Can stress cause labor
Effect of maternal stress during pregnancy on the risk for preterm birth | BMC Pregnancy and Childbirth
- Research article
- Open Access
- Published:
- Caroline Lilliecreutz1,
- Johanna Larén1,
- Gunilla Sydsjö1 &
- …
- Ann Josefsson1
BMC Pregnancy and Childbirth volume 16, Article number: 5 (2016) Cite this article
-
35k Accesses
-
68 Citations
-
83 Altmetric
-
Metrics details
Abstract
Background
Preterm birth defined as birth prior to 37 weeks of gestation is caused by different risk factors and implies an increased risk for disease and early death for the child. The aim of the study was to investigate the effect of maternal stress during pregnancy on the risk of preterm birth.
Methods
A case–control study that included 340 women; 168 women who gave birth preterm and 172 women who gave birth at term. Data were manually extracted from standardized medical records. If the medical record contained a psychiatric diagnosis or a self-reported stressor e.g., depression or anxiety the woman was considered to have been exposed to stress during pregnancy.
Adjusted odds ratio (AOR) was used to calculate the attributable risk (AR) of maternal stress during pregnancy on preterm birth, both for the women exposed to stress during pregnancy (AR1 = (AOR-1)/AOR) and for the whole study population (AR2 = AR1*case fraction).
Results
Maternal stress during pregnancy was more common among women who gave birth preterm compared to women who gave birth at term (p <0. 000, AOR 2.15 (CI = 1.18–3.92)). Among the women who experienced stress during pregnancy 54 % gave birth preterm with stress as an attributable risk factor. Among all of the women the percentage was 23 %.
000, AOR 2.15 (CI = 1.18–3.92)). Among the women who experienced stress during pregnancy 54 % gave birth preterm with stress as an attributable risk factor. Among all of the women the percentage was 23 %.
Conclusions
Stress seems to increase the risk of preterm birth. It is of great importance to identify and possibly alleviate the exposure to stress during pregnancy and by doing so try to decrease the preterm birth rate.
Peer Review reports
Background
Each year 18 000 children in the Nordic countries are born preterm i.e., 6.6 % of all births and 12.9 million worldwide i.e., 9.6 % [1]. Preterm birth is the major risk factor for perinatal mortality and morbidity and deaths among preterm infants represent 63 % of all deaths in children <5 years [1]. More than two-thirds of all perinatal deaths are associated with preterm birth [2]. Due to technological advances in neonatal care the survival rate for extreme preterm births has increased [3].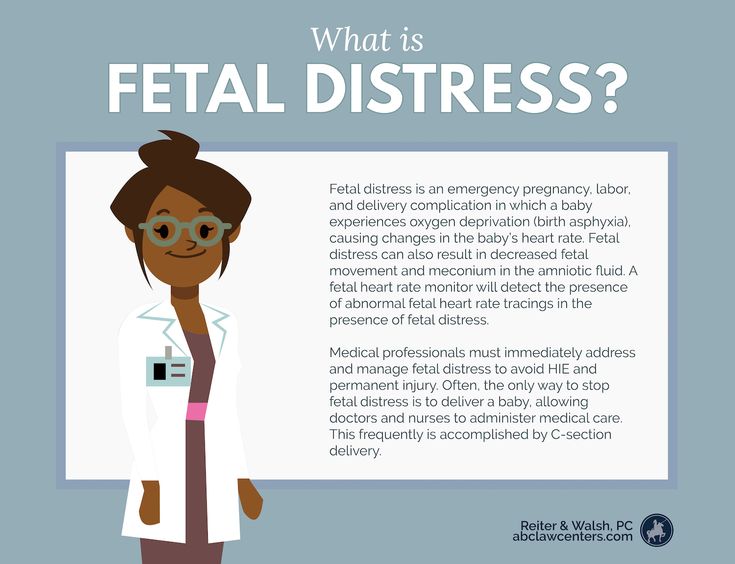 Preterm birth (<37 weeks of completed gestation) is associated with numerous risk factors and the causes is thought to be initiated by multiple mechanisms that might be interacting.
Preterm birth (<37 weeks of completed gestation) is associated with numerous risk factors and the causes is thought to be initiated by multiple mechanisms that might be interacting.
Multiple pregnancies, vaginal bleeding during pregnancy, and polyhydramnios or oligohydramnios are all associated with an increased risk for premature delivery [4]. Intrauterine infection leads to an activation of the immune system, and may subsequently lead to preterm birth. Low body mass index (BMI) during pregnancy is associated with increased risk for preterm delivery, and obesity is associated with disorders like preeclampsia and diabetes, which carry an increased risk for preterm birth. Maternal thyroid disease, asthma, hypertension as well as a history of cervical surgical procedures and uterus anomalies are associated with preterm birth [4]. Cigarette smoking carries an increased risk for preterm birth [5]. Nicotine and carbon monoxide are potent vasoconstrictors that are thought to cause placental damage and decreased uteroplacental blood flow [4]. Previous preterm delivery is also associated with an increased risk (OR 1.39, 95 % CI =1.29–1.50) for preterm birth in the next pregnancy [6]. These are all risk factors and probably indifferent of the presence of maternal stress.
Previous preterm delivery is also associated with an increased risk (OR 1.39, 95 % CI =1.29–1.50) for preterm birth in the next pregnancy [6]. These are all risk factors and probably indifferent of the presence of maternal stress.
Accumulating evidence both in human and animal studies suggests that maternal psychological and social stress during pregnancy represents conditions that may adversely affect the pregnancy outcome such as increased risk of morbidity for the child, lower birth weight and increase the risk for preterm birth. This is evident even after adjusting for other biomedical, socio-demographic and behavioral risk factors. The linking systems between mental and psychosocial processes within the mother to the fetus involve autonomic, neuroendocrine and immune systems [7–14]. Low socioeconomic and educational status, low and high maternal ages and single marital status have also been associated with preterm birth. Depression has been suggested to carry up to a 2-fold increased risk for preterm delivery [1].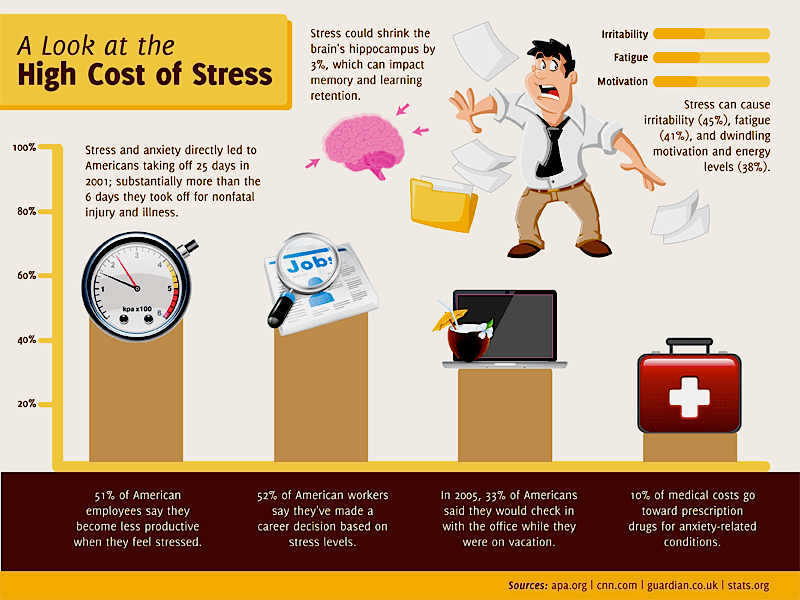 In utero exposure to either continuous SSRI treatment for depression or continuous depression without treatment has been associated with preterm birth [15–17]. Experience of stress during pregnancy is important to consider when caring for the pregnant women. Preterm birth has an impact on the newborn baby, the family and the health care system. The quantity and the load of stress needed for stress to become a risk factor for adverse outcome is still unknown.
In utero exposure to either continuous SSRI treatment for depression or continuous depression without treatment has been associated with preterm birth [15–17]. Experience of stress during pregnancy is important to consider when caring for the pregnant women. Preterm birth has an impact on the newborn baby, the family and the health care system. The quantity and the load of stress needed for stress to become a risk factor for adverse outcome is still unknown.
Hence our hypothesis was that maternal stress during pregnancy can attribute to the adverse outcome of preterm labor.
Thus, the aim of the study was to investigate the effect of maternal stress during pregnancy on the risk for preterm birth. This will be analyzed through the statistical method attributable risk (AR) which will be calculated in two different ways. First to estimate the proportion of women exposed to stress during pregnancy that give birth preterm due to stress as an attributable risk factor. Second to estimate the proportion of all women giving birth preterm due to stress during pregnancy as an attributable risk factor.
Methods
The study was designed as a case–control study with prospectively collected data. All women who gave birth before gestational week 37 during one year (2010) at Linköping University hospital were identified with the ICD-code for premature labour O60 in the computerized chart system Obstetrix®. All pregnancies and deliveries are registered in the chart system along with medical information and diagnosis during the antenatal period and admission to the delivery ward. The medical information of all study subjects were retrieved by manually inspecting the entries in Obstetrix® and transferring information to a spreadsheet. This was done by a senior medical student together with the first author (C L) in 2011. One hundred and sixty-eight women were diagnosed with preterm delivery and constitute the women from the index group. The control group consists of 172 women who gave birth after gestational week 37 at the same hospital during the same year. They were consecutively chosen from the chart system and matched for parity and age +/− 5 years. As for the study subjects who had delivered preterm, these individuals were retrieved by manually checking the entries in Obstetrix®.
As for the study subjects who had delivered preterm, these individuals were retrieved by manually checking the entries in Obstetrix®.
The total study population comprised 332 women as eight women in the index group experienced an intrauterine fetal death (IUFD) before term and therefore were excluded.
Risk factors for preterm birth were scrutinized in each woman’s medical record. Age, marital status (married/cohabiting or single), sick leave at first visit with the midwife (yes or no), level of socioeconomics/education (higher education, lower education, unemployed/parental leave, student), BMI in the beginning of the pregnancy (−24.9, 25–29.9, 30-), use of tobacco products (yes or no), alcohol or drugs (yes or no), and parity (0,1, 2 or more previous deliveries). Earlier pregnancies were divided into groups with no previous preterm deliveries and one or more previous preterm delivery, previous and/or current diseases (yes or no) e.g., diabetes, asthma, uterus malformation, cervix insufficiency, conization, systemic lupus erythematosus, fibromyalgia, urinary tract infections/bacteriuria, pyelonephritis, genital infection, inflammatory bowel disease, hepatitis, hypothyroidism, hyperthyroidism, mediterranean fever, and congenital heart defects. SSRI use during pregnancy (yes or no), twin pregnancies (yes or no), amniotic fluid pathology examined with ultrasonography (divided into three groups: normal amount of amniotic fluid, polyhydramnios and oligohydramnios) clinical signs of chorioamnionitis (yes or no), reported or observed premature contractions (yes or no), observed cervical changes (yes or no), reported or observed vaginal bleeding (yes or no), anemia defined as Hemoglobin <100 (yes or no), observed preterm premature rupture of membranes (PPROM) (yes or no), small for gestational age (SGA) defined as a birth weight < −2 SD of the mean weight for the gestational length, observed congenital defects by a pediatrician (yes or no), observed ablation (yes or no), observed preeclampsia (yes or no), onset of labor (spontaneous or induced), mode of delivery (vaginal, vaccum extraction or cesarean section), and gestational week at birth were manually extracted from the records.
SSRI use during pregnancy (yes or no), twin pregnancies (yes or no), amniotic fluid pathology examined with ultrasonography (divided into three groups: normal amount of amniotic fluid, polyhydramnios and oligohydramnios) clinical signs of chorioamnionitis (yes or no), reported or observed premature contractions (yes or no), observed cervical changes (yes or no), reported or observed vaginal bleeding (yes or no), anemia defined as Hemoglobin <100 (yes or no), observed preterm premature rupture of membranes (PPROM) (yes or no), small for gestational age (SGA) defined as a birth weight < −2 SD of the mean weight for the gestational length, observed congenital defects by a pediatrician (yes or no), observed ablation (yes or no), observed preeclampsia (yes or no), onset of labor (spontaneous or induced), mode of delivery (vaginal, vaccum extraction or cesarean section), and gestational week at birth were manually extracted from the records.
Maternal stress exposure was define as: having a psychiatric diagnosis according to medical records (depression, anxiety, fear of childbirth, psychosis, phobia and/or eating disorder) or if the patient’s medical record revealed self-reported stress.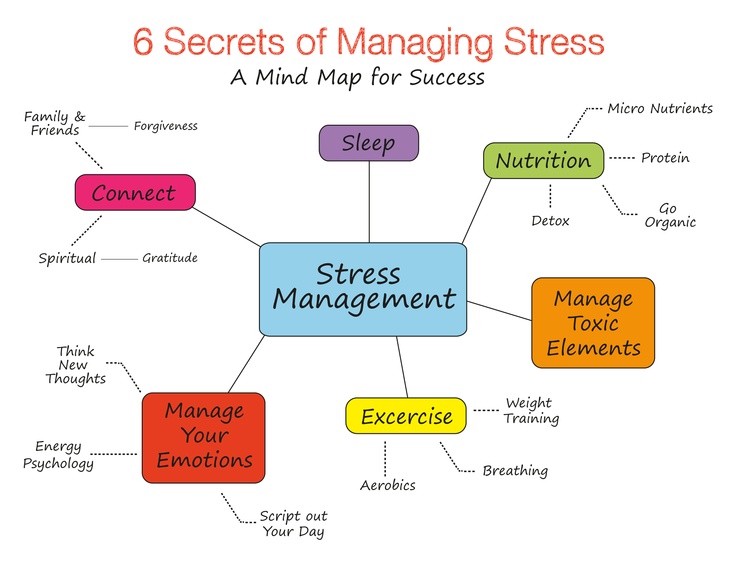 Self-reported maternal stress could be due to the pregnancy itself, previous traumatic experiences from pregnancy and childbirth, fear of congenital defects in the unborn child or injury. Lack of social support or a problematic relationship between the woman and her partner or with significant others as well as economic and work related problems were considered as stress exposure. These women were considered to have been exposed to stress during pregnancy.
Self-reported maternal stress could be due to the pregnancy itself, previous traumatic experiences from pregnancy and childbirth, fear of congenital defects in the unborn child or injury. Lack of social support or a problematic relationship between the woman and her partner or with significant others as well as economic and work related problems were considered as stress exposure. These women were considered to have been exposed to stress during pregnancy.
Statistics
The statistical analyses were done with SPSS (version 18). The rejection of the null-hypothesis was set to 0.05 (two-sided) in all statistical analyses. Student t-test was used to test differences between quantitative variables. Pearson’s Chi-square test was used to for testing differences in frequencies between categories. The possible effects of confounders were estimated through multiple logistic regression analyses and the adjusted odds ratios (AOR) were presented with a 95 % confidence interval. In these models, preterm delivery was set as dependent variable and identified confounding factors were considered as independent variables.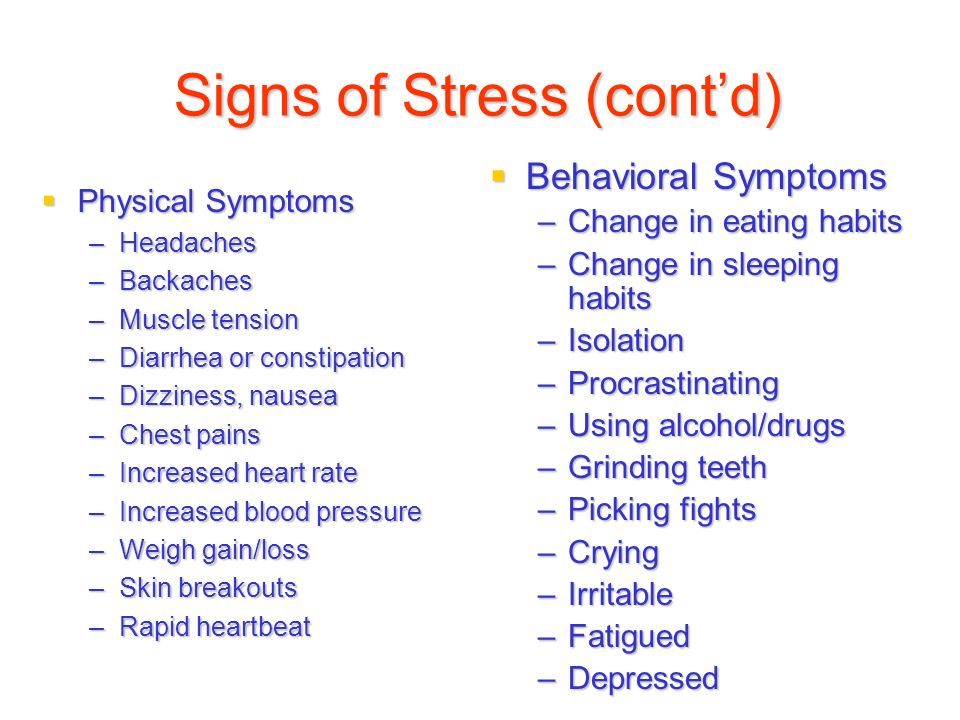 A variable theoretically causing both prematurity and maternal stress was considered a confounder. Of all the risk factors that were examined in this study; premature contractions, tobacco use, previous premature delivery, genital tract infection and twin pregnancy were considered as confounders. To verify these confounders correlations were computed. The correlations between stress and confounding factors were found to range between −0.062 and 0.268. Even though the correlations between stress and previous preterm delivery (ρ = 0.072), infection (ρ = 0.092), and twin pregnancy (ρ = −0.062) were low it was decided to keep this factors in the models based on previous theories on their importance with respect to preterm delivery [4].
A variable theoretically causing both prematurity and maternal stress was considered a confounder. Of all the risk factors that were examined in this study; premature contractions, tobacco use, previous premature delivery, genital tract infection and twin pregnancy were considered as confounders. To verify these confounders correlations were computed. The correlations between stress and confounding factors were found to range between −0.062 and 0.268. Even though the correlations between stress and previous preterm delivery (ρ = 0.072), infection (ρ = 0.092), and twin pregnancy (ρ = −0.062) were low it was decided to keep this factors in the models based on previous theories on their importance with respect to preterm delivery [4].
Attributable risk (AR), was estimated in two different ways. AR1 = (AOR-1)/AOR, was used to estimate how many of the women exposed to stress during pregnancy had delivered preterm because of the exposure as an attributable risk factor. AR2 = AR1*case fraction, with case fraction standing for the proportion of women delivering preterm who were exposed to stress during pregnancy.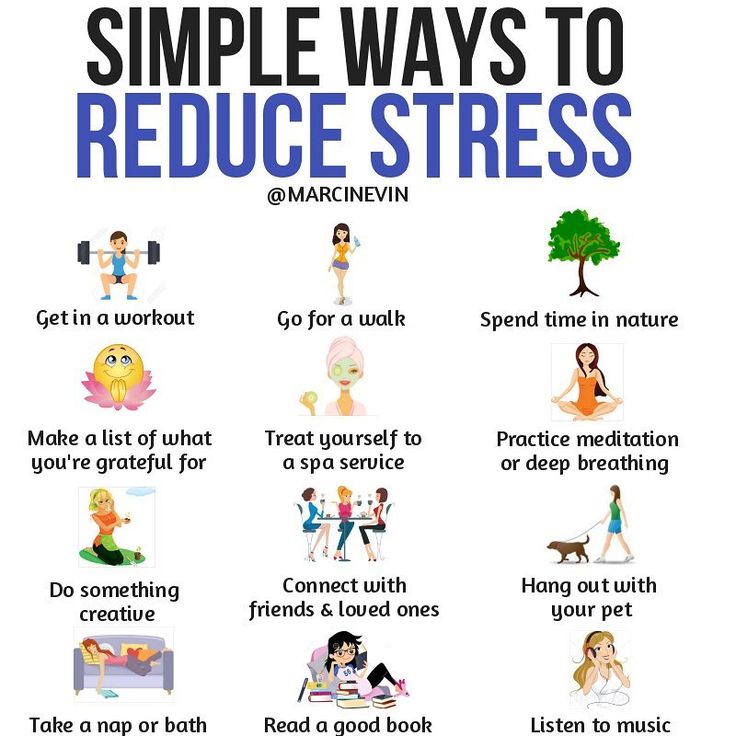 AR2 estimates how many women who delivered preterm in our study population did so because of the exposure to stress during pregnancy as an attributable risk factor.
AR2 estimates how many women who delivered preterm in our study population did so because of the exposure to stress during pregnancy as an attributable risk factor.
The present study was approved by the Ethical Review Board in Linköping, nr. 2011/183-31. Written informed consent for use of patient records in research is not required by the ethics committee standards.
Results
The distribution of the socio-demographic variables is shown in Table 1. Tobacco use as well as sick leave in early pregnancy were more common among the women from the index group compared with the control group (p = 0.007; p = 0.014). There were no women with drug addiction and one woman had an alcohol addiction during pregnancy in the index group.
Table 1 Socio-demographic data for the study populationFull size table
Previous and/or current diseases and conditions are shown in Table 2. Previous preterm birth was more common in the women from the index group compared with the control group (p <0. 000). There were two women in the index group and one woman in the control group with a uterus malformation. One woman in the index group had a cervical insufficiency.
000). There were two women in the index group and one woman in the control group with a uterus malformation. One woman in the index group had a cervical insufficiency.
Full size table
Obstetric variables are shown in Table 3. Women in the index group more often had a genital tract infection (p <0.000), premature contractions (p <0.000) or PPROM (p <0.000). SGA (p <0.000) was also more common in the women from the index group compared to women who gave birth at term. Preeclampsia was more frequent among the women in the index group (p <0.000). In 11 of the 14 cases with preeclampsia in the women from the index group, the labor was induced. Eight women with preeclampsia in the index group were delivered by cesarean section because of the preeclampsia. Labor was induced in three of the five cases with preeclampsia in the control group.
Table 3 Obstetric variablesFull size table
Induced labor and cesarean section were more frequent in the women from the index group (p = 0.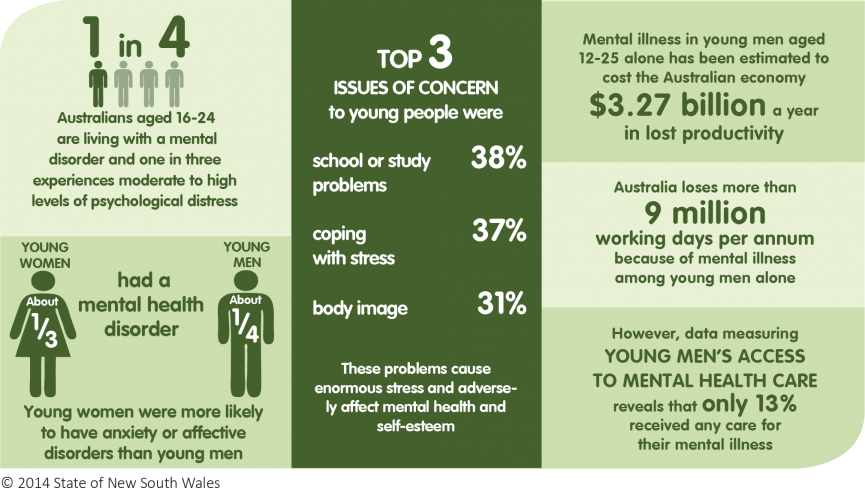 005; p <0.000). Women who gave birth at term were more often doing so spontaneously and by vaginal birth compared to the women from the index group (p = 0.005; p <0.000).
005; p <0.000). Women who gave birth at term were more often doing so spontaneously and by vaginal birth compared to the women from the index group (p = 0.005; p <0.000).
The differences in premature contractions, previous preterm delivery and genital tract infection between the women from the index group and the control group remained after adjustment for the identified confounders maternal stress during pregnancy, premature contractions, tobacco use, previous preterm delivery and genital tract infection (Table 4).
Table 4 Unadjusted and adjusted odds ratios for risk factors among women giving birth preterm compared to women giving birth at termFull size table
Maternal stress during pregnancy was more common among women who delivered preterm (p <0.000) compared to the control group and was still evident after adjusting for premature contractions, tobacco use, previous preterm delivery and genital tract infection (Table 4). The difference also remained in the multiple logistic regressions with the same adjustment after excluding the 24 cases of twin pregnancies from the total study population.
The difference also remained in the multiple logistic regressions with the same adjustment after excluding the 24 cases of twin pregnancies from the total study population.
There were 94 cases of PPROM in the women from the index group, and one woman with PPROM in the control group. Due to this, we could not estimate odds ratio (OR) for PPROM, and we were therefore unable to include PPROM in the multiple logistic regression. When excluding all cases of PPROM the unadjusted OR for maternal stress was estimated to be 2.82 (p = 0.002), compared to unadjusted OR, without exclusion of PPROM, at 2.94 (p <0.000). PPROM is considered more as a link in the process preceding preterm birth, rather than as a confounder.
There were 24 cases of twin pregnancies (no other multiple pregnancies were found in the study population) in the women from the index group, and no cases of twin pregnancies in the control group. As we were unable to calculate OR for twin pregnancies these were not included in the multiple logistic regression. OR for maternal stress after adjustment was estimated to be 2.15 (p = 0.012). After excluding all the cases of twin pregnancies from the women from the index group, the difference between the index group and the control group remained, when AOR for maternal stress was estimated to 1.91 (p = 0.049).
OR for maternal stress after adjustment was estimated to be 2.15 (p = 0.012). After excluding all the cases of twin pregnancies from the women from the index group, the difference between the index group and the control group remained, when AOR for maternal stress was estimated to 1.91 (p = 0.049).
Attributable risk (AR) was estimated in two different ways. AR1 was estimated to be 54 %, when using the adjusted OR. This means that 54 % of the women exposed to stress during pregnancy delivered preterm because of the exposure as an attributable risk. AR2 was estimated to be 23 %. This means that 23 % of all the women who delivered preterm in our study population did so because of exposure to stress during their pregnancy as an attributable risk.
Discussion
Several studies have previously suggested that women who experience psychological or social stress during pregnancy are at significantly increased risk for shorter gestation, earlier onset of spontaneous labor, low birthweight infant (<2500 g) and preterm delivery [7–15].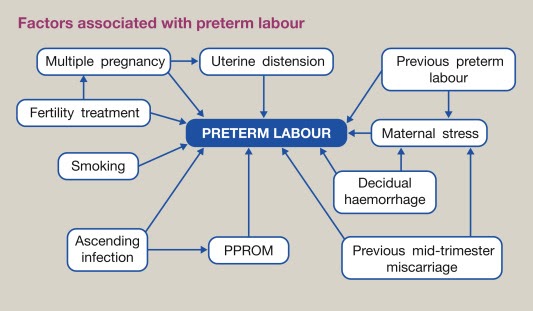
We have shown that maternal stress during pregnancy is more than twice as common among women who gave birth preterm compared to women who gave birth at term. The vast majority of the women exposed to stress during pregnancy, no matter what the origin or level of the stress was, gave birth preterm because of the exposure of stress as an attributable factor and in the total study population more than one fifth of the women gave birth preterm due to maternal stress during pregnancy as an attributable factor. Our study further establishes the already well-known risk factors like tobacco use, genital tract infection, previous preterm delivery and premature contractions.
The medical records in the Obstetrix® data system are standardized and prospectively recorded by midwives and obstetricians. The completion of information collected about women depends on accurate recording by medical staff and womens disclosure of personal information. This might be both strength and a limitation in the study.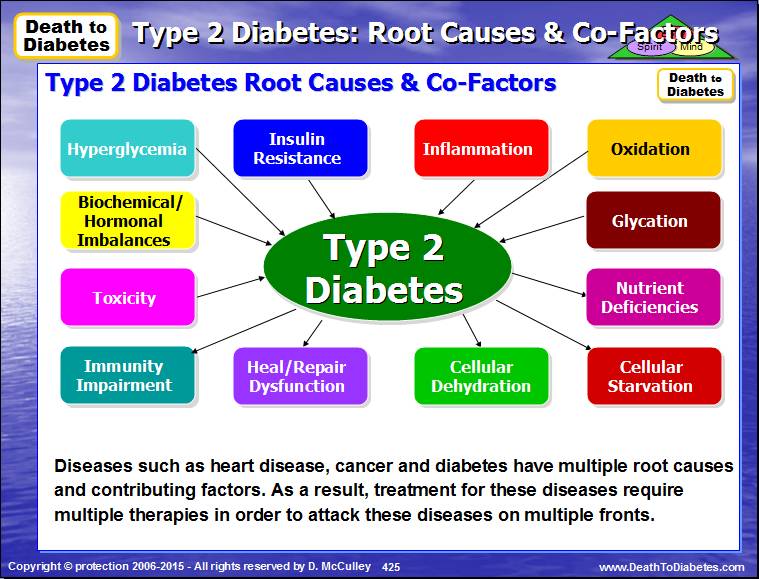 The effect is decreased or eliminated due to the fact that this problem exists in both the index and the control group.
The effect is decreased or eliminated due to the fact that this problem exists in both the index and the control group.
Another limitation in this study is the awareness of the pregnancy outcome as the medical records are retrospectively scrutinized. There is a risk that a woman with preterm delivery will be classified as having been exposed to stress during the pregnancy because of preconceived ideas about stress. This weakness has perhaps been decreased through discussions with a senior obstetrician/researcher not aware of the delivery being preterm or full term. A strength in this study is that the material comes from an unselected group of women giving birth during 1 year.
In the study we have not divided the material into spontaneous or induced labor. The reason for that is multiple; medical treatment sometimes prevents spontaneous start, induction of labor could be due to conditions caused by for example stress or infection. An induction is sometimes started shortly before spontaneous labor. The medical practice is therefore something that interferes with the natural course.
The medical practice is therefore something that interferes with the natural course.
In order to be considered a confounder in this study, the factor must be able to provoke both maternal stress and preterm birth independently. Thus sick leave in early pregnancy, amniotic fluid pathology, cervical changes, vaginal bleeding, placental abruption and preeclampsia where not considered as confounders and were therefore not adjusted for in the multiple logistic regression analyses. Twin pregnancies are associated with a high risk for preterm birth, with almost 60 % of all twins being delivered preterm. The cause is thought to be due to uterine distension which results in contractions and PPROM [4]. In our study the effect of maternal stress on preterm birth remained after exclusion of all the twins in the sample.
The relatively high AR1 might be due to our definition of maternal stress during pregnancy. We are not aware of any other study with this approach but if the study had concentrated on a specific diagnosis e. g., major depression the AR1 would probably have been lower. Clinical depression is suggested to carry up to a 2-fold increased risk for preterm delivery [16–17].
g., major depression the AR1 would probably have been lower. Clinical depression is suggested to carry up to a 2-fold increased risk for preterm delivery [16–17].
Our definition is interesting and important from a clinical perspective. It implies that even a stressor not causing a clinical diagnosis can have an impact on the risk for preterm birth. It seems that psychosocial risk factors e.g., financial problems, unemployment and unstable relationships can be of importance for the pregnancy outcome. A problem yet to be solved is what levels of stress affect the risk for preterm childbirth.
The findings in this study may also be the basis for discussions of the care of pregnant women exposed to stress. Future studies to examine interventions to reduce stress during pregnancy and the effect on preterm birth could be of importance.
Conclusions
Preterm birth negatively affects the newborn child, both in the short and long term. In conclusion, approximately 20 % of the preterm births in this study were estimated to be due to maternal stress exposure during pregnancy as an attributable risk factor.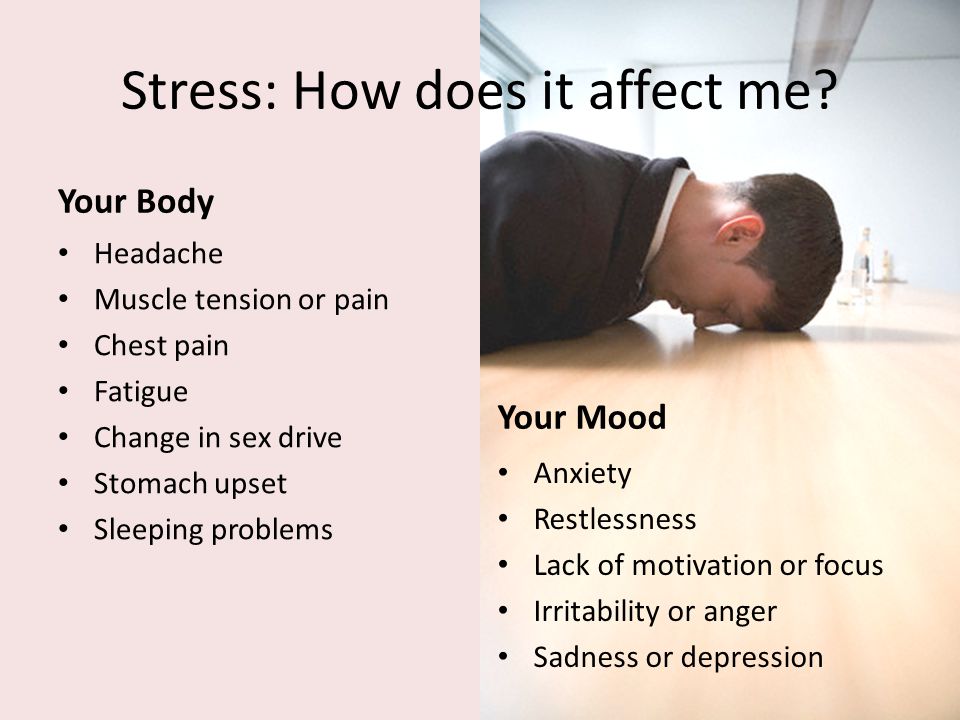 Thus it is of great importance to identify and possibly alleviate the exposure to stress during pregnancy and by doing that try to decrease the preterm birth rate.
Thus it is of great importance to identify and possibly alleviate the exposure to stress during pregnancy and by doing that try to decrease the preterm birth rate.
Abbreviations
- AOR:
-
adjusted odds ratio
- AR:
-
attributable risk
- IUFD:
-
intrauterin fetal death
- PPROM:
-
preterm, premature rupture of membranes
- SGA:
-
small for gestation age
References
Keller M, Felderhoff-Mueser U, Lagercrantz H, Dammann O, Marlow N, Huppi P, et al. Policy benchmarking report on neonatal health and social policies in 13 European countries. Acta Paediatr.
 2010;11:1624–9. 10.1111/j.1651-2227.2010.01894.x
2010;11:1624–9. 10.1111/j.1651-2227.2010.01894.xArticle Google Scholar
Murphy DJ. Epidemiology and environmental factors in preterm labour. Best Pract Res Clin Obstet Gynaecol. 2007;5:773–89. 10.1016/j.bpobgyn.2007.03.001
Article Google Scholar
Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;9608:261–9. 10.1016/S0140-6736(08)60136-1
Article Google Scholar
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;9606:75–84. 10.1016/S0140-6736(08)60074-4
Article Google Scholar
Crump C, Sundquist K, Sundquist J, Winkleby MA. Gestational age at birth and mortality in young adulthood.
 JAMA. 2011;11:1233–40. 10.1001/jama.2011.1331
JAMA. 2011;11:1233–40. 10.1001/jama.2011.1331Article Google Scholar
Bladh M, Josefsson A, Carstensen J, Finnström O, Sydsjö G. Intergenerational cohort study of preterm and small-for-gestational-age birth in twins and singletons. Twin Res Hum Genet. 2015;18:581–90. 26330196, 10.1017/thg.2015.60
Article PubMed Google Scholar
Federenko IS, Wadhwa PD. Women's mental health during pregnancy influences fetal and infant developmental and health outcomes. CNS Spectr. 2004;9:198–206. 14999160
Article PubMed Google Scholar
Entringer S, Buss C, Wadhwa PD. Prenatal stress, development, health and disease risk: a psychobiological perspective-2015 Curt Richter Award Paper. Psychoneuroendocrinology. 2015;62:366–75. 26372770, 10.1016/j.psyneuen.
 2015.08.019
2015.08.019Article PubMed Google Scholar
Wadhwa PD, Culhane JF, Rauh V, Barve SS. Stress and preterm birth: neuroendocrine, immune/inflammatory, and vascular mechanisms. Matern Child Health J. 2001;5:119–25. 11573837, 1:STN:280:DC%2BD3MrislCruw%3D%3D, 10.1023/A:1011353216619
Article CAS PubMed Google Scholar
Hoirisch-Clapauch S, Brenner B, Nardi AE. Adverse obstetric and neonatal outcomes in women with mental disorders. Thromb Res. 2015;135.
Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: a systematic review. Women Birth. 2015;28:179–93. 25765470, 10.1016/j.wombi.2015.02.003
Article PubMed Google Scholar
Christian LM. Effects of stress and depression on inflammatory immune parameters in pregnancy. Am J Obstet Gynecol. 2014;211:275–7. 24956551, 1:CAS:528:DC%2BC2cXhs1KltbbN, 4159131, 10.1016/j.ajog.2014.06.042
Article CAS PubMed PubMed Central Google Scholar
Glover V. Prenatal stress and its effects on the fetus and the child: possible underlying biological mechanisms. Adv Neurobiol. 2015;10:269–83. 25287545, 10.1007/978-1-4939-1372-5_13
Article PubMed Google Scholar
Brown S, Yelland J, Sutherland G, Baghurst P, Robinson J. Stressful life events, social health issues and low birthweight in an Australian population-based birth cohort: challenges and opportunities in antenatal care. BMC Public Health. 2011;11:196. 21450106, 3080815, 10.1186/1471-2458-11-196
Article PubMed PubMed Central Google Scholar
Straub H, Adams M, Kim JJ, Silver RK. Antenatal depressive symptoms increase the likelihood of preterm birth. Am J Obstet Gynecol. 2012;207:329e1–4. 10.1016/j.ajog.2012.06.033
Article Google Scholar
Wisner KL, Si DK, Hanusa BH, Moses-Kolko EL, Bogen DL, Hunker DF, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009;5:557–66. 10.1176/appi.ajp.2008.08081170
Article Google Scholar
Grigoriadis S, Vonder Porten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74:321–41. 10.4088/JCP.12r07968
Article Google Scholar
Download references
Acknowledgments
This investigation was supported by grants from The Medical Research Council of Southeast Sweden. We also thank PhD Ann-Britt Wiréhn for valuable statistical assistance.
We also thank PhD Ann-Britt Wiréhn for valuable statistical assistance.
Author information
Authors and Affiliations
Division of Obstetrics and Gynaecology, Department of Clinical and Experimental Medicine, Faculty of Health Sciences, Linköping University, SE-581 85, Linköping, Sweden
Caroline Lilliecreutz, Johanna Larén, Gunilla Sydsjö & Ann Josefsson
Authors
- Caroline Lilliecreutz
View author publications
You can also search for this author in PubMed Google Scholar
- Johanna Larén
View author publications
You can also search for this author in PubMed Google Scholar
- Gunilla Sydsjö
View author publications
You can also search for this author in PubMed Google Scholar
- Ann Josefsson
View author publications
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Caroline Lilliecreutz.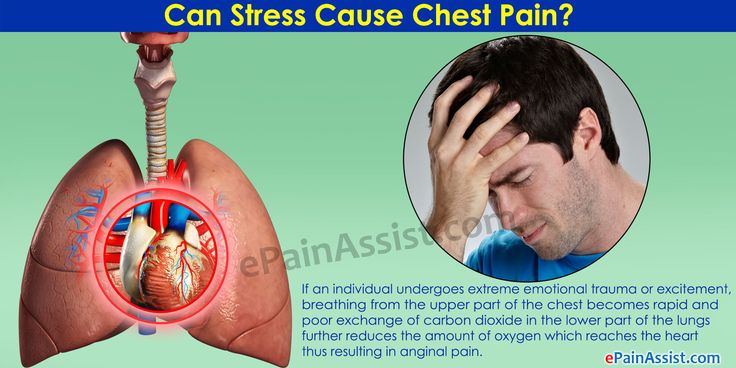
Additional information
Competing interests
The authors declare that they have no competing interests
Authors’ contributions
CL had the original idea for the study, planned the study, analysed the data and drafted the article. GS had the original idea for the study and planned the study, AJ had the original idea for the study and planned the study, JL planned the study, analysed the data and drafted the article. All authors contributed to the interpretation of the data, revisions, and gave input at all stages of the study. All authors have approved the final version of the article for publication.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.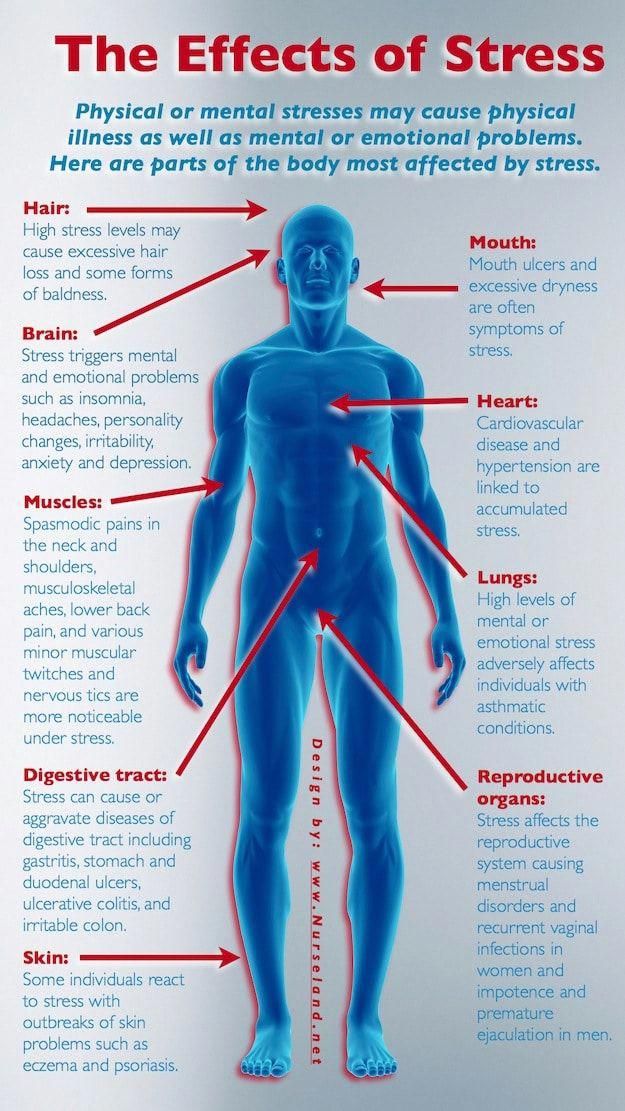 The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Reprints and Permissions
About this article
Can Stress Cause You To Go Into Labour?
There are many issues pregnant women worry about during their pregnancies.
It can be stressful talking with human resources about maternity leave, getting the nursery painted, studying or finishing off loose ends at work, as well as working out if there enough money to cover the rent each month.
The to-do lists and questions about life can seem never ending, and more so as you prepare for the arrival of your new addition.
If life seems to be going a million miles an hour and your stress levels are starting to feel sky high, you might wonder if all this stress could cause you to go into labour.
This might be particularly concerning if you’re not quite full term and feeling lots of stressors piling up. Of course, everyday life can be stressful. But add in unexpected circumstances such as a loss or break-up in the family or a physical stress (an injury or chronic pain), and it’s easy to see that most women wont be sailing through an entire pregnancy, without experiencing at least some stress.
Of course, everyday life can be stressful. But add in unexpected circumstances such as a loss or break-up in the family or a physical stress (an injury or chronic pain), and it’s easy to see that most women wont be sailing through an entire pregnancy, without experiencing at least some stress.
While stress can be a part of life, can too much stress impact when you’ll go into labour?
Can a sudden rise in stress trigger labour to begin?
In short, stress hormones can impact pregnancy, but whether or not it can result in labour is a bit more complex.
Stress Hormones And Pregnancy
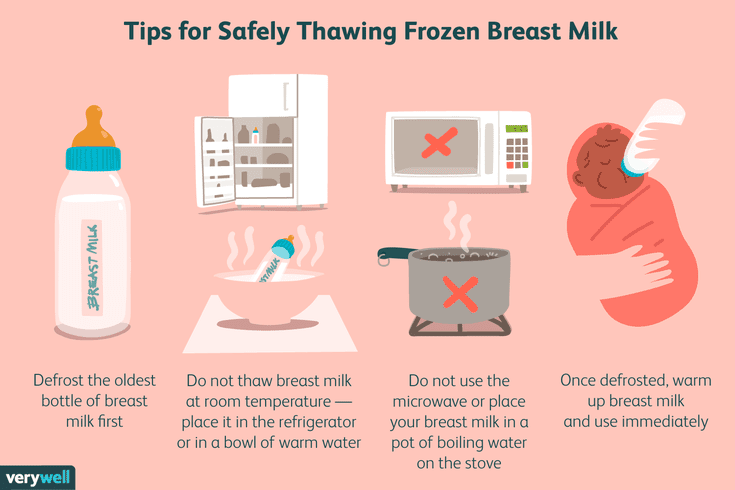
Conception, pregnancy and birth are very complex hormonal processes. While they’re natural processes, our bodies do a lot of work to conceive, grow, birth and breastfeed a baby.
During each stage of that process, several hormones work together to nourish and protect the baby, then eventually they all work together to birth the baby. However, the hormones of pregnancy and birth can be impacted by other hormones in our body.
When we experience ongoing stress, our bodies release cortisol (a major stress hormone), as well as pro-inflammatory proteins (cytokines) from immune cells.
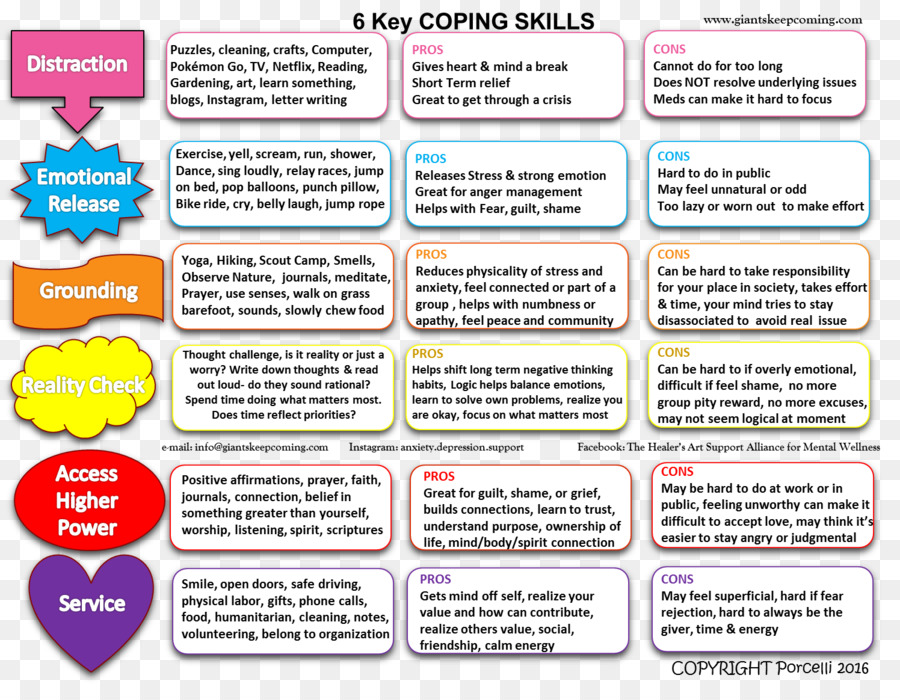
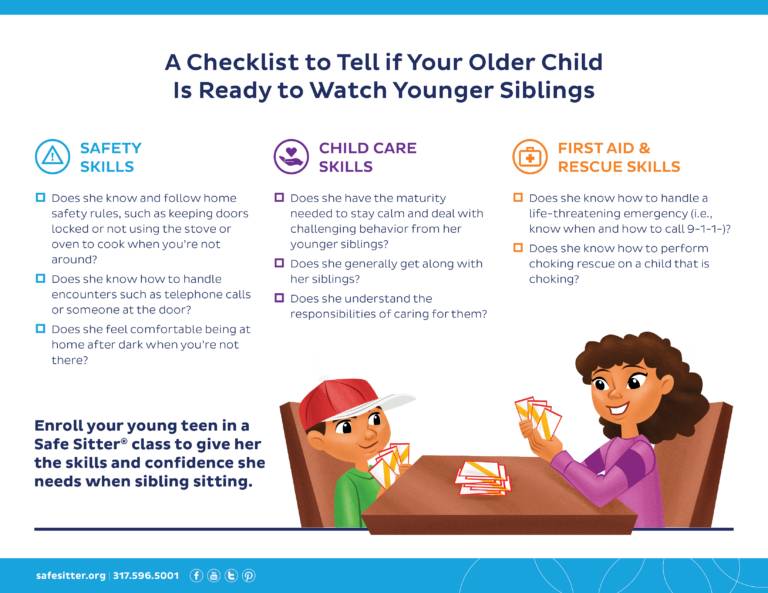
We all experience little daily stressors, and sometimes big events which are very stressful. If you have a good support system, have learned everyday stress coping techniques, and if you practice self-care, you’re likely able to manage those stressful situations in a healthy way.
However, for those who have ongoing stress (everyday stress and especially big events), it may lead to releasing cortisol and cytokines, which may then have an effect on pregnancy.
Inflammation which is caused by the cytokines and elevated levels of cortisol are linked to adverse pregnancy outcomes including:
- Pre-term birth
- Hypertension
- Babies with low birthweight
- Diabetes
- Preeclampsia
- Miscarriage
Reading that list can be a bit frightening, and you may think, “Um, don’t we all experience stress sometimes?!?”
Of course, we all experience stress sometimes. However, it’s important to realise that if you’re able to cope with daily stressors, your body is unlikely to be releasing ongoing inflammatory proteins and cortisol, which is what’s linked to adverse birth outcomes. Ongoing, poorly managed stress is what is related to pre-term birth and other adverse outcomes.
However, it’s important to realise that if you’re able to cope with daily stressors, your body is unlikely to be releasing ongoing inflammatory proteins and cortisol, which is what’s linked to adverse birth outcomes. Ongoing, poorly managed stress is what is related to pre-term birth and other adverse outcomes.
Can Sudden Stressful Situations Cause You To Go Into Labour?
Perhaps you’re able to keep a handle on everyday stress, but what about a sudden stressful event? The loss of a loved one, being laid off from work or having to suddenly move can all be unexpected and very stressful situations.
The evidence linking stress to triggering labour is related to ongoing, chronic stress. This means your body would have elevated levels of cortisol and cytokines for an extended period time, maybe even the length of your pregnancy. When these are elevated for a long period of time, the hormones can impact many bodily functions, and therefore your pregnancy.
It would be very unusual for a sudden and isolated incident of stress to trigger labour. Sometimes stress is the result of something physical, such as a car accident. In these situations, labour might be triggered, but it’s more than likely due to the physical impact of the event, rather than the emotional stress of the situation.
Sometimes stress is the result of something physical, such as a car accident. In these situations, labour might be triggered, but it’s more than likely due to the physical impact of the event, rather than the emotional stress of the situation.
Managing Stress During Pregnancy
We can’t always control our environments. Sometimes work will be stressful, toddlers will press all our buttons and unexpected bills might pop up. However, we can take steps to help control stress during pregnancy. An external stressor doesn’t always need to become a physical response.
Taking steps to manage stress, learning how to cope with stress and practicing self-care to recharge ourselves can make your pregnancy journey healthier.
Consider some of the following for effective stress management:
- Meditation (or prayer if religious) to take time to refocus
- Journaling to help process your experiences
- Enlisting help around the house with day to day tasks to lighten your load
- Coordinate childcare help or support to provide you with rest as needed
- Epsom salt baths or soaks, as well as aromatherapy
- Meet with a therapist (ideally experienced in prenatal issues) to help process challenging experiences
- Choose a maternity healthcare provider that offers continuity of care so coordinating your maternity care isn’t stressful
- Start planning and budgeting your maternity leave early in your pregnancy to avoid last minute rushing and stress
- If making your basic financial needs met is a major and ongoing stressor, find out what local resources are available for financial assistance, baby items, food, etc
- Make time for self-care, do an activity you enjoy
Recommended Reading: For more tips to help control stress during pregnancy check out BellyBelly’s article Stress During Pregnancy – 10 Tips To Combat Stress.
Psychological causes of premature birth - Charity Foundation "Give Sunshine"
Crisis of change
Pregnancy is perceived by our culture as a period of blissful expectation and strong contact of a woman with her nature. However, by awakening the most natural and joyful maternal instincts, pregnancy can activate fears and previously unresolved conflicts in a woman. These fears often develop on an unconscious level. Of course, this can also affect the development of the baby in the womb, and in some cases, strong intrapersonal conflicts and experiences can be one of the factors affecting preterm birth. nine0005
One of the reasons for the experiences of the expectant mother is often the theme of change. The familiar and the ordinary are replaced by the unknown. The fear comes that because of the birth of a child, you will have to change the whole way of life, devote less time to your hobbies, work, career. That is, life may completely change direction, all this causes background stress, which can affect the course of pregnancy.
Women who have a hard time accepting changes in their figure lose control of the situation here. Psycho-emotional instability increases the risk of premature birth or some kind of violation. Therefore, during pregnancy, you should carefully monitor your thoughts, beliefs, try to work out your fears and not withdraw into yourself, sometimes you should turn to an experienced psychologist. nine0005
Fear and anxiety about changes in life, fear of the future - this is inherent in many people, especially expectant mothers, but there is always a choice: to succumb to this fear or accept changes that can bring something wonderful to life.
Irritability
There are many reasons for preterm labor, both physiological and psychological. Each case is individual, previous experience, external environment, emotional trauma, losses and much, much more - all this can affect the health and condition of a pregnant woman, and, accordingly, a child. nine0005
Premature births are considered between 22 and 37 weeks of gestation.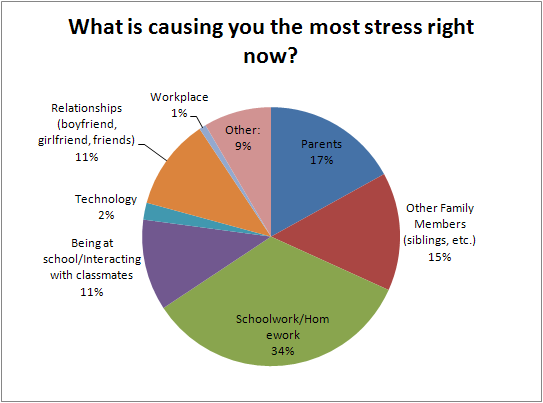 One of the serious psychological reasons for too early birth is often stress - the internal tension of the body in response to external stimuli.
One of the serious psychological reasons for too early birth is often stress - the internal tension of the body in response to external stimuli.
Irritability in pregnant women is more common in the second trimester and before childbirth. The reasons for this unstable state are due to several factors:
• The production of progesterone increases, during pregnancy its level rises many times. nine0005
• Increased physical and emotional stress along with changes in hormonal levels.
The psychological component is that a woman during the period of bearing a child is very vulnerable, she needs to feel the warmth and care of loved ones. Many pregnant women experience fear of childbirth and future motherhood, so the appearance of some increased irritability is quite natural.
In the third trimester of pregnancy, the child's nervous system is formed, so stress and strong irritability of the expectant mother is highly undesirable. Emotional turmoil and instability can threaten the normal development of the fetus.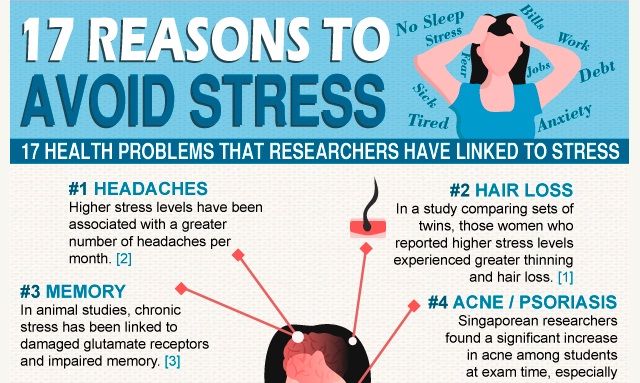 Poor psychological well-being and mood swings in the later stages should be more or less manageable. nine0005
Poor psychological well-being and mood swings in the later stages should be more or less manageable. nine0005
To control irritability, vitamins are sometimes prescribed, a varied diet, drawing is recommended (at least anti-stress coloring), moderate physical activity, such as yoga, Pilates and swimming. Along with this, it is worth enlisting the support of loved ones, explaining your condition to them and asking them to be attentive to their requests. At the same time, if you understand what specifically affects you in such a way that leads to irritability, try to formulate your request quite precisely and specifically, but without hurting the feelings of other people. nine0005
Misunderstanding
Throughout pregnancy, very complex hormonal changes occur in a woman's body, this affects her well-being and mood - whims, irritability for no particular reason, mood swings. About 20% of women experience depression during this period.
It is very difficult for the representatives of the stronger sex to understand what a woman feels during pregnancy, not only in terms of the physical, but also on the emotional level.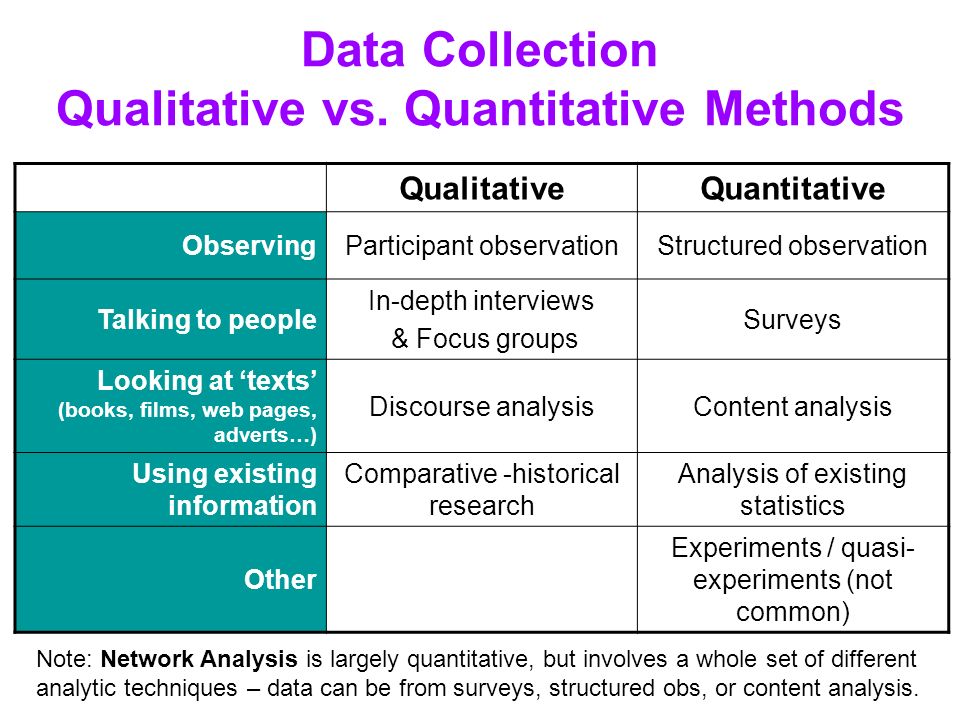 As a result, small disagreements begin to flare up in the family, which can gradually develop into serious disagreements. The lack of a sincere conversation about what is happening to each of the spouses negatively affects the relationship of the couple during pregnancy. nine0005
As a result, small disagreements begin to flare up in the family, which can gradually develop into serious disagreements. The lack of a sincere conversation about what is happening to each of the spouses negatively affects the relationship of the couple during pregnancy. nine0005
Here you need to turn on prudence and avoid serious stressful situations, because global shocks affect the development of the fetus and the child's bearing.
• Learn to talk to your partner without reproach.
• Start the conversation by explaining how you feel and the importance of what's going on
• Don't forget to celebrate your partner's importance to you and thank them.
Unfortunately, there are no universal rules about how spouses should behave when they are expecting a baby. How to talk to each other, how to share responsibilities, how to keep track of the domestic and financial aspects of life. This is something that each couple must create for themselves, choosing the best option possible. Interest in each other and a common goal can become the basis for creating your own family space and building understanding between spouses while expecting a baby. nine0005
Interest in each other and a common goal can become the basis for creating your own family space and building understanding between spouses while expecting a baby. nine0005
Impressibility
During pregnancy, the psycho-emotional state of the future mother can be greatly shaken, equanimity is replaced by a panic reaction to any remarks of people, reasoning and warnings of the doctor. Reading articles on the Internet, scenes from movies, watching the news can all bring you to tears. It's okay to let your emotions out, but everything is good in moderation.
A large number of fears during pregnancy create a negative emotional background. The expectant mother needs a calm and peaceful atmosphere, a sense of security, confidence in her own safety and, of course, positive emotions for the entire period of bearing the crumbs. Any phobias at this stage can develop into catastrophic anxiety, panic, anxiety, provoking sleep disturbances in a pregnant woman, depressive states, nervous breakdowns, and tantrums.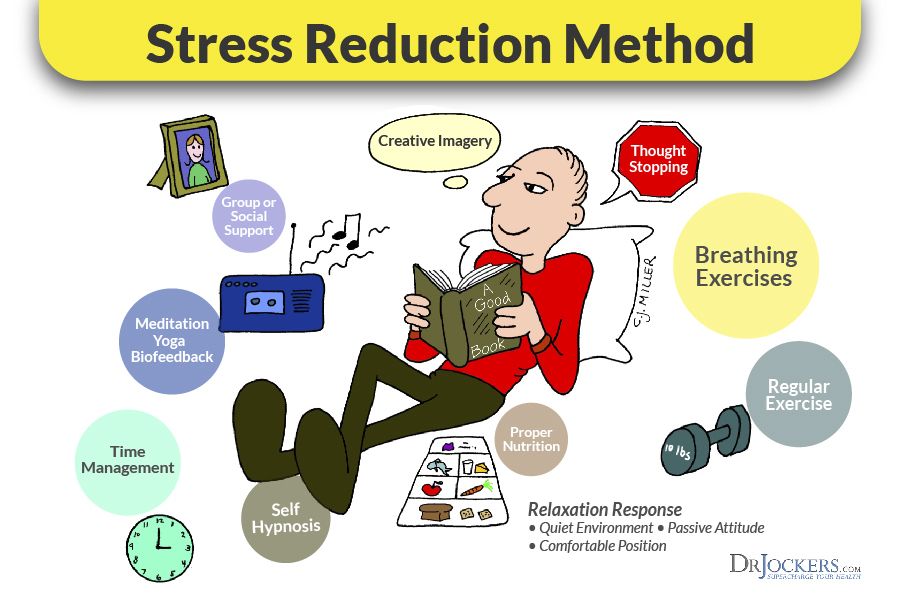 This can become a significant threat to the development and life of the child. nine0005
This can become a significant threat to the development and life of the child. nine0005
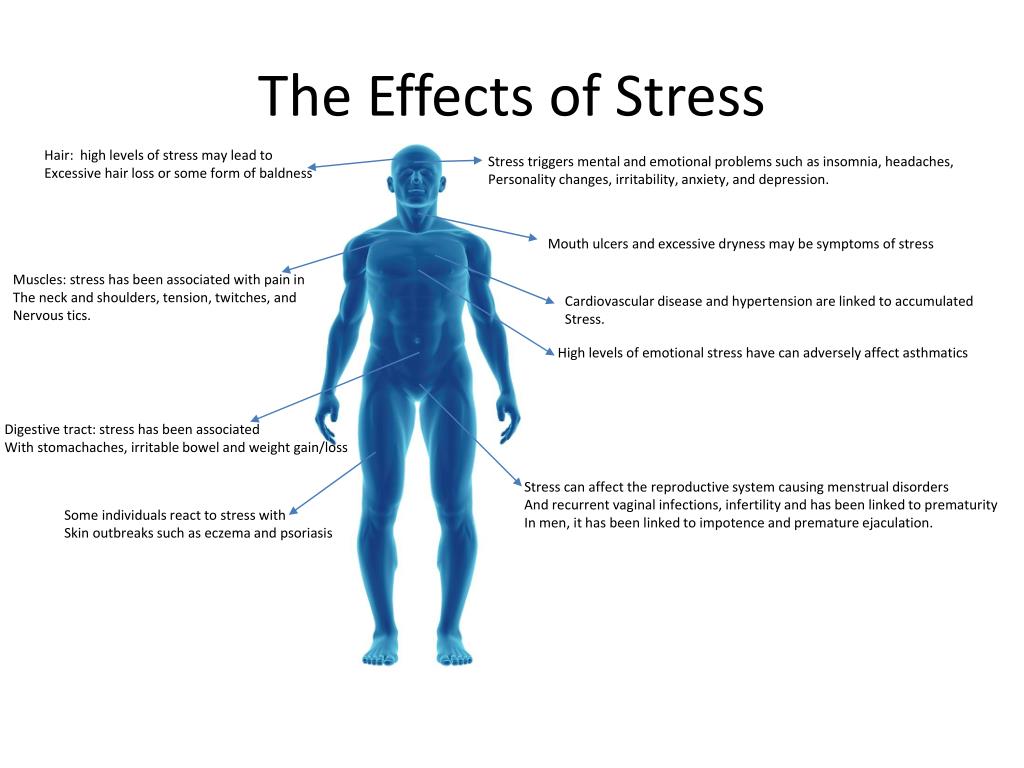
Stress in late pregnancy has a bad effect on the formation of the baby's nervous system, such children may experience various psychological problems even in adulthood. Children of women who have experienced severe stress during pregnancy are often born prematurely or debilitated, they are more likely to get asthma, diabetes, malformations or allergies.
Impressibility has a downside - the ability to take a fresh look at the world. Fill yourself and your unborn child with pleasant impressions and enjoy the beautiful aspects of life. For example, more often go to the theater or cinema, get out into nature. Choose to communicate with people who are pleasant to you, this is normal if you decide to refuse to communicate with someone for a while. Watch what impresses you, contrary to popular belief, you can control it. nine0005
Loneliness
The life of a pregnant woman changes rapidly, filled with fears, restrictions and anxieties. The body, the internal state, the way of life is changing, and for those around it, everything is the same as before. That is, pregnancy is sometimes about loneliness, more often internal. In a position, you can no longer fit into the usual adventures, or even into the workflow. In a state of loneliness, strong feelings can rush.
The body, the internal state, the way of life is changing, and for those around it, everything is the same as before. That is, pregnancy is sometimes about loneliness, more often internal. In a position, you can no longer fit into the usual adventures, or even into the workflow. In a state of loneliness, strong feelings can rush.
During pregnancy, a radical change occurs and all aspects of a woman's life change, pregnancy provokes profound changes in self-awareness, attitudes towards others and the world, there is a transformation of the value-semantic components of the image of the world, one's own identity in new conditions. Psychological factors play an important role in the occurrence of toxicosis, neurotic disorders, and are also a threat of miscarriage and premature birth. Therefore, in psychology, the very situation of motherhood is considered as requiring adaptation, both to the physical and to the psychosomatic state. Preterm birth is sometimes seen as an unconscious, repressed disclaimer, fear of change. nine0005
nine0005
Experts recommend using pregnancy for self-knowledge, sharing experiences with loved ones, with a psychologist, and communicating with other expectant mothers. This is the time when special attention should be paid to the formation of a new social circle that will meet the needs of the expectant mother, where the woman will feel understood. For this, only one factor is not enough, for example, such as the “community of pregnant women”, choose people who are close to you in spirit, who share your values and worldview. nine0005
Anxiety about the baby's health
In general, fears can be divided into two types - constructive and destructive. The first one is based on the instinct of self-preservation, they help the expectant mother to be constantly on the alert and not miss the alarm bells. And at the heart of destructive or pathological fear is an obsessive state, a phobia, which leads to mental disorders of the personality. In this state, a woman is not capable of normal life.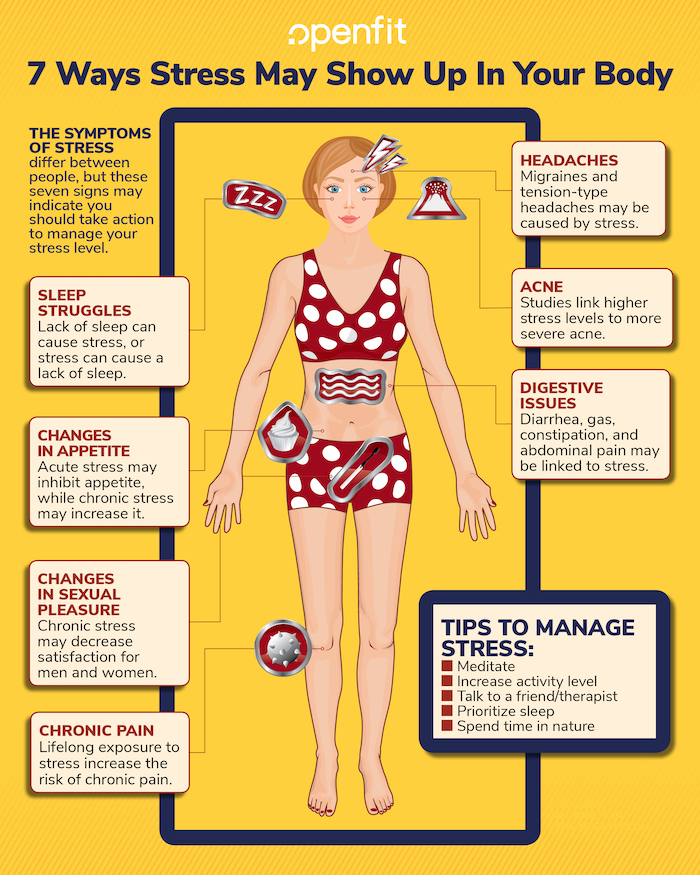 Anxiety and fear can paralyze a woman and she stops all activities except those that support or correspond to her condition. Pathological fear is dangerous and can lead not only to premature birth, but also negatively affect the formation of the baby's psyche. nine0005
Anxiety and fear can paralyze a woman and she stops all activities except those that support or correspond to her condition. Pathological fear is dangerous and can lead not only to premature birth, but also negatively affect the formation of the baby's psyche. nine0005
Anxiety about the health of the unborn child appears almost from the first days after conception. After all, a woman cannot control the development of the fetus, she does not
see how her baby is developing, so there are unrest. For many, anxiety remains, despite all the ultrasound, tests and examinations of doctors.
Most babies are born healthy. A high level of medicine allows you to diagnose various fetal pathologies during pregnancy. For this, a screening study is carried out at 10-13 weeks and 16-20 weeks. nine0005
To get rid of fear, you need to trust yourself and nature. Do not listen to the negative stories of others. Tune in for the best, realizing that almost all problems are solvable. Even before the birth, you can find a good pediatrician who will observe the child from birth.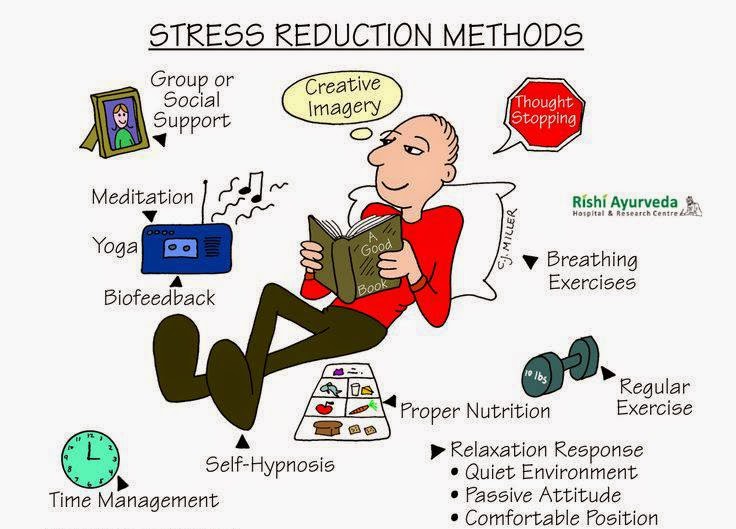
It should be understood that anxiety during childbearing is quite a common phenomenon, but it is necessary to notice the negative impact of fears on the life of a pregnant woman in time. Often, hyperanxiety is a factor in high blood pressure, unexpected bleeding, and more serious consequences. nine0005
Simple bodily practices such as breathing, light exercise for pregnant women, meditative practices, and walks in nature help relieve anxiety. Any creative activity, applied arts (drawing, embroidery, knitting, etc.), singing also help to direct the energy of the body to other activities, preventing it from being localized only in the experience of anxiety.
Fear of childbirth as a cause of preterm labor
Every woman in the third trimester of pregnancy experiences an inexplicable fear of childbirth, especially if this is the first child. Some more, some less, but the anxiety is understandable. There is even such a scientific term - tokophobia - this is a pathological anxiety before childbirth.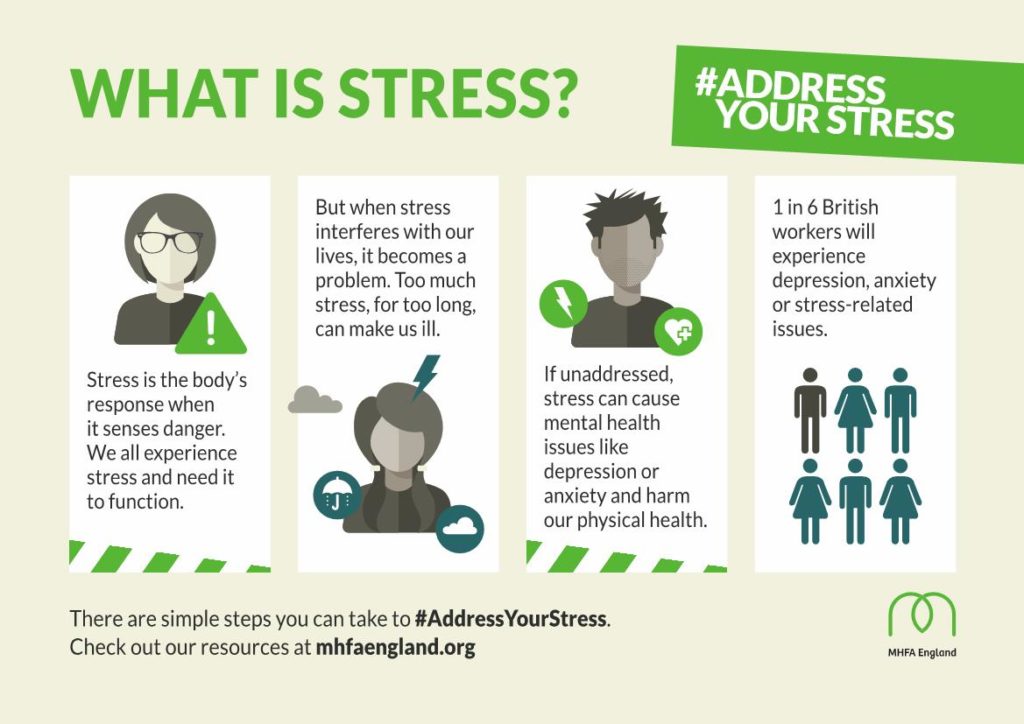 There are cases when tokophobia is so strong that it can lead to serious deviations in the course of pregnancy, including premature birth of a child.
There are cases when tokophobia is so strong that it can lead to serious deviations in the course of pregnancy, including premature birth of a child.
What could be the reasons for a woman's anxiety? nine0004
• • For primiparas, this is the fear of the unknown, pain and discomfort.
• • There are women who read all sorts of information about dire consequences during pregnancy. And they try on all the worst outcomes for themselves.
• • Hormonal changes (decreased production of progesterone and increased levels of estrogen in the blood). This is more difficult to deal with, because the hormonal background cannot be changed at the snap of a finger.
• • Fear may appear if there have already been complications from previous births or pregnancies. Here, sometimes it is even worth contacting a psychologist so as not to program yourself for a bad outcome again. nine0029 • • Panic about the child's health
• • Fear of not being able to cope with one's parental responsibilities.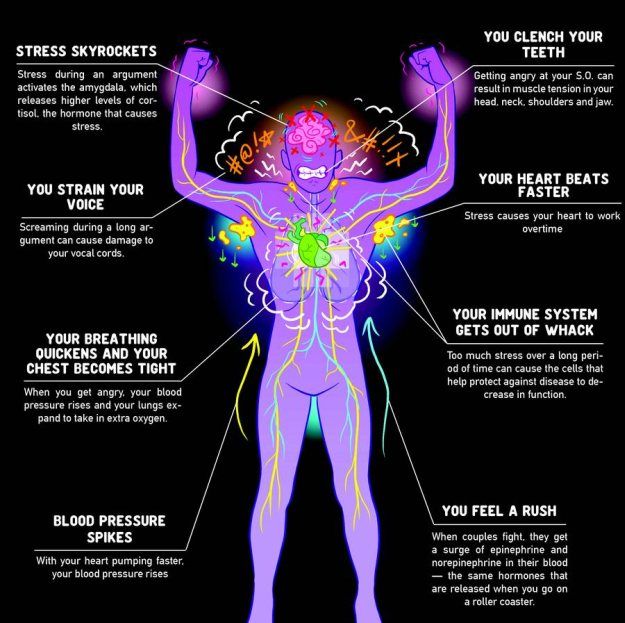
There are many reasons to worry, but they can be dealt with, sometimes on your own, and sometimes with the help of specialists.
How can you cope with the coming attacks of fear of childbirth?
Trust your doctor, use distraction hobbies, breathing practices, exercise, take pregnancy courses to stay informed. Massage and support from loved ones can also help. nine0005
Unconscious fears. Rejection of one's body
Women can perceive their body as an object that must always be perfect. Therefore, pregnancy and the birth of a child may seem like a threat to a beautiful, slender body. If the fear of change is strong enough, it can cause psycho-emotional instability. And it, in turn, increases the risk of premature birth.
This is a very painful topic for many women. And changes in the figure and body parameters are almost unpredictable, as are the likelihood and timing of the return of pre-pregnant forms. And yes, someone, having given birth to three, quickly returns to the previous parameters, and someone, even after the first pregnancy, cannot bring himself into the desired shape for years. nine0005
nine0005
The figure may not change much, or vice versa. When feeding, the chest changes, stretch marks may appear on the stomach, the stomach may not go away.
Yes, even during pregnancy itself, the body changes at a great speed and it is difficult to get used to it, but you should not be afraid of this, and even more so, let fear fill all your thoughts.
There may be a fear of unattractiveness for your man during pregnancy, but it is worth discussing with him right away, and not driving thoughts in your head. You need to understand that most experiences are unfounded, but can lead to serious consequences. nine0029 What can you really do for your figure?
• Healthy diet. Stay adequate at this point, no need to chase unique diets. A simple rule, after looking at your diet, think about which of these products is good for the body (in any conditions, during pregnancy and not), and which would you classify as junk food?
• Stay as active as possible. At this point, be sure to consult your doctor.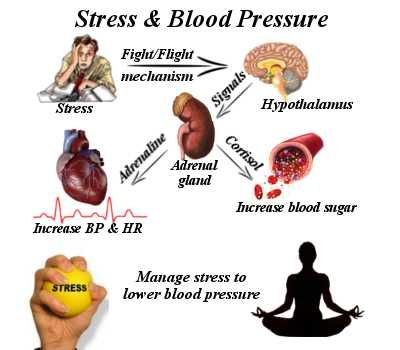 If you are used to active training several times a week, choose a safe set of exercises during pregnancy. If you did not play sports before pregnancy, you should not introduce a frantic pace of training during pregnancy. Enough regular walks and light gymnastics. nine0029 • Drink water. This is always important, and now we should not forget about it.
If you are used to active training several times a week, choose a safe set of exercises during pregnancy. If you did not play sports before pregnancy, you should not introduce a frantic pace of training during pregnancy. Enough regular walks and light gymnastics. nine0029 • Drink water. This is always important, and now we should not forget about it.
• Take care of your skin. Refuse to evaluate at this time, just do not forget about the care and nutrition for your skin.
Makagonova Yuliya Yuryevna
special psychologist, perinatal psychologist, gestalt therapist,
supervisor of the school for parents "New Life Together" of the Charitable Foundation for Helping Children Born at Early Term "Give Sunshine"
5
doubles stress risk of preterm birthPosted
Text: Alexander Minaev/Infox.ru
health children pregnancy obstetrics stress premature birth gynecology caesarean section
Like it?
Share with your friends! nine0005
Stress is harmful to everyone, but especially to pregnant women: negative factors affect at least two people at once. Chinese scientists have established at what specific moments of pregnancy it is most important to protect the peace of the expectant mother.
Chinese scientists have established at what specific moments of pregnancy it is most important to protect the peace of the expectant mother.
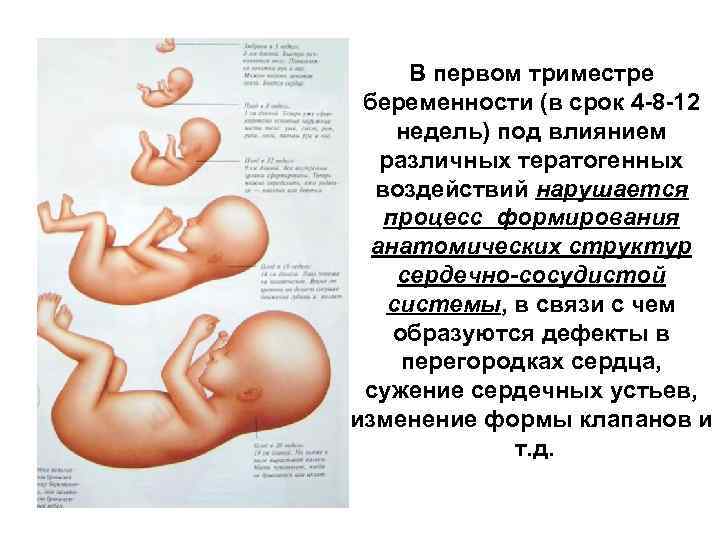
Dangerous first trimester
Researchers from Anhui Medical University of China studied the history of about 1800 women who were observed for pregnancy in 2008. Of these, 5.3% gave birth prematurely (96 cases), and 3.1% (55 cases) developed infants with pathologically low weight. Among those who gave birth prematurely more than 60 women experienced severe stress at the beginning or middle of pregnancy. AT in particular, many of them lost their jobs because of their position, some in this time the husbands left, most simply announced the deplorable economic the position of their families. Scientists have determined that the risk of preterm birth increases by 100% precisely in cases where women experience stress in the first or second three months of pregnancy. As for negative factors in last trimester, they, oddly enough, do not provoke preterm labor. Risk the birth of a child with low body weight is almost three times higher in those mothers who experienced stress in the first trimester. nine0005
Risk the birth of a child with low body weight is almost three times higher in those mothers who experienced stress in the first trimester. nine0005
Chinese research paper published in a specialized publication of the American Journal of Obstetrics and Gynecology.
Early birth
Preterm birth One of the most important causes of infant mortality in developing countries. According to WHO, out of about 13 million cases per year, up to 85% occur in Africa and Asia. The lowest rates, about 6%, are recorded in Europe.
Premature labor activity is considered to occur from the 28th to 37th week of pregnancy. From the 38th to the 42nd week, this is a normal delivery at term. If, on the other hand, a premature baby is born between the 22nd and 28th weeks and survives within a week, this is considered an extremely low preterm birth. body weight of the newborn. Statistical frequency of preterm birth in the world quite high - from 7 to 15%.