Child getting sick
Kids and viruses: Why do my kids keep getting sick? | HealthFocus SA
Currently we are seeing high rates of many different viruses affecting children within our area, including RSV, flu and rhinovirus/enterovirus. Schools, daycares, stores, restaurants and other crowded places expose children to these viruses.
Given the high number of infection rates, a child could be sick with multiple viruses. Their symptoms from one illness may not have completely resolved before they start to have symptoms from another virus.
Dr. Mandie Tibball Svatek answers common questions from parents about protecting kids from illness.
When can I send my child back to school after they’ve been sick?
Many schools have their own guidelines for returning to school, so you should call and ask if you aren’t sure. Typically, a child should be fever-free for 24 hours and not have symptoms like vomiting, diarrhea, mouth sores or rashes.
Cough and congestion may still be present after some of the common viruses, but as long as other symptoms have resolved, cough and congestion can be allowed.
They got better and within three days they had another fever. Can they get the same virus twice?
If there are different variants of the virus in the community — such as the flu —there is the potential to get repeat infections. This is similar to what we’ve seen with COVID-19 infections.
It’s also not unusual for a child to start daycare for the first time and develop 8-12 viral respiratory infections within that first year. As a child’s immune system develops, the number of infections will usually decrease with time.
When should I take my child to the emergency department?
Take your child to the emergency room if they have symptoms such as:
- Difficulty breathing
- Not being able to tolerate oral intake
- Fever that does not resolve after five days or is getting worse
- Change in mental status
Is it important to know which virus they have?
A swab is not needed to identify viruses.
If your child has flu-like symptoms such as fever, cough, congestion, headache, muscle aches and fatigue and they are presenting within the first 48 hours of symptoms then they can be tested.
Their pediatrician may decide to start a medication such as Tamiflu to help shorten the duration of symptoms.
For COVID-19, a parent may choose to get their child tested for the following reasons:
- Patients who have symptoms consistent with COVID-19 should be tested immediately.
- Patients who are asymptomatic but have had close contact with an individual who has confirmed or probable COVID-19 should be tested at least five days after last exposure. However, these patients should be tested immediately if they develop symptoms consistent with COVID-19.
- Patients who are required to obtain screening tests based on local public health authorities, school districts or other local organizations should be tested as required.
Overall, it is important to contact your health care provider for your child to help guide you in decisions about testing and potential treatments for your child. The health care provider can also provide direction on when to return to school and activities that the child may be participating in.
How do we boost their immune system?
Vaccines such as the COVID-19 vaccine and flu vaccine can provide protection and can shorten the duration of symptoms. Keeping your child up to date on all vaccines is also extremely important to help protect your child from vaccine-preventable diseases.
Eating a well-balanced diet is also important in keeping the body healthy.
Once they are sick, what’s the best way to quickly flush the virus from their system?
It’s important to keep a child hydrated during their illness, so giving them plenty of fluids is important. Treating the fever with fever-reducing medications can also make the child feel better as the virus runs through their body.
Allowing a child to rest and stay out of activities will also help lead to an easier recovery.
What can I do to prevent my child from getting sick?
Different viruses are spread in different ways either through the air and/or on surfaces. Although they are not 100% effective, mask wearing and hand washing can help keep a child from getting sick.
If there is a vaccine available, that is the most effective way of protecting against an illness.
If one of my children is sick, how do I prevent others in the household from getting the virus as well?
It may be difficult to prevent the spread of the virus to others in your house, but it’s especially important to have a plan to protect young infants, older individuals, and those who may have health problems that can be worsened by an illness.
You can encourage good hand hygiene at home and clean surfaces that a sick child may have touched. You can also ask family members to wear a mask and/or have the child wear a mask to potentially reduce spread to other individuals in the house, and separate individuals who are susceptible from those who are sick.
Should kids wear masks to avoid getting flu and other respiratory infections?
Face masks for children two years and older can definitely be considered during this time where viruses such as the flu are predominant in our area.
You may also consider mask wearing for children when COVID-19 infection rates are high, for those children that have a weakened immune system, and to protect other family members that may be at risk in the household as noted above.
How to Keep Your Child Safe Amid the 'Tripledemic' > News > Yale Medicine
Originally published: Aug. 11, 2022. Updated: Jan. 11, 2023.
Note: Information in this article was accurate at the time of original publication. Because information about COVID-19 changes rapidly, we encourage you to visit the websites of the Centers for Disease Control & Prevention (CDC), World Health Organization (WHO), and your state and local government for the latest information.
A major concern for parents this past fall was how to protect their kids in what was shaping up to be a “tripledemic”—the chance of flu, COVID-19, and RSV (respiratory syncytial virus) happening at the same time and sending more people to already overstretched hospitals. But in the first weeks of the new year, the situation had changed: While COVID-19 is on the rise, flu (while still circulating) is declining after an early surge. Meanwhile cases of RSV are plummeting.
But in the first weeks of the new year, the situation had changed: While COVID-19 is on the rise, flu (while still circulating) is declining after an early surge. Meanwhile cases of RSV are plummeting.
The last several months are still concerning, however. Kids got sick earlier than usual last fall, and in higher numbers. Common colds and other viruses that nearly vanished during the pandemic came back, and children with respiratory viruses crowded emergency rooms in some parts of the country.
This winter, fewer people have been practicing infection control, even as the highly contagious Omicron and its subvariants (like the recent XBB.1.5) continue to circulate. Doctors believe that relaxing mitigation efforts have opened the door to non-COVID diseases, which have been behaving erratically—for instance, causing infections at odd times of the year.
Yale Medicine experts answered some common virus questions on parents’ minds.
1. What viruses should parents be concerned about this winter?
“We're paying attention to everything,” says Thomas Murray, MD, PhD, a Yale Medicine pediatric infectious diseases specialist. He notes that many types of viruses circulate among kids in a given year, including influenza and rhinoviruses, which cause common colds and are not typically worrisome. But there are many other viruses that parents should look out for, including:
He notes that many types of viruses circulate among kids in a given year, including influenza and rhinoviruses, which cause common colds and are not typically worrisome. But there are many other viruses that parents should look out for, including:
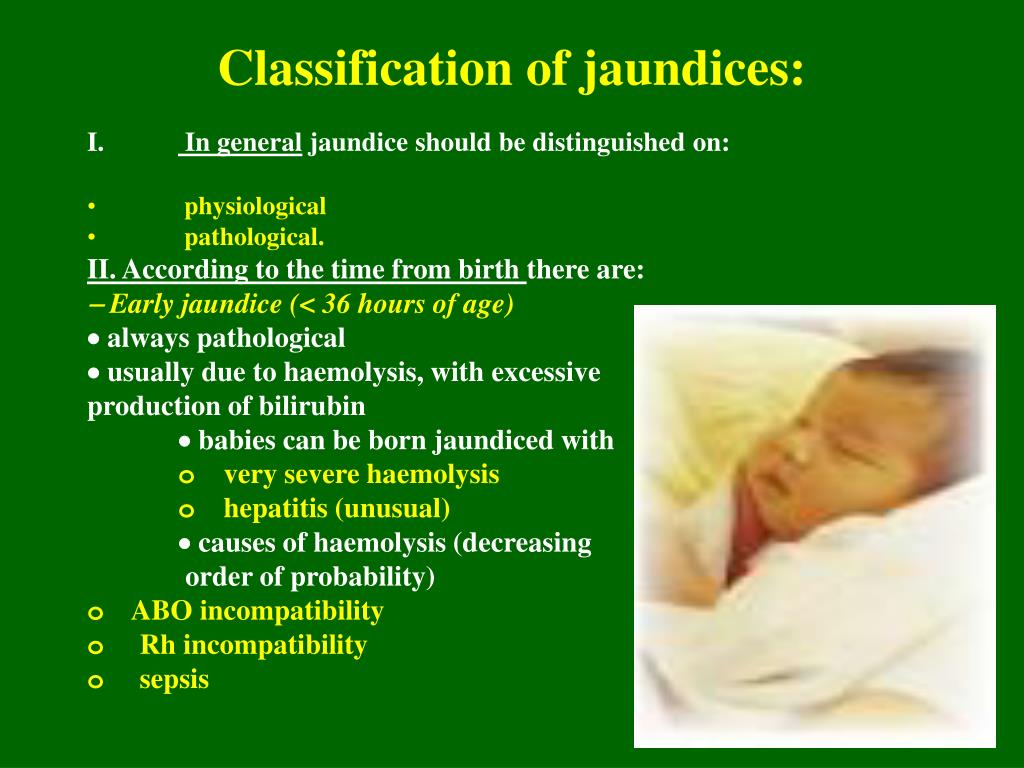
- RSV, which causes cold-like symptoms and can lead to serious complications in young children. It has landed up to 60,000 children in the hospital in pre-pandemic winters—in the season when it is most common. RSV seemed to disappear in 2020-2021, then returned off-season in the spring and summer last year. It flooded many children’s hospitals this past fall.
- Adenoviruses, which are common and usually cause mild cold- or flu-like symptoms. It's worth noting that the Centers for Disease Control and Prevention (CDC) currently has a Health Alert Notice for clinicians and a media statement for parents as it investigates a rise in cases of hepatitis of unknown origin in children; some of the cases tested positive for adenovirus.

- Human parainfluenza viruses (HPIV), which causes symptoms that may include fever, runny nose, and cough. Patients usually recover on their own. However, HPIV also can cause more severe illness, such as pneumonia.
- Human parechovirus (PeV), a common virus that causes fever, rash, and respiratory infection. But a variant known as "type three" (PeV-A3) can be life-threatening to young infants. The CDC issued a health advisory in July 2022, when the virus was found circulating in multiple states, and urged pediatric health providers to monitor for the disease in newborns and babies younger than a year old who show signs of severe illness.
- Enterovirus D68, another virus that experts are monitoring, most commonly affects infants, children, and teenagers, and can pose especially serious risk for children with asthma. This virus also is suspected of causing a polio-like disorder called acute flaccid myelitis (AFM).
 Although small numbers of the virus have been reported since 1987, the CDC reported outbreaks between August and November in 2014, 2016, and 2018. Interestingly, there was no outbreak reported in 2020, the first year of the pandemic. “So again, we're always vigilant for different viruses like this,” Dr. Murray says.
Although small numbers of the virus have been reported since 1987, the CDC reported outbreaks between August and November in 2014, 2016, and 2018. Interestingly, there was no outbreak reported in 2020, the first year of the pandemic. “So again, we're always vigilant for different viruses like this,” Dr. Murray says. - Mpox (formerly known as monkeypox), a rare disease, similar to smallpox, but less severe, that has recently been spreading mostly in men who have sex with men. Pediatricians are on alert because its spread during this outbreak is so unusual. It causes such symptoms as chills and fever, and sometimes a very painful rash. “Right now, the probability that your child's rash is going to be mpox in the absence of a known exposure is pretty low,” says Dr. Murray, adding that other illnesses, like chickenpox, can cause a similar rash. Families should always notify their pediatrician about exposures to mpox or any other unusual disease, he adds.

2. What does it mean when viruses appear during an ‘off-season’?
There has been a heightened sense of unpredictability around all infectious diseases.
The timing of influenza cases in 2022 was an example of erratic viral behavior. In May, at the end of a mild pandemic flu season, cases ticked upward when they should have petered out, and the season extended into June, which is rare, Dr. Murray says.
The Yale Clinical Virology Laboratory produces weekly virus summaries that provide a small snapshot of other odd viral activity. In one week in July 2022, for example, the summary included RSV, flu, parainfluenza virus, adenovirus, HMPV, rhinoviruses, PeV, and norovirus, most of which are rarely seen in the summer. These numbers reflect a phenomenon experts are monitoring around the world.
While the numbers were low—only one case of PeV that week, for instance—it is still worth noting that those types of infections occurred off-season, Dr. Murray explains.
3. Are "off-season" viruses more severe?
Early last fall, Dr. Dias said that, as far as individual infections were concerned, the answer seemed to be no. “I think we're seeing potentially the same percentage of people getting admitted to the hospital, but a larger number because there are just more people getting sick right now.”
Viruses tend to spread themselves out, and it is unusual for kids to get more than one virus at a time. But some young patients admitted to Yale New Haven Children’s Hospital in 2022 were diagnosed with two or even three viruses at the same time.
“We have seen that before, so it's not completely unusual, but it does seem to be happening more now than it did before,” Dr. Dias says.
4. Should parents still worry about the coronavirus?
Yes. COVID-19 cases began to rise again toward the end of November, and in early 2023 the highly contagious Omicron subvariant XBB.1.5. was spreading rapidly throughout the country. In the Yale virology report ending the week of Jan. 1, there were 681 COVID-19 cases.
In the Yale virology report ending the week of Jan. 1, there were 681 COVID-19 cases.
Children tend to experience mild disease with COVID-19, but prevention remains important, since a significant number of children have died from the disease, explains Dr. Dias. Some also develop long COVID, a condition marked by lingering symptoms that is not yet well understood, she adds.
5. What symptoms should parents look for?
Many respiratory infections share similar symptoms, and Dr. Murray doesn’t expect those symptoms to be different than in previous years. “They include high fevers and difficulty breathing. If there is a new rash or you are worried about your child’s breathing, you should make the pediatric provider aware,” he says, adding that some symptoms can be signs not only of viruses, but also of other bacterial infections and/or typical baby infections.
In the case of COVID-19 and flu, the CDC lists a wide range of symptoms, including cough, shortness of breath, runny or stuffy nose, fatigue, sore throat, and even loss of taste or smell (although the latter is more frequent with COVID-19). In both cases, symptoms can vary from person to person: Some children have no symptoms at all; others have cases that range from asymptomatic to mild to severe.
In both cases, symptoms can vary from person to person: Some children have no symptoms at all; others have cases that range from asymptomatic to mild to severe.
6. When should a parent call the pediatrician?
While it’s not necessary to call about every symptom, some can be confusing, says Dr. Murray. “Any time a parent is concerned, it's best to call and be reassured.”
It may also be important to call the doctor if a child has a chronic medical condition, since that puts them at higher risk for severe symptoms or complications from viruses. The same goes for young babies, Dr. Murray adds.
Parents should also contact their pediatrician if a baby younger than three months old has a fever or is difficult to console. “If they’re cranky and you hold them and they settle down, that’s fine. But if you hold them and they're still absolutely irritable—and you cannot calm them down no matter what you do—that's a baby that needs to be evaluated,” he says.
7. How can doctors diagnose a child when there are different viruses with similar symptoms?
If a child has respiratory symptoms, the first thing a pediatrician will do is recommend a COVID-19 test. “The symptoms for many of these diseases overlap considerably,” Dr. Murray says. “So, it can be virtually impossible for a doctor to tell the difference between COVID-19 and another virus without a test.”
“The symptoms for many of these diseases overlap considerably,” Dr. Murray says. “So, it can be virtually impossible for a doctor to tell the difference between COVID-19 and another virus without a test.”
If the COVID test is negative, it’s helpful to know that mild colds or viruses usually start to get better in a few days, but if symptoms get worse, the doctor might consider testing your child for the flu, which can benefit from treatment.
Testing for RSV is done mostly for surveillance purposes. But it’s also helpful in deciding whether to isolate a child from other children if they are in the hospital, or at home with a sibling who either has a chronic medical condition that puts them at risk or is a very young baby.
8. How can parents treat kids for these illnesses?
While each virus is different, many of the common respiratory ones respond to the same types of therapy, explains Dr. Murray. “If the COVID test is negative, most of the time parents just need to make sure that the baby or child is OK—and that their breathing is OK—and provide supportive care,” Dr. Murray says. They should make sure their children are well-hydrated, and give them over-the-counter medicines, like ibuprofen or acetaminophen, if they have a fever, he adds. “The vast majority of kids are going to do fine with that.”
Murray says. They should make sure their children are well-hydrated, and give them over-the-counter medicines, like ibuprofen or acetaminophen, if they have a fever, he adds. “The vast majority of kids are going to do fine with that.”
If their symptoms continue, parents need to talk to the health provider again, he adds.
9. How can parents help their kids to stop coughing?
“If they're above age 1, we recommend giving a teaspoon of honey, which has been shown in clinical trials to actually help with cough,” says Dr. Dias. “They usually cough the most when they're sleeping because they're lying flat, and that position disturbs the child from sleep.”
For children ages 1 and older, she also advises putting two pillows under the child’s head or raising the head of the bed so they are sleeping on an angle “so that gravity can help phlegm flow downward,” she adds.
10. Why are COVID-19 and flu vaccines important for kids and when should they get them?
“Vaccination is really the number one tool that we have for preventing many infectious diseases,” says Dr. Dias. When so many viruses are circulating, it can reduce confusion, she adds.
Dias. When so many viruses are circulating, it can reduce confusion, she adds.
The COVID-19 vaccine followed by a bivalent booster shot decreases the risk of hospitalization and death, and children ages 6 months and older can get vaccinated anytime. For influenza, however, the CDC recommends getting the flu vaccine before the end of October, although it’s still available and recommended after that. (Some children ages 6 months through 8 years will require two doses of the flu vaccine.)
While the flu shot is not always a perfect match for the predominant strain in a given year, it’s a strong tool for preventing an infection that can be deadly in some children. Also, it can mean the difference between mild and severe illness in a child who gets sick despite getting the vaccine.
There is no vaccine yet to prevent RSV infection, but several are in development.
If possible, Dr. Murray encourages families to schedule a wellness checkup to assess their children’s overall health and to update them on immunizations they may have missed during the pandemic, including vaccinations against measles, pertussis (whooping cough), and other diseases.
“When the vaccination levels in the population go down, these viruses do come back,” says Dr. Murray. He adds that measles, in particular, is “super contagious and kids can get quite sick from it.”
11. How do you keep children healthy without worrying them?
Mental health issues among kids are a major concern, says Dr. Murray. Parents should avoid piling new worries on top of any anxiety kids may already have about school. “The primary mission now is to figure out how to do things as safely as possible, because it’s important for everyone’s mental health.”
He recommends having conversations about mental health or anything kids have on their minds. “You can also take time to talk at dinner, go for an evening walk, or go for a hike on the weekends," he says. "Spend time talking to your kids about how they're doing.”
As far as the infections, Dr. Dias says most kids will do well. “Viruses have always been out there, and kids are generally resilient in fighting infections, even when they are hospitalized,” she says. “But vaccination and regular checkups with the pediatrician can provide the support needed to help your kids get better.”
“But vaccination and regular checkups with the pediatrician can provide the support needed to help your kids get better.”
If a child falls ill - articles from the specialists of the clinic "Mother and Child"
Archegova Galina Altafovna
Gastroenterologist, Gastroenterologist for children, Nutritionist
MD GROUP Clinical Hospital
It is known that children in the first months of life rarely get sick, for example, SARS. This is due not only to the fact that they do not visit public places, but also to the fact that there are protective factors in their blood that were passed on to them by their mothers. Gradually, the level of these factors decreases, and the likelihood of respiratory disease, respectively, increases. nine0003
If a child of the first 6 months of life has a viral infection, which theoretically should be protected by immunity inherited from the mother, then this is a situation that goes beyond the norm. Therefore, in this case, you should immediately consult a doctor. Even if the disease is mild, only in the form of a runny nose and sneezing.
Therefore, in this case, you should immediately consult a doctor. Even if the disease is mild, only in the form of a runny nose and sneezing.
If a child of the second half of life who already “has the right” to get sick falls ill, then in cases of a mild form of the disease with a temperature within 38 °, with minor symptoms of a cold, one can independently, based on one’s own experience, begin treatment using certain means. nine0003
It has been known for many years that one of the protective factors, interferon, is weakly secreted at temperatures below 38°C, which can weaken the immune response in general. Therefore, there is no reason to consider a decrease in temperature in all cases as necessary. In addition, the use of antipyretics can lead to side effects.
When the temperature rises, the skin vessels dilate, which allows the body to balance heat production and heat loss. Therefore, it is not necessary to wrap up a feverish child, to cover him with blankets, this can only impede heat transfer. There is no need to be afraid that the temperature will “roll over the top”, will rise indefinitely. In the vast majority of patients, the temperature does not exceed 39°. However, at higher temperatures, the heat output may not match its products.
There is no need to be afraid that the temperature will “roll over the top”, will rise indefinitely. In the vast majority of patients, the temperature does not exceed 39°. However, at higher temperatures, the heat output may not match its products.
Such a situation - it is called a malignant temperature - is extremely dangerous. It is not difficult to recognize it - while the surface of the child's body acquires a motley "marble" color, the skin, especially the hands and feet, remains cold despite the fever. In these cases, it is necessary to rub the skin vigorously until it turns red and give an antipyretic. A child with a fever should be put to bed and provided with plenty of fluids to prevent excessive fluid loss. nine0003
If a child is ill, the first thing to do is DON'T PANIC. Most problems are born out of panic. Call your pediatrician immediately.
Before he arrives, take a temperature measurement.
Make sure that the room where the child is located is ventilated and the air is fresh. Don't forget to increase your drinking. Experts note that if the child drinks enough, then you can not be afraid that the temperature will pose a danger to him.
Don't forget to increase your drinking. Experts note that if the child drinks enough, then you can not be afraid that the temperature will pose a danger to him.
There is a very small group of children who, in response to any infection, overreact, that is, they immediately develop a high temperature, heart and lung failure, loss of consciousness, convulsions immediately occur. Therefore, if a child's temperature creeps up, despite the measures you take, the bill goes to hours and minutes. nine0003
The easiest and best way out in this situation is to call an emergency or a pediatrician and hospitalize the baby in a hospital, where all the necessary examinations will be performed and treatment prescribed, and, most importantly, the child will be under the supervision of a doctor around the clock, since the children have a condition can get heavy in a matter of hours.
As the head of the children's consultative and diagnostic center of the Perinatal Medical Center, which includes not only a polyclinic, but also a boxed department for infants and older children, I categorically do not advise you to go to hospitals yourself, “choosing” a hospital. For this, there is emergency care, which, in accordance with the diagnosis, will take the child to a specialized medical institution, depending on the availability of vacant places in it. nine0003
For this, there is emergency care, which, in accordance with the diagnosis, will take the child to a specialized medical institution, depending on the availability of vacant places in it. nine0003
I would like to note that the conditions of his stay in the hospital are of great importance for a child, especially at an early age. Individual wards - boxes, round-the-clock stay of a mother with a child, everything necessary for a comfortable stay, modern materials in interior decoration, colors of walls and floors - taking into account the favorable psychological impact on the child - all this is available in the rehabilitation department of the Perinatal Medical Center. In addition, the uniqueness of this department for Moscow lies in the fact that the Center has not only a children's hospital, but also a polyclinic children's department, and specialized traveling children's teams. Thus, the principles of continuity and phasing are fully respected. In the event of a critical situation, a team of pediatricians goes to provide medical assistance and, if necessary, the child is transported to the children's boxed department. Therefore, it is not for nothing that the medical staff of the PMC departments is considered one of the most qualified, because they have to deal with the most difficult situations. nine0003
Therefore, it is not for nothing that the medical staff of the PMC departments is considered one of the most qualified, because they have to deal with the most difficult situations. nine0003
Of course, a child's illness is a misfortune. But faith in the successful resolution of the situation, in the child’s own strengths and strengths, and the professionalism of doctors can work wonders. The purpose of our article is not to intimidate future and current parents, but to warn. Convince to be as attentive as possible to the health of the child. After all, as you know, forewarned is forearmed. So, if you notice even minimal deviations in the condition of the baby, then do not treat yourself, consult your doctor. nine0003
For every family, the most important thing in life is the happiness and health of their child. But, unfortunately, children often get sick. We sincerely wish you and your children good health, but if the child gets sick, try to "pull yourself together" and do not panic! Your task is to help your child as much as possible! Emotions should fade into the background.
Make an appointment
to the doctor - Archegova Galina Altafovna
Clinical Hospital MD GROUP
GastroenterologyPediatric gastroenterology
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
nine0002 Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Children's Clinic KG "Lapino" in New Riga (branch)Clinic "Mother and Child" KuntsevoClinic "Mother and Child" SavelovskayaClinic "Mother and Child" South-WestClinic "Mother and child" NovogireevoAll directionsKinesiotherapy for childrenSpecialist consultations (adults)Specialist consultations (children)Massage / manual therapy for childrenTherapeutic research
nine0002 01.
Kinesiotherapy for children
02.
Consultations of specialists (adults)
03.
Consultations of specialists (children)
04.
Massage/ manual therapy for children
05.
Therapeutic studies
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
When the child is ill. First Aid
Dear parents!
If the child becomes acutely ill, the body temperature rises, an injury, electrical injury, burn, poisoning, vomiting, breathing difficulties and other cases of a threat to the child's health occur, you must immediately call an ambulance!
Next, pay attention to the memo, perhaps you can provide first aid, which will help the child in his condition. nine0003
nine0003
From the moment a child begins to walk, he exposes himself to a number of dangers: bruises, dislocations, burns. In this regard, the task of parents is to eliminate all sources of danger, since a child left unattended is more prone to accidents. If an accident took place, then you need to know and remember about the first aid that you can provide to your baby before the doctors arrive.
Foreign body in the eye
Do not try to remove chips, glass shards and other objects embedded in the eyeball. Apply a sterile bandage over the eye.
Urgently call an ambulance!
Foreign body in the nasopharynx
Do not try to remove a foreign body stuck in the nasopharynx - you can push it deeper.
Urgently call an ambulance!
Foreign body in ear
Don't try to remove a foreign body stuck in your ear - you can push it deeper. If an insect gets into the ear, inject a few drops of warm vegetable or vaseline oil, cologne or vodka into the ear.
Urgently call an ambulance!
Nosebleed
For nosebleeds, move the child to an upright position. Put cold on the bridge of your nose. nine0003
Urgently call an ambulance!
Eye burns
Rinse eyes with plenty of cold water.
Urgently call an ambulance!
Skin burns
Immediately apply cold to the burned surface - a bubble with ice, snow or cold water. You can wash the burnt surface with a stream of cold water. Do not try to clean the surface of the burn, forcefully separate adhered clothing, open blisters, apply any creams, ointments or powders, except those specifically designed for burns. nine0085
Apply a sterile bandage to the burn.
Urgently call an ambulance!
Burns of the esophagus
In case of burns of the esophagus with a caustic liquid - acid or alkali, one should not induce vomiting or give the child plenty to drink - this worsens his condition. You just need to rinse your mouth with clean cold water.
You just need to rinse your mouth with clean cold water.
Urgently call an ambulance! nine0003
Poisoning
The actions of the first aid provider depend on the type of poisonous substance. You can determine what the victim was poisoned by by empty vials, bottles, medicine packages, as well as by the smell from the victim’s mouth.
For acid and alkali poisoning
Don't let your child drink! In no case do not use acid or alkali solutions to neutralize the drunk substance! Don't try to induce vomiting. nine0003
Urgently call an ambulance!
In case of poisoning with drugs and other substances (not caustic acids or alkalis!)
If the child is conscious and able to swallow, give him plenty of clean water. Do not inject any neutralizing substances inside. If the child is unconscious, it is necessary to monitor the cleanliness of his respiratory tract and oral cavity by turning his head to one side. Tilt the victim's head back. Cover the lips of the victim with your mouth, while pinching the victim's nose with your fingers. Exhale into the victim's mouth with a frequency of 1 time for 6-7 chest compressions. Artificial respiration should be continued even after the victim has spontaneous respiratory movements. nine0003
Urgently call an ambulance!
High temperature
You can lower the temperature as follows:
Give the patient an age dose of aspirin or paracetamol, Panadol. Make sure you drink plenty of soft drinks. Free the child from excess clothing. Make sure that the room temperature does not exceed 15 degrees. In extreme heat, wiping with a sponge dipped in slightly warm water helps. nine0003
Urgently call an ambulance!
Eye injury
Apply a sterile dressing if the wound is open, do not try to remove foreign bodies! Cold to the injured eye.
Urgently call an ambulance!
Chest and abdomen injury
With a closed injury - cold, with an open one - a sterile bandage. Do not give your child painkillers. nine0003
Urgently call an ambulance!
Bone and joint injury
Apply cold to the injured area as soon as possible, make a tight bandage.
Urgently call an ambulance!
Trauma of the facial skeleton
Cold on the face.
Urgently call an ambulance!
Spinal injury
Lay the child on a flat, hard surface. If there is no concomitant damage to the organs of the chest and abdomen.
Urgently call an ambulance!
Trauma of the skull
Lay the child on a flat hard surface, turn his head to one side (if there is no spinal injury!) and monitor the airway - free the mouth and nasopharynx from vomit. The life of a child depends on the patency of the airways. Put cold on your head. nine0003
Urgently call an ambulance!
Traumatic amputations
Apply a sterile dressing to the wound. In case of arterial bleeding (scarlet blood spurts), apply a tourniquet above the wound for no more than 2 hours. ATTENTION! Replantation (engraftment) of the severed part of the limb is carried out within 12 (in some cases up to 20) hours from the moment of traumatic amputation. Engraftment is possible only if the severed limb is properly stored until the victim is admitted to a medical institution. Put the cut part into a dry, undamaged and clean plastic bag, tie it up and place it in the second bag. Ice, snow or cold water should be placed at the bottom of the second bag. The cut off part must not come into contact with ice, snow or water. nine0003
Urgently call an ambulance!
snakebite
Immediately suck the poison out of the wound with your mouth. Suck out the contents of the wound for 10-15 minutes, spitting it out. Before that, open the wounds by squeezing the skin folds in the bite area. the procedure is safe, since snake venom that gets into the mouth and stomach does not cause poisoning.