Cervical pain pregnancy
Why It Happens and What to Do About It
Causes of vaginal pain during pregnancy
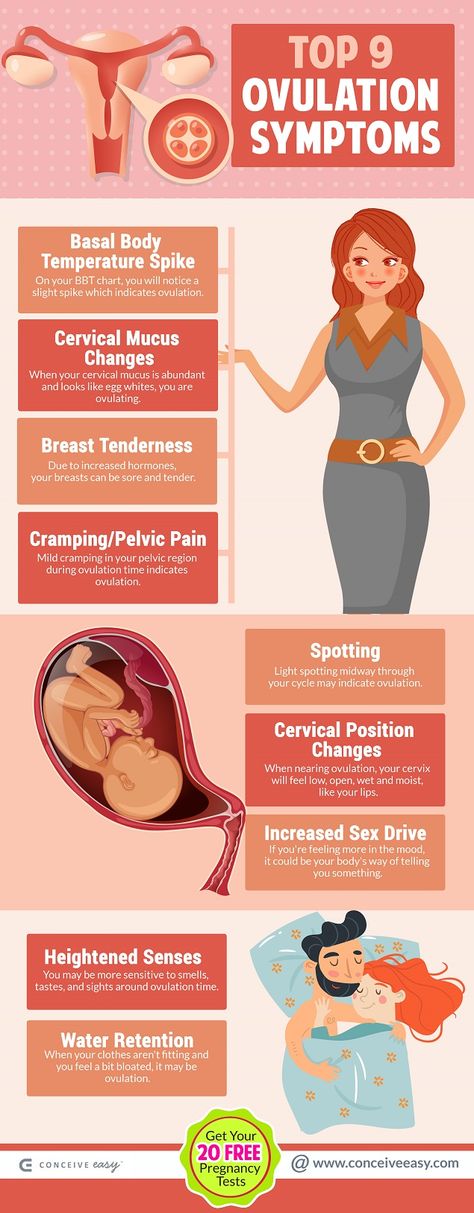
A growing fetus, dilation of the cervix, increased blood flow to the vagina, and fungal infections can all contribute to vaginal pain during pregnancy.
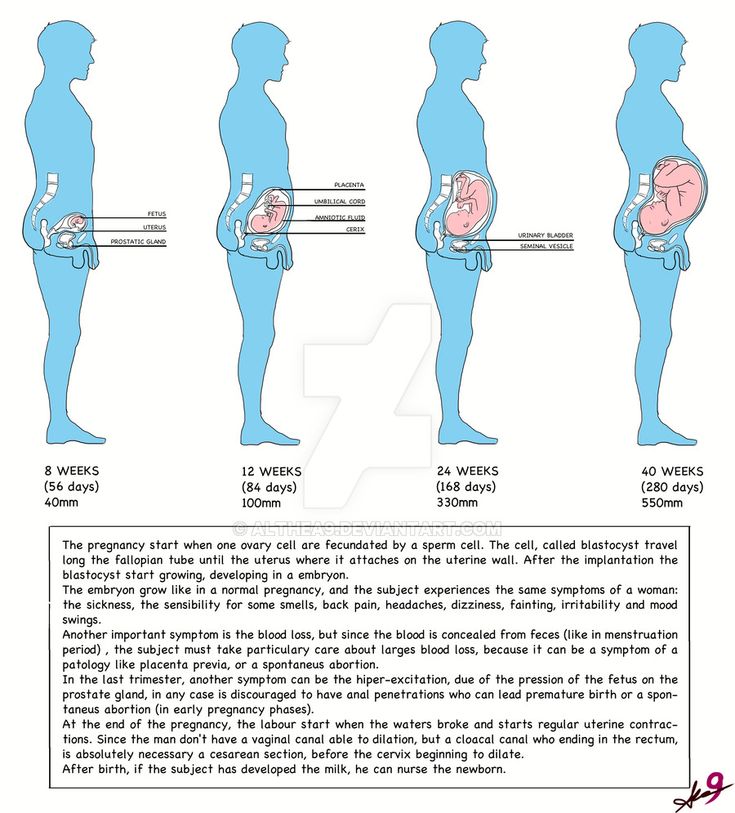
Growing fetus
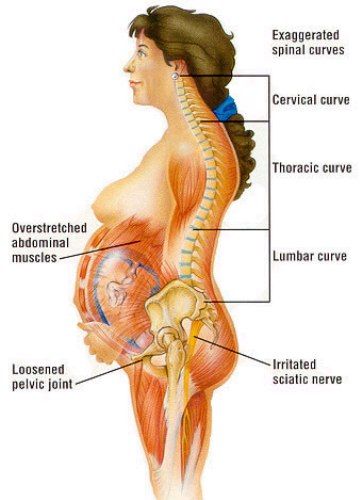
As your baby and your uterus grow, your pelvic ligaments stretch to accommodate the extra weight. When ligaments and vaginal muscles are overstretched, it can cause a sharp, shooting pain. If you’re already feeling vaginal pain in the first trimester, though, be sure to consult your doctor.
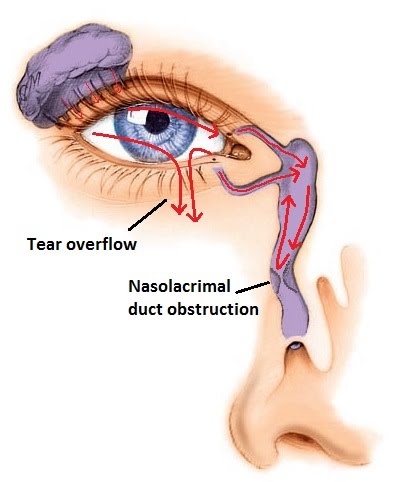
Dilation of the cervix
Dilation refers to the eventual opening of your cervix. Occasionally, cervical dilation is to blame for sharp, shooting vaginal pains in the final stages of pregnancy. This is a perfectly normal process that helps the body prepare for labor and delivery. But should the pain present in the lower abdomen, consult a doctor right away.
Take a quiz
Find out what you can do with our Health Assistant
During labor, uterine contractions open the cervix while the baby moves into the proper position. Effacement (when the cervix stretches and thins) and dilation allow the baby to pass through the birthing canal. This happens near the end of the third trimester, but varies with each individual. Some people start to efface and dilate over several weeks, and others shortly before the baby is born. First-time moms might not dilate until they’re in actual labor. An OB-GYN may check the cervix manually to monitor progress as part of prenatal care.
Increased blood flow
Increased blood flow to the vagina, accompanied by heavy vaginal discharge, are normal during pregnancy. Higher levels of estrogen and progesterone produce these changes. The increased overall volume of blood can cause vaginal discomfort or pain.
Fungal infections
If you’re experiencing vaginal pain during pregnancy and suspect it’s the result of a fungal infection, talk to your physician. The most common infection is candida (yeast infection), which is common during pregnancy because of compromised immunity.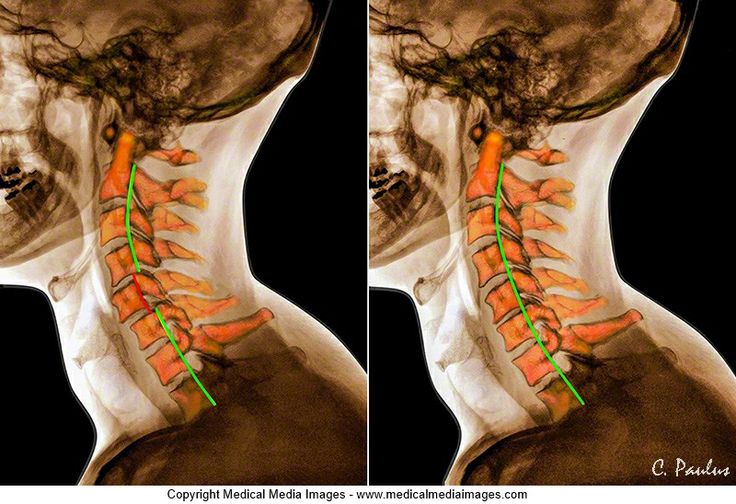
During pregnancy, recovering from candida might take longer than usual, as healthcare providers hesitate to prescribe cortisone medications. Consider treating it with an OTC antifungal cream or suppositories. Just remember to discuss this with your doctor first.
Lightning pain
Sometimes pain originating in the pelvic ligaments as they stretch to accommodate a baby can cause startling pain. It can be shocking enough to make some people think they’ve gone into labor. This is called lightning pain.
Some women naturally produce more relaxin and progesterone hormones, encouraging extra stretching and loosening of the ligaments. When round ligaments are stretched too quickly, it produces a sensation similar to that of lightning shooting through your crotch.
In certain cases, this does actually signal the start of labor. Constant back or lightning pain, contractions, or fluid leakage are all signs that the baby could be on their way. If you observe any of the above symptoms prior to 37 weeks, seek medical attention.
Ectopic pregnancy
Another potential cause of vaginal pain is ectopic pregnancy. This is when the fertilized egg implants anywhere other than the uterus. Most often, the fertilized egg will attach inside a uterine tube.
Ectopic pregnancies cannot be carried to term. The fertilized egg is unable to survive outside of the uterus. In certain cases, an ectopic pregnancy may cause the uterine tube to rupture, resulting in vaginal pain, bleeding, lightheadedness, and nausea. Seek medical help if you show any signs of ectopic pregnancy.
How to cope with vaginal pain during pregnancy
Vaginal pain occurs at some point during nearly every pregnancy. Besides pain medications (which should be approved by a doctor), there are a few different ways to find temporary relief:
- Lying on the left side to improve blood circulation and reduce vaginal pressure
- Sitting elevated feet, which could also decrease pressure levels and alleviate vaginal pain
- Elevating the hips to lessen cervical pain during pregnancy (which usually aggravates existing vaginal discomfort)
- Taking warm baths to soothe and relax achy muscles throughout the body
- Engaging in activities such as yoga or swimming to help boost blood circulation and strengthen muscles.

- Getting a doctor-approved pelvic massage that can simultaneously offer much needed pelvic support and a reprieve from vaginal pain during pregnancy.
When to see a doctor
Vaginal pain is a normal part of pregnancy for most people. Although a few minor lifestyle changes can help, a doctor is the best source of guidance, especially in later trimesters.
Additionally, there are various options available for treating vaginal pregnancy pain that you can research. Just remember that certain conditions, like infection or irregularities in the cervix, could potentially lead to miscarriage. That’s why it’s always a good idea to speak with a doctor about any questions, concerns, or possible treatments first.
Why It Happens, 5 Pain Remedies, and More
Lightning Crotch: Why It Happens, 5 Pain Remedies, and MoreMedically reviewed by Deborah Weatherspoon, Ph.D., MSN — By Chaunie Brusie on December 12, 2018
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Pain “down there”
At a party I once attended, one of my pregnant friends suddenly stood up from the table and stretched her arms above her head.
“Ugh,” she said, rubbing her side. “This kid is killing me. It’s like these shooting pains down there. Do you know what I’m talking about?” Boy, did I know what she was talking about.
I’ve never been one to have a comfortable pregnancy. Grateful as I am to have experienced pregnancy and grow our family, I’ve always struggled with the physical demands of pregnancy.
One of those demands definitely is the aches and pains that come along with growing a human being in your body, so let’s take a look at pain “down there.” It’s actually not crotch pain due to lightning.
It’s important to learn what causes it, when you should be concerned, how to stay comfortable, and when it’s a sign that you should head to the hospital.
Symptoms of lightning pain
Like my friend, I experienced a lot of pain down there and it can be confusing to know what’s happening exactly.
Is it normal? Is the pain a sign that you should be worried? There are a lot of questions that go through a pregnant woman’s mind other than, “I wonder if there’s any ice cream left?”
Lightning pain might actually feel like what it sounds like: lightning shooting in your pelvic area.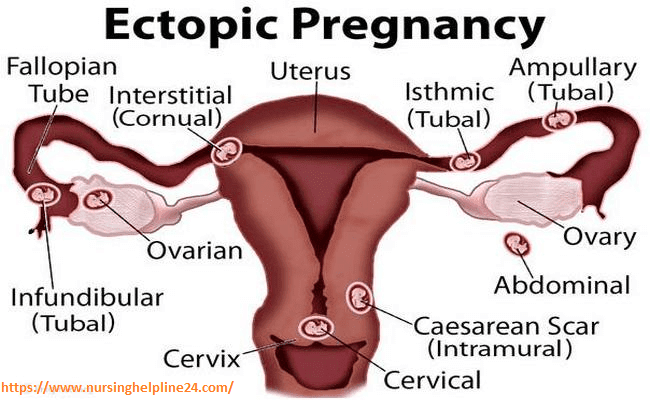
It almost feels like a little “zing” of pain, especially when you move or shift or feel the baby move or shift. It can come and go and might actually be quite uncomfortable.
Causes of lightning pain
Lightning pain is caused by the pressure and position of the baby as they descend into the birth canal to get ready for delivery.
The good news is lightning pain means you are getting closer to delivery day. The bad news is that lightning can happen for weeks before you actually go into labor.
With my second daughter, I had so much pain and pressure I felt like I was constantly walking around with a bowling ball between my legs. At that point, I was a good month before delivery.
Babies can change positions, but the lightning pain typically has two main causes:
- the actual pressure of the baby’s head on your cervix
- the baby putting pressure on nerve endings around your pelvis
Is lightning pain serious?
Most of the time, lightning pain isn’t serious, especially if it’s not interfering with your daily activities and isn’t accompanied by any other symptoms.
If you’re having pain or any other symptoms such as fever, increased or abnormal discharge, bleeding, or fluid leaking, schedule an appointment with your doctor. Be especially cautious if you’re under 37 weeks in your pregnancy.
5 tips for relieving the pain
There are a few ways you can help reduce your pain during pregnancy.
Stay active
It might sound counterproductive, but staying active will help a lot during your pregnancy.
Not only will it help ward off any excess pounds that might make you more uncomfortable, but it will help keep your joints open and flexible, which is important as they take on a heavier workload from your growing baby.
Focus on a mixture of cardio, weight training, and lots and lots of stretching, especially in the hip area. Get more tips on exercising in your third trimester.
Change up your workload
A large Norwegian study from 1995 found an increased prevalence of pelvic and lower back pain in pregnant women who performed physical jobs that involved a lot of twisting and bending or lifting.
A more recent study from Jordan in 2018 noted that long working hours were also associated with back pain in pregnant women.
If your job involves a lot of manual, hands-on labor or long hours, and you find yourself frequently in pain, consider talking to your boss.
See if you can take a reduced workload or do some temporary relocating to help you get through the rest of your pregnancy more comfortably.
Try a pregnancy massage
I had a lot of trouble with pain in my pregnancies. My massage therapist would apply counter-pressure to my back and sacral area, which helped ease some of those sore muscles that were pulling on the nerves around my hips. Relaxing those muscles really helped reduce the pain.
Just keep swimming
Sometimes, unfortunately, there really isn’t a lot you can do about the lightning pain. Your baby’s head and your cervix may be stuck together like glue.
I found that swimming a lot in the last weeks of pregnancy really made a difference, to just take some of the pressure off my poor body.
Wear a support brace
There are many different types of supportive garments and braces for pregnant women, but their function is usually the same. They help lift and support your belly to take some of that pressure off of your hips, joints, and yes, even cervix.
I used a BLANQI support tank top for my larger-than-life last pregnancy (I had polyhydramnios, so I was literally huge) and it made a big difference in my comfort and pain level.
Pain as a sign of labor
In some women, lightning pain is the first sign that they’re in labor. Some women can even feel their cervix as it dilates.
If you’re experiencing lightning pain and have any other symptoms like regular contractions, consistent backache, or any leaking of fluid, you might be in labor.
If you experience any of these symptoms and are under 37 weeks, be sure to seek medical treatment right away.
The takeaway
In general, lightning pain is a normal part of pregnancy and nothing to be too worried about.
If you’re concerned about your pain or it’s disrupting your day-to-day life, be sure to ask your doctor the following questions at your next checkup to rule out any other reasons for your pain.
- Will I need to be checked for dilation?
- Are there any signs of an infection?
- Can you tell if my baby is in the right position?
- Can you recommend some safe exercises I can do to help my baby get in the best position and help me be comfortable?
If everything checks out and you’re still experiencing lightning pain, you may actually want to congratulate yourself because your body is giving you a pretty clear sign that it’s getting ready to bring your baby into the world.
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing. She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on December 12, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Endresen EH. (1995). Pelvic pain and low back pain in pregnant women--an epidemiological study. Scandinavian Journal of Rheumatology, 24(3), 135-41.
ncbi.nlm.nih.gov/pubmed/7777823 - Gharaibeh A, et al. (2018). Prevalence of low back pain in pregnant women and the associated risk factors.
medwinpublishers.com/JOBD/JOBD16000157.pdf - Mayo Clinic Staff. (2016). Signs of labor: Know what to expect.
mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/signs-of-labor/art-20046184 - Pregnancy: labor and birth. (2018).
womenshealth.gov/pregnancy/childbirth-and-beyond/labor-and-birth
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 12, 2018
Written By
Chaunie Brusie
Medically Reviewed By
Deborah Weatherspoon, Ph.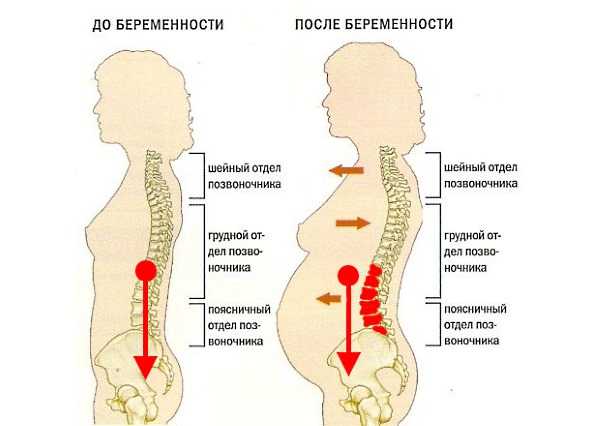 D., MSN
D., MSN
Share this article
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN — By Chaunie Brusie on December 12, 2018
related stories
What Do Different Types of Labor Contractions Feel Like?
Cervix Dilation Chart: The Stages of Labor
Why Vaginal Pressure During Pregnancy Is Totally Normal
Do’s and Don’ts When a Loved One Is Experiencing a Stroke
How to Deal with Butt Pain During Pregnancy
Read this next
What Do Different Types of Labor Contractions Feel Like?
Medically reviewed by Michael Weber, MD
If you’re a first-time mom, you might be wondering what contractions feel like. Here’s a guide to contractions and how to tell if you’re in labor.
READ MORE
Cervix Dilation Chart: The Stages of Labor
Medically reviewed by Carolyn Kay, M.
 D.
D.Ready to deliver and welcome your little one? Here’s a look at the stages of labor.
READ MORE
Why Vaginal Pressure During Pregnancy Is Totally Normal
Medically reviewed by Nicole Galan, RN
Many pregnant women experience vaginal and/or pelvic pressure. Here's why it happens and how to find relief.
READ MORE
Do’s and Don’ts When a Loved One Is Experiencing a Stroke
Medically reviewed by Seunggu Han, M.D.
A stroke can be life-threatening, so it's important to act fast. If you think a loved one is having a stroke, here's what you should and shouldn't do.
READ MORE
How to Deal with Butt Pain During Pregnancy
Medically reviewed by Janine Kelbach, RNC-OB
Many pregnant women report butt pain as a symptom during the third trimester.
 These treatment options will help you stay comfortable until delivery.
These treatment options will help you stay comfortable until delivery. READ MORE
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
A miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
11 Foods and Beverages to Avoid During Pregnancy - What Not to Eat
By Adda Bjarnadottir, MS, RDN (Ice)
Certain foods can be very harmful for pregnant women and their babies. This is a list of 11 foods and drinks that pregnant women should avoid.
READ MORE
Pregnancy Complications
Medically reviewed by Michael Weber, MD
Sometimes a pregnant woman’s existing health conditions can contribute to problems, and other times new conditions arise because of body and hormonal…
READ MORE
The Best Pregnancy Apps of 2020
These are the best iPhone and Android apps to find information, answers, tools, and tracking during your pregnancy.
 From scheduling doctor’s visits…
From scheduling doctor’s visits…READ MORE
Maintaining a Healthy Pregnancy
Medically reviewed by Stacy Sampson, D.O.
Pregnant people who eat well and exercise regularly along with regular prenatal care are less likely to have complications during pregnancy.
READ MORE
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2. 5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth.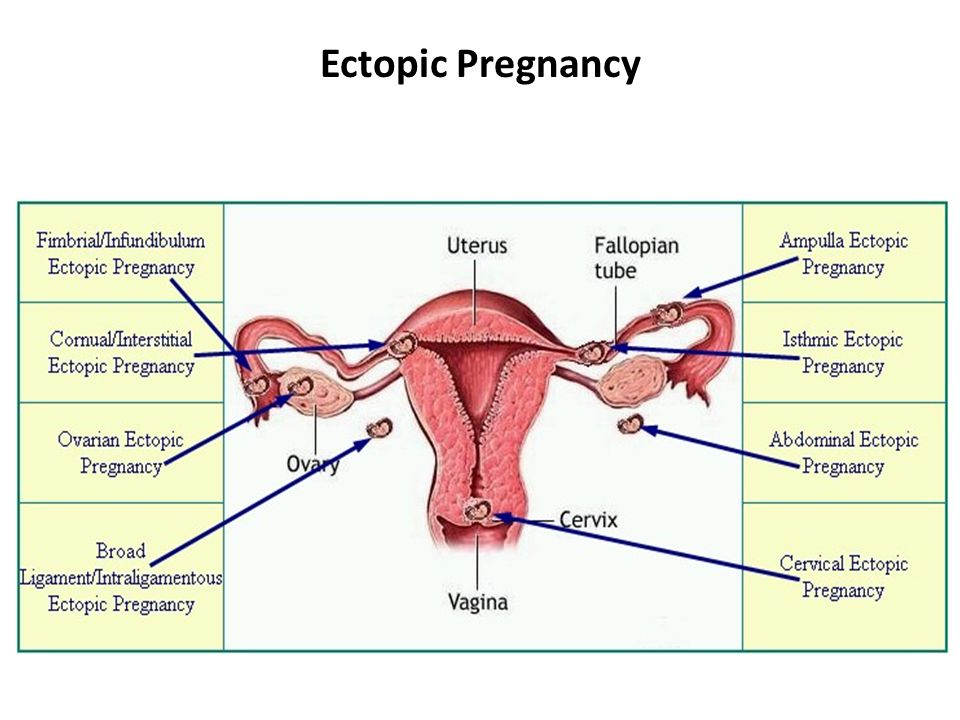 That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion .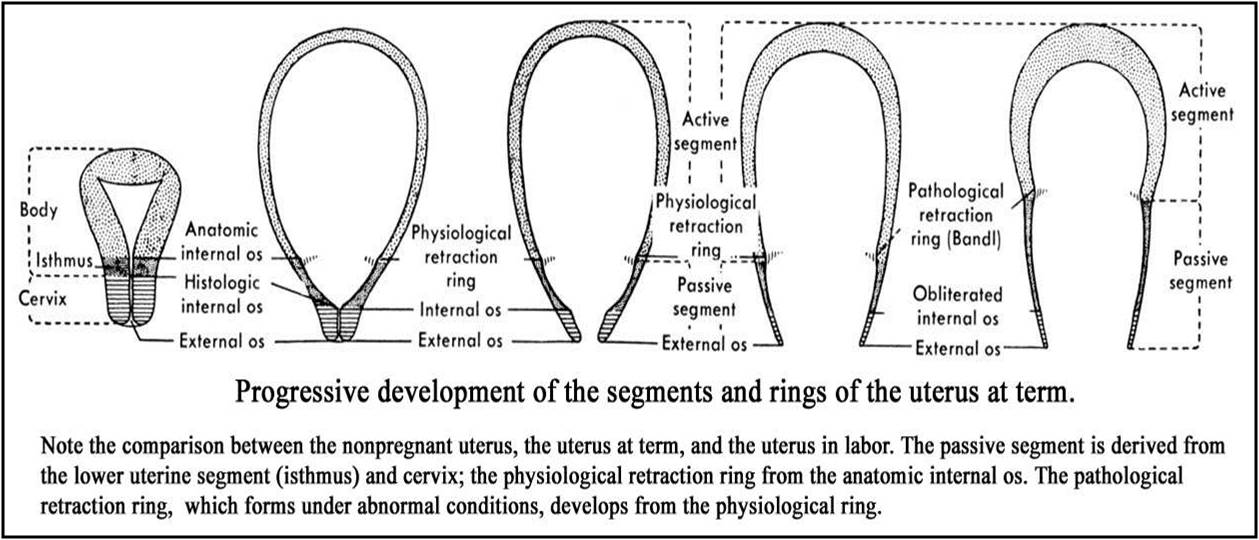 Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.

The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital of IDKClinic "Mother and Child" Entuziastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children's)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults
01.
Specialist consultations (adults)
02.
Specialist consultations (children)
03.
Laboratory of molecular genetics
04.
General studies
05.
Procedure cabinet
06.
other gynecological operations
07.
Telemedicine for adults
08. examinations
09.
Adult ultrasound examinations
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
causes, symptoms, diagnostics and treatment methods on the Alfa Health Center website
Inflammation of the cervix, or cervicitis, refers to inflammation of the narrow lower part of the organ. A healthy uterus is normally covered with epithelium that produces a mucous secretion. This substance plays a protective role and prevents the penetration of infections into the internal cavity. In violation of the secretory function of cells, an active growth of pathogenic microflora occurs, symptoms of inflammation of the cervix develop.
This substance plays a protective role and prevents the penetration of infections into the internal cavity. In violation of the secretory function of cells, an active growth of pathogenic microflora occurs, symptoms of inflammation of the cervix develop.
According to statistics, cervicitis is diagnosed in 30% of women of childbearing age. Pathology can be in the cervical canal, then they talk about endocervicitis, or in the vaginal part of the cervix - exocervicitis. The peak incidence is recorded in the age group of 17-28 years, when a woman shows maximum sexual activity and rarely uses barrier contraceptives.
Treatment of inflammation of the cervix in the initial stage is carried out by conservative methods and does not require radical measures. The prognosis is favorable. But for this, a woman should regularly undergo medical examinations and consult a gynecologist when the first symptoms of the disease appear.
You can undergo an examination with signs of cervicitis in Moscow at the Alfa Health Center clinic.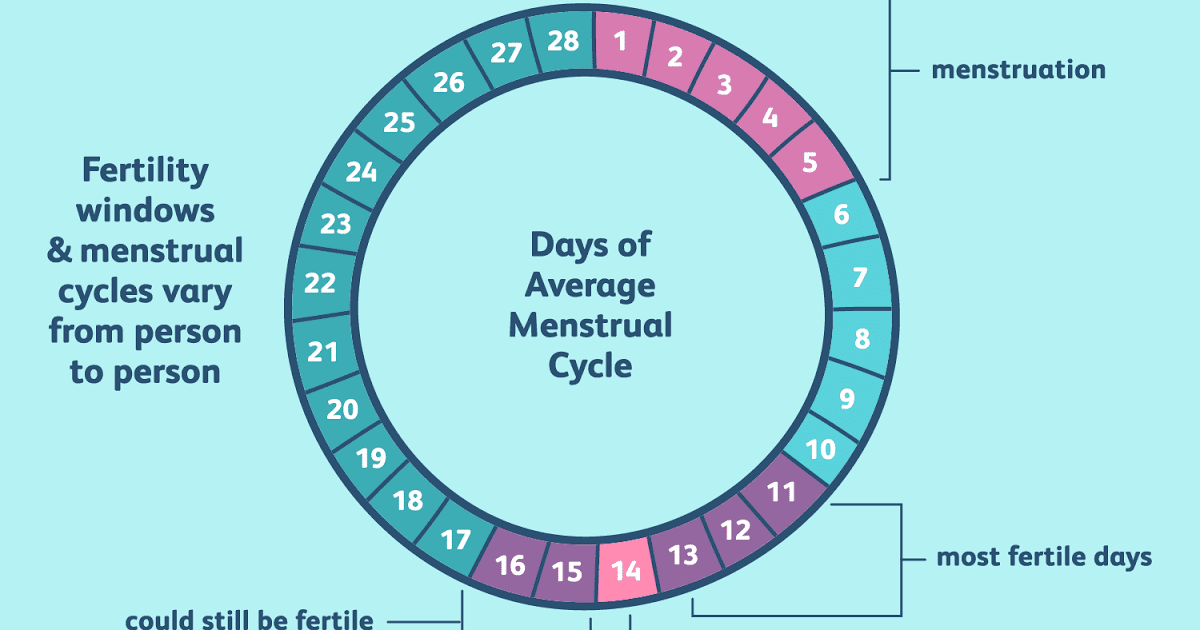
Signs of inflammation of the cervix
Complaints of patients are different in acute and chronic cervicitis.
The main symptoms of inflammation in the cervix:
- discharge from the genital organs of a purulent or mucous type;
- pain, heaviness in the uterus;
- discomfort, burning in the urinary tract, aggravated by sex, urination;
- a slight rise in temperature to 37-37.2ºС.
In some cases, the inflammatory process proceeds without pronounced clinical signs and is determined by the results of a gynecological smear.
Causes of cervicitis
Inflammation of the cervix and appendages can be caused by the following factors:
- sexually transmitted disease: gonorrhea, trichomoniasis, chlamydia and other infections;
- microorganisms that are normally present on the vaginal mucosa;
- mechanical injuries during gynecological operations, conization, childbirth, from the use of the uterine ring, treatment with iodine, dimexide, and other means;
- hormonal disorders;
- antibiotic treatment, chemotherapy courses;
- Allergy to latex or substances used to treat condoms
- diseases of the female genitourinary system: colpitis, endometritis, cystitis, erosion and others.
A common cause of inflammation of the cervix is an independent, uncontrolled intake of antibiotics. Medicines inhibit the beneficial microflora of the vagina, reduce local immunity. Organisms resistant to antibiotics appear in the woman's biota. These are the most difficult cases of mixed infections that require an individual treatment plan.
There are also such risk factors as young age, frequent change of sexual partners.
Types of cervicitis due to inflammation
- Purulent. Occurs when infected with a sexually transmitted disease. For purulent cervicitis, mucous discharge with an unpleasant odor is characteristic, involvement of nearby organs and tissues in the process.
- Viral. The mucous membrane becomes inflamed when infected with cytomegalovirus, human papillomavirus or other pathogens. The disease may be accompanied by itching, the appearance of polyps.
- Bacterial. Cervicitis develops from vaginosis, when there is an active reproduction of pathogens of the natural microflora of the vagina.
 Possible infection from a sexual partner.
Possible infection from a sexual partner. - atrophic. The cause of the disease is the thinning of the mucous membranes. Atrophic cervicitis is often found in women during menopause.
Cervicitis diagnostics
The first stage is an examination by a gynecologist and a colposcopy. Reddened, swollen mucous membranes, discharge clearly indicate a pathology. To clarify the diagnosis, a vaginal smear, a PCR test, and a biopsy of the affected tissue are performed. Ultrasounds, blood and urine tests may also be required. The doctor prescribes the studies necessary for the differential diagnosis of inflammation with dysplasia (precancerous condition), erosion and other diseases.
Treatment of cervicitis
To select an adequate treatment regimen for cervical disease, the duration, severity of the disease, and the cause are taken into account. With the infectious nature of cervicitis, therapy will also be required for the sexual partner.
To treat acute inflammation of the cervix, the doctor may prescribe:
- Antibiotics of the fluoroquinolone or macrolide group.
 At the same time, it is recommended to take antimycotic drugs that will prevent the development of candidiasis;
At the same time, it is recommended to take antimycotic drugs that will prevent the development of candidiasis; - Means for restoration of microflora. A woman is prescribed therapeutic suppositories, gels with lactobacilli;
- Immunomodulators. Preparations strengthen local immunity, help beneficial microflora to resist the effects of antibiotics. Immunomodulators are taken in the form of powders or tablets;
- Hormonal drugs with estrogens for the regeneration of the thinned mucous layer;
- Physiotherapy: endocervical electrophoresis, magnetotherapy, irradiation of the cervix with ultraviolet, laser, microwaves, low-frequency ultrasound. Treatment is primarily aimed at restoring blood and lymph microcirculation in the affected tissues. In chronic inflammation of the cervix, physiotherapy is carried out in courses several times a year to prevent exacerbation.
In rare cases, surgery is indicated. As a rule, the operation is performed with severe and extensive inflammation, when the woman did not seek diagnosis at the onset of the disease.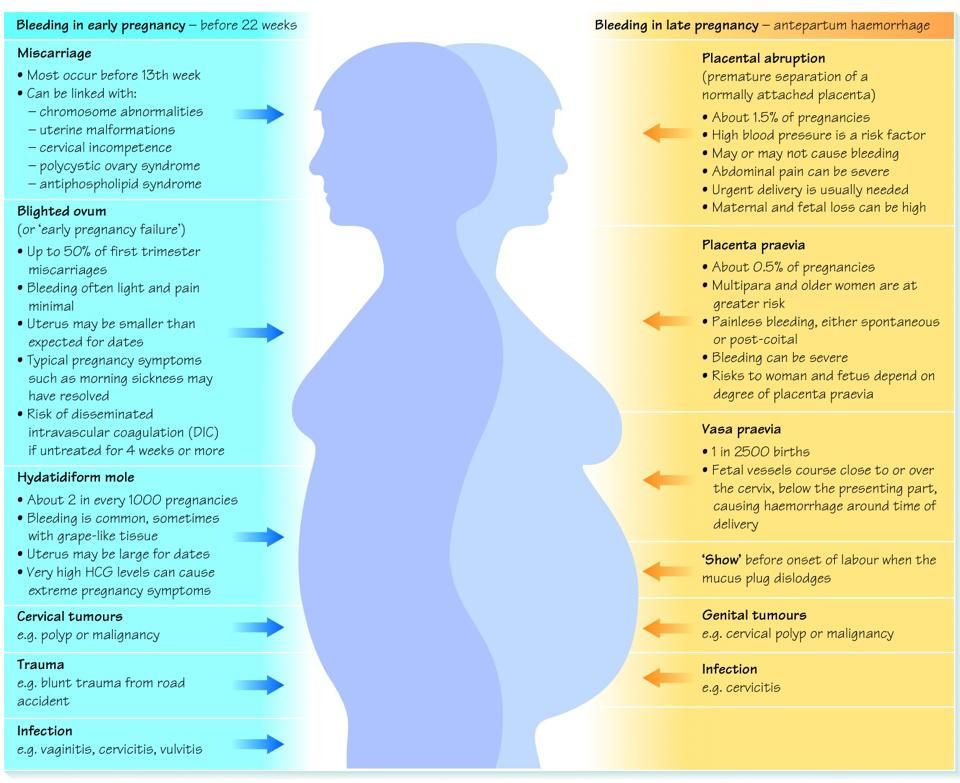 For treatment, the method of cryodestruction, diathermocoagulation or chemical coagulation of pathological areas is used.
For treatment, the method of cryodestruction, diathermocoagulation or chemical coagulation of pathological areas is used.
Particular attention is paid to the treatment of exacerbation of cervicitis in pregnant women. The doctor carefully selects drugs and calculates the dosage in order to eliminate risks to the fetus.
What is dangerous inflammation of the cervix
Self-medication is risky with complications, so only a doctor should decide how to treat a woman. If the patient does not seek help in a timely manner, acute cervicitis becomes chronic. A woman is threatened with such consequences as erosion, miscarriage, the spread of the inflammatory process to the appendages. The risk of developing cancer increases. Chronic cervicitis leads to the formation of adhesions and infertility. Patients often experience chronic pelvic pain, menstrual irregularities, and other symptoms that reduce quality of life.
Inflammation of the cervix during pregnancy
Cervicitis occurs in two out of three pregnant women at different gestation periods.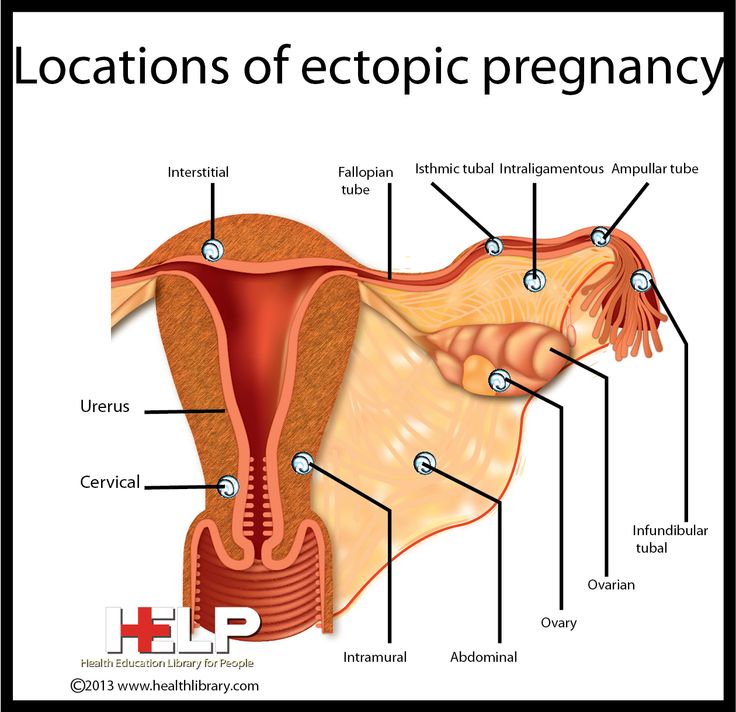 The disease is acute, not only the wall of the vagina becomes inflamed, but also the labia. Women complain of burning, itching in the perineum, discomfort. Inflammation of the cervix during pregnancy is one of the factors of miscarriage, so you need to see a doctor as soon as possible.
The disease is acute, not only the wall of the vagina becomes inflamed, but also the labia. Women complain of burning, itching in the perineum, discomfort. Inflammation of the cervix during pregnancy is one of the factors of miscarriage, so you need to see a doctor as soon as possible.
Cervicitis in this case is chronic. A woman may not be aware of inflammation until pregnancy, when the pathology manifests itself against the background of natural immunodeficiency.
Doctor's recommendation
Every year more and more women come to us for the treatment of chronic inflammation of the cervix. The reason is that the patient simply does not notice or ignores the first signs of cervicitis. Often we identify inflammation when dealing with completely different complaints. This is dangerous for future motherhood. We recommend that couples with a history of stillbirth, miscarriage, intrauterine infection of the fetus undergo a thorough examination to identify hidden infectious agents.