Pregnant achy legs at night
Restless leg syndrome (pregnancy sleep)
In this article
- What is restless legs syndrome (RLS)?
- What causes restless legs syndrome (RLS) in pregnancy?
- What are the symptoms of restless legs syndrome?
- Can you get restless legs during the day?
- How is restless legs syndrome (RLS) diagnosed?
- How to relieve restless legs
- Can I take medication for treating RLS during pregnancy?
- Will my restless legs go away when my baby is born?
If you feel an overwhelming urge to move your legs because of a creeping, tingling sensation in them, you may have restless legs syndrome (RLS). RLS is common in pregnancy and can affect other parts of your body, including your arms and feet. Symptoms usually get worse when you're resting and many pregnant women experience restless legs at bedtime. Find out what causes restless arms and legs, and how to relieve symptoms.
What is restless legs syndrome (RLS)?
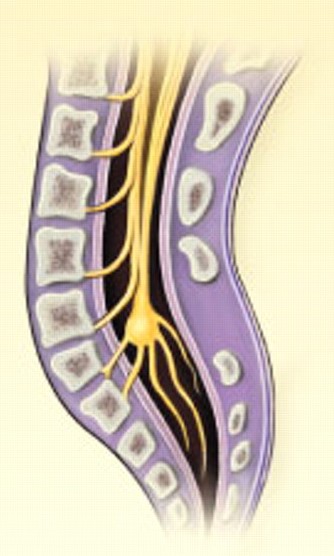
Restless legs syndrome (RLS), also known as Willis-Ekbom disease, is a medical condition of the nervous system. It’s common in pregnancy, with up to one in five women experiencing symptoms. Around two thirds of women who have RLS in pregnancy have pregnancy-induced RLS.
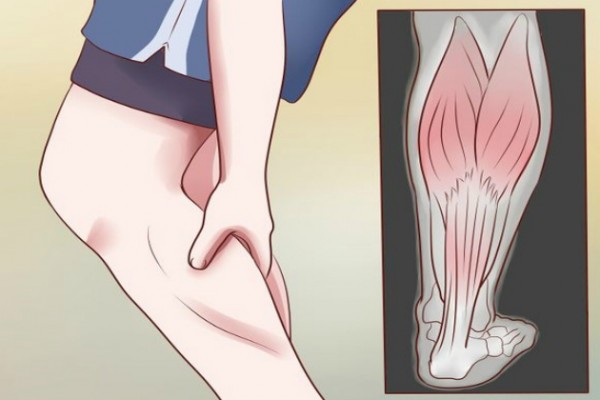
The main symptom of restless legs syndrome is an overwhelming urge to move your legs. You may also have an unpleasant crawling or creeping sensation in your feet, calves and thighs. The sensation is often worse in the evening or at night.
Restless legs syndrome can also affect other parts of your body, including your arms, feet, chest and face.
You may find that your limbs move and jerk around during the night. This is known as ‘periodic limb movements of sleep’, and happens in more than 80 per cent of people with RLS.
Most women with RLS develop it in their third trimester, but it can sometimes start earlier than this.
What causes restless legs syndrome (RLS) in pregnancy?
Experts aren’t exactly sure why RLS happens in pregnancy, but it may be caused by a change in hormones which could affect circulation.
It may also be caused by iron-deficiency anaemia, which is common in pregnancy, or folate deficiency anaemia.
You may hear your GP referring to your RLS as secondary restless legs syndrome, which means you have RLS because you’re pregnant. This helps to differentiate it from RLS that has no obvious cause (primary restless legs syndrome).
What are the symptoms of restless legs syndrome?
The most common symptom of RLS is an overwhelming urge to move your legs. This is sometimes, but not always, accompanied by other unpleasant sensations, such as:
- Crawling, creeping, tingling, burning, itching or throbbing sensations in the legs, usually below the knee.
- Cramping, aching or pain in the legs.
- Sensations in other parts of the body, such as the arms.
Can you get restless legs during the day?
Yes, you can. You may find that it’s hard to sit still for long periods of time. So you may notice symptoms happening on long train journeys or at your desk when you’re at work.
So you may notice symptoms happening on long train journeys or at your desk when you’re at work.
Symptoms are usually worse at night though, and can be a real nuisance when you're trying to wind down to sleep.
How is restless legs syndrome (RLS) diagnosed?
There is no test for RLS, so your GP will ask you about your symptoms and your medical history.
In some cases, restless legs syndrome is caused by an underlying health condition, such as Parkinson’s disease or rheumatoid arthritis. If your GP thinks this may be the case, they may need to carry out more tests. Certain medications, such as antidepressants, antiepileptic drugs and antihistamines have also been linked to RLS. In some cases they may trigger the condition, and in others, they may make it worse.
RLS can also run in families. Around half of people with RLS have a family member who also has or had the condition.
How to relieve restless legs
There are some things you can do to help ease the symptoms of RLS. You can also make some general lifestyle changes in order to prevent or reduce symptoms.
You can also make some general lifestyle changes in order to prevent or reduce symptoms.
Try one or more of the following to help ease your symptoms during an episode of RLS:
- Stretch and bend your legs by walking around.
- Massage your legs.
- Use a hot water bottle on the affected area, or have a warm bath.
- Use an ice pack instead, or a combination of ice pack and hot water bottle.
- Try to distract your mind from the sensations by reading or listening to a podcast.
- Practise some simple relaxation exercises, such as yoga.
A few simple lifestyle changes may help to prevent an episode from happening, or ease some of the symptoms.
Take regular exercise
Regular, moderate exercise may help to relieve RLS. Walking, swimming and yoga are all great choices during pregnancy.
Try to avoid vigorous exercise in the evening though, as it could make it harder for you to sleep. If RLS strikes, try gentle stretches or a slow stroll to relieve the symptoms.
If RLS strikes, try gentle stretches or a slow stroll to relieve the symptoms.
The best pregnancy exercises
Getting moving will help you to have a healthier pregnancy. Discover the best exercises to do when you’re expecting. More pregnancy videos
Cut down on caffeine
While you're pregnant, try not to have more than 200mg of caffeine a day, which is about two mugs of tea or one mug of filter coffee. Caffeine can make RLS worse and keep you awake. So cut down on tea (including green tea), coffee, cola and chocolate, especially in the late afternoon and evening.
Ask your midwife about supplements
In some cases, RLS can happen as a result of an iron deficiency, in which case iron supplements may help. Always speak to your GP, midwife or pharmacist for advice before taking any supplements in pregnancy though. If you’re not deficient in iron, it can be harmful for your baby if you take supplements.
Get into a sleep routine
Frustratingly, while restless legs can make it hard to sleep, not getting enough shut-eye can also make the symptoms worse. Going to bed and getting up at the same time every day will help to regulate your body clock and may make it easier for you to sleep.
Practising good ‘sleep hygiene’ may help you get a better night’s sleep. This means having good sleep habits, such as making your bedroom as dark and comfortable as possible, avoiding screens for a couple of hours before bed and keeping your bedroom solely for sleep or sex.
Don’t smoke or have alcohol
If you haven't already, stop smoking. Nicotine is a stimulant, so it can increase your heart rate and make you feel more alert at night. It’s also harmful for you, and your unborn baby. Here’s how to get help if you have trouble quitting smoking.
Alcohol is also a stimulant that can disrupt your sleep. Experts can’t be sure exactly how much alcohol, if any, is safe during pregnancy. That’s why they agree that the best advice is to avoid alcohol completely while you’re expecting.
That’s why they agree that the best advice is to avoid alcohol completely while you’re expecting.
Can I take medication for treating RLS during pregnancy?
It’s unlikely that your GP will prescribe medication for RLS during pregnancy. Instead, they will work with you to manage and control your symptoms with lifestyle changes and practical tips. If an iron deficiency is causing your RLS, then an iron supplement may be all you need to reduce your symptoms.
However, if your symptoms are affecting your quality of life, and nothing seems to be helping, speak to your GP. Certain medications may help to relieve symptoms, but should only be used for a short period of time.
Will my restless legs go away when my baby is born?
If you have pregnancy-induced RLS, it should go away within a few weeks of giving birth. However, women who suffer from RLS during pregnancy are more likely to develop it again, later in life.
If you find your symptoms continue after you have your baby, see your GP. There may be an underlying condition that’s causing your RLS.
RLS is one problem that can make it nearly impossible to sleep. Nausea, heartburn, or indigestion are other culprits. Read our tips for getting comfortable in bed when you're pregnant.
More on coping with pregnancy sleep disturbances:
- Find out if it's safe to take sleep medicine in pregnancy.
- Discover if a lack of sleep in your third trimester will harm your baby.
- Tried and tested: real-life tips for coping with tiredness during the day.
- Leg cramps keeping you awake at night? Find out if taking prenatal vitamins such as magnesium can help.
References
NHS. 2018. Restless legs syndrome . NHS, Health A-Z. www.nhs.uk [Accessed March 2021]
NHS. 2020a.Foods to avoid in pregnancy. NHS, Health A-Z. www.nhs.uk [Accessed March 2021]
NHS. 2020b.Drinking alcohol while pregnant. NHS, Health A-Z. www.nhs.uk [Accessed March 2021]
2020b.Drinking alcohol while pregnant. NHS, Health A-Z. www.nhs.uk [Accessed March 2021]
NICE. 2020a. Restless legs syndrome. National Institute for Health and Care Excellence. Health Topics. www.cks.nice.org.uk [Accessed March 2021]
NICE. 2020b. Insomnia National Institute for Health and Care Excellence. Health Topics. www.cks.nice.org.uk [Accessed March 2021]
Picchietti DL. 2019. Restless legs syndrome during pregnancy and lactation. UpToDate. www.uptodate.com [Accessed March 2021]
Pietrangelo A. 2018. Everything You Need To Know About Restless Leg Syndrome (RLS). Healthline. www.healthline.com [Accessed March 2021]
RLS-UK. nd. RLS in pregnancy. RLS-UK. www.rls-uk.org [Accessed March 2021]
Show references Hide references
Restless leg syndrome (pregnancy sleep)
In this article
- What is restless legs syndrome (RLS)?
- What causes restless legs syndrome (RLS) in pregnancy?
- What are the symptoms of restless legs syndrome?
- Can you get restless legs during the day?
- How is restless legs syndrome (RLS) diagnosed?
- How to relieve restless legs
- Can I take medication for treating RLS during pregnancy?
- Will my restless legs go away when my baby is born?
If you feel an overwhelming urge to move your legs because of a creeping, tingling sensation in them, you may have restless legs syndrome (RLS). RLS is common in pregnancy and can affect other parts of your body, including your arms and feet. Symptoms usually get worse when you're resting and many pregnant women experience restless legs at bedtime. Find out what causes restless arms and legs, and how to relieve symptoms.
RLS is common in pregnancy and can affect other parts of your body, including your arms and feet. Symptoms usually get worse when you're resting and many pregnant women experience restless legs at bedtime. Find out what causes restless arms and legs, and how to relieve symptoms.
What is restless legs syndrome (RLS)?
Restless legs syndrome (RLS), also known as Willis-Ekbom disease, is a medical condition of the nervous system. It’s common in pregnancy, with up to one in five women experiencing symptoms. Around two thirds of women who have RLS in pregnancy have pregnancy-induced RLS.
The main symptom of restless legs syndrome is an overwhelming urge to move your legs. You may also have an unpleasant crawling or creeping sensation in your feet, calves and thighs. The sensation is often worse in the evening or at night.
Restless legs syndrome can also affect other parts of your body, including your arms, feet, chest and face.
You may find that your limbs move and jerk around during the night. This is known as ‘periodic limb movements of sleep’, and happens in more than 80 per cent of people with RLS.
Most women with RLS develop it in their third trimester, but it can sometimes start earlier than this.
What causes restless legs syndrome (RLS) in pregnancy?
Experts aren’t exactly sure why RLS happens in pregnancy, but it may be caused by a change in hormones which could affect circulation.
It may also be caused by iron-deficiency anaemia, which is common in pregnancy, or folate deficiency anaemia.
You may hear your GP referring to your RLS as secondary restless legs syndrome, which means you have RLS because you’re pregnant. This helps to differentiate it from RLS that has no obvious cause (primary restless legs syndrome).
What are the symptoms of restless legs syndrome?
The most common symptom of RLS is an overwhelming urge to move your legs. This is sometimes, but not always, accompanied by other unpleasant sensations, such as:
This is sometimes, but not always, accompanied by other unpleasant sensations, such as:
- Crawling, creeping, tingling, burning, itching or throbbing sensations in the legs, usually below the knee.
- Cramping, aching or pain in the legs.
- Sensations in other parts of the body, such as the arms.
Can you get restless legs during the day?
Yes, you can. You may find that it’s hard to sit still for long periods of time. So you may notice symptoms happening on long train journeys or at your desk when you’re at work.
Symptoms are usually worse at night though, and can be a real nuisance when you're trying to wind down to sleep.
How is restless legs syndrome (RLS) diagnosed?
There is no test for RLS, so your GP will ask you about your symptoms and your medical history.
In some cases, restless legs syndrome is caused by an underlying health condition, such as Parkinson’s disease or rheumatoid arthritis. If your GP thinks this may be the case, they may need to carry out more tests. Certain medications, such as antidepressants, antiepileptic drugs and antihistamines have also been linked to RLS. In some cases they may trigger the condition, and in others, they may make it worse.
If your GP thinks this may be the case, they may need to carry out more tests. Certain medications, such as antidepressants, antiepileptic drugs and antihistamines have also been linked to RLS. In some cases they may trigger the condition, and in others, they may make it worse.
RLS can also run in families. Around half of people with RLS have a family member who also has or had the condition.
How to relieve restless legs
There are some things you can do to help ease the symptoms of RLS. You can also make some general lifestyle changes in order to prevent or reduce symptoms.
Try one or more of the following to help ease your symptoms during an episode of RLS:
- Stretch and bend your legs by walking around.
- Massage your legs.
- Use a hot water bottle on the affected area, or have a warm bath.
- Use an ice pack instead, or a combination of ice pack and hot water bottle.
- Try to distract your mind from the sensations by reading or listening to a podcast.

- Practise some simple relaxation exercises, such as yoga.
A few simple lifestyle changes may help to prevent an episode from happening, or ease some of the symptoms.
Take regular exercise
Regular, moderate exercise may help to relieve RLS. Walking, swimming and yoga are all great choices during pregnancy.
Try to avoid vigorous exercise in the evening though, as it could make it harder for you to sleep. If RLS strikes, try gentle stretches or a slow stroll to relieve the symptoms.
The best pregnancy exercises
Getting moving will help you to have a healthier pregnancy. Discover the best exercises to do when you’re expecting. More pregnancy videos
Cut down on caffeine
While you're pregnant, try not to have more than 200mg of caffeine a day, which is about two mugs of tea or one mug of filter coffee. Caffeine can make RLS worse and keep you awake. So cut down on tea (including green tea), coffee, cola and chocolate, especially in the late afternoon and evening.
So cut down on tea (including green tea), coffee, cola and chocolate, especially in the late afternoon and evening.
Ask your midwife about supplements
In some cases, RLS can happen as a result of an iron deficiency, in which case iron supplements may help. Always speak to your GP, midwife or pharmacist for advice before taking any supplements in pregnancy though. If you’re not deficient in iron, it can be harmful for your baby if you take supplements.
Get into a sleep routine
Frustratingly, while restless legs can make it hard to sleep, not getting enough shut-eye can also make the symptoms worse. Going to bed and getting up at the same time every day will help to regulate your body clock and may make it easier for you to sleep.
Practising good ‘sleep hygiene’ may help you get a better night’s sleep. This means having good sleep habits, such as making your bedroom as dark and comfortable as possible, avoiding screens for a couple of hours before bed and keeping your bedroom solely for sleep or sex.
Don’t smoke or have alcohol
If you haven't already, stop smoking. Nicotine is a stimulant, so it can increase your heart rate and make you feel more alert at night. It’s also harmful for you, and your unborn baby. Here’s how to get help if you have trouble quitting smoking.
Alcohol is also a stimulant that can disrupt your sleep. Experts can’t be sure exactly how much alcohol, if any, is safe during pregnancy. That’s why they agree that the best advice is to avoid alcohol completely while you’re expecting.
Can I take medication for treating RLS during pregnancy?
It’s unlikely that your GP will prescribe medication for RLS during pregnancy. Instead, they will work with you to manage and control your symptoms with lifestyle changes and practical tips. If an iron deficiency is causing your RLS, then an iron supplement may be all you need to reduce your symptoms.
However, if your symptoms are affecting your quality of life, and nothing seems to be helping, speak to your GP. Certain medications may help to relieve symptoms, but should only be used for a short period of time.
Certain medications may help to relieve symptoms, but should only be used for a short period of time.
Will my restless legs go away when my baby is born?
If you have pregnancy-induced RLS, it should go away within a few weeks of giving birth. However, women who suffer from RLS during pregnancy are more likely to develop it again, later in life.
If you find your symptoms continue after you have your baby, see your GP. There may be an underlying condition that’s causing your RLS.
RLS is one problem that can make it nearly impossible to sleep. Nausea, heartburn, or indigestion are other culprits. Read our tips for getting comfortable in bed when you're pregnant.
More on coping with pregnancy sleep disturbances:
- Find out if it's safe to take sleep medicine in pregnancy.
- Discover if a lack of sleep in your third trimester will harm your baby.
- Tried and tested: real-life tips for coping with tiredness during the day.

- Leg cramps keeping you awake at night? Find out if taking prenatal vitamins such as magnesium can help.
References
NHS. 2018. Restless legs syndrome . NHS, Health A-Z. www.nhs.uk [Accessed March 2021]
NHS. 2020a.Foods to avoid in pregnancy. NHS, Health A-Z. www.nhs.uk [Accessed March 2021]
NHS. 2020b.Drinking alcohol while pregnant. NHS, Health A-Z. www.nhs.uk [Accessed March 2021]
NICE. 2020a. Restless legs syndrome. National Institute for Health and Care Excellence. Health Topics. www.cks.nice.org.uk [Accessed March 2021]
NICE. 2020b. Insomnia National Institute for Health and Care Excellence. Health Topics. www.cks.nice.org.uk [Accessed March 2021]
Picchietti DL. 2019. Restless legs syndrome during pregnancy and lactation. UpToDate. www.uptodate.com [Accessed March 2021]
Pietrangelo A. 2018. Everything You Need To Know About Restless Leg Syndrome (RLS). Healthline. www.healthline.com [Accessed March 2021]
Healthline. www.healthline.com [Accessed March 2021]
RLS-UK. nd. RLS in pregnancy. RLS-UK. www.rls-uk.org [Accessed March 2021]
Show references Hide references
Reduces legs during pregnancy at night - Articles - Official website of Intex
Many young mothers after childbirth recall how much cramps the calves of the legs at night during pregnancy . Unfortunately, it reduces the calves of the legs at night, not only during pregnancy.
According to statistics, varicose disease of the lower extremities, one of the symptoms of which during childbearing are night cramps in the legs, persists after the birth of a baby in 60-75% of women. In this article, we will look at the stages of development of varicose veins in late pregnancy, explain why, as the disease develops cramps legs during pregnancy at night , and we will show you how to avoid the development of varicose veins during childbearing.
Why does he twist his legs at 37-39 weeks of pregnancy
If, during pregnancy, legs cramp at night due to “macronutrient hunger”, pain can be avoided by taking multivitamins containing potassium, calcium and magnesium. However, the causes of night pain in the legs during pregnancy, caused by other factors, are not so easy to deal with. In the third trimester of pregnancy, it reduces the calves of the legs at night more and more often. This is due to the influence of the hormone progesterone, the biological role of which is to relax the smooth muscle of the uterus. Simultaneously with the relaxation of the uterus, the smooth muscles of the venous walls lose their tone. Because of this, during pregnancy veins become very distensible . An increase in body weight in the third trimester is associated with an increased load on the legs, and, therefore, on the veins of the lower extremities. At the same time, the volume of fluid circulating in the blood increases. The pressure inside the veins weakened by progesterone increases, so the walls and valves of the veins begin to stretch. Because of this, also brings her legs together at night during pregnancy . Venous blood, seeping through the valves of the veins, returns to the legs and stagnates in the veins, causing extensive swelling.
However, the causes of night pain in the legs during pregnancy, caused by other factors, are not so easy to deal with. In the third trimester of pregnancy, it reduces the calves of the legs at night more and more often. This is due to the influence of the hormone progesterone, the biological role of which is to relax the smooth muscle of the uterus. Simultaneously with the relaxation of the uterus, the smooth muscles of the venous walls lose their tone. Because of this, during pregnancy veins become very distensible . An increase in body weight in the third trimester is associated with an increased load on the legs, and, therefore, on the veins of the lower extremities. At the same time, the volume of fluid circulating in the blood increases. The pressure inside the veins weakened by progesterone increases, so the walls and valves of the veins begin to stretch. Because of this, also brings her legs together at night during pregnancy . Venous blood, seeping through the valves of the veins, returns to the legs and stagnates in the veins, causing extensive swelling. The situation is aggravated by the pregnant uterus, which compresses the veins and additionally prevents the outflow of blood from the legs. Edema increases, the veins stretch, and varicose veins develop.
The situation is aggravated by the pregnant uterus, which compresses the veins and additionally prevents the outflow of blood from the legs. Edema increases, the veins stretch, and varicose veins develop.
What to do if your legs hurt while you sleep during pregnancy
If your legs hurt during pregnancy at night, you need to see a phlebologist as soon as possible. Since drug therapy is contraindicated for pregnant women, the doctor will help choose compression stockings for the prevention of varicose veins. Compression stockings and tights "Intex" are designed by especially for pregnant women . Elastic underwear exerts distributed pressure on the legs, stimulating the outflow of blood from the legs, and allowing you to maintain the vascular walls and valves of the veins. Improved blood flow allows you to get rid of edema , and the external support of the venous vessels does not allow the veins to stretch, and helps to avoid the situation when legs are pulled during pregnancy at night.
Bringing legs together during pregnancy: what to do?
Pregnancy is a time of waiting and doubts. Probably, women never have so many questions. Why does it bring her legs together so often? What to do if you wake up with cramps at night? How to deal with this scourge and avoid bouts of pain in the legs? We are looking for answers to these and other questions.
What are seizures?
Legs cramps not only during pregnancy, from time to time every person faces unpleasant painful cramps. A cramp is a sudden, uncontrollable muscle contraction that a person cannot relax. This condition can be caused by neurological disorders (for example, seizures are characteristic of epilepsy), a number of diseases (such as diabetes mellitus, osteochondrosis, and others), and can also be associated with physiological conditions. After all, convulsions occur, for example, after a strong overload, dehydration, hypothermia, etc. Sometimes cramps cause severe sharp pain. Sometimes it seems that the legs are pulling. During pregnancy, this condition, unfortunately, is noted quite regularly.
Sometimes it seems that the legs are pulling. During pregnancy, this condition, unfortunately, is noted quite regularly.
Why do pregnant women cramp their legs?
The mechanism of muscle contraction is quite complex, it involves different ions (charged particles): potassium, calcium, sodium and magnesium. If we are talking about a cramp, that is, a condition when we cannot relax a muscle, then magnesium ions play a leading role here. It is their lack that leads to the fact that women cramp their calves during pregnancy at night.
The lack of minerals in the body of the expectant mother is simply explained: such consequences are the restructuring of metabolism and functioning in the "double load" mode. In particular, the expectant mother needs one and a half times more magnesium than usual.
In addition to helping muscles relax, magnesium is also involved in a number of important physiological processes. In particular, magnesium is needed to regulate the processes of formation and expenditure of energy, it is involved in several hundred enzymatic reactions, and if there is little magnesium, then disturbances can occur in the work of almost any body system. Therefore, if magnesium preparations are prescribed during pregnancy, this recommendation should not be ignored.
Therefore, if magnesium preparations are prescribed during pregnancy, this recommendation should not be ignored.
Why do pregnant women have cramps at night?
The answer to this question is very simple. The fact is that during the day the body of the expectant mother bears an increased load. And the longer the gestation period, the greater this load. Violation of blood circulation, increased stress on the muscles - all this can cause night cramps.
What should I do if my legs cramp during pregnancy?
To begin with, tell the doctor you are seeing about this. The magnesium preparations already mentioned, which he most likely recommends to you, can help solve the problem.
However, the reason that the expectant mother cramps her legs during pregnancy may be not only a metabolic disorder. Often muscle spasms begin as a result of varicose veins - the "faithful" companion of pregnancy. The veins of a woman carrying a baby are subject to increased stress.