Can being pregnant make you sick
Vomiting and morning sickness - NHS
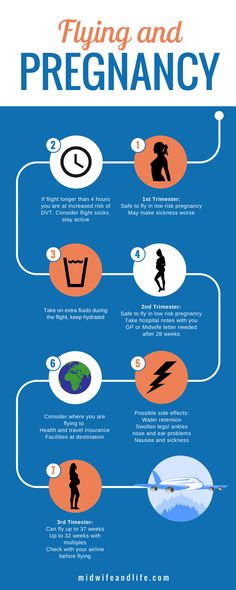
Nausea and vomiting in pregnancy, often known as morning sickness, is very common in early pregnancy.
It can affect you at any time of the day or night or you may feel sick all day long.
Morning sickness is unpleasant, and can significantly affect your day-to-day life. But it usually clears up by weeks 16 to 20 of your pregnancy and does not put your baby at any increased risk.
There is a chance of developing a severe form of pregnancy sickness called hyperemesis gravidarum. This can be serious, and there's a chance you may not get enough fluids in your body (dehydration) or not get enough nutrients from your diet (malnourishment). You may need specialist treatment, sometimes in hospital.
Sometimes urinary tract infections (UTIs) can also cause nausea and vomiting. A UTI usually affects the bladder, but can spread to the kidneys.
Non-urgent advice: Call your midwife, GP or 111 if:
you're vomiting and:
- have very dark-coloured urine or have not had a pee in more than 8 hours
- are unable to keep food or fluids down for 24 hours
- feel severely weak, dizzy or faint when standing up
- have tummy (abdominal) pain
- have a high temperature
- vomit blood
- have lost weight
Treatments for morning sickness
Unfortunately, there's no hard and fast treatment that will work for everyone’s morning sickness. Every pregnancy will be different.
But there are some changes you can make to your diet and daily life to try to ease the symptoms.
If these do not work for you or you're having more severe symptoms, your doctor or midwife might recommend medicine.
Things you can try yourself
If your morning sickness is not too bad, your GP or midwife will initially recommend you try some lifestyle changes:
- get plenty of rest (tiredness can make nausea worse)
- avoid foods or smells that make you feel sick
- eat something like dry toast or a plain biscuit before you get out of bed
- eat small, frequent meals of plain foods that are high in carbohydrate and low in fat (such as bread, rice, crackers and pasta)
- eat cold foods rather than hot ones if the smell of hot meals makes you feel sick
- drink plenty of fluids, such as water (sipping them little and often may help prevent vomiting)
- eat foods or drinks containing ginger – there's some evidence ginger may help reduce nausea and vomiting (check with your pharmacist before taking ginger supplements during pregnancy)
- try acupressure – there's some evidence that putting pressure on your wrist, using a special band or bracelet on your forearm, may help relieve the symptoms
Find out more about vitamins and supplements in pregnancy
Anti-sickness medicine
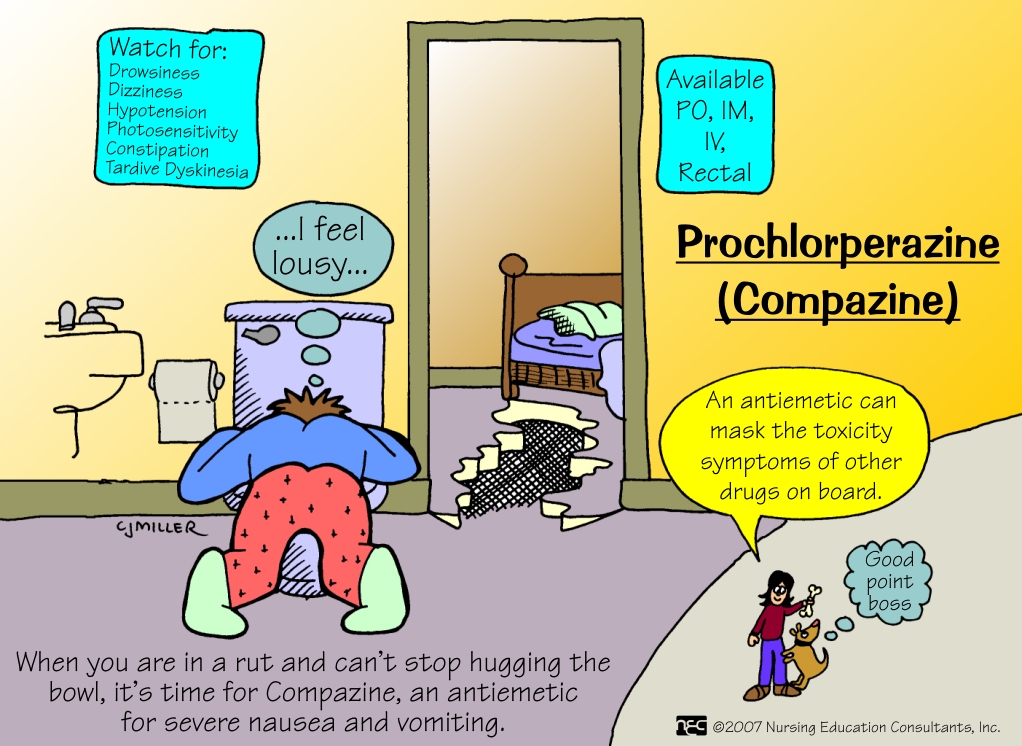
If your nausea and vomiting is severe and does not improve after trying the above lifestyle changes, your GP may recommend a short-term course of an anti-sickness medicine, called an antiemetic, that's safe to use in pregnancy.
Often this will be a type of antihistamine, which are usually used to treat allergies but also work as medicines to stop sickness (antiemetic).
Antiemetics will usually be given as tablets for you to swallow.
But if you cannot keep these down, your doctor may suggest an injection or a type of medicine that's inserted into your bottom (suppository).
See your GP if you'd like to talk about getting anti-sickness medication.
Risk factors for morning sickness
It's thought hormonal changes in the first 12 weeks of pregnancy are probably one of the causes of morning sickness.
But you may be more at risk of it if:
- you're having twins or more
- you had severe sickness and vomiting in a previous pregnancy
- you tend to get motion sickness (for example, car sick)
- you have a history of migraine headaches
- morning sickness runs in the family
- you used to feel sick when taking contraceptives containing oestrogen
- it's your first pregnancy
- you're obese (your BMI is 30 or more)
- you're experiencing stress
Visit the pregnancy sickness support site for tips for you and your partner on dealing with morning sickness.
Find maternity services near you
Sign up for pregnancy emails
Sign up for Start4Life's weekly emails for expert advice, videos and tips on pregnancy, birth and beyond.
Video: how can I cope with morning sickness?
In this video, a midwife gives advice on how to deal with morning sickness during your pregnancy.
Media last reviewed: 25 January 2023
Media review due: 25 January 2026
Page last reviewed: 13 April 2021
Next review due: 13 April 2024
Morning sickness | March of Dimes
Morning sickness is when you have nausea and vomiting during pregnancy. Even though it’s called morning sickness, it can happen any time of day.
Morning sickness usually starts at about 6 weeks of pregnancy and goes away in the second trimester.

Lots of pregnant women have morning sickness. It usually doesn’t cause harm to you or your baby.
Hyperemesis gravidarum is severe nausea and vomiting that needs treatment (sometimes in a hospital) to help you get better.
If your morning sickness is severe or if it goes into your fourth month of pregnancy, tell your health care provider right away.
What is morning sickness?
Morning sickness (also called nausea and vomiting of pregnancy) is nausea (feeling sick to your stomach) and vomiting that happens in the first few months of pregnancy. Even though it's called morning sickness, it can last all day and happen any time of day.
At least 7 in 10 pregnant women have morning sickness in the first trimester (first 3 months) of pregnancy. It usually starts at about 6 weeks of pregnancy and is at its worst at about 9 weeks. Most women feel better in their second trimester, but some have morning sickness throughout pregnancy. If you have morning sickness, tell your health care provider.
If you have morning sickness, tell your health care provider.
Mild morning sickness doesn’t harm you or your baby. But if nausea and vomiting becomes severe (called hyperemesis gravidarum), it can cause serious problems during pregnancy. You may need to stay in the hospital for treatment.
What is hyperemesis gravidarum?
About 3 in 100 women may have hyperemesis gravidarum. This is extreme, excessive nausea and vomiting during pregnancy. It can cause you to lose weight and become dehydrated (not have enough water in your body). It can start early in pregnancy and last the entire pregnancy. If you have hyperemesis gravidarum, you need treatment to help keep you and your baby safe.
You may be at risk for hyperemesis gravidarum if you:
- Are pregnant for the first time.
- Are pregnant with a girl.
- Are pregnant with multiples (twins, triplets or more). Being pregnant with more than one baby may increase your risk for severe morning sickness because you may have a large placenta and increased pregnancy hormones.
 The placenta grows in your uterus (womb) and supplies your babies with food and oxygen through the umbilical cord.
The placenta grows in your uterus (womb) and supplies your babies with food and oxygen through the umbilical cord. - Had mild or severe morning sickness in a previous pregnancy, or your mother or sister had severe morning sickness during pregnancy. Take your family health history to help you find out about health conditions that run in your family.
- Have motion sickness or migraines. A migraine is a severe headache that may make you sensitive to bright lights and sound.
- Are overweight.
- Have trophoblastic disease, a condition that leads to abnormal cell growth in the uterus (womb).
Signs and symptoms of hyperemesis gravidarum include:
- Vomiting more than 3 to 4 times a day
- Vomiting that makes you dizzy or lightheaded
- Vomiting that makes you dehydrated. Signs and symptoms of dehydration include feeling thirsty, dry mouth, a fast heart beat or making little to no urine.
- Losing more than 10 pounds in pregnancy
If you have hyperemesis gravidarum, your provider may treat you with medicine to help relieve your nausea and vomiting. You may need treatment in a hospital with intravenous (also called IV) fluids. IV fluids go through a needle into your vein. They help you stay hydrated and can give you nutrients that you usually get from food. If you continue to lose weight, you may need a feeding tube to make sure you’re getting enough nutrients for you and your baby.
You may need treatment in a hospital with intravenous (also called IV) fluids. IV fluids go through a needle into your vein. They help you stay hydrated and can give you nutrients that you usually get from food. If you continue to lose weight, you may need a feeding tube to make sure you’re getting enough nutrients for you and your baby.
What causes morning sickness?
We don’t know for sure what causes morning sickness. It may be caused by low blood sugar or increased pregnancy hormones. Morning sickness may be worse if you’re stressed or overly tired, if you eat certain foods or if you’re traveling (if you often have motion sickness).
Can you prevent or relieve morning sickness?
Yes. Here’s what you can do to help you feel better and even prevent morning sickness:
- Take a prenatal vitamin before you get pregnant. Talk to your health care provider about which one to take. Sometimes vitamins can upset your stomach, so take it with a snack.
- Keep snacks by your bed. Eat a few crackers before you get up in the morning to help settle your stomach.
- Eat 5 or 6 small meals each day instead of 3 larger meals.
- Eat foods that are low in fat and easy to digest, like cereal, rice and bananas. Don’t eat spicy or fatty foods.
- Eat healthy snacks between meals. This can help keep your stomach from being empty and helps prevent nausea. Try snacks that are high in protein, like milk or yogurt.
- Drink plenty of fluids, especially water.
- Avoid smells that upset your stomach.
You may have heard about these ways to prevent or relieve morning sickness. Talk to your provider before trying any of these:
- Acupressure and acustimulation (also called electrical nerve stimulation) wristbands. These involve putting pressure on or stimulating certain points of the body (called pressure points) to help prevent nausea.
- Acupuncture. This is a kind of treatment in which thin needles are put into your skin.
 If you’re thinking about acupuncture to help with morning sickness, tell your provider and find an acupuncturist who is trained to work with pregnant women.
If you’re thinking about acupuncture to help with morning sickness, tell your provider and find an acupuncturist who is trained to work with pregnant women. - Ginger. Ginger is an herb (plant) used in cooking and medicine. Ginger ale, tea or candies may help relieve morning sickness.
Even if it’s legal where you live for either personal or medical use, it’s not safe to use marijuana to treat morning sickness. No amount of marijuana has been proven safe to use during pregnancy. If you’re thinking of using marijuana to help with morning sickness, talk to your provider about other treatments that are safer for your baby.
Is there medical treatment for morning sickness?
Yes. If you can’t relieve morning sickness on your own or if you have severe nausea and vomiting of pregnancy, your provider may treat you with these medicines:
- Vitamin B6 and doxylamine. Your provider may treat you with these medicines separately or together.
 You can get vitamin B6 and doxylamine over-the-counter (OTC), which means you don’t need a prescription for them from your provider. Doxylamine is found in some OTC sleep aids (medicines that help you sleep). Or your provider may prescribe you a medicine that combines them.
You can get vitamin B6 and doxylamine over-the-counter (OTC), which means you don’t need a prescription for them from your provider. Doxylamine is found in some OTC sleep aids (medicines that help you sleep). Or your provider may prescribe you a medicine that combines them. - Antiemetic drugs. These are drugs that help prevent vomiting. If Vitamin B6 and doxylamine don’t work, your provider may prescribe an antiemetic drug for you. Not all are safe to use during pregnancy, so talk to your provider to make sure the medicine is a good choice for you.
Talk to your provider before you take any medicine during pregnancy, even medicine to help treat morning sickness.
When should you call your health care provider about morning sickness?
For most women, morning sickness is mild and goes away over time. But call your provider if:
- Your morning sickness continues into your 4th month of pregnancy.
- You lose more than 2 pounds.

- Your vomit is brown in color or has blood in it. If so, call your provider right away.
- You vomit more than 3 times a day and can’t keep food or fluids down.
- Your heart beats faster than usual.
- You’re tired or confused.
- You’re making much less urine than usual or no urine at all.
Last reviewed: September, 2020
Sore throat during pregnancy
What to do if the mother-to-be gets sick? Consider acceptable methods of treating a sore throat during pregnancy.
The appearance of pain in the throat, perspiration during the period of bearing a baby often causes a lot of unrest in expectant mothers. This is not at all surprising, because any infection suffered by a woman during pregnancy can adversely affect the development of the fetus in the womb. Why do sore throats occur during pregnancy? Consider the most likely reasons.
Causes of sore throat
The main cause of discomfort and sore throat during pregnancy is bacterial or viral flora on the mucous membrane of the nasopharynx or exacerbation of existing chronic diseases. Sometimes perspiration can be observed against the background of problems with the stomach, when the contents of the stomach are thrown into the oropharynx. Very rarely, the cause of pain when swallowing can be a foreign body.
Sometimes perspiration can be observed against the background of problems with the stomach, when the contents of the stomach are thrown into the oropharynx. Very rarely, the cause of pain when swallowing can be a foreign body.
If, in addition to sore throat, you also have an elevated body temperature and swelling of the mucous membrane of the pharynx, then most likely that you develop acute inflammatory process. This condition requires a woman to immediately consult a doctor, because many pathogenic microorganisms can freely penetrate the placental barrier, thereby causing developmental abnormalities in the baby. No need to try to treat a sore throat on your own at home, or even worse, ask for recommendations about treatment at the nearest pharmacy. Only the gynecologist leading the pregnancy can prescribe the drug that is most safe for the fetus in the womb, and, if necessary, refer to other specialists.
First aid for sore throat
During pregnancy, it is especially important not to start the disease and to eliminate all its clinical signs at the initial stage. So, if you feel a sore throat, not very pronounced pain when swallowing and discomfort while eating, but the body temperature remains within the normal range, then you can try alternative methods of treatment and local antiseptics.
So, if you feel a sore throat, not very pronounced pain when swallowing and discomfort while eating, but the body temperature remains within the normal range, then you can try alternative methods of treatment and local antiseptics.
Excellent help at the initial stage of a sore throat inhalation with the addition of a decoction of sage or chamomile. These medicinal plants have a pronounced anti-inflammatory and antibacterial effect and do not cause any side effects on the fetus growing in the womb.
Raspberries, cranberries and lingonberries are natural antibiotics. For sore throats, warm raspberry tea or freshly prepared lingonberry and cranberry juice helps well. Perfectly relieve pain, perspiration and swelling of the mucous membrane of the pharynx, gargling with infusions of medicinal plants (oak bark, chamomile, sage).
In addition to the traditional treatment of sore throats during pregnancy, try to avoid eating too hot or cold food and liquids. Compliance with a certain temperature regime is necessary so as not to additionally injure the inflamed mucous membrane of the pharynx. As a rule, if treatment with folk remedies was started immediately, then the mucous membrane of the pharynx is restored after 2-3 days.
Folk remedies
Milk with honey
For sore throat accompanied by difficulty in swallowing, warm milk with honey is very helpful. It is better to drink such a drink before going to bed and immediately cover yourself with a warm blanket. Until the morning, the pain in the throat will be almost imperceptible. In addition, warm milk with honey has a calming effect on the nervous system and helps the expectant mother fall asleep quickly.
Chamomile
Chamomile is a very effective folk remedy for the first symptoms of pharyngitis, tonsillitis. This plant has strong anti-inflammatory and antibacterial properties. To prepare herbal infusion, add 1 tablespoon of chamomile flowers to 1 liter of hot water. Put this mixture in a water bath and boil for 15 minutes, then strain and pour into a thermos. Use a warm infusion for gargling. Sage grass and oak bark have similar properties.
Prevention of viral infections during pregnancy
To prevent diseases during pregnancy, it is often recommended to spend time outdoors, eat healthy and healthy, and avoid crowded places. In the apartment, ventilate the room more often, maintain the optimum temperature regime - 22 degrees, air humidity in the room - 70-80%. Daily wet cleaning.
To prevent vitamin C deficiency during pregnancy, you can drink rosehip broth, cranberry fruit drinks. Thus, you not only maintain your immunity, but also strengthen blood vessels.
Essential oils are an excellent way to prevent many viral diseases. Only gynecologists do not recommend the use of aromatherapy in the first 12 weeks of pregnancy. Oils such as fir, eucalyptus, lemon, orange, grapefruit have a pronounced antiseptic effect. You can add 3-4 drops to a container of water and place near heating appliances or drip into an aroma lamp.
Consequences of a sore throat for an expectant mother
No matter how sad it may sound, in most cases we take our health very lightly. It is especially sad when pregnant women do not monitor their health. After all, they are responsible not only for themselves, but also for the baby growing in the stomach. When the first symptoms of the disease occur, including sore throat, the expectant mother should be aware of the possible consequences if treatment is not started in a timely manner. For example, bacterial throat infections left untreated during pregnancy can lead to threatened miscarriage or premature birth. It is unlikely that a sane expectant mother would risk the life of her baby like that simply because there was no time and desire to see a doctor.
Drug treatment of a sore throat during pregnancy
What to do if local antiseptics are ineffective or the woman has already started an inflammatory process? First of all, you should immediately consult a doctor, and not self-medicate at home. Delay can lead to the progression of the inflammatory process, which can result in severe tonsillitis. With the development of complications of inflammation of the pharynx, with streptococcal infection, antibiotics are often necessary, you should not worry about this, since antibiotics are always prescribed, which are allowed during pregnancy and cannot harm the health of the baby in the womb.
Antiseptics in the form of sprays or lozenges for resorption can reduce sore throat and relieve inflammation of the mucous membrane. They have proven absolute safety for pregnant women and the baby in the womb. What drugs, your gynecologist will advise you.
If white plaque or purulent plugs appear on the tonsils, do not wash the plaque or squeeze out the plugs on your own, you should immediately consult a doctor.
What can I take if I have a high temperature?
Pregnancy is a burden for a woman's body, there is a restructuring of many body systems, first of all, the immune system is suppressed. Due to a decrease in immunity in the future mother, viral infections and colds are often observed. For sore throats, as mentioned above, some medicinal plants, essential oils and antiseptic solutions help well. But what should a pregnant woman do if an increase in body temperature is added to the general symptoms of a viral infection? After all, many drugs can not be taken during the period of bearing a baby, so as not to expose the fetus to unjustified risk. So, consider what to do if the disease progresses.
So, consider what to do if the disease progresses.
First of all, if the pain in the throat is accompanied by increased body temperature, put aside all your affairs and call the consultation to call a doctor at home. Now you absolutely do not need to go to the clinic on your own, wait in line for an appointment and put your child at risk.
Drugs such as analgin, ibuprofen, coldrex, antigrippin, acetylsalicylic acid are categorically contraindicated during childbearing, regardless of the duration of pregnancy! Such drugs not only adversely affect the overall development of the fetus, but can also provoke uterine bleeding in the mother and impaired placental circulation.
Paracetamol is a relatively safe drug for reducing fever during pregnancy. It is allowed at any stage of pregnancy, but not more than 2000 mg per day. Paracetamol and its analogues not only reduce body temperature, but also relieve muscle aches, headaches and malaise.
However, it is very important not to bring down the body temperature if the thermometer does not exceed 38 degrees. It is with an increase in body temperature above this mark that the body begins to actively produce interferon, a substance that fights viruses and strengthens the immune system.
It is with an increase in body temperature above this mark that the body begins to actively produce interferon, a substance that fights viruses and strengthens the immune system.
A cold compress can be applied to the forehead to help reduce fever. This procedure helps to more easily endure elevated body temperature and relieves headaches a little. For such a compress, a gauze bandage is moistened in cold water, squeezed out and applied to the forehead. As the compress heats up, the gauze is moistened again. Instead of a moistened handkerchief, you can use an ice pack, but first you need to wrap it in several layers of fabric so as not to cause frostbite on the skin.
To reduce elevated body temperature, cold compresses can be applied to the main blood vessels (popliteal arteries, inguinal arteries, elbows).
If the body temperature of a pregnant woman does not exceed 37.5 degrees, it is highly recommended to drink hot linden tea. Linden has a diaphoretic effect and lowers body temperature.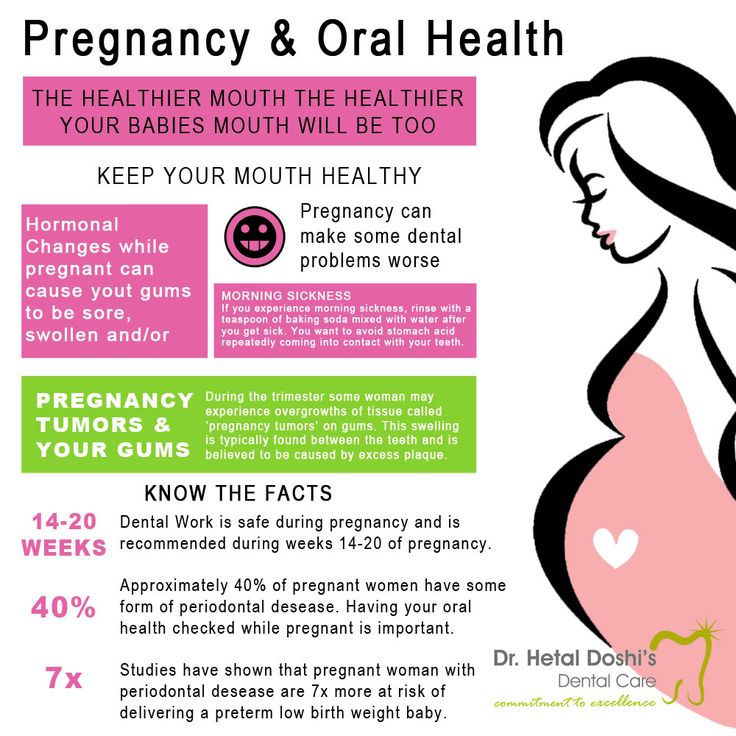 The main thing - do not forget about drinking plenty of water, this is 2.0-2.5 liters of fluid per day.
The main thing - do not forget about drinking plenty of water, this is 2.0-2.5 liters of fluid per day.
Remember that at the slightest symptoms of illness, it is best to see a doctor right away. After all, any viral infection, even without an increase in body temperature and severe ailments, transferred during pregnancy can end very badly for the woman herself and her baby growing in her stomach.
Make an appointment with a gynecologist
For more details, consult a qualified specialist at the Semeynaya clinic.
To clarify the prices for a gynecologist's appointment or other questions, follow the link below:
Pregnancy with epilepsy - GBUZ MO MONIIAG
Having healthy children is a natural desire of every woman. Many myths and prejudices prevent women with epilepsy from deciding to have a child, while many misconceptions have no basis. With the right approach to pregnancy planning and drug therapy, it is likely that a woman suffering from epilepsy will be able to give birth to a healthy child.
Epilepsy complicates approximately 0.3-0.5% of pregnancies. From 14 to 32% of these patients report an increase in the frequency of seizures during pregnancy. Pregnant women with ongoing or newly diagnosed seizures are at high risk and require close monitoring by a neurologist and an obstetrician-gynecologist.
There is also a risk of having a child with malformations due to the fact that most antiepileptic drugs (AEDs) have a negative effect on the fetus. This exposure is called a "teratogenic effect" and can cause birth defects in a child or developmental and learning disabilities as the child grows.
If a woman is not planning a pregnancy during treatment for epilepsy, it is recommended to use reliable contraception to avoid an unplanned pregnancy.
What are the actions of a woman with epilepsy who is planning a pregnancy?
BEFORE CONCEPTION, IT IS NECESSARY TO OBTAIN A CONSULTATION WITH AN EPILEPTOLOGIST
TO SOLVE THE FOLLOWING ISSUES
1. The need for anticonvulsant therapy.
The need for anticonvulsant therapy.
2. Determination of the minimum amount (ideally monotherapy) and the minimum effective dose of AEDs that do not cause seizures.
3. Taking slow-release AEDs or dividing the daily dose to reduce peak blood levels, which may reduce the risk of malformations in the child.
4. Start taking folic acid at a dosage of at least 1 mg per day.
TERATOGENIC EFFECT OF ANTIEPILEPTIC DRUGS
1. All AEDs are teratogenic, there is no consensus on which AED is the safest.
2. The risk of fetal abnormalities increases with the number and dosage of AEDs taken.
3. Anomalies in the development of the fetus, due to the use of AEDs, can occur only in the first weeks of pregnancy, when all systems and organs of the fetus are formed.
4. Changing AED therapy after the first trimester does not affect the risk of congenital malformations.
5. 95% of children born to mothers receiving AED treatment have no abnormalities!
I HAVE BEEN PREGNANT, WHAT'S NEXT?
1. Epilepsy is not a contraindication for pregnancy.
Epilepsy is not a contraindication for pregnancy.
2. Do not cancel PEP! Do not change the dosage of PEP yourself! Do not replace AEDs that have resulted in remission of epilepsy - taking AEDs during pregnancy is vital, as many factors increase the risk of recurrence of even well-controlled seizures before pregnancy. The most common provocateurs of seizures during pregnancy are skipping AEDs, emotional stress and sleep disturbances!!!
3. It is necessary to register for pregnancy for timely prenatal screening, get advice from an epileptologist.
4. Treatment of obstetric complications is carried out according to clinical guidelines.
5. Epilepsy is not a contraindication for natural childbirth, and labor management and pain relief are consistent with generally accepted standards. In most cases, prolonged epidural analgesia can be used.
6. Epilepsy is not an indication for caesarean section, even if there are several seizures during pregnancy!!! Indications for cesarean section are an increase in epileptic seizures, convulsive seizures more than once a week in the 3rd trimester of pregnancy, serial or status epilepsy, and a seizure during childbirth.
POSTPARTUM AND BREASTFEEDING
1. Continue taking AED!!! There is a risk of epilepsy decompensation in the postpartum period!!!
2. In case of drowsiness, double vision and involuntary movement in the eyes, ataxia, an urgent study of the concentration of AED in the blood is necessary. If the dosage of the drug was increased during pregnancy, then it is advisable to return to the daily dose used before pregnancy.
3. Breastfeeding a newborn is not contraindicated! An exception should be made for phenobarbital and lamotrigine. The mechanisms of their excretion from the body of the newborn are not formed, which can lead to the accumulation of the drug.
4. Take AED after feeding!
5. The most common complication in newborns is skin manifestations in the form of allergic reactions. The use of phenobarbital during pregnancy can lead to both sedative manifestations (drowsiness, poor sucking, muscle weakness, lethargy, lethargy) and withdrawal syndrome (motor agitation, restless sleep, frequent unreasonable crying), if for any reason breastfeeding milk stops.