Breastfeeding with low supply
Low Milk Supply | WIC Breastfeeding Support
Many moms worry about low milk supply, but most of the time your body makes exactly what your baby needs, even if you don't realize it. There are also ways to tell if your baby is getting enough milk. If you aren't making enough, there are ways you can build your supply. And your WIC breastfeeding staff is always there to help!
Am I Making Enough Milk?
First, look for these signs that your baby is getting enough milk. For example, pay attention to the number of wet and dirty diapers and your baby's weight gain.
Things you should NOT worry about:
- How your breasts feel. Your breasts will feel softer and less full as your milk supply adjusts to your baby's needs. This does not mean you have low supply.
- If your baby nurses for shorter periods of time, such as only 5 minutes on each breast.
- If your baby's feeds are bunched together. This is called cluster feeding and happens when your baby starts nursing more often and for longer.
This can happen in the evenings or because of growth spurts.
- Not getting much milk when you express. Your baby is much more effective than a pump or hand expression at getting out milk. Find tips to help you pump.
If you are still concerned, talk to your baby's doctor about their growth.
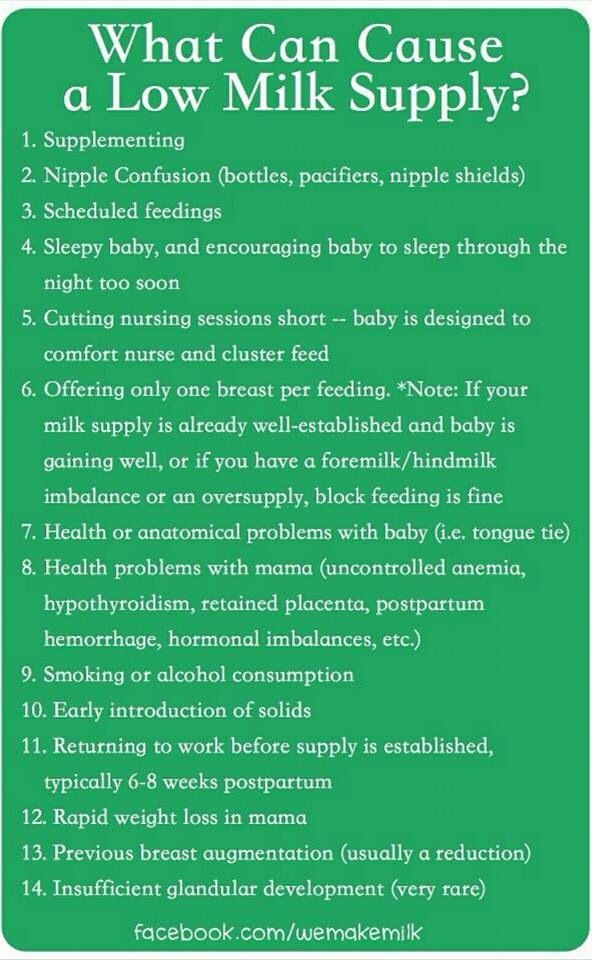
Causes of Low Milk Supply
While most moms make plenty of milk, some do have low milk supply. This might happen if you:
- Limit your baby's breastfeeding sessions. Remember, the more you feed on demand, the more milk you make.
- Give your baby infant formula instead of breastfeeding.
- Introduce solid foods before baby is 4-6 months old.
- Take certain birth control pills or other medicine.
- Don't get enough sleep.
- Drink alcohol or smoke.
- Have had breast surgery.
Talk to your doctor if you have hepatitis B or C, herpes, or diabetes. These conditions may also affect milk supply.
Increasing Your Milk Supply
Breastfeeding frequently—especially in the first hours, days, and weeks—is the main way to increase your milk supply. Your body will make milk to meet your baby's demand.
Try these tips to help you make more milk:
- Breastfeed every time your baby is hungry. In the early weeks, your baby will eat 8-12 times every 24 hours. It's best not to put your baby on a strict feeding schedule. Follow your baby's cues, and let your baby tell you when it's time to eat.
- Make sure your baby is latching well.
- Offer both breasts at each feeding. Let your baby finish the first side, then offer the other side.
- Empty your breasts at each feeding.
 Hand express or pump after a feeding to draw out all the milk and signal your body to make more.
Hand express or pump after a feeding to draw out all the milk and signal your body to make more. - Avoid bottles and pacifiers in the early weeks. Feed your baby from your breast whenever you can.
- Get plenty of sleep, and eat a healthy diet.
- Pump or express your milk. Pumping or expressing milk frequently between nursing sessions, and consistently when you're away from your baby, can help build your milk supply.
- Relax and massage. Relax, hold your baby skin-to-skin, and massage your breasts before feeding to encourage your milk to let down.
- Take care of yourself. Get plenty of rest, eat well, drink enough fluids, and let others help you.
Consider Charting Your Progress
Record how often your baby is breastfeeding, for how long, and on which sides. If you are supplementing with infant formula, record how much your baby is getting and decrease the infant formula as your milk supply increases. WIC breastfeeding staff can help you determine how much infant formula your baby needs.
WIC breastfeeding staff can help you determine how much infant formula your baby needs.
Still Have Questions?
Contact your WIC breastfeeding expert. They can talk to you about supply concerns and give you tips to increase your supply to meet your baby's needs.
Low milk supply? How to increase breast milk supply
Many mums worry they have a poor milk supply, but it can be hard to know for sure. Read on to find out whether you really have low milk supply and what you can do about it
Share this content
“Have I got enough breast milk?” is something new mothers often worry about – but chances are, if your baby’s healthy and growing well you’re doing great. However, if you’re concerned about your breast milk supply, it’s important to seek advice early. If it turns out things are fine, you’ll quickly be reassured. Plus, you’ll avoid the trap of giving your baby formula unnecessarily, which may cause your own milk supply to drop.
Reasons for low milk supply
A small number of new mums have difficulty producing enough breast milk due to medical reasons, which include:
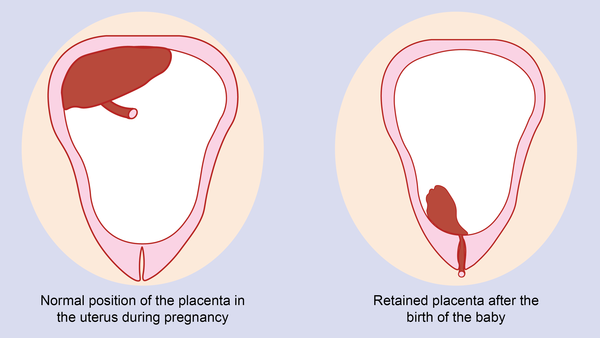
- Excessive blood loss (more than 500 ml/17.6 fl oz) during the birth or retained fragments of the placenta can delay your milk coming in (which usually happens around three days after the birth).1
- A history of polycystic ovarian syndrome, diabetes, thyroid or other hormonal disorders. Mums with these conditions sometimes experience a low milk supply.2
- The rare medical condition mammary hypoplasia, in which there isn’t enough milk-producing glandular tissue within the breast.3
- Previous breast surgeries or breast trauma – although many mums who have had surgery go on to breastfeed successfully.4
If any of these conditions applies to you, see a lactation consultant or breastfeeding specialist.
How breast milk supply works
Once your breast milk has come in, your breasts start to make milk through a process of ‘supply and demand’. Each time milk is removed, either by your baby feeding or by expressing, your breasts make more.
Each time milk is removed, either by your baby feeding or by expressing, your breasts make more.
That’s why giving bottles of formula can reduce your milk supply – your body isn’t getting the message to produce more breast milk, because none is being removed.
The way your baby nurses also affects your supply. The more frequently and effectively she breastfeeds, the more milk you’ll make. If your baby doesn’t take enough milk during a feed, it’s essential to express regularly to protect your milk supply – see below for more advice.
Signs your baby isn’t getting enough milk
Even though low milk supply is rare, your baby may still struggle to get enough for other reasons during her first few weeks. She may not be breastfeeding frequently enough, or for long enough, particularly if you’re trying to stick to a breastfeeding schedule rather than feeding on demand. She may not be latching well, or might have a condition that makes it harder to take in milk.
The following are signs your baby isn’t getting enough milk:
- Poor weight gain.
 It’s normal for newborns to lose 5% to 7% of their birth weight in the first few days – some lose up to 10%. However, after that they should gain at least 20 to 30 g (0.7 to 1 oz) per day and be back to their birth weight by day 10 to 14.5,6,7 If your baby has lost 10% or more of her birth weight, or she hasn’t started gaining weight by days five to six, you should seek medical advice immediately.
It’s normal for newborns to lose 5% to 7% of their birth weight in the first few days – some lose up to 10%. However, after that they should gain at least 20 to 30 g (0.7 to 1 oz) per day and be back to their birth weight by day 10 to 14.5,6,7 If your baby has lost 10% or more of her birth weight, or she hasn’t started gaining weight by days five to six, you should seek medical advice immediately. - Insufficient wet or dirty nappies. The number of poos and wees your baby has per day is a good indicator of whether or not she is getting enough milk – see our article explaining the pattern your baby should be following in Breastfeeding your newborn: What to expect in the first week. Seek medical advice if you’re concerned or if you have noticed her dirty nappies decreasing in wetness and heaviness.
- Dehydration. If your baby has dark-coloured urine, a dry mouth or jaundice (yellowing of the skin or eyes), or if she is lethargic and reluctant to feed, she could be dehydrated.
 6 Fever, diarrhoea and vomiting, or overheating, can cause dehydration in infants. If you notice any of these symptoms, seek medical advice quickly.
6 Fever, diarrhoea and vomiting, or overheating, can cause dehydration in infants. If you notice any of these symptoms, seek medical advice quickly.
Find out the top 5 tips to know if your baby is getting enough milk
Misconceptions about low milk supply
Newborns typically feed very often – around 10 to 12 times a day, or every two hours – and this is not a sign that you don’t have enough milk. Don’t forget that your baby also nurses for comfort, and it’s difficult to tell how much milk your baby takes during each feed – amounts can vary.
The following are all perfectly normal and are not signs of a poor milk supply:
- your baby wants to feed frequently
- your baby doesn’t want to be put down
- your baby is waking in the night
- short feeds
- long feeds
- your baby will take a bottle after a feed
- your breasts feel softer than they did in the early weeks
- your breasts don’t leak milk, or they used to leak and have stopped
- you can’t pump much milk
- you have small breasts
What to do if you have low milk supply
If you suspect your baby is not getting enough milk, see a lactation consultant or breastfeeding specialist. They will assess whether you have low milk supply and observe a breastfeed to see if your baby is latched on well and taking in enough milk. They may suggest adjusting your feeding position or your baby’s latch so she can feed more efficiently.
They will assess whether you have low milk supply and observe a breastfeed to see if your baby is latched on well and taking in enough milk. They may suggest adjusting your feeding position or your baby’s latch so she can feed more efficiently.
You could also try having more skin-to-skin contact with your baby before and during feeds to stimulate the hormone oxytocin, which gets your milk flowing. Or use relaxation techniques, such as listening to your favourite calming music, to reduce any anxiety that could be affecting your supply.8
With support, most mums with low milk supply are able to partially breastfeed their babies, and some will manage to develop a full milk supply.
If your baby is not yet taking enough milk directly from the breast, perhaps because she was premature or has special needs, you may need to express to protect your milk supply, and your healthcare professional may prescribe galactogogues (medication to increase milk production).
If you’re not yet able to express enough breast milk for your baby, you’ll need to supplement her with donor milk or formula, under the guidance of a medical professional. A supplemental nursing system (SNS) can be a satisfying way for her to get all the milk she needs at the breast.
A supplemental nursing system (SNS) can be a satisfying way for her to get all the milk she needs at the breast.
How to increase milk supply with a breast pump
If you need to encourage your milk supply in the first five days after birth, you can use a double electric breast pump with initiation technology, such as the Medela Symphony. This type of pump is designed to mimic the way a baby stimulates the breasts while feeding, and has been found to increase longer-term milk production.9
Once your milk has come in, double pumping means you can express more milk in less time.10 This method also drains the breasts better, which also helps with milk supply.
Although every mum is different, it’s often a good idea to express milk straight after, or an hour after, a feed. This may seem counterintuitive, because it’s usually easier to pump from a full breast. But you should think of your pumping session as ‘putting in a milk order’ for the next day.
At first you may only collect small amounts, but don’t be discouraged – with regular pumping, this will increase. Aim to be removing milk (by breastfeeding as well as pumping) eight to 12 times a day, including one session at night when your levels of the milk-producing hormone prolactin are highest. The more frequently milk is removed, the better. After two or three days of regular pumping you should see a significant increase in supply. For advice on getting more milk from each pumping session, read breast pumping tips.
Hands-on pumping to increase expressed milk
If your baby is not breastfeeding directly at all, or you can’t yet pump enough milk for her, a technique called ‘hands-on pumping’ can be useful. It has been shown to increase the amount of milk mums can express in a session.11,12 The whole process takes around 25 to 30 minutes. Remember, the emptier your breasts, the more quickly they’ll make milk.
Follow these simple steps:
- Massage your breasts.

- Double pump using an expressing bra to keep your hands free.
- While pumping, use your fingers and thumb to compress your breast for a few seconds. Release and repeat. Use compressions on both breasts until your milk flow slows to a trickle.
- Massage your breasts again.
- Finish by hand expressing or single pumping, using breast compressions and switching between breasts to drain them as fully as possible.
Once your baby is gaining weight and you’ve increased your supply, then you can move on to feeding her exclusively at the breast.
References
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Vanky E et al. Breastfeeding in polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2008;87(5):531-535.
3 Neifert MR et al. Lactation failure due to insufficient glandular development of the breast. Pediatrics. 1985;76(5):823-828.
4 Neifert M et al. The influence of breast surgery, breast appearance, and pregnancy-induced breast changes on lactation sufficiency as measured by infant weight gain. Birth. 1990;17(1):31-38.
5 C Tawia S, McGuire L. Early weight loss and weight gain in healthy, full-term, exclusively-breastfed infants. Breastfeed Rev. 2014;22(1):31-42.
6 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p.
7 World Health Organisation. [Internet]. Child growth standards; 2018 [cited 2018 Feb]
8 Keith DR et al. The effect of music-based listening interventions on the volume, fat content, and caloric content of breast milk-produced by mothers of premature and critically ill infants. Adv Neonatal Care. 2012;12(2):112-119
9 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J Perinatol. 2012;32(2):103-10.
J Perinatol. 2012;32(2):103-10.
10 Prime DK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med. 2012;7(6):442-447.
11 Stanford University School of Medicine [Internet]. Stanford, CA, USA: Maximizing Milk Production with Hands-On Pumping; 2017. [Accessed 30.04.2018].
12 Morton J et al. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J Perinatol. 2009;29(11):757-764.
Signs of lack of milk | Improving lactation
Many mothers are concerned about insufficient milk production, but it is not always easy to find out if milk is really low. Read our article to understand if this is true and what can be done about it.
Share this information
“Do I have enough milk?” - a question that is often asked by young mothers. If your baby is healthy and growing well, there is no reason to worry. However, if you are still worried about milk production, it is best to consult a specialist as soon as possible. If everything is in order, he will be able to calm you down. In addition, you will not needlessly feed the baby formula, because of which milk production can really decrease.
However, if you are still worried about milk production, it is best to consult a specialist as soon as possible. If everything is in order, he will be able to calm you down. In addition, you will not needlessly feed the baby formula, because of which milk production can really decrease.
Causes of insufficient milk supply
Some mothers do not produce enough breast milk for medical reasons, which include: approximately three days after birth). 1
If you have any of the conditions listed, contact your lactation consultant or healthcare provider.
How milk is produced
With the advent of milk, the breast begins to work on the principle of supply and demand. Each time after it is emptied, whether it is feeding the baby or pumping, even more milk will be produced.
This is why milk production may be reduced if you give formula to your baby - your body will not get the signal to produce more milk because it will remain.
The way your baby eats also affects milk production. The more often and better he sucks the breast, the bigger it will be. If your baby eats only a small portion at one feeding, it is necessary to express milk regularly to maintain the level of its production. Read more about this below.
Signs that the baby is not getting enough milk
Although low milk production is rare, the baby may have difficulty feeding in the first few weeks, but for other reasons. You may not be feeding him often enough or for enough time, especially if you're trying to stick to a specific schedule. The baby may not latch on properly, or it may have features that make it difficult to take in milk.
The baby may not latch on properly, or it may have features that make it difficult to take in milk.
The following signs indicate that the baby is not getting enough milk:
- Poor weight gain. In the first few days of life, newborns normally lose 5 to 7%, and sometimes even up to 10%, of their birth weight. However, after that, they should gain at least 20–30 g per day and regain their birth weight by 10–14 days. 5,6,7 If your baby has lost 10% or more of their weight in the early days, or has not started gaining weight by 5-6 days, you should contact your doctor immediately.
- Not enough wet and soiled diapers. A good indicator of whether a baby is getting enough milk is the number of diapers used per day. Check out our article detailing the norm for wet and soiled diapers in Breastfeeding Your Newborn: What to Expect in the First Week. Seek medical advice if something bothers you or you notice that the number of soiled diapers has begun to decrease.

- Dehydration. If your baby has dark urine, dry mouth or jaundice (yellowing of the skin or eyes), or baby is lethargic, has lost appetite, and may be dehydrated. 6 Dehydration can be caused by fever, diarrhoea, vomiting or overheating. If you notice any of these symptoms, seek medical attention as soon as possible.
Misconceptions about lack of milk
Newborns usually eat very frequently, about 10-12 times a day or every two hours. This does not mean that they do not have enough milk. Keep in mind that breastfeeding is also about comfort, so it's hard to tell how much milk a baby eats at each feed as the amount can vary.
You have enough milk even if:
- the child wants to eat often;
- the child does not want to be laid down;
- the child wakes up at night;
- feeding is fast;
- feeding takes a long time;
- after feeding, the child takes another bottle;
- Your breasts are softer than in the first weeks;
- milk does not leak or has stopped leaking;
- You cannot express much milk;
- You have small breasts.

What to do if your milk supply is low
If you suspect that your baby is not getting enough milk, contact your lactation consultant or your doctor. It will determine if you are getting enough milk and check how your baby is latch-on and getting enough milk. He may also suggest changing the feeding position or the way the baby is attached to the breast to make it easier.
Also try holding your baby close to you more often to increase skin-to-skin contact before and during feedings. This stimulates the production of the hormone oxytocin, which promotes milk flow. Use relaxation techniques, such as listening to your favorite soothing music, to reduce anxiety that can negatively impact milk production. 8
With proper support, most under-lactating mothers can breastfeed their babies at least partially, and some manage to normalize production.
If your baby is unable to get enough milk directly from the breast (perhaps because he was born prematurely or has special needs), you need to express milk to support his production. Your doctor may prescribe you special drugs that stimulate lactation.
Your doctor may prescribe you special drugs that stimulate lactation.
If you are unable to express enough milk, you will need to supplement your baby with donor milk or formula. This should also take place under the supervision of a physician. The Supplemental Nursing System (SNS)* is a great way to help your baby get all the milk he needs at the breast.
How to increase your milk production with a breast pump
If you need to increase your milk production in the first five days after giving birth, you can use a dual electronic breast pump with lactation start technology, such as the Medela Symphony**. Such a breast pump imitates the sucking of the breast by a child and helps to increase milk production in the future. 9
After your milk comes in, double pumping will allow you to get more milk in less time. 10 This method helps to better empty the breast, which also improves lactation.
Although every mother is different, it is often recommended to express milk immediately or one hour after a feed. This may seem strange, since it is usually easier to express milk from a full breast. However, the pumping session should be seen as an "investment in tomorrow."
This may seem strange, since it is usually easier to express milk from a full breast. However, the pumping session should be seen as an "investment in tomorrow."
You will probably only be able to express a little milk at first, but don't be discouraged - if you express regularly, your milk supply will increase. Aim to empty your breasts—whether by breastfeeding or expressing milk—8 to 12 times a day, including one at night when your prolactin (milk-producing hormone) levels are highest. The more often you empty your chest, the better. After two to three days of regular pumping, you will notice a significant increase in milk production. For tips on how to get more milk with every pump, see Tips for Using a Breast Pump.
Pumping with massage to get more milk
If your baby is not lating at all or you are not yet able to express enough milk for him, a technique called “massage pumping” may be helpful. It helps mothers increase the amount of milk they get in one pumping session.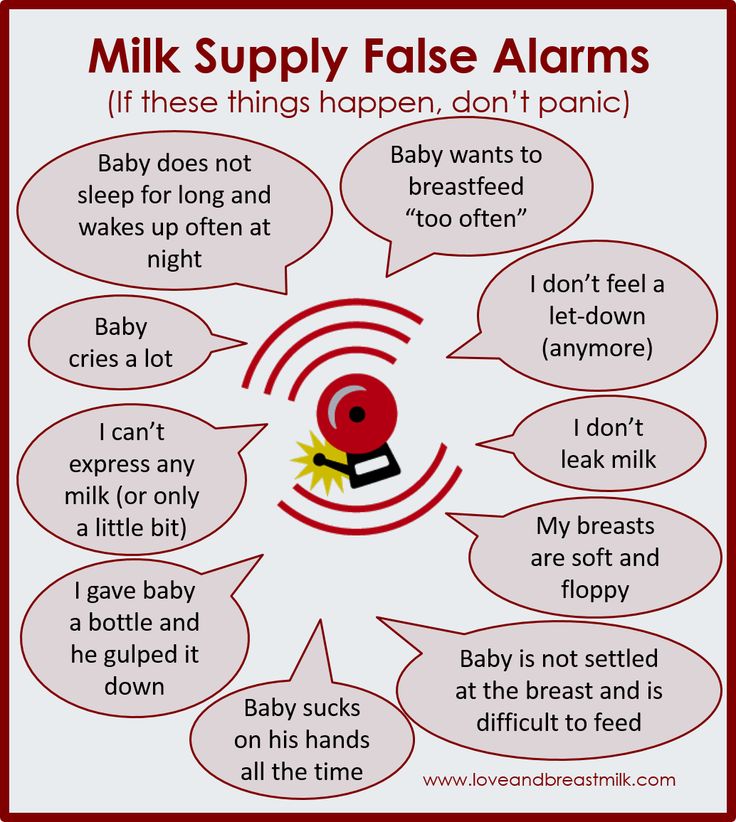 11.12 The whole process takes about 25-30 minutes. Remember that the better you empty your breast, the faster milk is produced in it.
11.12 The whole process takes about 25-30 minutes. Remember that the better you empty your breast, the faster milk is produced in it.
A few simple steps are required:
- Massage your breasts.
- Perform a double pump while wearing a special bustier top that allows you to keep your hands free.
- While expressing, squeeze the chest with all fingers for a few seconds. Release and repeat. Squeeze both breasts until the milk flows in a thin stream.
- Massage your chest again.
- Express milk manually or with a single breast pump, squeezing each breast in turn to empty them as completely as possible.
When your baby starts to gain weight and milk production increases, you can switch to exclusive breastfeeding.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." J Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
- Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." J Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Vanky Breastfeeding in polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2008;87(5):531-535. - Wanky, I. et al., "Breastfeeding in the setting of polycystic ovaries." Akta Obstet Ginecol Scand. 2008;87(5):531-535.
3 Neifert MR et al. Lactation failure due to insufficient glandular development of the breast. Pediatrics. 1985;76(5):823-828. - Neifert M.R. et al., "Inability to Lactate Due to Deficiency of Glandular Breast Tissue". Pediatrix (Pediatrics). 1985;76(5):823-828.
4 Neifert M et al. The influence of breast surgery, breast appearance, and pregnancy-induced breast changes on lactation sufficiency as measured by infant weight gain. Birth. 1990;17(1):31-38. - Neifert M. et al., "Influence of breast surgery, breast appearance, and pregnancy-induced breast changes on milk supply as measured by weighing the baby." Bers. 1990;17(1):31-38.
Birth. 1990;17(1):31-38. - Neifert M. et al., "Influence of breast surgery, breast appearance, and pregnancy-induced breast changes on milk supply as measured by weighing the baby." Bers. 1990;17(1):31-38.
5 C Tawia S, McGuire L. Early weight loss and weight gain in healthy, full-term, exclusively-breastfed infants. Breastfeed Rev . 2014;22(1):31-42. - S. Tavia S., McGuire L., Neonatal Weight Loss and Gain in Healthy, Exclusively Breastfed Full-Term Infants. Brestfeed Rev (Breastfeeding Review). 2014;22(1):31-42.
6 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
P. 1128.
7 World Health Organization. [Internet]. Neonatal Care . 2012;12(2):112-119 - Keith D.R. et al., "Effects of listening to music on the quantity, fat content, composition and calorie content of breast milk in mothers of premature and seriously ill children." Adv Neonatal Care. 2012;12(2):112-119
9 Meier PP et al. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. J. Perinatol. 2012;32(2):103-10. - Meyer P.P. et al., "Pumping patterns that mimic breastfeeding behavior: more milk and less time for constantly pumping mothers of preterm infants." J Perinatol (Journal of Perinatology). 2012;32(2):103-10.
10 Prime DK et al. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med . 2012;7(6):442-447. - Prime D.K. and co-authors. "During the period of breastfeeding, the simultaneous pumping of both breasts is more productive than consecutive." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
Breastfeed Med . 2012;7(6):442-447. - Prime D.K. and co-authors. "During the period of breastfeeding, the simultaneous pumping of both breasts is more productive than consecutive." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
11 Stanford University School of Medicine [Internet]. Stanford, CA, USA: Maximizing Milk Production with Hands-On Pumping; 2017. [ Accessed 04/30/2018]. - Stanford University School of Medicine [Internet]. Stanford, CA, USA: "Increased milk production from hand expression"; 2017. [Page accessed 04/30/2018].
12 Morton J et al. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J. Perinatol. 2009;29(11):757-764. - Morton J. et al., "Manual pumping combined with an electric breast pump increases breast milk production in mothers of preterm infants. " J Perinatol (Journal of Perinatology). 2009;29(11):757.
" J Perinatol (Journal of Perinatology). 2009;29(11):757.
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. ФСЗ 2010/07352 dated 07/19/10
** RU No. ФСЗ 2010/06525 dated 03/17/2021
Lack of milk in a nursing mother
The ideal food for a baby is breast milk, which contains enough enzymes, hormones and vitamins. There is no equivalent analogues to this unique product. It consists of almost 700 components, each of which plays an important role in the growth of the baby. Many of the constituents of breast milk cannot be artificially recreated. For example, in the milk formula of any brand, presented on the shelves of stores and pharmacies, contains 10 times fewer components.
The advantages of breast milk are expressed in its nutritional value, good digestibility. It contains leukocytes, various anti-infectious factors that protect the newborn from dangerous diseases. The polyunsaturated fatty acids contained in this product help the child's brain to fully develop. The indisputable advantages of breastfeeding include the possibility of forming a close emotional connection between the baby and mother.
The polyunsaturated fatty acids contained in this product help the child's brain to fully develop. The indisputable advantages of breastfeeding include the possibility of forming a close emotional connection between the baby and mother.
Every woman who carries a 9-month-old baby under her heart has heard about the benefits of natural lactation. All this time she is waiting for a meeting with the baby, not doubting how she will feed him. Therefore, after the first meeting and an exciting adaptation period, the situation becomes completely unexpected when one morning the feeling of fullness disappears in the chest. Not fully understanding what is happening, the mother tries to feed the screaming baby, but for some reason he refuses to eat: he cries, takes the breast again, then quits, behaves anxiously and does not calm down.
Frequent attachment, changing breasts and feeding positions are completely ineffective. After a few days of such a struggle, the woman falls into despair and decides to stop breastfeeding. The child is bought infant formula, hoping to end this turbulent period as soon as possible. However, such drastic decisions should not be made in a hurry.
The child is bought infant formula, hoping to end this turbulent period as soon as possible. However, such drastic decisions should not be made in a hurry.
The main task of the mother is to find the strength in herself to fight for the preservation of lactation. It is important to remember that such a problem, regardless of the reasons that provoked it, in most cases can be solved with a positive outcome.
How to understand that there is a shortage of milk
Put the panic on the back burner and put in a little effort to sort out the situation. If after feeding the baby cries, after a short time it again requires a breast, then it is worth being worried about his condition. However, it is important to understand that the cause of such behavior of the child is not always hunger.
Possible causes:
-
A highly developed sucking reflex, which the baby will be able to realize with close tactile contact with his mother.

-
The child is weak or unwell, which is why he refuses to eat.
-
A lactation crisis has set in - a nursing woman can encounter such a phenomenon at 1.5-2 months, and it is usually associated with the growth of the baby (more milk is required, but the female body needs some time to adapt to new conditions).
-
The psychological mood of the mother is disturbed - an important fact that should not be underestimated. It is extremely important that comfortable conditions are created for a nursing woman, excluding stressful situations. Family statements such as “You don’t have enough milk” significantly increase the chances of stopping breastfeeding.
-
A small child is incorrectly applied to the breast - the mouth is not open wide, most of the chest areola is under the baby's mouth (and should be placed above it), the mother feels constant pain during feeding (the result of an incorrectly taken posture, due to which the child's tongue does not take up space on gum or there is a problem with a short frenulum).

The easiest way to make sure you're getting enough milk is to do the "wet diaper test". To do this, you will need to remove the diaper from the crumbs for a day to calculate the amount of urination. If there are at least 8 of them, then there is no reason to worry.
Signs of lack of milk:
-
Problems with weight gain - the child's body weight increases slightly, remains unchanged or decreases.
-
A small daily amount of urination - less than 8 times, concentrated urine (dark, with a strong odor).
-
Decreased stool frequency - less than 3 times a day (for a child 1.5 months old).
Even after making sure of the presence of these factors, a nursing woman should not independently decide on the completion of lactation. It is recommended that you talk to your doctor, breastfeeding consultants (if available in your area), moms with positive lactation experiences, and try to make some successful breastfeeding strategies a reality.
How to solve the problem of lack of milk
To stimulate lactation, lactating women are recommended:
-
Apply regularly to the breast, without a regimen, on demand - in the first six months of a baby's life, you do not need to try to withstand 2-3 hours between feedings. The principle of operation of the mammary glands is simple: the more often and more the child eats, the more milk is produced. Especially important are night feedings, which stimulate the production of the hormone oxytocin (responsible for the appearance of milk).
-
Develop a positive attitude - block bad thoughts, think only about yourself and the baby. Avoid stressful situations during which the production of oxytocin is blocked. The key to successful lactation is also a good rest - physical and emotional.
-
Eat right - this item is relevant for any person on the planet, and nursing mothers cannot be an exception. Unfortunately, the appearance of a new family member who requires maximum attention is often accompanied by problems in the nutrition of the new mother.
 In this situation, it is important to remember that good lactation cannot exist without good nutrition. A balanced, thoughtful diet affects not only the quality of milk, but also its quantity.
In this situation, it is important to remember that good lactation cannot exist without good nutrition. A balanced, thoughtful diet affects not only the quality of milk, but also its quantity. -
Use physiotherapy methods to improve lactation - a set of special physical exercises for the back muscles, massage of the chest, the area between the shoulder blades, massage of the collar zone, the use of a contrast shower, warming the legs, hands in hot water will help improve blood flow in the mammary glands (an important condition for normal lactation) .
| Important! Properly organized co-sleeping allows you to make night feedings as comfortable as possible. For example, a crib can be moved to the parents' bed. As a result, the mother will be able to feed the baby without getting up. If he is sleeping, do not wake him up, but simply offer a breast - most babies can eat even in a dream. |
The benefits of lactation infusions and teas for a nursing mother
Drinking enough fluids plays an important role in milk production. The category of popular methods for improving breastfeeding includes special herbal teas, for example, "LaktoMama" , manufactured by the company "Evalar". This product is a collection of herbs grown in the ecologically clean foothills of Altai. It does not contain chemicals, pesticides or other hazardous substances.
As part of LaktoMama tea:
-
Stinging nettle has a pronounced hemostatic effect, which is especially important for the normalization of the contractile function of the uterus of a nursing mother and a significant increase in lactation, it is used to combat anemia, atherosclerosis, beriberi.
-
Fennel seeds - promote milk production, improve appetite, reduce the risk of gas formation in the gastrointestinal tract of a small child.

-
Melissa - helps to achieve an increase in milk production, shows a slight sedative effect.
-
Oregano is another component that activates lactation, the work of the gastrointestinal tract, helps to get rid of spasms, headaches, has multiple properties, including urinary, bile, diaphoretic.
-
Cumin - has a lactagon effect, also shows an antispasmodic and wind-relieving effect.
Tea "Evalar BIO LaktoMama" is presented in the form of convenient filter bags, each of which should be brewed in 200 ml of boiling water. In order for the herbs to give up their beneficial substances, the tea must be infused for 10-15 minutes. Drinking such a herbal drink is recommended twice a day - in the morning and in the evening.
Benefits of tea "Evalar BIO LaktoMama":
-
antimicrobial treatment of plant materials (the "instant steam" method using a French installation) - contributes not only to disinfection, but also to the fermentation of the finished product, which significantly increases its usefulness;
-
packaging in the form of multilayer protective envelopes that preserve the healing properties, delicate taste and aroma of herbs;
-
more favorable cost in comparison with available analogues.