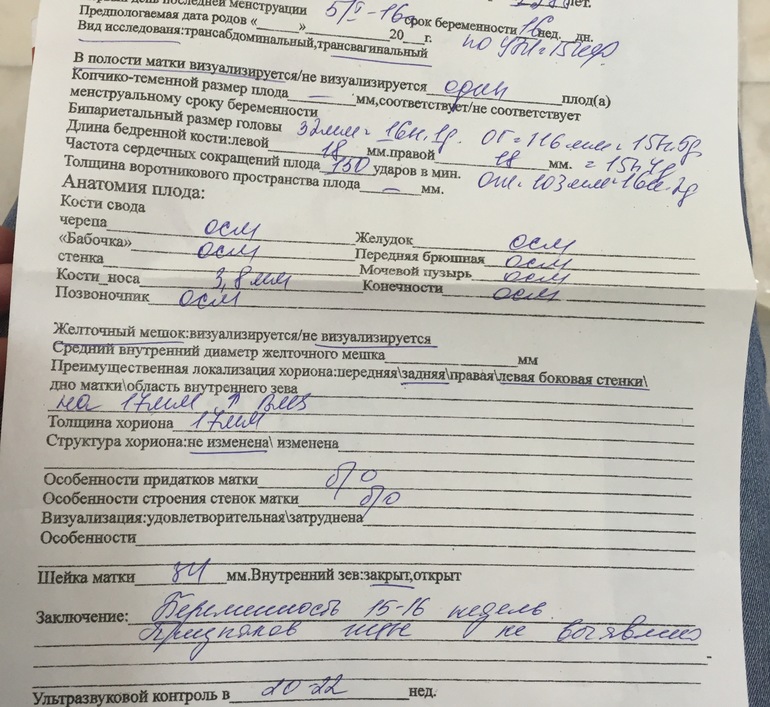
Cervix closed at 41 weeks
Cervical ripening methods when induction is part of the birth plan | Your Pregnancy Matters
There are many reasons moms-to-be might be interested in or need induction of labor. Patients might have decided that they:
- Are tired of being pregnant (and have made it to at least 39 weeks).
- Want to avoid a certain delivery date, such as a holiday. Alternatively, some patients have determined that some dates are favorable and want to deliver their babies on those specific dates.
- Need to arrange delivery around a loved one’s schedule. We’ve had women ask to be induced so their parents can arrange travel from overseas to be with them or a partner can be furloughed from the military and attend the delivery.
If your pregnancy is uncomplicated, it is best to wait to go into natural or spontaneous labor. In some situations, induction will be necessary because a complication has arisen that warrants delivery, such as preeclampsia or going significantly past your due date.
Your cervix plays a big role in determining the success of induction of labor. During pregnancy, the cervix usually is firm and stiff enough to help hold the baby in the uterus. That’s a good thing for most of the pregnancy. But in the final days or weeks before delivery, the cervix starts to soften and open up. Basically, it’s getting ready for labor. When this happens, we say that the cervix is becoming “favorable.”
If your cervix is has already started the process of softening and dilating, any method for induction has about an equal chance of success. But what if your cervix isn’t ready? If your cervix is still closed and firm, it might need some help before induction of labor is started. Your doctor may use the words “unripe” or “unfavorable.” In our experience, many women and their families don’t understand this part of process. In the following segment, we’ll describe commonly used methods to ripen the cervix so you and your family know what to expect.
Types of induction
During cervical ripening, we can use various methods to start preparing the cervix for contractions.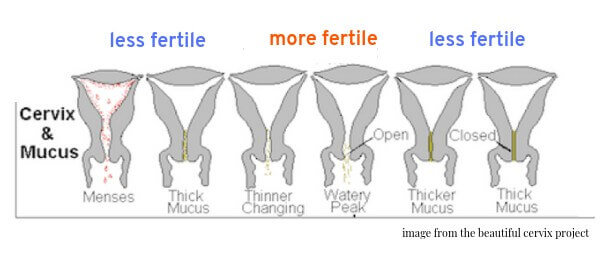
1. Mechanical cervical ripening
To say that we are mechanically ripening the cervix means that we are forcibly dilating it. A Foley catheter is typically used to drain urine from the bladder. The tip of the catheter has a balloon, which holds about 2 TBSP of water. If we place the tip of the Foley into the cervix and inflate the balloon, the balloon will push the cervix open over time.
Protocols vary, and the bulb will either be left inside the cervix for at least 12 hours or until it falls out. The cervix can also be dilated just by an examination by your provider. The finger can gently dilate the cervix and separate the membranes from the uterine wall. This is called “membrane stripping.” It may be uncomfortable for the patient, but it can be effective.
2. Medical cervical ripening
Medications also can be given to help induce softening and dilatation of the cervix. Oral or vaginal suppository drugs, such as misoprostol and other prostaglandins, are also commonly used to ripen the cervix. These medications come in different formulations, and the type you receive typically depends on what your doctor is familiar with and what is available at your delivery hospital.
These medications come in different formulations, and the type you receive typically depends on what your doctor is familiar with and what is available at your delivery hospital.
Misoprostol comes in tablets that can be given by mouth or placed directly against the cervix. The medicine will be absorbed and will start softening your cervix over time. After several hours and several doses, you might end up 2 or 3 cm dilated, and, if you’re lucky, perhaps in early labor.
Other common formulations of medical induction agents include endocervical gels and vaginal inserts. They are similarly safe and effective and tend to be well tolerated by most patients. However, all of these medications can sometimes trigger too much uterine activity. If your doctor is worried about this, she may choose a mechanical form of cervical ripening.
3. Combination methods
In some protocols for cervical ripening, the mechanical and the medical agents are used simultaneously. Some studies have shown that using both methods at the same time is safe and can achieve the same result in less time.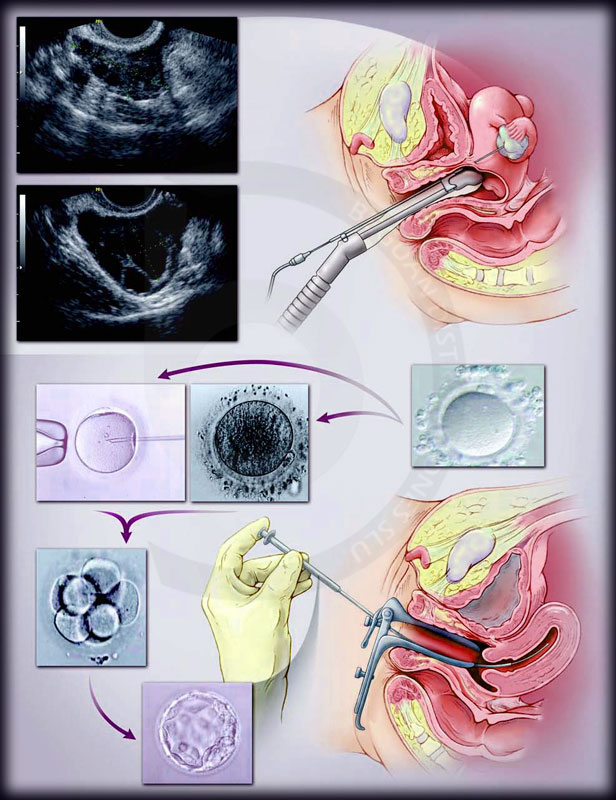
Other considerations in cervical ripening
Misoprostol and other prostaglandins are not used for cervical ripening in term pregnancies with a prior cesarean birth or other prior major uterine surgeries, such as extensive myomectomies. These patients face an increased risk for uterine rupture.
You may not need cervical ripening if your cervix is already dilated, or if you’ve had a vaginal delivery before. If you do require cervical ripening before your induction of labor, we want you to understand that it is just the first step to having your baby. During the process, you may sleep some of the time and feel frustrated that not a whole lot is happening. It can be slow-going and pretty boring. If you are a low-risk patient, you might be allowed to have a light meal through the process.
We understand that patients and families are in a hurry to get the new baby here! But be patient. At the end, we hope to have a cervix that is ready for labor.
Join our mailing list to stay current on pregnancy news. Subscribe today.
Subscribe today.
When your baby is overdue...
When your baby is overdue... | Bounty Parents Email Address: Password:Show password
Remember MeForgot password?
Not a member? Join Now!
First Name: Last Name: Email Address: Password:Show password
Are you pregnant?
Yes No
Due Date:By clicking Join Now, you agree to receive Marketing communication and to our Terms of Use, and Privacy Policy
Conditions apply, see https://www.bountyparents.com.au/for-you-bugaboo-competition/. Commences 01/06/2022. Ends 11:59 AEST/AEDST on 31/05/23.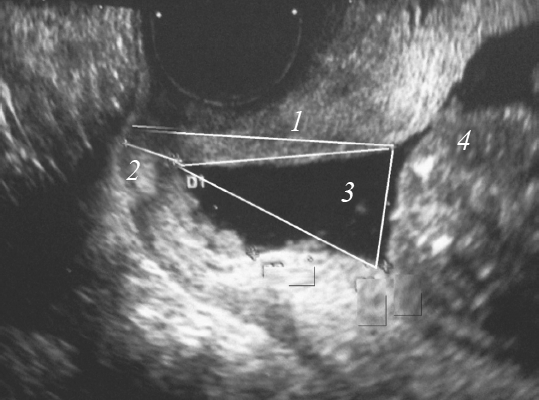 AU residents 18+. Drawn at Are Media, Level 3, 54 Park St, Sydney, NSW, 2000 at 11:00am AEST/AEDST, 1 monthly draw (total of 12 draws) between 07/07/22 – 07/06/23, see full terms for draw schedule. Prizes: 1x Bugaboo Bee 6 base with a black chassis and a yellow canopy, valued at up to $1,169 AUD. The Promoter is Are Media Pty Limited (ABN 18 053 273 546) of 54 Park Street, Sydney, NSW 2000. Authorised under permit numbers: NSW: TP/00018, ACT: TP/00721, SA: T22/555.
AU residents 18+. Drawn at Are Media, Level 3, 54 Park St, Sydney, NSW, 2000 at 11:00am AEST/AEDST, 1 monthly draw (total of 12 draws) between 07/07/22 – 07/06/23, see full terms for draw schedule. Prizes: 1x Bugaboo Bee 6 base with a black chassis and a yellow canopy, valued at up to $1,169 AUD. The Promoter is Are Media Pty Limited (ABN 18 053 273 546) of 54 Park Street, Sydney, NSW 2000. Authorised under permit numbers: NSW: TP/00018, ACT: TP/00721, SA: T22/555.
Your due date has come and gone and while an induction may not be part of your birth plan, here’s what to expect if your baby needs a hurry-up.
by Fiona Wright | 4 March 2022
Once your due date has passed, you’ll notice every little twinge and minor ache, looking for a sign you might be finally about to meet your bub.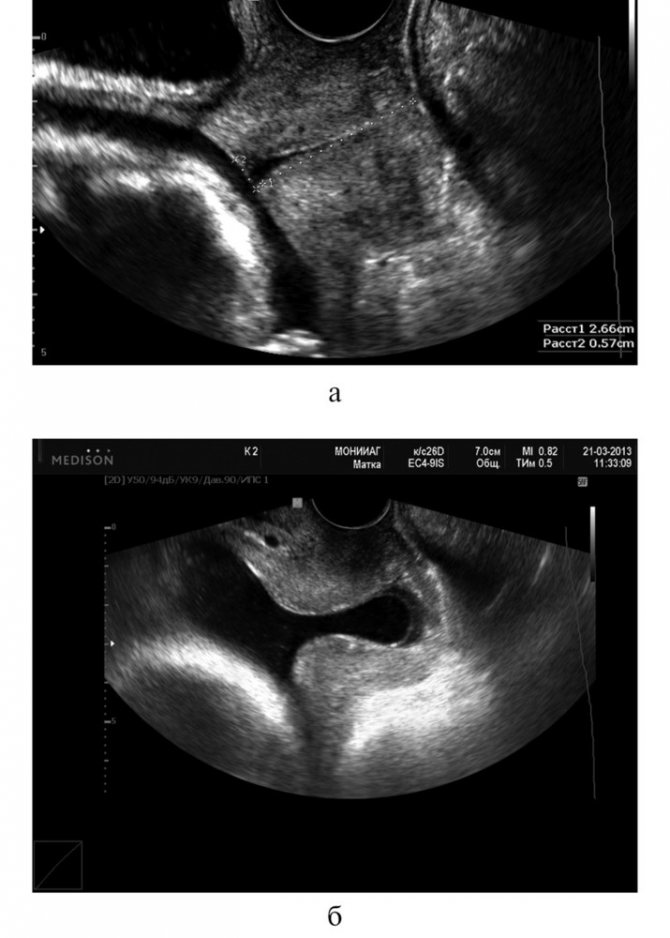
But for many mums, nature needs a helping hand to set off labour, with of the 80% of women that labour (20% opt for an elective caeserean), 43.9% of them have their labour started or sped up. The most common method is via the drug Syntocin which promotes uterine contraction.
Here’s what might happen if your doctor – or you – suggests getting things moving with an induction.
Why the hurry?
The most common reason for having an induction is being overdue. An induction is when we don’t wait for the normal onset of labour and we get the labour going with various so-called artificial means.
Inductions can be done for medical reasons relating to the baby’s – or mum’s – health, including being overdue, not growing properly or the mother having high blood pressure.
Typically, once you’ve reached 41 weeks your doctor will discuss the possibility of undergoing an induction by 10 days to two weeks after your due date.
At 41 weeks, your doctor will discuss the possibility of an induction. (Image: Getty Images)
(Image: Getty Images)
Preparing for action
To get an induction going, you need an open cervix. If the cervix is open, you can proceed to do an induction. But if the cervix is not open enough, you’ll need an initial preparatory step, otherwise the induction is less likely to work.
One way is to have a vaginal sweep of the membranes. Your midwife or doctor inserts a finger just inside your cervix and makes a circular motion to separate your baby’s membranes from the cervix. This encourages the release of prostaglandins to help open the cervix. Or, once in hospital, a prostaglandin gel may be inserted into your vagina.
It’s hoped this will soften your cervix. Sometimes it gets labour going or a balloon catheter can be inserted into the vagina where it sits above the closed cervix, gradually opening it overnight.
Game on!
The most common methods for induction involve artificially rupturing the membranes or a Syntocinon drip.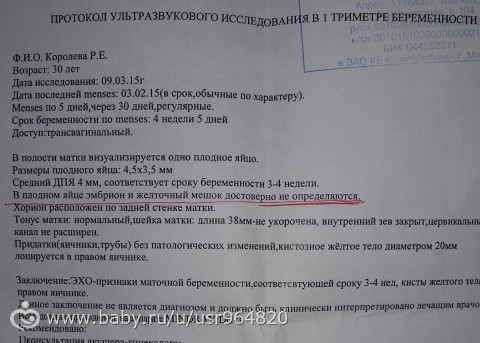 Administered via intravenous drip, Syntocinon is a drug that’s identical to oxytocin, the natural hormone that causes contractions. In the case of inductions, the amount given is gradually increased until labour is fully established.
Administered via intravenous drip, Syntocinon is a drug that’s identical to oxytocin, the natural hormone that causes contractions. In the case of inductions, the amount given is gradually increased until labour is fully established.
If your labour slows down, an intervention known as ‘augmentation of labour’ may be used to speed up or increase the intensity. This process involves the same techniques as induction but is done after labour has started on its own.
A ‘normal’ labour is medically defined as one that’s spontaneous and unassisted, is between 37 and 42 weeks of pregnancy and where the baby’s head is in an anterior position – upside down and facing backwards. It lasts between four and 24 hours, requires no artificial intervention and has no complications.
If an induction is required, it won’t be long before the wait is over and you meet your baby for the first time.
NATURAL METHODS
Keen to try other methods to kick-start labour? Try the following: drinking raspberry leaf tea, going for a brisk walk and stimulating your nipples may all help. Sex can also bring on labour – but don’t go for this option if your waters have already broken, as it can increase the risk of infection.
Sex can also bring on labour – but don’t go for this option if your waters have already broken, as it can increase the risk of infection.
Read This Next
RELATED TAGS: bounty, Motherhood, Parenting, Pregnancy Week 40
Fiona Wright
More From Bounty
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital of IDKClinic "Mother and Child" Entuziastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children's)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults
01.
Specialist consultations (adults)
02.
Specialist consultations (children)
03.
Laboratory of molecular genetics
04.
General studies
05.
Procedure cabinet
06.
other gynecological operations
07.
Telemedicine for adults
08. examinations
09.
Adult ultrasound examinations
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
EP stories after KS
Hello!
My name is Masha, I am 33 years old.
And this is my story of the fourth birth!
It so happened that the first three were delivered by caesarean section. All my previous pregnancies, all the gynecologists with whom I talked convinced me that it was impossible to give birth on my own after a cesarean section !!! By the fourth pregnancy, I had already lost hope.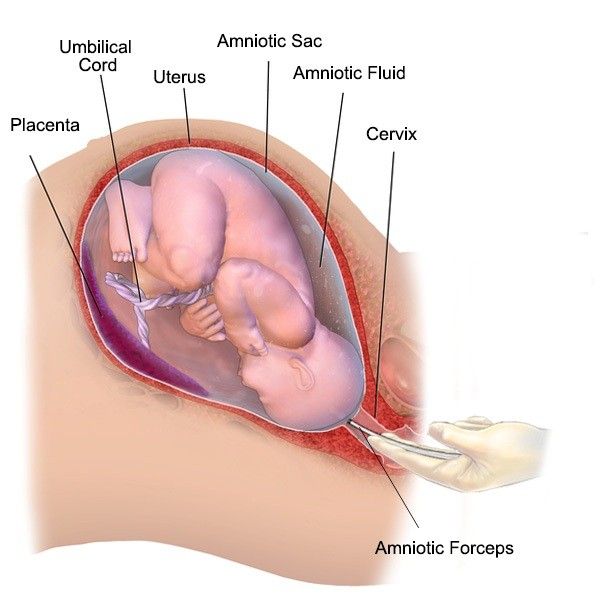 But then I came across articles of girls who gave birth after one and even after two caesarean sections. I began to search, and found out that there are maternity hospitals specializing in natural childbirth after a caesarean section!!! And they told me that everyone is the same!
But then I came across articles of girls who gave birth after one and even after two caesarean sections. I began to search, and found out that there are maternity hospitals specializing in natural childbirth after a caesarean section!!! And they told me that everyone is the same!
I asked the antenatal clinic for a referral to the 16 Maternity Hospital. And then miracles began!
The first thing that struck me was the attitude towards women!!! Before that, in other pregnancies, for various reasons, I was in 17 and 10 maternity hospitals, and that attitude was formal, like a piece of paper - I came, got up, sat down, everything was ordered. And here!!! They spoke to me like a person, not just, but affectionately !!!
Despite the fact that at the time of my arrival there was an influx of patients and no one was abandoned!!! Everyone got attention. And so, at the examination, I hinted at natural childbirth. Tatyana Igorevna, the doctor who received me, although she was surprised, did not refuse! She explained that this is possible if my health condition allows it!
And here it is HOPE!!!
The next day I was scheduled for an examination. There was a commission headed by the head of the department. She said that they would conduct all the necessary tests, assess the condition of the scar, the child, and after that they would say whether it was possible. After the examination, I was informed that everything is possible, provided that labor begins on its own. At that time it was already 39 weeks. The doctor who was leading me at that time, Anna Anatolyevna, discharged me at 40 weeks to wait for the onset of labor or to come back at 41 weeks. All week we tried hard to start this very activity, but it didn’t work out and at 41 weeks I returned to the 16 Maternity Hospital.
There was a commission headed by the head of the department. She said that they would conduct all the necessary tests, assess the condition of the scar, the child, and after that they would say whether it was possible. After the examination, I was informed that everything is possible, provided that labor begins on its own. At that time it was already 39 weeks. The doctor who was leading me at that time, Anna Anatolyevna, discharged me at 40 weeks to wait for the onset of labor or to come back at 41 weeks. All week we tried hard to start this very activity, but it didn’t work out and at 41 weeks I returned to the 16 Maternity Hospital.
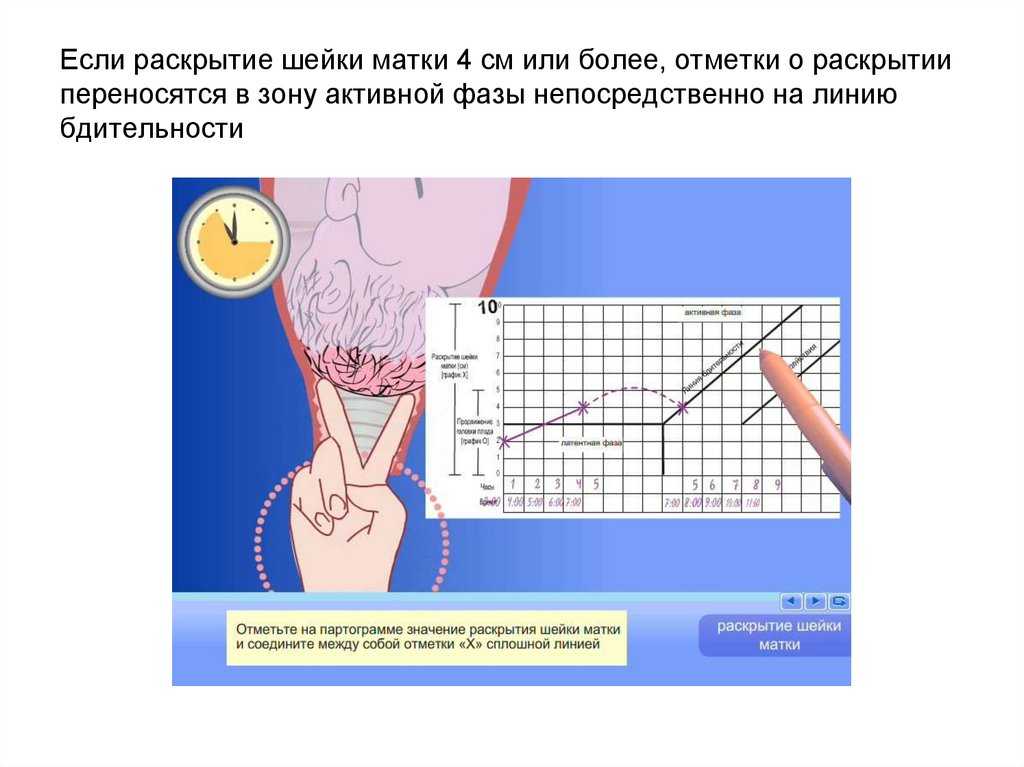
After the examination, they said that the cervix had become smaller, but not yet ready, but still they gave time until Friday, so that after the examination they decided whether it was worth waiting for more.
On Friday, the neck turned out to be not ready again, but it became even shorter, it missed one finger, which was not enough. It was decided to wait for Monday and if a miracle does not happen, then on Tuesday PKS.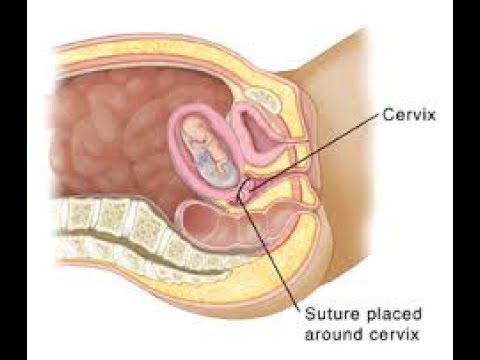
And then on Friday evening, or rather, even on Saturday night, I felt the first contractions. The fact that I was delighted to say nothing. Realizing that this is only the beginning, I began to wait for regularity. The contractions went on all night, but there was no regularity from 10 to 5 minutes. In the morning they took me to the maternity ward to make sure everything was fine with the baby. They checked the water, did a CTG and left her in the prenatal ward. All indicators were normal, but the neck is closed!!! The doctor Chergaziya Rita Givievna, who received me, warned that they would monitor the condition, and if something suddenly went wrong, there would be an emergency caesarean section, and yet there was still hope. I was advised to tune in, and I did it to myself that I was giving birth !!! I spent the whole day in the ward, the contractions were from 8 to 5 minutes. At 18 o'clock they looked at me, there was no dilatation, but according to the CTG everything was fine, after examining the contractions went more intense after 3 minutes. At 3 am on Sunday, there was no opening, but the neck completely smoothed out from that time on, time stopped for me, the contractions went on almost without a break on CTG, it became impossible, I went to lie down in the shower, it was easier to bear the pain there. At 6 in the morning they came for me and took me to the delivery room, they did a CTG, it was painful, and after that I began to grieve. Irina Edikovna came running to my screams, who told me the opening had begun and this was the happiest news. At that moment I was in semi-consciousness, but through the state I remember that my bladder was pierced and I heard the cherished phrase - “full disclosure”. There was a large team around, they gave me a mask with nitrous oxide and told me not to push yet, however, as it turned out, this was the most difficult! I didn't really understand what was going on. I heard the voice of Rita Givievna, who picked up a position for me to try, followed the seam, told me how to push, and everything was like in a dream.
At 3 am on Sunday, there was no opening, but the neck completely smoothed out from that time on, time stopped for me, the contractions went on almost without a break on CTG, it became impossible, I went to lie down in the shower, it was easier to bear the pain there. At 6 in the morning they came for me and took me to the delivery room, they did a CTG, it was painful, and after that I began to grieve. Irina Edikovna came running to my screams, who told me the opening had begun and this was the happiest news. At that moment I was in semi-consciousness, but through the state I remember that my bladder was pierced and I heard the cherished phrase - “full disclosure”. There was a large team around, they gave me a mask with nitrous oxide and told me not to push yet, however, as it turned out, this was the most difficult! I didn't really understand what was going on. I heard the voice of Rita Givievna, who picked up a position for me to try, followed the seam, told me how to push, and everything was like in a dream.