Burning vagina while pregnant
Answers to 6 burning questions about yeast infection during pregnancy | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
September 20, 2022
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
Vaginal candidiasis, also known as a yeast infection, can be a real pain. The itching, burning, and discharge can be especially worrisome during pregnancy.
In most cases, though, vaginal yeast infections and most treatment options pose minimal risk to the patient or pregnancy.
After bacterial vaginal infections, yeast infections are the second most common cause of vaginal inflammation, and 75% of women will have at least one in their lifetime. Common symptoms can include redness, itching, or irritation on the external genital area (vulva), an increase in white or tan vaginal discharge, and a burning sensation during urination or intercourse.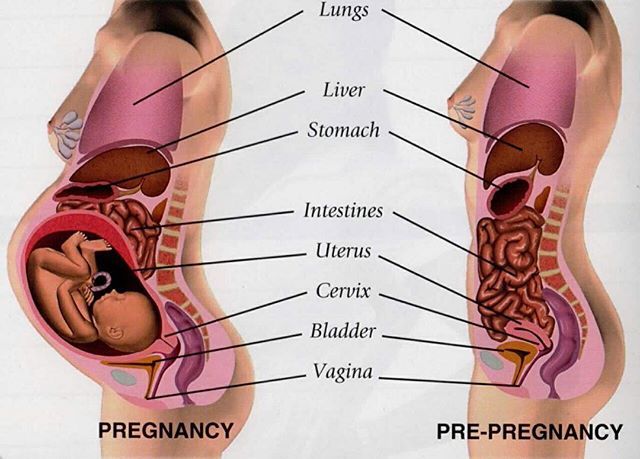
There are a range of over-the-counter and prescription treatments, and an Ob/Gyn or gynecologist can help you choose the safest, most effective option during pregnancy.
I’ve invited Meredith McClure, M.D., a UT Southwestern gynecologist, to answer the top questions pregnant and breastfeeding patients ask about yeast infection treatment and prevention.
Meredith McClure, M.D.Q: How common are yeast infections during pregnancy?
A: Studies have found that 20%-30% of women develop a yeast infection during pregnancy. An increase in the hormone estrogen creates a more hospitable climate for yeast to colonize the vagina because it binds to the protein factor H on the surface of the cells that cause vulvovaginal candidiasis.
Some women are more likely to develop yeast infections due to their genetics. Mutations of several genes can interfere with the immune system’s ability to defend against candida yeast, resulting in recurring infections for some people. This inherited predisposition is called familial candidiasis.
This inherited predisposition is called familial candidiasis.
Q: Can a yeast infection harm my pregnancy?
A: No. A yeast infection won’t affect your developing baby – that’s why we don’t treat yeast infections that don’t have symptoms. However, most symptomatic yeast infections get worse when left untreated. This means more itching, redness, and inflammation. If the skin becomes cracked or torn from repeated scratching, a skin infection can result. In rare cases, an untreated yeast infection can lead to fatigue, oral thrush, or digestive problems.
Q: Do yeast infections appear throughout pregnancy?
A: Yeast infections can occur any time, but they are most common during the second trimester. Talk with your doctor if you notice signs of a yeast infection while pregnant, even if you have had one before. Some more serious infections have similar symptoms, so your doctor will perform a simple fungal culture swap in the office to check for the presence of yeast.
Q: What treatment options are available?
Talk with your doctor about the safest and most effective options for treating yeast infections during pregnancy.A: Topical creams or vaginal suppositories are the recommended yeast infection treatment options during pregnancy or while breastfeeding. Over-the-counter medications such as Miconazole, Clotrimazole, and Terconazole have been shown to eliminate a yeast infection safely and effectively. They are usually applied for three to seven days. It is important to finish the entire course of medication to prevent the infection from coming back. Studies have demonstrated these medications are safe to use during pregnancy.
The oral medication Diflucan (fluconazole) is not recommended for most patients during pregnancy. Though taking a single pill is simpler, quicker, and less messy, some studies suggest fluconazole carries a slightly increased risk of miscarriage, birth defects, or stillbirth, especially at high doses taken over long periods of time.
While the increase is small – approximately 12 incidents per 10,000 births – the convenience of single-pill treatment might not outweigh the risk. However, in the event you have already taken or need to take fluconazole while pregnant, the additional risk at a normal dose is unlikely to pose any problems for your baby.
Q: Are yeast infection treatments safe while breastfeeding?
A: Yeast infections are less common among breastfeeding patients because estrogen levels drop dramatically in the postpartum period, making it hard for yeast to thrive. But if they occur, fluconazole may be taken by women who are breastfeeding as the levels secreted into breast milk are small.
It is possible for a breastfeeding mother and baby to pass thrush, a fungal infection that typically grows in the mouth and throat, back and forth between nipple and mouth. If that happens, both must be treated to stop the infection. Thrush is usually minor and is often caused by the same fungus – and treated with a 7- to 14-day course of the same antifungal medicines – as a yeast infection in the vagina.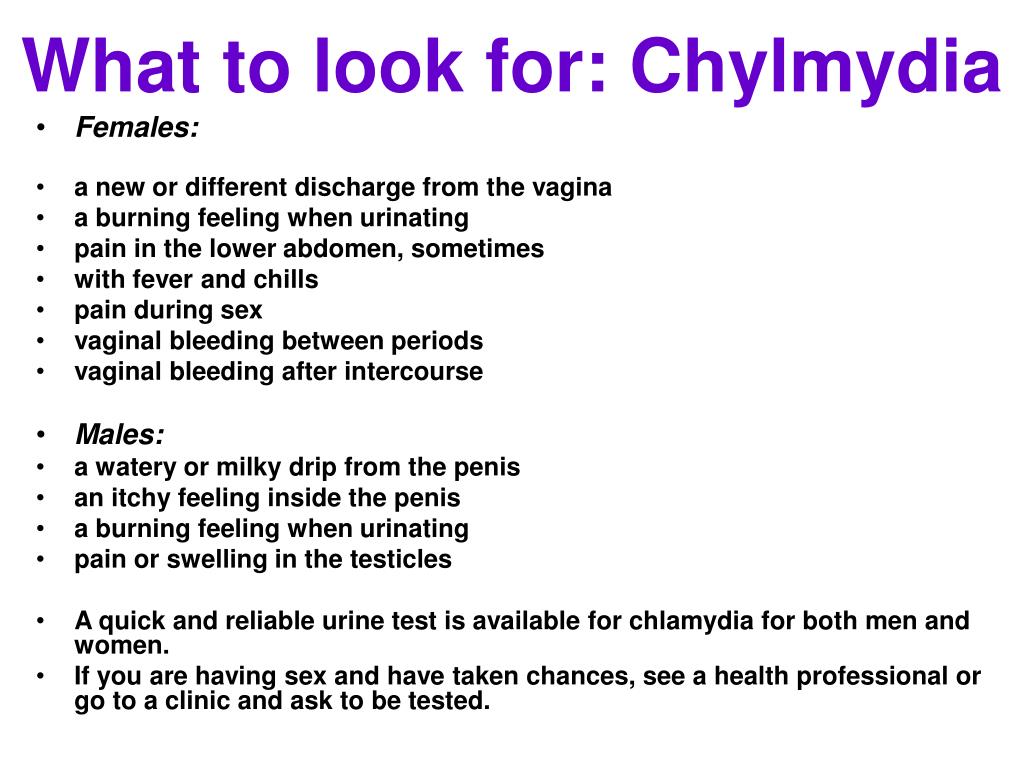
Q: What steps can reduce the risk of yeast infection?
A: During pregnancy and otherwise, take the following precautions:
- Wipe front to back after using the toilet.
- Avoid using scented tampons, pads, and pantyliners.
- Change tampons, pads, and pantyliners often.
- Avoid very hot baths and hot tubs.
- Wear underwear with a cotton lining to promote airflow.
- Do not douche, which removes healthy vaginal bacteria that prevent infection.
- Wear loose fitting clothing.
- Manage your blood sugar if you have diabetes or gestational diabetes.
- Remove wet workout clothes and swimsuits as soon as possible after activities.
If you’re pregnant and notice signs of a yeast infection, discuss treatment options with your doctor so you can eliminate these disruptive symptoms. To request an appointment, call 214-645-8300 or request online.
More in: Your Pregnancy Matters
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
February 14, 2023
Your Pregnancy Matters
- Melissa Mauskar, M.D.
February 7, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
January 31, 2023
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D. - Kyler Elwell Silver, M.D.
January 24, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
January 10, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
December 20, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
December 13, 2022
Pediatrics; Your Pregnancy Matters
- Jessica Morse, M.
 D.
D.
December 6, 2022
Your Pregnancy Matters
- Shivani Patel, M.D.
November 22, 2022
More Articles
Vaginal Burning: Causes, Relief, Pregnancy
Vagina burning like you’re in an inferno? No your pants aren’t on fire, but something is causing your bits to burn. Ummm… so should you be worried about this vaginal burning?
The occasional itch or irritation in your lower region is completely common and generally nothing to worry about. But, if persistent burning, itching, or irritation start to become your norm, something may be up.
But, if persistent burning, itching, or irritation start to become your norm, something may be up.
Burning can creep up anywhere in your vaginal area, including your:
- vaginal opening
- labia
- clitoris
Here’s why you may be feeling the burn and what to do about it.
Some of the products you use on the daily might be working against you with chemicals that can irritate your vag. This can cause burning, itching, stinging, rawness, or even pain.
You may notice symptoms right away after switching to a new product, or it may take a few uses.
Products that can cause irritation include:
- scented soaps
- detergents
- bubble baths
- menstrual pads
- scented toilet papers
What to do about it? The best way to remedy this is to stop using the products and avoid using other scented or perfumed products on your nether region.
If symptoms continue after you’ve stopped using these products, talk to your doctor to discover if something else is going on downtown.
Some products or substances that are made to be in or around your vagina can irritate your genitals and fuel that fiery feeling. This includes:
- tampons
- latex condoms
- sprays
- creams
- douches
- certain topical medications
- semen
- spermicides
What to do about it? If you have a product that you’ve just started using, stop using it to see if the burning goes away. Not sure which product that is? Try patch testing a small area to help identify the irritant.
If you discover that the culprit is your preferred method of contraception, like latex condoms, talk to your doctor. They can help you find an alternative that won’t impede on your sexy time fun.
Certain clothing can also cause burning and irritation down below, such as:
- tight underwear
- tights
- tight or fitted pants/shorts
The culprit is most likely chafing or extra moisture irritating your bits. While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
What to do about it? Avoid irritation by not wearing tight clothing too often or for too long of periods of time. Be careful with wet clothing, too. Sitting too long in a wet swimsuit can lead to bacteria growth in your vagina and infections.
Bacterial vaginosis (BV) happens when there’s too much of certain bacteria in your vagina, throwing off your hoo-ha’s normal balance. And a not-so-fun fact: It’s the most common vaginal infection for women ages 15 to 44, according to the Centers for Disease Control and Prevention (CDC).
In some cases, you may not experience any symptoms of BV. For those that do, however, symptoms can include:
- burning
- itching
- pain
- white or gray vaginal discharge
- a fish-like odor, especially after sex
What to do about it? BV may disappear on its own, but you’ll usually need to see your doctor for antibiotics to clear the infection up. It’s essential that you take every dose prescribed, even if you start feeling better.
It’s essential that you take every dose prescribed, even if you start feeling better.
Yeast infections have nothing to do with quarantine bread-making, and everything to do with what happens when there’s excessive yeast growth in the vagina. Along with burning, signs of a yeast infection may be:
- soreness
- red rash outside your vagina
- itching or swelling of the vagina or the vulva
- pain when you pee or during sex
- thick, white discharge (think cottage cheese)
Nearly 75 percent of women experiencing at least one yeast infection in their lifetime. And, while the risk of getting a yeast infection is already high, it’s even higher for women who:
- are pregnant
- have diabetes
- are now or were recently on antibiotics
- are using hormonal birth control
- have a compromised immune system
What to do about it? Yeast infections can often be treated at home or with an over-the-counter (OTC) antifungal medication such as a cream, ointment, or suppository.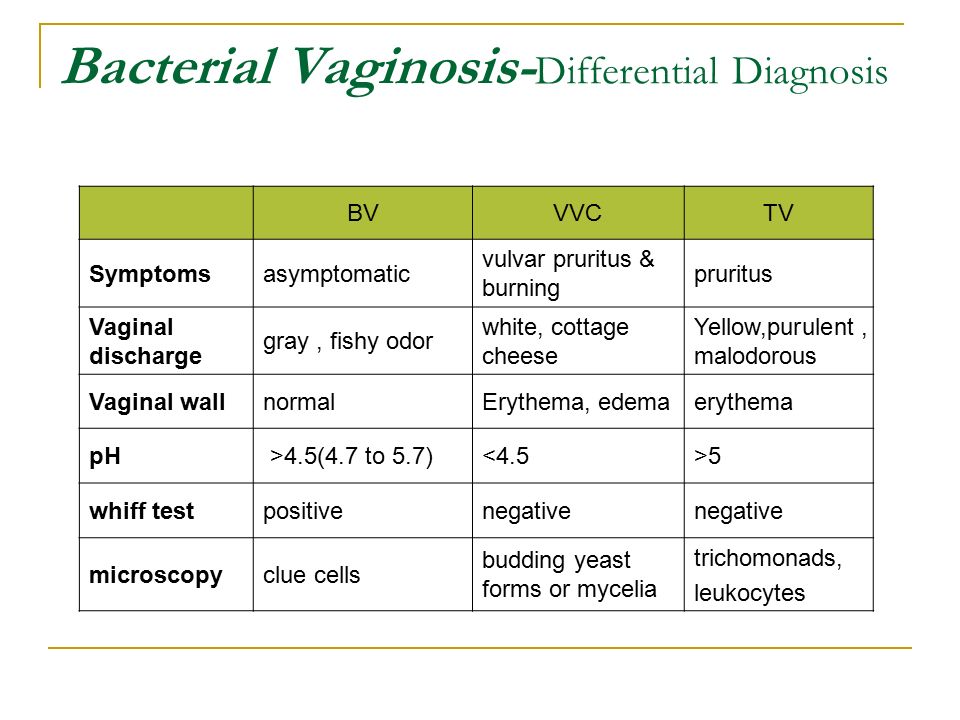
However, if you experience frequent yeast infections, your infection doesn’t clear up after treatment, or this is your first yeast infection ever, it’s best to see your doctor. They can confirm your diagnosis and help you determine the best treatment plan for you.
Urinary tract infections (aka UTIs) happen when bacteria gets in your urinary tract or bladder. You’ll likely experience a burning sensation when you pee, as well as other symptoms like:
- a frequent need to pee (often with little results)
- strong-smelling urine
- cloudy urine
- blood in your urine, making it red or pink
- fever or chills
- pain in the stomach, back, or pelvic area
What to do about it? Think you have a UTI? See your doctor. They’ll be able to prescribe you antibiotics to treat your infection.
Be sure to drink plenty of fluids and to take the full course of medication, even if symptoms have disappeared. If you don’t, you risk the infection returning.
Trichomoniasis (aka trich) is an STI, and one of the most common ones in the U.S. to boot. It appears more often in women than men. Symptoms only appear in about 30 percent of cases, so most women don’t even realize they have the infection.
Those that that do experience symptoms will likely have:
- vaginal burning, irritation, and/or itching
- clear, white, yellow, or green discharge
- lower abdominal pain
- foul odors down below
- discomfort while peeing or during sex
What to do about it? You’ll need to see your doctor, as prescription antibiotics are needed to clear up the infection. Typically, only a single dose will do the trick to treat your trich. Left untreated, however, trich can cause long-term complications, as well as increase your risk of getting other STIs.
Gonorrhea is another STI where bacteria infects mucous membranes like the cervix, uterus, or fallopian tubes. It’s most common in those ages 15 to 24 and rarely causes symptoms.
When symptoms do appear, they include:
- vaginal burning or irritation
- unusual discharge
- bleeding or spotting between periods
- burning or pain when urinating
What to do about it? Gonorrhea is treated with prescription antibiotics, so a trip to the doc is necessary. In some cases, a doctor may prescribe dual therapy, where two different meds will need to be taken at the same time.
Gonorrhea can lead to serious complications if it’s left untreated, including infertility and pelvic inflammatory disease (PID).
Chlamydia is another common STI caused by bacteria. It’s often known as a “silent” infection because, much like trich, about 70 percent of those with the infection don’t experience symptoms.
Those that do exhibit symptoms will likely experience:
- burning sensations
- abnormal discharge
- bleeding between periods or during sex
- pain during urination or sex
What to do about it? Prescription antibiotics are needed to cure chlamydia, so a trip to the doctor is necessary.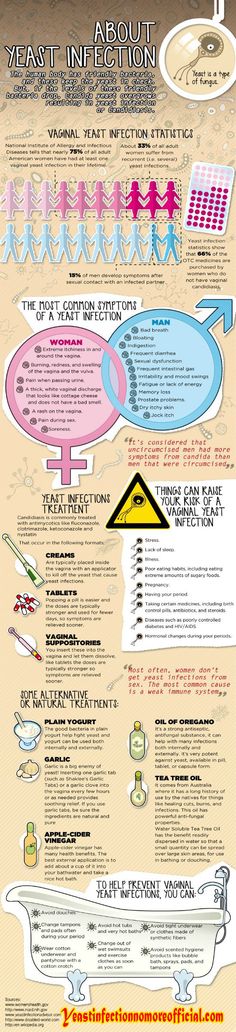 Health professionals are also required to report chlamydia cases in order to track the infection.
Health professionals are also required to report chlamydia cases in order to track the infection.
If left untreated, chlamydia can wreak havoc on your reproductive system, and cause permanent damage. Repeat infection is also common with chlamydia, and each time you contract the infection can increase your chances of having issues with fertility.
Genital herpes is an incurable viral infection that’s caused by skin-to-skin contact with someone who has the herpes simplex virus (HSV). According to the CDC, an estimated 1 in 6 people in the U.S. between ages 14 to 49 has genital herpes.
Symptoms may not develop right away — in fact, it could be years before the virus becomes active and symptoms appear. When symptoms do appear, they’ll likely include:
- burning, itching, or tingling sensation in the vagina
- painful sores, blisters, or ulcers
- swollen glands
- vaginal pain, especially during urination
- flu-like symptoms
- abnormal vaginal discharge
What to do about it? The herpes virus stays in your body forever; there is no cure. However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
Your doctor about can also prescribe medication to help reduce the risk of transferring genital herpes to others.
The most common STI in the U.S. is human papillomavirus, more commonly known as HPV. HPV can cause genital warts, which can appear:
- on your vulva, vagina, cervix, or anus
- in clusters or as one or two bumps
- as white or flesh-colored bumps
What to do about it? While genital warts may disappear on their own, there’s no cure for them. You can choose to have them medically removed, which can lower your risk of transmitting the infection to others. HPV is also linked to different cancers, including anal cancer and cervical cancer.
Did you get the HPV vaccine?
To reduce the risk of HPV-related diseases and infections, the CDC, American Academy of Family Physicians, and other health experts recommend that preteens receive an HPV vaccination before becoming sexually active.
A rare skin condition, lichen sclerosus causes thin, white patches to appear on the vagina — especially around the vulva. These patches can lead to permanent scarring.
Other symptoms include:
- itching or burning
- pain or discomfort
- redness
- bleeding
- blisters or sores
- painful sex
Women can develop lichen sclerosis at any age, but it’s most common in postmenopausal women.
What to do about it? To treat lichen sclerosus, you’ll need to see your doctor, who can prescribe a strong topical steroid to ease symptoms. You’ll also want to regularly see your doctor to monitor any changes in the skin or permanent complications, like scarring, or thinning of the skin.
Wait, aren’t you a little young to be worried about menopause? Premature menopause is when you go through menopause before age 40. It isn’t very common and only affects about 1 percent of women (and a lot of times it’s genetic).
During menopause your estrogen and progesterone levels get super low, and you’ll stop having a menstrual cycle. This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
Menopause can also cause symptoms like:
- hot flashes
- irritability
- insomnia
- fatigue
- reduced sex drive
- night sweats
What to do about it? Menopause can’t be stopped, but it’s symptoms can be eased. One thing your doc may do is prescribe an estrogen supplement or other hormone therapy. If hormonal supplements aren’t your cup of tea, your doctor can work with you to find the best option for you.
If sex conjures up images of burning naughty bits rather than burning passion, you’re not alone. It’s not uncommon to experience a burning sensation after and during sex.
This can generally be attributed to:
- too much friction
- not enough lubricant being used
- allergic reaction to semen
- allergic reaction to products being used (like latex condoms, toys, or scented lotions)
- PH imbalance caused by douching
- hormonal birth controls
- UTIs, STIs, or other infections
How to find relief
Working in some extra lube or some additional foreplay to make matters more slippery can help you avoid that burning feeling in the future.
However, if sex continues to cause pain or other symptoms arise, it’s time to see the doctor. They can help figure out what’s going on and help you determine treatment or next steps.
Vaginal irritation is normal during pregnancy, and you’ll likely experience it more than once. This can be caused by a variety of reasons, including:
- increase in vaginal discharge
- vaginal dryness
- sensitivity to products
- hormonal changes
- UTIs or other bacterial infections
How to find relief
In many cases, it’s nothing to worry about, and you can ease your itch right at home by:
- taking a cool bath or using a cool compress
- using product elimination to determine the cause
- taking a bath with baking soda
Because pregnancy is a delicate time and you’re experiencing many physical changes, it’s always best to talk to your doctor if you have questions or something seems out of sorts.
If you think your symptoms are caused by an infection of any kind, talk to your doctor before taking any medications, including common OTC treatments. They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
Occasional itching or irritation on your vagina is normal, and there generally isn’t cause for concern. However, if you begin to experience persistent burning, increased irritation, or other symptoms that are out of the norm, there may be an underlying condition at play.
Talk to your doctor if you think something’s up (or even if you don’t… better safe than sorry!). In some cases, a simple prescription medication will make your condition disappear while others will require lifelong treatment or monitoring.
Your doctor can help identify what’s setting your bits to be on fire and help you find relief.
Itching and burning in the intimate area during pregnancy: vagina during pregnancy
ANGELINI Expecting a baby is one of the most wonderful times in a woman's life. Her thoughts are focused on dreams about the future of the baby and joyful chores about children's things, strollers, toys. But changes in the body sometimes prepare the expectant mother for unpleasant surprises. So, many women feel dryness, itching and burning in the intimate area during pregnancy. What are they caused by?
But changes in the body sometimes prepare the expectant mother for unpleasant surprises. So, many women feel dryness, itching and burning in the intimate area during pregnancy. What are they caused by?
Why there is itching and burning in the intimate area during pregnancy
While waiting for the baby, the woman's hormonal background is completely rebuilt, as a result, the vaginal microflora also changes, which leads to the appearance of pathogenic bacteria and fungi that cause discomfort. If this is added to the wearing of synthetic underwear, the use of sanitary pads with fragrances, too hot weather, then unpleasant symptoms such as dryness, burning and itching in the intimate area during pregnancy may appear. Many women are willing to sacrifice good health for the health of the baby. Fearing to take medication, they endure discomfort until the very birth. However, itching, pain and burning during pregnancy make the expectant mother to be in a state of constant stress, which only increases the discomfort. If you feel discomfort in the intimate area, consult a doctor who will tell you what caused it and help you choose the right treatment.
If you feel discomfort in the intimate area, consult a doctor who will tell you what caused it and help you choose the right treatment.
What diseases of the intimate zone can occur during pregnancy? The cause may be one of the infections:
- thrush. Proliferation of yeast fungi on the mucous membrane of the intimate zone leads to its appearance. The infection can be transmitted to the child during childbirth, affecting the mucous membranes of the mouth and genitals;
- bacterial vaginosis. Caused by pathogenic bacteria and manifests itself in the form of gray discharge with an unpleasant odor;
- urinary tract infections . Hostile microorganisms during urination from the intimate area penetrate into the urinary organs. Cutting and burning are the first signs of this condition. This does not harm the baby, but it can lead to inflammation of the kidneys, which is dangerous for the expectant mother.
If you consult a doctor in time and undergo the necessary treatment, you can avoid dangerous complications.
Intimate hygiene tips for expectant mothers
Burning and itching in the intimate area during pregnancy can be prevented. Here are 6 simple tips to help reduce your risk of developing infections:
- Do not shower more than twice a day. Water and soap remove natural defenses - beneficial microbes.
- Choose intimate hygiene gels containing lactic acid or plant extracts: linden, chamomile, blue lotus, white tea. These natural ingredients have a positive effect on the condition of the most delicate area of our body.
- Dry your body thoroughly after using a cotton towel. Do not share towels with other family members.
- Wear panties made of 100% cotton, which help the skin to breathe and do not create a "greenhouse effect", especially in hot weather.
- Use pads filled with cotton extract. They pass oxygen well, which destroys yeast fungi.
- Replace the bath with a shower. Hot soapy water can bring dirt into the body and washes away beneficial bacteria.
 If you really want to soak in the bath, first wash yourself in the shower. Use sea salt instead of foam.
If you really want to soak in the bath, first wash yourself in the shower. Use sea salt instead of foam.
Tantum® Rose for intimate comfort during pregnancy
To relieve pain, itching and burning during pregnancy, you can use a douche solution or powder to prepare a Tantum® Rose solution. The drug works already 20 minutes after the first application of 1 . It affects only the pathogenic microflora 2 and also helps the body fight inflammation on its own. Tantum® Rose is approved for douching by pregnant women and new mothers during breastfeeding 3 .
The material was prepared on the basis of the following sources:
https://mytinysecrets.com/expecting-and-the-unexpected-vaginal-infections-during-pregnancy/
https://www.carefreearabia.com/en/understand-your-body/how-to-cleanse-your-vagina-intimate-hygiene-during-pregnancy
http://www.onlymyhealth.com/remedies-vaginal-itching-during-pregnancy-1340226504
https://www. parents.com/pregnancy/my-body/aches-pains/pregnancy-vaginal-discharge-infections/
parents.com/pregnancy/my-body/aches-pains/pregnancy-vaginal-discharge-infections/
Access - August 2017
Back to article list
Tantum® Rose preparations:
- Relieve pain, itching and burning from the 20th minute after application 1
- Help restore microflora 2
- Helps fight inflammation 3
- No restrictions during pregnancy and lactation 3
- Suitable for women of all ages 3
Tantum® Rose Solution Powder Tantum® Rose
Candles for thrush
February 6, 2023
Vaginal suppositories from thrush are used for candidiasis - damage to the vaginal mucosa by yeast-like fungi of the genus Candida. ...
Find out more
Curdled discharge from women
January 30, 2023
Vaginal discharge is a physiological secret produced by the female genital organs. These secretions perform a number of functions aimed at maintaining the health of women ...
These secretions perform a number of functions aimed at maintaining the health of women ...
Find out more
why does it occur and how to solve the problem?
Pregnancy is one of the important and responsible stages in a woman's life. In most cases, this is 9 months of anxious waiting to meet your baby. However, during pregnancy, a woman's body undergoes major hormonal changes and pleasant emotions can go hand in hand with painful and uncomfortable sensations in different areas of the body. Including unpleasant symptoms may appear in the intimate area.
Discomfort in the vagina often manifests itself in the form of itching, burning, irritation and swelling. The main thing, when these symptoms appear, is to understand that it is necessary to establish their cause and eliminate it as soon as possible, because there are risks of harming the health of the fetus.
Various sexual infections can affect the appearance of discomfort in the perineum.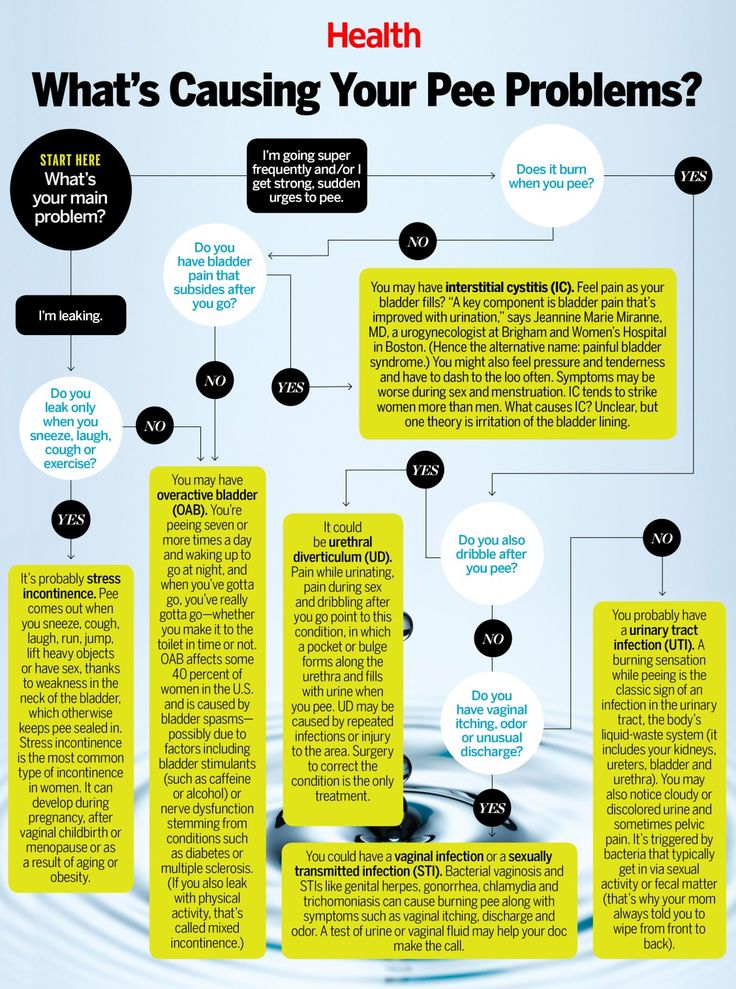 Unfortunately, during pregnancy, a woman is prone to various infectious diseases. As mentioned above, bearing a baby causes a restructuring of the hormonal background in a woman's body: the level of the hormone progesterone rises and the activity of the immune system naturally decreases, which creates favorable conditions for the exacerbation of chronic infections and the emergence of new ones.
Unfortunately, during pregnancy, a woman is prone to various infectious diseases. As mentioned above, bearing a baby causes a restructuring of the hormonal background in a woman's body: the level of the hormone progesterone rises and the activity of the immune system naturally decreases, which creates favorable conditions for the exacerbation of chronic infections and the emergence of new ones.
How dangerous is the development of infectious diseases of the vagina and vulva during the bearing of a baby? Normally, during pregnancy, the amniotic bladder and water, as well as the mucous plug of the cervix, protect the fetus from various infections and bacteria, so your unborn baby is safe.
The presence in the body of a woman in an interesting position of an infectious disease and the lack of necessary therapy can adversely affect the course of pregnancy. For example, an untreated infection can lead to damage to the membranes, the fluid in which the unborn child is located, and the fetus itself.
There is also a high probability of physical contact of the child with the infection during passage through the birth canal. Therefore, in case of any discomfort in the intimate area during pregnancy, you should consult a specialist.
You can suspect the appearance of an infection of the vagina and vulva by a series of symptoms: cramps, itching, burning. Often, sexual infections provoke colpitis - inflammation of the mucous membrane of the vagina and the vaginal part of the cervix. By itself, colpitis often causes discomfort in the groin of pregnant women. It can be provoked not only by sexual infections, but also by endocrine or chronic diseases, stress, lack of hygiene.
Bacterial vaginosis can also cause discomfort. This pathology, caused by a decrease in the number of lactobacilli in the vagina, as a result, their place is taken by other microorganisms that are always present in the vagina, but in excess lead to the development of dysbiosis. Bacterial vaginosis can occur without symptoms, but sometimes it occurs with clinical manifestations. It is usually accompanied by discomfort, as well as vaginal discharge that is white, gray, or yellow-green in color with an unpleasant "fishy" odor.
Bacterial vaginosis can occur without symptoms, but sometimes it occurs with clinical manifestations. It is usually accompanied by discomfort, as well as vaginal discharge that is white, gray, or yellow-green in color with an unpleasant "fishy" odor.
Bacterial vaginosis also adversely affects the course of pregnancy, can provoke inflammation of the pelvic organs, premature birth, chorioamnionitis - inflammation of the amniotic membranes and infection of the amniotic fluid.
Itching in the intimate area during pregnancy can appear with vulvovaginal candidiasis - infection of the mucous membranes of the vulva and vagina with yeast-like fungi of the genus Candida. It should be noted that the first episode of the incidence of vulvovaginal candidiasis is observed during pregnancy. This is due to changes in hormonal levels, reduced immunity. This disease, in addition to discomfort in the groin area, itching and burning, is characterized by: moderate hyperemia, white and thick discharge like cottage cheese, sour smell from the vagina, pain during sexual intercourse and urination.
However, itching and burning are not always symptoms of serious pathologies. Occasionally, discomfort can occur with the use of poorly fitting underwear or aggressive pH soaps.
Feeling discomfort in the groin, you should consult with a specialist. The specialist can conduct an examination, collect an anamnesis and prescribe, if necessary, laboratory and / or other diagnostic tests. All this will help to establish a diagnosis and choose an individual treatment regimen.
In order to prevent the appearance of discomfort in the intimate area and not spoil the pleasant waiting time for the addition, it is necessary to follow preventive recommendations.
- It is necessary to carry out external hygiene of the intimate area. Normally 2 times a day - no more and no less. Frequent washing can lead to “overdrying” of the skin and mucous membranes of the intimate area, and a lack of hygiene can lead to the development of various inflammations.
 You should not self-douche or vaginal lavage unless recommended by a specialist in your particular case.
You should not self-douche or vaginal lavage unless recommended by a specialist in your particular case. - Choose a quality cleanser. Ideally, this should be a hypoallergenic product that is dermatologically tested, contains lactic acid and components that care for the skin of the genital organs. Epigen Intim Gel is ideal for daily hygiene of the inguinal zone during pregnancy and after childbirth. Epigen Intim gel contains activated glycyrrhizic and lactic acids in its composition. Its pH is slightly acidic, which corresponds to the normal acid-base balance of the skin of the intimate area. The tool helps to eliminate discomfort (irritation) due to wearing panty liners or not very comfortable underwear. It has a very pleasant aroma and helps to neutralize unpleasant odors in the intimate area with constant use.
- Abandon synthetic underwear in favor of natural fabrics. Cotton panties do not create a "greenhouse effect", especially in the heat.
Treatment of discomfort in the intimate area will be different. The diagnosed disease will influence the choice of therapy. Spray Epigen Intim can be included in the complex treatment of diseases accompanied by discomfort - nonspecific colpitis (vaginitis), bacterial vaginosis, thrush, herpes.
The diagnosed disease will influence the choice of therapy. Spray Epigen Intim can be included in the complex treatment of diseases accompanied by discomfort - nonspecific colpitis (vaginitis), bacterial vaginosis, thrush, herpes.
Spray Epigen Intim
More
Buy
Epigen Intim Spray
The drug has antipruritic and anti-inflammatory action. Thanks to the active ingredient - activated glycyrrhizic acid, Epigen Intim spray helps to eliminate itching and irritation. It also helps to eliminate inflammation, swelling and redness of tissues. The drug is also able to increase the local immunity of the vagina, by stimulating the production of its own interferons. Spray Epigen Intim promotes healing and restoration of the integrity of the damaged mucosa, due to which the protective function of the mucosa will be restored and the number of lactobacilli will increase.
The drug is successfully used to treat viral infections (caused by the human papillomavirus, genital herpes), diseases associated with a decrease in local immunity (nonspecific vaginitis, thrush, bacterial vaginosis), etc. It can be used to treat exacerbations in conjunction with antiviral, antifungal and antimicrobial drugs, and for the prevention of these vaginal infections.
It can be used to treat exacerbations in conjunction with antiviral, antifungal and antimicrobial drugs, and for the prevention of these vaginal infections.
more
By the way, while carrying a baby, the use of many drugs sold in pharmacies is limited or prohibited.
But Epigen Intim spray is approved for use in pregnant and lactating women and is dispensed without a doctor's prescription. The drug is applied both externally and intravaginally, depending on the disease.
In the presence of itching, burning, irritation and swelling in the groin area, a woman feels as uncomfortable as possible. Intimate discomfort can bring especially many experiences to women during pregnancy. To minimize the risks of discomfort, try to follow the simple rules indicated in the article. When discomfort appears in the perineum, the most correct thing is to visit a specialist and not self-medicate, since now you are responsible not only for yourself, but also for the unborn baby.