Can someone be born with an std
Sexually transmitted infections, pregnancy, and breastfeeding
Sexually transmitted infections (STIs) are also called sexually transmitted diseases, or STDs. STIs include chlamydia, gonorrhea, trichomoniasis, genital herpes, genital warts, HIV, and syphilis. Some STIs can pass from mother to baby during pregnancy and through breastfeeding.
How do STIs affect pregnant women?
STIs can cause many of the same health problems in pregnant women as in women who are not pregnant. But having an STI also can hurt the unborn baby's health.
Having an STI during pregnancy can cause:
- Premature labor (labor before 37 weeks of pregnancy). Early (preterm) birth is the number one cause of infant death and can lead to long-term developmental and health problems in children.1
- Infection in the uterus (womb) after birth
Can I pass an STI to my baby?
Yes. Some STIs can be passed from a pregnant woman to the baby before and during the baby's birth.
- Some STIs, such as syphilis, cross the placenta and infect the baby in the womb.
- Other STIs, like gonorrhea, chlamydia, hepatitis B, and genital herpes, can pass from the mother to the baby as the baby passes through the birth canal.
- HIV can cross the placenta during pregnancy and infect the baby during delivery.
What are the harmful effects of passing an STI to a baby?
The harmful effects to babies may include:
- Low birth weight (less than 5 pounds)
- Eye infection
- Pneumonia
- Infection in the baby's blood
- Brain damage
- Lack of coordination in body movements
- Blindness
- Deafness
- Acute hepatitis
- Meningitis
- Chronic liver disease, which can lead to scarring of the liver (cirrhosis)
- Stillbirth
I'm pregnant. What can I do to prevent problems from STIs?
You can prevent some of the health problems caused by STIs and pregnancy with regular prenatal care. Your doctor will test you for STIs early in your pregnancy and again closer to childbirth, if needed.
Your doctor will test you for STIs early in your pregnancy and again closer to childbirth, if needed.
- STIs caused by bacteria, such as chlamydia and gonorrhea, can be cured with antibiotics. Some antibiotics are safe to take during pregnancy. Your doctor can prescribe antibiotics for chlamydia, gonorrhea, syphilis, and trichomoniasis during pregnancy.
- STIs caused by viruses, such as genital herpes and HIV, have no cure.
- If you have herpes, antiviral medicine may help reduce symptoms. If you have symptoms of herpes or active genital herpes sores at the start of labor, you may need a cesarean section (C-section). This can help lower the risk of passing the infection to your baby.
- If you have HIV, antiviral medicines can lower the risk of giving HIV to your baby to less than 1%.2 You also may need to have a C-section.
You also can take steps to lower your risk of getting an STI during pregnancy.
Can I breastfeed if I have an STI?
Maybe. Some STIs affect breastfeeding, and some don't. The following are some general guidelines, but talk to your doctor, nurse, or a lactation consultant about the risk of passing the STI to your baby while breastfeeding:
- If you have HIV, do not breastfeed. You can pass the virus to your baby. In countries like the United States where clean water is available, using a breastmilk substitute like formula is recommended.
- If you have chlamydia, gonorrhea, or HPV, you can breastfeed your baby.
- If you have trichomoniasis, you can take the antibiotic metronidazole if you are breastfeeding. You may need to wait 12 to 24 hours after taking the medicine to breastfeed.
- If you have syphilis or herpes, you can breastfeed as long as your baby or pumping equipment does not touch a sore. It is possible to spread syphilis or herpes to any part of your breast, including your nipple and areola.
 If you have sores on your breast, pump or hand-express your milk until the sores heal. Pumping will help keep up your milk supply and prevent your breast from getting overly full and painful. You can store your milk to give to your baby in a bottle for another feeding. But if parts of your breast pump also touch the sore(s) while pumping, you should throw the milk away.
If you have sores on your breast, pump or hand-express your milk until the sores heal. Pumping will help keep up your milk supply and prevent your breast from getting overly full and painful. You can store your milk to give to your baby in a bottle for another feeding. But if parts of your breast pump also touch the sore(s) while pumping, you should throw the milk away.
Are STI treatments safe to use while breastfeeding?
If you are being treated for an STI, ask your doctor about the possible effects of the medicine on your breastfeeding baby. Most treatments for STIs are safe to take while breastfeeding.
Did we answer your question about STIs, pregnancy, and breastfeeding?
For more information about STIs, pregnancy, and breastfeeding, call the OWH Helpline at 1-800-994-9662 or contact the following organizations:
- Food and Drug Administration (FDA), HHS
Phone Number: 888-463-6332 - National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), CDC, HHS
Phone Number: 800-232-4636 - National Institute of Allergy and Infectious Diseases (NIAID), NIH, HHS
Phone Number: 866-284-4107 (TDD: 800-877-8339) - American Sexual Health Association
Phone Number: 800-227-8922
Sources
- Centers for Disease Control and Prevention.
 (2015). Preterm Birth.
(2015). Preterm Birth. - Centers for Disease Control and Prevention. (2015). HIV Among Pregnant Women, Infants, and Children.
The Office on Women's Health is grateful for the medical review by:
- Jill E. Long, M.D., M.P.H., FACOG, Commander, U.S. Public Health Service Commissioned Corps, Medical Officer, Sexually Transmitted Diseases Branch, Division of Microbiology and Infectious Diseases, National Institute of Allergy and Infectious Diseases
- Centers for Disease Control and Prevention (CDC) staff
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U.S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 22, 2021
Can You Be Born With An STD? L Pregnancy And STDs
If you’re sexually active, the idea of contracting sexually transmitted diseases (STDs) can result in feelings of anxiety and uncertainty. However, if you’re an expecting mother, you may feel even more concerned about your health — and the health of your developing baby.
However, if you’re an expecting mother, you may feel even more concerned about your health — and the health of your developing baby.
You may find yourself wondering, “Can you be born with an STD?” or “Can STDs affect my pregnancy?” While these questions are common, many pregnant women cannot find a clear answer due to the stigma and lack of education surrounding STDs.
Our staff at Rapid STD Testing compiled this detailed guide with answers to common questions and concerns regarding rapid STD tests, sexually transmitted infections (STIs), and pregnancy. Here, you can find the answers you need to ensure a healthy pregnancy.
Types of STIs That Can Infect a Baby in the WombAccording to the Centers for Disease Control and Prevention (CDC), STDs can impact both you and your developing baby. While you can’t naturally develop an STD, you can contract an infection from sexual partners through:
- Unprotected vaginal, anal, or oral sex
- Contact with bodily fluids
- Intimate contact with an infected person
To reduce the risk of transmitting infections to babies during pregnancy, the CDC outlines specific recommendations for prenatal STI screenings. Most expectant mothers receive comprehensive testing at their first prenatal visit. However, if you are at high risk for contracting an STD, your healthcare provider will likely re-screen you during your third trimester for potential infections, including:
Most expectant mothers receive comprehensive testing at their first prenatal visit. However, if you are at high risk for contracting an STD, your healthcare provider will likely re-screen you during your third trimester for potential infections, including:
Syphilis
You may contract syphilis through direct contact with syphilis sores or unprotected sex with an infected person. When detected early, you can treat syphilis and reduce the risk of spreading the infection to your baby. If left untreated, your baby may contract congenital syphilis. This preventable STD can result in infant death. It is crucial to get tested for STIs and prevent infection during pregnancy.
Chlamydia
Though chlamydia is the most common bacterial STD in the United States, most infected women don’t have any symptoms. Still, you can pass chlamydia to children through vaginal delivery, making it critical to detect and treat the infection as quickly as possible. Untreated chlamydia can cause eye and lung infections in your newborn.
Gonorrhea
Like chlamydia, many women infected with gonorrhea don’t have any symptoms. However, if left untreated, the infection can impact your pregnancy and labor or transmit to your baby during delivery.
Genital Herpes
You can contract genital herpes from direct contact or unprotected sex, but can you be born with an STD like herpes? Yes, you can pass herpes to your baby during pregnancy or delivery.
Women who contract herpes or experience their first outbreak near their delivery are more likely to infect their children. Even so, most healthcare providers recommend a C-section to prevent your baby from contracting the infection.
Hepatitis B and Hepatitis C
Hepatitis B — also known as Hep B — spreads through unprotected sex and contact with infected fluids, such as saliva, vaginal fluid, semen, or blood. The infection often has no symptoms, but the long-term effects can cause liver damage, disease, or cancer. In addition, your baby can contract chronic Hepatitis B if infected at birth.
Hepatitis C creates an infection in your liver, which you can transmit to your baby. That said, pregnant mothers generally have a reduced likelihood of passing Hep C to their babies. If the baby does contract Hep C, the infection usually clears up without any treatment.
HIV
HIV — also known as human immunodeficiency virus — attacks your body’s immune system and can lead to AIDS if left untreated. You can infect your developing baby with HIV during pregnancy, labor, delivery, or breastfeeding. However, when diagnosed and treated, you can reduce the risk of infecting your baby to 2% or less.
Effects of Having an STD While PregnantIf left untreated, an STD can result in serious health concerns for both you and your developing baby. Certain STDs can lead to complications, while others can cause neonatal conditions or chronic diseases.
Fortunately, you can protect yourself and your baby by receiving regular check-ups and testing in the first and third trimesters. In addition, you can take advantage of same-day STD testing from our staff at Rapid STD Testing for quick, confidential results that can help keep you and your baby healthy.
In addition, you can take advantage of same-day STD testing from our staff at Rapid STD Testing for quick, confidential results that can help keep you and your baby healthy.
STDs can impact your pregnancy in several ways, including:
Premature Delivery
Premature delivery means that you go into labor and deliver your child too early. Typically, medical professionals consider a birth that occurs before the 37th week of pregnancy as premature. Premature babies may experience developmental delays as well as other health conditions.
Premature Rupture of Membranes (PROM)
Also known as PROM, premature rupture of membranes occurs when the amniotic sac around your baby bursts before you go into labor. As a result, you have a higher chance of developing an infection or experiencing a premature delivery.
Low Birth Weight
Some STDs can result in low birth weight, meaning that your baby weighs less than five pounds and eight ounces when born.
Chorioamnionitis
Chorioamnionitis occurs when bacteria infect the membranes and amniotic fluid surrounding your baby. The infection can cause premature births and severe infections that enter your bloodstream or uterine lining. In some cases, you may require a C-section to deliver your baby safely. Untreated chorioamnionitis can also lead to meningitis or pneumonia in newborns.
The infection can cause premature births and severe infections that enter your bloodstream or uterine lining. In some cases, you may require a C-section to deliver your baby safely. Untreated chorioamnionitis can also lead to meningitis or pneumonia in newborns.
Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease, or PID, can infect your reproductive system, including your womb, fallopian tubes, ovaries, and cervix. In many cases, PID can impact your ability to become pregnant or result in ectopic pregnancy, a life-threatening condition in which a fertilized egg implants outside of your uterus.
Prenatal STD Transmission
Some STDs, such as Hepatitis B, HIV, Zika, or syphilis, can pass to your baby while still in the womb if left undiscovered or untreated. For example, you can transmit Hep B to your child through the placenta, resulting in a prenatal infection and potential liver damage.
Chronic Health Conditions
If your baby becomes infected with an STD during pregnancy, labor, delivery, or breastfeeding, they may endure life-long side effects.
The effects of prenatal (pre-delivery) or neonatal (post-delivery) exposure to STDs can affect your baby in several ways. Some STDs, such as chlamydia or gonorrhea, may result in eye infections, lung infections, joint infections, blood infections, or pneumonia.
Others, such as Hepatitis B or C, can cause liver damage, liver disease, or even liver cancer. Untreated HIV may spread to your baby, resulting in an HIV infection. Finally, syphilis can result in premature delivery, fatal illnesses, or organ damage.
Miscarriage or Stillbirth
Finally, some untreated STDs can result in miscarriages or stillbirths. A miscarriage occurs when a baby dies in the womb before the 20th week of pregnancy. Stillbirths occur following the 20th week of pregnancy.
Testing and Diagnosis of STD PregnancyBecause sexually transmitted infections can result in serious or even fatal conditions for you and your child, most pregnant women get tested during their first prenatal visit. Your doctor will typically check for STIs such as HIV, chlamydia, gonorrhea, syphilis, and Hep B.
Your doctor will typically check for STIs such as HIV, chlamydia, gonorrhea, syphilis, and Hep B.
If you engage in high-risk sexual activities, such as unprotected sex with multiple sexual partners, your doctor will likely screen you for certain STDs throughout your pregnancy.
Even if you don’t have any symptoms, you should still get tested to ensure a healthy pregnancy. Most STDs have very few, if any, symptoms. As a result, many pregnant women don’t know that they’ve contracted an STD for months or years. That said, some of the most common STD symptoms include:
- Genital warts, sores, or bumps
- Redness, swelling, or inflammation near the vagina
- Flu-like symptoms, such as headache or fatigue
- Abdominal pain
- Vaginal discharge
- Pain during or after sex
- Bleeding after sex or between menstrual cycles
- Eye infections
- Mouth sores
- Skin rash
- Pain while urinating
- Itching near the vagina
- Weight loss
- Night sweats
If you experience any of these STD symptoms or believe you were exposed to an STD, early detection and treatment can help keep you and your baby safe. However, our team at Rapid STD Testing knows that you can’t always wait until your next prenatal visit to get the answers you need. You may also feel too embarrassed or afraid to speak with your doctor.
However, our team at Rapid STD Testing knows that you can’t always wait until your next prenatal visit to get the answers you need. You may also feel too embarrassed or afraid to speak with your doctor.
That’s why we offer a full range of same-day STI tests and panels. Our discreet testing facilities and rapid results make it easy to take control of your health. We’ve opened more than 4,000 testing centers across the United States, even in rural areas without easily accessible medical care. We also offer same-day testing and results in three days or less.
Depending on your needs, you can choose from our comprehensive 10-panel STD test or twelve individual tests, including:
- Hepatitis A
- Hepatitis B
- Hepatitis C
- HIV 1 and 2 Antibody
- HIV RNA Early Detection
- Syphilis
- Herpes I
- Herpes II
- Chlamydia
- Gonorrhea
- Chlamydia and Gonorrhea
- Trichomoniasis
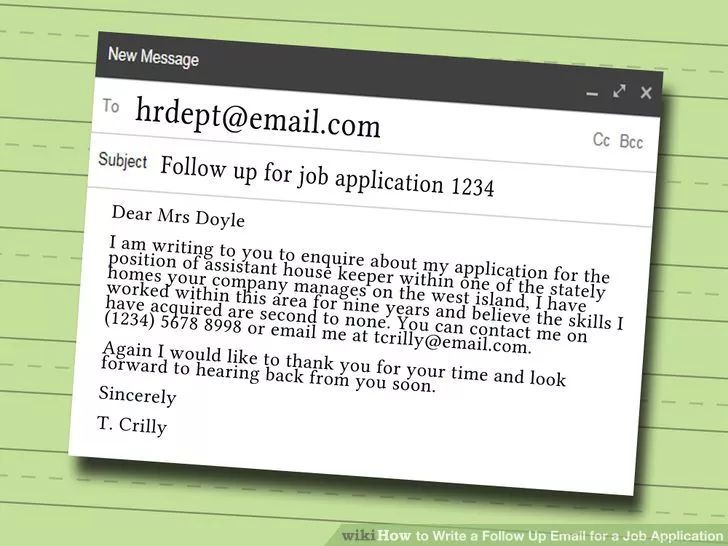
In the event of a positive test result, you’ll receive a confidential consultation with one of our doctors. During the appointment, we will:
During the appointment, we will:
- Go over the results of your screening
- Help you determine the best treatment options for you and your baby
- Send your prescription to the pharmacy of your choice.
Finally, if you test positive for HIV, we’ll ensure that you get the help you need to prevent transmission and live a healthy life.
After receiving your results, you can also share your panel with your healthcare provider and work with your prenatal care team to protect your developing baby throughout the rest of your pregnancy. Your doctor may decide to run additional tests, especially if you test positive for Hepatitis B or HIV.
Your doctor can then determine if you’re likely to spread the infection to your child during pregnancy or delivery and take action to prevent transmission. Finally, your doctor may perform a blood test to check your baby for evidence of an STD at birth.
Treatments for STD During PregnancyLearning that you’ve contracted an STD while pregnant can create intense fear. Lack of education surrounding STDs — as well as the stigma that comes with a positive STD test — can make you feel isolated, anxious, and embarrassed. You may not know how to talk to your doctor or tell your partner you have an STD.
Lack of education surrounding STDs — as well as the stigma that comes with a positive STD test — can make you feel isolated, anxious, and embarrassed. You may not know how to talk to your doctor or tell your partner you have an STD.
That said, early detection and treatment of STDs can significantly reduce the risk of complications during pregnancy, labor, and delivery. Doctors can effectively treat some STIs during pregnancy. In fact, pregnant women can usually take antibiotics while pregnant and cure most bacterial or parasitic infections, including:
- Chlamydia
- Gonorrhea
- Syphilis
- Trichomoniasis
Doctors can’t always cure viral infections like herpes, Hep B, Hep C, and HIV. However, you can take certain antiviral medications and therapies to reduce the impact of viral STDs on your body and manage your symptoms. In addition, you can make a birth plan that helps prevent your baby from contracting the infection, typically through a C-section.
Learning to protect you and your baby from STDs can help prevent the stress of a diagnosis. Fortunately, the best way to prevent your baby from dealing with the effects of an STD is to protect yourself from STDs.
That said, if you think you’ve been exposed to an STD, you should immediately get tested by your doctor or at one of our Rapid STD Testing facilities. You can also take several steps to reduce the risk of contracting an STD, including:
Abstaining from Sex
While you can now choose from dozens of birth control methods to help prevent infection, abstaining from sex ensures that you won’t contract an STD. Abstinence includes oral, vaginal, and anal sex.
Limiting Your Sex Partners
The only way to contract an STD is through intimate physical contact, exposure to infected bodily fluids, or unprotected sex. With that in mind, you can protect yourself from exposure by having sex with one partner who doesn’t have any infections and practices monogamy. Before you have sex with a new partner, ensure that both you and your partner get tested.
Before you have sex with a new partner, ensure that both you and your partner get tested.
Using Barrier Birth Control Methods
Barrier birth control methods help prevent pregnancy by keeping sperm away from an egg. These methods include condoms, cervical caps, contraceptive sponges, and diaphragms.
While barrier methods may help prevent pregnancy, diaphragms, cervical caps, and sponges won’t protect you from STDs. Neither will IUDs, hormonal implants, or birth control pills. Male condoms are typically the most effective way to prevent exposure to an STD. You may also consider female condoms or dental dams for oral sex.
Reducing Drug and Alcohol Use
While drugs and alcohol don’t cause STDs, the substances may lower your inhibitions. As a result, you may engage in high-risk activities, such as unprotected sex with a new partner. Limiting your use of drugs and alcohol can help you make informed, educated decisions that keep you and your baby safe from STDs.
Getting Tested
Finally, you can protect yourself, your partner, and your baby through regular STD testing. Can you be born with an STD? Yes, in some cases, the mother can pass an STD to the baby during vaginal birth.
A confidential, quick STD test from our team at Rapid STD Testing can empower you with the information and peace of mind you need to take control of your health without raising your insurance rates or disrupting your busy schedule.
Test for STDs During Pregnancy with Rapid STD TestingIf you’re pregnant and think you may have been exposed to STDs, you don’t have to wait any longer to get the answers you need. For more information or help finding the right test, please call one of our experienced Rapid STD Testing counselors today at (866) 872-1888.
STIs and pregnancy - KVD №2
- home
- Articles
- STIs and pregnancy
The presence of an STI in a pregnant woman can cause serious harm to the fetus. Untreated infections can lead to miscarriage, premature birth, stillbirth, underweight babies, blindness, hearing loss, chronic respiratory disease, mental retardation, and other serious developmental problems. Untreated syphilis can lead to the birth of a child with congenital syphilis. Activation of STIs during pregnancy is manifested by symptoms of intrauterine infection, leading to miscarriage and intrauterine lesions of the fetus up to its death. Infection of the placenta, according to histological studies, in half of the cases is associated with chlamydia, ureaplasmas, mycoplasmas and HSV (herpes simplex virus), CMV (cytomegalovirus). In newborns, STIs cause conjunctivitis, pneumonia, cerebrovascular accidents, intracranial hemorrhages (one of the causes of cerebral palsy), and sepsis. nine0015
Untreated infections can lead to miscarriage, premature birth, stillbirth, underweight babies, blindness, hearing loss, chronic respiratory disease, mental retardation, and other serious developmental problems. Untreated syphilis can lead to the birth of a child with congenital syphilis. Activation of STIs during pregnancy is manifested by symptoms of intrauterine infection, leading to miscarriage and intrauterine lesions of the fetus up to its death. Infection of the placenta, according to histological studies, in half of the cases is associated with chlamydia, ureaplasmas, mycoplasmas and HSV (herpes simplex virus), CMV (cytomegalovirus). In newborns, STIs cause conjunctivitis, pneumonia, cerebrovascular accidents, intracranial hemorrhages (one of the causes of cerebral palsy), and sepsis. nine0015
Untreated gonococcal infection often results in ectopic pregnancy or pelvic inflammatory disease. Chronic gonorrhea may worsen immediately after childbirth. At the same time, the risk of gonococcal sepsis is high. Women who become infected in the last 20 weeks of pregnancy or after childbirth are at high risk of gonococcal arthritis. In acute gonorrhea, there is an increased risk of premature rupture of amniotic fluid, spontaneous abortion, and preterm birth.
Women who become infected in the last 20 weeks of pregnancy or after childbirth are at high risk of gonococcal arthritis. In acute gonorrhea, there is an increased risk of premature rupture of amniotic fluid, spontaneous abortion, and preterm birth.
Infection of the fetus with gonorrhea occurs in utero or during childbirth. Intrauterine infection is manifested by gonococcal sepsis in the newborn and chorioamnionitis. Infection during childbirth can lead to gonococcal conjunctivitis, otitis externa, and vulvovaginitis. The most common complication in children born to gonorrhea mothers is a highly contagious eye disease (newborn ophthalmia) which, if left untreated, can lead to blindness. Rare complications in children born to gonorrhea mothers are childhood meningitis and arthritis. nine0015
Most doctors test women for gonorrhea at their first pregnancy visit, and many do another test in the third trimester. If your doctor has not given you the results of the tests, ask him what disease you were tested for.
Trichomoniasis, according to most doctors, does not belong to those diseases that can have a fatal effect on the fetus, but, of course, trichomoniasis during pregnancy is an extremely undesirable condition.
Trichomoniasis in a pregnant woman increases the risk of preterm labor and premature rupture of amniotic fluid. nine0015
Chlamydial infection in 80% of pregnant women is latent. The frequency of occurrence of urogenital chlamydia among pregnant women, according to various sources, is 6.0 - 8.0%. The most common consequences of untreated genital chlamydia during pregnancy are:
- missed pregnancy,
- spontaneous miscarriages,
- premature or delayed birth,
- untimely outpouring of waters,
- blood loss more than 300 ml,
- puerperal fever,
- endometritis,
- intrauterine infection of the fetus.
Transmission of the pathogen to the child is possible both in the presence and in the absence of obvious clinical manifestations of infection in the mother (the probability of its transmission is 50-70%). The fetus is infected both by direct contact with the birth canal of the mother, and in utero: by ingestion or aspiration of amniotic fluid.
The fetus is infected both by direct contact with the birth canal of the mother, and in utero: by ingestion or aspiration of amniotic fluid.
The most common manifestation of congenital chlamydial infection in infants is conjunctivitis (inflammation of the mucous membrane of the eyes), pneumonia develops in 10% of infected newborns, and otitis media is somewhat less common. In some children born to infected mothers, these microbes are isolated from the oropharynx, nasopharynx, and rectum. The total percentage of newborns infected with chlamydia reaches 9.eight%.
Finally, what do you need to know about the impact of STIs on pregnancy, childbearing and breastfeeding?
A pregnant woman can pass on most STIs during pregnancy or childbirth to her children, and some diseases can be passed through breast milk (eg HIV). However, the chance of transmission can be drastically reduced if treatment is started on time.
Once you decide to become pregnant, visit your doctor and make sure that neither you nor your partner have an STI. If you are infected, take a course of treatment and get tested again before pregnancy. nine0015
If you are infected, take a course of treatment and get tested again before pregnancy. nine0015
If you are already pregnant, you will need a complete examination. At any time during your pregnancy, be sure to tell your doctor if you notice any symptoms of an STI or suspect you may have contracted it.
Contact-household transmission of sexual infections - Useful information
April 3, 2013
Many believe that since infections are called STIs, that is, sexually transmitted, it is impossible to get infected in other ways. Unfortunately, this is not the case. Very rarely, however, it happens that sexually transmitted infections are transmitted by household means. That is, STIs can be transmitted:
- with kisses
- close hugs
- through common items
- unsterilized medical instruments
However, you shouldn't be too scared. According to dermatovenereologist of the Healthcare Institution "Minsk Regional Dermatovenerologic Dispensary", Zhdanovich Zhanna Sergeevna, "The probability of contracting sexually transmitted infections for adults is unlikely and almost equal to zero.
According to dermatovenereologist of the Healthcare Institution "Minsk Regional Dermatovenerologic Dispensary", Zhdanovich Zhanna Sergeevna, "The probability of contracting sexually transmitted infections for adults is unlikely and almost equal to zero.
In adulthood, even infection with chlamydia does not occur in water bodies. Therefore, the majority of STIs among adults are transmitted sexually.
Children, more often girls, who have not yet menstruated (usually up to 6-7 years old) can become infected through the household route. Moreover, any STD - and gonorrhea, and chlamydia, and ureaplasmosis.
Moreover, the latter are primary-chronic, that is, they can be asymptomatic and are detected during certain examinations. Children can also become infected through the household route and from sick parents. "
However, forewarned is forearmed. And stocking up on useful information will never be superfluous.
Syphilis:
95-98% of all cases of syphilis infection occur through sexual contact with a sick person. Rarely, however, the household route of infection with syphilis is likely, which in this case is more correctly called household syphilis. Modes of infection:
- kissing
- when biting
- through objects contaminated with the pathogen
- through minor skin lesions
People with weakened immune systems are susceptible to infection (according to statistics, 3% of cases of infection).
What to do? The carrier of the disease should be allocated separate personal household items, dishes.
The causative agent of syphilis is pale triponema. It is well preserved in humid environments, insensitive to cold. However, high temperatures are not well tolerated. nine0015
Gonorrhea :
The main way of spreading gonorrhea is sexual. Nevertheless, it is not excluded that infection by household means, which, however, is extremely rare (gonococci, the causative agents of gonorrhea, need a humid environment to maintain their vital activity, and cannot exist outside the human body).
Nevertheless, it is not excluded that infection by household means, which, however, is extremely rare (gonococci, the causative agents of gonorrhea, need a humid environment to maintain their vital activity, and cannot exist outside the human body).
Domestic transmission of gonorrhea possible:
- in general use with the sick personal hygiene items, bed linen
- when touching the eyes with hands contaminated with the secretions of the patient
- when using shared towels, washcloths, sponges
It is worth knowing that in the secretions of a sick person on objects, for example, underwear, gonococcus is able to maintain viability and pathogenic properties until it dries out (up to 4 hours).
What to do? Direct sunlight and heating above 56 degrees are detrimental to gonorrhea pathogens. Gonococci are not resistant to external influences, therefore they quickly die outside the human body. nine0015
Chlamydia :
Chlamydia is transmitted mainly through sexual contact, but the possibility of spreading chlamydia through the household is not excluded.
Household infection with chlamydia is possible:
- when using the same bath with the patient, hygiene items, bedding, towels
In such ways, chlamydia can get not only on the mucous membrane of the genital organs, but also on the mucous membrane of the eye, which causes chlamydial conjunctivitis. nine0015
Papillomavirus:
The main route of transmission of papillomavirus is the sexual route. The possibility of transmission of the virus by household means is not excluded:
- through the hands of an infected person
- through household items, such as dishes
- in public places (pools, baths, etc.)
- through kissing (if the oral mucosa is infected)
To prevent infection with the virus during sexual intercourse, it is recommended to use barrier methods of contraception. Prevention of infection by household means is possible with vaccination.
Herpes:
Genital herpes in the vast majority of cases is transmitted sexually. However, infection can occur in the household way:
- saliva
- linen, towels
- common dishes
- hygiene products
- toilet seats
- pools, baths
Infection with the herpes virus through household items is unlikely, because at room temperature the virus dies quickly.
Candidiasis :
Unfortunately, the household way of infection with candidiasis, or "thrush" is very common. Fungal infection can occur:
- through common items
- thru bed linen
- through dishes
- microorganisms may be airborne
Thrush can also occur in the mouth area. In children, infection in this case often occurs through unsterilized nipples or dirty pacifiers, in adults - poorly washed vegetables and fruits.
Pediculosis :
Pubic lice are transmitted mainly through sexual contact, but the household route of infection through underwear is also possible. nine0015
nine0015
What to do?
- observe basic hygiene rules
- regularly change underwear and bed linen
- to iron clothes with an iron
- do not allow other people to use your hairbrush, hats
Trichomoniasis :
The probability of contracting trichomoniasis by household means is small, but not excluded. Trichomoniasis can be contracted:
- when using someone else's underwear
- when using a shared towel or washcloth
The causative agent of the disease is Trichomonas, which can survive in a humid environment for up to several hours. It is able to maintain viability on dishes, walls of bathtubs and pools, on toilet seats.
What to do?
Observe basic hygiene standards.
nine0079 Mycoplasmosis:
Infection by household transmission of mycoplasmas is unlikely, but possible:
- in the bath, swimming pool
- at the gym
- through towel
- through household items
- through crockery, cutlery
- through dirty hands
- through bed and underwear
- through a washcloth, sponge
- through the toilet seat
Mycoplasmas are unstable in the external environment. However, this is often not a barrier to infection by household means.
However, this is often not a barrier to infection by household means.
Scabies :
Scabies is characterized by both sexual and contact mechanism of transmission. Infection with scabies can occur in public places (baths, pools, trains, clubs)
What to do?
- a patient with scabies should use a personal towel, bedding and underwear, sleep separately. nine0004
- the patient's personal belongings must be disinfected
- in the room where the patient is located, it is necessary to carry out daily wet cleaning using disinfectants
Remember that many microorganisms that cause sexually transmitted diseases can remain on a damp towel or washcloth for several hours. Therefore, it is extremely important to observe the basic rules of hygiene. Have personal items for hygiene (washcloth, toothbrush, etc.), do not wear other people's things (clothes, shoes, earrings). In this case, the risk of becoming infected by the household route is negligible.