Ease contraction pain
Ouch! Managing Labor Pains
We’ve all seen those movie scenes when a woman in a wheelchair is being rushed through the hospital doors after her water breaks. Cut to the mother-to-be screaming at the top of her lungs while pushing the baby out. Then, the money shot of the new parents staring adoringly at their newborn. But in real life, childbirth can take a lot longer than a few minutes of edited screen time, and there are a variety of ways to manage the pain that comes with bringing a baby into the world.
Erica Vu, certified nurse midwife at UC San Diego Health, talks about the stages of labor, the pain associated with the process and the interventions — both medicated and non-medicated — that are available.
How does a pregnant woman know when she is in labor?
Labor is very mysterious and one can never exactly know when it will start. Most women start to have various labor signs a few hours or weeks even before labor officially begins. These may include:
- Increased vaginal discharge — brown, pink or increased mucous discharge in general is a good sign the cervix is starting to ripen and the mucous plug, the sealed entrance to the uterus, is released.
- Many women notice more pelvis pressure as the baby’s head descends in her pelvis. Some call this “lightening” and it can happen weeks before or just as labor is starting.
- Some women start to have more nausea and loose stools or even diarrhea as the body is preparing for labor.
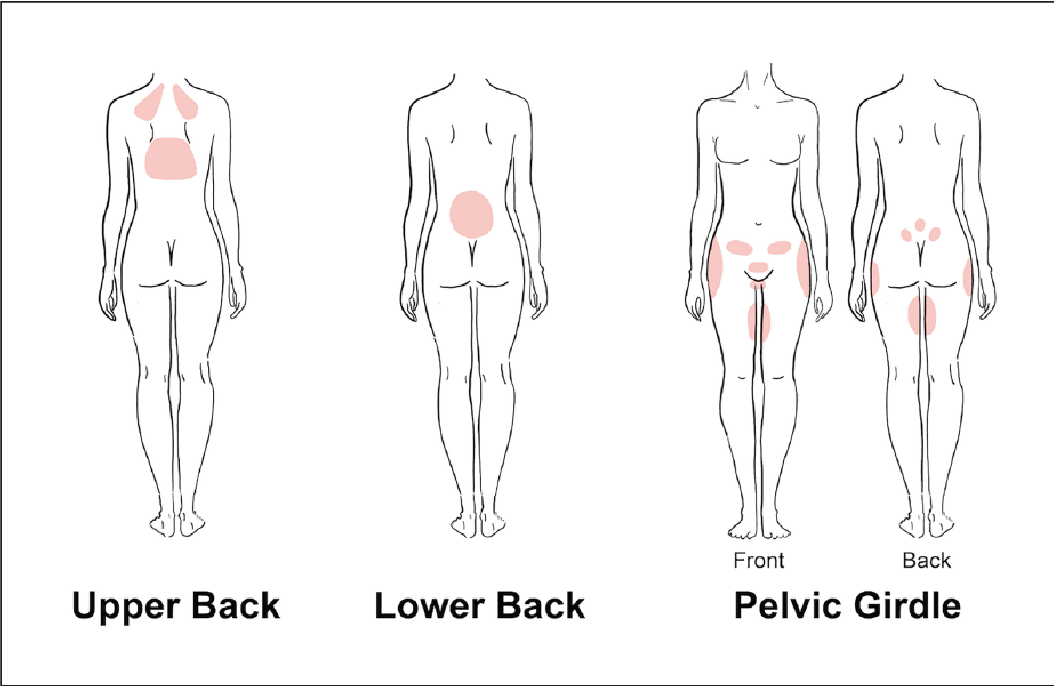
- The most common sign of labor is the increase in cramping associated with abdomen tightening or Braxton hicks. These early contractions usually start in the lower abdomen/pubic area and radiate towards the lower back. The frequency and duration of these start to increase and become more regular and rhythmic. At times, these contractions can start and increase rapidly, but for most, this can take several hours or even several days. We time the contractions from the start of one to the start of the next contraction. When they are still irregular and more than five minutes apart, most women are still in the cervical ripening/very early labor stage. These irregular contractions may even slow down or stop to give the mom’s a break.
 When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
What are the stages of labor and the pain associated with each stage?
The first stage of labor is cervical dilation, or the opening of the cervix, from 0 to 10 centimeters. Early labor is when the cervix starts to dilate from closed to five centimeters with regular contractions. Early labor contractions tend to be a bit shorter in duration (60 seconds or less) and more menstrual like-cramping in the lower abdomen and back. Early labor can take several hours or even a day or more.
When the contractions intensify, include the upper abdomen and are around two to three minutes apart, active labor is most likely starting, which is the stage from 6 to 10 centimeters. Active labor contractions are a lot stronger, longer (one to two minutes in duration) and almost always necessitate more focus, breathing and position changes/labor support.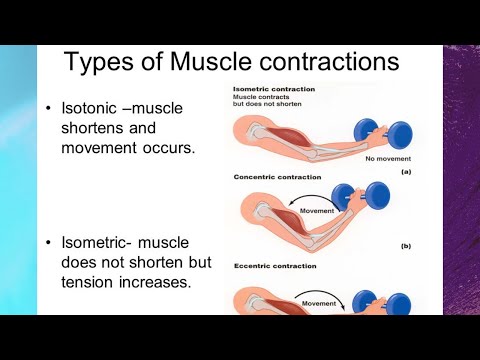 Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Once women get to 10 centimeters, the second stage of labor starts and pushing begins until the baby is delivered. This can take minutes to hours depending on the baby’s position, maternal effort and anesthesia interventions.
The third stage of labor is when the baby is out and the placenta is delivered.
What type of non-medicated interventions does UC San Diego Health provide for labor pain?
Still of Katherine Heigl and Seth Rogen from Universal Picture's Knocked Up.
Multiple position changes: Walking, lunges, squats, birthing balls, birthing stools and using Rebozos (a fabric shawl originally from Mexico that when placed appropriately can help to lift lower abdomen weight off the pubic bone, squeeze hips with back labor or help during the pushing stage by pulling on the fabric in different positions both sitting, squatting or standing). All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
Doulas: Women can hire private doulas or ask for one of our volunteer Hearts & Hands Program. Doulas are beneficial in so many ways, but specifically they give continuous non-medical labor support, including help with breathing techniques, counter pressure, position changes and massage and can be an advocate for your preference of labor process and birth.
Hydrotherapy (Labor tubs): Buoyancy can help with freedom of movement during contractions. Warm water helps to relax between contractions, eases body aches, including back aces, improves circulation and is a safe and effective form of pain relief.
Showers: Warm water helps with relaxation and decreases maternal tension during the peak of the contractions. Partners are invited to join to help with support.
Partners are invited to join to help with support.
Waterproof Wireless Monitors: These allow laboring women to be in the shower for pain relief while still allowing the benefits of hydrotherapy and close monitoring of the baby. The wireless monitors also allow women to change positions easily and walk freely about in their rooms or down the hallways if they so desire.
What type of medicated interventions does UC San Diego Health provide for labor pain?
Nitrous Oxide: Nitrous is a gas women breathe in through a mask during contractions. Women are still aware of the contractions, but the nitrous helps to decrease anxiety during them. Some women may experience nausea or dizziness initially but that usually resolves in a few minutes. This intervention allows freedom of movement, such as standing or sitting on a birthing ball, to help the baby descend down the birthing canal. Women can use nitrous as the only form of pain relief or it can also be used as a bridge to other forms of pain relief as labor progresses. It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
Intravenous Pain Relief: Narcotics or opioids help to relax the mind and body during the peak of the contractions. These help to decrease the sensations of pain, and depending on the stage of labor, may even allow the woman to rest and sleep a bit. It does cross over to the baby through the placenta but in time, just like the mother, it wears off and has little side effects. Some women feel initial dizziness and nausea as well but that often resolves with time. We often combine the narcotic with an anti-emetic (anti-nausea) medication to help but also to prolong the duration of the pain relief. There are different types of narcotics used for different stages of labor to decrease side effects in the newborn in case of a quick delivery.
Regional Anesthesia (Epidurals): This is a pain relief method that decreases pain sensations from the abdomen and below by placing a small tube into in an area surrounding the spinal cord in the lower back and is connected to a pump. The medicine is continuously infusing during the course of labor while women remain awake and alert. Most women do not feel the majority of the pain sensations of contractions, but some will feel the pressure of the baby descending in the pelvis, which helps women to push when ready. Women are not allowed to walk with epidurals but are able to change positions in bed.
Learn more about labor pain management options at UC San Diego Health.
About UC San Diego Health Midwives
To learn more about the featured medical specialties, please visit:
- Pregnancy and Birth Care
Dealing With Pain During Childbirth (for Parents)
Learning all you can about labor and delivery is one of the best ways to help you manage the pain of childbirth when the time comes.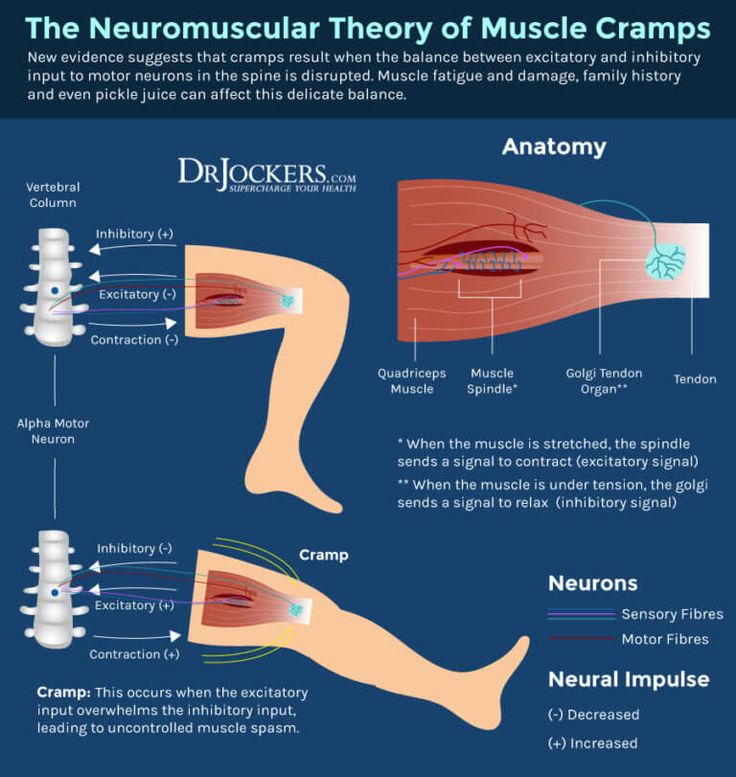
Pain During Labor and Delivery
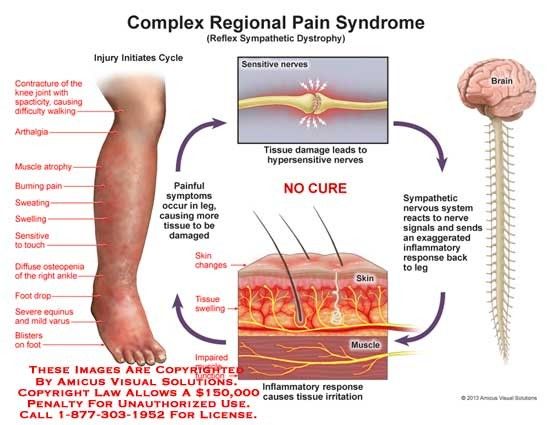
Pain during labor is caused by contractions of the muscles of the uterus and by pressure on the cervix. This pain can be felt as strong cramping in the abdomen, groin, and back, as well as an achy feeling. Some women experience pain in their sides or thighs as well.
Other causes of pain during labor include pressure on the bladder and bowels by the baby's head and the stretching of the birth canal and vagina.
Pain during labor is different for every woman. It varies widely from woman to woman and even from pregnancy to pregnancy.
It's often not the pain of each contraction on its own that women find the hardest, but the fact that the contractions keep coming — and that as labor progresses, there is less and less time between contractions to relax.
Preparing Yourself
To help with pain during labor, here are some things you can start doing before or during your pregnancy:
Regular and reasonable exercise (that your doctor says is OK) can help strengthen your muscles and prepare your body for the stress of labor. Exercise also can increase your endurance, which will come in handy if you have a long labor. The important thing to remember with any exercise is not to overdo it — and this is especially true if you're pregnant. Talk to your doctor about what he or she considers to be a safe exercise plan for you.
Exercise also can increase your endurance, which will come in handy if you have a long labor. The important thing to remember with any exercise is not to overdo it — and this is especially true if you're pregnant. Talk to your doctor about what he or she considers to be a safe exercise plan for you.
If you and your partner attend childbirth classes, you'll learn different techniques for handling pain, from visualization to stretches designed to strengthen the muscles that support your uterus. The two most common childbirth philosophies in the United States are the Lamaze technique and the Bradley method.
The Lamaze technique is the most widely used method in the United States. The Lamaze philosophy teaches that birth is a normal, natural, and healthy process and that women should be empowered to approach it with confidence. Lamaze classes educate women about the ways they can decrease their perception of pain, such as through relaxation techniques, breathing exercises, distraction, or massage by a supportive coach. Lamaze takes a neutral position toward pain medicine, encouraging women to make an informed decision about whether it's right for them.
Lamaze takes a neutral position toward pain medicine, encouraging women to make an informed decision about whether it's right for them.
The Bradley method (also called Husband-Coached Birth) emphasizes a natural approach to birth and the active participation of the baby's father as birth coach. A major goal of this method is the avoidance of medicines unless absolutely necessary. The Bradley method also focuses on good nutrition and exercise during pregnancy and relaxation and deep-breathing techniques as a method of coping with labor. Although the Bradley method advocates a medicine-free birth experience, the classes do discuss unexpected complications or situations, like emergency cesarean sections.
Medicine-free ways to handle pain during labor include:
- hypnosis
- yoga
- meditation
- walking
- massage or counterpressure
- changing position
- taking a bath or shower
- listening to music
- distracting yourself by counting or performing an activity that keeps your mind otherwise occupied
Pain Medicines
A variety of pain medicines can be used during labor and delivery, depending on the situation.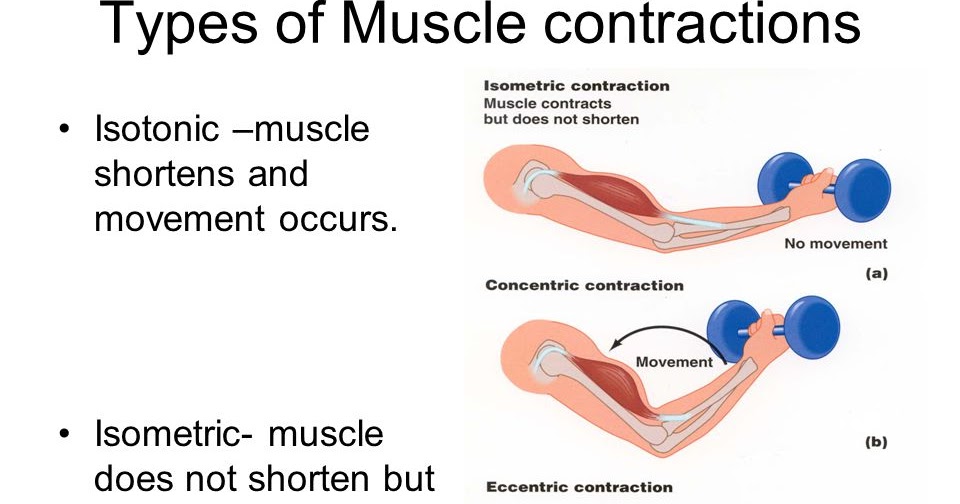 Many women rely on such medicines, and it can be a huge relief when pain is quickly eased and energy can be focused on getting through the contractions. Talk to your health care provider about the risks and benefits of each type of medicine.
Many women rely on such medicines, and it can be a huge relief when pain is quickly eased and energy can be focused on getting through the contractions. Talk to your health care provider about the risks and benefits of each type of medicine.
Analgesics. Analgesics ease pain, but don't numb it completely. They don’t affect sensation or muscle movement. They can be given many ways. If they are given intravenously (through an IV into a vein) or through a shot into a muscle, they can affect the whole body. These medicines can cause side effects in the mother, including drowsiness and nausea. They also can have effects on the baby.
Regional anesthesia. This is what most women think of when they consider pain medicine during labor. By blocking the feeling from specific regions of the body, these methods can be used for pain relief in both vaginal and cesarean section deliveries.
Epidurals, a form of local anesthesia, relieve most of the pain from the entire body below the belly button, including the vaginal walls, during labor and delivery. An epidural involves medicine given by an anesthesiologist through a thin, tube-like catheter that's inserted in the woman's lower back. The amount of medicine can be increased or decreased according to a woman's needs. Very little medicine reaches the baby, so usually there are no effects on the baby from this method of pain relief.
An epidural involves medicine given by an anesthesiologist through a thin, tube-like catheter that's inserted in the woman's lower back. The amount of medicine can be increased or decreased according to a woman's needs. Very little medicine reaches the baby, so usually there are no effects on the baby from this method of pain relief.
Epidurals do have some drawbacks — they can cause a woman's blood pressure to drop and can make it difficult to pee. They can also cause itching, nausea, and headaches in the mother. The risks to the baby are minimal, but include problems caused by low blood pressure in the mother.
Tranquilizers. These drugs don't relieve pain, but they may help to calm and relax women who are very anxious. Sometimes they are used along with analgesics. These drugs can have effects on both the mother and baby, and are not often used. They also can make it difficult for women to remember the details of the birth. Discuss the risks of tranquilizers with your doctor.
Natural Childbirth
Some women choose to give birth using no medicine at all, relying instead on relaxation techniques and controlled breathing for pain. If you'd like to experience childbirth without pain medicine, discuss this with your health care provider.
Things to Consider
Here are some things to think about when considering pain control during labor:
- Medicines can relieve much of your pain, but probably won't relieve all of it.
- Labor may hurt more than you expected. Some women who had said they want no pain medicine whatsoever end up changing their minds when they're actually in labor.
- Some medicines can affect your baby, making the baby drowsy or causing changes in the heart rate.
Talking to Your Health Care Provider
You'll want to review your pain control options with the person who'll be delivering your baby. Find out what's available, how effective they're likely to be, and when it's best not to use some medicines.
If you want to use pain-control methods other than medicine, make sure your health care provider and the hospital staff know. You might want to also consider writing a birth plan that makes your preferences clear.
Remember, many women make decisions about pain relief that they abandon — often for very good reason — at the last minute. Your ability to endure the pain of childbirth has nothing to do with your worth as a mother. By preparing and educating yourself, you can be ready to decide what pain management works best for you.
What to do if the child has a stomachache
Many mothers will read this article after their baby complains of pain in the tummy. For them, I will say right away - urgently see a doctor! And I’ll tell everyone else about the possible and very dangerous causes of abdominal pain in children and about what needs to be done immediately.
It so happened that in all three years as a mother, I have never encountered a situation where a baby clutches its tummy and screams “It hurts!”.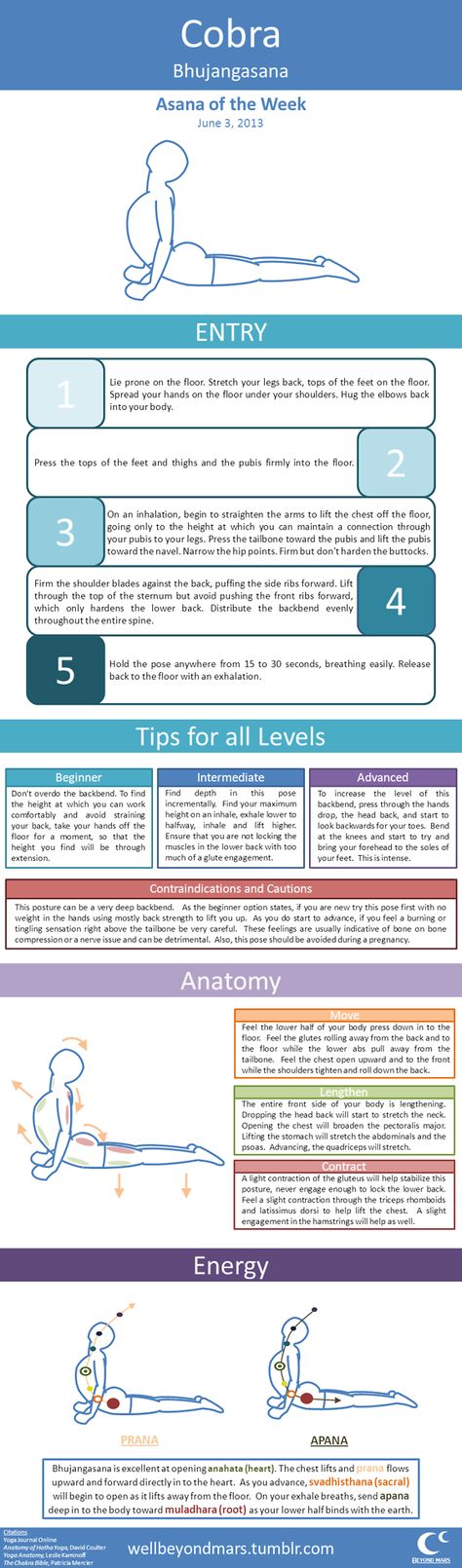 I lived calmly, treated ARVI and did not even think that I would have to go through what, fortunately, had already ended. nine0003
I lived calmly, treated ARVI and did not even think that I would have to go through what, fortunately, had already ended. nine0003
One September afternoon after a walk, my son bent over and, holding his stomach, croaked “Mom, it hurts!”. I put him in the crib and tried to lull him to sleep. The pain intensified, and when the son had already stopped crying and huddled into a ball, she called a taxi and rushed to her private pediatrician. She examined her son and sent him to a pediatric surgeon, and she told me that the situation was very similar to acute appendicitis. The surgeon had a different opinion and sent us to the hospital with a diagnosis of colitis. My baby spent two days in intensive care and almost died from a painful shock. Then we were treated for an acute intestinal infection for a week, and then we were discharged home. A month later, the situation repeated itself with shocking accuracy. Now, without hesitation, I took my son to the surgeon, and he grinned and reproached me for the fact that I again “feed something” to the child.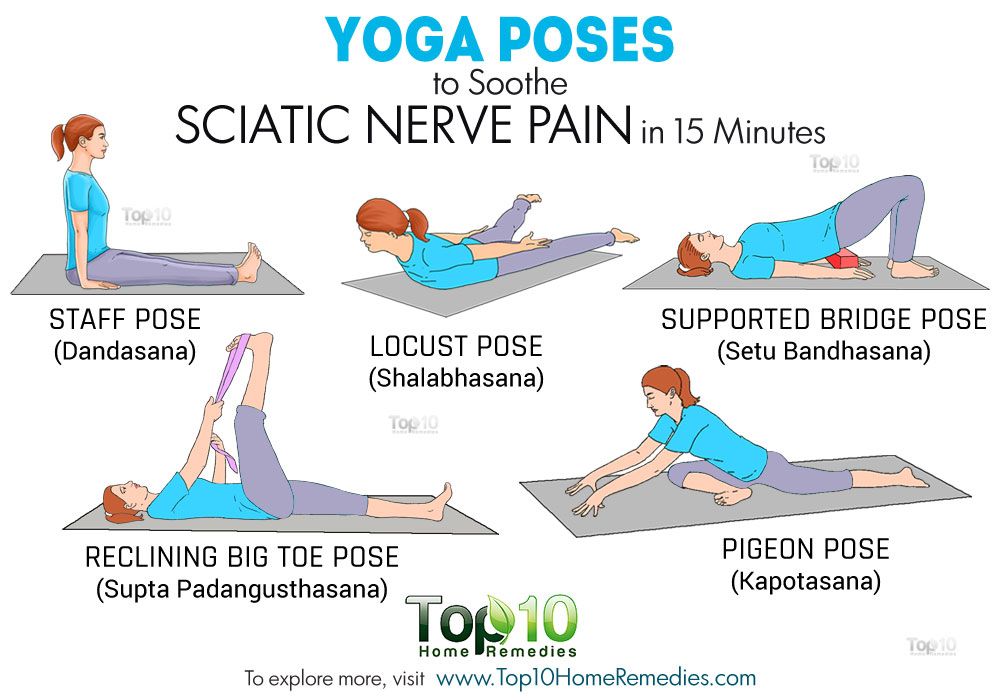 Again, resuscitation, from which we were taken by ambulance to the regional children's surgery. And then an urgent operation and 3 weeks of a nightmare in the department. My son's appendix was cut out. A month ago, he (the appendix) was simply "stabbed" with antibiotics. For a month, the child walked on the edge of a knife, and after the operation, the surgeon said that if we had arrived a day later, he would have done nothing. nine0003
Again, resuscitation, from which we were taken by ambulance to the regional children's surgery. And then an urgent operation and 3 weeks of a nightmare in the department. My son's appendix was cut out. A month ago, he (the appendix) was simply "stabbed" with antibiotics. For a month, the child walked on the edge of a knife, and after the operation, the surgeon said that if we had arrived a day later, he would have done nothing. nine0003
I didn't tell this story to scare you, dear mothers. It's just that my situation is not an isolated case. It's all over the place! And such "professional" doctors too! But, having gone through all this hell, I realized that a child's tummy is not something that is treated at home or with advice from the Internet. I want to tell you about everything.
AII (acute intestinal infection)
This is the most common cause of abdominal pain. Children under the age of 6 suffer from various intestinal infections most often. Why? The child's immunity is imperfect, and the intestines are far from always able to cope with the infection on their own.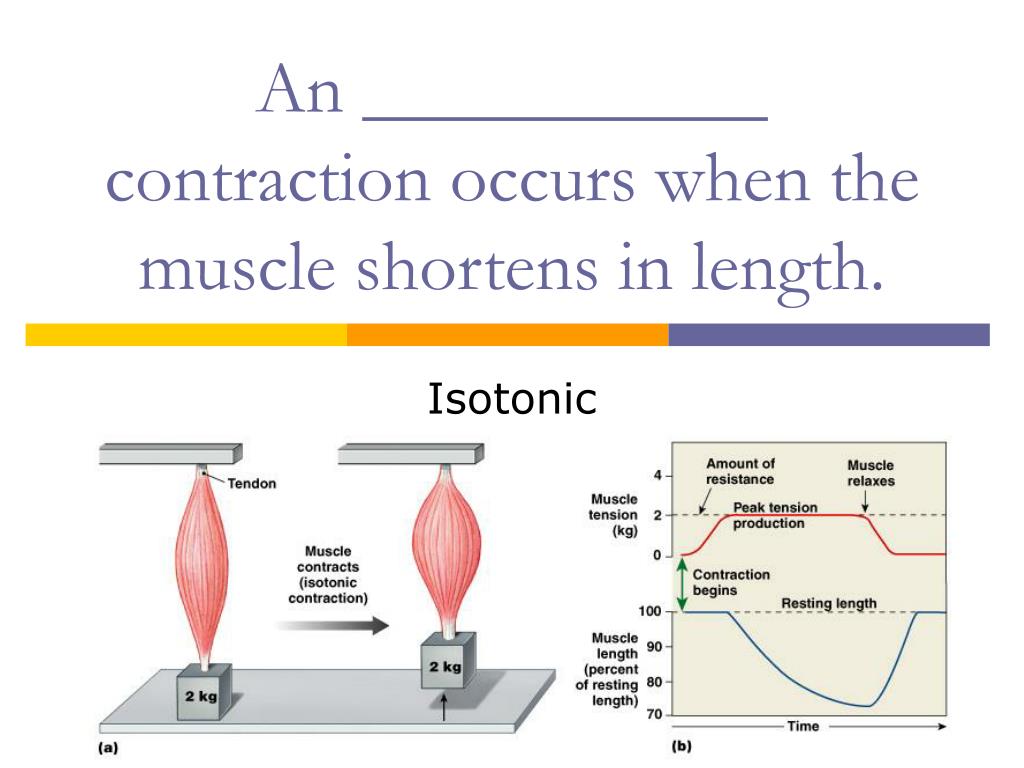 Germs live everywhere - on the kitchen table, doorknobs, toys, TV remote control, etc. Any infection causes vomiting, diarrhea, abdominal pain, weakness, fever, and in small children the body is instantly dehydrated. And if it is enough for an adult to drink activated charcoal and drink a lot of liquid in case of poisoning, then serious losses of the child's body can be restored only in a hospital (antibiotics, droppers). nine0003
Germs live everywhere - on the kitchen table, doorknobs, toys, TV remote control, etc. Any infection causes vomiting, diarrhea, abdominal pain, weakness, fever, and in small children the body is instantly dehydrated. And if it is enough for an adult to drink activated charcoal and drink a lot of liquid in case of poisoning, then serious losses of the child's body can be restored only in a hospital (antibiotics, droppers). nine0003
What should mother do? If you suspect poisoning, try to provide your child with a plentiful fractional (a teaspoon every 5 minutes) alkaline drink (Borjomi without gas, Humana-electrolyte). Along with this, exclude dairy products, raw vegetables and fruits. Giving a disinfectant in such cases is strictly contraindicated!
Monitor your child closely. As soon as you notice that the baby is lying exhausted, or vomiting / diarrhea does not stop, get ready and go to the children's infectious diseases department. And don't be afraid, it just sounds so scary.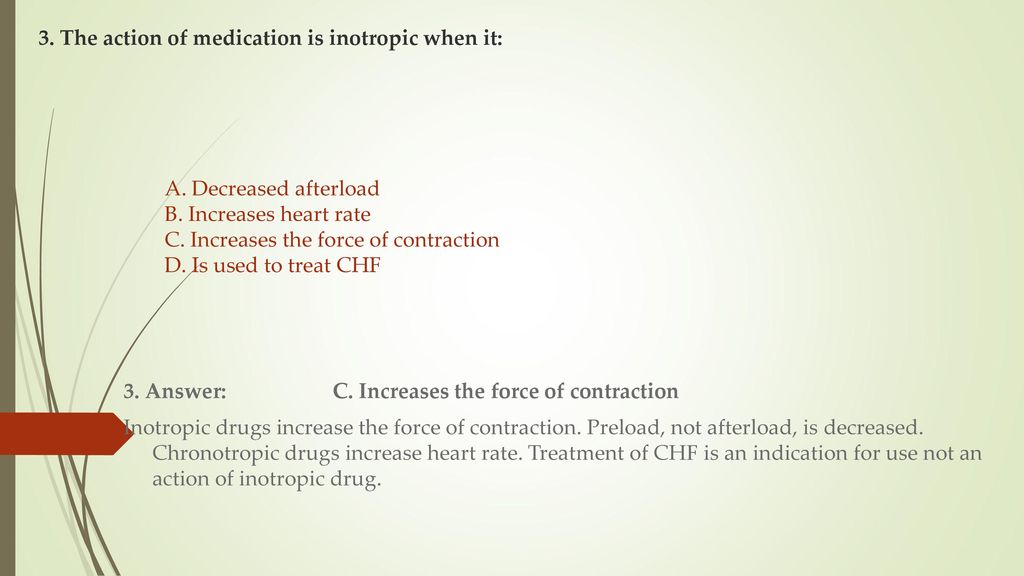 The child will be dripped, and in a day or two they will be allowed to go home. nine0003
The child will be dripped, and in a day or two they will be allowed to go home. nine0003
To prevent infection, I recommend carefully monitoring the baby's diet. Eggs, meat, fish, milk require careful and lengthy heat treatment. All kitchen surfaces, toys, floors should be washed once a week with laundry soap. Do not give your baby products with a dubious expiration date (often children are poisoned by Rastishka, Masha, ice cream, citrus fruits). From an early age, teach children to wash their hands, not to take anything from the floor, not to pet cats and dogs.
Mesadenitis
This terrible word means inflammation of the lymph nodes of the peritoneum. The cause of mesadenitis can be a common ARVI (most often it happens) or an intestinal infection. Lymphogenic spread of infection - from one node to another - gives a similar complication. At the same time, the lymph nodes on the neck, behind the ear, and near the joints can become inflamed, but only inflammation of the lymphatic tissue in the intestine causes such acute pain. nine0003
nine0003
What should mom do? The worst thing about this disease is that it can only be diagnosed by ultrasound. That is, at home, you will not distinguish between mesadenitis (symptoms: acute pain, nausea, diarrhea).
Another unpleasant moment - neglected mesadenitis can cause suppuration of the lymph nodes, and this, as you can easily understand, is very scary and can only be treated surgically.
So the only thing that mom can do is to ensure that she is admitted to the surgical department as soon as possible. Timely recognized mesadenitis is treated with antibiotics, however, for a long time. nine0003
To prevent. No matter how trite it sounds, but the prevention of mesadenitis is the absence of infections, both viral and bacterial. So, dear mothers, increase your child's immunity in all possible ways!
Acute appendicitis
Each of us lives with an appendix. And everyone knows about it. But not many of us are aware of the symptoms of inflammation of appendicitis. An increase in temperature (and the vomiting that occurs against it), diarrhea and acute pain in the right iliac region (and even radiating to the groin and perineum) are far from a complete list of them. Does the baby complain about the tummy, curl up, can only lie on its side? There is every reason for parents to be concerned. Moreover, each child has individual symptoms, for all, only acute pain is characteristic. The most acute pain occurs when you release your hand from the place of pressure in the painful area - this is the first sign that you need to lead to surgeons. nine0003
An increase in temperature (and the vomiting that occurs against it), diarrhea and acute pain in the right iliac region (and even radiating to the groin and perineum) are far from a complete list of them. Does the baby complain about the tummy, curl up, can only lie on its side? There is every reason for parents to be concerned. Moreover, each child has individual symptoms, for all, only acute pain is characteristic. The most acute pain occurs when you release your hand from the place of pressure in the painful area - this is the first sign that you need to lead to surgeons. nine0003
In children, appendicitis proceeds especially rapidly, it becomes complicated very quickly. No one knows the exact causes of inflammation of the caecum. Do not listen to grandmothers, the cause of acute appendicitis is not eating seeds with husks. As the surgeon answered me, most often it is an individual feature of the body. Although nutritional errors play a significant role.
What should mother do? Many believe that the appendix becomes inflamed in children aged 6-10 years. Such is the critical period. But in our surgery, a seven-day-old child was operated on. Therefore, we do not read nonsense about age characteristics on the Internet, but immediately go to surgery. Better to be safe, as they say. nine0003
Such is the critical period. But in our surgery, a seven-day-old child was operated on. Therefore, we do not read nonsense about age characteristics on the Internet, but immediately go to surgery. Better to be safe, as they say. nine0003
Even if a child cannot tolerate pain, never give him pain medication until the diagnosis is made - the result will be a blurred clinic and an incorrect diagnosis. Do not try to inject but-shpu - it greatly lowers the pressure, and this is fraught!
Don't be afraid to take your child to the hospital, no one will “cut” him at random. The diagnosis will be confirmed (or not confirmed) by ultrasound, and only then a decision will be made about the operation.
To prevent. Proper nutrition will significantly reduce the likelihood of inflammation of appendicitis. People who eat a lot of plant foods are practically out of the risk group. And you should also constantly monitor the child's stool, because constipation can lead to various intestinal inflammations. nine0003
nine0003
In addition, I would like to say that some people (2-4%) have more than one appendix.
Intussusception and intestinal obstruction
My grandmother always forbade my sister and me to run and jump after meals. She said that there would be a volvulus of the intestine. “Some fears,” we thought, and were not going to listen to her. But she was right. In three weeks in the surgical department, I realized this. You should have seen how many children come in with suspected intussusception. In an accessible language, this is a twisting of the intestine or a situation where one intestine seems to be “inserted” into another ... Symptoms of intussusception: constipation, acute cramping pain in the abdomen, vomiting, weakness. The symptoms of obstruction are added by the absence of gas removal, a sharp subsidence of peristalsis (no rumbling in the stomach is heard). nine0003
What should mother do? And again, only an ultrasound will establish the correct diagnosis. To relieve the pain, you can give your child an antispasmodic and take it to the doctor ASAP. The fact is that in the first few hours this situation is reversible - the baby will be given an enema, the intestines will be blown with air or a special substance is administered, and an ultrasound scan will be repeated. If the intussusception has disappeared, the baby will drink a suspension of barium, which will come out with the first stool (evidence of intestinal patency), and you will be allowed to go home. If the situation is started, one cannot do without an operation! nine0003
The fact is that in the first few hours this situation is reversible - the baby will be given an enema, the intestines will be blown with air or a special substance is administered, and an ultrasound scan will be repeated. If the intussusception has disappeared, the baby will drink a suspension of barium, which will come out with the first stool (evidence of intestinal patency), and you will be allowed to go home. If the situation is started, one cannot do without an operation! nine0003
To prevent. Most often, intussusception occurs in children under five years old, mainly in boys. If your child is at risk, try to monitor his diet, do not allow outdoor games after meals.
I would like to add that a child's tummy is the most inaccessible place for diagnosis. If you can notice the symptoms of tonsillitis or allergies yourself, then diagnosing the listed diseases is a matter for an experienced surgeon! And you, as a loving parent, owe it to such an experienced child surgeon to show that this is your main task!!! nine0003
Relief of pain caused by postpartum cramps or uterine involution
This updated review examines the efficacy and safety of drug and non-drug pain relief in women experiencing postpartum pain after vaginal delivery.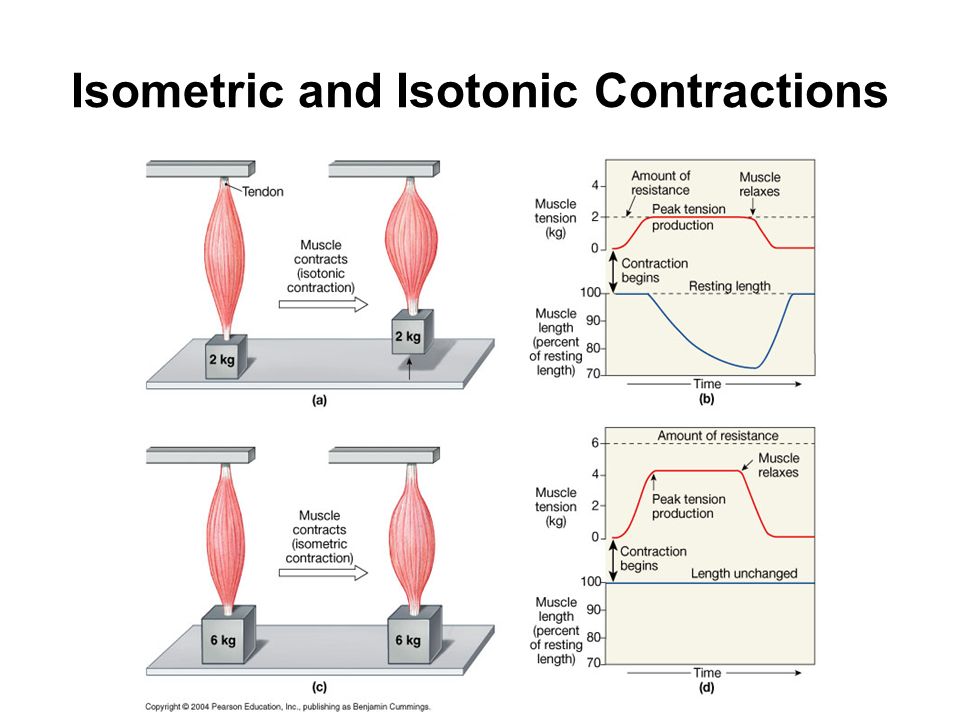 Randomized controlled trials compared the use of a drug for pain relief with an inactive placebo, no treatment, or another drug.
Randomized controlled trials compared the use of a drug for pain relief with an inactive placebo, no treatment, or another drug.
What is the problem? nine0074
After giving birth, women may experience cramping pain and discomfort caused by the contraction of the uterus as it returns to normal prenatal size. Typically, such pain continues for two to three days after childbirth. Previously giving birth women are more prone to such pain. Breastfeeding stimulates uterine contractions and increases pain.
Types of pain relief used to treat pain include paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs) ibuprofen and naproxen, opioids including codeine, and non-drug methods such as herbal preparations and transcutaneous electrical nerve stimulation (TENS). nine0003
Why is this important?
Postpartum pain management is very important, as the pain can interfere with the mother's normal daily activities and her bond with and care for the baby. Postpartum pain can interfere with the establishment of breastfeeding.
Postpartum pain can interfere with the establishment of breastfeeding.
What evidence did we find?
We searched for evidence from randomized controlled trials (October 2019years) and identified 28 studies (2749 mothers) who were in the hospital after an uncomplicated singleton birth. Most of the evidence is of low certainty because the studies did not include enough women. Many studies did not include breastfeeding women. This makes the evidence less relevant to a wider group of women. None of the studies reported adverse events in neonates.
NSAIDs are probably better than placebo (sham treatment) in providing adequate pain relief reported by women (11 studies, 946 women; moderate-certainty evidence) and may reduce the need for additional pain relief (4 studies, 375 women; low-certainty evidence). The difference between NSAIDs and placebo in maternal risk of adverse events may not be significant (9 studies, 598 women; low-certainty evidence).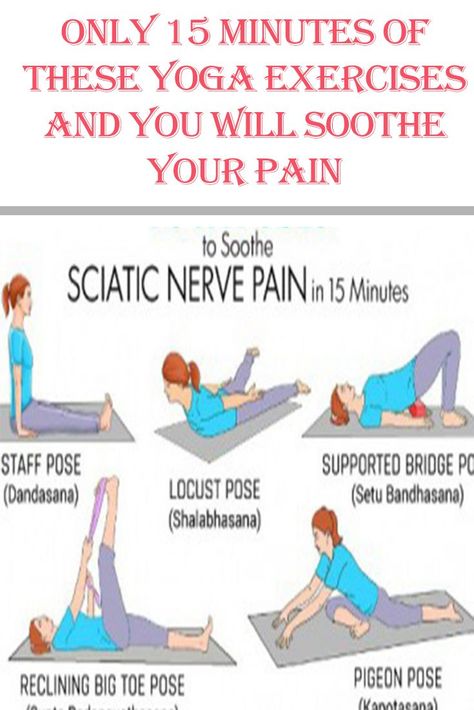
NSAIDs seem to be better than opioids for providing adequate pain relief reported by women (5 studies, 560 women; moderate-certainty evidence) and may reduce the risk of maternal adverse events (3 studies, 255 women; low-certainty evidence). NSAIDs may slightly reduce the need for additional pain relief compared to opioids (2 studies, 232 women; low-certainty evidence). nine0003
Opioids may be better than placebo for adequate pain relief reported by women (5 studies, 299 women; low-certainty evidence) and for the need for additional pain relief (3 studies, 273 women; low-certainty evidence). Compared with placebo, opioids increase the risk of maternal adverse events (3 studies, 188 women; low-certainty evidence).
Very low-certainty evidence means that we are not sure that paracetamol is better than placebo in terms of adequate pain relief, women reported need for additional pain relief, or risk of maternal adverse events (2 studies, 123 women). nine0003
Very low-certainty evidence means that we are not sure if there is a difference between paracetamol and NSAIDs in terms of adequate pain relief reported by women or the risk of adverse events in mothers (2 studies, 112 women).
Very low-certainty evidence means we are not sure NSAIDs are better than herbal pain relievers in terms of adequate pain relief reported by women (4 studies, 394 women), the need for additional pain relief (1 study, 90 women) or maternal risk of adverse events (1 study, 108 women).
Very low-certainty evidence means we are uncertain if there is a difference between TENS and no TENS in terms of adequate pain relief reported by women (1 study, 32 women).
What does this mean?
NSAIDs may be better than placebo and probably better than opioids in relieving postpartum pain after vaginal delivery. The quality of the evidence was low, and we are uncertain about the effectiveness of other forms of pain relief. Future trials need to recruit enough women and ensure greater relevance by including women who are breastfeeding. Further research could also include interviewing postpartum women about their experience of postpartum pain after vaginal delivery.