Why is my baby foaming at the mouth
Why Your Baby Foams at Mouth and How to Deal with It
It is always a cause of worry when you wake up at night and found your baby foaming at the mouth. In such situation the baby is not able to cry and breathe and appears distressed and trapped. It is an alarming scenario, which must have been experienced by many parents. Let’s get some insight into why your baby may foam at the mouth during sleep and other aspects of the situation.
Why Does My Baby Foam at the Mouth?
A lot of causes exist for this. It may be just that the baby is asleep and foam at their mouth saliva and air. But at other times breathing of the baby may appear to be constrained or fully blocked. In such cases, you should not panic. Incline your baby or prop them up. Many things can be done to ease their breathing depending on their current condition.
Following is a list of causes which can be used as reference, but it should not replace the advice of the doctor of your child.
1. Overfeeding
During each feeding, a newborn baby can consume only one or two fluid oz of milk. When you overfeed you will find your baby foaming at the mouth to expel the excess milk. Babies also swallow saliva while sleeping, and the saliva bubbles expel from the mouth of the baby and form foam.
You cannot measure overfeeding while breastfeeding, but check the time. For newborn babies, limit breastfeeding to 10 minutes on each breast. If your baby is not full or contented, you can repeat the feeding after a gap of 15 minutes. Make sure to feed them slowly.
In case you bottle feed your baby, choose the correct bottle. If the hole of nipple is very big, the flow of milk will be very fast and your baby may not be able to cope with it. More air will enter stomach than milk, which will result in gas formation and also foaming at mouth.
2. Failure to Burp Well
It is necessary to burp babies. When they are not burped well after feeding, it results in spitting of milk and baby foaming during sleep.
You can make your baby burp in a number of ways. The most common and popular among them is to make your baby face you and let their body lean onto you. Their head must lie in line of your shoulder and their stomach must press directly in your chest. You should massage their back and induce a burp.
You may also place the baby on their belly, the gas may expel due to the pressure on the stomach. Or moving their legs up and down in the bicycle movements may also induce a burp.
3. Amniotic Fluid
Sometimes, amniotic fluid may remain in the stomach of infants (newborn). They expel it by spitting it through their mouths. This situation generally clears by second or third post partum day. Keep calm and observe your baby after birth.
4. Reflux
In case your baby has acid reflux, they may spit more milk than babies normally do. Due to reflux the milk they ingest comes back and due to this you will found your baby foaming at the mouth.
You should make your baby sleep on their side as sleeping on back raises the possibility of reflux. It also increases the risk of your baby getting choked with milk.
You can also make your baby sleep on an incline bassinet or bed to prevent foaming at the mouth. This posture will also reduce the reflux of stomach acid into the mouth of the baby. You can also gently rub the chest of the baby to soothe them if your baby is in distress.
5. Infection
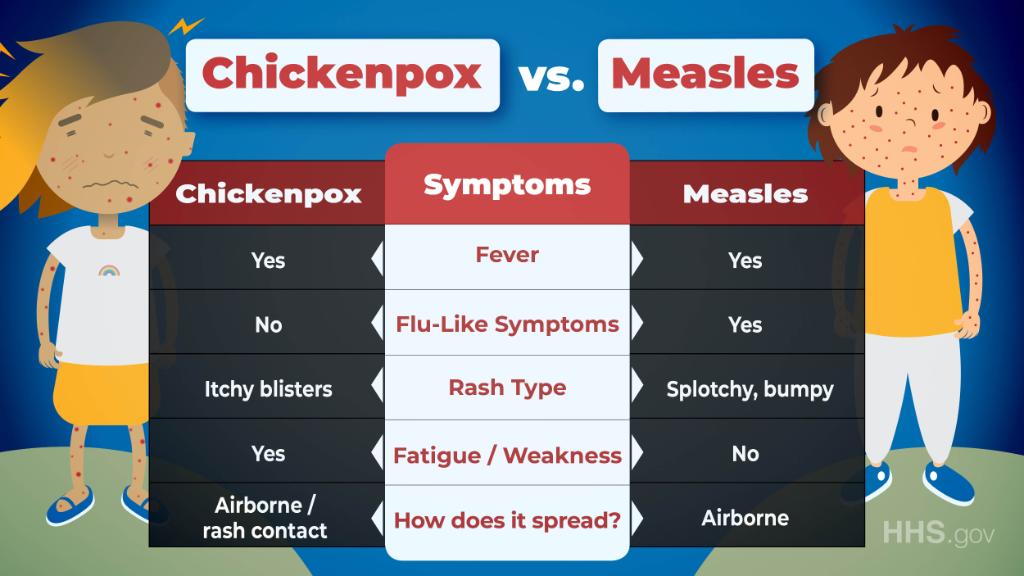
Infections such as bronchiolitis and pneumonia may also produce symptoms of foaming at mouth during sleep in babies. The baby may appear fussy, sick and the temperature may be raised. They may have difficulty breathing. In such cases, contact your physician immediately.
When to Worry About Baby Foaming at the Mouth
A content and peaceful baby who is foaming at mouth during sleep should not be a cause for worry. However, following are the factors when you should seek immediate medical advice:
- If your baby is choking, crying, in distress or having other signs or symptoms of illness including listlessness and fever, then you should contact a physician.
 These can indicate a negative reaction to any food or any infection or other condition including gastrointestinal disorder.
These can indicate a negative reaction to any food or any infection or other condition including gastrointestinal disorder. - If your baby has got vaccines on that day, then it may be due to a reaction to any of the shots. You can call the physician for medical advice regarding the reactions to vaccines.
- If you have introduced a new food to your baby, then they may develop foaming at mouth due to intolerance to that food. Eliminate that food from your baby’s diet for few months. You should seek advice of a physician if there are other symptoms.
- If your baby is not gaining sufficient weight or has lost weight, then you should seek medical advice to address the problem. Your kid may be suffering from reflux to such an extent that they are not receiving enough nutrition.
- If the foam at the mouth is green, yellow, purple, red or black in color, then this may indicate infection or other serious illness. You should see your physician immediately.
- If your baby is having difficulty in breathing or their color is becoming blue, then you should contact emergency medical service immediately.

How to Help with Baby Foaming
You should keep calm as this is very normal and happens to many babies for reasons ranging from trivial to medium to rarely severe.
The reasons for which you should be concerned occur in association with other symptoms; hence, you should keep a watch for these symptoms and consult your physician in case you have any concern.
- If the symptom of foaming at mouth is due to improper digestion of food, then the condition will disappear gradually as the digestive system of your baby grows and improves.
- You may help your baby by feeding them small quantity of food at short intervals, giving them assistance and lots of time to burp and keeping them upright whenever it is possible. You can also pop them on their belly to help expel the intestinal gas.
- Do baby massage to help encourage your baby’s digestive system to move the food down and expel the air upwards and out. You can learn burping techniques, chest massage and back massage.
 Massage can also help to soothe and calm your baby and may also help to make an excellent bonding time between you and your baby.
Massage can also help to soothe and calm your baby and may also help to make an excellent bonding time between you and your baby.
Reflux | Pregnancy Birth and Baby
Reflux | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Reflux is when your child brings the contents of their stomach back up into their food pipe or mouth. They may bring up small amounts of milk along with air when they are burped. Reflux, also called spitting up, posseting or regurgitation, is very common in newborns.
The medical term for reflux is gastro-oesophageal reflux, or GOR. If GOR is more serious or has complications it may lead to gastro-oesophageal reflux disease or GORD.
Reflux occurs because a muscle at the top of the stomach, called the sphincter, is loose. It can also be caused by air bubbles in the stomach or by eating too much food too quickly.
It can also be caused by air bubbles in the stomach or by eating too much food too quickly.
Spitting up may not cause discomfort and your baby may seem not notice.
Reflux is not the same as vomiting. Vomiting is forceful, is usually more than a tablespoon or 2, and upsets the baby. Vomiting can be a sign of illness.
Reflux is not the same as drooling and blowing bubbles, which is especially common once babies start teething.
Spitting up often peaks by 4 months of age and by 7 months many babies no longer do it, although for some it takes longer.
Tips for managing reflux
Here are some things you can do to minimise your baby’s reflux:
- Make each feed calm and relaxed.
- Hold your baby in an upright position, not lying down, while you feed them. Keep your baby upright for 30 minutes after feeding. An infant seat or car seat works well.
- Feed your baby smaller amounts at a time.
- Feed your baby without delay. If the baby has cried for a long time before a feed, they may have swallowed air.
 Spitting up is more likely if the baby has air in the stomach at the beginning of a feed.
Spitting up is more likely if the baby has air in the stomach at the beginning of a feed. - Check the size of the opening in the teat if you are bottle feeding. The bottle should leak several drops of milk per second. A hole that is too big will let the baby swallow formula too quickly and baby is likely to spit up the excess. A hole that is too small forces the baby to suck very hard and swallow air.
- Burp your baby several times during each feed. It works best to support the infant's head and burp them sitting on your lap. Burping your baby over your shoulder may put too much pressure on their stomach.
- If you are supervising your baby, you can place them on their tummy for an hour or so after the feed. Take care not to let baby sleep on their tummy because of the link with sudden unexpected death in infancy. Always place your baby on their back to sleep.
- Make sure nappies are not too tight and do not put pressure on the baby's stomach.
When to see the doctor about reflux
If your baby is otherwise healthy and happy and they are just bringing up milk, nothing needs to be done. Talk to your doctor or child health nurse if:
Talk to your doctor or child health nurse if:
- you have any other concerns
- your baby is not gaining weight
- there is a change in bowel movements or urination
- your baby shows signs of discomfort or pain.
Reflux and lactose intolerance - video
Video provided by Raising Children Network.
Sources:
Raising Children Network (Gastro-oesophageal reflux and GORD), Reflux Infant Support Association (Management tips - reflux), Sydney Children's Hospitals Network (Reflux)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2021
Back To Top
Related pages
- Vomiting in babies
- Vomiting in children
Need more information?
Gastro-oesophageal reflux & GORD: babies | Raising Children Network
Gastro-oesophageal reflux is when your child brings stomach contents back up into his foodpipe or mouth. GORD is when reflux leads to complications.
GORD is when reflux leads to complications.
Read more on raisingchildren.net.au website
What is Reflux? - Reflux Infants Support Association Inc
What is Gastro-Oesophageal Reflux? 'Reflux' means to flow back; ‘gastro’ relates to the stomach;‘oesophageal’ relates to the oesophagus (food pipe).
Read more on Reflux Infants Support Association website
Kids reflux - the facts and the stats - Reflux Infants Support Association Inc
Presents a selection of interesting facts and statistics about paediatric reflux
Read more on Reflux Infants Support Association website
Reflux | Sydney Children's Hospitals Network
What is reflux? Gastro-oesophageal reflux (GOR) happens when stomach contents are brought back up into the oesophagus (the food pipe leading from the mouth to the stomach)
Read more on Sydney Children's Hospitals Network website
What is Silent Reflux? - Reflux Infants Support Association Inc
Caring for a baby or child who suffers from gastro-oesophageal reflux can be extremely stressful and you may find yourself on an emotional rollercoaster ride. You may not realise your experience and emotions can be perfectly normal for your situation but this is where the Reflux Infants Support Association (RISA) Inc can help.
You may not realise your experience and emotions can be perfectly normal for your situation but this is where the Reflux Infants Support Association (RISA) Inc can help.
Read more on Reflux Infants Support Association website
How Reflux presents - Reflux Infants Support Association Inc
Caring for a baby or child who suffers from gastro-oesophageal reflux can be extremely stressful and you may find yourself on an emotional rollercoaster ride. You may not realise your experience and emotions can be perfectly normal for your situation but this is where the Reflux Infants Support Association (RISA) Inc can help.
Read more on Reflux Infants Support Association website
Reflux Reality: A Guide for Families - Reflux Infants Support Association Inc
Caring for a baby or child who suffers from gastro-oesophageal reflux can be extremely stressful and you may find yourself on an emotional rollercoaster ride. You may not realise your experience and emotions can be perfectly normal for your situation but this is where the Reflux Infants Support Association (RISA) Inc can help.
You may not realise your experience and emotions can be perfectly normal for your situation but this is where the Reflux Infants Support Association (RISA) Inc can help.
Read more on Reflux Infants Support Association website
Baby food reactions, allergies and reflux | Raising Children Network
Most babies spit up some breastmilk or formula. This is often called reflux. Sometimes this can be a sign of food reactions or food allergies or intolerance.
Read more on raisingchildren.net.au website
My Baby Has Reflux | Red Nose Australia
Read more on Red Nose website
Reflux: Sleeping Position for Babies with Gastro-Oesophageal Reflux (GOR) | Red Nose Australia
Read more on Red Nose website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Epilepsy in children
Epilepsy is a chronic disease of the central nervous system that occurs due to excessive electrical activity in the brain and is expressed in convulsive and non-convulsive seizures, loss of consciousness, impaired sensory, motor, mental functions of the body and other manifestations epileptic seizure.
Epilepsy is most common in childhood and its manifestations and causes differ significantly from those in adults. For example, not all convulsions and seizures in children are associated with epilepsy and need to be treated with antiepileptic drugs. Often epilepsy is accompanied by other diseases and pathologies associated with hereditary diseases in children, metabolic disorders, chromosomal, neurological diseases, etc.
Causes of epilepsy in children:
- complicated pregnancy, hypoxia, birth trauma, etc.;
- intrauterine infections of the nervous system, brain;
- the presence of epilepsy in parents or close relatives;
- viral infectious diseases (encephalitis, meningitis, etc.), colds accompanied by very high fever;
- chromosomal diseases;
- tumors, cysts of the brain;
- brain injury.
The most common types of epilepsy in children are primary and secondary form of the disease.
- The primary form of epilepsy may occur spontaneously in a child, regardless of provoking factors, and until the causes of such attacks are clearly established in medicine;
- Secondary epilepsy in children may occur due to brain injury, infections, tumors, etc.
First of all, parents should notice alarming symptoms and manifestations of the disease in a child.
Main symptoms of epilepsy in children:
- short-term loss of consciousness;
- high temperature;
- convulsions lasting 1 to 20 minutes;
- temporary cessation of breathing;
- severe muscle tension;
- bluing of the skin;
- foam at the mouth.
If your child has these signs, you should contact a pediatric specialist who will make an accurate diagnosis and prescribe treatment. Some forms of epilepsy, despite the frightening symptoms and manifestations, are successfully treated, and the sooner the disease is detected, the more likely it is that the disease will pass without leaving serious consequences. With many types of epilepsy, the child can attend regular preschool and school facilities and lead a normal life with some restrictions on sports activities.
With many types of epilepsy, the child can attend regular preschool and school facilities and lead a normal life with some restrictions on sports activities.
In addition to the typical form of epilepsy, children can be diagnosed with absence epilepsy (minor epilepsy), which is not always noticeable to others. Most often, it occurs at the age of 5-7 years, mainly in girls and is expressed in a sudden fading of the child, a temporary lack of reaction to actions around, a gaze at one point. At the same time, convulsions and fainting are not observed, but when the child comes to himself, he does not remember what happened. Absence epilepsy may resolve by adolescence, but may develop into other forms of the disease.
Diagnosis of epilepsy in a child can be made by a child psychiatrist or neurologist by general symptoms, as well as by EEG, MRI , CT , allowing to determine the form and type of epilepsy. After confirming the diagnosis, the pediatric specialist will prescribe treatment and give recommendations to parents on caring for and assisting the child during seizures.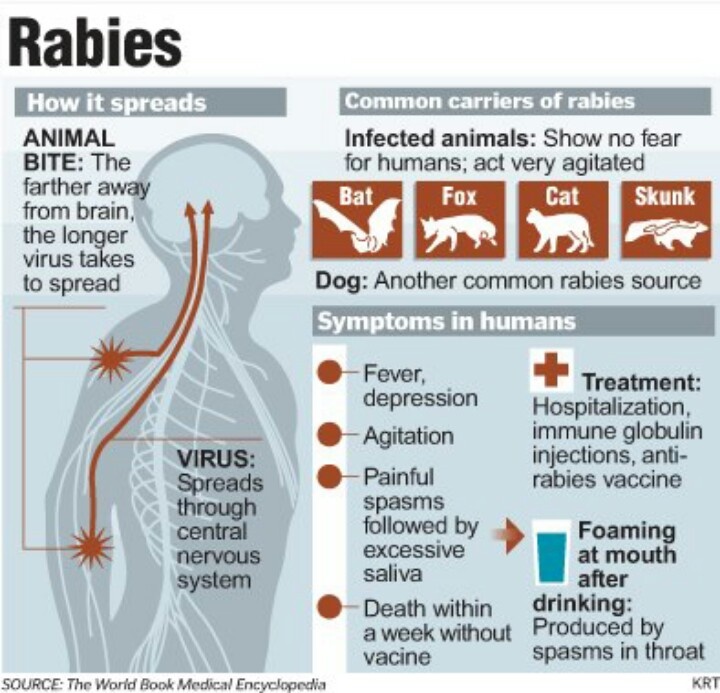
Treatment of epilepsy in children, as a rule, is carried out with medication, neurosurgical and psychotherapeutic methods, depending on the age of the child, his individual characteristics, the form and severity of epilepsy.
At the Medical Center "Medicentr" in the Department of Pediatrics, qualified child psychiatrists and neurologists receive appointments with many years of experience working with children of all ages and in their practice they encounter the most difficult cases and severe mental and neurological diseases in children.
Our clinics in St. Petersburg
Structural subdivision
Polikarpova
Alley Polikarpova 6k2
Primorsky district
- Pionerskaya
- Specific
- Komendantskiy
Structural subdivision
Zhukov
Prospekt Marshala Zhukov 28k2
Kirovsky district
- Avtovo
- Veterans Avenue
- Leninsky Prospekt
Structural subdivision
Devyatkino
Okhtinskaya alley 18
Vsevolozhsk district
- Devyatkino
- Civil Avenue
- Academic
You can get detailed information and make an appointment by calling +7 (812) 640-55-25
Make an appointment
Respiratory distress syndrome of newborns - description, signs, treatment, prevention and diagnosis Respiratory distress syndrome of newborns (respiratory disorder syndrome) is non-infectious pathological processes (primary atelectasis, hyaline membrane disease, edematous hemorrhagic syndrome) that form in the prenatal and early neonatal periods of a child's development and manifest as respiratory failure.
 The incidence of respiratory distress depends on the degree of prematurity and averages 60% in children born at a gestational age of less than 28 weeks, 15-20% - at a period of 32-36 weeks and 5% - at a period of 37 weeks or more. With rational nursing of such children, mortality approaches 10%.
The incidence of respiratory distress depends on the degree of prematurity and averages 60% in children born at a gestational age of less than 28 weeks, 15-20% - at a period of 32-36 weeks and 5% - at a period of 37 weeks or more. With rational nursing of such children, mortality approaches 10%. Features
Most children are born in a state of asphyxia and congenital hypoxia, but respiratory disorders may not appear immediately, but several hours after birth. Typical are pronounced signs of respiratory failure: shortness of breath with a respiratory rate of 60 or more per minute (often with aperiodic breathing), cyanosis (perioral, acrocyanosis, generalized), pallor of the skin, participation in the act of breathing of auxiliary muscles (tension of the wings of the nose, retraction compliant places of the chest - intercostal spaces, xiphoid process of the sternum, retraction of the supraclavicular fossae), chest rigidity, sometimes foam at the mouth, difficult "grunting" breath (glottis spasm), swelling of the cheeks. There is a decrease in motor activity, hyporeflexia, muscle hypotension. For early detection and assessment of the severity of respiratory disorders in newborns, the Silverman scale is used. The assessment is made in dynamics every 6 hours for 2-3 days.
There is a decrease in motor activity, hyporeflexia, muscle hypotension. For early detection and assessment of the severity of respiratory disorders in newborns, the Silverman scale is used. The assessment is made in dynamics every 6 hours for 2-3 days.
As the disease progresses, respiratory disorders and symptoms of depression of the nervous system increase, cyanosis intensifies, apnea, grunting exhalation and paradoxical breathing appear (when exhaling, the anterior lower chest is retracted and the abdomen protrudes), diffuse crepitus. Often there are local and generalized edema; frothy, sometimes bloody discharge from the mouth. The cardiovascular system is affected, tachycardia, muffled heart sounds are observed, fetal communications with the right-hand shunt persist, signs of pulmonary hypertension increase, cardio- and hepatomegaly develops.
Description
It develops mainly in premature babies from mothers with a burdened obstetric history (cardiovascular disease, diabetes mellitus, nephropathy, placental pathology, uterine bleeding). Intrauterine hypoxia, asphyxia and hypercapnia during childbirth are important in the presence of lung tissue immaturity. Under the influence of hypoxia and hypercapnia, a violation of the pulmonary circulation occurs, the interalveolar septa are impregnated with serous fluid with the release of plasma components, in particular fibrin, into the lumen of the alveoli. The formation of hyaline membranes is also possible as a result of a decrease in the fibrinolytic activity of the blood. There is also a lack or a sharp decrease in the activity of the anti-atelectatic factor (surfactant), which contributes to the occurrence of atelectasis. Of certain importance is the deficiency of plasminogen, alpha2-macroglobulin and the development of local or disseminated intravascular coagulation. Underdevelopment of the elastic tissue of the lung, immaturity of the alveoli, aspiration of amniotic fluid and mucus are noted, especially in very premature babies.
Intrauterine hypoxia, asphyxia and hypercapnia during childbirth are important in the presence of lung tissue immaturity. Under the influence of hypoxia and hypercapnia, a violation of the pulmonary circulation occurs, the interalveolar septa are impregnated with serous fluid with the release of plasma components, in particular fibrin, into the lumen of the alveoli. The formation of hyaline membranes is also possible as a result of a decrease in the fibrinolytic activity of the blood. There is also a lack or a sharp decrease in the activity of the anti-atelectatic factor (surfactant), which contributes to the occurrence of atelectasis. Of certain importance is the deficiency of plasminogen, alpha2-macroglobulin and the development of local or disseminated intravascular coagulation. Underdevelopment of the elastic tissue of the lung, immaturity of the alveoli, aspiration of amniotic fluid and mucus are noted, especially in very premature babies.
Diagnostics
The diagnosis of respiratory distress is based on clinical findings. It can be predicted based on the study of the content of lecithin or thromboplastic activity of amniotic fluid.
It can be predicted based on the study of the content of lecithin or thromboplastic activity of amniotic fluid.
If the ratio of levels of sphingomiapine - lecithin in the amniotic fluid is more than 2.0, then the probability of developing respiratory distress is 2%, if less than 2.0-50%, if less than 1.0-100%. A simple lung maturity test, the Clements "foamy test" with gastric contents obtained by probing, can also be used.
Differential diagnosis is carried out with pneumonia, malformations of the lungs and heart, intracranial birth trauma, diaphragmatic hernia.
Treatment
First of all, it is the prevention of cooling (the latter reduces or stops the synthesis of surfactant). Immediately after birth, the child is wrapped and placed under a radiant heat source, and then in an incubator. Carry out activities to revitalize and restore breathing. Antiacidotic therapy gives good results. The main indication for correction with sodium bicarbonate is the general serious condition of the child (less than 6 points according to Apgar) and the development of decompensated acidosis (pH<7. 3). The sodium bicarbonate solution is re-introduced in the next 2-3 days until the indicators of the acid-base state are normalized (pH 7.35-7.4). The introduction of vitamins, cardiac drugs, aminophylline, etc. is widely used.
3). The sodium bicarbonate solution is re-introduced in the next 2-3 days until the indicators of the acid-base state are normalized (pH 7.35-7.4). The introduction of vitamins, cardiac drugs, aminophylline, etc. is widely used.
Infusion therapy should be carried out slowly in a small volume at a rate of 3-5 drops per 1 minute. The composition of the injected liquid is determined by the goal: delivery of calories to the body, reduction of catabolism and the degree of acidosis, improvement of water-salt metabolism, prevention of hypo- or hyperkalemia and hyperaminoacidemia. With shock and blood loss, blood transfusions are indicated. A constant inhalation of a 30% oxygen-air mixture is required.
The use of oxygen-helium mixtures is effective. Care is of great importance: rest, keeping in a couveuse. The start time of feeding is determined individually, taking into account the functional state of the child and the degree of prematurity. In severe cases, especially in violation of the coordination of swallowing, sucking and breathing, tube feeding is prescribed.