Can you give birth at 5 months
Premature baby | Pregnancy Birth and Baby
Premature baby | Pregnancy Birth and Baby beginning of content10-minute read
Listen
What is a premature baby?
Most pregnancies last 40 weeks. A baby born before the 37th week is known as a premature or pre-term baby. Medical advances have meant that more than 9 out of 10 premature babies survive, and most go on to develop normally.
In Australia, almost 1 in every 10 babies is born prematurely. Most Australian premature babies are born between 32 and 36 weeks and don't have any serious long-term problems.
Very premature babies are at a higher risk of developmental problems. It is possible for babies born at 23 to 24 weeks to survive, but they are at a greater risk of health complications.
Many babies born before 32 weeks, and those weighing 2. 5 kg or less, may need help breathing. They will usually be cared for in a neonatal intensive care unit (NICU) until they have developed enough to survive on their own. Babies born between 32 and 37 weeks may need care in a special care nursery (SCN).
Why are babies born prematurely?
Often the cause of premature birth is not known. However, some of the reasons babies are born prematurely include:
- problems with the cervix, when it is too weak to hold the weight of the baby and uterus so it starts to open prematurely (your doctor may call this ‘cervical incompetence’)
- multiple pregnancy (twins or more)
- birth parent has a medical condition that means the baby must be induced early, such as pre-eclampsia
- problems with the placenta such as placental insufficiency, placenta praevia, placenta accreta or placental abruption
- preterm (premature) rupture of membranes, when the amniotic sac spontaneously ruptures (also known as ‘waters breaking’)
- the birth parent has a health condition like diabetes, or an infection
- the birth parent has a history of premature labour
Signs of premature labour include:
- contractions
- your waters breaking
- a 'show' of mucus from your vagina, or a change in your vaginal discharge, or mucous, blood or fluid leaking from your vagina
- a sudden decrease in your baby's movements
- pressure in the pelvis, as if the baby is pushing down
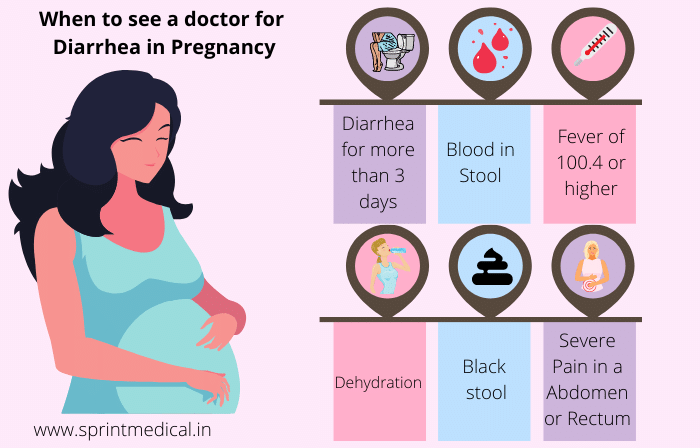
- cramping in the lower part of the belly, diarrhoea, nausea or vomiting
- constant lower back pain
You should also contact your midwife or doctor if you experience swelling in your face, hands or feet, or double vision, blurred vision or other eye disturbances. These are signs of pre-eclampsia, which is a common cause of pre-term births.
These are signs of pre-eclampsia, which is a common cause of pre-term births.
Find out more about the signs of labour.
What should I do if I experience signs of premature labour?
If you are less than 37 weeks pregnant and you experience any of the signs of premature labour, contact your doctor or nearest birthing centre immediately. It may be possible to slow down or stop the labour. Each day your baby stays inside your womb, the better their outcomes are likely to be.
If your labour starts prematurely, it’s best to go to a hospital that can care for your newborn, such as a hospital with a neonatal intensive care unit (NICU) or special care nursery (SCN). You can find your nearest suitable hospital on the Miracle Babies Foundation website.
How is a premature labour managed?
At the hospital, you will probably have a pelvic examination or an ultrasound. The medical team will check whether your cervix has started to open for labour and monitor your baby. If the hospital where the baby is born does not have an NICU, you and your baby may be transferred to another hospital.
If the hospital where the baby is born does not have an NICU, you and your baby may be transferred to another hospital.
When you are in labour, you may be given medicines to stop the contractions for a while. This allows you to be transferred to another hospital if necessary. You may also receive injections of corticosteroids 12 to 24 hours before the birth. Steroids will reduce your baby’s risk of some of the complications of being born very early (for example, breathing difficulties).
Premature babies can be born very quickly. They will usually be born through the vagina. However, in some cases the doctor may decide it is safest for you to give birth to your baby by caesarean section. Your doctor will discuss this decision with you.
A medical team from the neonatal (newborn) unit will be there for the birth. As soon as your baby is born, they will care for the baby in your room. The health team might use some specialised equipment, for example, your baby may need a neonatal resuscitation bed.
The team will keep your baby warm and may help them to breathe with an oxygen mask or breathing tube, and possibly medicine. Some babies need help to keep their heart beating with cardio-pulmonary resuscitation (CPR) or an injection of adrenalin.
Once your baby is stable, they may be transferred to the NICU or SCN.
Will I be able to hold my baby?
How soon you are able to hold your baby will depend on their medical condition. You may be able to hold them on the day they are born, but you might need to wait a few days or weeks until they are stable enough.
Holding your baby, known as kangaroo care, is an important part of your baby’s health and wellbeing, and the maternity staff will support you to do this as soon as you are able to.
Will my baby be able to breast feed?
After your baby is born, you’ll be asked to start expressing breastmilk. Maternity staff, lactation consultants and Australian Breastfeeding Association counsellors can help you.
Breastmilk is full of antibodies and nutrients that will be very important for your baby’s health and growth. Your baby may be given breast milk through a feeding tube initially because if they aren’t able to breastfeed. However, there are things you can do to help your baby learn to breastfeed:
- Holding your baby skin-to-skin, as soon as it is safe to do so, can help your baby feel secure and can help to stimulate your milk supply. Skin-to-skin feeding can be a good way to help prepare both you and your baby for breastfeeding.
- When your baby is held skin-to-skin you may notice them becoming more alert, sucking their fingers or lips, and moving closer towards your breast. These are signs that your baby may be ready to feed.
- Babies in the NICU usually progress through several stages when starting to breast feed. They may start by nuzzling and licking your nipple. They may then move towards your breast and take a few sucks. With time they will take more sucks and start to swallow, and will do so for longer periods of time.
 Eventually they will be looking to breastfeed with every feed.
Eventually they will be looking to breastfeed with every feed. - If your baby is very premature or sick it may take time for your baby to breastfeed well. It may take weeks – this is very normal. Hold your baby skin-to-skin when you can, and always go at their pace. With time your baby will start to feed better.
- If you do not want to breastfeed or don't produce enough milk, the staff will discuss formula feeding with you.
What will my premature baby look like?
Babies born at 36 to 37 weeks usually look like small full-term babies. Very premature babies will be small (perhaps fitting in your hand) and look very fragile.
Skin: Your baby’s skin might not be fully developed, and may appear shiny, translucent, dry or flaky. Your baby may not have any fat under the skin to keep them warm.
Eyes: The eyelids of very premature babies may be fused shut at first. By 30 weeks they should be able to respond to different sights.
Immature development: Your baby might not be able to regulate their body temperature, breathing or heart rate. They may twitch, become stiff or limp or be unable to stay alert.
Hair: Your baby may have little hair on its head, but lots of soft body hair (called 'lanugo').
Genitals: Your baby's genitals may be small and underdeveloped.
Will my premature baby's development be delayed?
Some common issues for premature babies include:
- breathing problems
- heart problems
- problems in their digestive tract
- jaundice
- leukaemia and anaemia
- infections
Most premature babies will develop normally, but they have a higher risk of developmental problems and will need regular health and developmental checks at the hospital or with a paediatrician. If you are worried about your child's development, talk to your doctor.
Problems that may occur later in children who were born prematurely include:
- language delays
- growth and movement problems
- problems with teeth
- problems with vision or hearing
- thinking and learning difficulties
- social and emotional problems
How do I calculate my baby's ‘corrected age’?
When you're considering whether your premature baby is developing normally, it is important to understand their 'corrected age'.
The corrected age is your baby's chronological age (how long ago they were born) minus the number of weeks or months they were born early. For example, a 6-month-old baby who was born 2 months early would have a corrected age of 4 months. That means they might be doing the things that other 4-month-olds do. Most paediatricians recommend correcting age when assessing growth and development until your child is 2 years old.
When will my baby be able to come home?
The hospital will not send your baby home until they are confident both you and your baby are ready. Staff will make sure you understand how to care for your baby at home. They will also show you how to use any equipment you may need.
You will need appointments to see a neonatologist (newborn baby doctor) or paediatrician. Your local child health nurse will also see you regularly.
It is normal to feel a little worried when you are looking after your baby yourself after a while in hospital. Take it slowly, and try to create a calm and quiet environment, until you both become confident being at home.
How do I cope with the stress of having a premature baby?
Having a premature baby can be an overwhelming and stressful experience for many parents. If you have a baby in the NICU or special care nursery you may feel distant from your baby and feel that it is difficult to bond with your baby. You may feel anxious about your baby’s health, now and in the future.
It might be helpful for you to think about other times in your life when you were feeling stressed or anxious and consider the different things you did to help you cope. Talking to close family and friends, speaking to people in similar situations to you, seeking professional help and writing down your feelings, may be useful ways to cope during this challenging time.
Who can I talk to for advice and support?
If you need support, contact the Miracle Babies Foundation's website 24-hour support line on 1300 622 243.
The Australian Breastfeeding Association can provide advice and support on feeding your baby on 1800 686 268.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Miracle babies foundation (What is prematurity), Miracle babies foundation (Causes of prematurity), Royal Women's (Stages of labour), Miracle babies foundation (Corrected and chronological age), The Royal Women’s Hospital (The Royal Women’s Hospital), Miracle Babies Foundation (Going home), South Australian Perinatal Practice Guidelines (Preterm Labor and Birth), Miracle babies foundation (Kangaroo care), The Royal Women\u2019s Hospital (Helping your baby to breast feed in the NICU), The parent infant research institute (Having a premature baby), Miracle Babies Foundation (Understanding your feelings)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2022
Back To Top
Related pages
- Neonatal intensive care unit (NICU)
- Special care nursery (SCN)
- What is kangaroo care?
Need more information?
Premature birth & premature babies | Raising Children Network
This essential guide for parents of premature babies covers gestational age, premature birth risk factors, premature labour and premature development.
Read more on raisingchildren.net.au website
Premature babies and birth | Raising Children Network
Premature babies are born before 37 weeks of pregnancy. Our essential guide covers premature birth, babies, development, NICU and more.
Read more on raisingchildren. net.au website
net.au website
Dads: premature birth and premature babies | Raising Children Network
After a premature birth, it can be hard for dads. Our dads guide to premature babies and birth covers feelings, bonding, and getting involved with your baby.
Read more on raisingchildren.net.au website
Premature birth: questions & checklist | Raising Children Network
Our checklist has answers to questions about premature birth and labour, covering where and how premature babies are born, and things to ask medical staff.
Read more on raisingchildren.net.au website
Bonding with premature babies in the NICU | Raising Children Network
For parents with premature babies in the NICU, bonding might seem hard. This guide explains how to use touch, song, play and daily care to bond with baby.
This guide explains how to use touch, song, play and daily care to bond with baby.
Read more on raisingchildren.net.au website
Premature birth: coping with your feelings | Raising Children Network
After a premature birth and while caring for a premature baby, it’s normal to have powerful and mixed feelings. Here’s how to cope with your feelings.
Read more on raisingchildren.net.au website
NICU: sleep & noise for premature babies | Raising Children Network
Noise in the neonatal intensive care unit (NICU) can affect how premature babies sleep. Here’s how you and staff can help your premature baby sleep better.
Read more on raisingchildren.net.au website
Sleeping - Miracle Babies
A premature baby’s success at sleeping is vitally important to their health and growth
Read more on Miracle Babies Foundation website
What is Prematurity? - Miracle Babies
Prematurity is the term used to describe when a baby is born early
Read more on Miracle Babies Foundation website
Premature birth: practical ways to prepare | Raising Children Network
If you know you’ll be having a premature birth, you can do lots of practical things to prepare – organising help at home, stocking the freezer and more.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
the long-term impacts of being born extremely early
Scientists are watching out for the health of adults born extremely premature, such as these people who took part in a photography project. Credit: Red Méthot
Credit: Red Méthot
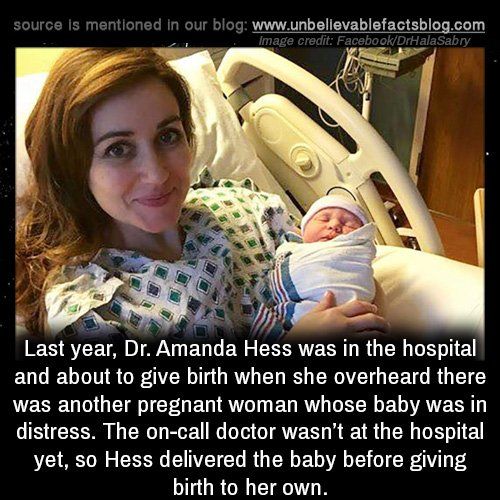
They told Marcelle Girard her baby was dead.
Back in 1992, Girard, a dentist in Gatineau, Canada, was 26 weeks pregnant and on her honeymoon in the Dominican Republic.
When she started bleeding, physicians at the local clinic assumed the baby had died. But Girard and her husband felt a kick. Only then did the doctors check for a fetal heartbeat and realize the baby was alive.
The couple was medically evacuated by air to Montreal, Canada, then taken to the Sainte-Justine University Hospital Center. Five hours later, Camille Girard-Bock was born, weighing just 920 grams (2 pounds).
Babies born so early are fragile and underdeveloped. Their lungs are particularly delicate: the organs lack the slippery substance, called surfactant, that prevents the airways from collapsing upon exhalation. Fortunately for Girard and her family, Sainte-Justine had recently started giving surfactant, a new treatment at the time, to premature babies.
After three months of intensive care, Girard took her baby home.
Today, Camille Girard-Bock is 27 years old and studying for a PhD in biomedical sciences at the University of Montreal. Working with researchers at Sainte-Justine, she’s addressing the long-term consequences of being born extremely premature — defined, variously, as less than 25–28 weeks in gestational age.
Families often assume they will have grasped the major issues arising from a premature birth once the child reaches school age, by which time any neurodevelopmental problems will have appeared, Girard-Bock says. But that’s not necessarily the case. Her PhD advisers have found that young adults of this population exhibit risk factors for cardiovascular disease — and it may be that more chronic health conditions will show up with time.
Camille Girard-Bock, born at 26 weeks of gestation, is now studying the effects of prematurity for a PhD.Credit: Red Méthot
Girard-Bock doesn’t let these risks preoccupy her. “As a survivor of preterm birth, you beat so many odds,” she says. “I guess I have some kind of sense that I’m going to beat those odds also.”
“I guess I have some kind of sense that I’m going to beat those odds also.”
She and other against-the-odds babies are part of a population which is larger now than at any time in history: young adults who are survivors of extreme prematurity. For the first time, researchers can start to understand the long-term consequences of being born so early. Results are pouring out of cohort studies that have been tracking kids since birth, providing data on possible long-term outcomes; other studies are trialling ways to minimize the consequences for health.
These data can help parents make difficult decisions about whether to keep fighting for a baby’s survival. Although many extremely premature infants grow up to lead healthy lives, disability is still a major concern, particularly cognitive deficits and cerebral palsy.
Researchers are working on novel interventions to boost survival and reduce disability in extremely premature newborns. Several compounds aimed at improving lung, brain and eye function are in clinical trials, and researchers are exploring parent-support programmes, too.
Researchers are also investigating ways to help adults who were born extremely prematurely to cope with some of the long-term health impacts they might face: trialling exercise regimes to minimize the newly identified risk of cardiovascular disease, for example.
“We are really at the stage of seeing this cohort becoming older,” says neonatologist Jeanie Cheong at the Royal Women’s Hospital in Melbourne, Australia. Cheong is the director of the Victorian Infant Collaborative Study (VICS), which has been following survivors for four decades. “This is an exciting time for us to really make a difference to their health.”
The late twentieth century brought huge changes to neonatal medicine. Lex Doyle, a paediatrician and previous director of VICS, recalls that when he started caring for preterm infants in 1975, very few survived if they were born at under 1,000 grams — a birthweight that corresponds to about 28 weeks’ gestation. The introduction of ventilators, in the 1970s in Australia, helped, but also caused lung injuries, says Doyle, now associate director of research at the Royal Women’s Hospital. In the following decades, doctors began to give corticosteroids to mothers due to deliver early, to help mature the baby’s lungs just before birth. But the biggest difference to survival came in the early 1990s, with surfactant treatment.
In the following decades, doctors began to give corticosteroids to mothers due to deliver early, to help mature the baby’s lungs just before birth. But the biggest difference to survival came in the early 1990s, with surfactant treatment.
“I remember when it arrived,” says Anne Monique Nuyt, a neonatologist at Sainte-Justine and one of Girard-Bock’s advisers. “It was a miracle.” Risk of death for premature infants dropped to 60–73% of what it was before1,2.
Marcelle Girard looks in at baby Camille, born weighing just 920 grams (2 pounds).Credit: Camille Girard-Bock
Today, many hospitals regularly treat, and often save, babies born as early as 22–24 weeks. Survival rates vary depending on location and the kinds of interventions a hospital is able to provide. In the United Kingdom, for example, among babies who are alive at birth and receiving care, 35% born at 22 weeks survive, 38% at 23 weeks, and 60% at 24 weeks3.
For babies who survive, the earlier they are born, the higher the risk of complications or ongoing disability (see ‘The effects of being early’). There is a long list of potential problems — including asthma, anxiety, autism spectrum disorder, cerebral palsy, epilepsy and cognitive impairment — and about one-third of children born extremely prematurely have one condition on the list, says Mike O’Shea, a neonatologist at the University of North Carolina School of Medicine in Chapel Hill, who co-runs a study tracking children born between 2002 and 2004. In this cohort, another one-third have multiple disabilities, he says, and the rest have none.
There is a long list of potential problems — including asthma, anxiety, autism spectrum disorder, cerebral palsy, epilepsy and cognitive impairment — and about one-third of children born extremely prematurely have one condition on the list, says Mike O’Shea, a neonatologist at the University of North Carolina School of Medicine in Chapel Hill, who co-runs a study tracking children born between 2002 and 2004. In this cohort, another one-third have multiple disabilities, he says, and the rest have none.
“Preterm birth should be thought of as a chronic condition that requires long-term follow-up,” says Casey Crump, a family physician and epidemiologist at the Icahn School of Medicine at Mount Sinai in New York, who notes that when these babies become older children or adults, they don’t usually get special medical attention. “Doctors are not used to seeing them, but they increasingly will.”
Outlooks for earliesWhat should doctors expect? For a report in the Journal of the American Medical Association last year4, Crump and his colleagues scraped data from the Swedish birth registry. They looked at more than 2.5 million people born from 1973 to 1997, and checked their records for health issues up until the end of 2015.
They looked at more than 2.5 million people born from 1973 to 1997, and checked their records for health issues up until the end of 2015.
Source: Ref. 4
Of the 5,391 people born extremely preterm, 78% had at least one condition that manifested in adolescence or early adulthood, such as a psychiatric disorder, compared with 37% of those born full-term. When the researchers looked at predictors of early mortality, such as heart disease, 68% of people born extremely prematurely had at least one such predictor, compared with 18% for full-term births — although these data include people born before surfactant and corticosteroid use were widespread, so it’s unclear if these data reflect outcomes for babies born today. Researchers have found similar trends in a UK cohort study of extremely premature births. In results published earlier this year5, the EPICure study team, led by neonatologist Neil Marlow at University College London, found that 60% of 19-year-olds who were extremely premature were impaired in at least one neuropsychological area, often cognition.
Such disabilities can impact education as well as quality of life. Craig Garfield, a paediatrician at the Northwestern University Feinberg School of Medicine and the Lurie Children’s Hospital of Chicago, Illinois, addressed a basic question about the first formal year of schooling in the United States: “Is your kid ready for kindergarten, or not?”
To answer it, Garfield and his colleagues analysed standardized test scores and teacher assessments on children born in Florida between 1992 and 2002. Of those born at 23 or 24 weeks, 65% were considered ready to start kindergarten at the standard age, 5–6 years old, with the age adjusted to take into account their earlier birth. In comparison, 85.3% of children born full term were kindergarten-ready6.
Despite their tricky start, by the time they reach adolescence, many people born prematurely have a positive outlook. In a 2006 paper7, researchers studying individuals born weighing 1,000 grams or less compared these young adults’ perceptions of their own quality of life with those of peers of normal birthweight — and, to their surprise, found that the scores were comparable.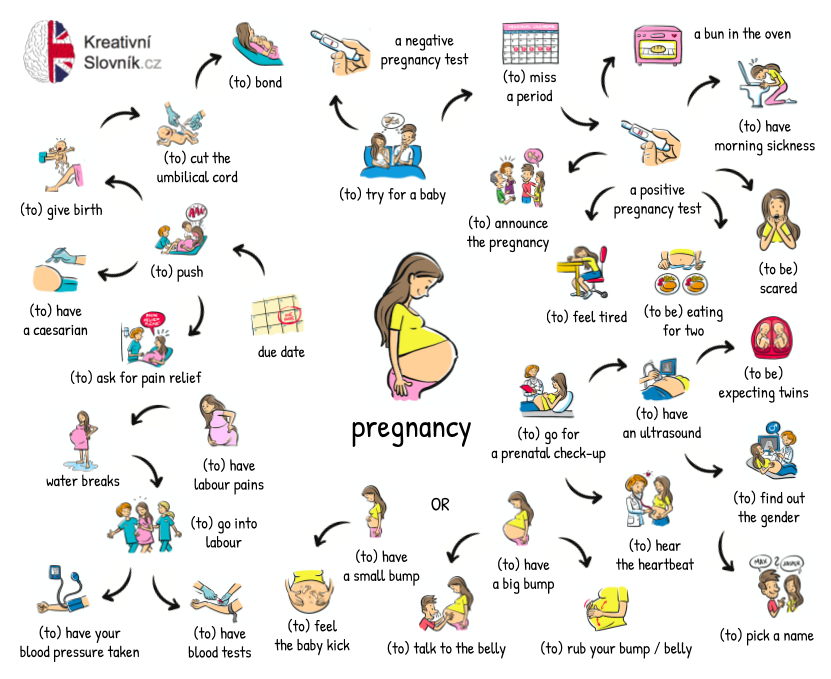 Conversely, a 2018 study8 found that children born at less than 28 weeks did report having a significantly lower quality of life. The children, who did not have major disabilities, scored themselves 6 points lower, out of 100, than a reference population.
Conversely, a 2018 study8 found that children born at less than 28 weeks did report having a significantly lower quality of life. The children, who did not have major disabilities, scored themselves 6 points lower, out of 100, than a reference population.
As Marlow spent time with his participants and their families, his worries about severe neurological issues diminished. Even when such issues are present, they don’t greatly limit most children and young adults. “They want to know that they are going to live a long life, a happy life,” he says. Most are on track to do so. “The truth is, if you survive at 22 weeks, the majority of survivors do not have a severe, life-limiting disability.”
A nurse uses electroencephalography (EEG) to carry out a check of brain development on a baby born at 25 weeks.Credit: BSIP/Universal Images Group via Getty
BreathlessBut scientists have only just begun to follow people born extremely prematurely into adulthood and then middle age and beyond, where health issues may yet lurk. “I’d like scientists to focus on improving the long-term outcomes as much as the short-term outcomes,” says Tala Alsadik, a 16-year-old high-school student in Jeddah, Saudi Arabia.
“I’d like scientists to focus on improving the long-term outcomes as much as the short-term outcomes,” says Tala Alsadik, a 16-year-old high-school student in Jeddah, Saudi Arabia.
When Alsadik’s mother was 25 weeks pregnant and her waters broke, doctors went so far as to hand funeral paperwork to the family before consenting to perform a caesarean section. As a newborn, Alsadik spent three months in the neonatal-intensive-care unit (NICU) with kidney failure, sepsis and respiratory distress.
The complications didn’t end when she went home. The consequences of her prematurity are on display every time she speaks, her voice high and breathy because the ventilator she was put on damaged her vocal cords. When she was 15, her navel unexpectedly began leaking yellow discharge, and she required surgery. It turned out to be caused by materials leftover from when she received nutrients through a navel tube.
The brain, interrupted
That certainly wasn’t something her physicians knew to check for. In fact, doctors don’t often ask if an adolescent or adult patient was born prematurely — but doing so can be revealing.
In fact, doctors don’t often ask if an adolescent or adult patient was born prematurely — but doing so can be revealing.
Charlotte Bolton is a respiratory physician at the University of Nottingham, UK, where she specializes in patients with chronic obstructive pulmonary disease (COPD). People coming into her practice tend to be in their 40s or older, often current or former smokers. But in around 2008, she began to notice a new type of patient being referred to her owing to breathlessness and COPD-like symptoms: 20-something non-smokers.
Quizzing them, Bolton discovered that many had been born before 32 weeks. For more insight, she got in touch with Marlow, who had also become concerned about lung function as the EPICure participants aged. Alterations in lung function are a key predictor of cardiovascular disease, the leading cause of death around the world. Clinicians already knew that after extremely premature birth, the lungs often don’t grow to full size. Ventilators, high oxygen levels, inflammation and infection can further damage the immature lungs, leading to low lung function and long-term breathing problems, as Bolton, Marlow and their colleagues showed in a study of 11-year-olds9.
Treatments for premature babies have improved in recent decades, but survival rates vary by age and country.Credit: Mohammed Hamoud/Getty
VICS research backs up the cardiovascular concerns: researchers have observed diminished airflow in 8-year-olds, worsening as they aged10, as well as high blood pressure in young adults11. “We really haven’t found the reason yet,” says Cheong. “That opens up a whole new research area.”
At Sainte-Justine, researchers have also noticed that young adults who were born at 28 weeks or less are at nearly three times the usual risk of having high blood pressure12. The researchers figured they would try medications to control it. But their patient advisory board members had other ideas — they wanted to try lifestyle interventions first.
The scientists were pessimistic as they began a pilot study of a 14-week exercise programme. They thought that the cardiovascular risk factors would be unchangeable. Preliminary results indicate that they were wrong; the young adults are improving with exercise.
Preliminary results indicate that they were wrong; the young adults are improving with exercise.
Girard-Bock says the data motivate her to eat healthily and stay active. “I’ve been given the chance to stay alive,” she says. “I need to be careful.”
From the startFor babies born prematurely, the first weeks and months of life are still the most treacherous. Dozens of clinical trials are in progress for prematurity and associated complications, some testing different nutritional formulas or improving parental support, and others targeting specific issues that lead to disability later on: underdeveloped lungs, brain bleeds and altered eye development.
For instance, researchers hoping to protect babies’ lungs gave a growth factor called IGF-1 — which the fetus usually gets from its mother during the first two trimesters of pregnancy — to premature babies in a phase II clinical trial reported13 in 2016. Rates of a chronic lung condition that often affects premature babies halved, and babies were somewhat less likely to have a severe brain haemorrhage in their earliest months.
Could baby’s first bacteria take root before birth?
Another concern is visual impairment. Retina development halts prematurely when babies born early begin breathing oxygen. Later it restarts, but preterm babies might then make too much of a growth factor called VEGF, causing over-proliferation of blood vessels in the eye, a disorder known as retinopathy. In a phase III trial announced in 2018, researchers successfully treated 80% of these retinopathy cases with a VEGF-blocking drug called ranibizumab14, and in 2019 the drug was approved in the European Union for use in premature babies.
Some common drugs might also be of use: paracetamol (acetaminophen), for example, lowers levels of biomolecules called prostaglandins, and this seems to encourage a key fetal vein in the lungs to close, preventing fluid from entering the lungs15.
But among the most promising treatment programmes, some neonatologists say, are social interventions to help families after they leave the hospital. For parents, it can be nerve-racking to go it alone after depending on a team of specialists for months, and lack of parental confidence has been linked to parental depression and difficulties with behaviour and social development in their growing children.
For parents, it can be nerve-racking to go it alone after depending on a team of specialists for months, and lack of parental confidence has been linked to parental depression and difficulties with behaviour and social development in their growing children.
At Women & Infants Hospital of Rhode Island in Providence, Betty Vohr is director of the Neonatal Follow-Up Program. There, families are placed in private rooms, instead of sharing a large bay as happens in many NICUs. Once they are ready to leave, a programme called Transition Home Plus helps them to prepare and provides assistance such as regular check-ins by phone and in person in the first few days at home, and a 24/7 helpline. For mothers with postnatal depression, the hospital offers care from psychologists and specialist nurses.
The results have been significant, says Vohr. The single-family rooms resulted in higher milk production by mothers: 30% more at four weeks than for families in more open spaces. At 2 years old, children from the single-family rooms scored higher on cognitive and language tests16. After Transition Home Plus began, babies discharged from the NICU had lower health-care costs and fewer hospital visits — issues that are of great concern for premature infants17. Other NICUs are developing similar programmes, Vohr says.
After Transition Home Plus began, babies discharged from the NICU had lower health-care costs and fewer hospital visits — issues that are of great concern for premature infants17. Other NICUs are developing similar programmes, Vohr says.
With these types of novel intervention, and the long-term data that continue to pour out of studies, doctors can make better predictions than ever before about how extremely premature infants will fare. Although these individuals face complications, many will thrive.
Alsadik, for one, intends to be a success story. Despite her difficult start in life, she does well academically, and plans to become a neonatologist. “I, also, want to improve the long-term outcomes of premature birth for other people.”
Premature birth - Juno
Premature birth: content of the article
What is preterm birth
The birth of a baby weighing more than 0.5 kg from 22 to 37 weeks is considered early. According to statistics, 15 million babies are born prematurely around the world.
In our country, until 2012, babies were registered who were born at 28 weeks, and all those born earlier - a week later. The development of obstetrics made it possible to nurse critically premature babies and increased their survival statistics.
Who is at risk
Any pregnant woman can give birth prematurely. Some expectant mothers have a higher chance of preterm birth. The risk zone includes pregnant women:
- under 17 and over 35;
- have more than one fetus;
- have structural features of the uterus or its cervix;
- use harmful substances - drugs, alcohol, smoke;
- have heavy physical activity;
- have a history of preterm birth;
- work in hazardous production;
- are subjected to sexual, emotional abuse, stress, mental stress.
At risk are expectant mothers who are not registered during the gestation period or ignore ultrasound, screenings, laboratory tests.
The threat of early preterm birth is more common with diagnoses: diabetes mellitus, anemia, hypertension, genitourinary infections, hypothyroidism, problems with weight before conception (deficiency or obesity), thrombophilia, vaginal bleeding. There is also a risk when conceiving through IVF, with congenital malformations of the fetus.
If a woman has previously given birth to a child ahead of schedule, the chances of premature birth remain in subsequent pregnancies. The same applies to the weight of the crumbs: if the firstborn was born with a lack of body weight, then his brother or sister may be underweight.
Risk factors
Doctors point to a number of factors that take place long before the conception of a child. These include:
- Gynecological diseases suffered in childhood or adolescence;
- Early initiation of intimate life;
- Hereditary factor;
- Pathologies of previous pregnancy: preeclampsia, fetoplacental insufficiency, premature birth;
- Excessive uterine distension in multiple pregnancies, polyhydramnios;
- Threat of early miscarriage.
Another risk factor is surgery or trauma to the abdominal organs during the gestation period.
Risk of preterm birth at different terms
The birth of a child prematurely has many negative consequences for him. It depends on the trimester in which the pregnancy ended.
The most severe consequence is the death of the infant. With early preterm birth in the period of 22-24 weeks, the threat is the highest - up to 80% of babies die. This occurs against the background of intracranial hemorrhage of 3-4 degrees, cardiopulmonary insufficiency, intrauterine infection of the fetus.
Among those born in the period of 25 - 26 weeks, 40% of babies die, in 27 - 28 - about 20%, in 29 - 32 - no more than 10%, and in 33 - 34 - 2% of newborns are at risk.
Modern medicine is able to provide care for a premature baby and save his life. But no one can guarantee a full healthy life. Such a child can subsequently be given disappointing diagnoses: cerebral palsy, mental retardation, retinopathy of prematurity. He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
For a woman in labor, preterm labor is usually not dangerous. Without concomitant pathologies, the mother's body does not care how long the child is born. There are only psychological problems: stress, fear and worries about the baby. It is better for a mother to tune in that her child, in case of severe prematurity, will be taken to the intensive care unit for nursing, so she will not see him immediately.
A newly minted mother needs rehabilitation. Therapy is prescribed, depending on the cause of the pathology: a complex of vitamins, antioxidants, hormones.
Why preterm birth is dangerous
Infants are immature: their body is covered with a large amount of cheese-like lubricant, there is a deficiency of subcutaneous fatty tissue, few hairs on the head and fluff on the body, cartilage on the ears and nose are soft, the nails do not go beyond the fingertips, the navel is located closer to the pubis.
Babies are underweight. Depending on the weight of the crumbs, 4 degrees of prematurity are distinguished: at the 1st degree, the baby weighs from 2500 to 2001 g, the 2nd - from 2000 to 1500 g, the 3rd - from 1500 to 1001 g, the 4th - 1000 g and below .
The development of the genital organs has not been completed: the testicles in boys are not lowered into the scrotum, and in girls the large labia do not cover the small and clitoris.
Children have immature lungs. They cannot breathe adequately - often they need help. The cry is weak. There are also problems with digestion. The body cannot absorb all the components from mother's milk.
Extrauterine life for children becomes a strong stress. It's hard to deal with him. They poorly resist infections, quickly lose heat, thermoregulation is impaired. They are subject to hemorrhages against the background of fragile vessels. Especially dangerous are hemorrhages in the cervical spinal cord and ventricles of the brain.
Among the complications of preterm birth are intracranial hemorrhages, asphyxia, intrauterine growth retardation.
Types of preterm birth
Several classifications have been adopted. Let's consider them.
- By term: critically early - up to 28 weeks, significantly early - from 28 to 32 weeks, moderately early or late - from 32 to 37 weeks;
- By the mechanism of attack: induced and spontaneous. Induced cause artificially for medical reasons. Occurs in 40% of cases. Spontaneous in 60% of cases begin with contractions, in 40% - with a rupture of the membranes;
- By the nature of the course: spontaneous, with regular labor activity, without it and artificially provoked. In 80% of cases, preterm labor begins spontaneously. At the same time, the fetal bladder can be intact - and then the contractions are regular, growing. Or amniotic fluid may pour out, labor activity is chaotic. For medical reasons, early delivery can be artificially induced.
 For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life;
For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life; - According to symptoms: threatening, incipient and incipient. With threatening early premature birth, the lower abdomen and lower back hurt, the tone rises. Her neck remains unchanged, the external os is closed. When the process begins, pains appear in the lower abdomen. Regular contractions may begin. The neck is flattened or shortened. The main symptom of the onset of preterm labor is regular labor activity. The cervix opens by 2 - 3 cm, it happens quickly.
In 40% of women in labor, water breaks, 35% gave birth quickly and quickly. The active phase lasts less than when the baby appears on time. The contractions are monotonous, long and painful, the pauses between them are small.
Causes of preterm birth
Doctors indicate the main causes of the pathology:
- Early activity of the fetal endocrine system;
- Infections and inflammatory processes - ureaplasmosis, mycoplasmosis, pyelonephritis, bacterial vaginosis.
 They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth;
They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth; - Placental bleeding. They occur with incorrect presentation or detachment. The situation is serious, there is a threat to the life of the mother. Therefore, with presentation, hospitalization is indicated;
- Neck weakness. In 20% of cases, it leads to preterm birth. This also includes such factors: the interval between the current and previous gestation is less than 2 years, the woman is expecting 4 children or more;
- Isthmic-cervical insufficiency. The cervix opens itself - a miscarriage or premature birth occurs. It is possible to open mechanically - when scraping after a miscarriage, IVF, abortion;
- Pathologies on the part of the baby - intrauterine infection, malformations of internal organs.
Chronic ailments, dental problems, angina, health status during gestation, genetic factors are all common reasons for early delivery. Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Symptoms of preterm labor
We list the signs by which you may suspect that the baby is in a hurry to be born ahead of time.
Spasms over the pubis. They are similar to pain during menstruation.
Pain, pressure and discomfort in the genitals, thighs, pelvis. There is a dull pain in the lumbar region.
Feeling of pressure, pressure in the back.
Diarrhea, spasms and pain in the intestines.
Vaginal discharge - they get worse. May be watery, pink, brown, bloody.
Contractions of varying intensity. Touch your stomach with your fingertips - you will feel the contraction and relaxation of the uterus. Counted more than 4 contractions in 60 minutes? Call an ambulance - you need an urgent examination by an obstetrician.
The following symptoms are also dangerous: sudden blurred vision, flashes and “flies” before the eyes, incessant migraine, swelling of the face or hands, temperature of 38º C and above, painful urination, abdominal trauma, decreased fetal activity in the 3rd trimester (less than 10 movements in 12 hours).
Any of the above symptoms indicate the risk of preterm birth. Seek medical attention.
Diagnosis of preterm birth
Includes several stages.
Transvaginal ultrasound. The length of the cervix is measured, fetal fibronectin is determined - a kind of "biological glue" that binds the fetal sac to the uterine mucosa.
Gynecological examination. Allows you to assess the degree of opening of the neck, its length.
Rapid test for the determination of phosphorylated protein-1. The test determines the possibility of preterm birth. In the future, this helps prevent iatrogenic complications.
When diagnosing, 2 parameters are evaluated:
- Regularity of contractions;
- Neck changes - shortening and smoothing. informative method. For example, with a neck length of 3 cm, the risk of preterm birth in the next week is 1%. The patient is not admitted to the hospital, there is no danger to her and the fetus.
Differential diagnosis
Its goal is to correctly diagnose. The early birth of a baby is accompanied by cramps in the lower abdomen, diarrhea, pain in the lumbar region. These same symptoms are characteristic of other conditions: appendicitis, colitis, cystitis, pyelonephritis.
When complaining of pain in the lower abdomen, the patient is examined for the consistency of the scar after the previous cesarean section, for example. When the temperature rises, flu, sore throat, viral infection are excluded.
Diagnosis
Preterm birth is stated based on the clinical picture. Doctors are guided by such markers.
The first is the length of the neck - less than 2 - 2.5 cm.
The second is the determination of phosphorylated protein-1.
The third is the regularity of contractions. There should be at least 4 in 20 minutes.
Fourth - neck changes in dynamics.
Fifth - assessment of the degree of maturity of the neck.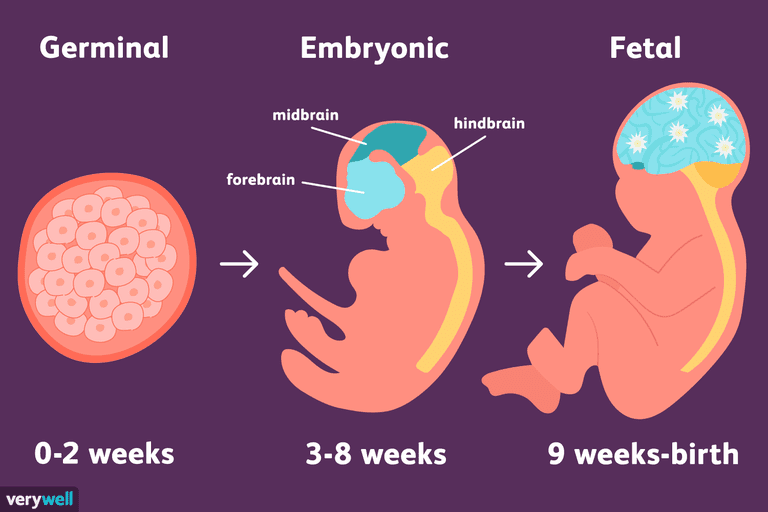 Determined by the level of PSIFR-1 in the cervical canal.
Determined by the level of PSIFR-1 in the cervical canal.
Usually the process begins rapidly, suddenly and intensely.
Treatment for preterm birth
The goal is to reduce the tone of the myometrium, reduce uterine contractions. This is achieved by blocking oxytocin receptors - it is the hormone oxytocin that triggers the birth process.
Such antagonists of oxytocin receptors are tocolytics. One of the modern representatives of this group of drugs is atosiban.
The remedy is effective, but has contraindications. It is forbidden to treat pregnant women for less than 24 and more than 33 weeks, with uterine bleeding, growth retardation, distress or fetal death, severe preeclampsia, with rupture of the fetal membrane after 30 weeks, placenta previa or its detachment.
5 stages of preterm labor
The first stage is forecasting their onset. Depends on the situation: the process is starting, has begun, or it is a threat.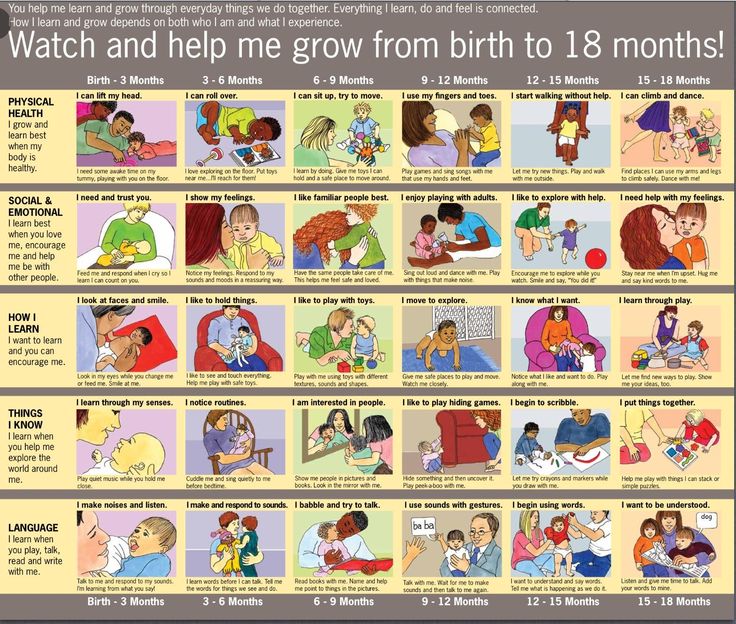
Stage two - prevention of respiratory distress syndrome in a child. Doctors stimulate the maturation of the lungs. Apply funds from the group of glucocorticoids.
Stage three - prolongation of pregnancy. Doctors try to delay preterm labor by giving the baby's lungs and placenta time to mature. For this, tocolytics are used - they inhibit the contractile activity of the uterus. Usually prophylaxis is carried out - tocolysis is carried out before contractions. When started, therapy is ineffective. The duration of treatment is a maximum of 48 hours.
Stage four - preparation for the birth of a premature baby. The woman in labor is transferred to a higher-level hospital. The physiology of preterm labor does not differ from the birth of a child at term. But close attention is required from doctors to minimize complications for mom and baby.
The fifth stage is the prevention of infections and their complications. At risk are women in labor whose waters have broken. If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
OB sequence
When registering a patient with preterm birth, the doctor gets acquainted with the exchange card, studies the general, gynecological and infectious anamnesis, and the results of examinations. Clarifies complaints and evaluates the condition of the woman in labor. He examines her, measures the pulse and respiration rate, temperature, pressure, abdominal circumference and the height of the uterus.
Clarifies data on the fetus: movements, measures heart rate by auscultation - listening to the heart through the mother's stomach through the device. To assess the condition of the crumbs, the doctor performs cardiotocography. The device records the heart rate.
Ultrasound is performed to assess the condition of the child and mother's organs.
A gynecological examination is carried out: with intact membranes - external, with their rupture - internal. This is necessary to determine the position and position of the child, to assess the degree of disclosure.
Conduct a laboratory examination. They take a smear from the vagina: culture for β-hemolytic streptococcus, bacteriological culture, take blood and urine for a general analysis.
According to the results of the examination, the obstetrician confirms or refutes preterm birth, their stage.
The expectant mother is informed about her condition, forecasts for the child. At the slightest opportunity, they try to prolong the pregnancy. If the child is ready to be born in the near future, the doctor determines the tactics of assistance, coordinates the issue of anesthesia with the woman in labor.
In the absence of indications for a caesarean section, they give birth naturally. This is the best way - it is less traumatic for the baby. A gentle approach is what a weak newborn needs.
A gentle approach is what a weak newborn needs.
Preterm birth care policy
The woman in labor is provided with continuous psychological support. Describe the current obstetric situation.
With head presentation, they give birth naturally.
With pelvic - take into account clinical indications. Caesarean section is not the only effective method in this case. The operation does not improve the prognosis for a premature baby, but it puts an additional burden on the mother's body: it increases infection, morbidity, and complications.
With foot presentation, only a caesarean section is done.
Anesthesia is carefully selected. Avoid opiates - they depress the respiratory center, which is dangerous for premature babies.
At the birth of a baby before 34 weeks, vacuum aspiration is prohibited. It increases the risk of neonatal morbidity. Dosed episiotomy, exit forceps for the birth of the head and epidural anesthesia are performed.
The umbilical cord is clamped at least 1 minute after the baby is born. This tactic reduces the frequency of intraventricular hemorrhage in preterm pregnancies up to 37 weeks of gestation.
Control the state of the crumbs. CTG is done every hour for 40 minutes, auscultation - periodically.
General recommendations for prevention
You need to think about it from the first trimester. If you want to inform the baby, follow the advice of gynecologists.
- Take care of yourself. Rest, avoid nervous overload. Sleep at least 7 hours;
- Eat well. Eat foods rich in vitamins, exclude fast food, fatty, fried, spicy and salty foods from the diet. Give up coffee and strong tea;
- Observe the drinking regimen. Try not to feel thirsty - drink water every 2 hours. If you don't want to - don't force yourself;
- Avoid physical activity. Active training, hard work, general cleaning alone are taboo for a pregnant woman.
 Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth;
Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth; - Maintain personal hygiene. Wash your face after a bowel movement. Always wash and dry from front to back. This way you will not bring bacteria from the intestine into the vagina. Infections are provocateurs of premature birth;
- Lead a healthy lifestyle. Alcohol and cigarettes are taboo. Smoking pregnant women are predisposed to preterm labor. If you take medications on a regular basis, tell your gynecologist about it. Walk outdoors. Cancel active workouts in favor of leisurely walks in the park;
- Register at the antenatal clinic in the first trimester - at 6 ‒ 8 weeks. Visit a gynecologist, listen to him, take tests, undergo ultrasound, screenings;
- Be careful with sex. In the first trimester, it is better to limit or abstain from it as much as possible - the embryo must be fixed. With placenta previa and other pathologies, the gynecologist may forbid you to have intimate contacts - listen to him;
- Learn to understand your body.
 In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth;
In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth; - Maintain bed rest. A gynecologist can advise you to rest. For example, with increased uterine contractions, tone;
- Rest every hour. Sit in a chair, lift your legs up. This will relax the muscles, eliminate swelling;
- Be aware of the signs of preterm labor. In case of their threat, you will not miss a moment and consult a doctor. Perhaps the process can be stopped with the help of drugs. Treatment minimizes complications in the premature baby.
Preterm birth prevention
It is divided into 2 stages: before conception and after.
Preventive measures before conception
It is advisable to carry them out to mothers from the risk zone. The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
Hydration is shown - enhanced drinking regimen. It improves fetoplacental blood flow and reduces the risk of preterm birth.
Eliminate infections. It is advisable to do this at the planning stage, since antibiotic treatment during gestation harms the fetus.
It is recommended to postpone the conception of a child soon after the birth of an older brother or sister. Mommy's body needs to recover from the previous pregnancy. It takes him at least 2 years to do this. During this time, the uterus will return to its previous state, strength, vitamin reserves and body reserves will be restored.
Vitamin complexes are prescribed for predisposition to preterm birth for planning and expectant mothers. Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Secondary prevention of early delivery
With the threat of premature birth, the condition of the pregnant woman is monitored at critical periods: from 2 to 12 and from 18 to 22 weeks. During these periods, it is better to stay in the hospital of the perinatal center. Doctors prescribe drugs to maintain and prolong pregnancy.
Therapy is selected on an individual basis.
With a short neck from 1 to 2.5 cm, progesterone suppositories are prescribed vaginally. The hormone is also shown in previous preterm births. This tactic reduces their risk by 35%. This is a natural hormone. It is efficient and safe. It is prescribed in the first trimester. Synthetic hormone is harmful: it can provoke gestational diabetes.
If there is a threat of early birth of the crumbs, sutures are placed on the neck. The expectant mother is out of the risk zone in this situation, stitches may not be applied.
The expectant mother is out of the risk zone in this situation, stitches may not be applied.
Another option is to install a pessary on the neck.
These methods reduce the statistics of premature births. But the mortality rate of newborns is not affected.
When carrying twins, circular or U-shaped sutures can be applied. In most cases, such tactics with a short neck in multiple pregnancies can provoke preterm labor. Vaginal progesterone is not prescribed.
For infections (for example, bacteriuria, gonococcus, syphilis, β-hemolytic streptococcus, bacterial vaginosis, chlamydia), antibiotic prophylaxis is prescribed. Depending on the diagnosis, penicillin, ampicillin, metronidazole, erythromycin, ceftriaxone, josamycin may be prescribed.
Terminals
Premature birth is one of the fears of many expectant mothers. Nobody is immune from this. But you can minimize the risks. Follow the recommendations of the gynecologist, take care of yourself, listen to your body, do not refuse to stay in the perinatal center.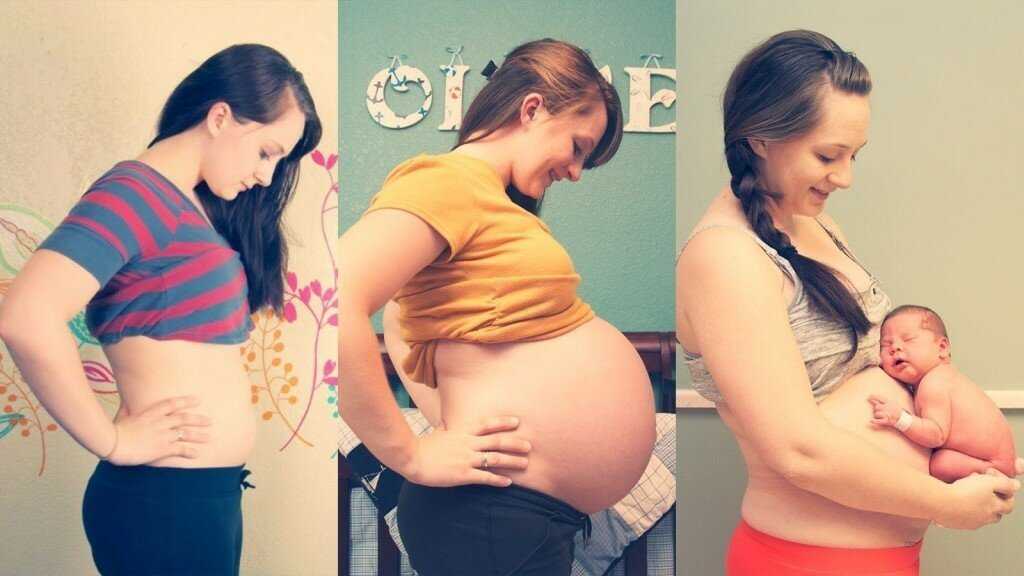
Don't think bad. Modern medicine successfully nurses premature babies, reduces the risks of complications and consequences.
"His organs and systems are not ready" Why in Russia they are trying to save children who have almost no chance to survive and be healthy: Society: Russia: Lenta.ru
In Russia, it was proposed to register only from the seventh day babies who were born very early (less than 22 weeks) and with extremely low birth weight (less than 500 grams). This happened after a series of criminal cases that the Investigative Committee initiated against obstetricians. So, neonatologist Elina Sushkevich from Kaliningrad was accused of killing a 22-week-old boy. Why are they trying to save 500-gram children in Russia at all today, what are their chances of surviving and whether they can grow up healthy - Lenta.ru learned from the doctor of medical sciences, head of the scientific department of neonatology and pathology of young children at the Research Clinical Institute of Pediatrics named after Yu. E. Veltishchev Elena Keshishyan.
E. Veltishchev Elena Keshishyan.
***
Lenta.ru: Now the minimum criteria for saving premature babies are 22-23 weeks and 500 grams of weight. Why?
Elena Keshishyan : In order to understand the limits of possibilities both in technical terms (creating an environment close to intrauterine) and in terms of the maturity of the child's brain, which is capable of developing out of utero, attempts were made in the world to give birth to premature babies of different ages. The greatest successes in this were achieved by the Japanese. They tried out babies born at 20 weeks. That is, the approximate gestational age was five months. The Japanese succeeded, but in isolated cases. And they saw that in children born at this age there is no differentiation of the brain, division into gray and white matter. Roughly speaking, this process determines the ability to think, to feel. This is called higher nervous activity. It is this ability that distinguishes man from animals.
Therefore, guided by research data and on the basis of a humanistic idea, the World Health Organization has set this limit for human live birth - 23 weeks, which corresponds to approximately 500 grams of weight. This is the minimum age at which the brain can differentiate into gray and white matter. And, accordingly, there is hope that it will already be a human person with mental abilities.
Countries with technological capabilities, including Russia, have agreed that those born at this gestational age can legally be considered human. That is, they have all human rights, including medical care.
Since 2012, Russia has switched to the WHO criteria for nursing premature babies. How many of these children have been saved during this time?
As a percentage of all those born, this is minuscule. I don't have exact numbers. But I want to say that the body of children born almost half prematurely is very immature. And their survival rate, conditionally, is one in a hundred. Still, 22-23 weeks is not childbirth in the full sense. From the point of view of nature, this is a miscarriage, this is a critical situation that may be associated with the health of the mother or the sick child herself. Therefore, the readiness for independent existence in such fruits is close to zero. Even if we assume that the maximum efforts of doctors are thrown to save the child, all the necessary equipment is connected, the chance that he will get out is very small. In such an infant, the kidneys, gastrointestinal tract, heart and other organs may not work. This is a very, very complex, jewelry work of doctors.
Still, 22-23 weeks is not childbirth in the full sense. From the point of view of nature, this is a miscarriage, this is a critical situation that may be associated with the health of the mother or the sick child herself. Therefore, the readiness for independent existence in such fruits is close to zero. Even if we assume that the maximum efforts of doctors are thrown to save the child, all the necessary equipment is connected, the chance that he will get out is very small. In such an infant, the kidneys, gastrointestinal tract, heart and other organs may not work. This is a very, very complex, jewelry work of doctors.
One of the world's smallest surviving premature babies. Amilya Taylor was born in 2006 in Miami, USA. She spent only 22 weeks in the womb and was born with a weight of 284 grams and a height of 24 centimeters.
Photo: Baptist Health South Florida / Reuters
And dear?
Of course. A day in a well-equipped neonatal intensive care unit costs several thousand dollars. And to leave such a child, months are needed. But I want to emphasize that the number of survivors in this period is minimal. And it is minimal in almost all countries where the WHO criteria apply.
And to leave such a child, months are needed. But I want to emphasize that the number of survivors in this period is minimal. And it is minimal in almost all countries where the WHO criteria apply.
If these children are not viable, cost too much, then why were these criteria established?
The medical task here is not at all to save all the children who are born within five months. It is clear that there is not a single person who does not understand that this child is at risk of being blind, deaf and immobilized. The task of medicine in this situation is to acquire knowledge and experience.
Obstetricians learn how to prolong pregnancy as much as possible. There is a whole range of activities: prenatal diagnosis of genetic chromosomal diseases, various fetal malformations, identification of risk groups among pregnant women, their special monitoring, prenatal logistics and routing. They also hone the ability to properly take birth at this time. This must be done as carefully as possible and do not forget about the "golden hour". It is necessary to have time to give the child, without waiting until his condition worsens, what he could not get from his mother. That is, even if the child screamed, you need to understand that soon he will stop doing this and will not be able to breathe. The "golden hour" essentially determines whether or not there will be damage to brain cells. This means whether or not a child will have a full life.
It is necessary to have time to give the child, without waiting until his condition worsens, what he could not get from his mother. That is, even if the child screamed, you need to understand that soon he will stop doing this and will not be able to breathe. The "golden hour" essentially determines whether or not there will be damage to brain cells. This means whether or not a child will have a full life.
And the qualifications of resuscitators working with such children are growing today. All this led to an important point: the quality of nursing of children born a little later, at 26-28 weeks, has become much better. I see these babies regularly. And I can say that over time, many of them are no different from their peers.
And before?
About 30 years ago, about six or seven out of ten children would become severely disabled. And today I had three 26-week-old babies at my appointment. And everyone is developing quite well, there is a slight backlog, but they will catch up. These children no longer have those possible malformations that, unfortunately, would have necessarily arisen in past years.
These children no longer have those possible malformations that, unfortunately, would have necessarily arisen in past years.
And this became possible thanks to the experience, the accumulation of knowledge about how such babies develop. There are no small things. This applies to everything - how to evaluate the heartbeat, how to interpret blood tests, and so on. Caring for a premature baby, both in the neonatal period and later, in the first or second year of life, is not the same as managing a normal, full-term baby. But knowledge allows timely adjustment of development, without even waiting for problems.
Photo: Science Photo Library / East News
It is important to understand that a premature baby is not a reduced copy of a normal one. This is a child who is forced to adapt to extrauterine life, when physiologically he should not do this. Its organs and systems are not prepared to function in the new conditions.
"This is painful love at the level of deep depression"
What do such children most often suffer from?
One of the typical pathologies is retinopathy of prematurity. In children, the mechanism that protects the eye from light has not yet matured. And they experience a real shock, suddenly falling into our bright world. Photons of light and the flow of oxygen begin to act on the retina, its vessels begin to grow rapidly, penetrate all the media of the eye, and, ultimately, exfoliate the retina, leading to total blindness. Earlier, even when I was just starting to work, although we knew about such a disease as retinopathy of prematurity, there were few children born and surviving at gestational ages of less than 30 weeks. Therefore, no one knew how to treat this disease. It's scary to remember, but premature babies were in wards with round-the-clock lighting. The light was needed so that doctors and nurses could observe the baby's condition and notice changes in time. At that time, six out of ten children whose birth weight was less than a kilogram went blind. Just then, the borders were opened in Russia, and we were amazed that in Europe, a maximum of two out of ten newborns had blindness.
In children, the mechanism that protects the eye from light has not yet matured. And they experience a real shock, suddenly falling into our bright world. Photons of light and the flow of oxygen begin to act on the retina, its vessels begin to grow rapidly, penetrate all the media of the eye, and, ultimately, exfoliate the retina, leading to total blindness. Earlier, even when I was just starting to work, although we knew about such a disease as retinopathy of prematurity, there were few children born and surviving at gestational ages of less than 30 weeks. Therefore, no one knew how to treat this disease. It's scary to remember, but premature babies were in wards with round-the-clock lighting. The light was needed so that doctors and nurses could observe the baby's condition and notice changes in time. At that time, six out of ten children whose birth weight was less than a kilogram went blind. Just then, the borders were opened in Russia, and we were amazed that in Europe, a maximum of two out of ten newborns had blindness.
But we started learning very quickly. Now in perinatal centers in all intensive care units for premature babies - twilight. The cuveuses are completely covered with dark blankets. The staff does not need to watch the baby all the time - all readings are automatically recorded by special devices. In good ICUs, nurses who approach babies have headlights. This is to avoid disturbing other children. In many intensive care units, a large “ear” hangs. If the decibel level in the room begins to exceed the allowable limit, the device lights up red.
After the birth of the child, every week they begin to look at the eyes with a special method. If there is proliferation of blood vessels, laser coagulation of the retina is performed. There are specialists in such operations in almost every major city.
Approximately 400-600 babies pass through me every year, born at 26-28 weeks. Over the past few years, not a single blind person has been among them. Although earlier in hospitals for such newborns it was necessary to open entire departments.
Is there any data on how many premature babies later became healthy?
Now, among premature babies born at five or six months (25-26 weeks of pregnancy), 25-30 percent become disabled. The same is true in developed countries. And even 20-30 years ago there were 75-80 percent of them.
The risks for these children are still very high. They require long-term observation and treatment. But still today they have incommensurably or better chances than before.
Photo: East News
Do unfortunate parents regret insisting on resuscitation at all costs?
As a doctor, no one has ever told me this. Naturally, the families had very different hopes for childbirth. In the doctor's office they cry, but they don't moan. These children are madly loved. But this is painful love at the level of deep depression. Probably, some of these mothers may think at night what would happen if they knew in advance how everything would turn out. Perhaps they voice this to their mothers, husbands, girlfriends . .. But not to doctors. This is where people prefer to stay.
.. But not to doctors. This is where people prefer to stay.
When a child is one or two years old, from a moral point of view, the situation is more difficult than in three days. Newborns are all wonderful bags, it is only then that children begin to differ from each other. These families have a very specific and difficult life. When a child lies at home, does not move, does not swallow, never looks at you, does not speak - this is very difficult. And parents need to be helped to turn their life into at least a relatively social one, not to make them outcasts.
What family support can I expect now?
When Russia switched to WHO standards, doctors began to say that if we started caring for such children, there would be a high incidence of cerebral palsy, mental retardation and other pathologies leading to severe disability. Without the development of a specialized service that will help such children, we will inflict enormous damage on a society that will not accept such an increase in the number of people with disabilities. Then a follow-up system for premature babies began to develop, which leads them up to three years. Because in the usual polyclinic network there are not always doctors who understand how a child born with low or extremely low body weight grows and develops. In parallel with this, the system of medical rehabilitation is developing quite rapidly.
Then a follow-up system for premature babies began to develop, which leads them up to three years. Because in the usual polyclinic network there are not always doctors who understand how a child born with low or extremely low body weight grows and develops. In parallel with this, the system of medical rehabilitation is developing quite rapidly.
The worst situation is with the social service. Help for these children is minimal. Few people explain to families how to care for such a child, how to develop him, how to maintain motor skills. If in large cities at least some minuscule can be achieved, then what can we say about the province? All this turns one of the parents out of social life. There are no places where it would be possible to transfer such a child at least for a week, a month, so that the parents could have a little rest. Since the state has taken such a step, since we have legally recognized a 500-gram fetus as a person, then they themselves also need to act humanly in the future with his family.
Is there a support system in other countries?
I know that in Europe and in the USA it is built very well. The emphasis is not on medical rehabilitation, but on social rehabilitation. They have social workers who come and relieve these families of a significant part of their worries. Somewhere there are social centers where a child can be taken to a kindergarten. Moreover, they are zoned - parents do not need to go to the other end of the city.
Photo: Alexander Kondratyuk / RIA Novosti
“Even if it is clear that a child has pathologies that are incompatible with life, they must be saved to the last”
You say that some time ago, 1kg premature babies were also considered “non-residents”, but now they are quite promising. Is it possible that in 30-40 years the same can be said about 500-gram ones?
Indeed, even 30-40 years ago, when it was not possible to maintain breathing, children born before seven months of age survived very rarely.
Then, when some first mechanisms appeared, the bar was raised until the 28th week of pregnancy, which is about six months. But technological progress is always moving forward, and this has allowed us to further gradually reduce the age of survival. We can now at least partially simulate intrauterine conditions. For example, when a child is not born on time, he does not yet have a substance in his lungs, thanks to which he can breathe - surfactants. They can be introduced immediately at birth, start artificial ventilation of the lungs and thereby support gas exchange. It also became possible to give nutritional subsidies not through the gastrointestinal tract, but through a vein with special substances that are already ready for inclusion in metabolism. There are many other adaptations: the creation of a thermal regime, humidity close to intrauterine.
But technological progress is always moving forward, and this has allowed us to further gradually reduce the age of survival. We can now at least partially simulate intrauterine conditions. For example, when a child is not born on time, he does not yet have a substance in his lungs, thanks to which he can breathe - surfactants. They can be introduced immediately at birth, start artificial ventilation of the lungs and thereby support gas exchange. It also became possible to give nutritional subsidies not through the gastrointestinal tract, but through a vein with special substances that are already ready for inclusion in metabolism. There are many other adaptations: the creation of a thermal regime, humidity close to intrauterine.
Technologically, the frontier could move indefinitely. If desired, you can simulate a situation where a woman is not needed at all to bear a child. But I have already said that scientists have established that the age of 22-23 weeks is the minimum period at which the cells of the cerebral cortex can develop postnatally. Still, the main criterion for the normal development of a child is not technological achievements, but the capabilities of the brain.
Still, the main criterion for the normal development of a child is not technological achievements, but the capabilities of the brain.
Is it true that they try to save all 500-gram children only in Russia and Turkey, and in other countries - only if the child has high chances for a normal life?
This is not true. In all countries where the WHO concept has been adopted, these children are subject to mandatory medical care. But there are nuances. If the baby was born between the 23rd and 25th weeks, parents can refuse resuscitation. To do this, in many countries there is a legal standard, reminiscent of the law on euthanasia.
There is a special service in perinatal centers. When it becomes clear that preterm labor has begun, representatives approach relatives - the father and, if possible, the mother. “We assume that a baby will be born with such and such parameters. In this case, there are such and such development risks ... You have the right to choose either full resuscitation or palliative care. And depending on what the parents decide, the doctors act.
And depending on what the parents decide, the doctors act.
Photo: Sergey Pyatakov / RIA Novosti
In Russia, you can also choose a palliative today, right?
This is not prescribed by law. Today, even if it is clear that a child has pathologies incompatible with life, they must be saved to the last. It happens that parents can sign a paper on their own that they would not like resuscitation, but this has no legal force. Parents can say, “Look, he is breathing, breathing. He opened his eyes. Let's revive him now!" And we lost time, which in this case is very important. This child initially has little chance, but it has become even less. And a situation may arise when parents accuse the doctors that their child was not specially treated, “talking teeth”.
The medical community is very concerned about this ambiguous position of doctors. And we have a number of proposals to solve the problem of their protection.
What exactly is offered?
Legislative initiative to allow parents to independently decide whether resuscitation care is appropriate for a child born between the 23rd and 25th weeks.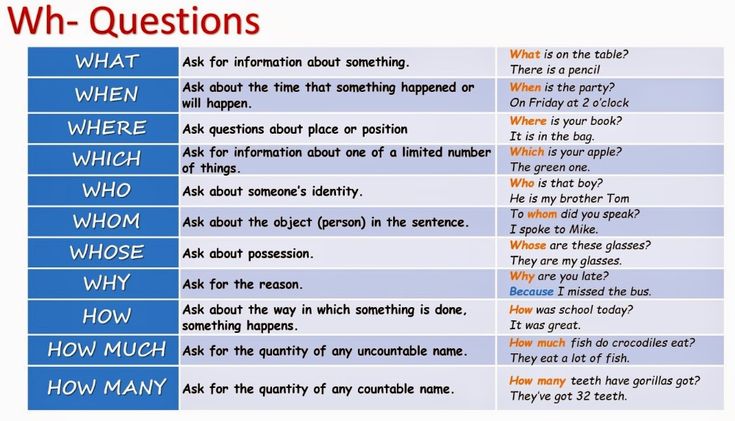 Naturally, all this should be discussed. It is necessary to involve the public in the discussion: these are lawyers, doctors, patient communities, representatives of religious denominations.
Naturally, all this should be discussed. It is necessary to involve the public in the discussion: these are lawyers, doctors, patient communities, representatives of religious denominations.
The Ministry of Health has now prepared new criteria for newborns born too early. In particular, it is proposed not to register such a child until he has lived seven days. Maybe this will fix the situation, protect doctors from murder charges?
There are a lot of pitfalls here. In Russia, there was a similar law on kilogram children. They were assisted from birth, but until the age of seven days the child was considered a fetus. If he died, then his mortality already went into other criteria, it was not considered the death of a newborn.
There are not many children born with extremely low rates, they simply cannot influence the demographic structure in any way. But if there is such a situation that you can not register for up to seven days, it seems to me that even more claims may arise against doctors regarding the failure to provide assistance.
These are very difficult questions. On the one hand, parents can say: you did not save the child. And others, on the contrary, will say: why are you torturing him in vain? And imagine a resuscitator who may be faced with an ethical choice: he has only one ventilator in the hospital, and a 23-week-old baby has been on it for the 40th day. And then a 32-week-old is born in the hospital. He needs help, hold him for three days on the device, and then the baby will cope on his own. In the first case, there will certainly be a disabled person. And in the second - almost healthy. And what should a doctor do?
Are you speaking theoretically now or do such situations occur?
We cannot have this in federal centers. We have enough equipment. I just illustrated with an example that the issue of nursing such children is the most difficult, all aspects are in common in it - from medical to ethical and religious.
Photo: Sergey Krasnoukhov / RIA Novosti
“The issue of infant mortality has always been political”
The issue of infant mortality has recently become political.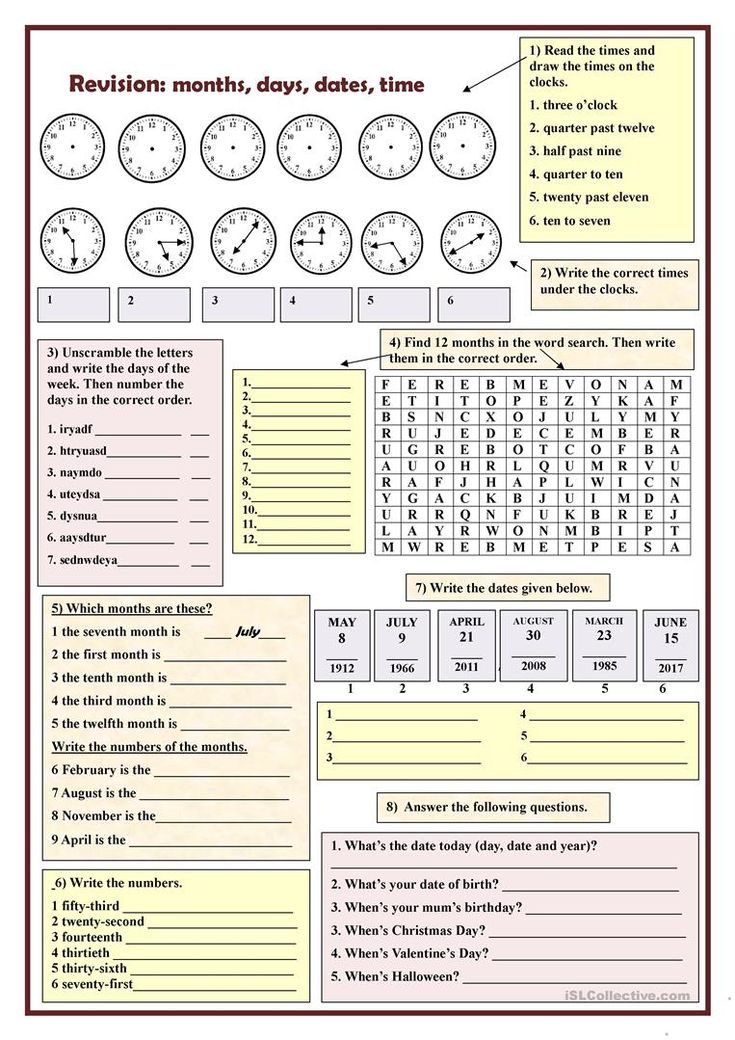 Perhaps that is why patient scandals associated with maternity hospitals are developing so sharply?
Perhaps that is why patient scandals associated with maternity hospitals are developing so sharply?
The issue of infant mortality has always been political. This is a socially significant parameter that determines the position of the country in terms of development. In our country as a whole, infant mortality has significantly decreased over ten years. However, in the last two years the rate of decline has slowed down. Our government says it's bad. From the point of view of doctors, this is not entirely true. There are objective reasons that cannot be overcome with a swoop.
The primary decrease in mortality occurred due to the high-quality saturation of hospitals with equipment, due to the construction of perinatal centers. This gave immediate results. And now these figures have reached a plateau. Another thing is that a plateau, for example, in Kaliningrad, St. Petersburg, is one thing. There mortality rates are at the European level. That is very low. And there are regions where mortality is high - the Altai Territory, the Jewish Autonomous Region, Magadan. There is a lack of doctors, a lack of equipment, very long distances, routing difficulties. And it's very difficult to do anything about it.
There is a lack of doctors, a lack of equipment, very long distances, routing difficulties. And it's very difficult to do anything about it.
We are not compact Switzerland. We have a huge country with difficult geographical conditions. There are regions where we cannot even deliver a woman by helicopter. At one time I spent a lot of time in Chukotka, watching the obstetric service. Often, if a premature baby is born there, you will not help him in any way.
There are no good hospitals there?
Everything is there, but in one city - in Anadyr. And if a woman gave birth in another place, then often she can be cut off from the world. There are periods when even planes do not fly: a snowstorm, something else. And with routing too you will not guess. Because when you are expecting your first child, you are not going to give birth at 24 weeks. This is if the situation with childbirth repeats, then you can plan something, come closer to specialized care at the “dangerous” time . ..
..
Is it true that there have been more premature births lately?
No, their number is stable. This is approximately 7-10 percent of all newborns. Significantly increased their survival rate.
One of the most "inciting" topics on parenting Internet forums is that children who are "culled out" by nature have a bad effect on the quality of the gene pool. Is there any reason to think so?
In order for the “survivors” to influence the population, there must be a lot of them in percentage terms. For example, there are very few 26-week-olds - no more than two percent of all births. It can't affect anything in any way.
I know that at one time they discussed: what will happen if my child marries in the future someone who was once premature, will the gene pool suffer? Firstly, I can say that, as for children born after the 30th week, they are completely healthy, adapted and no different from others. They themselves give birth to beautiful healthy children, we have already seen many generations.