Multiple fetus pregnancy
Multiple Pregnancy | ACOG
-
A pregnancy with more than one fetus is called a multiple pregnancy.
-
If more than one egg is released during the menstrual cycle and each egg is fertilized by a sperm, more than one embryo may implant and grow in the uterus. This type of pregnancy results in fraternal twins (or more). When a single fertilized egg splits, it results in multiple identical embryos. This type of pregnancy results in identical twins (or more). Fraternal twins are more common than identical twins.
-
The use of fertility drugs to induce ovulation often causes more than one egg to be released from the ovaries and can result in twins, triplets, or more.
In vitro fertilization (IVF) can lead to a multiple pregnancy if more than one embryo is transferred to the uterus.
Identical multiples also may result if the fertilized egg splits after transfer.
Women older than age 35 are more likely to release two or more eggs during a single menstrual cycle than younger women. So older women are more likely than younger women to become pregnant with multiples.
-
Women who are pregnant with multiples may have more severe morning sickness or breast tenderness than women who are pregnant with a single fetus. They also may gain weight more quickly. Most multiple pregnancies are discovered during an ultrasound exam.
-
Most women who are pregnant with multiples need to gain more weight than women who are pregnant with one fetus. An extra 300 calories a day is needed for each fetus. For example, if you are pregnant with twins, you need an extra 600 calories a day.
 For triplets and more, talk with your obstetrician–gynecologist (ob-gyn) about the right amount of weight gain for your pregnancy.
For triplets and more, talk with your obstetrician–gynecologist (ob-gyn) about the right amount of weight gain for your pregnancy. -
Staying active during multiple pregnancy is important for your health, but you may need to avoid strenuous exercise. Try low-impact exercise, such as swimming, prenatal yoga, and walking. You should aim for 30 minutes of exercise a day. If problems arise during your pregnancy, your ob-gyn may recommend that you avoid exercise.
-
You likely will have more frequent prenatal care visits with your ob-gyn. Starting in your second trimester, you may have ultrasound exams every 4 to 6 weeks. If a problem is suspected, you may have special tests or more frequent ultrasound exams.
-
The most common complication of multiple pregnancy is preterm birth.
 More than one half of all twins are born preterm. Triplets and more are almost always born preterm.
More than one half of all twins are born preterm. Triplets and more are almost always born preterm. -
Babies born before 37 weeks of pregnancy may have an increased risk of short-term and long-term health problems, including problems with breathing, eating, and staying warm. Other problems, such as learning and behavioral disabilities, may appear later in childhood or even in adulthood. Very preterm babies (those who are born before 32 weeks of pregnancy) can die or have severe health problems, even with the best of care.
Preterm multiples also have a greater risk of serious complications that can lead to cerebral palsy. Children born with problems related to being preterm may need lifelong medical care.
-
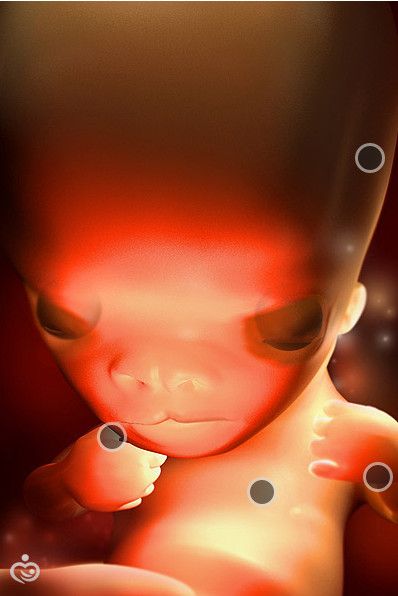
Early in a multiple pregnancy, an ultrasound exam is done to find out whether each fetus has its own chorion (chorionicity) and amniotic sac (amnionicity).
 There are three types of twins:
There are three types of twins:-
Dichorionic–diamniotic—Twins who have their own chorions and amniotic sacs. They typically do not share a placenta and can be fraternal or identical.
-
Monochorionic–diamniotic—Twins who share a chorion but have separate amniotic sacs. They share a placenta and are identical.
-
Monochorionic–monoamniotic—Twins who share one chorion and one amniotic sac. They share a placenta and are identical.
-
-
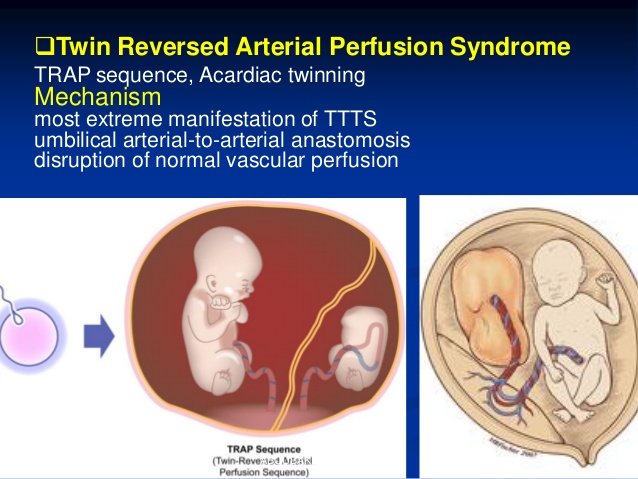
Monochorionic twins have a higher risk of complications than those with separate placentas. One problem that can occur in monochorionic–diamniotic babies is twin–twin transfusion syndrome (TTTS). In TTTS, the blood flow between the twins becomes unbalanced. One twin donates blood to the other twin. The donor twin has too little blood, and the recipient twin has too much blood.
 The earlier TTTS occurs in the pregnancy, the more serious the outcomes for one or both babies.
The earlier TTTS occurs in the pregnancy, the more serious the outcomes for one or both babies.Although monochorionic–monoamniotic babies are rare, this type of pregnancy is very risky. The most common problem is an umbilical cord complication. Women with this type of pregnancy are monitored more frequently and are likely to have a cesarean birth.
-
Preeclampsia is a blood pressure disorder that usually starts after 20 weeks of pregnancy or after childbirth. It occurs more often in multiple pregnancies than in singleton pregnancies. It also tends to occur earlier and is more severe in multiple pregnancies.
Preeclampsia can damage many organs in your body, most commonly your kidneys, liver, brain, and eyes. Preeclampsia that worsens and causes seizures is called eclampsia. When preeclampsia occurs during pregnancy, the babies may need to be delivered right away, even if they are not fully grown.

-
Women carrying multiples have a high risk of gestational diabetes. This condition can increase the risk of preeclampsia and of developing diabetes mellitus later in life. Newborns may have breathing problems or low blood sugar levels. Diet, exercise, and sometimes medication can reduce the risk of these complications.
-
Multiples are more likely to have growth problems than single babies. Multiples are called discordant if one fetus is much smaller than the others.
Discordant growth is common with multiples. It does not always signal a problem. Sometimes, though, a fetus’s restricted growth may be caused by an infection, TTTS, or a problem with the placenta or umbilical cord. If growth restriction is suspected in one or both fetuses, frequent ultrasound exams may be done to track how the fetuses are growing.

-
Screening tests for genetic disorders that use a sample of a woman's blood are not as sensitive in multiple pregnancy. It is possible to have a positive screening test result when no problem is present in either fetus.
-
Diagnostic tests for birth defects include chorionic villus sampling (CVS) and amniocentesis. These tests are harder to perform in multiples because each fetus must be tested. There also is a small risk of loss of one or all of the fetuses. Results of these tests may show that one fetus has a disorder, while the others do not.
-
The chance of cesarean birth is higher with multiples. In some cases, twins can be delivered by vaginal birth. How your babies are born depends on
-
the number of babies and the position, weight, and health of each baby
-
your health and how your labor is going
-
the experience of your ob-gyn
-
-
Having multiples might increase your risk of postpartum depression.
 If you have intense feelings of sadness, anxiety, or despair that keep you from being able to do your daily tasks, talk with your ob-gyn or other member of your health care team.
If you have intense feelings of sadness, anxiety, or despair that keep you from being able to do your daily tasks, talk with your ob-gyn or other member of your health care team. -
Yes, but it may take some practice. Your milk supply will increase to the right amount. You will need to eat healthy foods and drink plenty of liquids. Lactation specialists are available at many hospitals and in your community to help you work out any problems you may have.
[See How to Prepare for Breastfeeding in the Month Before Birth]
-
Amniocentesis: A procedure in which amniotic fluid and cells are taken from the uterus for testing. The procedure uses a needle to withdraw fluid and cells from the sac that holds the fetus.
Amnionicity: The number of amniotic (inner) membranes that surround fetuses in a multiple pregnancy.
 When multiple fetuses have only one amnion, they share an amniotic sac.
When multiple fetuses have only one amnion, they share an amniotic sac.Amniotic Sac: Fluid-filled sac in a woman’s uterus. The fetus develops in this sac.
Birth Defects: Physical problems that are present at birth.
Cerebral Palsy: A disorder of the nervous system that affects movement, posture, and coordination. This disorder is present at birth.
Cesarean Birth: Birth of a fetus from the uterus through an incision made in the woman’s abdomen.
Chorion: The outer membrane that surrounds the fetus.
Chorionic Villus Sampling (CVS): A procedure in which a small sample of cells is taken from the placenta and tested.
Chorionicity: The number of chorionic (outer) membranes that surround the fetuses in a multiple pregnancy.
Complication: A disease or condition that happens as a result of another disease or condition.
 An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.
An example is pneumonia that occurs as a result of the flu. A complication also can occur as a result of a condition, such as pregnancy. An example of a pregnancy complication is preterm labor.Diabetes Mellitus: A condition in which the levels of sugar in the blood are too high.
Diagnostic Tests: Tests that look for a disease or cause of a disease.
Discordant: A large difference in the size of fetuses in a multiple pregnancy.
Eclampsia: Seizures occurring in pregnancy or after pregnancy that are linked to high blood pressure.
Egg: The female reproductive cell made in and released from the ovaries. Also called the ovum.
Embryo: The stage of development that starts at fertilization (joining of an egg and sperm) and lasts up to 8 weeks.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Fraternal Twins: Twins that have developed from two different fertilized eggs.

Genetic Disorders: Disorders caused by a change in genes or chromosomes.
Gestational Diabetes: Diabetes that starts during pregnancy.
Identical Twins: Twins that have developed from a single fertilized egg that are usually genetically identical.
In Vitro Fertilization (IVF): A procedure in which an egg is removed from a woman’s ovary, fertilized in a laboratory with the man’s sperm, and then transferred to the woman’s uterus to achieve a pregnancy.
Menstrual Cycle: The monthly process of changes that occur to prepare a woman’s body for possible pregnancy. A menstrual cycle is defined as the first day of menstrual bleeding of one cycle to the first day of menstrual bleeding of the next cycle.
Multiple Pregnancy: A pregnancy where there are two or more fetuses.
Obstetrician–Gynecologist (Ob-Gyn): A doctor with special training and education in women’s health.

Ovaries: Organs in women that contain the eggs necessary to get pregnant and make important hormones, such as estrogen, progesterone, and testosterone.
Ovulation: The time when an ovary releases an egg.
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Postpartum Depression: A type of depressive mood disorder that develops in the first year after the birth of a child. This type of depression can affect a woman’s ability to take care of her child.
Preeclampsia: A disorder that can occur during pregnancy or after childbirth in which there is high blood pressure and other signs of organ injury. These signs include an abnormal amount of protein in the urine, a low number of platelets, abnormal kidney or liver function, pain over the upper abdomen, fluid in the lungs, or a severe headache or changes in vision.
Prenatal Care: A program of care for a pregnant woman before the birth of her baby.

Preterm: Less than 37 weeks of pregnancy.
Screening Tests: Tests that look for possible signs of disease in people who do not have signs or symptoms.
Sperm: A cell made in the male testicles that can fertilize a female egg.
Twin–Twin Transfusion Syndrome (TTTS): A condition of identical twins in which one twin gets more blood than the other during pregnancy.
Ultrasound Exam: A test in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Umbilical Cord: A cord-like structure containing blood vessels. It connects the fetus to the placenta.
Uterus: A muscular organ in the female pelvis. During pregnancy, this organ holds and nourishes the fetus. Also called the womb.
Don't have an ob-gyn? Search for doctors near you.
FAQ188
Last updated: February 2021
Last reviewed: June 2020
Copyright 2022 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information.
This information is designed as an educational aid for the public. It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer.
Twins, Triplets, Complications & Symptoms
What is a multiple pregnancy?
A multiple pregnancy is a pregnancy where you’re carrying more than one baby at a time. If you’re carrying two babies, they are called twins. Three babies that are carried during one pregnancy are called triplets. You can also carry more than three babies at one time (high-order multiples). There are typically more risks linked to a multiple pregnancy than a singleton (carrying only one baby) pregnancy.
How do multiple pregnancies happen?
There are two main ways that a multiple pregnancy can happen:
- One fertilized egg (ovum) splits before it implants in the uterine lining.
- Two or more separate eggs are fertilized by different sperm at the same time.
These two different types of multiple pregnancy result in either identical or fraternal siblings. The difference between identical and fraternal babies goes back to how the multiple pregnancy happens.
Identical twins or triplets happen when a single egg is fertilized and then later splits. These newly divided embryos are identical. Children that are identical multiples will look like each other and be the same sex.
Fraternal multiples develop from separate eggs that are fertilized by a different sperm. Because these are different eggs and different sperm, the genetic material is varied. These children won’t look identical and can be different sexes from each other.
In a pregnancy with triplets or more, your babies could be all identical, all fraternal or a mixture of both. This can happen if your body releases multiple eggs and more than one is fertilized. In a case where you have both identical and fraternal multiples, more than one egg was fertilized and then at least one of those eggs also split after fertilization.
This can happen if your body releases multiple eggs and more than one is fertilized. In a case where you have both identical and fraternal multiples, more than one egg was fertilized and then at least one of those eggs also split after fertilization.
Are identical twins or triplets always the same sex?
Because identical twins or triplets share genetic material, they are always the same sex. The sex of a baby is determined by the particular sperm cell that fertilizes the egg at conception. There are two kinds of sperm cells — those carrying an X chromosome or Y chromosome. The mother’s egg carries an X chromosome. If a sperm cell carrying an X chromosome fertilizes the egg, it will make a XX combination (female). If the sperm cell is carrying a Y chromosome, you end up with an XY pairing (male).
Identical multiples start as one egg and then split, so whatever chromosome combination is present at fertilization is the sex of all multiples.
What increases the chance of a multiple pregnancy?
There are several factors that can increase the risk of a multiple birth. You might be at a higher risk of getting pregnant with more than one baby at a time if you:
You might be at a higher risk of getting pregnant with more than one baby at a time if you:
- Are older (women in their 30s are at a higher risk of multiples because the body starts to release multiple eggs at one time when you get older).
- Are a twin yourself or have twins in your family.
- Are using fertility drugs.
You might also be at a higher risk of a multiple pregnancy if you are taller than average or have a higher body weight.
Another risk factor for a multiple pregnancy is genetic. There is an increased possibility of a multiple pregnancy if you are a multiple yourself, or if multiples run in your family. This heredity trait is generally passed down through the maternal (mother’s) side of the family.
The use of fertility drugs can be another reason you might have a multiple birth. Treatments for infertility can increase your risk of a multiple pregnancy because procedures, like in vitro fertilization (IVF), often involve transferring more than one fertilized egg into your uterus. Your provider usually transfers more than one egg at a time to increase the odds of a successful pregnancy.
Your provider usually transfers more than one egg at a time to increase the odds of a successful pregnancy.
How common are multiple births?
Multiple births have become more common in recent years because more people are using fertility drugs and procedures, such as IVF, to help conceive a baby.
What are the signs of a multiple pregnancy?
The only way to know if you’re pregnant with more than one baby during your pregnancy is through an ultrasound exam with your healthcare provider. During this test, your provider can look at images of the inside of your uterus and confirm how many babies are in there.
You might experience more intense symptoms during a multiple pregnancy than with a single pregnancy. These can include:
- Severe nausea and vomiting (morning sickness).
- Rapid weight gain in the first trimester of pregnancy.
- Sore or very tender breasts.
- High human chorionic gonadotrophin (hCG) levels — this hormone is made during pregnancy and is what a pregnancy test picks up.

- High amounts of the protein alpha-fetoprotein in your blood.
Apart from an ultrasound, your provider might suspect multiples if there’s more than one heartbeat detected during a fetal Doppler scan.
What complications are linked to multiple births?
Anyone can experience complications during pregnancy — regardless of how many babies you’re carrying. However, most healthcare providers consider multiple pregnancies higher risk than single pregnancies. This doesn’t mean that every woman who carries more than one baby during a pregnancy is going to have problems. If you’re pregnant with multiples, your provider will want to watch you for possible complications that can happen when you carry more than one baby at once. Your provider will talk to you about each risk factor and frequently check with you to make sure you aren’t experiencing anything concerning.
Possible complications include:
- Premature labor and birth: The most common complication of multiple births is premature labor.
 If you’re pregnant for multiples, you are more likely to go into premature labor (before 37 weeks) than a woman carrying only one baby. The goal for many moms of multiples is to complete 37 weeks. This is considered term in a twin pregnancy and reaching this week of gestation increases the chance the babies will be born healthy and at a good weight. Babies that are born prematurely are at risk of another complication of multiple births — low birth weight.
If you’re pregnant for multiples, you are more likely to go into premature labor (before 37 weeks) than a woman carrying only one baby. The goal for many moms of multiples is to complete 37 weeks. This is considered term in a twin pregnancy and reaching this week of gestation increases the chance the babies will be born healthy and at a good weight. Babies that are born prematurely are at risk of another complication of multiple births — low birth weight. - Preeclampsia or gestational hypertension (high blood pressure): High blood pressure is called hypertension. During pregnancy, your healthcare provider will watch your blood pressure carefully to make sure you don’t develop gestational hypertension (high blood pressure during pregnancy). This can lead to a dangerous condition called preeclampsia. Complications related to high blood pressure happen at twice the rate in women carrying multiples compared to women pregnant with only one baby.
 This complication also tends to happen earlier in pregnancy and be more severe in multiple pregnancies than single pregnancies.
This complication also tends to happen earlier in pregnancy and be more severe in multiple pregnancies than single pregnancies. - Gestational diabetes: You can develop diabetes during pregnancy. This happens because of the increased amount of hormones from the placenta. The size of the placenta can also be a factor in this condition. If you have two placentas, there’s an increased resistance to insulin.
- Placenta abruption: This condition happens when the placenta detaches (separates) from the wall of your uterus before delivery. This is an emergency situation. Placenta abruption is more common in women who are carrying multiples.
- Fetal growth restriction: This condition can also be called intrauterine growth restriction (IUGR) or small for gestational age (SGA). This condition happens when one or more of your babies is not growing at the proper rate. This condition might cause the babies to be born prematurely or at a low birth-weight.
 Nearly half of pregnancies with more than one baby have this problem.
Nearly half of pregnancies with more than one baby have this problem.
Fraternal twins always have two placentas. The risks of pregnancies with fraternal twins are similar to those of pregnancies with only one baby. However, the number of possible risks are increased when compared to pregnancies with one baby.
Identical twins may have one placenta (70% of the cases) or two placentas (30% of the cases). The risks of identical twins with two placentas are similar to those listed above for fraternal twins. Identical twins with one placenta (called monochorionic) have risks that are unique to them. In 5 to 15% of the cases, they may develop a condition called twin-twin-transfusion-syndrome (TTTS). This is the consequence of vascular communications at the placenta level between the twins. Due to these communications, the twins may share their blood. When this happens — if nothing is done — there is a 90% risk that the twins will die in-utero. In-utero procedures are performed to decrease the fetal death risk for the twins.
Another complication that can happen in identical twins with one placenta is called twin-anemia-polycythemia sequence (TAPS). This is due to blood that goes from one twin to the co-twin because of vascular communications at the placental level. In this condition, one twin becomes anemic (low red-blood cells), whereas the co-twin becomes polycythemic (too many red-blood cells). Several treatments/interventions are performed when this happens.
A third condition that can occur in identical twins with one placenta is called” selective IUGR”. One twin grows well, whereas the co-twin does not experience much growth.
Another condition typical of identical twins is called twin-reversed-arterial-perfusion syndrome. In this condition, the heart of one twin pumps blood for the circulation of both twins. One twin does not have the heart and will not survive following birth. The outcome of the twin with the normal heart varies. Fortunately, this syndrome is rare (1 in 20,000 to 40,000) and it is amenable to in-utero procedures.
Identical twins with one placenta may also be in the same sac. They are called monochorionic (one placenta)-monoamniotic (one gestational sac). This pregnancy occurs in 1% of multiple gestations and it’s associated with an increased risk for one or both twins.
Your healthcare provider will diagnose the above conditions with an ultrasound.
Am I more likely to have a C-section delivery if I’m carrying multiples?
A cesarean section is a procedure used to deliver a baby through an incision (cut) in the abdomen. This type of delivery might be used for a variety of reasons, but it’s fairly common in multiple births. Your chance of having a C-section for a multiple birth is higher than if you were pregnant for only one baby. However, even in single births, a C-section can sometimes be the safest option for delivery.
Often, the babies aren’t in the right position for birth — head down. A C-section can also happen if you have a complication during pregnancy that means a vaginal birth isn’t the safest option for you or your babies. Your healthcare provider will monitor you leading up to your due date and talk to you about the best option for delivery.
Your healthcare provider will monitor you leading up to your due date and talk to you about the best option for delivery.
What can I do to stay healthy during a multiple pregnancy?
Eating nutritious foods, getting enough rest, and visiting the doctor regularly are important steps for any pregnant woman to take toward a healthy pregnancy. These steps are especially important during multiple pregnancies.
If you’re expecting multiples, you have additional dietary needs to meet. Getting enough protein and enough hydration (fluids) is important. You’ll also need to make sure you get enough extra calories for the developing fetuses. One rule of thumb is to eat an extra 300 calories a day per baby. That means that if you’re pregnant with twins, you will need to add 600 calories to your daily diet. Talk to your healthcare provider about your diet and the specific amounts you’ll need for a healthy pregnancy.
Moms of multiples might also experience the typical discomforts of pregnancy more intensely. It’s important to take good care of yourself and get plenty of rest to help ease the stresses of pregnancy.
It’s important to take good care of yourself and get plenty of rest to help ease the stresses of pregnancy.
In some cases, you might want to find a healthcare provider who has experience with multiple births. Specialized healthcare can help ensure that you and your babies are receiving the best care available. The need for frequent, intensive prenatal care is very important in a multiple pregnancy. Talk to your family doctor or OBGYN about their recommendations for specialists.
Can I be active and exercise during a multiple pregnancy?
Exercise and activity is an important part of any pregnancy. In most cases, you can absolutely exercise during a multiple pregnancy. Low-impact exercises are a great way to stay in shape and maintain your health throughout pregnancy. Some low-impact exercises to try during a multiple pregnancy can include:
- Swimming.
- Walking.
- Prenatal yoga.
Even though activity is wonderful during pregnancy, you should talk to your healthcare provider about the best activities for you. Some more strenuous activities might not be a good idea during a multiple pregnancy, including:
Some more strenuous activities might not be a good idea during a multiple pregnancy, including:
- Jogging.
- Aerobics that involve jumping.
It’s also important to remember that your exercise routine might need to change over time if you experience any complications.
Multiple pregnancy
Author: Mikheeva Natalia Grigoryevna, Malyshok magazine
A multiple pregnancy is a pregnancy in which two or more fetuses develop simultaneously in the uterus. Multiple pregnancy occurs in 0.4 - 1.6% of all pregnancies. Recently, there has been an obvious trend towards an increase in the incidence of such pregnancies due to the active use of assisted reproduction technologies, including in vitro fertilization (IVF).
Types of multiple pregnancies
Children born in multiple pregnancies are called TWINS. There are two main types of twins: monozygotic (identical, homologous, identical, similar) and dizygotic (fraternal, heterologous, different). African countries have the highest twin birth rate, Europe and the USA have an average rate, and Asian countries have a low rate.
African countries have the highest twin birth rate, Europe and the USA have an average rate, and Asian countries have a low rate.
Dizygotic (fraternal) twins are more common (in 66-75% of all twins). The birth rate of dizygotic twins varies from 4 to 50 per 1000 births. Dizygotic twins occur when two separate eggs are fertilized. The maturation of two or more eggs can occur both in one ovary and in two. The predisposition to develop dizygotic twins may be maternally inherited. Dizygotic twins can be either same-sex or opposite-sex, they look like each other like ordinary brothers and sisters. With fraternal twins, two placentas are always formed, which can be very close, even touching, but they can always be separated. Two fruit spaces (i.e., fetal bladders or two “houses”) are separated from each other by a septum consisting of two chorionic and two amniotic membranes. Such twins are called dizygotic dichorionic diamniotic twins.
Monozygotic (identical) twins are formed as a result of the separation of one fetal egg at various stages of its development. The frequency of birth of monozygotic twins is 3-5 per 1000 births. The division of a fertilized egg into two equal parts can occur as a result of a delay in implantation (immersion of the embryo in the uterine mucosa) and oxygen deficiency, as well as due to a violation of the acidity and ionic composition of the medium, exposure to toxic and other factors. The emergence of monozygotic twins is also associated with the fertilization of an egg that had two or more nuclei. If the separation of the fetal egg occurs in the first 3 days after fertilization, then monozygotic twins have two placentas and two amniotic cavities, and are called monozygotic diamniotic dichoriones (Fig. A). If the division of the ovum occurs between 4 - 8 days after fertilization, then two embryos will form, each in a separate amniotic sac. Two amniotic sacs will be surrounded by a common chorionic membrane with one placenta for two. Such twins are called monozygotic diamniotic monochorionic twins (Fig. B). If division occurs by 9- 10th day after fertilization, then two embryos are formed with a common amniotic sac and placenta.
The frequency of birth of monozygotic twins is 3-5 per 1000 births. The division of a fertilized egg into two equal parts can occur as a result of a delay in implantation (immersion of the embryo in the uterine mucosa) and oxygen deficiency, as well as due to a violation of the acidity and ionic composition of the medium, exposure to toxic and other factors. The emergence of monozygotic twins is also associated with the fertilization of an egg that had two or more nuclei. If the separation of the fetal egg occurs in the first 3 days after fertilization, then monozygotic twins have two placentas and two amniotic cavities, and are called monozygotic diamniotic dichoriones (Fig. A). If the division of the ovum occurs between 4 - 8 days after fertilization, then two embryos will form, each in a separate amniotic sac. Two amniotic sacs will be surrounded by a common chorionic membrane with one placenta for two. Such twins are called monozygotic diamniotic monochorionic twins (Fig. B). If division occurs by 9- 10th day after fertilization, then two embryos are formed with a common amniotic sac and placenta. Such twins are called monozygotic monoamniotic monochorionic (Fig. B) If the egg is separated at a later date on the 13th - 15th day after conception, the separation will be incomplete, which will lead to the appearance of conjoined (undivided, Siamese) twins. This type is quite rare, approximately 1 observation in 1500 multiple pregnancies or 1: 50,000 - 100,000 newborns. Monozygotic twins are always the same sex, have the same blood type, have the same eye color, hair, skin texture of the fingers, and are very similar to each other.
Such twins are called monozygotic monoamniotic monochorionic (Fig. B) If the egg is separated at a later date on the 13th - 15th day after conception, the separation will be incomplete, which will lead to the appearance of conjoined (undivided, Siamese) twins. This type is quite rare, approximately 1 observation in 1500 multiple pregnancies or 1: 50,000 - 100,000 newborns. Monozygotic twins are always the same sex, have the same blood type, have the same eye color, hair, skin texture of the fingers, and are very similar to each other.
Twin births occur once in 87 births, triplets - once in 87 2 (6400) twins, quadruples - once in 87 3 (51200) triplets, etc. (according to the Gallin formula). The origin of triplets, quadruplets, and more twins varies. So, triplets can be formed from three separate eggs, from two or one egg. They can be monozygotic and heterozygous. Quadruples can also be identical and fraternal.
Features of the course of multiple pregnancy
In case of multiple pregnancies, the woman's body is subject to increased requirements.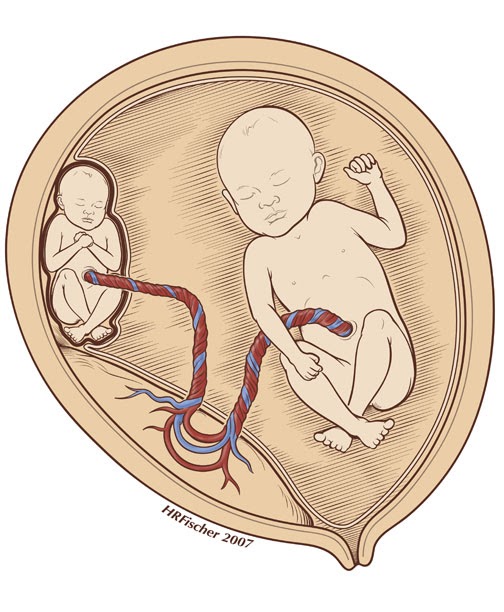 All organs and systems function with great tension. In connection with the displacement of the diaphragm by the enlarged uterus, the activity of the heart becomes difficult, shortness of breath, fatigue occur. Enlargement of the uterus, especially towards the end of pregnancy, leads to compression of the internal organs, which is manifested by impaired bowel function, frequent urination, and heartburn. Almost 4-5 times more often there is the development of preeclampsia, which is characterized by an earlier onset, a protracted and more severe clinical course, often combined with acute pyelonephritis of pregnant women. Due to the increased need and consumption of iron, iron deficiency anemia often develops in pregnant women. Significantly more often than with a singleton pregnancy, complications such as bleeding during pregnancy and childbirth, anomalies in labor, and a low location of the placenta are observed. Often, with multiple pregnancies, abnormal positions of the fetus occur. One of the most common complications in multiple pregnancy is its premature termination.
All organs and systems function with great tension. In connection with the displacement of the diaphragm by the enlarged uterus, the activity of the heart becomes difficult, shortness of breath, fatigue occur. Enlargement of the uterus, especially towards the end of pregnancy, leads to compression of the internal organs, which is manifested by impaired bowel function, frequent urination, and heartburn. Almost 4-5 times more often there is the development of preeclampsia, which is characterized by an earlier onset, a protracted and more severe clinical course, often combined with acute pyelonephritis of pregnant women. Due to the increased need and consumption of iron, iron deficiency anemia often develops in pregnant women. Significantly more often than with a singleton pregnancy, complications such as bleeding during pregnancy and childbirth, anomalies in labor, and a low location of the placenta are observed. Often, with multiple pregnancies, abnormal positions of the fetus occur. One of the most common complications in multiple pregnancy is its premature termination. Preterm birth is observed in 25-50% of cases of such pregnancies.
Preterm birth is observed in 25-50% of cases of such pregnancies.
The development of term twins is normal in most cases. However, their body weight is usually less (by 10% or more) than in singleton pregnancies. With twins, the weight of children at birth less than 2500 g is observed in 40-60%. The low weight of twins is most often due to insufficiency of the uteroplacental system, which is not able to adequately provide several fetuses with nutrients, trace elements and oxygen. The consequence of this is a delay in the development of the fetus, which is a common occurrence in multiple pregnancies. The mass of twins, respectively, decreases in proportion to their number (triplets, quadruplets, etc.).
With monochorionic twins in the placenta, anastomoses are often formed between the vascular systems of the fetus, which can lead to a serious complication - the syndrome of feto-fetal transfusion. In this case, there is a redistribution of blood from one fetus to another, the so-called "stealing". The severity of feto-fetal transfusion (mild, moderate, severe) depends on the degree of redistribution of blood through the anastomoses, which vary in size, number and direction.
Diagnosis in multiple pregnancy
The most reliable method for diagnosing multiple pregnancies is ultrasound, which allows not only early diagnosis of multiple pregnancies, but also to determine the position and presentation of fetuses, localization, structure and number of placentas, the number of amniotic cavities, the volume of amniotic fluid, congenital malformations and antenatal fetal death, the state of the fetus from a functional point of view, the nature of the uteroplacental and fetal-placental blood flow.
In multiple pregnancies, due to the higher risk of complications, ultrasound monitoring is performed more frequently than in singleton pregnancies. With dizygotic twins, about once every 3-4 weeks, with monozygotic twins - once every 2 weeks.
In addition, examinations and control of clinical tests are carried out with great care, and CTG is regularly recorded from 28 weeks of pregnancy.
Birth management
Indications for caesarean section associated with multiple pregnancies are triplets (quadruple), the transverse position of both or one of the fetuses, breech presentation of both fetuses or the first of them, and not associated with multiple pregnancy - fetal hypoxia, anomalies labor activity, prolapse of the umbilical cord, extragenital pathology of the mother, severe gestosis, placenta previa and abruption, etc.
-
ECO
In the department of assisted reproductive technologies of the Maternity Hospital No. 2
, IVF is performed at the expense of the Republican budget for couples
who received a positive decision from the Minsk city or regional commissions to provide one free IVF attempt.
No drug supply problem. There is no waiting list. -
Farewoman
-
Individual care for patients
-
Ultrasound diagnostics
Curious facts are
0
, how many are the Geminis? up to 80 million pairs of twins.
The number of twins born in relation to the total number of newborns in different countries and on different continents is different, but in general the trend is such that it continues to grow. Compared with the 60s, the percentage of twins has increased from 1.18 to 2.78, that is, almost 2.5 times.
The largest number of children
The largest number of children born to one mother, according to official data, is 69. According to reports made in 1782, between 1725 and 1765. The wife of a Russian peasant Fyodor Vasiliev gave birth 27 times, giving birth to twins 16 times, triplets 7 times and 4 twins 4 times. Of these, only 2 children died in infancy.
The most prolific mother of our contemporaries is considered to be Leontina Albina (or Alvina) of San Antonio, Chile, who at 1943-81 years gave birth to 55 children. As a result of the first 5 pregnancies, she gave birth to triplets, and exclusively male.
Most birthed
The record 38 births are said to be Elizabeth Greenhillies Abbots-Langley, c. Hertfordshire, UK. She had 39 children - 32 daughters and 7 sons.
The largest number of multiple births in one family
Maddalena Pomegranate from Italy (b. 1839) had triplets born 15 times.
There is also information about the birth on May 29, 1971 in Philadelphia, Pennsylvania, USA, and in May 1977 in Bagarhat, Bangladesh, 11 twins. In both cases, no child survived.
Most fertile pregnancies
Dr. Gennaro Montanino, Rome, Italy, claimed to have removed, in July 1971, the embryos of 10 girls and 5 boys from the uterus of a 35-year-old woman who was 4 months pregnant. This unique case of 15-fertility was the result of infertility pills.
9 children - the largest number in one pregnancy - were born on June 13, 1971 by Geraldine Broadrick in Sydney, Australia. 5 boys and 4 girls were born: 2 boys were stillborn, and none of the rest survived more than 6 days.
The birth of 10 twins (2 boys and 8 girls) is known from reports from Spain (1924), China (1936) and Brazil (April 1946).
The father with many children
The largest father in the history of Russia is Yakov Kirillov, a peasant from the village of Vvedensky, who in 1755 was presented to the court in connection with this (he was then 60 years old). The first wife of a peasant gave birth to 57 children: 4 times four, 7 times three, 9once twice and 2 times once. The second wife gave birth to 15 children. Thus, Yakov Kirillov had 72 children from two wives.
Longest Birth Intervals for Multiple Pregnancies
Peggy Lynn of Huntington Pennsylvania, USA, gave birth to a girl, Hanna, on November 11, 1995, and the second of the twins, Erika, only 84 days later (February 2, 1996).
Siamese twins
United twins were called "Siamese" after Chang and Eng Bunkers were born fused in the sternum on May 11, 1811 in the Maeklong region of Siam (Thailand). They married Sarah and Adelaide Yates of pc. North Carolina, USA, and had 10 and 12 children, respectively. They died in 1874, and with a difference of 3 hours.
The science of twins - gemellology.
"Secret language"
Twins often talk to each other in a language that others do not understand. This phenomenon is called cryptophasia.
Left-handed twins
18-22% of left-handed twins (for non-twins this percentage is 10).
Multiple pregnancy - signs, causes, features of management in the InTime clinic
Our services
Surrogate mothers are urgently needed.
Requirements: physical and mental health, presence of own children is obligatory, age up to 35 years. For all questions, please contact:
8(495)2235324, 8(926)0423057
home » Services of the center of reproduction and family planning » Multiple pregnancy
In multiple pregnancy, a woman's body is working to its limits. Carrying two or more fetuses is more difficult and is considered a high-risk pregnancy.
Turning to the InTime clinic at the very beginning of pregnancy, you will fall into the hands of real professionals. Specialists will take care of your health during the management of multiple pregnancy, during childbirth and support in the postpartum period. We will protect you from possible complications, develop an individual plan for managing pregnancy and upcoming childbirth, help you choose the right course of nutrition, and calculate the allowable physical activity.
We are easy to reach by car and metro - we are within walking distance of three stations: Sportivnaya, Park Kultury and Frunzenskaya.
The main advantages of the InTime clinic
Qualified staff
Obstetrician-gynecologists of the highest category with experience in managing multiple pregnancies, academicians, professors, candidates and doctors of medical sciences work at the InTime clinic. Qualified specialists are regular participants in many conferences and medical congresses on gynecology, obstetrics and ultrasound diagnostics.
Modern equipment
The laboratory of the InTime clinic is equipped with Japanese and German-made equipment. For the diagnosis of multiple pregnancies, high-precision ultrasound devices GE Logiq C5 and Mindray DC-3 with 3D function are used.
Service and comfort
By making an appointment in advance at a convenient time for you, you will save yourself from having to sit in line for hours. The clinic staff treats each patient with understanding. We take into account the emotional state of expectant mothers and, if necessary, provide qualified psychological support.
Peculiarities of managing a multiple pregnancy in the InTime clinic
Having determined a multiple pregnancy, qualified gynecologists-obstetricians of the InTime clinic will prescribe a number of tests and studies aimed at identifying a deficiency of nutrients or possible deviations in the body of the expectant mother.
Tests are standard, but if you have multiple pregnancies, you will have to do them more often and earlier. The number of mandatory ultrasound procedures increases to five.
The frequency of regular visits to the gynecologist is also increasing. During the reception, your weight, pressure, general condition are carefully monitored, and an examination is carried out to detect puffiness.
In the later stages, signs of multiple pregnancy are already clearly expressed: a very large belly, constant shortness of breath, pain in the back and lower abdomen. There is a possibility of premature birth. Monitoring the condition of the pregnant woman becomes more thorough.
If necessary, hospitalization is scheduled.
Considering the risks and possible complications, consultations of our specialists are available around the clock. You can contact us at a convenient time for you and get the help and support you need.