Can you get mastitis while pregnant
Infections in Pregnancy: Mastitis | Healthline
Infections in Pregnancy: Mastitis | HealthlineMedically reviewed by Janine Kelbach, RNC-OB — By the Healthline Medical Network on March 15, 2012
What Is Mastitis?
Mastitis is a breast infection. It commonly develops in breast-feeding women during the first few weeks after delivery. Occasionally, this infection occurs in breast-feeding women several months after the baby is born.
Mastitis develops when bacteria (usually staphylococci or streptococci) from the baby’s mouth enter into the breast through the mother’s nipple. This causes an infection and inflammation in and around the milk-producing glands. Typically, a woman with mastitis develops a fever and notices pain and redness in one area of the breast. She is likely to develop flu-like body aches and fatigue as well.
How Is Mastitis Diagnosed?
Mastitis is often easy to diagnose. Reporting the symptoms to your doctor should be enough for them to identify the problem and prescribe treatment. In fact, laboratory tests are seldom needed.
What Are the Complications of Mastitis?
If not recognized or treated, simple mastitis may progress into a collection of pus called an abscess. Your doctor will suspect an abscess if they find a lump beneath the area of redness on your skin.
The formation of an abscess is rare. Most women see their doctor when they experience breast pain and fever. However, it’s important to identify an abscess because it requires different treatment than mastitis.
What Are the Usual Treatments for Mastitis?
Mastitis typically responds to antibiotic treatment within 24 hours. Your doctor may prescribe the antibiotic dicloxacillin. If you’re allergic to penicillin, alternatives include erythromycin (Ery-Tab) or clindamycin (Cleocin). Also, you can clear the infection faster with continued breast-feeding or pumping. This will help remove milk from your breast.
If your mastitis doesn’t improve within 48 to 72 hours, you may develop an abscess. In these cases, treatment is more aggressive. A surgeon must lance (by incision) and drain the abscess. This may require a trip to the emergency or operating room. You may also need antibiotics. Depending on the severity of your infection, you may be given the antibiotics intravenously rather than orally.
In these cases, treatment is more aggressive. A surgeon must lance (by incision) and drain the abscess. This may require a trip to the emergency or operating room. You may also need antibiotics. Depending on the severity of your infection, you may be given the antibiotics intravenously rather than orally.
After the abscess is lanced, a sample of your breast tissue is sent to the laboratory. This will help doctors identify the bacteria that caused the infection. Doctors may also examine the sample to make sure cancer isn’t present. However, cancer is unusual in young women with mastitis.
What is the Outlook for Mastitis?
Antibiotics are usually effective when treating mastitis. However, in some cases antibiotic-resistant infections can be difficult to treat. In these cases, several antibiotics or probiotics may be prescribed.
Start a medication plan as soon as possible to reduce your risk of forming an abscess. If you follow treatment directions carefully, your case of mastitis will likely clear up within several days.
How Can You Prevent Mastitis?
Many new mothers find it helpful to speak with a lactation consultant before starting breast-feeding. A lactation consultant can give you information on how to properly breast-feed your baby and avoid breast-feeding problems such as mastitis.
Here are some other tips for reducing your risk of getting mastitis:
- Make sure you fully drain the milk from your breasts while breast-feeding
- Allow your baby to completely empty one breast before switching to another
- Change your breast-feeding position each time
- Check that your baby latches on properly during feedings
Q:
Can mastitis become a recurring problem during breast-feeding?
Anonymous patient
A:
Mastitis may reoccur for several reasons. Some of the factors include:
- – sore nipples or plugged ducts
- – a history of breast surgery or lumps
- – stress or fatigue
- – low iron (anemia)
- – breasts that aren’t fully drained (engorgement)
- – tight clothing (slows the flow of milk)
- – cigarette smoking (prevents the breast from emptying completely)
- – sleep position (may put too much pressure on the breast)
- – not finishing antibiotics from the original infection
Janine Kelbach RNC-OB Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
All content is strictly informational and should not be considered medical advice.
Last medically reviewed on February 18, 2016
- Parenthood
- Health & Well-being
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Arroyo, R., Martín, V., Maldonado, A., Jiménez, E., Fernández, L., & Rodríguez, J. M. (2010). Treatment of infectious mastitis during lactation: Antibiotics versus oral administration of lactobacilli isolated from breast milk. Clinical Infectious Diseases, 50(12), 1551-1558. Retrieved from
cid.oxfordjournals.org/content/50/12/1551.full - Mayo Clinic Staff. (2015, June 12).
 Mastitis. (2015, June 12)
Mastitis. (2015, June 12)
mayoclinic.org/diseases-conditions/mastitis/basics/definition/con-20026633 - Scott, J. A., Robertson, M., Fitzpatrick, J., Knight, C., & Mulholland, S. (2008). Occurrence of lactational mastitis and medical management: A prospective cohort study in Glasgow. International Breastfeeding Journal, 3, 21.
doi.org/10.1186/1746-4358-3-21 - What can I do about my repeated cases of mastitis? (2016, January 9)
llli.org/faq/repeatmastitis.html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Janine Kelbach, RNC-OB — By the Healthline Medical Network on March 15, 2012
Read this next
Mastitis
Medically reviewed by Michael Weber, MD
Mastitis is an inflammation of the breast tissue usually caused by infection.
 It occurs almost always in breast-feeding women. Find out about symptoms…
It occurs almost always in breast-feeding women. Find out about symptoms…READ MORE
What Causes Lumps in Breasts of Breastfeeding Women?
Medically reviewed by Karen Gill, M.D.
Lumps in the breasts of breastfeeding women are common. We explore seven possible causes for lumps and discuss home remedies and other treatment…
READ MORE
All About Breast Lymphoma: A Rare Form of Non-Hodgkin’s Lymphoma
Breast lymphoma is not breast cancer. It’s a rare type of non-Hodgkin's lymphoma, a cancer of the lymphatic system. Learn more.
READ MORE
Breast Self-Exam
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
A breast self-exam is a screening technique you can do at home to check for breast lumps. This exam can screen for tumors, cysts, or other…
READ MORE
When to Worry About Breast Pain
Most women will experience breast pain at some point in their lives, but only a few will be diagnosed with cancer.
 Learn the causes and when to visit…
Learn the causes and when to visit…READ MORE
What Can Cause Large Areolas and Is This Normal?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
The areola is the colored area around your nipple. Like breasts themselves, areolas come in all shapes, sizes, and colors. Many women worry that their…
READ MORE
Lipomas in the Breast: What You Need to Know
Medically reviewed by Meredith Goodwin, MD, FAAFP
Lipomas are common fatty tumors of the breast. They are generally harmless, but doctors will perform an exam to be sure the lump is a lipoma.
READ MORE
Why Are My Nipples Itchy?
Medically reviewed by Alana Biggers, M.D., MPH
Find out all you need to know about what causes an itchy breast or nipple, what treatments are available, and when you should seek medical help.

READ MORE
Infections in Pregnancy: Mastitis | Healthline
Infections in Pregnancy: Mastitis | HealthlineMedically reviewed by Janine Kelbach, RNC-OB — By the Healthline Medical Network on March 15, 2012
What Is Mastitis?
Mastitis is a breast infection. It commonly develops in breast-feeding women during the first few weeks after delivery. Occasionally, this infection occurs in breast-feeding women several months after the baby is born.
Mastitis develops when bacteria (usually staphylococci or streptococci) from the baby’s mouth enter into the breast through the mother’s nipple. This causes an infection and inflammation in and around the milk-producing glands. Typically, a woman with mastitis develops a fever and notices pain and redness in one area of the breast. She is likely to develop flu-like body aches and fatigue as well.
How Is Mastitis Diagnosed?
Mastitis is often easy to diagnose. Reporting the symptoms to your doctor should be enough for them to identify the problem and prescribe treatment. In fact, laboratory tests are seldom needed.
Reporting the symptoms to your doctor should be enough for them to identify the problem and prescribe treatment. In fact, laboratory tests are seldom needed.
What Are the Complications of Mastitis?
If not recognized or treated, simple mastitis may progress into a collection of pus called an abscess. Your doctor will suspect an abscess if they find a lump beneath the area of redness on your skin.
The formation of an abscess is rare. Most women see their doctor when they experience breast pain and fever. However, it’s important to identify an abscess because it requires different treatment than mastitis.
What Are the Usual Treatments for Mastitis?
Mastitis typically responds to antibiotic treatment within 24 hours. Your doctor may prescribe the antibiotic dicloxacillin. If you’re allergic to penicillin, alternatives include erythromycin (Ery-Tab) or clindamycin (Cleocin). Also, you can clear the infection faster with continued breast-feeding or pumping. This will help remove milk from your breast.
This will help remove milk from your breast.
If your mastitis doesn’t improve within 48 to 72 hours, you may develop an abscess. In these cases, treatment is more aggressive. A surgeon must lance (by incision) and drain the abscess. This may require a trip to the emergency or operating room. You may also need antibiotics. Depending on the severity of your infection, you may be given the antibiotics intravenously rather than orally.
After the abscess is lanced, a sample of your breast tissue is sent to the laboratory. This will help doctors identify the bacteria that caused the infection. Doctors may also examine the sample to make sure cancer isn’t present. However, cancer is unusual in young women with mastitis.
What is the Outlook for Mastitis?
Antibiotics are usually effective when treating mastitis. However, in some cases antibiotic-resistant infections can be difficult to treat. In these cases, several antibiotics or probiotics may be prescribed.
Start a medication plan as soon as possible to reduce your risk of forming an abscess. If you follow treatment directions carefully, your case of mastitis will likely clear up within several days.
If you follow treatment directions carefully, your case of mastitis will likely clear up within several days.
How Can You Prevent Mastitis?
Many new mothers find it helpful to speak with a lactation consultant before starting breast-feeding. A lactation consultant can give you information on how to properly breast-feed your baby and avoid breast-feeding problems such as mastitis.
Here are some other tips for reducing your risk of getting mastitis:
- Make sure you fully drain the milk from your breasts while breast-feeding
- Allow your baby to completely empty one breast before switching to another
- Change your breast-feeding position each time
- Check that your baby latches on properly during feedings
Q:
Can mastitis become a recurring problem during breast-feeding?
Anonymous patient
A:
Mastitis may reoccur for several reasons. Some of the factors include:
- – sore nipples or plugged ducts
- – a history of breast surgery or lumps
- – stress or fatigue
- – low iron (anemia)
- – breasts that aren’t fully drained (engorgement)
- – tight clothing (slows the flow of milk)
- – cigarette smoking (prevents the breast from emptying completely)
- – sleep position (may put too much pressure on the breast)
- – not finishing antibiotics from the original infection
Janine Kelbach RNC-OB Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
All content is strictly informational and should not be considered medical advice.
Last medically reviewed on February 18, 2016
- Parenthood
- Health & Well-being
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Arroyo, R., Martín, V., Maldonado, A., Jiménez, E., Fernández, L., & Rodríguez, J. M. (2010). Treatment of infectious mastitis during lactation: Antibiotics versus oral administration of lactobacilli isolated from breast milk. Clinical Infectious Diseases, 50(12), 1551-1558. Retrieved from
cid.oxfordjournals.org/content/50/12/1551.full - Mayo Clinic Staff. (2015, June 12).
 Mastitis. (2015, June 12)
Mastitis. (2015, June 12)
mayoclinic.org/diseases-conditions/mastitis/basics/definition/con-20026633 - Scott, J. A., Robertson, M., Fitzpatrick, J., Knight, C., & Mulholland, S. (2008). Occurrence of lactational mastitis and medical management: A prospective cohort study in Glasgow. International Breastfeeding Journal, 3, 21.
doi.org/10.1186/1746-4358-3-21 - What can I do about my repeated cases of mastitis? (2016, January 9)
llli.org/faq/repeatmastitis.html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Janine Kelbach, RNC-OB — By the Healthline Medical Network on March 15, 2012
Read this next
Mastitis
Medically reviewed by Michael Weber, MD
Mastitis is an inflammation of the breast tissue usually caused by infection.
 It occurs almost always in breast-feeding women. Find out about symptoms…
It occurs almost always in breast-feeding women. Find out about symptoms…READ MORE
What Causes Lumps in Breasts of Breastfeeding Women?
Medically reviewed by Karen Gill, M.D.
Lumps in the breasts of breastfeeding women are common. We explore seven possible causes for lumps and discuss home remedies and other treatment…
READ MORE
All About Breast Lymphoma: A Rare Form of Non-Hodgkin’s Lymphoma
Breast lymphoma is not breast cancer. It’s a rare type of non-Hodgkin's lymphoma, a cancer of the lymphatic system. Learn more.
READ MORE
Breast Self-Exam
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
A breast self-exam is a screening technique you can do at home to check for breast lumps. This exam can screen for tumors, cysts, or other…
READ MORE
When to Worry About Breast Pain
Most women will experience breast pain at some point in their lives, but only a few will be diagnosed with cancer.
 Learn the causes and when to visit…
Learn the causes and when to visit…READ MORE
What Can Cause Large Areolas and Is This Normal?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
The areola is the colored area around your nipple. Like breasts themselves, areolas come in all shapes, sizes, and colors. Many women worry that their…
READ MORE
Lipomas in the Breast: What You Need to Know
Medically reviewed by Meredith Goodwin, MD, FAAFP
Lipomas are common fatty tumors of the breast. They are generally harmless, but doctors will perform an exam to be sure the lump is a lipoma.
READ MORE
Why Are My Nipples Itchy?
Medically reviewed by Alana Biggers, M.D., MPH
Find out all you need to know about what causes an itchy breast or nipple, what treatments are available, and when you should seek medical help.

READ MORE
Pregnancy and the mammary gland
During pregnancy, in addition to growing hips and tummy, the breast undergoes one of the most amazing transformations. From the end of the first trimester, she prepares to produce milk.
From the end of the first trimester, she prepares to produce milk. It is especially important to monitor the condition of the mammary glands during this period, because many hormonal changes occur in the body.
In order for the expectant mother to feel good and also be able to easily establish breastfeeding, let's figure out together how to protect yourself from breast diseases.
What happens to the breasts during pregnancy
At 4-5 weeks, the breasts become more sensitive , soreness similar to PMS symptoms may appear. This is normal and you should not be afraid. Hypersensitivity usually goes away after the first trimester, but sometimes persists until the very birth. After 6 weeks, there is more melanin in the woman's body, which is why the nipples and areolas become darker.
After 6 weeks, there is more melanin in the woman's body, which is why the nipples and areolas become darker.
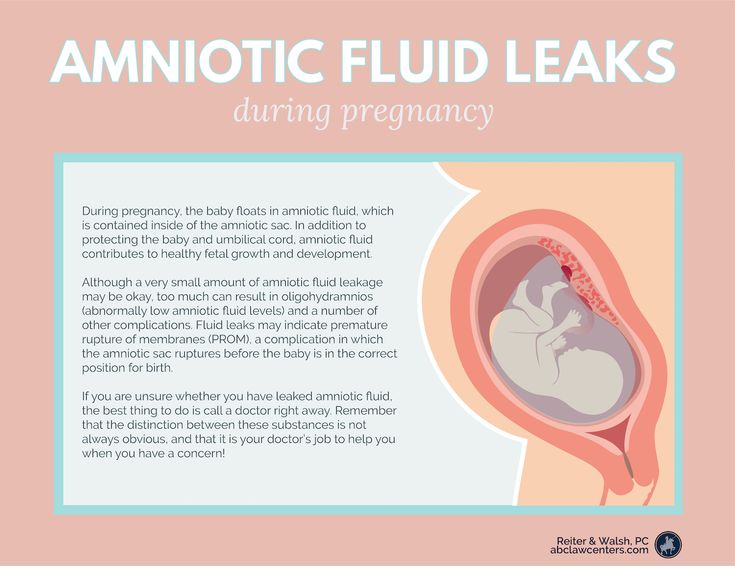
By 10-12 weeks of gestation, a complex system of ducts develops in the breast , the glandular tissue grows, and the nipples become more swollen and bulging, a noticeable vein network appears on the chest. This is normal and usually goes away after the baby is born.
At the beginning of the second trimester, yellowish discharge appears from the nipples . This is not milk yet, but similar in composition, but more nutritious colostrum is the first food for babies. So the mother's body prepares for a meeting with a newborn. Colostrum may be more actively secreted during intimacy or after a shower. Some women may experience even slight spotting from the nipple. They are associated with the destruction of small capillaries caused by the growth of ducts. Do not worry, but be sure to inform the gynecologist who is observing you
By 18 weeks, the bust may increase by 1-3 sizes . Therefore, it is very important to choose the right underwear that will not restrict movement and will be able to support the grown volumes well. It is recommended to pay attention to cotton bras with wide straps, pitted, but with lower support.
Therefore, it is very important to choose the right underwear that will not restrict movement and will be able to support the grown volumes well. It is recommended to pay attention to cotton bras with wide straps, pitted, but with lower support.
How to prepare your breasts for pregnancy
If you are just planning to become a mother, you should definitely pay attention to breast health.
Usually, experts recommend a routine ultrasound, but if you are over thirty years old or women in your family have breast problems, it is better to have a mammogram as well.
Mammograms are X-rays that are good at identifying even small tumors and cysts in tissues. In case of urgent need, it is also done for pregnant women, protecting the tummy from X-rays with a special apron. But such studies are not routinely carried out so as not to risk the health of the fetus.
If any pathologies, such as a cyst, have been identified, removal of will most likely be recommended. This is important to do before pregnancy and childbirth, as during lactation, cysts can block the ducts and become inflamed, causing mastitis.
This is important to do before pregnancy and childbirth, as during lactation, cysts can block the ducts and become inflamed, causing mastitis.
Therefore, it is very important to trace any diseases or changes before conception and stop them surgically or conservatively.
Bad advice: what not to do
There are many myths around breast preparation for lactation. For example, that the nipples need to be trained and rubbed with a wet towel to avoid cracks on them later.
In fact, the nipples of a woman who has given birth are quite capable of withstanding feeding, and cracks appear not from excessive sensitivity, but due to improper attachment of the baby.
In addition, the areola secretes its own protective layer, which helps the skin adapt to lactation. And if you often rub and wash your breasts, especially with soap, it will break down, which will lead to cracks in the nipples. If you have uterine tone, actively rubbing your nipples is also not recommended, as this can increase muscle tension.
Marketers actively advertise creams and oils for cracks and stretch marks. However, the effectiveness of such funds has not been scientifically proven. The number of stretch marks is associated to a greater extent with the hereditary elasticity of the skin.
So, to combat them, it is better to choose good supportive underwear and take a contrast shower.
Pregnancy risk factors
Hormonal changes and other changes in the body of a future mother can be a big test for a woman's body. Pregnancy usually does not provoke the appearance of pathologies. But, if a woman had an untracked tumor before pregnancy, during these 9 months under the influence of hormones, it can begin to grow actively, because up to 70% of tumors are estrogen-dependent.
Pregnancy, childbirth and lactation have long been thought to reduce the risk of breast cancer. Researchers have now found that this is not true.
Firstly, the risk of oncology decreases only for hormone-dependent cancers and in the long term, that is, after 15-20 years.But immediately after pregnancy increase.
This means that all women, regardless of age or status, should have an annual screening.
Sometimes women, experiencing pain in the chest, are afraid to go to the doctor, so as not to hear a frightening diagnosis. But breast cancer does not hurt, it is usually accompanied by other symptoms, such as :
- Formation of dense lumps and bumps in breast tissues;
- Asymmetric lumps and swellings in the chest;
- Sudden retraction of one or both nipples;
- Enlargement of lymph nodes in the armpits.
During pregnancy, the diagnosis is complicated by the peculiarities of the physiological state of the woman. Fatigue, breast enlargement, pain can also occur in healthy pregnant women.
In general, the same risk groups are distinguished for pregnant women as for other women:
- patients with hereditary predisposition;
- age after 40-45 years;
- early menarche;
- overweight;
- bad habits;
- lack of physical activity
How to protect yourself from breast cancer
Of course, the risk of breast cancer is present in all women and increases with age. Our task is to have time to identify it at an early stage.
Our task is to have time to identify it at an early stage.
If treatment is started at an early stage, then the percentage of patients in complete remission is very high
This means that every woman should give up bad habits, lead an active lifestyle and regularly visit a mammologist. If there are no associated risks, it is optimal to have a mammogram once a year after age 45.
Next article: Influenza vaccine Influvac
causes, symptoms, diagnosis and treatment in Moscow
Mastitis is an acute or chronic inflammation of the mammary gland caused by the penetration of a bacterial infection through the injured nipple or breast skin through the lymphatic tract. Most often, mastitis is diagnosed in a nursing woman. Also, the disease can develop in a pregnant woman, less often in girls, and sometimes, as a result of a malfunction of metabolic processes and disruption of the endocrine system, and in men.
At the very first symptoms of mastitis (tight and painful breasts, reddened skin, chills, fever), an examination by a specialist - a qualified mammologist - is necessary. Specialists of the NEARMEDIC network of clinics treat mastitis in accordance with international protocols. Experienced doctors provide professional medical care.
Specialists of the NEARMEDIC network of clinics treat mastitis in accordance with international protocols. Experienced doctors provide professional medical care.
If you notice signs of mastitis, call us and make an appointment online.
Why are we
Experienced doctors
In the network of NEARMEDIC clinics, breast mastitis is treated by highly qualified mammologists, some of them have more than 25 years of experience. The most experienced specialists constantly improve their skills, undergo training in leading specialized centers, regularly take part in seminars and conferences dedicated to problems in mammology.
Powerful modern equipment
The clinics are equipped with the latest equipment manufactured by the world's leading companies: high-precision digital ultrasound machines, X-ray units with reduced radiation dose, highly sensitive sensors, analog mammographs, etc.
Features of diagnosis and treatment of mastitis
Acute lactational mastitis begins abruptly and unexpectedly. Cracks appear on the nipples, bursting pains in the mammary gland. The chest swells, becomes painful, the skin may turn red, chills and hyperthermia appear - the body temperature rises to 39-40 degrees. It becomes more and more difficult to express breast milk, and severe pain is felt in the area of redness.
Cracks appear on the nipples, bursting pains in the mammary gland. The chest swells, becomes painful, the skin may turn red, chills and hyperthermia appear - the body temperature rises to 39-40 degrees. It becomes more and more difficult to express breast milk, and severe pain is felt in the area of redness.
Is it possible to breastfeed a child with mastitis? This is one of the most common questions, which, unfortunately, experts give a negative answer. Breastfeeding with any form of mastitis is prohibited due to the presence of pathogenic microorganisms in the milk, which can cause disruption of the gastrointestinal tract in an infant
But the chest must be pumped constantly, even when the pain is severe.
In some forms of the disease - infiltrative and serous mastitis, if there is no improvement after three days of treatment, mammologists suggest suppressing lactation.
If the cause of mastitis in women is not related to lactation or pregnancy, then we are talking about non-lactational mastitis. It occurs, as a rule, during the period of hormonal disorders - in women during menopause and menopause, in adolescents, and not only in girls, but also in boys. Sometimes mastitis in non-nursing occurs against the background of a decrease in immunity.
It occurs, as a rule, during the period of hormonal disorders - in women during menopause and menopause, in adolescents, and not only in girls, but also in boys. Sometimes mastitis in non-nursing occurs against the background of a decrease in immunity.
Diagnosis of mastitis
To confirm mastitis, a mammologist prescribes a microbiological examination of milk from both mammary glands. Laboratory research identifies the pathogen and assesses the degree of microbial colonization. The doctor also prescribes an analysis of women's milk for leukocytes. The number of leukocytes in the disease is significantly increased, especially with purulent mastitis.
In destructive forms of the disease, a mammologist prescribes an ultrasound examination of the mammary glands, which makes it possible to accurately determine the localization of purulent contents. In chronic mastitis, mammography is prescribed - an X-ray examination of the breast, as well as a biopsy and subsequent histological examination for differential diagnosis with breast cancer.
Treatment of mastitis
Conservative treatment of the disease is carried out in the following cases:
- satisfactory general condition of the patient;
- no more than three days have passed since the onset of mastitis;
- body temperature not higher than 37.5 degrees;
- no signs of purulent inflammation;
- the size of the palpable infiltrate is not more than one quadrant of the gland;
- moderate soreness in the area of the infiltrate;
- indicators of the general blood test are normal.
If conservative treatment does not give visible results, this most often indicates purulent inflammation and is an indication for surgical intervention.
Treatment of acute non-lactational mastitis depends on the degree of the disease. Conservative antibiotic treatment is carried out if the formation of an abscess has not yet begun. If an abscess has begun, an abscess is opened.
Preventive measures
Prevention of mastitis consists in strict observance of personal hygiene during pregnancy and in the postpartum period, increased immunity, proper care of the mammary glands, timely treatment of nipple cracks and lactostasis.