Can babies produce sperm
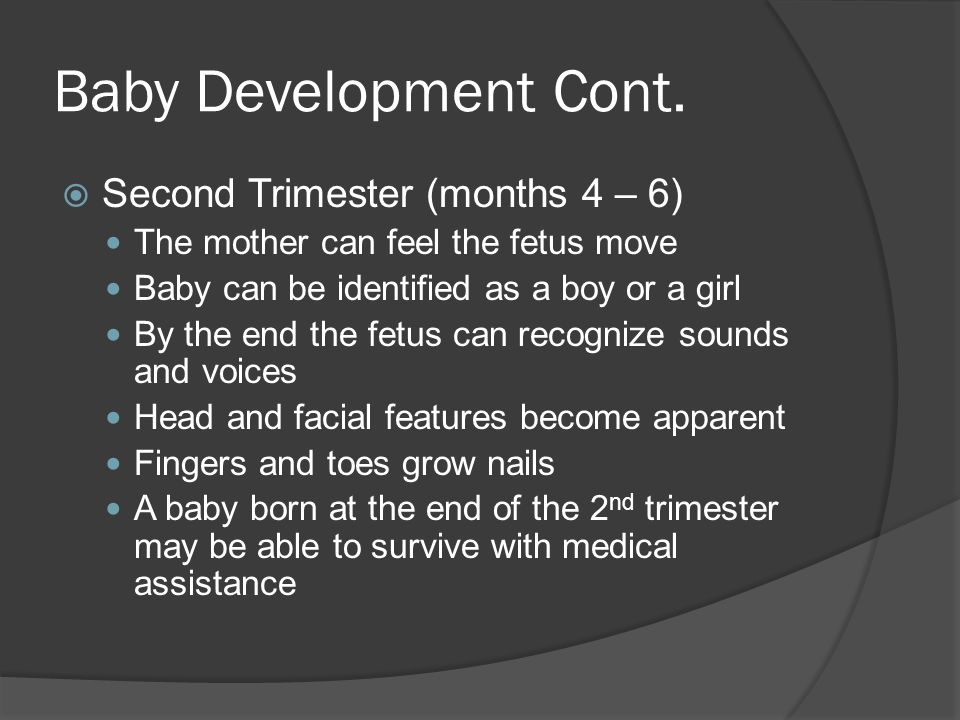
Fertility Throughout Life by Lexi Krock Fetus Male: By the tenth week of pregnancy, a fetus's gender is evident, and by week 14 sex organs have formed. Female: At 20 weeks, a female fetus has a fully developed reproductive system, replete with six to seven million eggs. Infant Male: Boys do not produce sperm until puberty, so a male infant's reproductive system is largely unchanged between the fetal stage and infancy. Female: At birth, a girl's pair of ovaries contain up to 1,000,000 follicles, which are hollow balls of cells, each with an immature egg (or ovum) in the center. A girl is born with all the eggs she will ever have. Adolescent Male: While women are only fertile during a few days in their menstrual cycles, men are constantly fertile from the onset of puberty (usually at 10 years of age) when a surge in testosterone triggers the production of an average of 200 million sperm each day. Female: During childhood, a girl's ovaries absorb almost half of the 1,000,000 immature eggs with which she was born. Of the 400,000 eggs present during her first menstrual period, only 300 to 500 of them will develop into mature eggs across her reproductive life span. Her body reabsorbs the rest before they complete development. Ovulation and menstruation start near the end of puberty, generally when a girl is about twelve-and-a-half, though any age from nine to 18 is normal. Each month during a woman's reproductive years, ten to 20 follicles begin maturing under the influence of hormones. These hormones, which are low during childhood and increase exponentially during the reproductive years, regulate the entire reproductive process. Two distinct cycles govern menstruation and ovulation, the uterine cycle (commonly called the menstrual cycle) and the ovarian cycle, which is responsible for ovulation. Hormones coordinate these two cycles, which last from 20 to 40 days each to prepare the lining of the uterus (endometrium) each month for a possible conception. Ovulation generally occurs about two weeks after the last day of a woman's menstrual period. A follicle discharges a single egg to the surface of the ovary, whence it is slowly carried down the fallopian tube and into the uterus. This process lasts about two days, after which conception is not possible. If the egg reaches the uterus without fertilization by a sperm, it will pass unnoticed out of the woman's body. If fertilization occurs, the egg will embed itself in the endometrium and begin its growth. Twenty-something Male: Both men and women are normally at their peak of fertility in their early to mid-20s. Female: Though girls menstruate throughout their teens, many women do not regularly ovulate until their mid-20s, when hormone levels become more regular and women begin to ovulate each month. Thirty-something Male: Male fertility in the 30s is much the same as in the 20s. Female: Though many women conceive and give birth to healthy babies into their 40s, conception becomes more difficult for women in their mid-to-late 30s and early 40s, and women over 35 are more likely to carry a baby with abnormalities. Middle-age Male: While women's fertility in middle age begins to decrease, men of the same age are still highly fertile. Female: Menstruation and ovulation continue until the age of 50, on average, but any time between 40 and the late 50s is a normal age to begin menopause. The body changes that occur between the reproductive and post-reproductive phases of a woman's life, most notably the end of monthly bleeding, are called the "climacteric" and often take place over as many as 15 years. During the gradual process of menopause, the ovaries stop maturing eggs and releasing large amounts of hormones. A woman is not considered to have completed menopause until she has passed one full year with no period. Old age Male: Men are capable of fathering healthy children throughout their lives. It is not uncommon, however, for older men to experience some sexual dysfunction. In addition, some studies have shown that children conceived by a father over the age of 50 have an increased risk for mental illness, particularly schizophrenia. Female: Post-menopausal women carry some eggs in their ovaries, but they are not viable and cannot be fertilized. Many women take hormones during and after menopause in order to ease the process of menopause and help prevent post-menopausal bone-density loss. However, hormone-replacement therapy does not maintain a woman's fertility into old age. Lexi Krock is editorial assistant of NOVA Online.
The 18 Ways (And Then Some) | On Human Cloning | Fertility Throughout Life | How Cells Divide Resources | Teacher's Guide | Transcript | Site Map | 18 Ways to Make a Baby Home Search | Site Map | Previously Featured | Schedule | Feedback | Teachers | Shop Join Us/E-Mail | About NOVA | Editor's Picks | Watch NOVAs online | To print PBS Online | NOVA Online | WGBH © | Updated October 2001 |
Age and Sperm: How Are They Related?
As you likely know, age is a critical factor for both men and women when it comes to conceiving a child. In fact, there are few more likely determinants of a couple’s chances of having a baby than their respective ages.
In fact, there are few more likely determinants of a couple’s chances of having a baby than their respective ages.
For women, the primary age-based factors determining the likelihood of conception are egg count and egg quality, which correlate to the number of healthy eggs available to be fertilized. These factors diminish over time, meaning for the majority of women that their biological fertility clock often starts to tick more quickly in their 30s and eventually expires in their 40s.
For men, the biological clock still ticks, but it relies on different factors: sperm count, sperm motility and sperm structure. While the vast majority of men produce several million fresh sperm each day (even past 80 years old), their fertility still decreases over time. This change is typically gradual, but it sometimes sneaks up on older men hoping to start a family.
To help you understand how these biological changes can affect men of all ages, let’s break down the lifecycle of sperm, what makes for healthy sperm and the factors that control the efficacy of sperm:
At What Age Do Boys Start Producing Sperm?
During puberty, men (on average) start producing sperm between the ages of 12 and 15 years old, according to studies from the National Institute of Health.
Where the average male falls within this range depends on several factors, such as when they began puberty and how quickly they move through each stage of the adult male maturation process.
At What Age Do Men Stop Producing Sperm?
This question has an easy, while (potentially) misleading, answer:
The vast majority of men never stop producing sperm, but sperm count and sperm motility decrease dramatically for males as they reach the latter stages of life, particularly after the age of 70.
This overall reduction in the prevalence and quality of remaining sperm translates into increasingly lower fertility rates for men into their 50s and beyond.
What Is A Healthy Sperm Count?
If you’re reading this article, you’re likely wondering how your current (or future) sperm count will affect your likelihood of conception.
To make this admittedly complicated topic a little simpler, we have created the following charts to help you understand healthy and unhealthy sperm counts:
| Healthy Sperm Count: 15-200 million sperm per milliliter |
| Unhealthy Sperm Count: under 15 million sperm per milliliter |
Another method for measuring healthy sperm count, sometimes used by male fertility experts, is counting sperm per ejaculate:
| Healthy Sperm Count per Ejaculate: over 39 million |
| Unhealthy Sperm Count per Ejaculate: under 39 million |
How Does Sperm Affect Fertility?
As widely reported, many modern couples choose to have children later than previous generations -- often for lifestyle reasons.
This widespread societal shift leads many men to wonder if they will still have enough healthy sperm if they wait to conceive a child until their 30s, 40s or beyond. In addition to consulting medical professionals and dedicated support resources like Modamily, many men seek a clear explanation of how their sperm diminishes as they age.
The simple answer is this: average sperm count and quality do diminish over time, but science shows more men than ever are fertile past the age of 30. In fact, the average age of fatherhood in the United States has risen to the age of 31.4, according to research from Stanford University.
Still, the correlation between age and diminishing sperm very much exists, so here’s what you need to know about the three primary factors affecting your fertility:
Sperm Count
As mentioned before, a healthy sperm count is 15-200 million, with a peak in the average male’s 20s and 30s followed by as much as a 50% decrease in their 40s and 50s, according to studies from the National Institute of Health.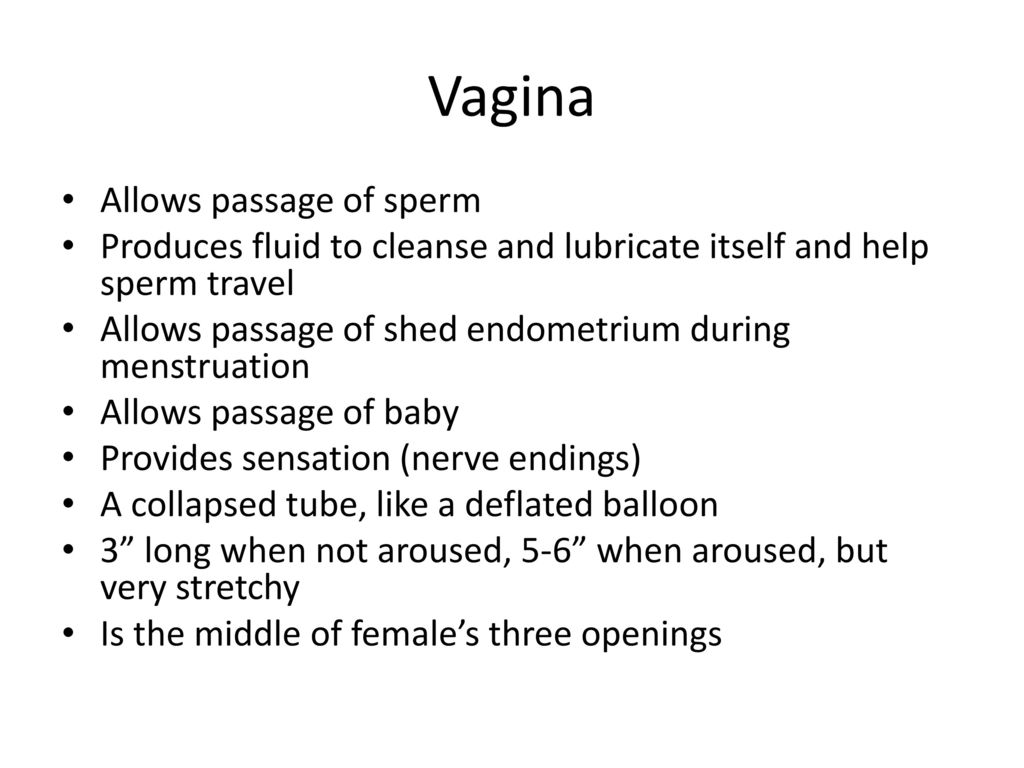
While figures aren’t precise on the average sperm count by age (based on per milliliter or ejaculate measurements), the general scientific consensus is that after their 50s, men have a much more difficult time maintaining higher sperm counts.
Sperm Motility
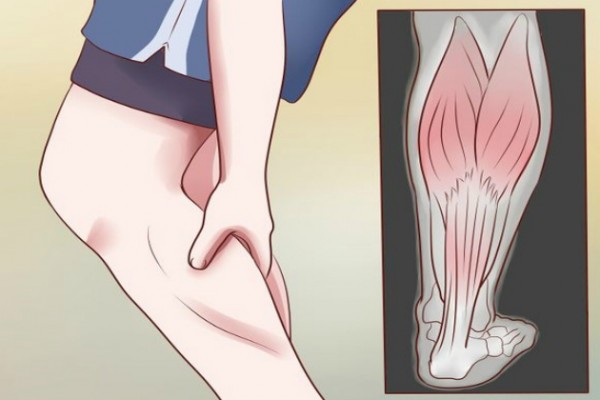
Sperm motility is the ability of sperm to move at the required speed necessary to reach and fertilize an egg and is also affected by age.
While sperm count can remain stable (or rarer, increase) over time, science is pretty firm on the fact that sperm motility almost universally diminishes over time.
Unlike sperm count, however, multiple studies recorded by the National Institute of Health document evidence of exactly how much motility decreases over time: around .17-.6% per year, leading to a decrease of 3-12% on average a period of two decades.
The same studies presume a link between this decline with age and a reduction in the function of glands like the epididymis and the prostate, famous issues of health concern for aging men.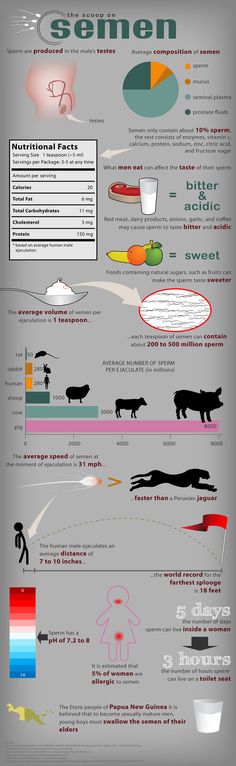
Sperm Structure
The final, primary way sperm can affect male fertility is sperm structure.
Proper sperm structure is critically important to conception because it gives sperm the ability to effectively dissolve the outer shell of the female egg, which is vital for fertilization.
Just like motility, it is generally accepted that the quality of a man’s sperm structure decreases with age. According to N.I.H. studies, this reduction ranges between a .2-.9% decrease per year, leading to a 4-18% decrease in structural quality (aka morphology) over a two-decade period.
Modamily
At Modamily, we are dedicated to helping you start the family of your dreams. Our team of experts is excited and ready to help you begin the life you’ve always wanted, and the journey can begin sooner than you might think.
You don’t need to put your dream of starting a family on hold. You can start the conception and family planning process RIGHT NOW and begin developing that trust and rapport that every type of parenting partnership needs to successfully raise children together.
If you’re interested in more about sperm, planning for birth and starting a family in general, be sure to check out our blog with weekly topics for you! Here are some articles to start with:
- Writing a Birth Plan
- How To Keep Your Sperm Healthy
- How a Baby Changes Your Life
- Starting A Family As A Co-Parent: A Guide
Schedule your free consultation today!
How the male reproductive system works
Unlike women, in men, most of the reproductive system is outside and located outside the pelvic cavity. There is a funny theory according to which the male genital organs perform the same function as the antlers of deer, the magnificent tails of peacocks, the fangs of lions and tigers. In primates, the genitals serve to demonstrate physical strength and superiority over other males.
Apparently, this is why many men feel so strongly if they experience problems in the intimate sphere, and do not dare to visit a doctor for a long time, fearing that "everyone will find out about it. "
"
If we leave the psychological aspects aside and talk only about physiology, then the male reproductive system performs three main functions:
- production of spermatozoa and seminal fluid;
- delivery of semen to the female genital organs;
- synthesis of the male sex hormone - testosterone.
MALE EXTERNAL GENITAL ORGANS
Male external genital organs include: penis, testicles and scrotum, epididymis.
- The penis, or penis, is an organ designed for sexual intercourse and the ejection of semen into the woman's vagina. It consists of three parts: the root (with the help of which the penis is attached to the pubic region), the body and the head, covered with a fold of skin - the foreskin. In the area of the foreskin there are many glands that produce a sebaceous lubricant - smegma. Inside the penis consists of three parts (they are called bodies). Two cavernous (cavernous) bodies are on top. It is they who, filling with blood, provide an erection.
 Below is a spongy (spongiform) body - the urethra passes through it. During sexual intercourse, when semen erupts from the penis, the path for urine is blocked.
Below is a spongy (spongiform) body - the urethra passes through it. During sexual intercourse, when semen erupts from the penis, the path for urine is blocked. - The testicles of an adult male are the size of large olives. They produce testosterone and produce sperm. Nature knowingly placed the male testicles, unlike the female ovaries, outside the pelvic cavity. For normal spermatogenesis (the process of sperm formation), the temperature of the testicles must be slightly lower than inside the body. In this case, the scrotum acts as a "climate control" system.
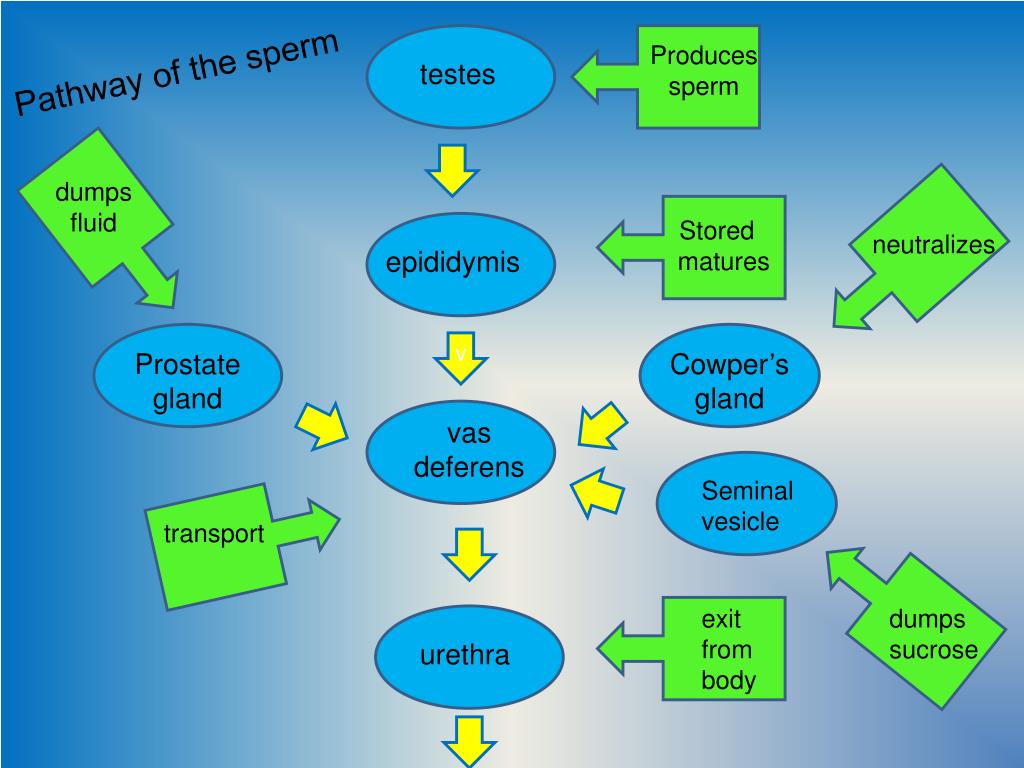
- The epididymis is a long, twisted, twisted canal in which spermatozoa are stored and mature. The appendages are located inside the scrotum behind the testicles. From them, spermatozoa enter the vas deferens.
INTERNAL SEXUAL ORGANS
Urologists say that every man has two hearts. The “upper” is located in the chest and pumps blood, and the “lower” is near the bladder, where the urethra departs from it.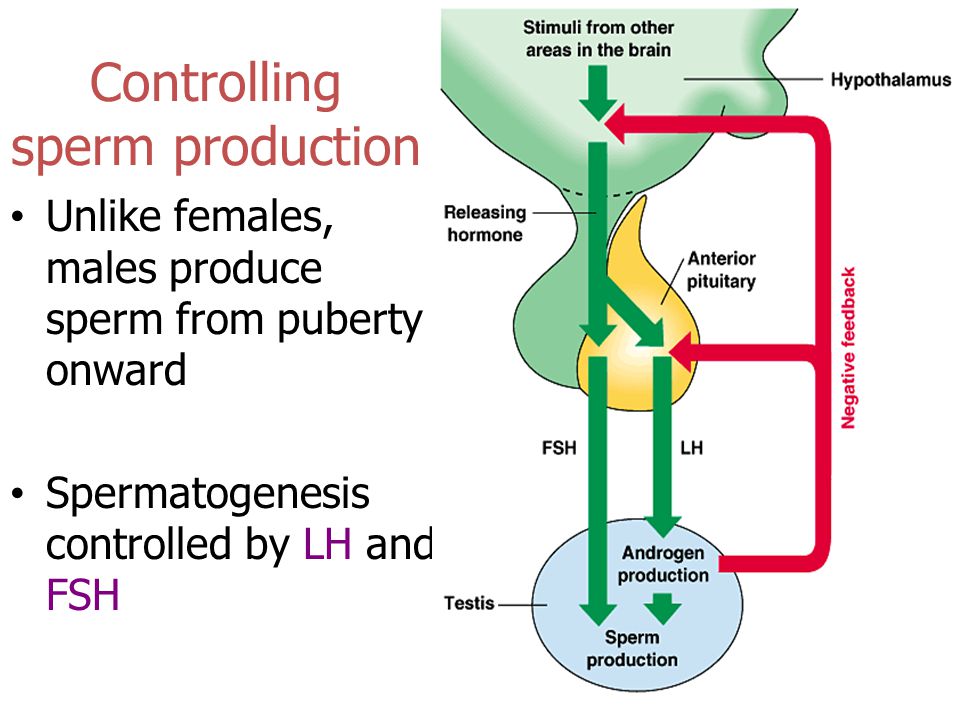 The “second heart” of a man is called the prostate gland (prostate). The prostate is about the size of a walnut, it adds its secret to the sperm, which contains nutrients.
The “second heart” of a man is called the prostate gland (prostate). The prostate is about the size of a walnut, it adds its secret to the sperm, which contains nutrients.
Other internal male genital organs:
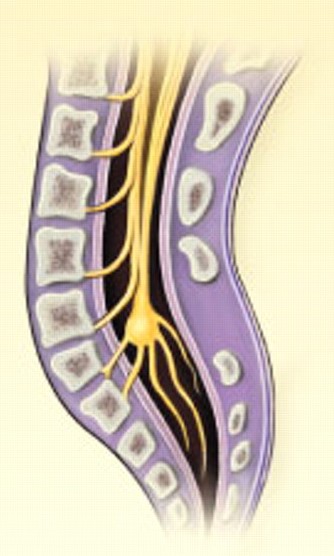
- The vas deferens originate from the epididymis and carry semen to the urethra. The urethra itself can also be considered as part of the male reproductive system.
- The seminal vesicles drain into the vas deferens near the bladder. The fluid they produce makes up most of the ejaculate. The secret of seminal vesicles contains a lot of sugar-fructose, it gives energy to spermatozoa.
- The bulbourethral (cooper) glands are about the size of a pea, located next to the prostate gland, secrete a secret into the urethra that lubricates its walls and neutralizes the acidity from the remaining urine.
Did you know that between 30 and 500 million spermatozoa leave a man's body during ejaculation?
WHAT HORMONES REGULATE THE
MALE REPRODUCTIVE SYSTEM?
The male reproductive system is mainly dependent on three hormones.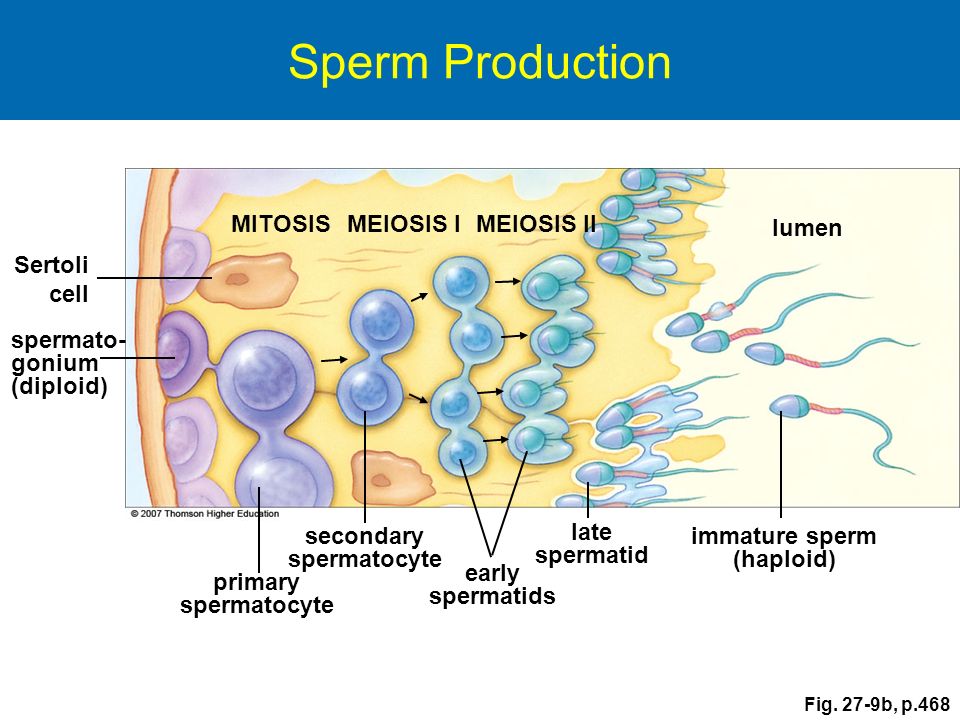 Luteinizing (LH) and follicle-stimulating (FSH) hormones are produced by the pituitary gland, a gland located at the base of the brain. FSH stimulates the formation of spermatozoa, LH stimulates the synthesis of testosterone.
Luteinizing (LH) and follicle-stimulating (FSH) hormones are produced by the pituitary gland, a gland located at the base of the brain. FSH stimulates the formation of spermatozoa, LH stimulates the synthesis of testosterone.
Testosterone is necessary for the production of sperm, as well as the appearance of secondary sexual characteristics: increased muscle mass, male-pattern body hair growth, sexual attraction to women, deep voice, etc.
HOW DOES SPERM FORM?
The production of sperm is called spermatogenesis. It can only occur under the influence of hormones, therefore, until puberty (12-16 years), the boy's body is not able to produce sperm.
When testosterone levels rise in a teenager's body, spermatogonia, special stem cells in the testicles, are activated. They turn into spermatocytes. These cells contain a double set of chromosomes; after division, secondary spermatocytes are formed from them, containing one set of chromosomes each.
A person has two sex chromosomes - X and Y.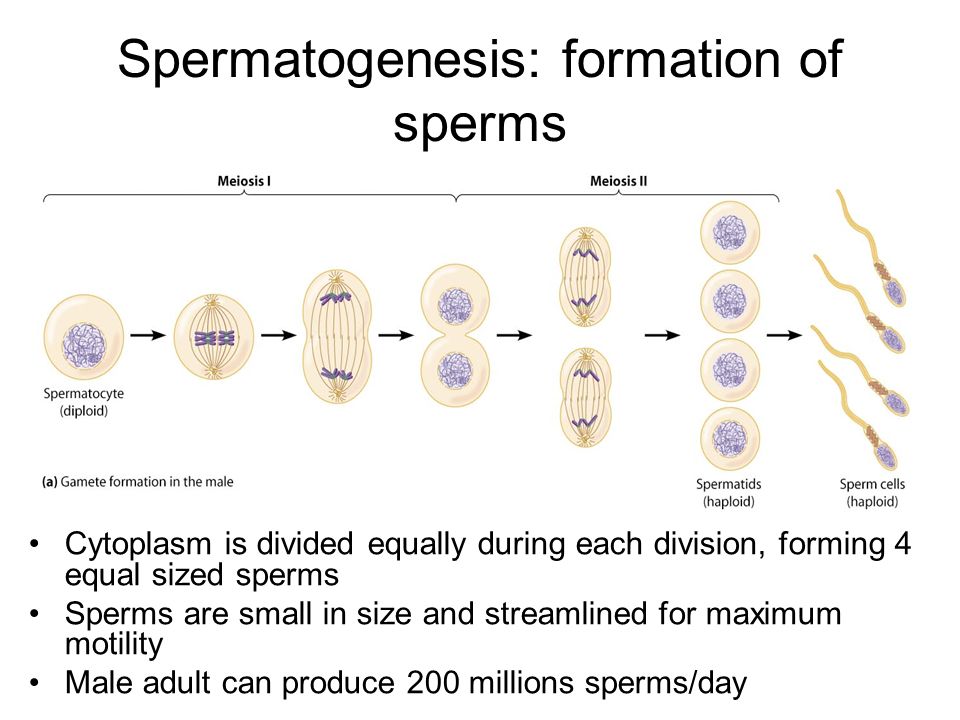 The egg can only contain the X chromosome. The sperm is either X or Y. If the egg is fertilized by a sperm with a Y chromosome, a boy is obtained, if with an X, a girl.
The egg can only contain the X chromosome. The sperm is either X or Y. If the egg is fertilized by a sperm with a Y chromosome, a boy is obtained, if with an X, a girl.
Spermatocytes are formed from spermatocytes. The complex process of sperm formation does not end there. Spermatid cells go through a process known as spermiogenesis. They grow tails, and they acquire features characteristic of spermatozoa. After maturation in the epididymis, they are ready to leave the body of a man in search of an egg.
Mature sperm can move at a speed of 20 cm per hour. And this despite the fact that its length is 0.05 mm.
DO MEN MENOPAUSE?
The term "menopause" refers to the cessation of menstruation in women. This happens due to a drop in the level of sex hormones. Normally, this should not happen in the male body. The testicles can produce sperm at age 80 and beyond.
However, in some men already in their 40s and 50s, testosterone levels decrease and sperm production drops. Often this occurs against the background of chronic diseases, such as diabetes. It is believed that this can lead to symptoms such as erectile dysfunction (weakening of erection), depression, weakness. This condition is sometimes referred to as "male menopause." With low testosterone levels, hormone replacement therapy is prescribed.
Often this occurs against the background of chronic diseases, such as diabetes. It is believed that this can lead to symptoms such as erectile dysfunction (weakening of erection), depression, weakness. This condition is sometimes referred to as "male menopause." With low testosterone levels, hormone replacement therapy is prescribed.
REMEDI doctors know everything about male reproductive health. We know how to preserve and restore it, to give a man the ability to have children.
Make an appointment
Childbirth may be possible without the participation of the egg
- James Gallagher
- BBC Science and Health Correspondent
events.
Image copyright SPL
Successful experiments show that science can achieve the birth of children without the participation of an egg.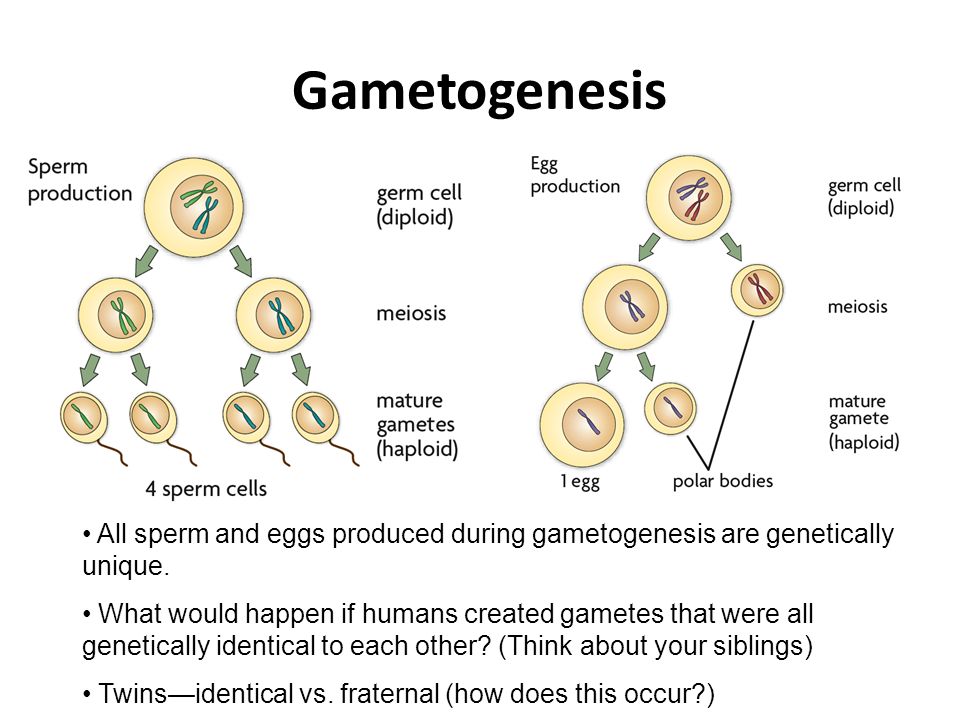
According to research published in the journal Nature Communications, it has already been possible to produce healthy mice by "convincing" sperm that they are fertilizing a normal egg.
This means, according to scientists, that in the distant future the process of childbearing may be possible without the participation of women.
At this stage, the experiments carried out help to better understand the process of fertilization.
Without mom and dad?
The scientists of the University of the British city of Bath started their experiments with an unfertilized egg.
Using various chemicals, they managed to "trick" her into a pseudoembryo.
These pseudoembryos are in many ways similar to ordinary cells, such as skin cells. They can divide and control their DNA.
The scientists hypothesized that if healthy mouse offspring could be produced by injecting sperm into such pseudoembryos of mice, this would mean that in the future a similar result could be achieved in human cells not derived from an egg.
In experiments on mice, the probability of achieving a successful pregnancy was 25%.
"For the first time, it has been shown that sperm, when combined with other non-egg cells, can produce healthy offspring," one of the researchers, Dr. Tony Perry, told the BBC.
"It turns all our centuries-old ideas upside down," he added.
The mice born as a result of the experiment were healthy, had a normal life expectancy and were able to give birth to healthy offspring.
Photo by Tony Perry
Fertilization
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of story Podcast
The purpose of the experiments was to investigate the exact mechanism of fertilization.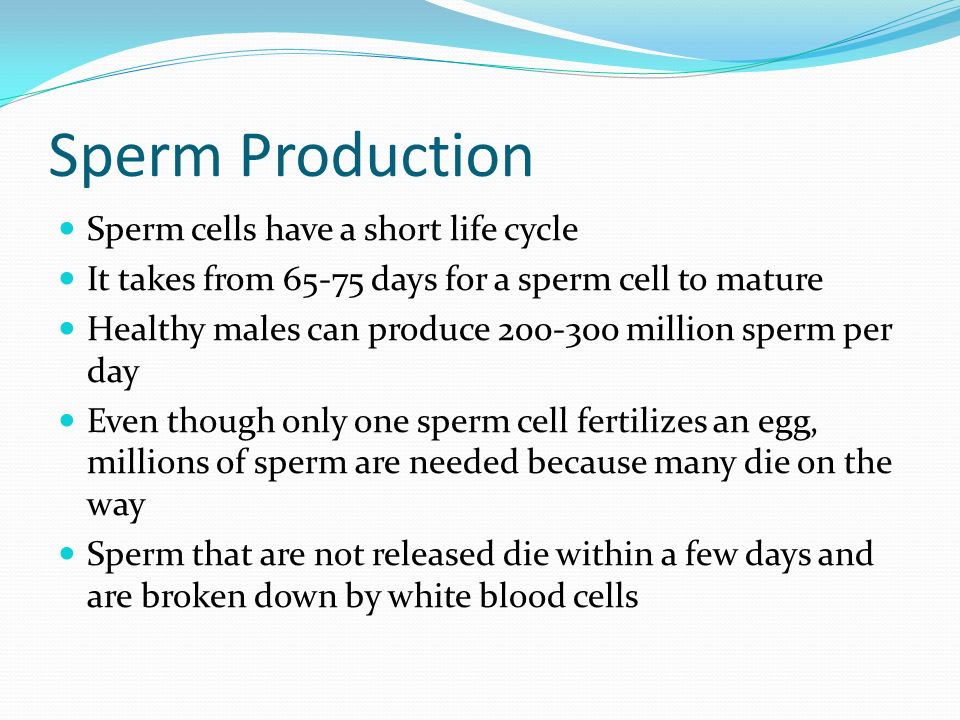 What exactly happens at the moment of the fusion of the sperm with the egg, has not yet been fully clarified.
What exactly happens at the moment of the fusion of the sperm with the egg, has not yet been fully clarified.
The ovum, for example, completely changes the entire chemical shell of the DNA of the sperm. As a result, the sperm stops behaving as such and behaves like an embryo. But how this "reincarnation" takes place is not yet clear.
Eliminating the need for an egg from the process of childbearing can have far-reaching social consequences.
"One possibility in the distant future is that ordinary cells of the human body, combined with sperm, could form an embryo," says Dr. Perry.
In other words, two men can be equally the biological parents of their child: one will give an ordinary cell, and the other will give sperm.
Or one man can become the parent of a child with the help of his own sperm and his own cell. In this case, the born child will be not so much a clone as a fraternal twin of his parent.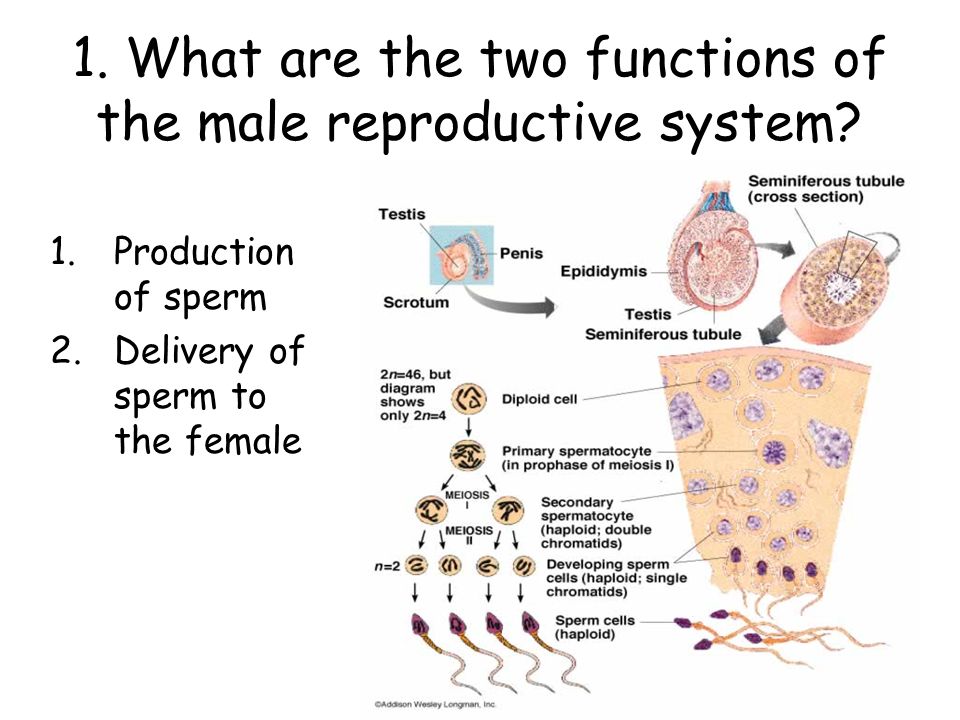

 Once menopause is complete, a woman can no longer conceive a child.
Once menopause is complete, a woman can no longer conceive a child.