Chlamydia in early pregnancy
Chlamydia and pregnancy | Pregnancy Birth and Baby
Chlamydia and pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Chlamydia is a bacterial sexually transmitted infection (STI) that affects both men and women. Chlamydia can also cause a number of issues during pregnancy.
Most people with chlamydia are unaware that they have the infection. Left untreated, chlamydia can cause serious complications including infertility and chronic pain. Chlamydia is fairly easy to treat if you know you have it — one course of antibiotics is usually enough.
Causes of chlamydia
Chlamydia is caused by an infection with the bacterium Chlamydia trachomatis. It is spread by unprotected (unsafe) vaginal or anal sex with an infected person.
Chlamydia is the most commonly reported STI in Australia.
What are the symptoms of chlamydia?
Most men and women with chlamydia have no signs or symptoms, which makes it very easy to spread. Some people have the infection for many months or years without knowing it.
Women who get symptoms may have:
- vaginal discharge
- bleeding between periods or after sex
- burning or pain when urinating
- abdominal or pelvic pain
- pain during sex
Men who get symptoms may have some clear discharge from the penis or pain during urination.
In rare cases, people with chlamydia have sore joints (arthritis) or inflammation of the eye (uveitis).
Diagnosing chlamydia
Chlamydia is easily diagnosed. Your doctor may take a sample from the vagina, cervix, anus or penis, and may ask for a urine test. These are sent to a laboratory for testing.
If you think you or your partner have chlamydia, see your doctor or sexual health clinic so you can both be tested.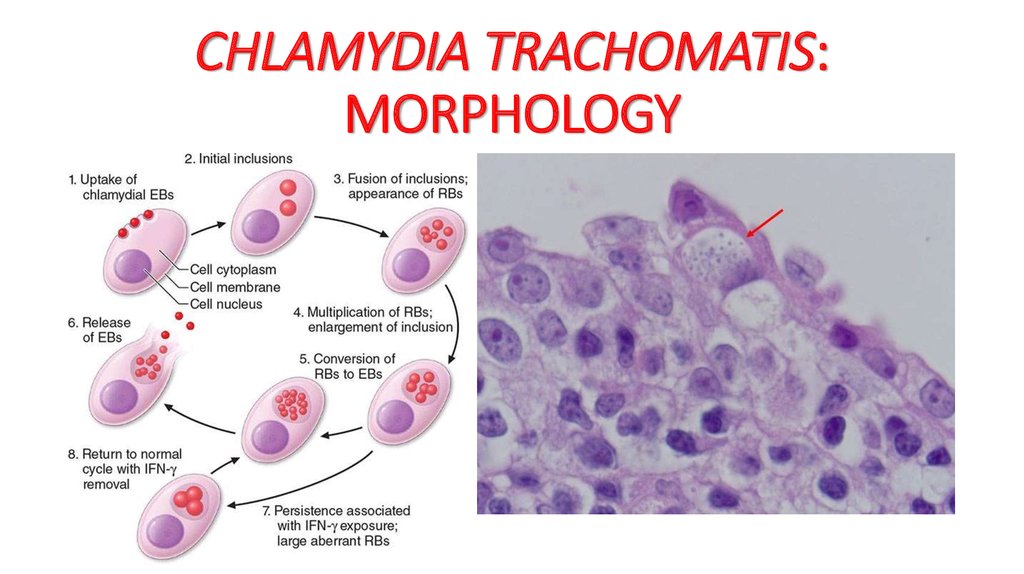 It is important that any sexual partners of people with chlamydia are tested, even if they don’t have symptoms.
It is important that any sexual partners of people with chlamydia are tested, even if they don’t have symptoms.
Treating chlamydia
Treatment for chlamydia is a course of antibiotics. It is important to avoid sex until the full course of treatment is finished, and for at least a week following. You should have another test 3 months after you are treated.
If you have chlamydia, all of your sexual partners should be informed, tested and treated, as they may be infected and can infect you, and others, again after treatment.
If your partner has had a positive test for chlamydia, you should be treated even if you have had a negative test result. As chlamydia infection increases the possibility of contracting other infections, it is important to be tested for other STIs such as gonorrhoea, hepatitis, HIV and syphilis. Using latex condoms and a water-based lubricant is the most effective way to prevent STIs. People who have chlamydia for long periods without treatment risk becoming infertile or developing arthritis.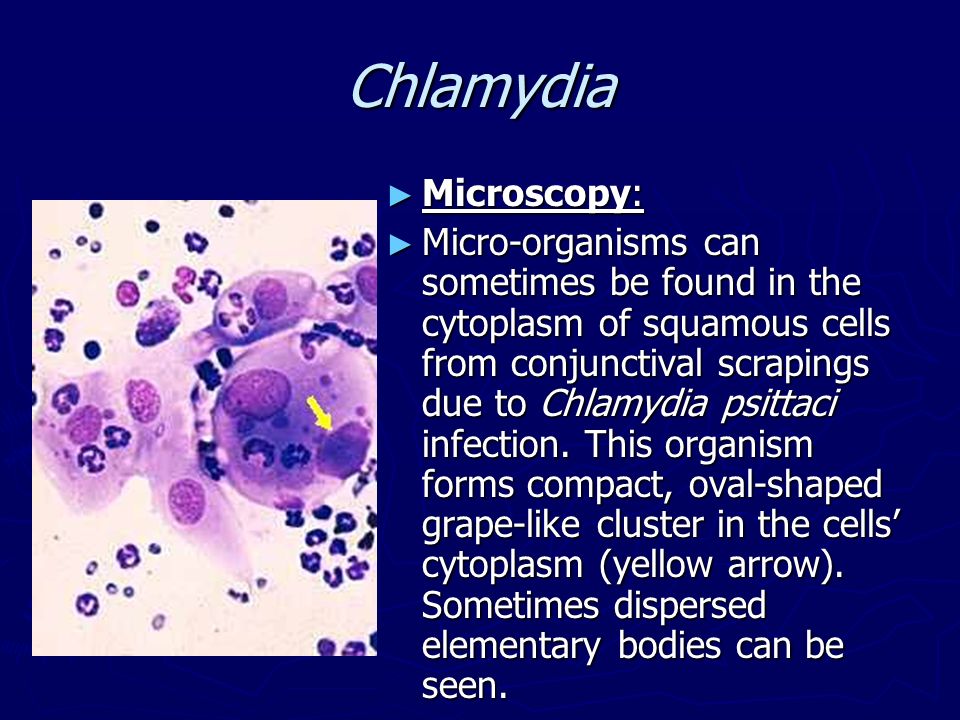 Women can get pelvic inflammatory disease, and men can get epididymitis (a painful infection near the testicle).
Women can get pelvic inflammatory disease, and men can get epididymitis (a painful infection near the testicle).
Chlamydia complications
If chlamydia isn't treated properly, it can cause serious complications. People who have chlamydia for long periods without treatment risk becoming infertile or developing arthritis.
For women, chlamydia can spread into the uterus and fallopian tubes, causing pelvic inflammatory disease. Pelvic inflammatory disease can lead to ectopic pregnancies, chronic pelvic pain and infertility.
In men, chlamydia can cause epididymitis (a painful infection near the testicle) or spread to the prostate gland, and the tubes that carry sperm, which may result in chronic pain and/or fertility problems.
Both men and women can develop arthritis, eye inflammation and inflammation of the rectum.
Chlamydia and pregnancy
Because of this, doctors recommend that pregnant women under the age of 30 should be screened for chlamydia.
Pregnant women who are infected with chlamydia have an increased risk of their waters breaking prematurely, causing the baby to be born early.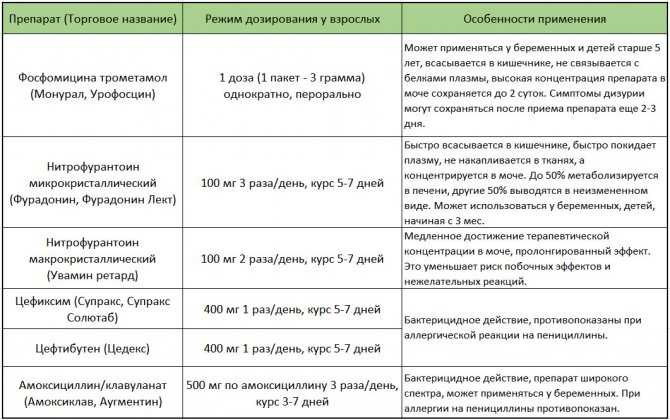
If a woman has chlamydia when giving birth, the baby might become infected during delivery. These babies can develop an eye infection (conjunctivitis) or pneumonia, and might need antibiotics. Chlamydia has also been associated with low birthweight.
The antibiotics used to treat chlamydia are safe in pregnancy and are used in pregnant women for many other types of infections.
Sources:
Australian Sexual Health Alliance (STI Management Guidelines for use in primary care; Chlamydia), King Edward Memorial Hospital Women and Newborn Health Service (Chlamydia clinical practice guideline), Lab Tests Online AU (Chlamydia), Melbourne Sexual Health Centre (National Management Guidelines for Sexually Transmissible Infections - Chlamydia), NSW Health (Chlamydia fact sheet)Learn more here about the development and quality assurance of healthdirect content.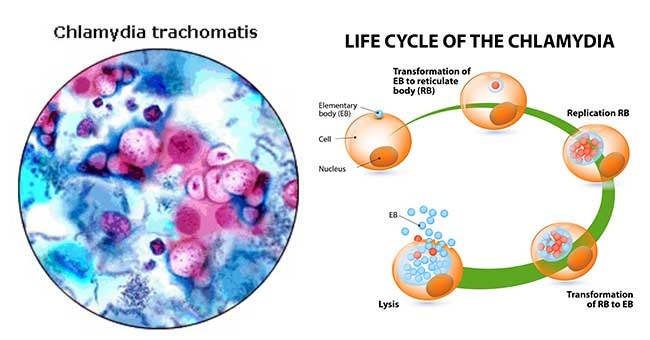
Last reviewed: November 2020
Back To Top
Related pages
- Antenatal care during your pregnancy
- Routine antenatal tests
Need more information?
Chlamydia - MyDr.com.au
Chlamydia is a sexually transmitted infection (STI). It affects both men and women, and it's spread by having sex with a person who has the infection.
Read more on myDr website
Chlamydia - Better Health Channel
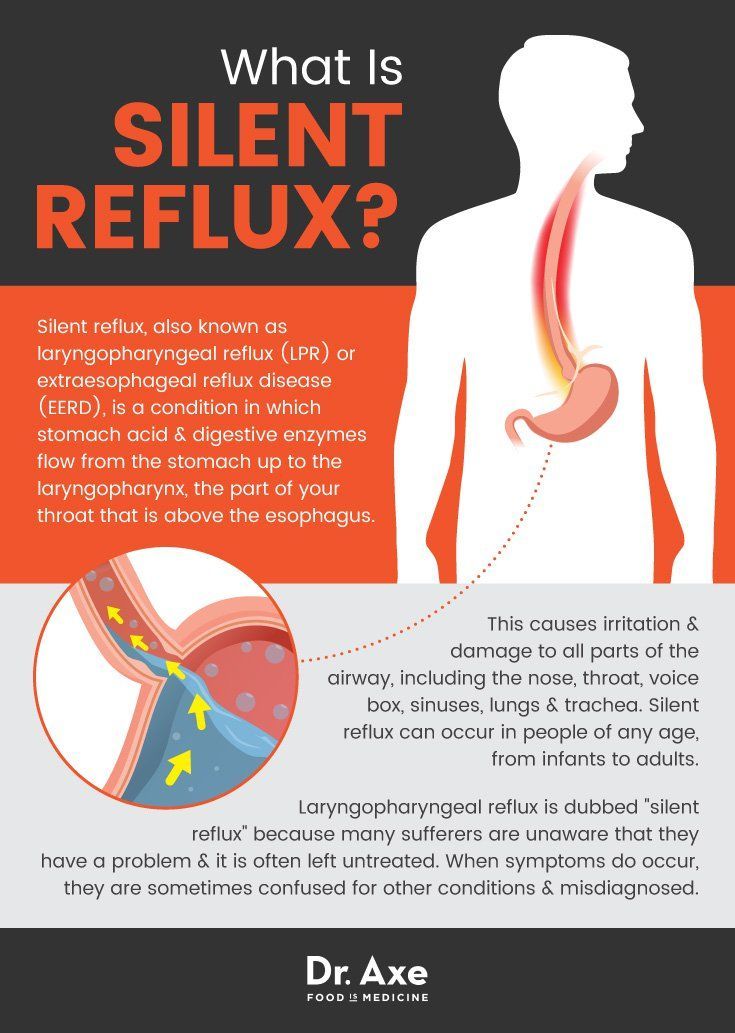
Chlamydia is often called the 'silent infection' because most people do not realise they have it.
Read more on Better Health Channel website
Chlamydia fact sheet - Fact sheets
Chlamydia is a sexually transmissible infection. Many people who are infected do not have symptoms of infection but can still spread the disease. Chlamydia can lead to infertility, and other complications if not treated.
Many people who are infected do not have symptoms of infection but can still spread the disease. Chlamydia can lead to infertility, and other complications if not treated.
Read more on NSW Health website
Chlamydia | Family Planning NSW
Chlamydia is a common sexually transmitted infection (STI) caused by a bacteria. It affects both men and women. Most people with chlamydia do not have symptoms. This means you can pass the infection to a partner without knowing it. Having a regular sexual health check-up can help you find out if you have chlamydia.
Read more on Family Planning Australia website
Chlamydia (Clam-id-ee-a) - Body Talk
Chlamydia is known as the ‘silent infection’ as most people have no signs or symptoms
Read more on Body Talk website
Chlamydia treatment for your partner - Play Safe
Did you know it’s possible for your partner to get treated for Chlamydia without ever having to see a GP or go to a sexual health clinic? This is known as Patient Delivered Partner Therapy (PDPT)
Read more on NSW Health website
The facts about Chlamydia, what it is, how to prevent it, and how to treat it
Chlamydia is on the rise in Australia and it’s the most important thing for young people to test for.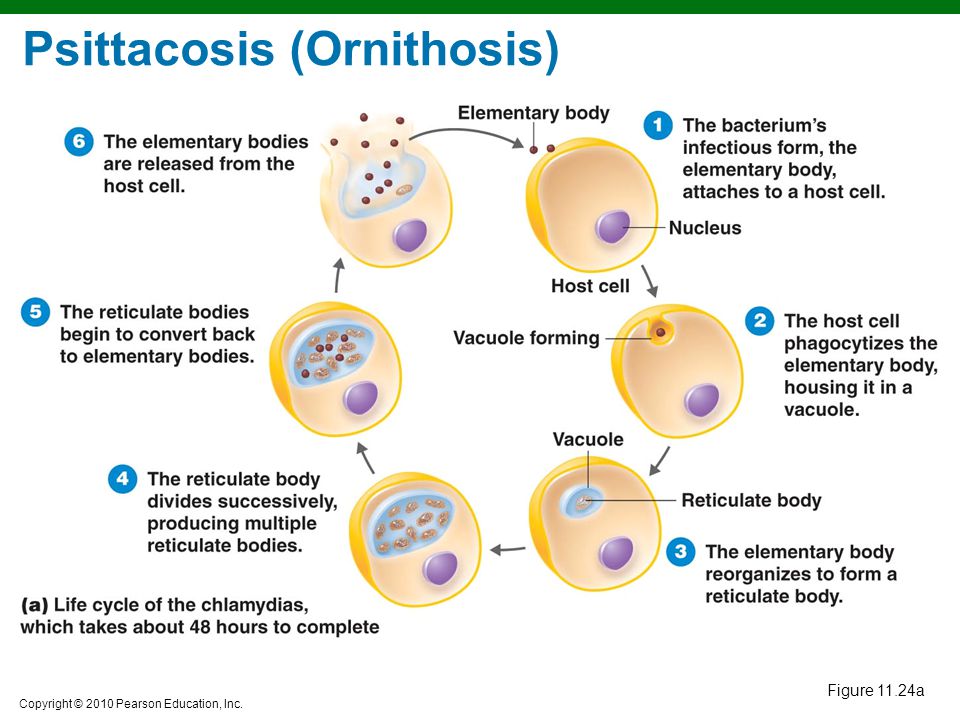 It often doesn’t have any symptoms which means that it’s easy to miss without regular STI testing.
It often doesn’t have any symptoms which means that it’s easy to miss without regular STI testing.
Read more on NSW Health website
Trachoma - Eye Infection
Trachoma is a preventable eye condition caused by repeated infections with eye strains of the bacterium Chlamydia trachomatis that lead to a roughening of the inner surface of the eyelid.
Read more on Queensland Health website
STIs and safe sex: I LOVE condoms! - Body Talk
What is the best way to tell if your partner has Chlamydia? They tell you they don’t have it They know how to use a condom They have no visible symptoms They have had a recent sexual check-up and got the all clear
Read more on Body Talk website
Gonorrhoea | Family Planning NSW
Gonorrhoea is a bacterial sexually transmitted infection (STI).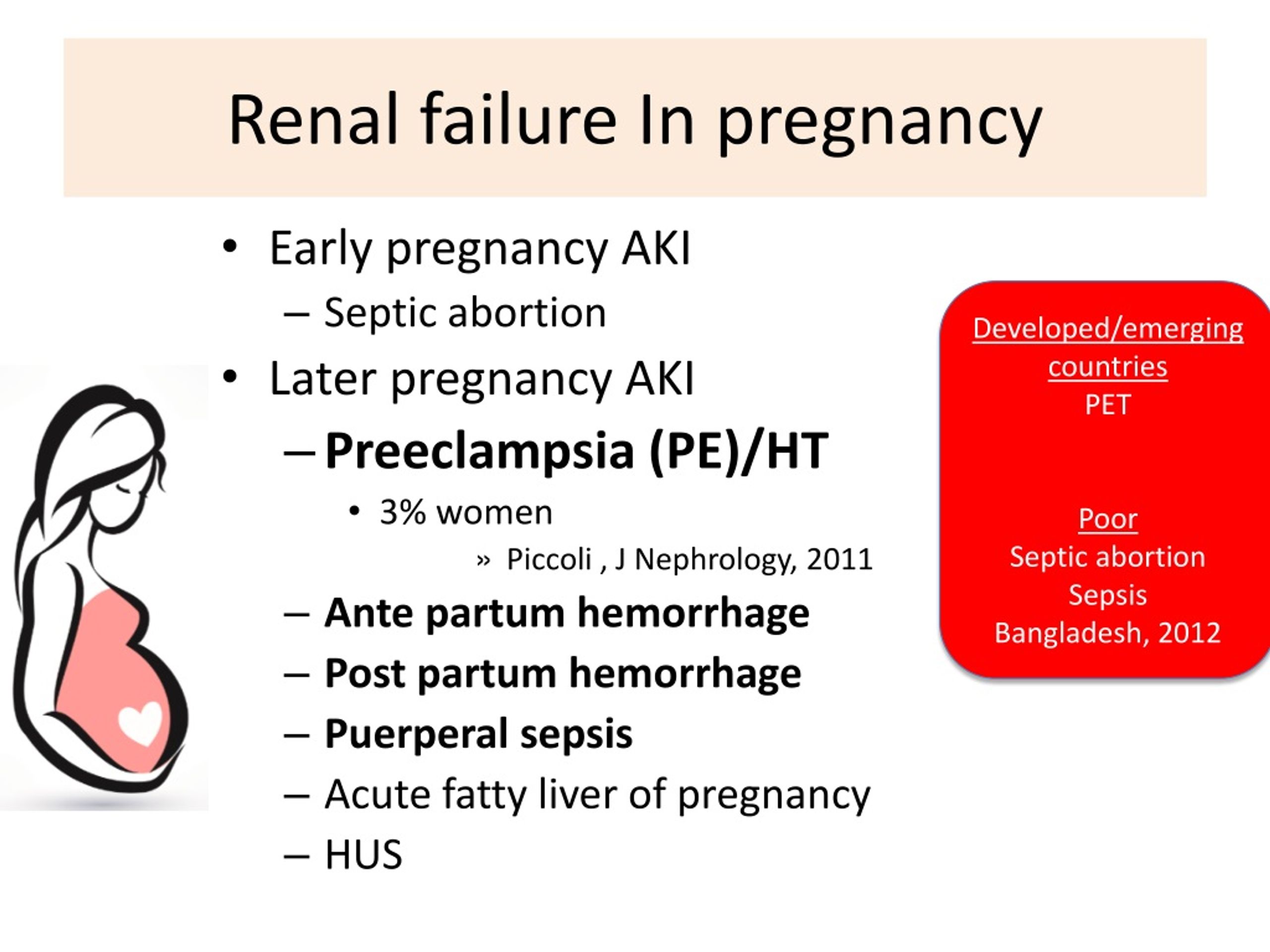 It is spread through vaginal, anal or oral sex, or by the fingers and hands from the genitals to the eyes. It is less common in the general community than other STIs such as chlamydia. Gonorrhoea can infect the throat, rectum (back passage), urethra (urine passage), cervix (neck of the womb) and eyes.
It is spread through vaginal, anal or oral sex, or by the fingers and hands from the genitals to the eyes. It is less common in the general community than other STIs such as chlamydia. Gonorrhoea can infect the throat, rectum (back passage), urethra (urine passage), cervix (neck of the womb) and eyes.
Read more on Family Planning Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.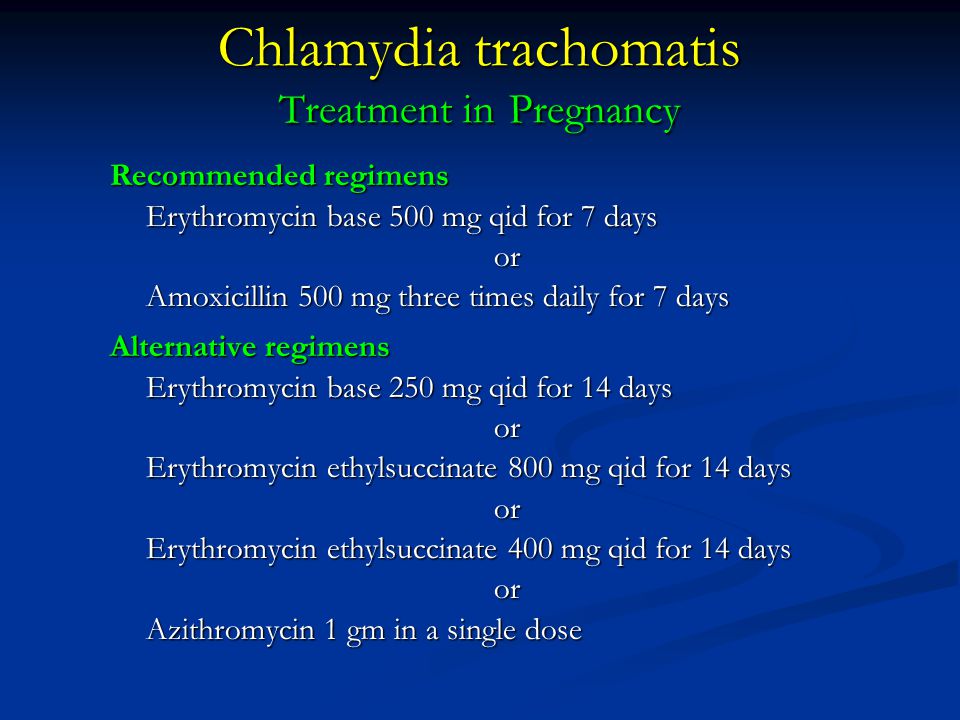
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Chlamydia in pregnancy: How STDs affect your baby
Chlamydia is a sexually transmitted infection that can be passed on to your baby with serious consequences.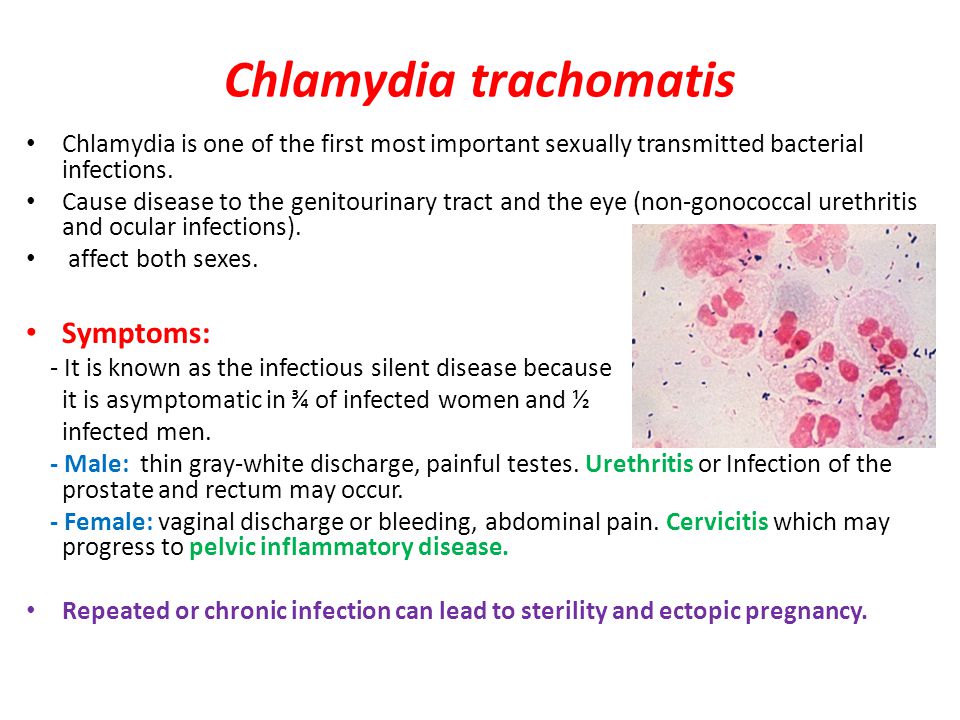 Because there are usually no symptoms, it's important to be tested for it early in pregnancy. If you test positive, both you and your partner will be treated with antibiotics.
Because there are usually no symptoms, it's important to be tested for it early in pregnancy. If you test positive, both you and your partner will be treated with antibiotics.
What is chlamydia?
Chlamydia is a curable bacterial infection that can be transmitted through genital, oral, or anal sex. It can also be passed from a woman to her baby during delivery.
The Centers for Disease Control and Prevention (CDC) estimates that 1.8 million people in the United States get chlamydia each year, making it the most common sexually transmitted bacterial infection. The rate increased 3 percent between 2017 and 2018. The highest rates are found in sexually active women under 30 years old, particularly those who are 20 to 24 years old.
How can chlamydia affect my pregnancy?
Prompt treatment may reduce the risk of these problems, but women who have chlamydia during pregnancy tend to have higher rates of:
- Infection of the amniotic sac and fluid
- Preterm premature rupture of the membranes (PPROM)
- Preterm birth
Some studies have linked chlamydia to an increased risk of miscarriage, although other studies have found no connection.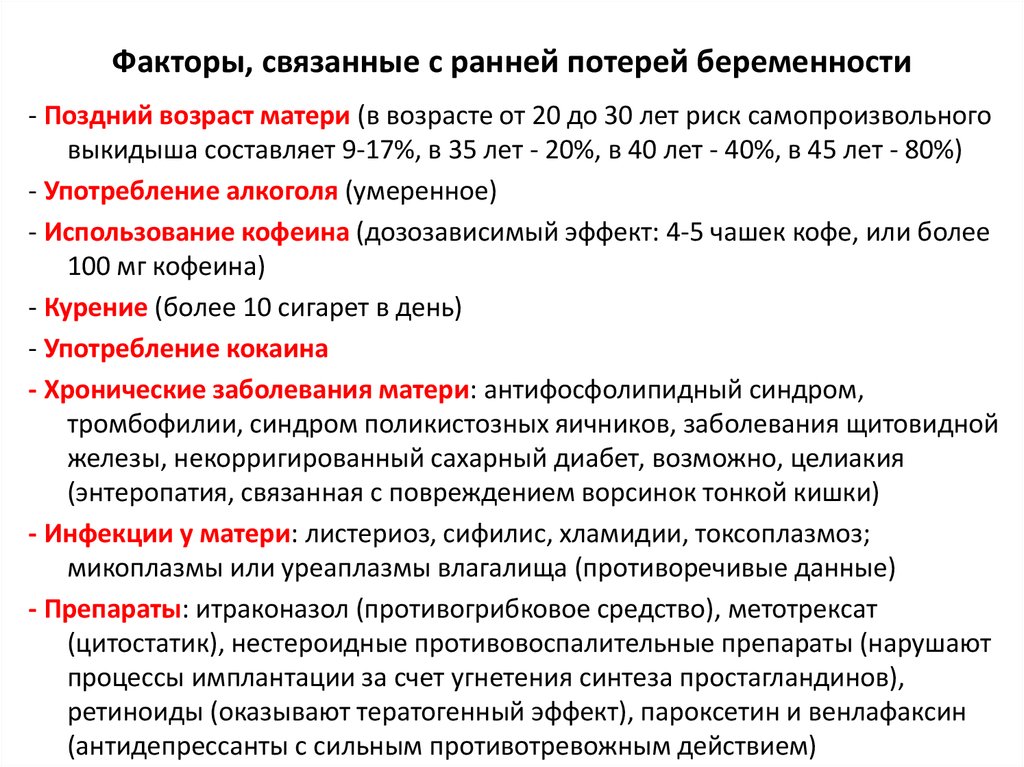
An untreated chlamydia infection also makes you more susceptible to HIV and some other sexually transmitted infections (STIs) if you're exposed to them. It also raises your risk of a uterine infection after you have your baby.
Can chlamydia in pregnancy affect my baby?
Yes, if you have a chlamydia infection when you go into labor, there's a chance that you'll pass the bacteria to your baby. In fact, up to half of babies born vaginally to mothers with untreated chlamydia (and even some babies born by c-section) will contract the infection.
Between 25 to 50 percent of these babies will develop an eye infection (conjunctivitis) a few days to a few weeks after birth. (The medicated drops or ointments put in your baby's eyes soon after birth to prevent gonorrheal conjunctivitis don't prevent chlamydial eye infections.) And 5 to 30 percent of babies who contract chlamydia during delivery develop pneumonia a few weeks to several months after birth.
Although these infections can be very serious, babies who are treated promptly with antibiotics generally do well.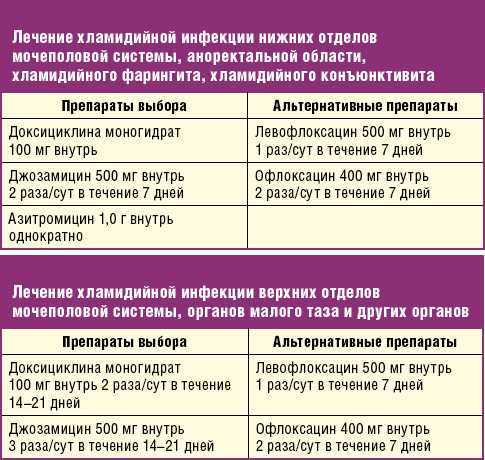 Of course, it's best to get treated before delivery to prevent your baby from becoming infected in the first place.
Of course, it's best to get treated before delivery to prevent your baby from becoming infected in the first place.
Advertisement | page continues below
What are the symptoms of chlamydia in pregnancy?
It's important to note that in the vast majority of chlamydia cases (up to 90 percent of women) there are no symptoms. If you do have symptoms, they're likely to show up about one to three weeks after you've been exposed. These symptoms may include:
- Burning or discomfort when you urinate
- Inflammation of your cervix
- Increased vaginal discharge or possibly spotting
- Abdominal pain
- Pain during sex
- If you engage in anal intercourse, you may also have inflammation of your rectum, rectal pain, and discharge.
- If you have oral sex with an infected partner, your throat can become infected and may feel sore.
Up to 70 percent of men infected with chlamydia have no symptoms. The most common symptoms include discharge from the penis, burning or pain while urinating, tender or swollen testicles, and inflammation of the rectum.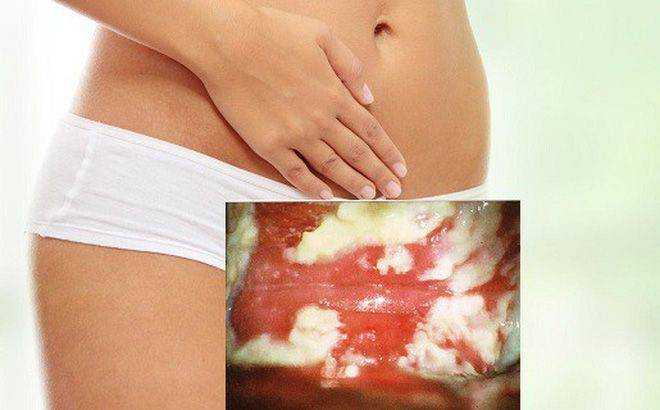 It's important to let your caregiver know if either you or your partner has symptoms of chlamydia and make sure you both get tested and treated if necessary.
It's important to let your caregiver know if either you or your partner has symptoms of chlamydia and make sure you both get tested and treated if necessary.
Can chlamydia in pregnancy cause pelvic inflammatory disease (PID)?
Yes. Before and after pregnancy, chlamydia can travel up from your cervix to infect your uterus or fallopian tubes, causing pelvic inflammatory disease (PID). In fact, up to 15 percent of women who aren't pregnant who have untreated chlamydia infections end up with PID. (It's possible to get PID during pregnancy, but it rarely happens.)
Symptoms of PID include:
- Pain in your lower abdomen or back
- Pain during sex
- Vaginal bleeding
- Fever
- Nausea
PID can result in permanent damage to your fallopian tubes and lead to chronic pelvic pain and infertility, as well as an increased risk of ectopic pregnancy if you do become pregnant.
Will I be screened for chlamydia during my pregnancy?
Most likely, yes. Because it's so important to detect and treat chlamydia during pregnancy, because it's a relatively common infection, and because the infection usually occurs without symptoms, the CDC recommends that all pregnant women be screened for chlamydia at their first prenatal visit.
Because it's so important to detect and treat chlamydia during pregnancy, because it's a relatively common infection, and because the infection usually occurs without symptoms, the CDC recommends that all pregnant women be screened for chlamydia at their first prenatal visit.
To test for chlamydia, your practitioner will send either a swab from your vagina or cervix or a urine specimen to the lab for analysis. If your chlamydia test is positive and you weren't tested for other STIs at the same time, your caregiver will do so now.
If you're under 25 years old or otherwise at high risk for contracting chlamydia (you or your partner has a new sex partner or more than one sex partner), your practitioner might repeat the test during your third trimester, to make sure you're not infected as you prepare for delivery. You'll also be retested if you've contracted another STI during your pregnancy or if you or your partner develops symptoms of chlamydia.
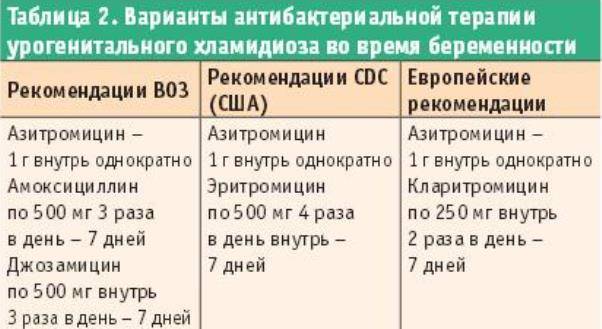
How is chlamydia treated during pregnancy?
Chlamydia is treated with antibiotics that are safe to take during pregnancy. Your practitioner may prescribe an antibiotic that you take in a single dose or one that you take over the course of a week. (Be sure to take the medicine exactly as prescribed.) In most cases, one round of treatment will cure the infection.
Your practitioner may prescribe an antibiotic that you take in a single dose or one that you take over the course of a week. (Be sure to take the medicine exactly as prescribed.) In most cases, one round of treatment will cure the infection.
Your partner should be treated at the same time, and both of you should abstain from sex until a week after completing treatment so you don't get reinfected.
The CDC recommends that pregnant women be tested again three to four weeks after completing treatment to make sure the infection is gone.
How can I avoid getting chlamydia in pregnancy?
Have sex only with a long-term partner who has sex only with you. Otherwise, use latex condoms during intercourse, and a dental dam during oral sex, to reduce your risk of getting chlamydia and certain other STIs.
Again, if it's possible that you've been exposed to chlamydia (or any other STI) during pregnancy, or you develop any symptoms, tell your practitioner right away so that you can be tested and treated if necessary.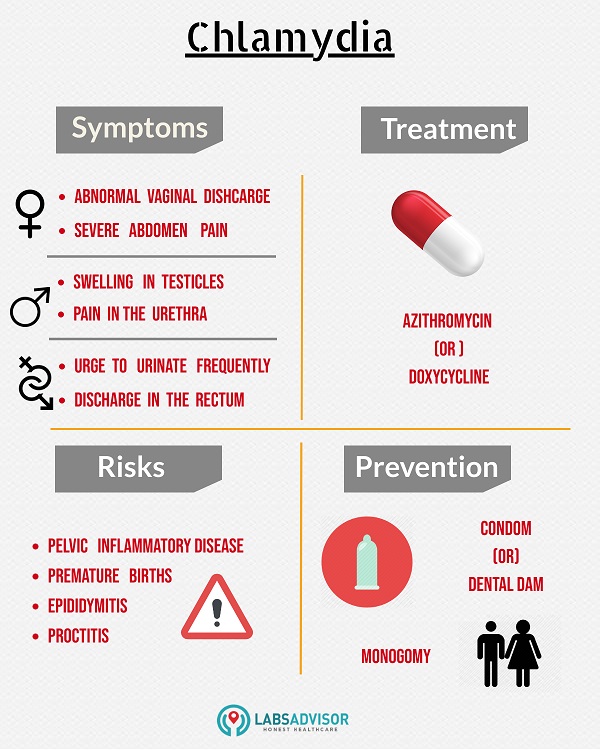
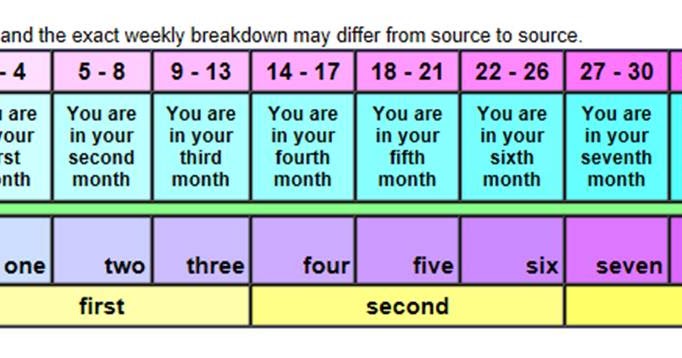
The test for chlamydia is one of the many tests you'll have during pregnancy. Here's an overview of what tests you can expect in each trimester.
Was this article helpful?
Yes
No
Chlamydia and pregnancy
Their favorite habitat is the cervix (more precisely, the mucous membrane of the cervical canal). It is there that they are located in colonies, i.e. are not found throughout. Such frequent cases are associated with this fact, when one doctor takes a smear from the cervical canal and chlamydia is found in it, and the other one also takes a smear a day later, but chlamydia is not found again. That is why the diagnostic value of swabs for chlamydia is quite low - about 30%.
How chlamydia manifests itself
During an exacerbation of the infectious process, women's complaints may be different, depending on the level of chlamydia spread.
When chlamydia is found in the cervix, there may be slight discharge from the vagina, accompanied by moderate pulling pains in the lower abdomen, which is typical with local exacerbation of the process (there are practically no complaints in the chronic form). If the infection spreads higher (uterine cavity, tubes), then the complaints are more pronounced, because, for example, inflammation of the appendages may begin.
If the infection spreads higher (uterine cavity, tubes), then the complaints are more pronounced, because, for example, inflammation of the appendages may begin.
Exacerbation of chlamydial infection is especially dangerous during pregnancy, as it can lead to various complications.
Possible complications:
- early miscarriages are possible,
- late term premature amniotic fluid and preterm labor,
- in childbirth, there is a high probability of infection of the fetus (conjunctivitis, pharyngitis, otitis and even pneumonia).
Chlamydia diagnostics
The most informative method is a blood test for antibodies (immunoglobulins) to chlamydia. If a small concentration of these antibodies is detected, then they speak of a chronic carriage of chlamydia. If the concentration is high, there is an exacerbation of chlamydial infection.
The diagnosis of "chlamydia" is legitimate when it is confirmed by two fundamentally different diagnostic methods: smear (microscopy) and blood for antibodies to chlamydia (biochemical method).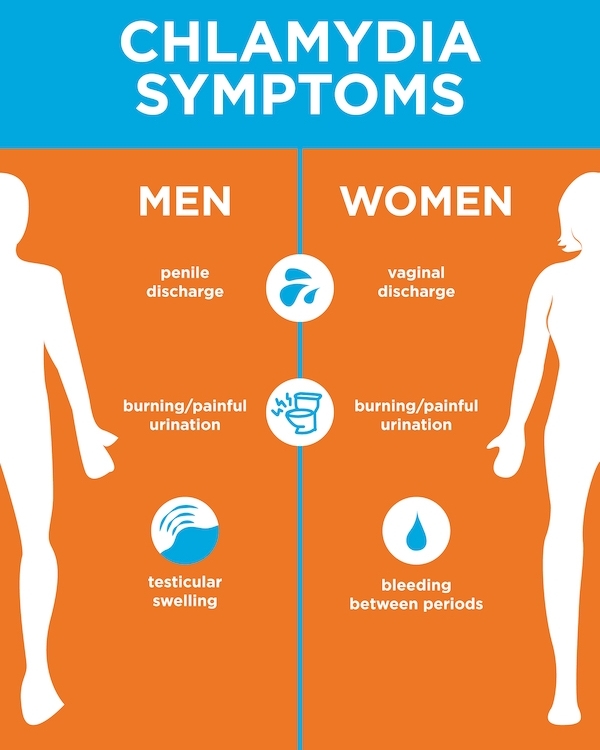 Only when the titer (concentration) of antibodies is high and / or in the presence of complaints specific to this infection, a course of treatment is indicated.
Only when the titer (concentration) of antibodies is high and / or in the presence of complaints specific to this infection, a course of treatment is indicated.
Digits must be multiples, i.e. more or less than twice, from the previous one (IgA 1:40 and IgG 1:80). Titers of 1:5 and less are doubtful and negative. Elevated IgG numbers indicate that the process is chronic. In this case, treatment is indicated if there are certain complaints, or if before that, the person has never been treated for this infection. High numbers of IgA are mainly found in an acute process (primary infection) or during an exacerbation of a chronic one that needs treatment.
What to do if the test is positive?
It must be remembered that today there are almost no 100% reliable methods, including the ELISA method (enzymatic immunoassay) is no exception. Quite often there are “false positive” results - you have to do either repeated tests or use other, fundamentally different methods.
These can be:
- taking smears for the PIF method (examination with a luminescent microscope) - where there may also be “false positive” answers,
- PCR blood test (based on the principle of genetic engineering, the study of DNA or its fragments) - today, its reliability is very high.

In the search for the truth of the diagnosis, quite often, everything can rest either on the financial capabilities of patients, or on the insufficient equipment of a particular laboratory. The better the body's defenses, the less likely it is to contract chlamydia. In which case, only “carriage” threatens you, it is not dangerous for you (only IgG, in low titers, will be determined in the blood test).
It is considered optimal if the whole family is examined at the same time (all interested persons, including children), because in this case, it is possible to identify who is at what stage and monitor the effectiveness of treatment.
In most cases, the pathogens of ureplasmosis and mycoplasmosis do not manifest themselves (hidden bacteriocarrier), and only when the process is exacerbated, they cause pregnancy complications similar to chlamydia and infection of the fetus. Therefore, when examining women who have had the above problems in the past, swabs and blood are taken at least immediately for these three pathogens. By the way, studies have shown that taking hormonal birth control pills reduces the risk of chlamydia infection, this effect is associated with an increase in the protective properties of cervical mucus (its permeability to bacteria decreases). As mentioned above, chlamydia is dangerous for pregnant women.
By the way, studies have shown that taking hormonal birth control pills reduces the risk of chlamydia infection, this effect is associated with an increase in the protective properties of cervical mucus (its permeability to bacteria decreases). As mentioned above, chlamydia is dangerous for pregnant women.
What to do?
But what to do if, after all, doctors found chlamydia in the acute stage in the expectant mother?
The placenta can be thought of as a mesh filter through which large molecules cannot pass (they remain in the mother's body). Therefore, in the treatment of a pregnant woman, antibiotics are used that are harmless to the fetus (i.e. those that do not pass through the placenta). These include drugs whose molecular weight is greater than the "capacity" of the capillaries. However, when taking these drugs, the effect on the fetus is still possible. The antibiotic acts primarily on the mother's body, however, during the period of treatment, it changes the metabolism in the body, which in turn affects the metabolism of the fetus. Antibiotics are always prescribed in short courses so that the effects are minimal.
Antibiotics are always prescribed in short courses so that the effects are minimal.
References
- Zofkie AC., Fomina YY., Roberts SW., McIntire DD., Nelson DB., Adhikari EH. Effectiveness of Chlamydia Trachomatis expedited partner therapy in pregnancy. // Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33894150
- Zofkie AC., Fomina YY., Roberts SW., McIntire DD., Nelson DB., Adhikari EH. Effectiveness of Chlamydia Trachomatis expedited partner therapy in pregnancy. // Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33894147
- Shilling HS., Garland SM., Costa AM., Marceglia A., Fethers K., Danielewski J., Murray G., Bradshaw C., Vodstrcil L., Hocking JS., Kaldor J., Guy R., Machalek D.A. Chlamydia trachomatis and Mycoplasma genitalium prevalence and associated factors among women presenting to a pregnancy termination and contraception clinic, 2009-2019. // Sex Transm Infect - 2021 - Vol - NNULL - p.; PMID:33782146
- Vercruysse J.
 , Mekasha S., Stropp LM., Moroney J., He X., Liang Y., Vragovic O., Valle E., Ballard J., Pudney J., Kuohung W., Ingalls RR. Chlamydia trachomatis Infection, when Treated during Pregnancy, Is Not Associated with Preterm Birth in an Urban Safety-Net Hospital. // Infect Dis Obstet Gynecol - 2020 - Vol2020 - NNULL - p.8890619; PMID:33082702
, Mekasha S., Stropp LM., Moroney J., He X., Liang Y., Vragovic O., Valle E., Ballard J., Pudney J., Kuohung W., Ingalls RR. Chlamydia trachomatis Infection, when Treated during Pregnancy, Is Not Associated with Preterm Birth in an Urban Safety-Net Hospital. // Infect Dis Obstet Gynecol - 2020 - Vol2020 - NNULL - p.8890619; PMID:33082702 - Olaleye AO., Babah OA., Osuagwu CS., Ogunsola FT., Afolabi BB. Sexually transmitted infections in pregnancy - An update on Chlamydia trachomatis and Neisseria gonorrhoeae. // Eur J Obstet Gynecol Reprod Biol - 2020 - Vol255 - NNULL - p.1-12; PMID:33059307
- Hoenderboom BM., van Bergen JEAM., Dukers-Muijrers NHTM., Götz HM., Hoebe CJPA., de Vries HJC., van den Broek IVF., de Vries F., Land JA., van der Sande MAB., Morré SA., van Benthem BHB. Pregnancies and Time to Pregnancy in Women With and Without a Previous Chlamydia trachomatis Infection. // Sex Transm Dis - 2020 - Vol47 - N11 - p.739-747; PMID:32701764
- He W., Jin Y.
 , Zhu H., Zheng Y., Qian J. Effect of Chlamydia trachomatis on adverse pregnancy outcomes: a meta-analysis. // Arch Gynecol Obstet - 2020 - Vol302 - N3 - p.553-567; PMID:32643040
, Zhu H., Zheng Y., Qian J. Effect of Chlamydia trachomatis on adverse pregnancy outcomes: a meta-analysis. // Arch Gynecol Obstet - 2020 - Vol302 - N3 - p.553-567; PMID:32643040 - Freeman J., Pettit J., Howe C. Chlamydia test-of-cure in pregnancy. // Can Fam Physician - 2020 - Vol66 - N6 - p.427-428; PMID:32532724
- Rajabpour M., Emamie AD., Pourmand MR., Goodarzi NN., Asbagh FA., Whiley DM. Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis among women with genitourinary infection and pregnancy-related complications in Tehran: A cross-sectional study. // Int J STD AIDS - 2020 - Vol31 - N8 - p.773-780; PMID:32517577
- Goggins ER., Chamberlain AT., Kim TG., Young MR., Jamieson DJ., Haddad LB. Patterns of Screening, Infection, and Treatment of Chlamydia trachomatis and Neisseria gonorrhea in Pregnancy. // Obstet Gynecol - 2020 - Vol135 - N4 - p.799-807; PMID:32168225
Chlamydia during pregnancy | Lisa.ru
Chlamydia: causes and symptoms
The causative agents of chlamydia are small rounded bacteria - chlamydia, which affect the mucous membranes of the organs and, above all, the organs of the genitourinary system.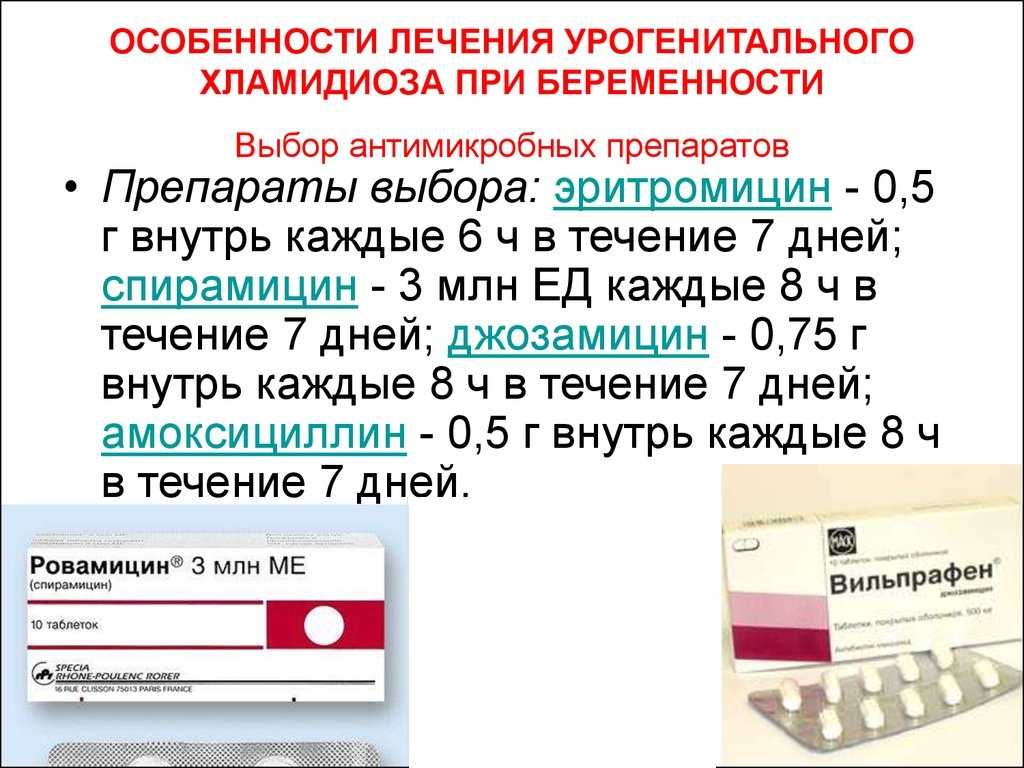 Chlamydia is considered one of the most common sexually transmitted diseases. According to statistics, about 100 million people fall ill with chlamydia every year in the world. There are acute and chronic forms of infection.
Chlamydia is considered one of the most common sexually transmitted diseases. According to statistics, about 100 million people fall ill with chlamydia every year in the world. There are acute and chronic forms of infection.
Chlamydia: acute
In 80% of cases, there are no symptoms of the disease, so reliable information can only be obtained after passing a urine test or a vaginal smear. Minor symptoms of chlamydia can occur in a woman within three weeks after infection - these are mucous or purulent discharge with a yellowish tinge and an unpleasant odor, itching in the perineum, pain during urination.
Chlamydia: chronic
In chronic chlamydia, pathogens enter the uterus through the cervix. 15-20% of all infected are carriers of the chronic form of the disease. Chlamydia, which has taken a chronic form, can be detected by short-term and minor bleeding between periods, pain in the lower abdomen and fever.
Chlamydia: complications
Without proper and timely treatment of chlamydia, inflammation in the uterus can spread to other organs. If during the illness the fallopian tubes and the fetal membrane were affected, then after recovery, adhesions may form in them. And adhesive processes increase the risk of infertility and ectopic pregnancy. Chlamydia during pregnancy can cause premature birth and rupture of the amniotic sac. Why chlamydia causes this effect is still unknown. Of particular danger is infection with chlamydia in late pregnancy, since in 60-70% of cases the disease is transmitted to the fetus. As a result, chlamydia can cause severe lung and eye disease.
If during the illness the fallopian tubes and the fetal membrane were affected, then after recovery, adhesions may form in them. And adhesive processes increase the risk of infertility and ectopic pregnancy. Chlamydia during pregnancy can cause premature birth and rupture of the amniotic sac. Why chlamydia causes this effect is still unknown. Of particular danger is infection with chlamydia in late pregnancy, since in 60-70% of cases the disease is transmitted to the fetus. As a result, chlamydia can cause severe lung and eye disease.
For the safety of the child during pregnancy, a woman is tested for chlamydia. If the disease was detected on time, then, as a rule, it can be effectively treated.
Chlamydia: prevention and treatment
Timely treatment of chlamydia in a pregnant woman before delivery is of particular importance, as this will reduce the chance of infection of the child. For this, an analysis for chlamydia in the early stages (as part of the planned management of pregnancy) is provided.