Bruise on baby's head from birth
What Do Bruises on a Newborn Child Indicate?
Childbirth is a physically demanding and stressful process that often pushes the physical limits of both the mother and baby. Many newborns look like they have just been in a little fist fight when they first come out. Bruises on the head and face of a newborn baby are a common sight. In most cases, bruises on a newborn are nothing to worry about and they go away on their own within a few days.
Bruises occur when damaged blood vessels leave dark blood spots beneath the skin. New parents are understandably concerned when they see bruises on their baby. However, the odds are overwhelming positive that your baby is just fine. In some rare cases, infant bruises are among the earliest indications that a more severe injury occurred during childbirth.
Newborn Bruises and Birth Injuries
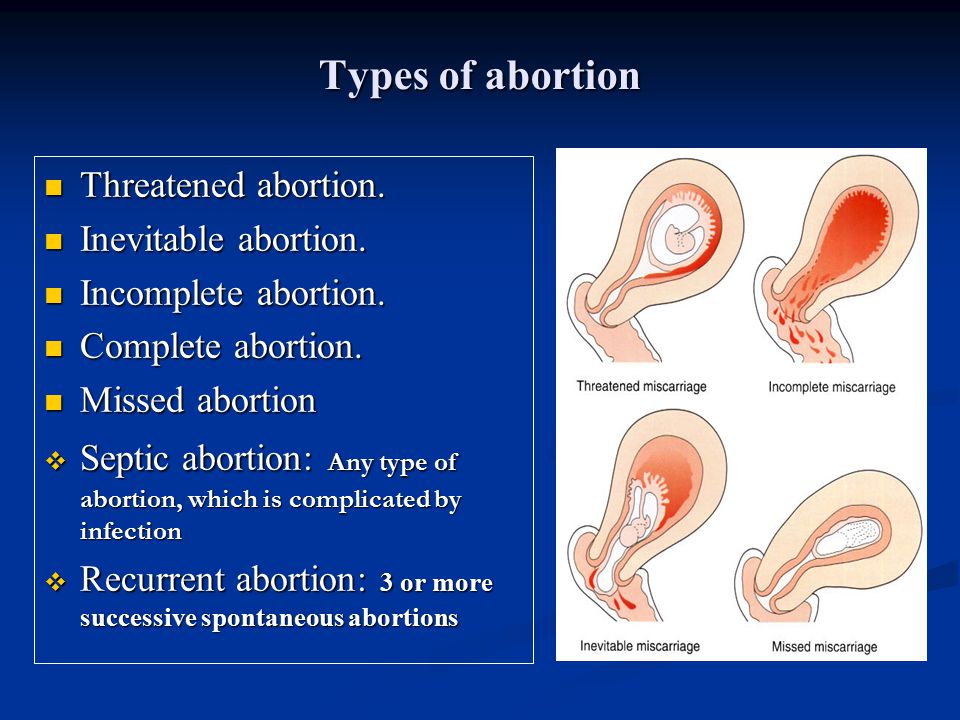
Although bruises are a common consequence of childbirth, not all babies are born with bruises. If a newborn has extensive bruising, it is a clear indication that they endured a particularly stressful passage through the birth canal which caused birth trauma. Common sites include the head, neck, and shoulders. Infant bruises can be related to the following events and medical conditions:
- Caput Succedaneum: Caput succedaneum is very common neonatal condition in which the newborn's skull has an area of edema or swelling caused by pressure as the head passed through the birth canal. The affected area, usually located on the forehead, will be puffy and soft. Caput succedaneum is a benign condition but it can lead to other complications including a higher risk of newborn jaundice.
- Forceps Trauma: If operative tools were used to facilitate delivery (e.g., obstetrical forceps or a vacuum extractor) bruises on the baby's head or neck may be evidence that the doctor used excessive force or improper technique when employing those tools. Negligent misuse of forceps and vacuum extractors is a common reason for major birth injuries such as Erb's palsy an even more serious types of brain injuries.
 If you see a child with bruises, abrasions, forceps marks, or lacerations, you have to question whether there was excessive pulling.
If you see a child with bruises, abrasions, forceps marks, or lacerations, you have to question whether there was excessive pulling. - Shoulder Dystocia: Shoulder dystocia occurs when one of the baby's shoulders becomes stuck behind the mother's pelvis during delivery. When this occurs, the shoulder must be physically dislodged in order to deliver the baby. Bruising to the neck and shoulder area often results from efforts to free the stuck shoulder.
- Disseminated Intravascular Coagulation: An extremely rare bleeding condition whose symptoms include bruising, bleeding, and uncontrolled blood clotting. In newborns, it can be onset by birth injuries like asphyxia, sepsis, and respiratory distress.
Bruises may be confused with "mongolian spots," a type of grey-blue birthmark that usually fades within a few days of birth.
Bruises in Childhood
The focus of this post is bruises that could be harbingers of a birth injury.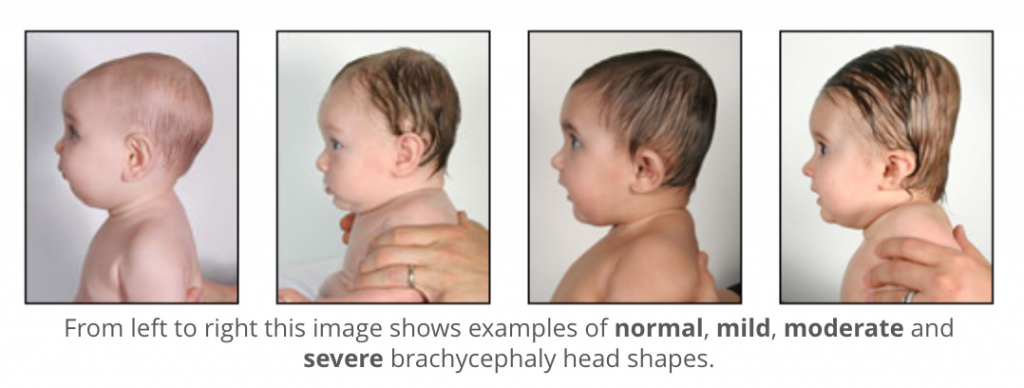 It is also important to underscore the importance of monitoring bruises in older children.
It is also important to underscore the importance of monitoring bruises in older children.
Bruises are a painful part of childhood. These minor injuries happen all the time from falls, accidents, and play. A rare condition that causes excessive bruising is hemophilia, also known as Factor VIII deficiency. People with hemophilia have difficulties forming blood clots, and bruise more easily than others. Idiopathic thrombocytopenic purpura (ITP) is another rare condition that limits the blood's ability to clot, leading to excessive bruising and bleeding.
But what should a parent do if they leave their child in the hands of a caregiver only to notice bruising that was not there previously? Most of us would assume that an accident occurred or a fall took place and think nothing of it. But when should a parent be concerned? In the following excerpt, we hope to paint a clearer picture of how to approach this difficult situation and what is considered to be abnormal.
First, talk with the caregiver and ask the following questions:
- What exactly happened?
- Where did this bruise come from?
- When did this occur?
- Why was I not informed of this prior to picking my child up?
A caregiver shoulder be able to reliably explain what happened in a manner that makes logical sense. If the story does not quite add up, the injuries described don't reflect what is seen on the child, or you suspect any suppression of truth, continue to ask questions. These questions allow you to get a picture of what happened.
If the story does not quite add up, the injuries described don't reflect what is seen on the child, or you suspect any suppression of truth, continue to ask questions. These questions allow you to get a picture of what happened.
Next, consider taking your child aside to talk with them one on one. If your child is older than the age of 5, they are likely able to provide more information as to what happened. It is very important to interview and talk with your child away from the caregiver as this can potentially reveal more information that would otherwise have not been disclosed. If possible, have the child point to where it hurts on his/her body, ask yes or no questions, and watch their reaction to the questions. Look at their eye contact and posture. Children can sometimes reveal when they are withholding something by looking down or playing with their hands and feet.
If your child is under the age of 1 or unable to speak, you will have to apply more critical thinking to the situation. Does the story match the injury? Are the bruises in an unusual location that you would not expect for their age group and ability? For example, infants below the age of 4 months are not capable of rolling, climbing furniture, or sitting up without support, thus falling off of changing tables from rolling over is unlikely. Infants between 4 and 7 months may grasp objects, put things in their mouths, roll over (closer to 7 months), sit up without support (closer to 7 months), and possibly even crawl (closer 7 months).
Does the story match the injury? Are the bruises in an unusual location that you would not expect for their age group and ability? For example, infants below the age of 4 months are not capable of rolling, climbing furniture, or sitting up without support, thus falling off of changing tables from rolling over is unlikely. Infants between 4 and 7 months may grasp objects, put things in their mouths, roll over (closer to 7 months), sit up without support (closer to 7 months), and possibly even crawl (closer 7 months).
Infants between 7 and 12 months can sit without support and crawl, but are unable to climb on top of furniture. However, they will begin to pull themselves up on furniture or chairs (closer to 10 months) in order to further explore. With further development, the transitions into walking a few steps either with or without support from furniture increases the chance of minor injuries from falls and collisions with furniture. Bruises on the knees, elbows, forehead, hands, and feet can begin to occur with falls around this age. After 12 months, children are more likely to walk without support, opening up more possibilities for accidental injury.
After 12 months, children are more likely to walk without support, opening up more possibilities for accidental injury.
Next, look for any behavioral changes in your child:
- Do they seem excited to see you when picked up or are they quivering, shaking, or crying uncontrollably when you pick them up?
- If they are currently potty-trained, do they now have relapses or episodes of bed wetting or wetting their underpants?
- Do they flinch with any sudden movements on your end, hold their hands up to protect their face, or cower in any way?
- Do they have urinary complaints resembling a UTI (hurts to pee, cries with trips to the bathroom, fearful of urinating or now showing embarrassment with going to the bathroom)
- Toddlers, especially females, can get vaginitis, a condition that results in irritation of the vagina from frictional contact from either the fabric of the diaper or sitting in a urine soaked diaper for too long.
- Excessive redness, pain, recurrent urinary symptoms, or any bleeding should always get evaluated by a medical professional as this can also be concerning for sexual abuse
- Is your child now fearful of getting undressed, changed or getting ready for bath-time? This may be concerning for sexual abuse
- Are they having vivid nightmares or dreams?
- Are they more "clingy" or more insecure than normal?
Bruising and trauma could be from abuse. Take particular notice of:
Take particular notice of:
- Burn marks in the shape of a cigarette tips, an iron, stove coils, and stocking and glove patterns
- Stocking and glove patterns result from placing a child's hands and/or feet into a boiling pot of water
- Bruises in the shape of a hand, fist, fingers or belt buckle
- Bruises on multiple body parts or that encompass a large portion of the child's body, particularly their abdomen, back, arms, legs, thighs, head or face
- Multiple stages of healing bruises, i.e. new bruises present with ones that are fading (black/blue/purple reflect recent injury while yellow/green reflect older injury)
- Bruises at joints (elbow, knee, ankle) that are noticeably swollen and the child cries with any movement of the joint or has severe restriction of the joint
- However, knees, elbows and ankles are common places for scrapes, mild bruises and trauma from falls that would not be considered abuse
- Bruises on the upper or lower legs that result in the child not wanting to walk or bear any weight on them
- Bruises on the thighs that result in one leg appearing shorter than the other
- Pain that is out of proportion to the appearance of the bruise or child
Any of the above should immediately be reported to the police:
- Do not leave the child alone while making the call
- This is especially important if picking up from a caregiver's home
- Do not leave the location where you picked your child up, have the police come to you
- If at a daycare, get the supervisor or manager involved
Birth injury (in the baby)
Birth injury (in the baby) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is birth injury?
Having a baby in Australia is very safe, although it’s estimated that more than 1,000 babies are injured during childbirth each year. It can be very upsetting if your baby has been injured, but most birth injuries are only temporary.
It can be very upsetting if your baby has been injured, but most birth injuries are only temporary.
Also called 'neonatal birth trauma', birth injury to a newborn baby can include many things, from bruising to nerve damage to a broken bone. Sometimes an injury occurs as a result of life-saving procedures.
About 49 in every 10,000 babies born in Australian hospitals suffer a birth injury. Here are some of the types of birth injury affecting babies.
Bruises and swelling of the scalp
Sometimes a baby can be born with minor, temporary injuries to their head or face. These include bruises, swelling (sometimes called a chignon), lumps caused by fluid under the skin (caput succedaneum) or bleeding under the skin (cephalohematomas), and blood inside the eye (subconjunctival haemorrhage).
Fractures
Fractures (breaks) can occur when there is difficulty getting a baby through the birth canal. The bone that most often breaks is the collarbone (clavicle), and this can happen when the baby's shoulder gets stuck (shoulder dystocia), or if the baby is born breech (bottom first).
Nerve damage
Nerves can be damaged during childbirth, particularly in the baby's face (which can lead to facial paralysis) and the shoulder (which can lead to brachial palsy — loss of arm movement). Usually, nerve damage in a newborn is only temporary.
Brain injury
In very rare cases, a baby can suffer a brain injury during childbirth. If the baby doesn’t get enough oxygen for a long time during labour (perinatal asphyxia), they can experience brain damage. Cerebral palsy is a type of brain damage, but only a very small percentage of cerebral palsy cases is due to complications at birth.
Bleeding on the brain
In rare cases, a baby can suffer bleeding in or around the brain during childbirth. This is more common among very premature babies, and most infants with bleeding don't have symptoms. Others may be lethargic, have difficulty feeding and/or have seizures.
What causes birth injury?
Birth injuries can occur simply because of the pressure and resistance involved in giving birth vaginally.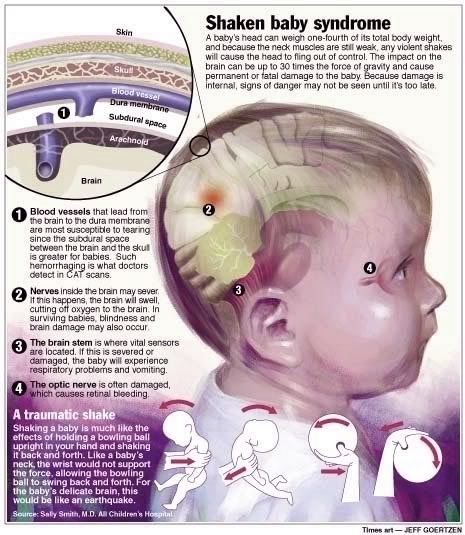 When the baby moves through the birth canal, there's pressure on its skull and body from the mother's pelvic bones.
When the baby moves through the birth canal, there's pressure on its skull and body from the mother's pelvic bones.
Large birth weight (more than 4kg) can increase the risk of injury during childbirth. There is also a greater risk if the baby is in a difficult position for labour and birth (such as the breech position). Premature babies born before 37 weeks are typically more fragile and may be injured more easily.
Other causes of birth injury to a baby include a difficult or prolonged labour, the shoulder becoming stuck in the birth canal and cephalopelvic disproportion (if the mother's pelvis isn't large enough or shaped in a way that allows for a vaginal birth).
Babies born with the assistance of forceps or ventouse (vacuum) are at higher risk of bruising, marks or swelling on the baby's head or face.
Lack of oxygen to the baby during birth could be caused by a number of things, such as problems with the umbilical cord, serious events in the mother such as haemorrhage or fever during labour, uterine rupture or abruption of the placenta (when it comes away from the uterus prematurely).
How are birth injury in babies treated?
Most birth injuries in babies are temporary. If the injury was to the soft tissue, then no treatment is normally needed — the medical team will just monitor the baby and may run tests to check for other injuries.
If there has been a fracture, your baby may need an x-ray or other imaging. The limb may need to be immobilised and some babies may need surgery.
If your baby has damaged nerves, the medical team will monitor them closely and recovery can take a few weeks. For more serious nerve damage, your baby may need special care.
Resources and support
- Talk to your doctor, midwife or obstetrician/gynaecologist.
- You can call Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse (7 days a week, 7am to midnight AEST).
- Call the healthdirect helpline on 1800 022 222.
- Contact the Australian Birth Trauma Association for support and resources.
Sources:
Stanford Children’s Health (Birth injury), Medical Hypotheses (The significance of incomplete skull fracture in the birth injury), Mater Mothers’ Hospital (Labour and birth — an assisted vaginal birth), Australian Commission on Safety and Quality in Health Care (Neonatal birth trauma), Cerebral Palsy Alliance (What causes cerebral palsy), Medscape (Birth trauma), Birth Asphyxia (Birth asphyxia), Merck Manual (Birth injuries in newborns), Mater Mothers' Hospital (Shoulder dystocia)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Related pages
- Neonatal intensive care unit (NICU)
- Special care nursery (SCN)
- When birth doesn't go to plan
- Birth trauma (emotional)
- Birth injury (to the mother)
Need more information?
What is Birth Trauma? - Birth Trauma
The delivery of a baby is a positive event for many women, but for some it can be a mixed experience or even very negative, resulting in physical and/or
Read more on Australasian Birth Trauma Association website
Birth After Birth Trauma - Birth Trauma
This is a question that we hear often. How can I have another baby?
Read more on Australasian Birth Trauma Association website
Considerations for birthing after birth trauma - Birth Trauma
In this post we consider some important points when making decisions about birthing after a birth trauma experience.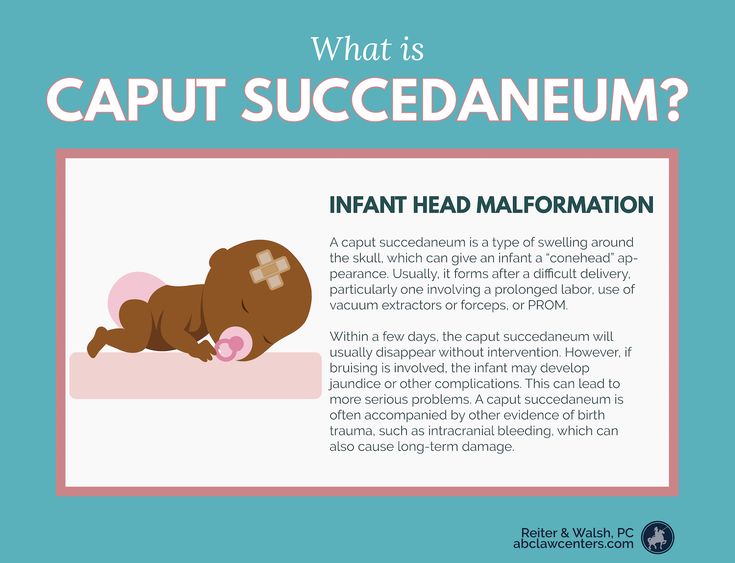
Read more on Australasian Birth Trauma Association website
Family & Friends - Birth Trauma
If you are reading this then you may have someone close to you that has been impacted by a difficult birth experience, be it a partner, loved one or someone
Read more on Australasian Birth Trauma Association website
Birth and beyond - Ngala
Exciting times are ahead!Birth comes after lots of anticipation and preparation
Read more on Ngala website
Physical Trauma - Birth Trauma
For many women who have suffered from physical trauma as a result of childbirth, and who are struggling to cope, is it vital that healthcare providers
Read more on Australasian Birth Trauma Association website
Early Postnatal - Birth Trauma
The early postnatal period is a time of emotional change for most women. Some women may experience distress or symptoms of depression at this time if they
Some women may experience distress or symptoms of depression at this time if they
Read more on Australasian Birth Trauma Association website
Childbirth trauma and recovery | PANDA
While many pregnant women and their partners know birthing their baby will be hard work, very few expect labour and childbirth could be complicated.
Read more on Perinatal Anxiety and Depression Australia (PANDA) website
Postpartum Trauma Disorders (e.g. PTSD) - Birth Trauma
Post Traumatic Stress Disorder (PTSD) is one of a group of trauma and stressor-related disorders. People often associate these with war veterans, police
Read more on Australasian Birth Trauma Association website
Recovering from a traumatic birth - COPE
COPE's purpose is to prevent and improve the quality of life of those living with emotional and mental health problems that occur prior to and within the perinatal period.
Read more on COPE - Centre of Perinatal Excellence website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Cephalhematoma in newborns - GBUZ YNAO
It only seems that when the baby is born, the baby slowly and leisurely leaves the mother's womb. In fact, in order to be born, the child has to make corkscrew, pendulum and other active movements of the body. Therefore, in the process of passing through the birth canal, the baby often gets injured.
Neonatal cephalohematoma refers to birth trauma to the head and is a small tumor that occurs as a result of rupture of blood vessels. This leads to the fact that between the bones of the skull and the periosteum begins to accumulate blood. Since the blood of newborns is characterized by low coagulability, the formation continues to increase in size within 2-3 days after birth. nine0003
Cephalhematoma occurs in 0.1 to 1.8% of newborns.
Causes of cephalohematoma in newborns As a result, the brain is compressed, and the child's head is slightly deformed. However, you should not worry about this - within a few days after the birth, the bones of the cranium return to their places. nine0003 Meanwhile, the scalp is displaced along with the periosteum, thereby provoking vascular rupture. Most often this happens if the newborn suffers from a deficiency of vitamins K, C, PP. The blood flowing from the damaged capillaries begins to accumulate in the pocket between the flat bone of the skull and the periosteum, forming a tumor. Other causes of cephalohematoma in newborns: Large fetus with narrow birth canal; Breech, parietal or facial presentation; nine0003 Rapid or, conversely, too slow delivery; Postterm pregnancy; Malformations and pathologies of fetal development; A woman's narrow pelvis or past trauma that deformed the pelvic bones. Also among the factors contributing to the formation of cephalohematoma in newborns, one can name chronic intrauterine fetal hypoxia. It can occur as a result of entanglement or squeezing of the umbilical cord. In addition, hemorrhages can be the result of the actions of obstetricians if forceps or vacuum are used in complicated births. nine0003 Treatment of cephalohematoma in newborns A cephalohematoma can be located in different parts of the head, but most often it occurs in the region of the crown, less often in the occipital, frontal or temporal regions. If the amount of blood in the cephalohematoma in newborns is small, then after a few days it begins to decrease in size and dissolve. The tumor disappears completely in about one and a half to two months without any intervention. If there was a significant hemorrhage, then resorption may take a longer period of time. Small cephalohematomas in newborns usually do not require treatment. Doctors observe the child, sometimes they prescribe vitamin K, which increases blood clotting. This is done in order to stop the leakage of blood and the increase in the size of the tumor. To avoid complications, it is recommended to feed the baby with breast milk, which contains maternal antibodies and contributes to the formation of his own immunity. If the size of the hemorrhage is significant, a puncture of the cephalohematoma is performed, but not earlier than 10 days of life, due to the high probability of rebleeding. Punctures are made in the periosteum with a special needle, through which the contents of the formation are sucked out. Then a pressure bandage is applied to the damaged area. If there is inflammation of the cephalohematoma, its redness, swelling, increase in body temperature, then there is infection and suppuration. In this case, instead of puncture of cephalohematoma in newborns, surgical intervention is required. The skin at the site of the formation of the tumor is cut, after which the blood accumulated there is removed and the edges of the wound are sutured. Further antibiotic therapy is carried out. After the operation, the child is under the supervision of doctors for several months. nine0003 Consequences of cephalohematoma in newborns Anemia resulting from blood loss; Jaundice (increased bilirubin), which develops as a result of tumor resorption, which is accompanied by the breakdown of hemoglobin and the entry of its products into the bloodstream; Extremely rare: Suppuration of cephalohematoma, development of an inflammatory process; Ossification or ossification of the mass, resulting in a deformity of the skull. Prevention of cephalohematoma in newborns consists in maintaining a healthy lifestyle for a pregnant woman and avoiding the use of drugs that can affect the development of the fetus. Main Medical Library Dobrobut Publication date: 2020-01-22 Cephalhematoma is a birth injury characterized by the formation of a hematoma. Pathology is diagnosed in 3% of babies, regardless of gender. Cephalhematoma in newborns on the head can be accompanied by various complications: deformation of the bones of the skull, suppuration, anemia and jaundice. Formations come in various sizes and depend primarily on the volume of accumulated blood. Due to the failure of the hemostasis system in the baby's body, blood can accumulate for several days after childbirth, contributing to an increase in the size of the hematoma. Causes of cephalohematoma during childbirth: As noted above, external cephalohematoma is a hemorrhage between the periosteum and the surface of the bones of the skull, which disappears by the end of the second month of a baby's life. Depending on the location, the hemorrhage can be frontal, occipital, parietal and temporal. According to the severity, cephalohematoma of I degree (hematoma volume 3-4 cm), II (4-9 cm) and III (hemorrhage more than 9 cm) are distinguished. The consequences of a generic cephalohematoma in the future depend on the size of the formation and the general condition of the newborn. A cephalohematoma occurs within a few hours after the baby is born. The next 2-3 days, the formation increases in size, after which a period of regression begins. Complete resorption of the hematoma occurs by the end of 8 weeks. Main symptoms: On our website Dobrobut.com you can make an appointment with a specialist and get an answer to any question. The doctor will tell you about the main signs of ossified cephalohematoma and about the methods of treating the pathology. The diagnosis is made after a thorough examination of the baby. Differentiate cephalohematoma from cerebral hernia, birth tumor, coagulopathy, congenital mycoplasmosis and hemorrhage under the aponeurosis will help research: ultrasound, CT, neurosonography and craniogram. nine0003 Hemorrhage is treated by a neonatologist or pediatric surgeon. With a small hematoma, special treatment is not necessary. The baby is prescribed calcium and vitamin K preparations for 5-7 days. The course of therapy for uncomplicated pathology is 7–10 days. It will take at least a month to treat a cephalohematoma in a child with complications. A baby with such a pathology must be registered with a surgeon and a neurologist. nine0003 Neonatologists recommend using Troxerutin to speed up the healing of the mass. The gel is applied to the hematoma area twice a day. The drug increases vascular tone and prevents further penetration of blood. In case of extensive hemorrhage (more than 9 cm in volume), the doctor will prescribe surgery. Puncture of cephalohematoma of the parietal bone is a safe procedure for the health of the baby, the duration of which takes no more than 10 minutes. The child's skin at the site of hematoma formation is pierced with a special needle, the accumulated blood is sucked off, after which the puncture site is disinfected and a pressure bandage is applied. Surgical removal of cephalohematoma is indicated in the presence of purulent contents of the cavity, as well as in the III degree of development of the pathology. nine0003 Doctor's recommendations after the puncture: In most cases, the prognosis is favorable. Most severe consequences: If you have any questions, sign up for a consultation by phone or fill out the form on the website. Related services: Download our Google Play and App Store app Our doctors See all doctors 712 Certificate No. Certificate no. QIZ 804 469 C1 Certificate No. QIZ 804 470 C1 Certificate no. QIZ 804 471 C1 View all certificates Request a call back Enter your phone number Other articles Symptoms of polyarthritis of the fingers - necessary information for patients Polyarthritis of the fingers: the main causes of the disease, clinical manifestations, drug treatment and prevention. How to treat polyarthritis - advice from a practitioner. nine0003 Symptoms of intrahepatic cholestasis of pregnancy: generalized itching What is gallbladder cholestasis syndrome. Indicators of biochemical analysis of blood in cholestasis. The main symptoms of cholestasis in pregnancy.
The borders of the tumor usually do not go beyond the sutures of the skull, where the periosteum is tightly fused with the bones. The blood in the cephalohematoma remains liquid for a long time, does not clot, so the formation is initially elastic in consistency. On palpation, you can feel the movement of fluid inside. nine0003
nine0003
nine0003
Consequences of childbirth cephalohematoma in the future - important information for parents - clinic "Dobrobut"
Cephalhematoma in newborns on the head - symptoms, treatment
nine0003
Classification of cephalohematoma
Given the localization of the hemorrhage, cephalohematoma can be left-sided, right-sided and bilateral. In some cases, the pathology is accompanied by concomitant injuries in the form of a fracture (crack) of the skull bones. nine0003
Signs of ossified cephalohematoma
Diagnosis
Treatment of cephalohematoma in a child
Consequences and prognosis
Serious consequences occur in a small percentage of babies due to the displacement of brain structures under the pressure of a hematoma and the accumulation of blood under the periosteum. nine0003
Pediatric consultation
Breastfeeding, its role in a child's life Do you want to get an online explanation from the doctor of the Dobrobut MS?
Our certificates
QIZ 804 468 C1