Burning vag early pregnancy
Vaginal Burning: Causes, Relief, Pregnancy
Vagina burning like you’re in an inferno? No your pants aren’t on fire, but something is causing your bits to burn. Ummm… so should you be worried about this vaginal burning?
The occasional itch or irritation in your lower region is completely common and generally nothing to worry about. But, if persistent burning, itching, or irritation start to become your norm, something may be up.
Burning can creep up anywhere in your vaginal area, including your:
- vaginal opening
- labia
- clitoris
Here’s why you may be feeling the burn and what to do about it.
Some of the products you use on the daily might be working against you with chemicals that can irritate your vag. This can cause burning, itching, stinging, rawness, or even pain.
You may notice symptoms right away after switching to a new product, or it may take a few uses.
Products that can cause irritation include:
- scented soaps
- detergents
- bubble baths
- menstrual pads
- scented toilet papers
What to do about it? The best way to remedy this is to stop using the products and avoid using other scented or perfumed products on your nether region.
If symptoms continue after you’ve stopped using these products, talk to your doctor to discover if something else is going on downtown.
Some products or substances that are made to be in or around your vagina can irritate your genitals and fuel that fiery feeling. This includes:
- tampons
- latex condoms
- sprays
- creams
- douches
- certain topical medications
- semen
- spermicides
What to do about it? If you have a product that you’ve just started using, stop using it to see if the burning goes away. Not sure which product that is? Try patch testing a small area to help identify the irritant.
If you discover that the culprit is your preferred method of contraception, like latex condoms, talk to your doctor. They can help you find an alternative that won’t impede on your sexy time fun.
Certain clothing can also cause burning and irritation down below, such as:
- tight underwear
- tights
- tight or fitted pants/shorts
The culprit is most likely chafing or extra moisture irritating your bits.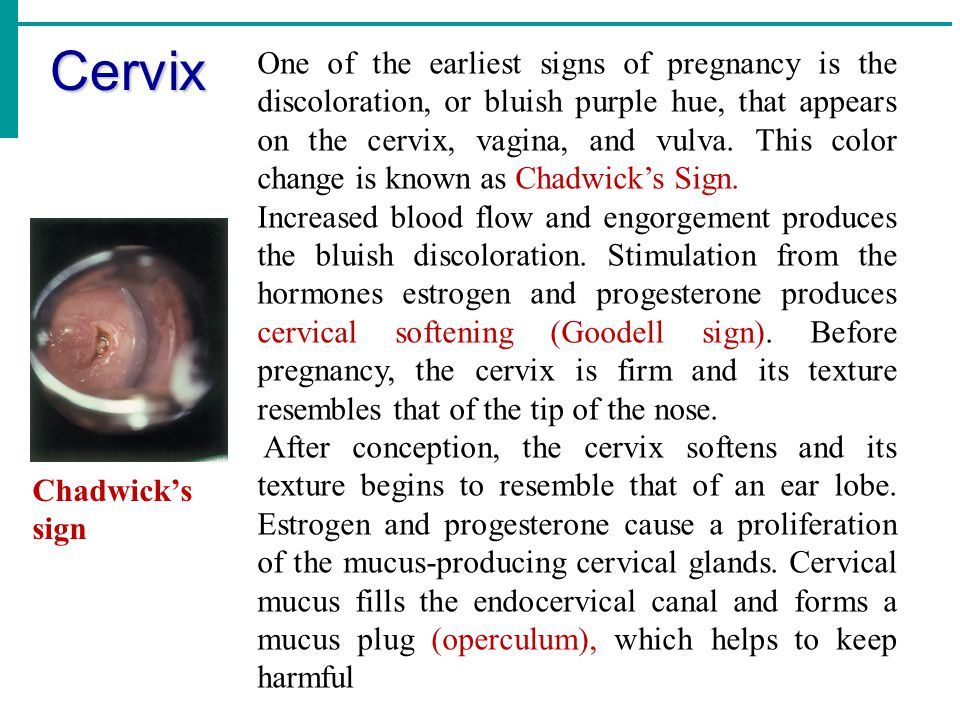 While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
What to do about it? Avoid irritation by not wearing tight clothing too often or for too long of periods of time. Be careful with wet clothing, too. Sitting too long in a wet swimsuit can lead to bacteria growth in your vagina and infections.
Bacterial vaginosis (BV) happens when there’s too much of certain bacteria in your vagina, throwing off your hoo-ha’s normal balance. And a not-so-fun fact: It’s the most common vaginal infection for women ages 15 to 44, according to the Centers for Disease Control and Prevention (CDC).
In some cases, you may not experience any symptoms of BV. For those that do, however, symptoms can include:
- burning
- itching
- pain
- white or gray vaginal discharge
- a fish-like odor, especially after sex
What to do about it? BV may disappear on its own, but you’ll usually need to see your doctor for antibiotics to clear the infection up. It’s essential that you take every dose prescribed, even if you start feeling better.
It’s essential that you take every dose prescribed, even if you start feeling better.
Yeast infections have nothing to do with quarantine bread-making, and everything to do with what happens when there’s excessive yeast growth in the vagina. Along with burning, signs of a yeast infection may be:
- soreness
- red rash outside your vagina
- itching or swelling of the vagina or the vulva
- pain when you pee or during sex
- thick, white discharge (think cottage cheese)
Nearly 75 percent of women experiencing at least one yeast infection in their lifetime. And, while the risk of getting a yeast infection is already high, it’s even higher for women who:
- are pregnant
- have diabetes
- are now or were recently on antibiotics
- are using hormonal birth control
- have a compromised immune system
What to do about it? Yeast infections can often be treated at home or with an over-the-counter (OTC) antifungal medication such as a cream, ointment, or suppository.
However, if you experience frequent yeast infections, your infection doesn’t clear up after treatment, or this is your first yeast infection ever, it’s best to see your doctor. They can confirm your diagnosis and help you determine the best treatment plan for you.
Urinary tract infections (aka UTIs) happen when bacteria gets in your urinary tract or bladder. You’ll likely experience a burning sensation when you pee, as well as other symptoms like:
- a frequent need to pee (often with little results)
- strong-smelling urine
- cloudy urine
- blood in your urine, making it red or pink
- fever or chills
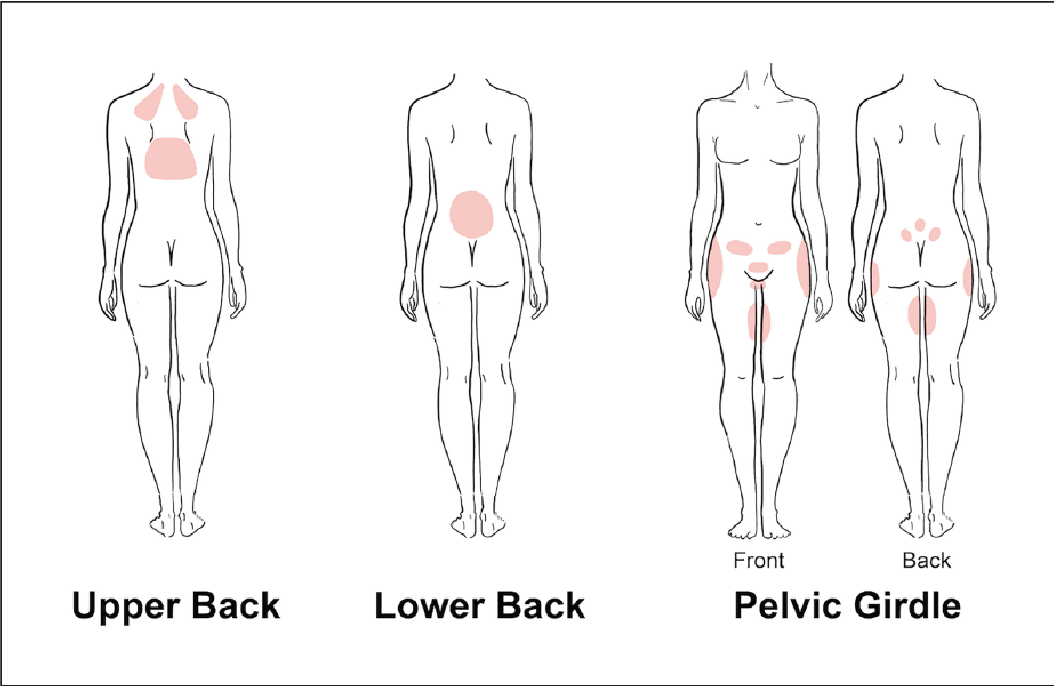
- pain in the stomach, back, or pelvic area
What to do about it? Think you have a UTI? See your doctor. They’ll be able to prescribe you antibiotics to treat your infection.
Be sure to drink plenty of fluids and to take the full course of medication, even if symptoms have disappeared. If you don’t, you risk the infection returning.
Trichomoniasis (aka trich) is an STI, and one of the most common ones in the U.S. to boot. It appears more often in women than men. Symptoms only appear in about 30 percent of cases, so most women don’t even realize they have the infection.
Those that that do experience symptoms will likely have:
- vaginal burning, irritation, and/or itching
- clear, white, yellow, or green discharge
- lower abdominal pain
- foul odors down below
- discomfort while peeing or during sex
What to do about it? You’ll need to see your doctor, as prescription antibiotics are needed to clear up the infection. Typically, only a single dose will do the trick to treat your trich. Left untreated, however, trich can cause long-term complications, as well as increase your risk of getting other STIs.
Gonorrhea is another STI where bacteria infects mucous membranes like the cervix, uterus, or fallopian tubes. It’s most common in those ages 15 to 24 and rarely causes symptoms.
When symptoms do appear, they include:
- vaginal burning or irritation
- unusual discharge
- bleeding or spotting between periods
- burning or pain when urinating
What to do about it? Gonorrhea is treated with prescription antibiotics, so a trip to the doc is necessary. In some cases, a doctor may prescribe dual therapy, where two different meds will need to be taken at the same time.
Gonorrhea can lead to serious complications if it’s left untreated, including infertility and pelvic inflammatory disease (PID).
Chlamydia is another common STI caused by bacteria. It’s often known as a “silent” infection because, much like trich, about 70 percent of those with the infection don’t experience symptoms.
Those that do exhibit symptoms will likely experience:
- burning sensations
- abnormal discharge
- bleeding between periods or during sex
- pain during urination or sex
What to do about it? Prescription antibiotics are needed to cure chlamydia, so a trip to the doctor is necessary. Health professionals are also required to report chlamydia cases in order to track the infection.
Health professionals are also required to report chlamydia cases in order to track the infection.
If left untreated, chlamydia can wreak havoc on your reproductive system, and cause permanent damage. Repeat infection is also common with chlamydia, and each time you contract the infection can increase your chances of having issues with fertility.
Genital herpes is an incurable viral infection that’s caused by skin-to-skin contact with someone who has the herpes simplex virus (HSV). According to the CDC, an estimated 1 in 6 people in the U.S. between ages 14 to 49 has genital herpes.
Symptoms may not develop right away — in fact, it could be years before the virus becomes active and symptoms appear. When symptoms do appear, they’ll likely include:
- burning, itching, or tingling sensation in the vagina
- painful sores, blisters, or ulcers
- swollen glands
- vaginal pain, especially during urination
- flu-like symptoms
- abnormal vaginal discharge
What to do about it? The herpes virus stays in your body forever; there is no cure. However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
Your doctor about can also prescribe medication to help reduce the risk of transferring genital herpes to others.
The most common STI in the U.S. is human papillomavirus, more commonly known as HPV. HPV can cause genital warts, which can appear:
- on your vulva, vagina, cervix, or anus
- in clusters or as one or two bumps
- as white or flesh-colored bumps
What to do about it? While genital warts may disappear on their own, there’s no cure for them. You can choose to have them medically removed, which can lower your risk of transmitting the infection to others. HPV is also linked to different cancers, including anal cancer and cervical cancer.
Did you get the HPV vaccine?
To reduce the risk of HPV-related diseases and infections, the CDC, American Academy of Family Physicians, and other health experts recommend that preteens receive an HPV vaccination before becoming sexually active.
A rare skin condition, lichen sclerosus causes thin, white patches to appear on the vagina — especially around the vulva. These patches can lead to permanent scarring.
Other symptoms include:
- itching or burning
- pain or discomfort
- redness
- bleeding
- blisters or sores
- painful sex
Women can develop lichen sclerosis at any age, but it’s most common in postmenopausal women.
What to do about it? To treat lichen sclerosus, you’ll need to see your doctor, who can prescribe a strong topical steroid to ease symptoms. You’ll also want to regularly see your doctor to monitor any changes in the skin or permanent complications, like scarring, or thinning of the skin.
Wait, aren’t you a little young to be worried about menopause? Premature menopause is when you go through menopause before age 40. It isn’t very common and only affects about 1 percent of women (and a lot of times it’s genetic).
During menopause your estrogen and progesterone levels get super low, and you’ll stop having a menstrual cycle. This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
Menopause can also cause symptoms like:
- hot flashes
- irritability
- insomnia
- fatigue
- reduced sex drive
- night sweats
What to do about it? Menopause can’t be stopped, but it’s symptoms can be eased. One thing your doc may do is prescribe an estrogen supplement or other hormone therapy. If hormonal supplements aren’t your cup of tea, your doctor can work with you to find the best option for you.
If sex conjures up images of burning naughty bits rather than burning passion, you’re not alone. It’s not uncommon to experience a burning sensation after and during sex.
This can generally be attributed to:
- too much friction
- not enough lubricant being used
- allergic reaction to semen
- allergic reaction to products being used (like latex condoms, toys, or scented lotions)
- PH imbalance caused by douching
- hormonal birth controls
- UTIs, STIs, or other infections
How to find relief
Working in some extra lube or some additional foreplay to make matters more slippery can help you avoid that burning feeling in the future.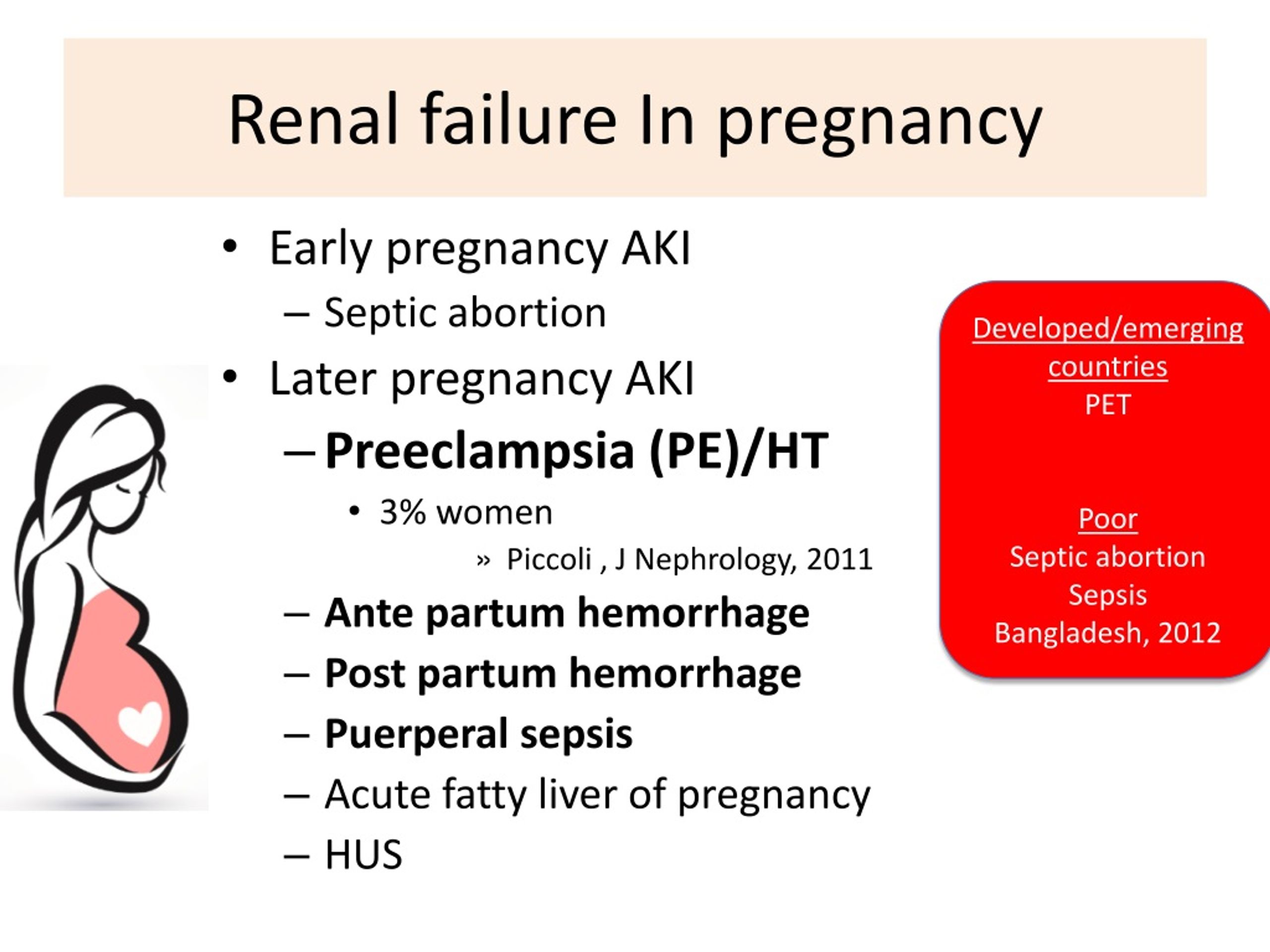
However, if sex continues to cause pain or other symptoms arise, it’s time to see the doctor. They can help figure out what’s going on and help you determine treatment or next steps.
Vaginal irritation is normal during pregnancy, and you’ll likely experience it more than once. This can be caused by a variety of reasons, including:
- increase in vaginal discharge
- vaginal dryness
- sensitivity to products
- hormonal changes
- UTIs or other bacterial infections
How to find relief
In many cases, it’s nothing to worry about, and you can ease your itch right at home by:
- taking a cool bath or using a cool compress
- using product elimination to determine the cause
- taking a bath with baking soda
Because pregnancy is a delicate time and you’re experiencing many physical changes, it’s always best to talk to your doctor if you have questions or something seems out of sorts.
If you think your symptoms are caused by an infection of any kind, talk to your doctor before taking any medications, including common OTC treatments.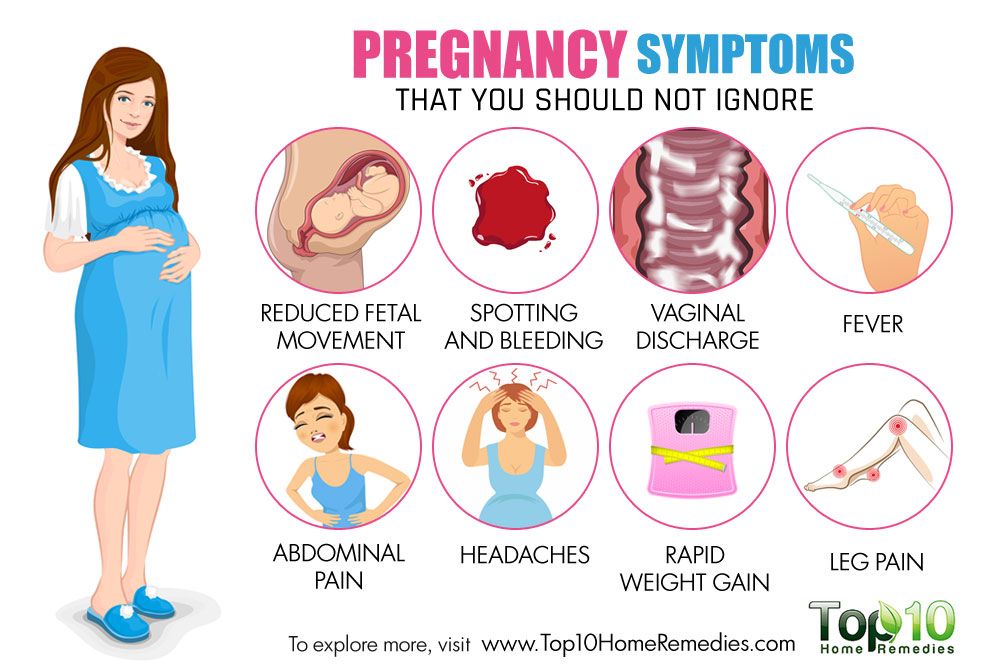 They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
Occasional itching or irritation on your vagina is normal, and there generally isn’t cause for concern. However, if you begin to experience persistent burning, increased irritation, or other symptoms that are out of the norm, there may be an underlying condition at play.
Talk to your doctor if you think something’s up (or even if you don’t… better safe than sorry!). In some cases, a simple prescription medication will make your condition disappear while others will require lifelong treatment or monitoring.
Your doctor can help identify what’s setting your bits to be on fire and help you find relief.
Vaginal Burning: Causes, Relief, Pregnancy
Vagina burning like you’re in an inferno? No your pants aren’t on fire, but something is causing your bits to burn. Ummm… so should you be worried about this vaginal burning?
The occasional itch or irritation in your lower region is completely common and generally nothing to worry about. But, if persistent burning, itching, or irritation start to become your norm, something may be up.
But, if persistent burning, itching, or irritation start to become your norm, something may be up.
Burning can creep up anywhere in your vaginal area, including your:
- vaginal opening
- labia
- clitoris
Here’s why you may be feeling the burn and what to do about it.
Some of the products you use on the daily might be working against you with chemicals that can irritate your vag. This can cause burning, itching, stinging, rawness, or even pain.
You may notice symptoms right away after switching to a new product, or it may take a few uses.
Products that can cause irritation include:
- scented soaps
- detergents
- bubble baths
- menstrual pads
- scented toilet papers
What to do about it? The best way to remedy this is to stop using the products and avoid using other scented or perfumed products on your nether region.
If symptoms continue after you’ve stopped using these products, talk to your doctor to discover if something else is going on downtown.
Some products or substances that are made to be in or around your vagina can irritate your genitals and fuel that fiery feeling. This includes:
- tampons
- latex condoms
- sprays
- creams
- douches
- certain topical medications
- semen
- spermicides
What to do about it? If you have a product that you’ve just started using, stop using it to see if the burning goes away. Not sure which product that is? Try patch testing a small area to help identify the irritant.
If you discover that the culprit is your preferred method of contraception, like latex condoms, talk to your doctor. They can help you find an alternative that won’t impede on your sexy time fun.
Certain clothing can also cause burning and irritation down below, such as:
- tight underwear
- tights
- tight or fitted pants/shorts
The culprit is most likely chafing or extra moisture irritating your bits. While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
While you may not notice any unpleasant sensations the first time you wear something new, symptoms may start to sneak up on you as you wear an item more.
What to do about it? Avoid irritation by not wearing tight clothing too often or for too long of periods of time. Be careful with wet clothing, too. Sitting too long in a wet swimsuit can lead to bacteria growth in your vagina and infections.
Bacterial vaginosis (BV) happens when there’s too much of certain bacteria in your vagina, throwing off your hoo-ha’s normal balance. And a not-so-fun fact: It’s the most common vaginal infection for women ages 15 to 44, according to the Centers for Disease Control and Prevention (CDC).
In some cases, you may not experience any symptoms of BV. For those that do, however, symptoms can include:
- burning
- itching
- pain
- white or gray vaginal discharge
- a fish-like odor, especially after sex
What to do about it? BV may disappear on its own, but you’ll usually need to see your doctor for antibiotics to clear the infection up. It’s essential that you take every dose prescribed, even if you start feeling better.
It’s essential that you take every dose prescribed, even if you start feeling better.
Yeast infections have nothing to do with quarantine bread-making, and everything to do with what happens when there’s excessive yeast growth in the vagina. Along with burning, signs of a yeast infection may be:
- soreness
- red rash outside your vagina
- itching or swelling of the vagina or the vulva
- pain when you pee or during sex
- thick, white discharge (think cottage cheese)
Nearly 75 percent of women experiencing at least one yeast infection in their lifetime. And, while the risk of getting a yeast infection is already high, it’s even higher for women who:
- are pregnant
- have diabetes
- are now or were recently on antibiotics
- are using hormonal birth control
- have a compromised immune system
What to do about it? Yeast infections can often be treated at home or with an over-the-counter (OTC) antifungal medication such as a cream, ointment, or suppository.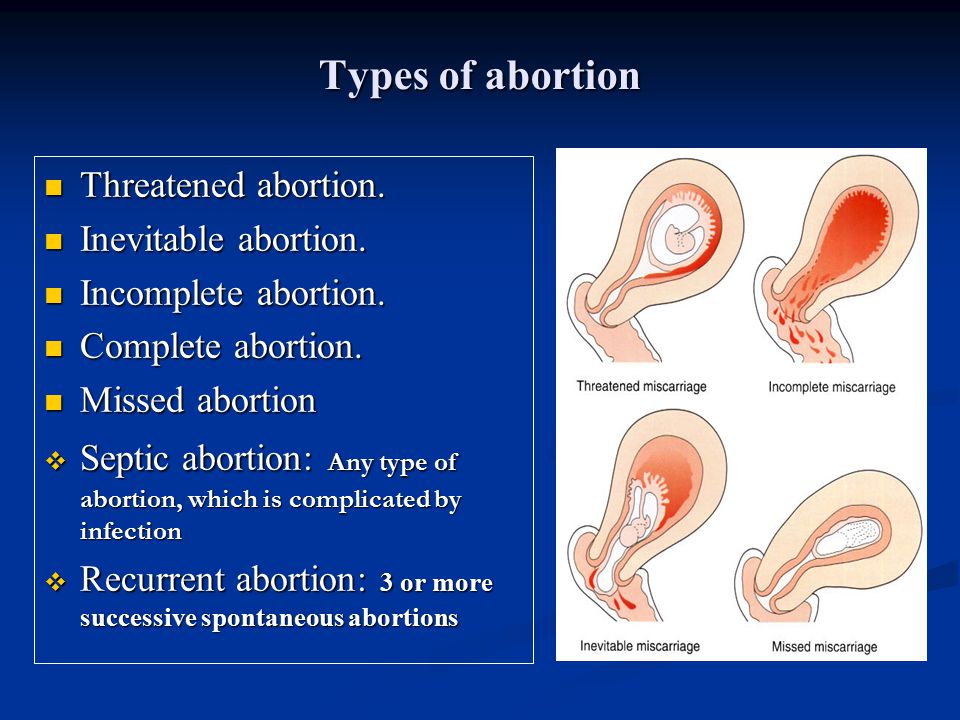
However, if you experience frequent yeast infections, your infection doesn’t clear up after treatment, or this is your first yeast infection ever, it’s best to see your doctor. They can confirm your diagnosis and help you determine the best treatment plan for you.
Urinary tract infections (aka UTIs) happen when bacteria gets in your urinary tract or bladder. You’ll likely experience a burning sensation when you pee, as well as other symptoms like:
- a frequent need to pee (often with little results)
- strong-smelling urine
- cloudy urine
- blood in your urine, making it red or pink
- fever or chills
- pain in the stomach, back, or pelvic area
What to do about it? Think you have a UTI? See your doctor. They’ll be able to prescribe you antibiotics to treat your infection.
Be sure to drink plenty of fluids and to take the full course of medication, even if symptoms have disappeared. If you don’t, you risk the infection returning.
Trichomoniasis (aka trich) is an STI, and one of the most common ones in the U.S. to boot. It appears more often in women than men. Symptoms only appear in about 30 percent of cases, so most women don’t even realize they have the infection.
Those that that do experience symptoms will likely have:
- vaginal burning, irritation, and/or itching
- clear, white, yellow, or green discharge
- lower abdominal pain
- foul odors down below
- discomfort while peeing or during sex
What to do about it? You’ll need to see your doctor, as prescription antibiotics are needed to clear up the infection. Typically, only a single dose will do the trick to treat your trich. Left untreated, however, trich can cause long-term complications, as well as increase your risk of getting other STIs.
Gonorrhea is another STI where bacteria infects mucous membranes like the cervix, uterus, or fallopian tubes. It’s most common in those ages 15 to 24 and rarely causes symptoms.
When symptoms do appear, they include:
- vaginal burning or irritation
- unusual discharge
- bleeding or spotting between periods
- burning or pain when urinating
What to do about it? Gonorrhea is treated with prescription antibiotics, so a trip to the doc is necessary. In some cases, a doctor may prescribe dual therapy, where two different meds will need to be taken at the same time.
Gonorrhea can lead to serious complications if it’s left untreated, including infertility and pelvic inflammatory disease (PID).
Chlamydia is another common STI caused by bacteria. It’s often known as a “silent” infection because, much like trich, about 70 percent of those with the infection don’t experience symptoms.
Those that do exhibit symptoms will likely experience:
- burning sensations
- abnormal discharge
- bleeding between periods or during sex
- pain during urination or sex
What to do about it? Prescription antibiotics are needed to cure chlamydia, so a trip to the doctor is necessary. Health professionals are also required to report chlamydia cases in order to track the infection.
Health professionals are also required to report chlamydia cases in order to track the infection.
If left untreated, chlamydia can wreak havoc on your reproductive system, and cause permanent damage. Repeat infection is also common with chlamydia, and each time you contract the infection can increase your chances of having issues with fertility.
Genital herpes is an incurable viral infection that’s caused by skin-to-skin contact with someone who has the herpes simplex virus (HSV). According to the CDC, an estimated 1 in 6 people in the U.S. between ages 14 to 49 has genital herpes.
Symptoms may not develop right away — in fact, it could be years before the virus becomes active and symptoms appear. When symptoms do appear, they’ll likely include:
- burning, itching, or tingling sensation in the vagina
- painful sores, blisters, or ulcers
- swollen glands
- vaginal pain, especially during urination
- flu-like symptoms
- abnormal vaginal discharge
What to do about it? The herpes virus stays in your body forever; there is no cure. However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
However, your doctor can prescribe antiviral medication to ease symptoms, reduce your risk of outbreak, and shorten the length of any flare-ups.
Your doctor about can also prescribe medication to help reduce the risk of transferring genital herpes to others.
The most common STI in the U.S. is human papillomavirus, more commonly known as HPV. HPV can cause genital warts, which can appear:
- on your vulva, vagina, cervix, or anus
- in clusters or as one or two bumps
- as white or flesh-colored bumps
What to do about it? While genital warts may disappear on their own, there’s no cure for them. You can choose to have them medically removed, which can lower your risk of transmitting the infection to others. HPV is also linked to different cancers, including anal cancer and cervical cancer.
Did you get the HPV vaccine?
To reduce the risk of HPV-related diseases and infections, the CDC, American Academy of Family Physicians, and other health experts recommend that preteens receive an HPV vaccination before becoming sexually active.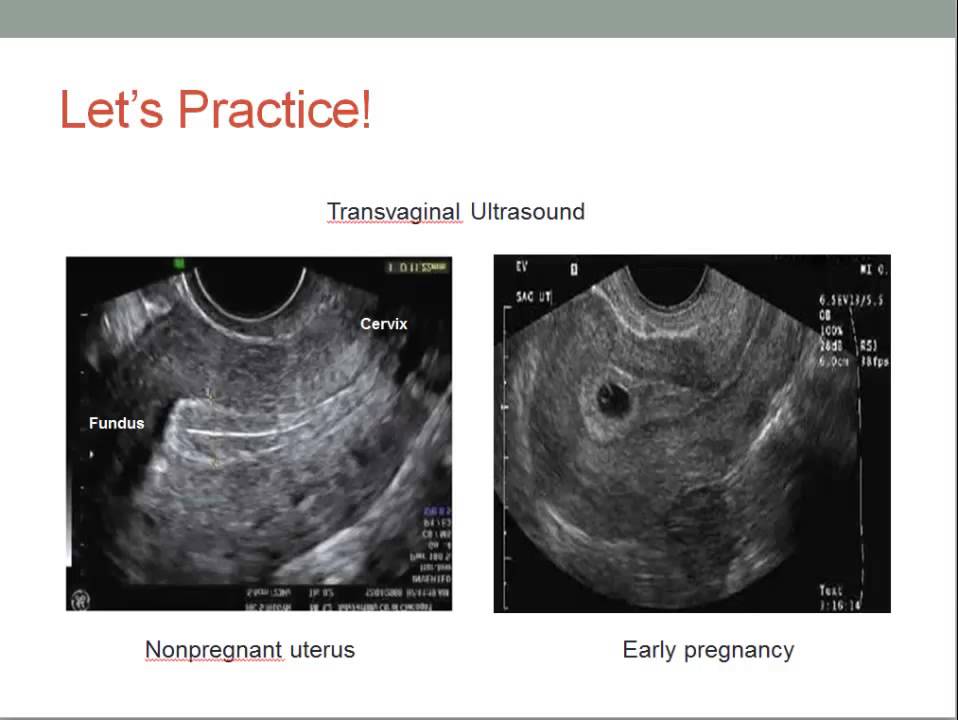
A rare skin condition, lichen sclerosus causes thin, white patches to appear on the vagina — especially around the vulva. These patches can lead to permanent scarring.
Other symptoms include:
- itching or burning
- pain or discomfort
- redness
- bleeding
- blisters or sores
- painful sex
Women can develop lichen sclerosis at any age, but it’s most common in postmenopausal women.
What to do about it? To treat lichen sclerosus, you’ll need to see your doctor, who can prescribe a strong topical steroid to ease symptoms. You’ll also want to regularly see your doctor to monitor any changes in the skin or permanent complications, like scarring, or thinning of the skin.
Wait, aren’t you a little young to be worried about menopause? Premature menopause is when you go through menopause before age 40. It isn’t very common and only affects about 1 percent of women (and a lot of times it’s genetic).
During menopause your estrogen and progesterone levels get super low, and you’ll stop having a menstrual cycle. This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
This can lead to vaginal dryness and burning. Plus, the burning is often worse during sex (bring out the extra lube!).
Menopause can also cause symptoms like:
- hot flashes
- irritability
- insomnia
- fatigue
- reduced sex drive
- night sweats
What to do about it? Menopause can’t be stopped, but it’s symptoms can be eased. One thing your doc may do is prescribe an estrogen supplement or other hormone therapy. If hormonal supplements aren’t your cup of tea, your doctor can work with you to find the best option for you.
If sex conjures up images of burning naughty bits rather than burning passion, you’re not alone. It’s not uncommon to experience a burning sensation after and during sex.
This can generally be attributed to:
- too much friction
- not enough lubricant being used
- allergic reaction to semen
- allergic reaction to products being used (like latex condoms, toys, or scented lotions)
- PH imbalance caused by douching
- hormonal birth controls
- UTIs, STIs, or other infections
How to find relief
Working in some extra lube or some additional foreplay to make matters more slippery can help you avoid that burning feeling in the future.
However, if sex continues to cause pain or other symptoms arise, it’s time to see the doctor. They can help figure out what’s going on and help you determine treatment or next steps.
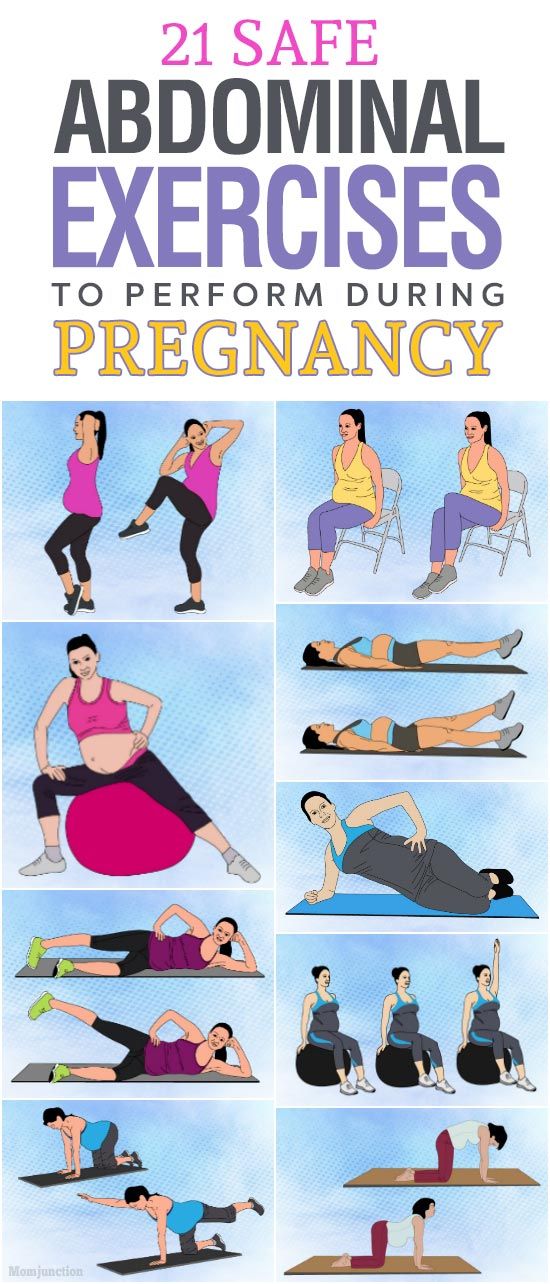
Vaginal irritation is normal during pregnancy, and you’ll likely experience it more than once. This can be caused by a variety of reasons, including:
- increase in vaginal discharge
- vaginal dryness
- sensitivity to products
- hormonal changes
- UTIs or other bacterial infections
How to find relief
In many cases, it’s nothing to worry about, and you can ease your itch right at home by:
- taking a cool bath or using a cool compress
- using product elimination to determine the cause
- taking a bath with baking soda
Because pregnancy is a delicate time and you’re experiencing many physical changes, it’s always best to talk to your doctor if you have questions or something seems out of sorts.
If you think your symptoms are caused by an infection of any kind, talk to your doctor before taking any medications, including common OTC treatments. They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
They can determine the proper medications or treatment plan to ensure there’s no impact on your pregnancy.
Occasional itching or irritation on your vagina is normal, and there generally isn’t cause for concern. However, if you begin to experience persistent burning, increased irritation, or other symptoms that are out of the norm, there may be an underlying condition at play.
Talk to your doctor if you think something’s up (or even if you don’t… better safe than sorry!). In some cases, a simple prescription medication will make your condition disappear while others will require lifelong treatment or monitoring.
Your doctor can help identify what’s setting your bits to be on fire and help you find relief.
Itching and burning in the vagina during pregnancy, causes of itching during pregnancy
Pregnancy is undoubtedly the most significant period in the life of every woman. Despite this, it does not always proceed as one would like - without complications and unpleasant diseases. The most common symptoms that occur in women are itching and burning in the vagina . During pregnancy, they can occur both separately and together.
The most common symptoms that occur in women are itching and burning in the vagina . During pregnancy, they can occur both separately and together.
Burning and itching in the vagina during pregnancy is observed in about every second woman. This may be due to both internal and external factors. However, in no case should you self-medicate, or hope that itching and burning in the vagina during pregnancy will go away on their own. These symptoms can signal serious illnesses, so it is advisable in this case to visit your gynecologist. nine0005
In this article we will tell you what causes burning and itching in the vagina during pregnancy, what diseases can accompany and how to get rid of these symptoms.
During pregnancy itching appeared in the vagina. Causes of itching
Why does itching occur in the vagina during pregnancy? The reasons for this symptom may be different. First of all, internal causes play a role, they are directly related to pregnancy - reduced immunity and changes in hormonal levels.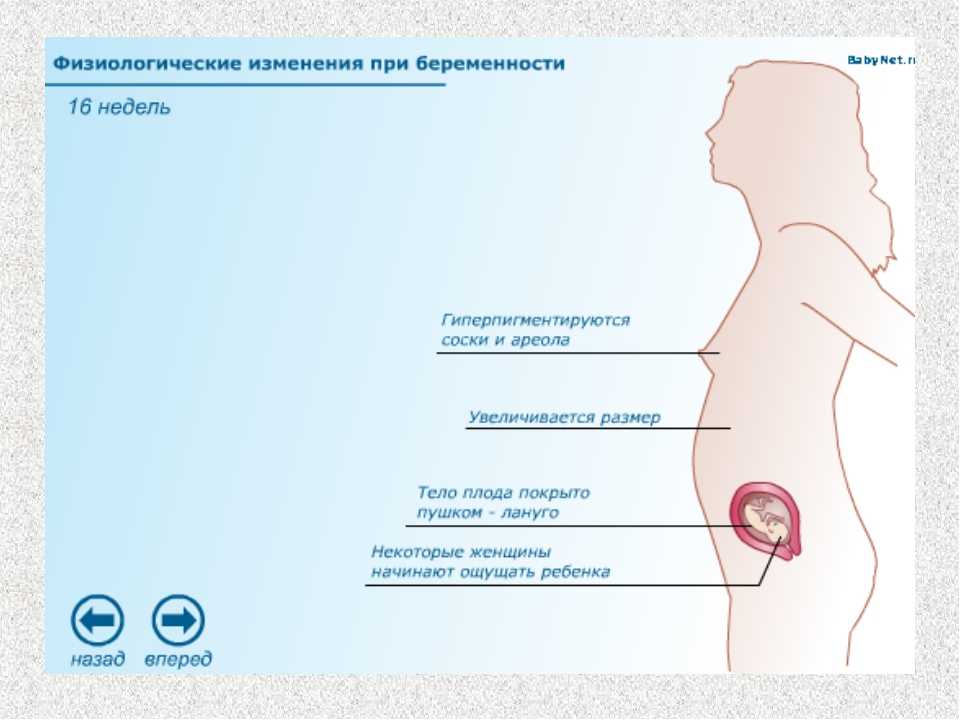 Reduced immunity increases the risk of various diseases - candidiasis, herpes, dysbacteriosis, chlamydia. Also, during pregnancy, already existing diseases of the organs of the reproductive system - colpitis, vaginitis - which can also often cause itching, can become aggravated. nine0005
Reduced immunity increases the risk of various diseases - candidiasis, herpes, dysbacteriosis, chlamydia. Also, during pregnancy, already existing diseases of the organs of the reproductive system - colpitis, vaginitis - which can also often cause itching, can become aggravated. nine0005
But if itching appeared during pregnancy in the vagina, the reasons can also be external - synthetic underwear, tight clothing, frequent douching, constant use of soap, shower gels that dry the mucous membrane.
How to eliminate itching and burning of the vagina during pregnancy?
To eliminate itching and burning in the vagina during pregnancy, you first need to find out the cause of these unpleasant symptoms. If it's all about intimate hygiene products, or underwear, then it will be enough to change them to relieve the burning sensation and itching of the vagina during pregnancy. Instead of soap and shower gel, you can use ordinary boiled water, or a decoction of chamomile, synthetic linen should be replaced with natural. nine0005
nine0005
But if burning and itching of the vagina during pregnancy are a manifestation of diseases, then etiological rather than symptomatic treatment is required first of all. However, only certain drugs are allowed during pregnancy, which greatly complicates the treatment process. The advantage is given to topical preparations, such as Gynoflor and Fluomizin. But if itching and burning in the vagina during pregnancy do not go away, systemic drugs are also used.
How to prevent burning and itching in the vagina during pregnancy. Prevention first! nine0011
How to eliminate itching, burning in the vagina? Pregnancy is a contraindication to the use of many drugs, which makes treatment a little difficult. Therefore, it is best to think about the likelihood of such symptoms in advance and carry out their prevention even before pregnancy!
To choose the right method of prevention, you need to know what causes itching, burning in the vagina. Pregnancy leads to a decrease in a woman's immunity, so it would be advisable to take vitamin and mineral preparations, tonics. To prevent dysbacteriosis, which is often the cause of itching and burning in the vagina, probiotics are often recommended, the introduction of more fermented milk products into the diet. Vaginal suppositories containing various bacteria (lactobacilli, bifidobacteria, acidobacteria), lactic acid are also often prescribed by gynecologists to prevent itching in the vagina. nine0005
To prevent dysbacteriosis, which is often the cause of itching and burning in the vagina, probiotics are often recommended, the introduction of more fermented milk products into the diet. Vaginal suppositories containing various bacteria (lactobacilli, bifidobacteria, acidobacteria), lactic acid are also often prescribed by gynecologists to prevent itching in the vagina. nine0005
Pregnancy is the most important and wonderful period in the life of every woman. But in order not to be spoiled by diseases, it is better to engage in their prevention than treatment in the future!
Buy
in your city
COLPITIS DURING PREGNANCY
During pregnancy, a woman, as a rule, takes special care of her health and reacts anxiously to every unusual symptom. nine0005
Unusual discharge and discomfort in the genital area are often the cause of the expectant mother's panic. Such a complex of symptoms most likely indicates the development of a pathological process, which in medicine is called vaginitis or colpitis. In pregnant women, this condition is noted especially often against the background of a decrease in immunity, hormonal changes in the body and high loads on all organs and systems of a woman.
In pregnant women, this condition is noted especially often against the background of a decrease in immunity, hormonal changes in the body and high loads on all organs and systems of a woman.
Vaginitis during pregnancy is a good reason to immediately contact a gynecologist and start treating this dangerous pathology. Diagnose the disease and determine how to treat colpitis during pregnancy without harming the mother and baby, qualified gynecologists will prompt. nine0005
Symptoms of colpitis during pregnancy
First of all, it should be determined that vaginitis or colpitis is an inflammatory disease that involves the mucous membranes of the vagina. The inflamed walls of the vagina swell and undergo hyperemia. Also, single hemorrhages are noted on the surface of the vaginal tissues. If the inflammation does not spread beyond the vagina, the woman does not notice visual manifestations of the disease, while in some cases the pathological process affects the external genitalia. In this case, inflammation can be seen with the naked eye. nine0005
In this case, inflammation can be seen with the naked eye. nine0005
The characteristic signs of colpitis during pregnancy do not differ from the symptoms of a non-pregnant woman:
- itching and burning in the vaginal area - the inflammatory process irritates the delicate mucous membranes, which causes discomfort and sometimes pain in the vaginal walls;
- pain in the lower abdomen - this symptom is especially frightening for pregnant women, but it is not associated with the tone of the uterus, as many assume, but with inflammation of the tissues; nine0005
- the appearance of specific discharge - the discharge during colpitis during pregnancy is very abundant and may have a different color and consistency. Most often, a woman visually notes a white curdled discharge, resembling a characteristic sign of thrush, but sometimes the vaginal discharge acquires a putrid odor and is greenish-yellow in color. This indicates the specific nature of the pathogen and requires immediate medical advice;
- swelling and redness of the genital organs - patients often notice hyperemia and swelling of the labia and clitoris, which become more sensitive and cause discomfort to the woman.
Acute vaginitis during pregnancy is accompanied by severe symptoms, which should make the patient seek professional help. This will help protect the child from possible negative consequences.
Causes and types of vaginitis during pregnancy
Inflammation of the mucous membranes of the vagina is usually of an infectious nature. This becomes possible due to vaginal dysbacteriosis, which often accompanies the period of pregnancy. Hormonal changes and high loads on all organs of the expectant mother cause a decrease in the body's defenses, which provokes an infectious and inflammatory process. In this case, the causative agent of the pathology can act as a bacterial flora that has penetrated into the body from the outside during sexual intercourse or in the household way, and that makes up the normal microflora of the vagina. The most likely infectious agents of colpitis in pregnant women include streptococci, fungi of the genus Candida, E. coli, trichomonas, ureaplasma, mycoplasma, etc.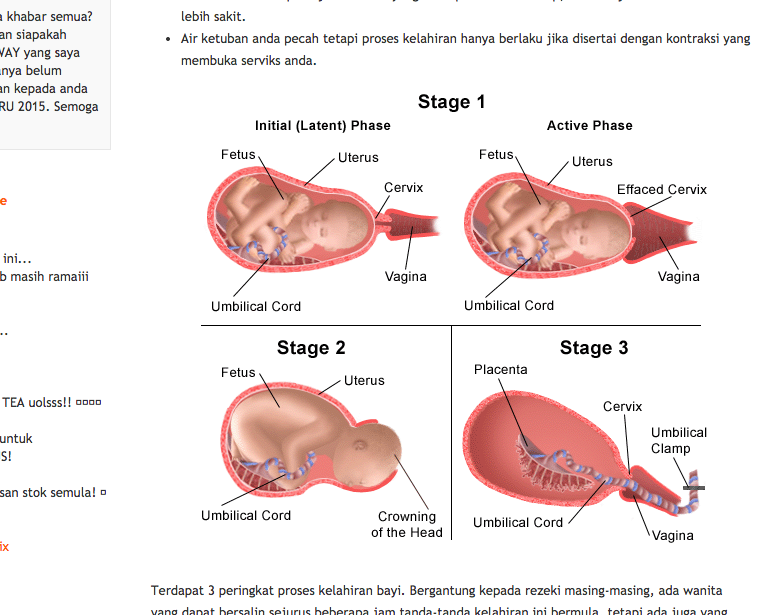
Interestingly, depending on the cause of the development of disease, its symptoms and manifestations may differ:
- candidal colpitis - accompanied by profuse cheesy discharge and severe itching of the genital organs, which manifests itself even at rest;
- emphysematous colpitis - a very common type of vaginitis in pregnant women. Pathology is accompanied by the formation of small watery vesicles on the surface of the mucous membranes of the genital organs. This form of colpitis resolves on its own in 2-3 weeks after childbirth; nine0005
- Trichomonas colpitis - a very dangerous form of pathology that develops when Trichomonas enter the vaginal environment. Infection occurs during intercourse or when using personal hygiene items shared with the carrier (towel, washcloth, etc.). It is manifested by characteristic putrefactive secretions with a sharp unpleasant odor.
Concomitant conditions for the development of colpitis in a pregnant woman, in addition to a decrease in immunity, can be allergic reactions, microtrauma of the vagina, non-observance of personal hygiene, the presence of chronic diseases. nine0005
nine0005
Colpitis during pregnancy: consequences for the child
Inflammation of the mucous membranes of the vagina poses a threat not only to the health of the expectant mother, but also to the baby. The ascending route of infection can lead to pregnancy abnormalities such as polyhydramnios, premature birth, and infection of the amniotic fluid. Vaginitis is especially dangerous during childbirth, when the baby passes through an infected maternal birth canal. In this moment there is a high probability of infection newborn.
Interestingly, colpitis after pregnancy can go away on its own, but this happens relatively rarely. The development of colpitis after childbirth is most often provoked by trauma to the vaginal membranes during delivery. In connection with this fact, doctors recommend abstaining from sexual activity for the first weeks after childbirth. Violating this prohibition, a woman increases the risk of developing colpitis after childbirth.