Can gestational diabetes be reversed
Gestational Diabetes and Pregnancy | CDC
Gestational diabetes is a type of diabetes that is first seen in a pregnant woman who did not have diabetes before she was pregnant. Some women have more than one pregnancy affected by gestational diabetes. Gestational diabetes usually shows up in the middle of pregnancy. Doctors most often test for it between 24 and 28 weeks of pregnancy.
Often gestational diabetes can be managed through eating healthy foods and regular exercise. Sometimes a woman with gestational diabetes must also take insulin.
Learn more about Diabetes Self-Management Education and Support Services
Blood sugar that is not well controlled in a woman with gestational diabetes can lead to problems for the pregnant woman and the baby:
An Extra-Large Baby
Diabetes that is not well controlled causes the baby’s blood sugar to be high. The baby is “overfed” and grows extra-large. Besides causing discomfort to the woman during the last few months of pregnancy, an extra-large baby can lead to problems during delivery for both the mother and the baby. The mother might need a C-Section to deliver the baby. The baby can be born with nerve damage due to pressure on the shoulder during delivery.
C-Section (Cesarean Section)
A C-section is an operation to deliver the baby through the mother’s belly. A woman who has diabetes that is not well controlled has a higher chance of needing a C-section to deliver the baby. When the baby is delivered by a C-section, it takes longer for the woman to recover from childbirth.
High Blood Pressure (Preeclampsia)
When a pregnant woman has high blood pressure, protein in her urine, and often swelling in fingers and toes that doesn’t go away, she might have preeclampsia. It is a serious problem that needs to be watched closely and managed by her doctor. High blood pressure can cause harm to both the woman and her unborn baby. It might lead to the baby being born early and also could cause seizures or a stroke (a blood clot or a bleed in the brain that can lead to brain damage) in the woman during labor and delivery.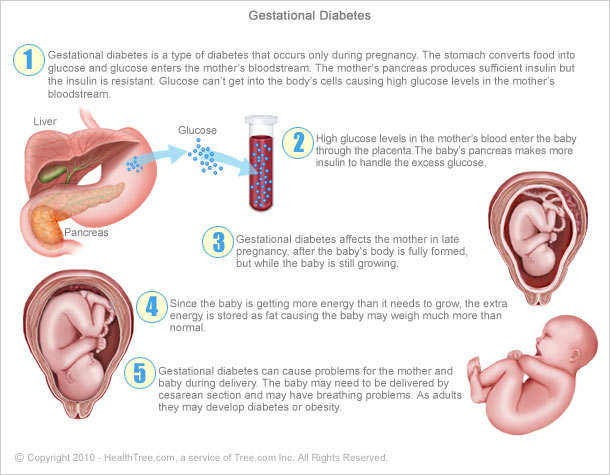 Women with diabetes have high blood pressure more often than women without diabetes.
Women with diabetes have high blood pressure more often than women without diabetes.
Low Blood Sugar (Hypoglycemia)
People with diabetes who take insulin or other diabetes medications can develop blood sugar that is too low. Low blood sugar can be very serious, and even fatal, if not treated quickly. Seriously low blood sugar can be avoided if women watch their blood sugar closely and treat low blood sugar early.
If a woman’s diabetes was not well controlled during pregnancy, her baby can very quickly develop low blood sugar after birth. The baby’s blood sugar must be watched for several hours after delivery.
5 Tips for Women with Gestational Diabetes
- Eat Healthy Foods
Eat healthy foods from a meal plan made for a person with diabetes. A dietitian can help you create a healthy meal plan. Learn more about diabetes meal planning. - A dietitian can also help you learn how to control your blood sugar while you are pregnant.
 To find a registered dietician near you, please visit The Academy of Nutrition and Dietetics website.
To find a registered dietician near you, please visit The Academy of Nutrition and Dietetics website.
- Exercise Regularly
Exercise is another way to keep blood sugar under control. It helps to balance food intake. After checking with your doctor, you can exercise regularly during and after pregnancy. Get at least 30 minutes of moderate-intensity physical activity at least five days a week. This could be brisk walking, swimming, or actively playing with children.Learn more about physical activity during pregnancy » - Monitor Blood Sugar Often
Because pregnancy causes the body’s need for energy to change, blood sugar levels can change very quickly. Check your blood sugar often, as directed by your doctor. - Take Insulin, If Needed
Sometimes a woman with gestational diabetes must take insulin. If insulin is ordered by your doctor, take it as directed in order to help keep blood sugar under control.
- Get Tested for Diabetes after Pregnancy
Get tested for diabetes 6 to 12 weeks after your baby is born, and then every 1 to 3 years.For most women with gestational diabetes, the diabetes goes away soon after delivery. When it does not go away, the diabetes is called type 2 diabetes. Even if the diabetes does go away after the baby is born, half of all women who had gestational diabetes develop type 2 diabetes later. It’s important for a woman who has had gestational diabetes to continue to exercise and eat a healthy diet after pregnancy to prevent or delay getting type 2 diabetes. She should also remind her doctor to check her blood sugar every 1 to 3 years.
Women who had gestational diabetes or who develop prediabetes can also learn more about the National Diabetes Prevention Program (National DPP), CDC-recognized lifestyle change programs. To find a CDC-recognized lifestyle change class near you, or join one of the online programs.
More Information
Gestational Diabetes and Pregnancy [PDF – 1 MB]
View, download, and print this brochure about gestational diabetes and pregnancy.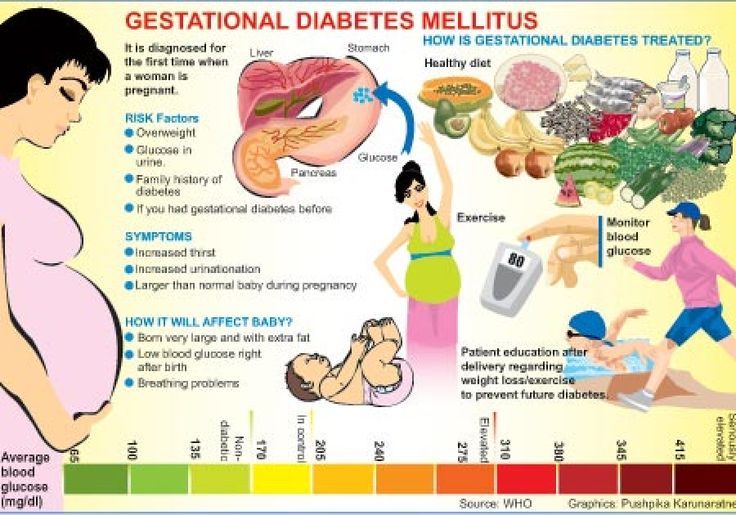
For more information on gestational diabetes, visit the American Diabetes Association’s website.
- Diabetes
- Before Pregnancy
- Healthy Pregnancy
- Birth Defects
- CDC’s National Center on Birth Defects and Developmental Disabilities
You can prevent and reverse gestational diabetes, and lower your child’s risk of autism
- Blood Sugar Control
| Jonathan Wright, MD
• Xanthurenic acid (XA)—a tryptophan metabolite—is high in serum in gestational diabetes
• Xanthurenic acid binds insulin, impeding it’s action
• Vitamin B6 lowers xanthurenic acid levels to normal
• In two 1970s research studies, 86% and 100% of women with gestational diabetes normalized their blood sugar in two weeks by taking vitamin B6
• Gestational diabetes increases autism risk for the unborn child; vitamin B6 eliminates that extra risk
No, not kidding! If you’re a pregnant woman who never had any sort of diabetes before you became pregnant, and developed high blood sugar only after becoming pregnant (gestational diabetes), you can safely eliminate it all by yourself within two to three weeks.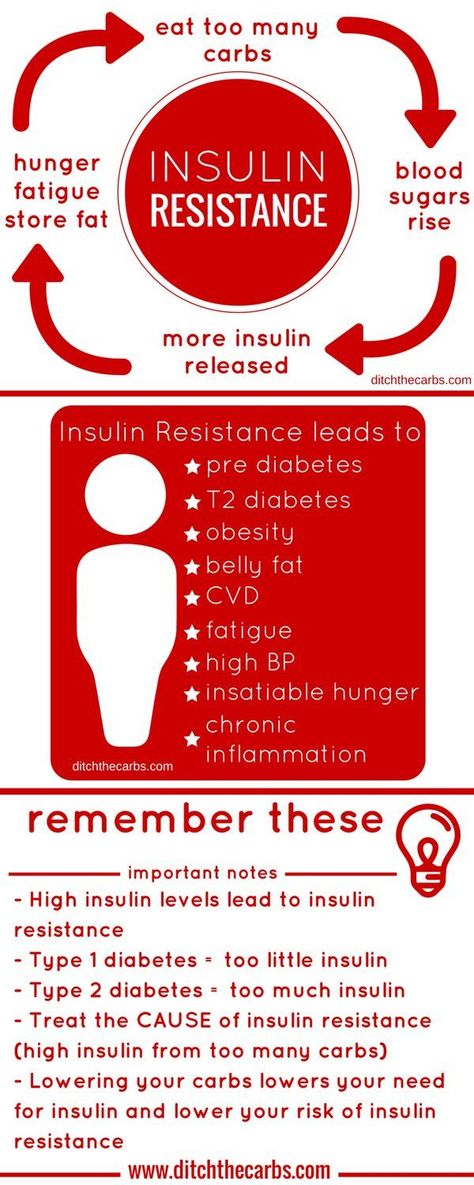 You might have the remedy at home already! If not, a trip to your favorite natural food store, compounding pharmacy, or maybe even an online order from the Tahoma Clinic Dispensary or other online source will equip you to eliminate gestational diabetes almost every time.
You might have the remedy at home already! If not, a trip to your favorite natural food store, compounding pharmacy, or maybe even an online order from the Tahoma Clinic Dispensary or other online source will equip you to eliminate gestational diabetes almost every time.
Of course, if you’re a man, you’ll never have this problem. However, your wife, sister, or daughter might, so keep this information in mind in case it’s ever needed.
One of many reasons gestational diabetes should be eliminated as rapidly as possible was discovered recently, and published in the Journal of the American Medical Association just last year. What is this reason? Autism!
Here’s what the researchers wrote: “Exposure to maternal gestational diabetes mellitus diagnosed by 26 weeks’ gestation was associated with increased risk of autism spectrum disorder in offspring.”[i] Yes, that’s extra risk for the child of developing autism!
But even though blood and urine sugar is higher than normal in those with gestational diabetes, gestational diabetes is not type 2 or even type 1 diabetes mellitus! To make this point clear to everyone, gestational diabetes should be renamed “diabetes mellitus xanthurenica” to clearly identify its cause: excess serum xanthurenic acid. When this renaming occurs, even conventional medicine might quit treating gestational diabetes with a “diabetic diet” and insulin and might instead actually treat the cause!
When this renaming occurs, even conventional medicine might quit treating gestational diabetes with a “diabetic diet” and insulin and might instead actually treat the cause!
Here’s what WebMD says is the cause of gestational diabetes:
During pregnancy, the placenta…releases hormones that help your baby grow. Some of these make it harder for your body to make or use insulin. This is called insulin resistance….To keep your blood sugar levels steady, your pancreas has to make…as much as three times more [insulin] than usual. If it can’t make enough extra insulin, your blood sugar will rise and you’ll get gestational diabetes.[ii]
And here’s what the American Diabetes Association tells women:
Treatment for gestational diabetes always includes special meal plans and scheduled physical activity. It may also include daily blood glucose testing and insulin injections.[iii]
Let’s send a note to WebMD and the ADA: “Read the medical research!” What actually causes gestational diabetes was well researched between the 1940s and 1975, when a report[iv]summarized the earlier research and then explained that gestational diabetes is caused by excessive amounts of xanthurenic acid, usually present in blood in very low levels.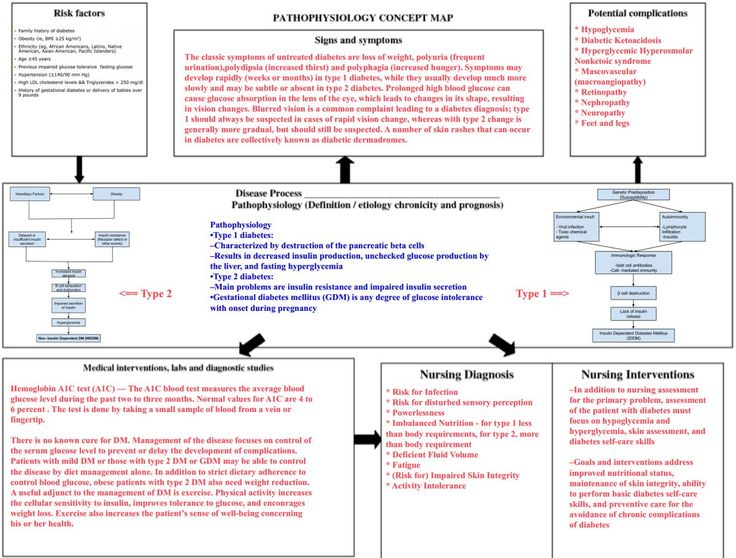 All this xanthurenic acid combines with insulin molecules and blocks its activity. The “xanthurenic acid-insulin complex” can’t activate insulin receptors nearly as well as insulin alone does, and blood sugar rises.
All this xanthurenic acid combines with insulin molecules and blocks its activity. The “xanthurenic acid-insulin complex” can’t activate insulin receptors nearly as well as insulin alone does, and blood sugar rises.
Back to the causes of diabetes mellitus type 2 and type 1. In type 2, the cause is overproduction of insulin in response to carbohydrates (and dairy, but an explanation for that at another time). As the March issue of Green Medicine explains, overproduced, chronically high insulin causes insulin resistance, which in turn leads to even more insulin secretion to overcome that resistance, which leads to even more insulin secretion.
This back-and-forth upward-trending interplay (more insulin, more resistance, even more insulin, even more resistance, and so on) goes on and on (unless “carbs”—and dairy—are significantly restricted) until the insulin resistance is so strong it can’t be completely overcome, no matter how much insulin there may be. Blood sugar then goes too high—and it’s diagnosed as type 2 diabetes. This known cause of type 2 diabetes is very different than the cause of diabetes mellitus xanthurenica!
This known cause of type 2 diabetes is very different than the cause of diabetes mellitus xanthurenica!
The cause of type 1 diabetes is much simpler. For a variety of reasons, the insulin-producing cells (“islet cells”) become weak and die. When that happens, insulin levels go lower and lower, until there’s very little insulin, or even none—and that’s type 1 diabetes. Again, a very different cause from diabetes mellitus xanthurenica.
But doesn’t everyone’s body chemistry make xanthurenic acid? (It’s a metabolite of tryptophan.) Indeed, 100% of us have this body chemistry. So why don’t we all have gestational diabetes even if we’re not pregnant or even women? The reason is that levels of xanthurenic acid are relatively low in most of us (unless we’re deficient in a certain B vitamin to be named later), so not very much of the “xanthurenic acid-insulin complex” is formed.
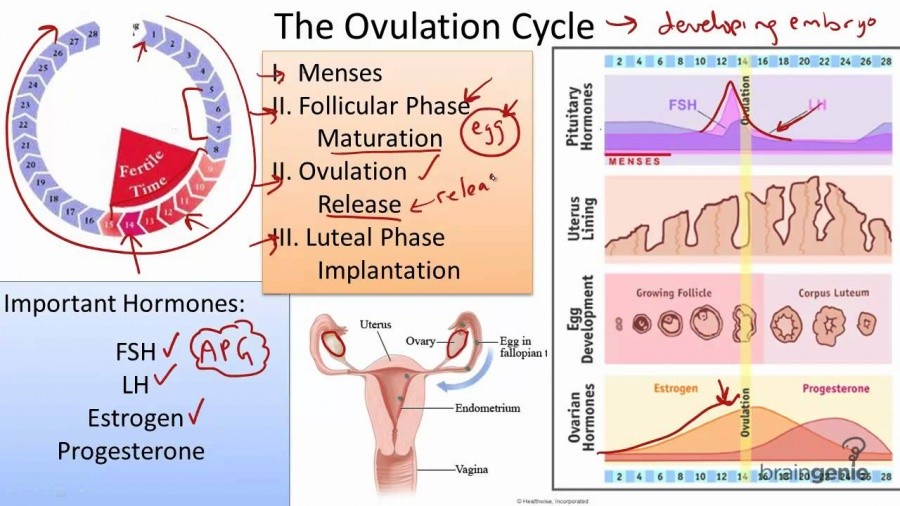
What’s different during pregnancy? Among other things, it’s a combination of “genetic” causes together with those really-high-estrogen levels that women’s bodies make when pregnant—way, way more than when not pregnant. But why does all that extra estrogen cause only a minority of women’s bodies to make lots more xanthurenic acid and develop gestational diabetes, when most women’s bodies don’t do that?
But why does all that extra estrogen cause only a minority of women’s bodies to make lots more xanthurenic acid and develop gestational diabetes, when most women’s bodies don’t do that?
That’s the “genetic” part: women who develop gestational diabetes have “weakness” in the enzymes that metabolize tryptophan into serotonin and melatonin, but no weakness in the enzymes that metabolize tryptophan into xanthurenic acid. Without the pregnancy levels of estrogen “putting pressure” on these weak enzymes, they can perform as they do in most women—metabolizing much less of their tryptophan into xanthurenic acid, and much more of it into many other molecules we’ve all heard about, including serotonin and melatonin.
With the high levels of estrogen during pregnancy, the weak enzymes falter and metabolize much more tryptophan than usual into xanthurenic acid and much less into melatonin, serotonin, and related molecules. If there’s much more xanthurenic acid, there’s much more “insulin-xanthurenic acid complex” formed, and greater impairment of insulin activity.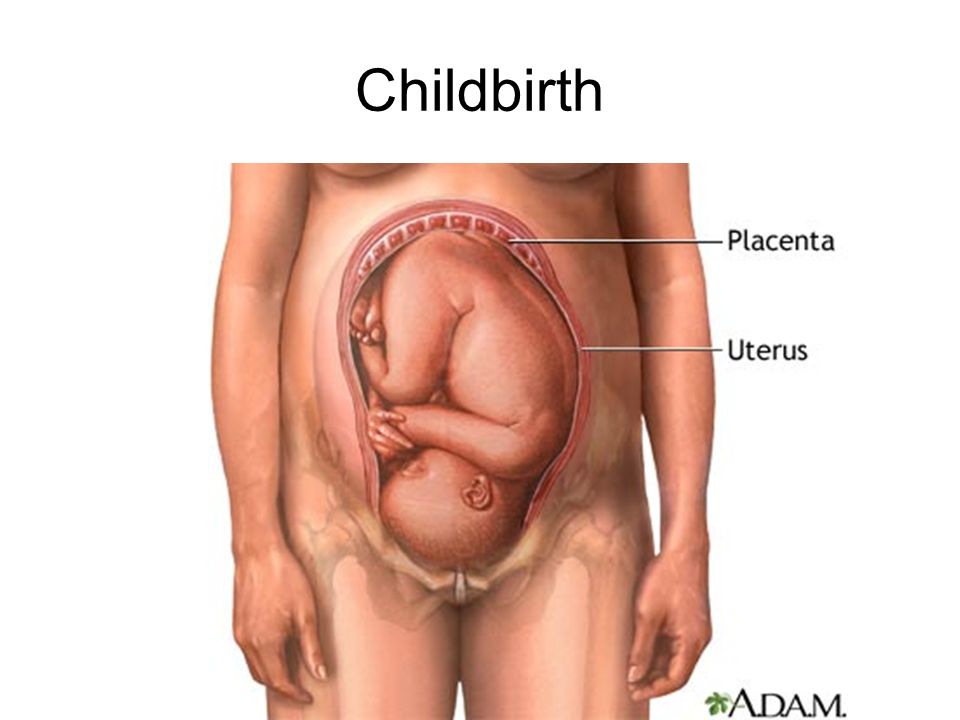 With enough insulin impaired, diabetes—“gestational”—is the result.
With enough insulin impaired, diabetes—“gestational”—is the result.
But a woman can’t stop being pregnant (for many months, anyway), and she definitely can’t change her genetics, so she can’t really rid herself of gestational diabetes, returning to normal blood sugar levels (while reducing her baby’s risk of autism, too) within two to three weeks. Or can she?
Yes, she can! To understand how, here is a refresher on what many of us learned—or should have learned—in high school and college chemistry about how enzymes change one molecule into another.
The key is that enzymes never work alone. They’re always aided by co-factors that are almost always “essential” (necessary to life) vitamins and minerals! Without those co-factors, the enzymes can’t function, and ultimately we die. That’s why they’re defined as “essential” nutrients!
“Weak” enzyme function can frequently be strengthened by adding in more co-factors! A key co-factor for the enzymes that metabolize tryptophan into serotonin and melatonin is vitamin B6. Here are the results that women with gestational diabetes achieved by taking extra vitamin B6 to strengthen their genetically “weak” enzymes.
Here are the results that women with gestational diabetes achieved by taking extra vitamin B6 to strengthen their genetically “weak” enzymes.
In 1975, fourteen pregnant women were diagnosed with gestational diabetes by the standard glucose tolerance test. All the women took 100 milligrams of vitamin B6 (as pyridoxine) daily for two weeks. Repeat testing found that twelve of the fourteen (86%) no longer had the problem![v]
In 1977, different researchers reported almost identical results in the same length of time for thirteen women.[vi] All took 100 milligrams daily of vitamin B6 (as pyridoxine). Glucose tolerance tests were done before and after. All fourteen women (100%) had “statistically significant” improvements in their glucose tolerance tests. The researchers wrote: “Low vitamin B6 levels appear to alter metabolic pathways which result in a lowering of the biologic activity of endogenous insulin.” In English: vitamin B6 strengthened specific weak enzymes so that less xanthurenic acid was available to be “complexed” with insulin, blocking its activity. Better blood sugar control was regained.
Better blood sugar control was regained.
The 1975 and 1977 research was actually done more than two decades after several groups of researchers[vii],[viii],[ix],[x] had confirmed in the early 1950s that vitamin B6 returned levels of xanthurenic acid to normal. For the technically inclined, all the 1950s research and much more was reviewed in a 1960 publication titled, “The Effect of Vitamin Supplementation on the Urinary Excretion of Tryptophan Metabolites by Pregnant Women”[xi]—which confirmed that pyridoxine lowered xanthurenic acid!
And one last fact: textbooks of laboratory medicine in the 1940s told us that higher-than-usual xanthurenic acid in urine is diagnostic for vitamin B6 deficiency! It’s 2016, yet despite all this forty- to seventy-year-old basic science and clinical research demonstrating the cause and cure of gestational diabetes, it’s still not being applied!
But you—yes, you, if you want to prevent gestational diabetes or cure yourself of it—can apply this extensive science. You can safely prevent or cure gestational diabetes yourself, and at the same time reduce your child’s risk of autism!
You can safely prevent or cure gestational diabetes yourself, and at the same time reduce your child’s risk of autism!
To eliminate gestational diabetes, use pyridoxal phosphate, not pyridoxine
Don’t use the “pyridoxine” form of vitamin B6. That’s actually the “inactive” form of vitamin B6,which actually does not activate the receptors for this vitamin. Most—but not all—humans can “activate” pyridoxine, but we have no way (without testing) to know if you are in the pyridoxine-activating group or not. (It’s quite possible that the 14% whose gestational diabetes didn’t disappear in the 1975 research summarized above were “poor activators” of pyridoxine.)
To make sure the pyridoxine actually does its job, it’s best to use the “active” form, pyridoxal-5-phosphate (usually shortened to P5P), fortunately available nearly everywhere supplements are sold, usually in a 50 milligram size. Don’t stop using your “pregnancy multivitamin/ mineral supplement” as it contains the rest of the B-complex vitamins which “back up” the pyridoxal-5-phosphate.
Check with your “natural medicine” doctor…
1. If you have any doubts at all about doing this!
2. Towards the anticipated delivery date. Vitamin B6 in both forms can inhibit the production of prolactin,[xii] the hormone necessary for normal lactation and nursing. Work with a physician skilled and knowledgeable in natural and nutritional medicine to help you determine (possibly while checking your own blood sugar) a P5P “tapering schedule” so you can nurse your child normally. This physician will also be able to tell you about botanicals used for centuries by to improve lactation should they be needed.
A special thank you to author Adelle Davis, whose description of the research findings in reference #4 has helped me to help women reverse gestational diabetes for more than thirty years!
Published in: Aug 5, 2016 | www.GreenMedicineNewsletter.com
References
[i] Xiang A, et al. “Association of Maternal Diabetes with Autism in Offspring. ” JAMA 2015;313(14):1425-1434.
” JAMA 2015;313(14):1425-1434.
[ii] http://www.webmd.com/diabetes/gestational-diabetes-guide/what-causes-gestational diabetes
[iii] http://www.diabetes.org/diabetes-basics/gestational/how-to-treat-gestational.html
[iv] Kotake Y, Ueda T, et al. “The Physiological Significance of the Xanthurenic Acid-InsulinComplex.” J Biochem 1975;77:685-687.
[v] Bennink HJ, Schreurs WH. “Improvement of oral glucose tolerance in gestational diabetes by pyridoxine.” Br Med J. 1975 Jul 5;3(5974):13-5.
[vi] Spellacy WN, Buhi WC, and Birk SA. “Vitamin B6 treatment of gestational diabetes mellitus: Studies of blood glucose and plasma insulin.” Am J Ob Gyn 1977;127(6):599-602.
[vii] Sprince H, Lowy, RS, et al. Studies on the urinary excretion of ‘”xanthurenic acid’” during normal and abnormal pregnancy: A survey of the excretion of ‘”xanthurenic acid” ’ in normal nonpregnant, normal pregnant, pre-eclamptic, and eclamptic women.” Am J Obstet Gyn. 1951;62:84.
[viii] Vandelli, I.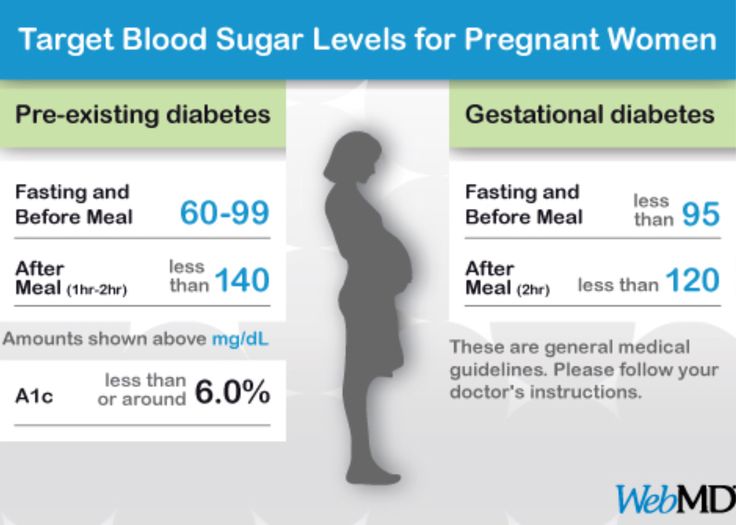 “The use of vitamin B. (pyridoxine) for suppressing the elimination of xanthurenic acid in pregnant and non-pregnant women following the oral intake of a measured quantity of tryptophan.” Acta vitamin. (Milano) 1951;5:55.
“The use of vitamin B. (pyridoxine) for suppressing the elimination of xanthurenic acid in pregnant and non-pregnant women following the oral intake of a measured quantity of tryptophan.” Acta vitamin. (Milano) 1951;5:55.
[ix] Wachstein M, Gudaitis A. “Disturbance of vitamin B6 metabolism in pregnancy. II. The influence of various amounts of pyridoxine hydrochloride upon the abnormal tryptophane load test in pregnant women.” J Lab Clin Med 1953;42:98.
[x] Wachstein M., Lobel S. “Abnormal tryptophan metabolites in human pregnancy and their relation to deranged vitamin B, metabolism.” Proc Soc Exp Biol (N.Y.) 1954;86:624.
[xi] Brown RR, Thornton MJ, Price JM. “The Effect of Vitamin Supplementation on the Urinary Excretion of Tryptophan Metabolites by Pregnant Women.” J Clin Invest 1961.
[xii] Ren S-G, Melmed S. Pyridoxal Phosphate Inhibits Pituitary Cell Proliferation And Hormone Secretion. Endocrinology 2006;147(8):3936-3942
Gestational diabetes in pregnancy - treatment and diagnosis of diabetes in pregnant women in Moscow, Clinical Hospital on Yauza
Consult a gynecologist
Service in two languages: Russian, English.
Leave your phone number and we will call you back.
Contents
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0006
Specialists of the Yauza Clinical Hospital diagnose and treat gestational diabetes and its complications. For a comfortable pregnancy and the safety of the expectant mother and baby, we exercise strict control over the blood sugar level of a pregnant woman, if necessary, prescribe a specially designed diet and medications.
Make an appointment with a gynecologist
- About 7% of pregnant women have manifestations of gestational diabetes. In 50% of cases, the disease is asymptomatic
- Gestational diabetes in pregnancy significantly increases the risk of pregnancy complications for both mother and fetus
- Perinatal mortality increases by 2-3% with a combination of diabetes mellitus and pregnancy
Pregnancy diabetes (gestational diabetes) is an increase in blood glucose that first occurs during pregnancy but is not high enough to warrant a diagnosis of diabetes mellitus. These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes mellitus. nine0006
These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes mellitus. nine0006
Pregnant blood glucose norm
During pregnancy, all women experience changes in insulin sensitivity and glucose tolerance. This is fine. The difference between the norm and pathology in the degree of change.
Blood tests for diabetes during pregnancy - norm and pathology
- If a fasting venous blood test shows a glucose level of more than 5.1 mmol/l, this is normal for pregnant women.
nine0022 From 5.1 to 7.0 mmol / l - gestational diabetes. - If 7.0 mmol / l or more - diabetes mellitus.
- Testing capillary blood (taken from a fingerstick) for the diagnosis of gestational diabetes mellitus is not recommended.
- If during an oral glucose tolerance test (when 75 g of glucose is taken orally during the study) after one hour the glucose level is more than 10.0 mmol/l, and after two hours the blood glucose level is in the range of 7.
 8-8.5 mmol/l - then for pregnant women this is a normal indicator. nine0023
8-8.5 mmol/l - then for pregnant women this is a normal indicator. nine0023
To better understand what gestational diabetes, or diabetes in pregnancy, is, you need to talk a little about hormonal changes in the body in pregnant women.
Causes of gestational diabetes
Hormonal changes that occur during pregnancy are associated with increased production of large amounts of steroid hormones. Some of them, such as cortisol and progesterone, have a significant effect on cell receptors, increasing their resistance to insulin. nine0005 This leads to an increase in blood glucose levels and requires a significant increase in insulin production by the pancreas. In cases where the compensatory capacity of the pancreas is not enough, sugar metabolism gets out of control and a condition called gestational diabetes or gestational diabetes develops.
This condition occurs quite often. Between 3 and 10% of pregnant women develop pathological insulin resistance leading to gestational diabetes.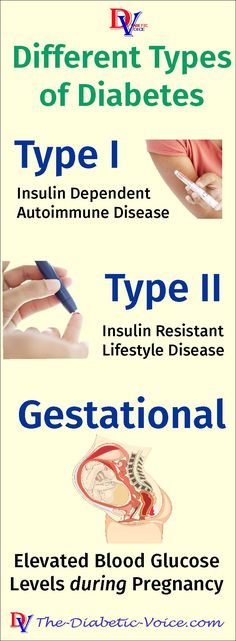 nine0005 Unlike diabetes mellitus diagnosed before pregnancy, pathological insulin resistance that develops during pregnancy does not cause fetal malformations and in most cases does not require insulin treatment. But, nevertheless, uncompensated gestational diabetes can significantly complicate the course of pregnancy.
nine0005 Unlike diabetes mellitus diagnosed before pregnancy, pathological insulin resistance that develops during pregnancy does not cause fetal malformations and in most cases does not require insulin treatment. But, nevertheless, uncompensated gestational diabetes can significantly complicate the course of pregnancy.
Specialists of the Clinical Hospital on Yauza diagnose, treat and prevent diabetes in pregnant women and its complications, such as impaired intrauterine growth of the fetus. Doctors of the Yauza Clinical Hospital strictly control the blood sugar level of a pregnant woman, and if necessary prescribe a specially designed diet. This ensures a comfortable pregnancy and the safety of the expectant mother and baby. nine0006
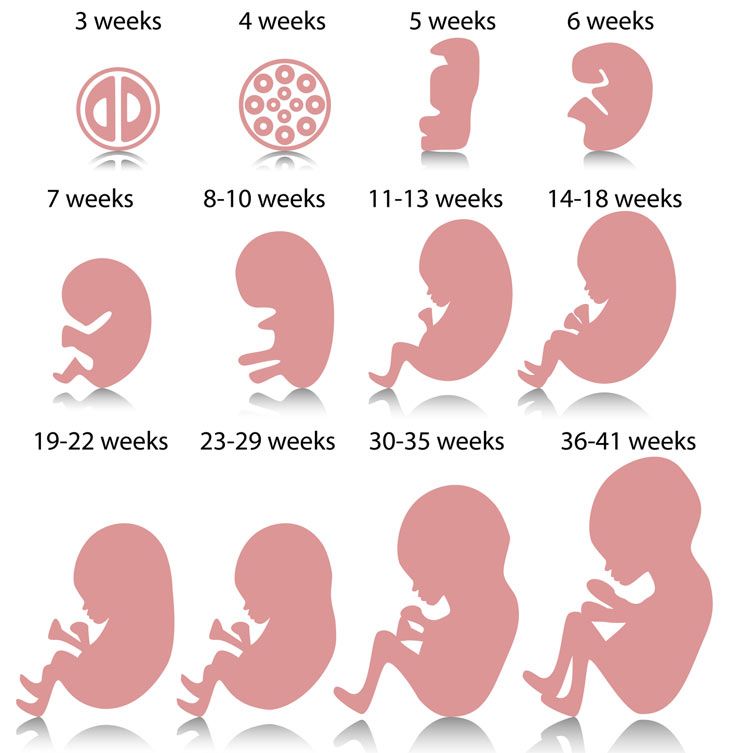
Pregnancy diabetes - consequences for the child
Large disproportionate fetus. The most important and frequent complication of gestational diabetes is fetal growth failure. Developing in conditions of increased blood glucose levels, which penetrate the fetoplacental barrier, the fetus is forced to compensate for the increased sugar level with its own insulin. Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate the growth of the fetus. The problem is that a large fetus develops. In such a fetus, body proportions differ from those of normally developing newborns, in which the volume of the head is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth after the fetus's head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the child, along with the mother, can be severely injured or die. nine0006
Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate the growth of the fetus. The problem is that a large fetus develops. In such a fetus, body proportions differ from those of normally developing newborns, in which the volume of the head is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth after the fetus's head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the child, along with the mother, can be severely injured or die. nine0006
Polyhydramnios or oligohydramnios. In addition, in gestational diabetes, the balance of the amount of amniotic fluid can be disturbed and either polyhydramnios or oligohydramnios develops. This is a serious risk factor for intrauterine fetal death or premature birth.
Underdevelopment of the lungs. In gestational diabetes, the lungs of the fetus mature later, as the production of surfactant (a special lubricant for the inner walls of the alveoli, where oxygen is exchanged in the lungs) is disrupted. Therefore, premature birth in gestational diabetes is especially dangerous. nine0006
Hypoglycemia and metabolic disorders in the fetus. Due to the constant increased production of its own insulin during pregnancy, immediately after birth, the child is in a state of hypoglycemia with electrolyte imbalance, which threatens his life.
All this dictates the need for the earliest possible detection of gestational diabetes in pregnant women, the level of sugar in the blood of a pregnant woman and to prevent the development of complications.
. nine0006
Diagnosis of diabetes in pregnant women at the Yauza Clinical Hospital
Signs of diabetes in pregnant women
Gestational diabetes in pregnancy is not usually associated with the classic symptoms of diabetes, such as thirst or excessive urination (polyuria).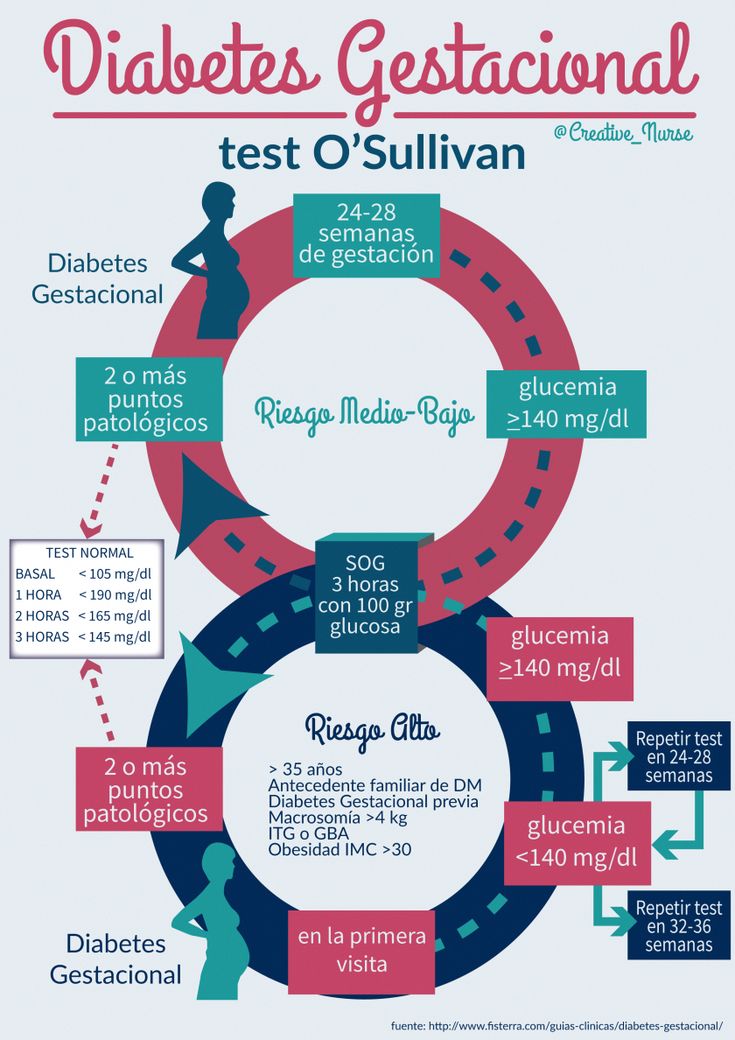
Pregnancy tests for diabetes mellitus
First phase. At the first visit of a pregnant woman to a doctor at any time, she is tested for glucose levels in venous blood - fasting glucose, regardless of food intake, glycated hemoglobin. This is the first phase of research to detect diabetes mellitus or gestational diabetes in pregnant women. If diabetes mellitus is detected, the patient is referred for observation and treatment to an endocrinologist. nine0006
Second phase. For a period of 24-28 weeks, all patients who did not show identified disorders of carbohydrate metabolism at the first study are called for a glucose tolerance test (PGTT) to detect "hidden diabetes". This is done because the occurrence of gestational diabetes is associated with the development of insulin resistance under the influence of hormones produced by the placenta. Therefore, in the vast majority of cases, gestational diabetes develops in the second half of pregnancy after 24 weeks, when there is a peak in the production of placental hormones. nine0006
nine0006
Glucose tolerance test
It is carried out to detect pathological insulin resistance, characteristic of latent diabetes in pregnant women. Pregnant women undergo a two-hour test, only in the laboratory.
During the 3 days leading up to the test, the woman should eat her usual diet, including carbohydrates (>150 g of carbohydrates per day), maintain her usual physical activity. The evening before testing, dinner should include 30-50 grams of carbohydrates. nine0005 On the day of the study, before the analysis, you should not smoke and take medications that can affect the level of glucose (vitamins, glucocorticoid hormones, iron preparations, which include carbohydrates, beta-agonists, beta-blockers). You can drink water.
Venous blood is taken on an empty stomach (after 8-14 hours of fasting, usually in the morning, before breakfast).
Then the patient takes a glucose solution (75 g).
And they take blood in an hour and two after the sugar load. Normally, the level of glucose in the blood after a sugar load should not exceed an hour later - 10 mmol / l, after 2 hours - 8.5 mmol / l. nine0005 If manifest diabetes mellitus is detected, the patient is referred to an endocrinologist, gestational diabetes mellitus is treated by an obstetrician-gynecologist or therapist.
Normally, the level of glucose in the blood after a sugar load should not exceed an hour later - 10 mmol / l, after 2 hours - 8.5 mmol / l. nine0005 If manifest diabetes mellitus is detected, the patient is referred to an endocrinologist, gestational diabetes mellitus is treated by an obstetrician-gynecologist or therapist.
Glucose tolerance test contraindications
- Strict bed rest for a pregnant woman (until doctor's approval).
- Pronounced toxicosis of pregnant women (with nausea and vomiting).
- Acute infectious or inflammatory disease. nine0023
- Exacerbation of chronic pancreatitis.
- Dumping syndrome (syndrome of resected stomach).
Prenatal diabetes monitoring
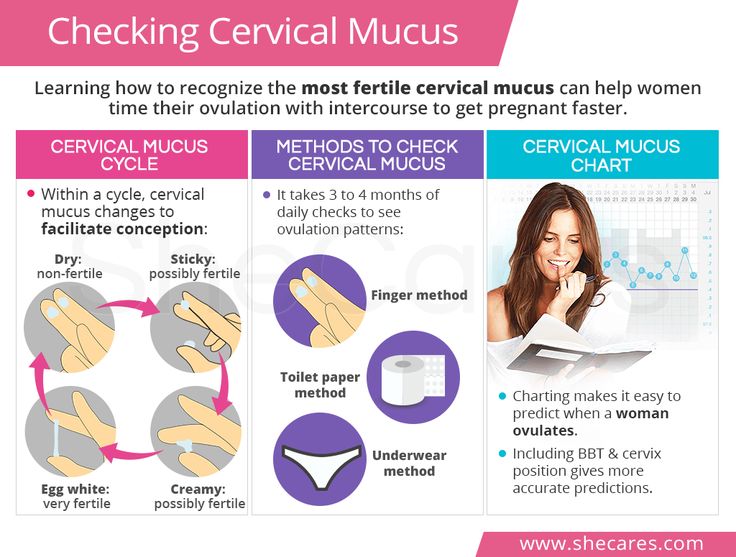
Blood glucose monitoring, self-monitoring diary
When diagnosing gestational diabetes, it is necessary to establish strict control of sugar levels throughout the subsequent pregnancy and during childbirth. To do this, regularly examine the blood for sugar (glucose). In addition, the patient conducts self-monitoring using a glucometer. nine0006
In addition, the patient conducts self-monitoring using a glucometer. nine0006
It is recommended that a pregnant woman keep a diary of observations in which to record:
- blood glucose level (normal <5.1 mmol/l),
- the presence of ketone bodies in the urine, which is determined by test strips sold in a pharmacy (normally, ketone bodies are absent),
- blood pressure readings (normal <130|80 mmHg),
- fetal movements,
- body weight, nine0022 diet.
Expert ultrasound
Conducting an expert ultrasound examination reveals signs of intrauterine suffering of the fetus (diabetic fetopathy), polyhydramnios. Most often, this is a sign of chronically elevated blood glucose levels, penetrating into the blood of the fetus. This requires urgent correction of the diet and normalization of the level of glycemia (blood sugar). If necessary, insulin therapy.
Make an appointment nine0006
Treatment of gestational diabetes
Diet for gestational diabetes
In most cases, it is sufficient to follow a special diet recommended by a nutritionist based on the body mass index of the pregnant woman and her taste preferences. The effectiveness of diet therapy is determined by the maintenance of normal blood glucose levels. Diet in pregnancy diabetes recommends:
The effectiveness of diet therapy is determined by the maintenance of normal blood glucose levels. Diet in pregnancy diabetes recommends:
- Avoid simple carbohydrates - sweets, pastries, white bread, honey, sugar, jam, sweet drinks and fruits, ice cream. nine0023
- Limit complex carbohydrates - cereals (semolina, rice - exclude), potatoes, corn, legumes, durum wheat pasta. Distribute their intake evenly over several meals throughout the day to eliminate starvation (causes the formation of ketone bodies).
- Eat enough protein - meat, fish, seafood, poultry, mushrooms, eggs, hard cheese, dairy and sour-milk products of medium fat content (3-5%).
- It is necessary to enrich the diet with fiber and vitamins - greens, vegetables (except for boiled carrots and beets), sweet and sour berries (excluding grapes). nine0023
- Correctly choose fats, do not exceed their amount recommended by the doctor - vegetable oils (add to ready-made meals), nuts, seeds.
 Animal fats (butter, sausages) - limit.
Animal fats (butter, sausages) - limit. - When cooking, boil, stew, steam and bake dishes. Don't fry. Do not deep fry.
A detailed menu for a pregnant woman with gestational diabetes will be compiled by a doctor, taking into account the individual characteristics of each particular woman. nine0005 It is not worth using table No. 9 in its pure form for pregnant women with diabetes mellitus due to a significant restriction of its calorie content.
In detail, what you can eat with diabetes in pregnant women will be told by the doctor at an in-person consultation.
Pharmacotherapy
In cases where the diet fails to achieve the desired control of the level of glycemia in the blood, there are signs of a negative effect on the fetus - they resort to prescribing drugs - insulin. In case of diabetes in pregnant women, antidiabetic drugs in tablets should not be used. Insulin therapy is prescribed by an endocrinologist. Pregnant women with diabetes who are on insulin therapy are jointly managed by an endocrinologist, an internist and an obstetrician-gynecologist. nine0006
nine0006
Physical activity
Patients are recommended regular physical activity - walking in the fresh air (at least 150 minutes per week), swimming.
Prenatal diabetes - childbirth
With a compensated course of gestational diabetes, normal development of the fetus and the condition of the woman, childbirth is carried out in time in a natural way. The question of early delivery, caesarean section may arise if there are appropriate indications from the mother or fetus. nine0006
Specialists of the Yauza Clinical Hospital included mandatory fetal development screenings and tests to diagnose sugar metabolism disorders in the pregnancy monitoring program. Recommendations are given on a special diet for women with manifestations of gestational diabetes. If necessary, strict glycemic control is carried out throughout pregnancy, ensuring its successful completion and the birth of a healthy child.
Make an appointment nine0006
Cost of services
Prices for services you can see in the price list or check by phone listed on the site.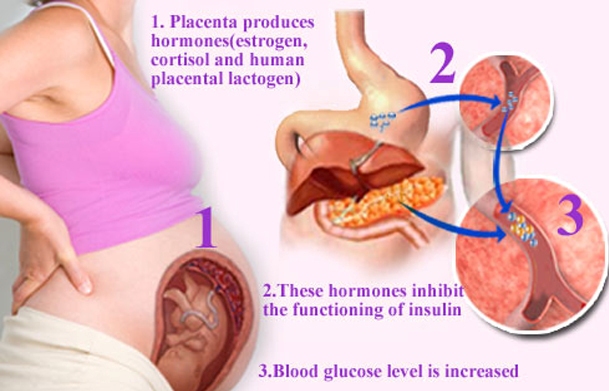
Attention! Website prices may vary.
Please check the current cost with the administrators by phone.
BOOK AN APPOINTMENT. WE WORK WITHOUT DAYS OFF
Service in two languages: Russian, English.
Leave your phone number and we will call you back. nine0006
Benefits of the clinic
More than 100
specialists
More than 35 000
satisfied clients
Hospital
with 15 beds
More than 30
Gestational diabetes during pregnancy
Gestational Diabetes
2What Causes Gestational Diabetes?
Doctors don't know exactly what causes gestational diabetes, but they have some ideas about it.
The placenta supports and nourishes the baby as it grows. Hormones from the placenta help the baby develop. But these same hormones also block the action of insulin, reducing its effectiveness. Gestational diabetes occurs when your body is no longer able to produce and use all the insulin it needs during pregnancy, resulting in high blood glucose levels if left untreated.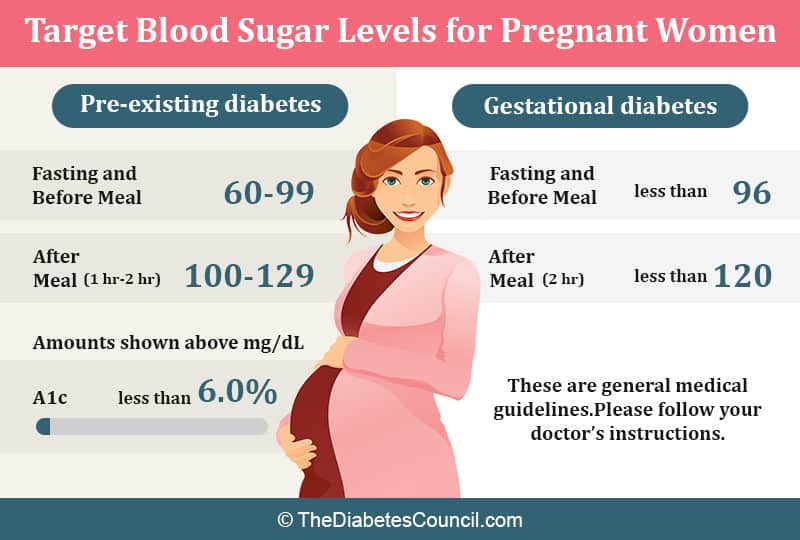
Some women are at higher risk of developing gestational diabetes. The following factors increase the risk of developing gestational diabetes:
- Overweight before pregnancy
- Too much weight gain during pregnancy (more than the recommended amount)
- Age over 25
- History of gestational diabetes
- Presence of diabetes in close relatives
- African American, Asian, Hispanic or Native American origin
How is gestational diabetes diagnosed?
Most women who receive good medical care during pregnancy are regularly screened for gestational diabetes between the 24th and 28th weeks of pregnancy. If you are at high risk of developing gestational diabetes, your doctor may test you earlier and/or more than once during your pregnancy. nine0006
During the test for gestational diabetes, your doctor will ask you to drink a sugary drink, and you will have a blood sample taken before and after you drink the drink.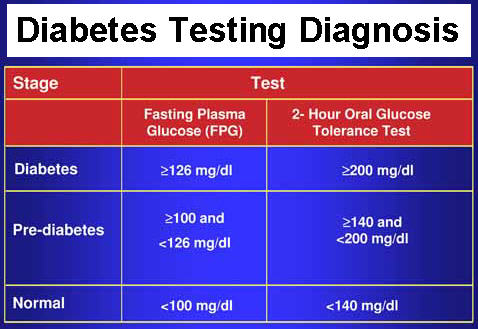 If the results show that the blood glucose level at the specified time is above the recommended limits, the diagnosis of gestational diabetes is confirmed. Your doctor will tell you about a plan for treating gestational diabetes.
If the results show that the blood glucose level at the specified time is above the recommended limits, the diagnosis of gestational diabetes is confirmed. Your doctor will tell you about a plan for treating gestational diabetes.
Why is it important to treat gestational diabetes?
A mother instinctively protects her child. It is important for the health of both mother and child that treatment for gestational diabetes be started as soon as the diagnosis is made. If left untreated, gestational diabetes can cause problems that include the following:
- An increased chance of having a large baby weighing more than 4 kg - this condition is called macrosomia. It increases the likelihood
- complications and injuries during vaginal delivery;
- cesarean section. (K-section)
- Your baby is at high risk for preterm labor and breathing problems (respiratory distress)
- Your baby is at high risk for low blood sugar (hypoglycemia) shortly after birth nine0022 You are more likely to have preeclampsia (high blood pressure and liver or kidney problems)
Following your doctor's instructions and carefully managing your gestational diabetes can greatly reduce your risk of developing these complications.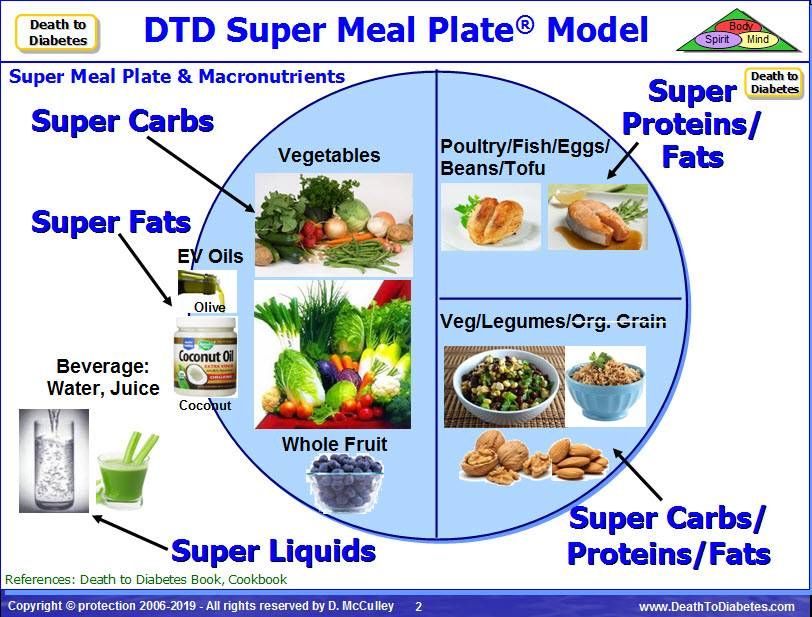
What to expect with a diagnosis of gestational diabetes?
If you have been diagnosed with gestational diabetes:
- Your doctor will recommend a healthy carbohydrate-controlled diet and exercise. In many cases, these measures will be sufficient to control blood glucose levels throughout pregnancy. nine0023
- You may need help from a dietitian in developing a healthy eating plan. A nutritionist can teach you how to control the amount and types of carbohydrates in your food so that you can manage your blood glucose levels while still meeting the needs of your growing child. You may also be asked to keep a food journal and monitor your weight.
- You may need to check your blood glucose daily with a glucometer. Ask your doctor or diabetes consultant to recommend a glucometer that is right for you. Checking and tracking your blood glucose levels will help you and your doctor manage your gestational diabetes. nine0023
As a rule, blood glucose levels should be checked at least 4 times a day, usually on an empty stomach, and then 1-2 hours after a meal.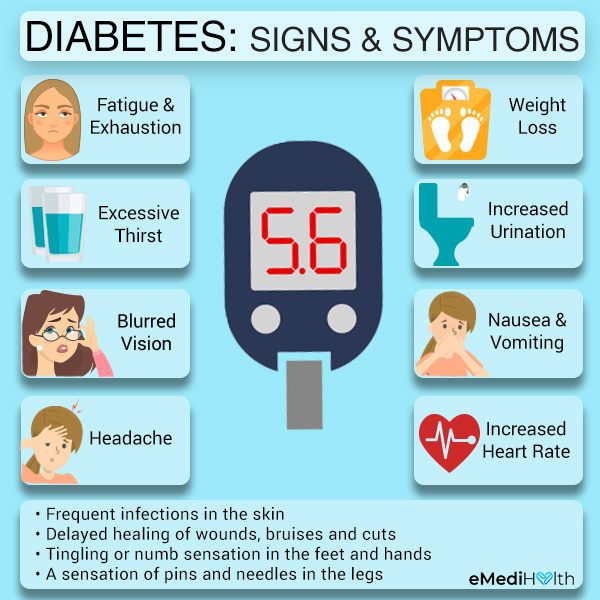 Your doctor or healthcare professional will tell you how often you should test and what your target blood glucose range is. Remember to record your blood glucose measurements, including the time and results of the test, before or after a meal, and how long after a meal the test was taken.
Your doctor or healthcare professional will tell you how often you should test and what your target blood glucose range is. Remember to record your blood glucose measurements, including the time and results of the test, before or after a meal, and how long after a meal the test was taken.
- Light exercise during pregnancy will help your body make better use of its own insulin and help control blood glucose levels. Types of exercise that can be safely performed by pregnant women include brisk walking and swimming. Talk to your doctor for advice on safe exercise during pregnancy. nine0023
At your appointment, the midwife can check your blood pressure and take a urine sample. You will also talk to your doctor about your blood glucose test results, how you eat, how much exercise you do, and how much weight you have gained. Your growing child will also be closely monitored. All this will help determine if the prescribed treatment plan for gestational diabetes is working and if it needs to be adjusted.
If dietary changes and exercise don't help control your blood glucose, your doctor may prescribe medication—pills or insulin—for the rest of your pregnancy. nine0006
Medications (pills, insulin)
Just because your doctor prescribes pills or insulin does not mean that you have failed to manage your gestational diabetes. In some cases, your body may simply not be able to produce enough insulin on its own that your body needs as your baby grows. It is very important to follow your doctor's recommendations to protect yourself and your baby. You may be able to stop taking antidiabetic drugs after the baby is born. nine0006
If your doctor prescribes insulin to treat gestational diabetes, you can get it by injection or by other means, such as an insulin pump. Someone in your family can learn this with you and help you take your insulin as prescribed by your doctor. Fortunately, today, thanks to insulin syringes with small, thin needles, injections are virtually painless.