menstruation is not recommended due to the risk of pill washout and must be completed before menstruation. For sanitation of the birth canal once 1 tablet immediately before childbirth. For children over 12 years of age, is the same way as for adults. Clotrimazole vaginal tablets are not recommended for use in children under 12 years of age . Repeat therapy is possible according to medical indications. Side effectsThe adverse events listed below are listed according to the damage to organs and organ systems and the frequency of occurrence. The frequency of occurrence is defined as follows: very often (≥1/10), often (≥1/100 and <1/10), infrequently (≥1/1000 and <1/100), rare (≥1/10,000 and < 1/1000), very rare (<1/10000, including isolated cases), not known (frequency cannot be estimated from currently available data). Frequency categories were formed on the basis of post-registration observation. From the immune system: unknown - allergic reactions (urticaria, fainting, arterial hypotension, shortness of breath). From the gastrointestinal tract: unknown - abdominal pain. From the genital organs and breast: unknown - discomfort in the vulva and vagina, hyperemia and swelling of the vaginal mucosa, vaginal discharge, burning, peeling, irritation, itching, pain in the pelvic area, burning sensation in the genitals member of a sexual partner, pain during intercourse, rash. If these symptoms appear, clotrimazole therapy should be discontinued. From the side of the nervous system: unknown - headache. From the side of the kidneys and urinary tract: unknown - frequent urination, intercurrent cystitis. Contraindications for use
Caution For the first case of candidal vaginitis, a doctor should be consulted. If any of the following factors are identified, a doctor should be consulted before prescribing Clotrimazole vaginal tablets:
Use in pregnancy and lactationUse of clotrimazole during pregnancy is allowed only if the expected benefit to the mother outweighs the potential risk to the fetus. In the conducted epidemiological studies, including a retrospective analysis, the use of clotrimazole during pregnancy (even in the first trimester) did not reveal any undesirable effects on the body of the pregnant woman, as well as congenital defects and undesirable effects in the fetus. The use of clotrimazole in women during breastfeeding is allowed only if the expected benefit to the mother outweighs the potential risk to the child. Fertility No data available. Special instructionsAvoid contact with eyes and ingestion. It is recommended that all affected areas of the body be treated simultaneously. Clotrimazole vaginal tablets should not be used if any of the following symptoms are present, unless otherwise directed by a physician:
Simultaneous treatment of sexual partners is necessary to prevent reinfection. Effect on the ability to drive vehicles and mechanisms Not studied. OverdoseSymptoms: dizziness, nausea, vomiting. Treatment: in case of accidental ingestion, symptomatic treatment should be carried out. Drug interactionsLaboratory data suggest that the use of contraceptives containing latex may cause damage when used together with Clotrimazole. Therefore, the effectiveness of such contraceptives may decrease. Patients should be advised to use alternative methods of contraception for at least five days after using Clotrimazole. Concomitant use of vaginal clotrimazole and oral tacrolimus (FK-506; immunosuppressant) may result in increased plasma concentrations of tacrolimus. Patients should be closely monitored for symptoms of tacrolimus overdose, with drug levels measured if necessary. Amphotericin B, nystatin, natamycin reduce the effectiveness of clotrimazole when used simultaneously. |

 vaginal 100 mg: 6 pcs. (7003)
vaginal 100 mg: 6 pcs. (7003)  02.17
02.17  The mechanism of action of clotrimazole is associated with a change in the permeability of cell membranes due to the effect on the synthesis of ergosterol and binding to fungal cell wall phospholipids. Clotrimazole inhibits the synthesis of proteins, fats, DNA, polysaccharides, damages nucleic acids in fungal cells and accelerates the excretion of potassium. It can also inhibit the activity of oxidant and peroxidant enzymes and the biosynthesis of triglycerides and phospholipids in fungal cells. At higher concentrations, clotrimazole causes damage to cell membranes by mechanisms independent of sterol synthesis. Clotrimazole prevents the transformation of Candida albicans blastospores into invasive forms of mycelium. A change in the activity of the cell membrane leads to cell death, and this process depends on the contact of the drug with microbes.
The mechanism of action of clotrimazole is associated with a change in the permeability of cell membranes due to the effect on the synthesis of ergosterol and binding to fungal cell wall phospholipids. Clotrimazole inhibits the synthesis of proteins, fats, DNA, polysaccharides, damages nucleic acids in fungal cells and accelerates the excretion of potassium. It can also inhibit the activity of oxidant and peroxidant enzymes and the biosynthesis of triglycerides and phospholipids in fungal cells. At higher concentrations, clotrimazole causes damage to cell membranes by mechanisms independent of sterol synthesis. Clotrimazole prevents the transformation of Candida albicans blastospores into invasive forms of mycelium. A change in the activity of the cell membrane leads to cell death, and this process depends on the contact of the drug with microbes.  , Cryptococcus neoformans), dimorphic fungi (Coccidioides immitis, Histoplasma capsulatum, Paracoccidioides brasiliensis), protozoa (Trichomonas vaginalis).
, Cryptococcus neoformans), dimorphic fungi (Coccidioides immitis, Histoplasma capsulatum, Paracoccidioides brasiliensis), protozoa (Trichomonas vaginalis).  Clotrimazole is active against Sporothrix, Cryptococcus, Cephalosporium, Fusarium.
Clotrimazole is active against Sporothrix, Cryptococcus, Cephalosporium, Fusarium.  .
.  Assign 1 tab. 2 times / day for 3 days or 1 tab. 1 time / day for 6-7 days, preferably at bedtime.
Assign 1 tab. 2 times / day for 3 days or 1 tab. 1 time / day for 6-7 days, preferably at bedtime.