Drinking in the first trimester
Drinking a little alcohol early in pregnancy may be okay
The usual message to pregnant women: Don't drink any alcohol. Clearly alcohol use can cause major problems for the pregnant woman and her baby.
While not drinking any alcohol during pregnancy is the safest choice, small amounts of alcohol early in pregnancy may be less risky to the mother’s health and the health of their babies than previously believed. Minimal alcohol use during the first trimester doesn’t appear to increase the risk for high blood pressure complications, or premature birth or low birth weights. That’s the findings of a study previously published in the journal Obstetrics and Gynecology.
Dr. Fergus McCarthy and colleagues from Ireland, England, New Zealand, and Australia compared birth outcomes among 5,628 women who were pregnant for the first time between 2004 and 2011. More than half of them reported drinking alcohol during the first three months of pregnancy. Some (19%) reported occasionally drinking alcohol. Twenty-five percent reported low alcohol consumption, or three to seven drinks per week ("a drink" defined as a glass of wine or a little less than a 12-ounce bottle of beer). Another 15% reported having more than seven drinks per week.
Rates of premature birth, babies with low birth weight or small size, and pre-eclampsia—a potentially life-threatening condition in which a pregnant woman develops high blood pressure—were similar across the alcohol consumption categories
The potential hazard of alcohol during pregnancy
For the past few decades, women have been urged to avoid alcohol during pregnancy. Respected medical societies like the American College of Obstetricians and Gynecologists and the United Kingdom's Royal College of Obstetricians and Gynaecologists Women both say women shouldn't drink any alcohol during pregnancy. The main reason for this is that heavy use of alcohol during pregnancy has been linked to a long-term and irreversible condition known as fetal alcohol syndrome (FAS).
Babies with FAS may be born early. They are often underweight and don't grow well. Some have characteristic facial features like a thin upper lip and small eye openings, or the small vertical groove between the upper lip and the nose may be flattened. Other physical signs that go along with fetal alcohol syndrome include a small head, short nose, and problems with the way the heart or the joints are formed.
Children with FAS are slower to learn language skills than other kids. When they reach school age they often have learning disabilities and difficulty with attention, memory and hyperactivity. They are more likely to have poor coordination and a hard time with problem-solving. And some have trouble making friends and relating to other kids. All of which can make school a really difficult time.
Despite this clear advice, up to half of women drink some alcohol during pregnancy.
Putting it into practice
How clear is the medical evidence supporting strict abstinence from alcohol during pregnancy? Not very strong. Other studies suggest pregnant women who have an occasional drink don't harm themselves or their baby. A 2012 Danish study, for example, found that low to moderate alcohol consumption during pregnancy did not affect executive functioning among 5-year-olds. Executive functioning is a catchall term that describes the ability to perform activities such as planning, organizing, strategizing, remembering details, and managing time.
Other studies suggest pregnant women who have an occasional drink don't harm themselves or their baby. A 2012 Danish study, for example, found that low to moderate alcohol consumption during pregnancy did not affect executive functioning among 5-year-olds. Executive functioning is a catchall term that describes the ability to perform activities such as planning, organizing, strategizing, remembering details, and managing time.
However, since it's not clear how much alcohol it takes to cause problems, the best advice remains the same: women should avoid alcohol if they are pregnant or might become pregnant.
For the many women that drank some alcohol before they realized they were pregnant, this and other studies should reassure them. They almost surely did no harm to their unborn children.
Image: The Good Brigade/Getty Images
Fetal Alcohol Exposure | National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Image
Fetal alcohol exposure occurs when a woman drinks while pregnant. Alcohol can disrupt fetal development at any stage during a pregnancy—including at the earliest stages before a woman even knows she is pregnant.
Alcohol can disrupt fetal development at any stage during a pregnancy—including at the earliest stages before a woman even knows she is pregnant.
Research shows that binge drinking and regular heavy drinking put a fetus at the greatest risk for severe problems.1 (The National Institute on Alcohol Abuse and Alcoholism defines binge drinking as a pattern of drinking alcohol that brings blood alcohol concentration [BAC] to 0.08 percent—or 0.08 grams of alcohol per deciliter—or higher. For a typical adult female, this pattern of alcohol consumption corresponds to consuming 4 or more drinks in about 2 hours. [NIAAA. (2007, November). Defining binge drinking. What Colleges Need to Know Now. Available at: https://www.collegedrinkingprevention.gov/media/1College_Bulletin-508_3….]) However, even lesser amounts can cause damage.2,3 In fact, there is no known safe level of alcohol consumption during pregnancy.
Alcohol passes easily from a mother’s bloodstream into her developing baby’s blood. Alcohol present in a developing baby’s bloodstream can interfere with the development of the brain and other critical organs, structures, and physiological systems.
Alcohol present in a developing baby’s bloodstream can interfere with the development of the brain and other critical organs, structures, and physiological systems.
Prenatal alcohol exposure is a leading preventable cause of birth defects and neurodevelopmental abnormalities in the United States. It can cause a range of developmental, cognitive, and behavioral problems, which can appear at any time during childhood and last a lifetime.
The most profound effects of prenatal alcohol exposure are brain damage and the resulting impairments in behavioral and cognitive functioning.
Fetal Alcohol Spectrum Disorders
Scientists define a broad range of effects and symptoms caused by prenatal alcohol exposure under the umbrella term Fetal Alcohol Spectrum Disorders (FASD).
The medical disorders collectively labeled FASD include the Institute of Medicine of the National Academies (IOM) diagnostic categories:4
-
Fetal Alcohol Syndrome (FAS)
-
Partial FAS (pFAS)
-
Alcohol-Related Neurodevelopmental Disorder (ARND)
-
Alcohol-Related Birth Defects (ARBD)
In addition to the IOM medical diagnoses, the latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–5) includes the psychiatric diagnosis, Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE). 5 People who meet criteria for an FASD diagnosis according to the IOM may also meet criteria for ND-PAE.
5 People who meet criteria for an FASD diagnosis according to the IOM may also meet criteria for ND-PAE.
The essential features common to the IOM medical diagnoses and the DSM–5 psychiatric diagnosis are prenatal alcohol exposure and central nervous system (CNS) involvement.
Evidence of CNS involvement can be structural (e.g., small brain size, alterations in specific brain regions) or functional (e.g., cognitive and behavioral deficits, motor and coordination problems). Advanced imaging studies have revealed differences in brain structure and activity that are consistent with data from neuropsychological testing, including deficits in sensory processing, cognition, and behavior in persons with FASD compared to people without FASD.6
FASD-Related Problems
Each individual with FASD experiences a unique combination of day-to-day challenges that may include medical, behavioral, educational, and social problems. People with FASD may have difficulty in the following areas:7
-
Learning and remembering
-
Understanding and following directions
-
Shifting attention
-
Controlling emotions and impulsivity
-
Communicating and socializing
-
Performing daily life skills, including feeding, bathing, counting money, telling time, and minding personal safety
FASD-related brain damage makes it difficult to address routine life situations. It causes people to make bad decisions, repeat the same mistakes, trust the wrong people, and have difficulty understanding the consequences of their actions.
It causes people to make bad decisions, repeat the same mistakes, trust the wrong people, and have difficulty understanding the consequences of their actions.
FASD cases are seriously under-diagnosed. FASD can be difficult for practitioners to distinguish from other developmental disorders since these disorders share certain learning and behavioral problems.
In addition, people with FASD are more likely to suffer from the following mental health disorders:8
-
Attention Deficit Hyperactivity Disorder (ADHD)
-
Depression and anxiety
-
Problems with hyperactivity, conduct, and impulse control
-
Increased incidence of alcohol and other substance use disorders
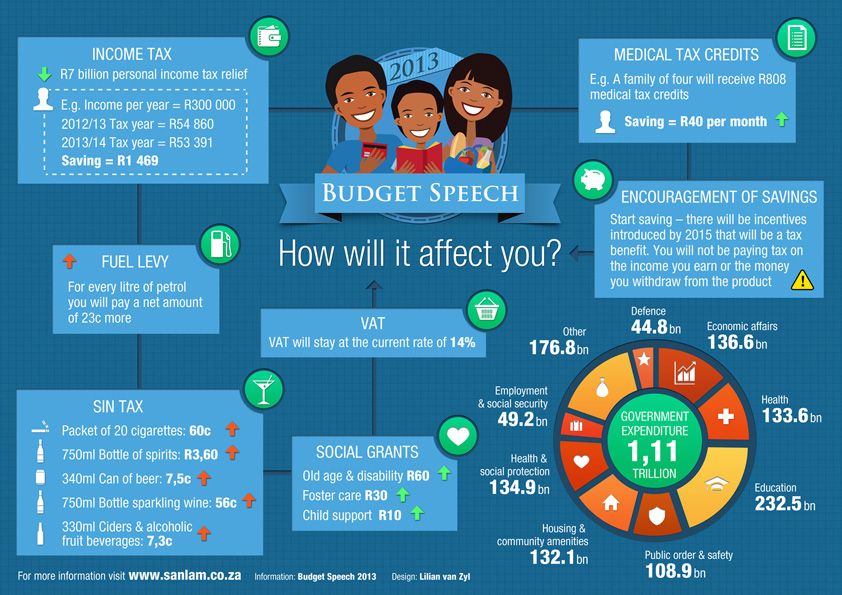
Key Statistics for the United States—Maternal Drinking
-
About 20 to 30 percent of women have reported drinking at some point during pregnancy—most typically during the first trimester.12
-
More than 8 percent of women have reported binge drinking at some time during pregnancy—most typically during the first trimester.
 12
12 -
Almost 10 percent of pregnant women reported drinking alcohol in the previous month.13
-
Almost 5 percent of pregnant women reported binge drinking in the previous month (4 or more drinks per occasion).13
Relevant Clinical Diagnoses
IOM DiagnosesImage
Fetal Alcohol Syndrome (FAS)
Fetal Alcohol Syndrome (FAS) was the first form of FASD discovered and is the most well-known. Heavy alcohol use during the first trimester of pregnancy can disrupt normal development of the face and the brain. In fact, exposure at any point during gestation may affect brain development. An FAS diagnosis requires:
-
Evidence of prenatal alcohol exposure
-
Evidence of central nervous system (CNS) abnormalities (structural or functional)
-
A specific pattern of three facial abnormalities: narrow eye openings, a smooth area between the lip and the nose (vs.
 the normal ridge), and a thin upper lip
the normal ridge), and a thin upper lip -
Growth deficits either prenatally, after birth, or both
Partial FAS (pFAS)
Partial FAS (pFAS) involves prenatal alcohol exposure, and includes some, but not all, of the characteristics of full FAS.
Alcohol-Related Neurodevelopmental Disorder (ARND)
A diagnosis of Alcohol-Related Neurodevelopmental Disorder (ARND) requires evidence of both prenatal alcohol exposure and CNS abnormalities, which may be structural or functional. Functional abnormalities may involve a complex pattern of cognitive or behavioral problems that are not consistent with developmental level, and that cannot be explained by factors other than prenatal alcohol exposure (e.g., family background, environment, and other toxicities). Facial abnormalities and growth retardation need not be present.
Alcohol-Related Birth Defects (ARBD)
This disorder includes medical conditions linked to prenatal alcohol exposure such as: heart, kidney, and bone problems and other malformations; difficulty seeing and hearing; and reduced immune function. Alcohol-Related Birth Defects (ARBD) is rarely seen alone but rather as a secondary disorder accompanying other FASD conditions (e.g., FAS and ARBD).
Alcohol-Related Birth Defects (ARBD) is rarely seen alone but rather as a secondary disorder accompanying other FASD conditions (e.g., FAS and ARBD).
DSM–5 Diagnosis
Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE)
Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE) is a new psychiatric diagnosis in the DSM–5. It requires evidence of both prenatal alcohol exposure and CNS involvement, as indicated by impairments in the following three areas: cognition, self-regulation, and adaptive functioning. This new diagnosis for use by mental health professionals will improve understanding of the multifaceted behavioral deficits seen in some people exposed to alcohol prenatally, and facilitate improved diagnosis and treatment of these individuals.
Risk Factors
9The severity of alcohol’s effects on a fetus primarily depends on the following:
-
Quantity—how much a pregnant woman drinks per occasion
-
Frequency—how often a pregnant woman drinks
-
Timing—in what stage of pregnancy a woman drinks and if she drinks heavily just as the fetus develops a particular feature or brain region
Other factors can also play a role in how prenatal alcohol exposure affects children. These include:
These include:
Image
Maternal Characteristics
Research demonstrates that children may be more affected by prenatal alcohol exposure if their mothers:
-
Have poor nutrition
-
Have had multiple pregnancies and births
-
Have lower-than-average weight, height, and body mass index (BMI)
-
Smoke
-
Are older
-
Are a member of a family of heavy drinkers
Environmental Factors
Research demonstrates that children can be more affected by prenatal alcohol exposure if their mothers experience adverse-living conditions and high levels of stress. These may include: social isolation, living in circumstances where alcohol misuse is common and accepted, and living in a community where resources for prenatal care are limited.
Genetics
The extent of FASD symptoms may depend on the mother’s genetic makeup, her child’s genetic makeup, and changes in gene activity caused by prenatal alcohol exposure.
Interventions
Researchers and clinicians have developed effective learning and behavioral interventions to help people with FASD. For example, school-based interventions can help children with FASD learn more easily. School-based interventions may include specialized teaching strategies that provide a consistent routine and allow children to practice new skills over and over again.10 Other promising interventions include:
-
Family support groups and classes to help parents better care for a child with FASD.10
-
Nutritional supplements for pregnant women and postnatal supplements for their children.11
-
Behavioral interventions for affected children, including training in social skills, problem solving, and personal safety.10
1 Maier, S.E., and West, J.R. Drinking patterns and alcohol-related birth defects. Alcohol Research and Health 25(3):168–169, 2001.
2 Hamilton, D.A., Barto, D., Rodriguez, C.I., Magcalas, C.M., Fink, B.C., Rice, J.P., Bird, C.W., Davies, S., and Savage, D.D. Effects of moderate prenatal alcohol exposure and age on social behavior, spatial response perseveration errors and motor behavior. Behavioral Brain Research 269: 44–54, 2014.
3 Day N.L., Helsel, A., Sonon, K., and Goldschmidt, L. The association between prenatal alcohol exposure and behavior at 22 years of age. Alcoholism: Clinical and Experimental Research 37(7):1171–1178, 2013.
4 Stratton, K., Howe, C., and Battaglia, F. (eds.) Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. The Institute of Medicine Report. Washington, DC: National Academy Press, 1996.
5 American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (pp. 86, 798–801). Washington, DC: American Psychiatric Association, 2013.
6 Moore, E.M., Migliorini, R., Infante, M.A., and Riley, E.P. Fetal alcohol spectrum disorders: Recent neuroimaging findings. Current Developmental Disorders Reports 1(3):161–172, 2014.
7 Mattson, S. N., Crocker, N., and Nguyen, T.T. Fetal alcohol spectrum disorders: Neuropsychological and behavioral features. Neuropsychology Review 21(2):81–100, 2011.
8 O’Connor, M.J. Mental health outcomes associated with prenatal alcohol exposure: Genetic and environmental factors. Current Developmental Disorders Reports 1(3):181–188, 2014.
9 May, P.A., and Gossage, J.P. Maternal risk factors for fetal alcohol spectrum disorders. Alcohol Research & Health 34(1):16–23, 2011.
10 Paley, B., and O’Connor, M.J. Intervention for individuals with fetal alcohol spectrum disorders: Treatment approaches and case management. Developmental Disabilities Research Reviews 15:258–267, 2009.
11 Warren, K.R.; Hewitt, B.G.; and Thomas, J.D. Fetal alcohol spectrum disorders: Research challenges and opportunities. Alcohol Research & Health 34(1):4–14, 2011.
12 Ethen, M.K., Ramadhani, T.A., Scheuerle, A.E., Canfield, M.A., Wyszynski, D.F., Druschel, C.M., and Romitti, P.A., National Birth Defects Prevention Study. Alcohol consumption by women before and during pregnancy. Maternal and Child Health Journal 13(2):274–285, 2009.
13 Substance Abuse and Mental Health Services Administration (SAMHSA). Table 6.20B—Alcohol Use, Binge Alcohol Use, and Heavy Alcohol Use in Past Month among Females Aged 15 to 44, by Pregnancy Status, Demographic, Socioeconomic, and Pregnancy Characteristics: Percentages, 2018 and 2019. Available at: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2018R2/NSDUHDetTabsSect6pe2018.htm#tab6-20b. Accessed 9/25/20.
The effect of alcohol during pregnancy on the fetus: a modern view of the problem
Many women believe that it is possible to drink alcohol during pregnancy, albeit in small quantities. Of course, we are not talking about hard liquor like vodka or cognac, but a glass of red wine or beer is another matter.
Of course, we are not talking about hard liquor like vodka or cognac, but a glass of red wine or beer is another matter.
However, everything is not as simple as it might seem at first glance, and even small doses of ethanol can cause irreversible changes in the development of the child. Medicine still does not give an exact answer about the permissible strength and volume of drinks that can be consumed during pregnancy without fear.
Important! Recent research has shown that even small amounts of alcohol during pregnancy can increase the chance of preterm birth and underweight babies (LBW).
Alcohol in early pregnancy
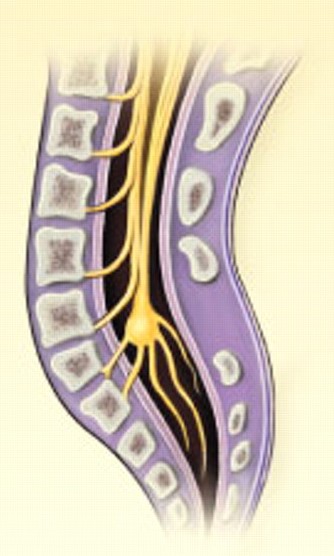
When ingested by a pregnant woman, ethanol crosses the placental barrier and has a devastating effect on the fetal brain. If a mother regularly drinks alcohol during early gestation, it can lead to damage to the white matter, cerebellum, and brainstem.
Drinking alcohol during pregnancy in the early stages is fraught with a violation of the formation of the brain structures of the child, and also contributes to the development of such serious defects as:
- mental retardation;
- micro-, hydrocephalus;
- mental retardation, etc.

It is believed that in the first days and even weeks after pregnancy, alcohol is allowed. The placenta is not yet formed, which means that there will be no harm to the baby. However, ethanol makes it difficult for the embryo to attach, thereby increasing the risk of miscarriage.
Pregnant women in the first trimester are strongly discouraged from drinking alcohol, even in small quantities. This also applies to beer, wine and other low-alcohol drinks. Get a remote consultation from our gynecologists to protect yourself and your baby.
The first week of pregnancy: a crucial stage
Alcohol is quite capable of harming the fetus in the first 5-7 days after conception, when it is only a fertilized egg. According to statistics, a huge number of miscarriages happen precisely in the early stages, when a woman does not yet know about pregnancy and, as they say, "misses a glass or two."
During the first week, the fertilized egg travels to the uterus through the fallopian tube. At this time, the drunk alcohol almost instantly enters the bloodstream and inevitably penetrates into the zygote. The result is very often spontaneous abortion, or miscarriage.
At this time, the drunk alcohol almost instantly enters the bloodstream and inevitably penetrates into the zygote. The result is very often spontaneous abortion, or miscarriage.
Case study:
When registering, the woman was worried that the child might be born handicapped, as there was alcohol consumption during pregnancy. She complained of nagging pain and heaviness in the lower abdomen, which was the reason for hospitalization. The pregnancy was saved.
What does "early" mean
By early is meant the gestation period in the first three months - that is, the 1st trimester. Conventionally, it can be divided into 2 periods:
- The first 10-12 days from the moment of conception.
- From 12-13 days to 13 weeks (end of the 1st trimester).
Effect of alcohol on the fetus during the first 10-12 days after pregnancy
Every woman from birth has a large set of follicles, of which there are about 500 thousand. New follicles no longer appear, and some die. This does not really matter, since no more than 500 of them will mature over the entire fertile period.
New follicles no longer appear, and some die. This does not really matter, since no more than 500 of them will mature over the entire fertile period.
But under the influence of ethanol, the death of follicles is accelerated, and some are damaged. If a spermatozoon fertilizes a damaged egg, a child may develop congenital malformations.
The less alcohol a woman drinks, the healthier her eggs are.
Even strong alcohol does not affect the state of the fertilized egg, if the pregnancy has already begun. A healthy oocyte is not threatened with damage, and the process of cell division will go according to the plan laid down by nature.
The danger lies in the fact that alcohol activates the production of a specific fluid in the fallopian tubes. The latter are the springboard through which the egg enters the uterus. If the fallopian tubes are blocked, the embryo will simply get stuck and attach to the wall of the tube before reaching the uterus.
On the 4-5th day after the onset of pregnancy, the embryo has about 58 cells and enters the uterus. It is built into its wall, and the formation of the chorion, the outer shell of the embryo, begins.
Up to 12-13 days, that is, before the circulatory system appears in the placenta, alcohol drunk by a pregnant woman can destroy the embryo, causing a miscarriage. However, he is not capable at this stage of pregnancy to cause any pathology.
All of the above does not apply to women suffering from alcoholism, and only applies to those who drink a little, rarely and only quality drinks.
If a pregnant woman drank alcohol at an early date, not yet knowing about her “interesting position”, you should not worry too much. It is unlikely that this will affect the health of the unborn child. However, you need to make sure that there is no ectopic pregnancy.
Why alcohol should not be drunk from the 12th-13th day to the 13th week of pregnancy
Around this time, the placental circulatory system begins to form. This means that the fetus takes oxygen and nutrition directly from the mother's body. If the mother drinks alcohol during pregnancy, the blood vessels will narrow, and the child will receive less oxygen: he will experience a state of hypoxia (oxygen starvation).
This means that the fetus takes oxygen and nutrition directly from the mother's body. If the mother drinks alcohol during pregnancy, the blood vessels will narrow, and the child will receive less oxygen: he will experience a state of hypoxia (oxygen starvation).
Even the liver of an adult perceives alcohol as a poisonous substance. In the fetus, the liver is just beginning to form and is not able to cope with the poison, the amount of which in his blood is similar to that in the blood of the mother, thanks to the placental circulatory system.
Case study:
The patient turned to the gynecologist for advice about a possible pregnancy with the question "to save or not to save." She admitted that she drank alcohol, not knowing about her condition. The term is 12 weeks. Ultrasound showed the absence of fetal abnormalities and the threat of miscarriage. In due time, the woman gave birth to a healthy child.
Pregnant women cannot drink alcohol in the 1st trimester, as all systems and organs of the baby are laid. You should be especially careful in the period from 28 to 49the day when the laying of facial features occurs. Drinking alcohol can negatively affect a child's appearance.
You should be especially careful in the period from 28 to 49the day when the laying of facial features occurs. Drinking alcohol can negatively affect a child's appearance.
Drinking alcohol during pregnancy at the very beginning of the term is highly undesirable. The consequences can be catastrophic:
| No. p / p | Consequences of drinking alcohol |
| one. | fetal alcohol syndrome (FAS), which includes a whole set of congenital malformations |
| 2. | dysfunction of the brain and spinal cord |
| 3. | problems with the nervous system, the manifestations of which can range from mood swings to psychosis and suicidal tendencies |
| four. | defects in the structure of the genital organs - for example, undescended testicles in boys, doubling of the uterus and vagina in girls |
Alcohol during early pregnancy significantly increases the risk of miscarriage and premature birth. But it is important to know that even with the birth of a healthy child, the consequences may appear later. Most often they occur during puberty.
But it is important to know that even with the birth of a healthy child, the consequences may appear later. Most often they occur during puberty.
Important! It doesn't matter what the mother drinks - red or white wine, beer, cider, low-alcohol cocktails or homemade liquor.
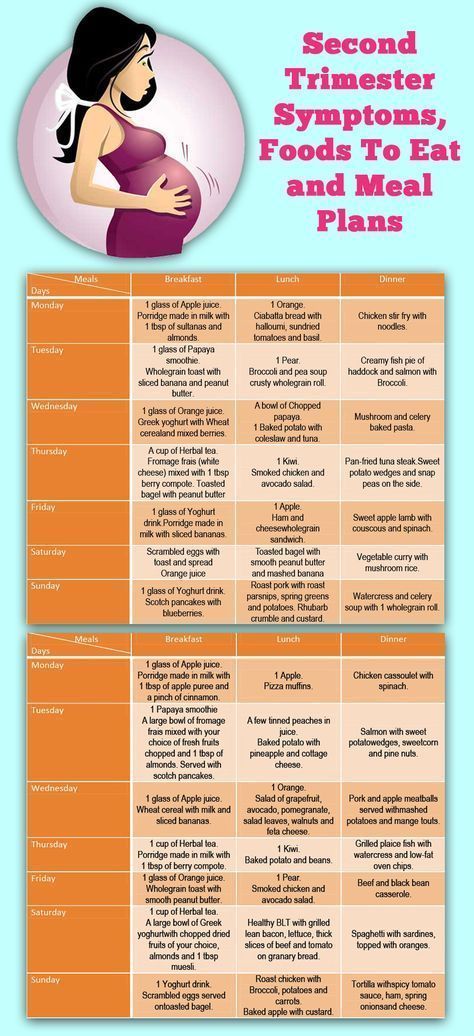
Is it possible to drink wine during pregnancy in the second trimester
With the second trimester, everything is both easier and more difficult. The question is how much and when. Of course, it is better to completely refrain from alcohol, replacing them with tasty and healthy juices.
Intemperance in relation to alcohol can provoke a child:
- heart disease;
- distortion of facial features, disproportion of body parts;
- reduced muscle tone;
- impaired ability to concentrate, which will lead to learning difficulties;
- violation of diction, speech;
- weak immunity;
- hyperactivity, etc.

One of the consequences of drinking alcohol by a pregnant woman is the fading of the fetus.
However, there is no complete ban on wine during pregnancy in the second trimester. That's just to afford alcohol is allowed only in the middle of the 2nd trimester. At the beginning of this period, the fetus is not yet protected by the placenta, and its organs are actively developing.
1 sip of wine is allowed to drink at the beginning of the 2nd trimester if nausea is tormented.
A glass of wine during pregnancy can help:
- increase hemoglobin and prevent anemia;
- strengthen the cardiovascular system;
- improve mood, normalize the emotional background;
- replenish stocks of trace elements;
- stabilize blood pressure.
Pregnant women in the second trimester are allowed to drink a little wine no more than 1 time in 2 weeks.
However, towards the end of the 2nd trimester, you can’t drink at all, since alcohol can harm the baby and provoke various pathologies.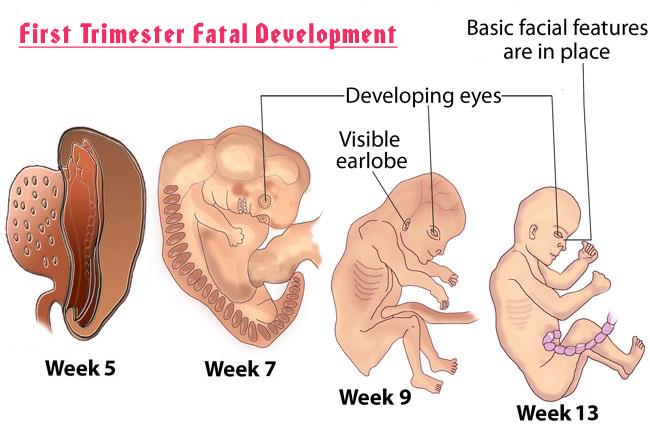 Some experts believe that the intake of alcohol by the mother during this period can lead to alcoholism in the child in the future.
Some experts believe that the intake of alcohol by the mother during this period can lead to alcoholism in the child in the future.
In addition, along with the period, the body weight of the mother and child increases, therefore, products that contribute to weight gain are limited. Red wine is one of them.
Why pregnant women shouldn't drink champagne
Despite the fact that champagne is a type of wine, it is more harmful. Champagne is quite strong and is quickly absorbed into the bloodstream due to carbon dioxide bubbles, causing almost instant intoxication.
Alcohol and pregnancy are incompatible. To make your pregnancy go smoothly, get a consultation with an obstetrician-gynecologist by phone. He will give valuable advice and recommendations.
Beer for pregnant women - is it possible or not
It is undesirable to drink beer during pregnancy, and not only because of the alcohol content in it. There are many different additives in the foamy drink - in particular, cobalt is the foam stabilizer in it. And this element is harmful to the expectant mother and her child.
There are many different additives in the foamy drink - in particular, cobalt is the foam stabilizer in it. And this element is harmful to the expectant mother and her child.
The amount of cobalt in beer exceeds the permissible norm by 10 times.
Case study:
A pregnant woman from a drinking family regularly drank beer, believing that weak alcohol could be drunk and even useful. By her own admission, sometimes she drank a little vodka. The result was the birth of a baby with fetal alcohol syndrome of the 1st degree (small head, low body weight). A full examination revealed a number of other irregularities.
Why You Shouldn't Drink Non-Alcoholic Beer While Pregnant
The so-called non-alcoholic beer contains from 0.5 to 1.5% ethanol, and drinking alcohol during pregnancy is not worth it, even such a weak one.
Any beer is also harmful because:
- contains many preservatives to ensure long-term storage;
- has a diuretic effect, undesirable for a pregnant woman;
- due to cobalt in its composition, it can cause inflammation in the esophagus and stomach.
Carbonated drinks
Doctors strongly advise pregnant women to exclude soda from the diet, as it adversely affects the stomach and increases gas formation in the intestines.
Carbonated water has a negative effect on the kidneys and gallbladder due to the content of phosphoric acid. This acid is responsible for the regulation of acidity and increases the risk of kidney and gallstone formation, especially in people with a predisposition to stone formation. During pregnancy, the load on the kidneys is already high, so it is better not to drink soda.
Alcohol in the 3rd trimester
Pregnant women in the third trimester are allowed to drink wine, but in an extremely limited amount. Half a glass of the drink can be drunk a maximum of 2 times a week.
The absence of a complete ban on alcohol is justified by the fact that by the third trimester all important processes in the fetal body have been completed, and the likelihood of a violation of its development is minimal.
FAQ
What is the best wine during pregnancy?
+
It is better for pregnant women to drink dry table wine. It helps to cope with low blood pressure, removes nausea, stimulates appetite. But for some, dry wines are too acidic, in which case they can be replaced with semi-sweet varieties.
Which is better - white or red wine during pregnancy?
+
There is not much difference here, a matter of personal preference. White wine has a positive effect on the functioning of the lungs and heart, but is inferior to red in the amount of antioxidants and the ability to increase hemoglobin. But after it, the head is less often dizzy and there is weakness in the body. Red wine reduces the risk of thrombosis, improves blood formation and helps to eliminate toxins from the body.
How about kvass?
+
Alcohol can be pregnant only at certain times described above. And in kvass, the volume of ethanol ranges from 0.3-2.5%. In addition, this drink can provoke an increase in the tone of the uterus due to active fermentation processes in the intestines and gas formation.
And in kvass, the volume of ethanol ranges from 0.3-2.5%. In addition, this drink can provoke an increase in the tone of the uterus due to active fermentation processes in the intestines and gas formation.
I drank homemade liqueur. What will happen to the child now?
+
If this happened after the start of the second trimester, and there is little alcohol consumed, then the chance of harming the baby is minimal. In addition, homemade drinks are prepared from quality products, and they do not contain harmful additives. Permissible dose - 150 ml.
Expert opinion:
Remember that alcohol and pregnancy are incompatible in principle. Even small doses of ethanol can cause irreversible changes in the development of the child. Alcohol at any stage of pregnancy has a negative impact on both the expectant mother and the baby. If you have been drinking alcohol, then in order to avoid unpleasant consequences, it is better to consult a doctor.
ALCOHOL AND PREGNANCY - Outpatient medical facility
The fact that you can not drink alcohol during pregnancy is known to most. However, different situations can arise in life: one woman is planning a pregnancy, continuing to drink alcohol on holidays in order to avoid uncomfortable questions; another drinks a glass of wine, unaware that she is already pregnant; the third during pregnancy cannot cope with the desire to drink beer, believing that "a little bit is possible." Let's look at these situations in more detail.
Alcohol consumption during pregnancy planning.
Alcohol is a toxin that adversely affects the human reproductive system. In women, alcohol consumption leads to disruption of the menstrual cycle and hormonal balance, which significantly affects the ability to conceive. There are also opinions that even episodic alcohol consumption can have a negative effect on the eggs, leading to their inferiority. Also, alcohol consumption affects the male reproductive system, significantly reducing the number of sperm capable of fertilization. Therefore, a couple planning a pregnancy should stop drinking alcohol at least 3 months in advance in order to increase the likelihood of conception.
Also, alcohol consumption affects the male reproductive system, significantly reducing the number of sperm capable of fertilization. Therefore, a couple planning a pregnancy should stop drinking alcohol at least 3 months in advance in order to increase the likelihood of conception.
Alcohol consumption in the first weeks after conception.
Without a special examination, a woman usually discovers the fact of pregnancy at 3 weeks after conception, when the next menstruation does not come. By this time, the embryo has already firmly attached to the uterine cavity and began to receive nutrition from the mother's blood. If negative factors, including alcohol, affect him before the moment of attachment, then this will lead to his rejection and death, and he will simply leave the uterus with the next menstruation. Thus, a woman may not know that she was pregnant.
According to most scientists, if alcohol did not disrupt the attachment process and the embryo continued to develop, then this would not lead to the formation of malformations in it. Thus, alcohol accidentally drunk during the first two weeks after conception will either lead to the termination of pregnancy or will not affect its further development.
Thus, alcohol accidentally drunk during the first two weeks after conception will either lead to the termination of pregnancy or will not affect its further development.
Alcohol use in early pregnancy.
As mentioned above, as early as the 3rd week after conception, the embryo begins to come into contact with maternal blood. This means that all the substances in the mother's blood come to him. including ethyl alcohol. From the 3rd to the 13th week of development, the laying of all the main systems of the body of the unborn child occurs and the effect of alcohol no longer leads to rejection and death of the embryo, but to the formation of malformations and deformities of the nervous, cardiovascular, and digestive systems.
Alcohol use in late pregnancy.
The negative impact of alcohol on the course of pregnancy is observed after the 13th week. Ethanol and its decay products lead to spasm of the vessels of the placenta and umbilical cord, impairing the delivery of oxygen and nutrients, leading to a delay in the development of the fetus, disruption of its nervous system and brain.