Breastfeeding swollen breast
Breast pain and breastfeeding - NHS
There are a number of reasons why you may experience breast pain while you're breastfeeding.
Always ask for help from your midwife, health visitor or breastfeeding specialist if you're having problems breastfeeding.
Here's how to deal with some of the most common causes.
Breast engorgement
Breast engorgement is when, for whatever reason, your breasts become overly full. They may feel hard, tight and painful.
In the early days, engorgement can be due to your milk coming in. Newborns need feeding little and often. It can take a few days for your milk supply to match your baby's needs.
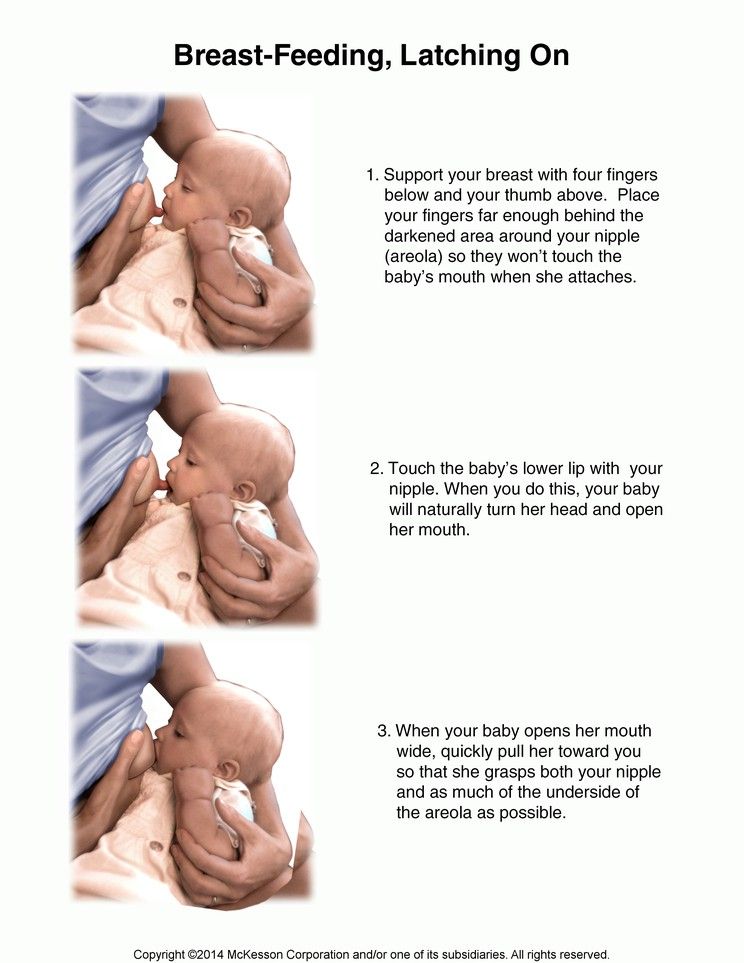
If your baby is not well attached to the breast, it may be hard for them to take your milk when your breast is engorged.
The nipple can become a little overstretched and flattened, and possibly painful.
Ask your midwife, health visitor or a breastfeeding specialist for advice immediately to help your baby relieve the engorgement and prevent it happening again.
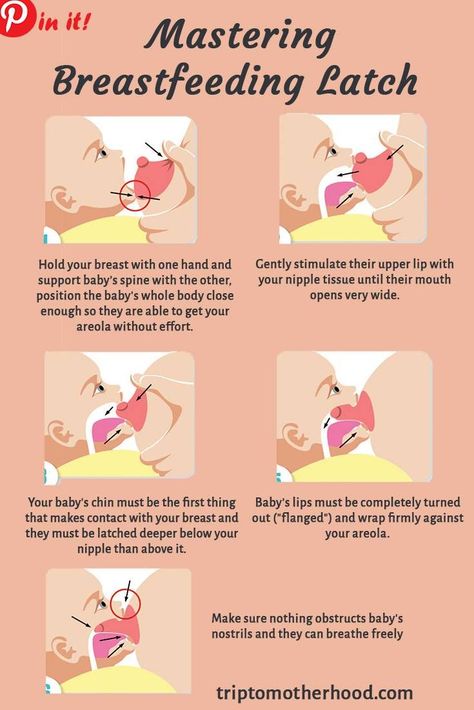
Find out more about positioning and attachment
Engorgement can still happen once you have learnt the skill of positioning and attachment, usually when your baby has not fed for a while.
Your baby usually knows when they need a feed, for how long and from which breast.
Early signs (cues) that your baby is ready to feed can include:
- moving their eyes rapidly
- putting their fingers into their mouth
- rooting (turning to 1 side with their mouth open as if seeking the breast)
- becoming restless
Crying is the very last sign that your baby needs feeding. Feeding them before they cry often leads to a much calmer feed.
Feeding them before they cry often leads to a much calmer feed.
Keeping your baby close so you can watch and learn their early feeding cues will help.
How to ease breast engorgement
To ease the discomfort of engorgement, apart from your baby feeding, you could try expressing a little breast milk by hand. Only express enough to relieve the discomfort because expressing more will make you produce more milk.
Ask your midwife, health visitor or breastfeeding specialist to show you how.
Find out more about expressing breast milk
You may also find it helps to:
- wear a well-fitting breastfeeding bra that does not restrict your breasts
- put warm flannels on your breasts just before hand expressing if they're leaking
- take some paracetamol or ibuprofen at the recommended dose to ease the pain (these are safe to take while you're breastfeeding)
Too much breast milk
Occasionally women make too much breast milk and their babies struggle to cope.
It's best to get your midwife, health visitor or breastfeeding specialist to watch a feed to see if they can spot why this is happening.
They can also suggest ways to decrease your supply.
Blocked breast milk ducts
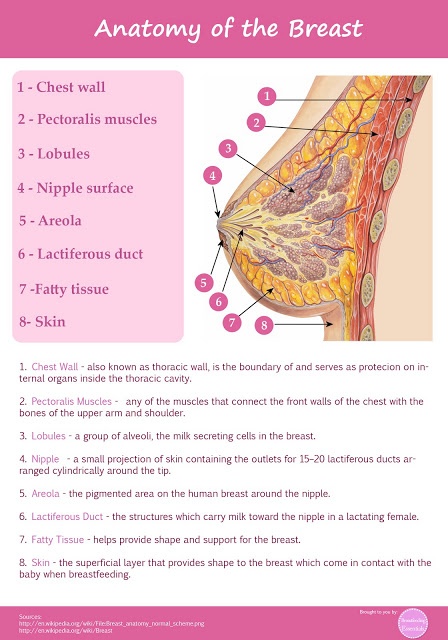
The milk-making glands in your breasts are divided up into segments, rather like an orange.
Narrow tubes called ducts carry the milk from each segment to your nipple.
If one of the segments is not drained properly during a feed (perhaps because your baby is not attached properly), this can lead to a blocked duct.
You may feel a small, tender lump in your breast.
Avoid wearing tight clothes or bras so your milk can flow freely from every part of your breast.
Other things that may help include:
- frequent feeding from the affected breast
- warm flannels or a warm shower to encourage the flow
- gently massaging the lump towards your nipple while your baby feeds
It's important to deal with a blocked duct quickly as, if left, it could lead to mastitis.
Mastitis
Mastitis (inflammation in the breast) happens when a blocked duct is not relieved.
It makes the breast feel painful and inflamed, and can make you feel very unwell with flu-like symptoms.
If you do not deal with the early signs of mastitis, it can turn into an infection and you'll need to take antibiotics.
Symptoms of mastitis include:
- a breast that feels hot and tender
- a red patch of skin that's painful to touch
- a general feeling of illness, as if you have flu
- feeling achy, tired and tearful
- a high temperature
If you think you're developing a blocked duct or mastitis, try the following:
- Carry on breastfeeding.

- Check your baby's positioning and attachment. Ask your midwife, health visitor or a breastfeeding specialist to watch a feed.
- Let your baby feed on the tender breast first.
- If the affected breast still feels full after a feed, or your baby cannot feed for some reason, express your milk by hand.
- Warmth can help the milk flow, so a warm flannel, or a warm bath or shower, can help.
- Get as much rest as you can. Go to bed if you can.
- Take paracetamol or ibuprofen to relieve the pain.
Contact your GP or NHS 111 if you feel worse at any time, or if you're no better within 12 to 24 hours.
You may need antibiotics, which will be fine to take while breastfeeding.
Stopping breastfeeding will make your symptoms worse, and may lead to a breast abscess.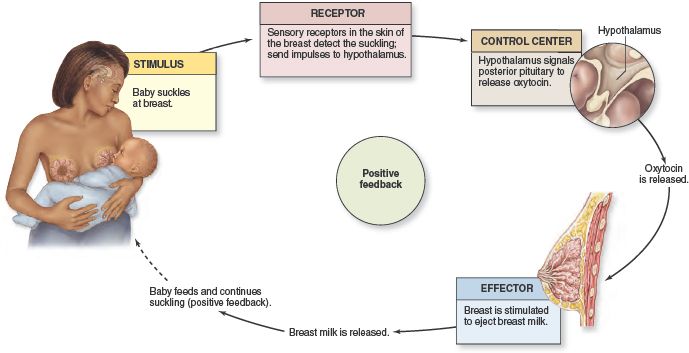
Breast abscess
If a mastitis infection is not treated, it can lead to a breast abscess, which may need an operation to drain it.
This can also develop if the mastitis does not respond to frequent feeding plus a course of antibiotics.
You can carry on breastfeeding after an abscess has been drained.
Find out more about breast abscesses
Thrush
If you experience pain in both breasts, often after a period of pain-free breastfeeding, and the pain lasts for up to an hour after a feed, you may have developed thrush.
Find out more about thrush and breastfeeding
Got a breastfeeding question?
Chat to the Start4Life Breastfeeding Friend on Amazon Alexa, Facebook Messenger or Google Home for fast, friendly, trusted NHS advice any time, day or night.
Breast Engorgement: Causes, Complications & Treatment
Overview
What is breast engorgement?
Breast engorgement is when your breasts are painful, swollen and tender because they’re overly full of milk. It occurs most often in the days and weeks after giving birth due to milk production and increased blood supply to your breasts (chest). The increase in blood supply helps your body make breast milk for your baby, but it can cause severe engorgement. Engorged breasts are a temporary problem but can happen as long as you produce milk.
The most common reasons for breast engorgement are:
- You’ve given birth and your milk is “coming in.”
- You’re breastfeeding (chestfeeding) and skip nursing sessions.
- Your baby changes their feeding schedule. For example, they start sleeping through the night.
- You skip pumping sessions or forget to pump when you’re away from your baby.
- You have an oversupply or make more milk than your baby needs.
- You’re weaning your child from breastmilk to another form of milk.
It can be tricky to balance managing your milk supply and preventing engorgement. However, there are ways you can relieve the discomfort and minimize complications from engorged breasts.
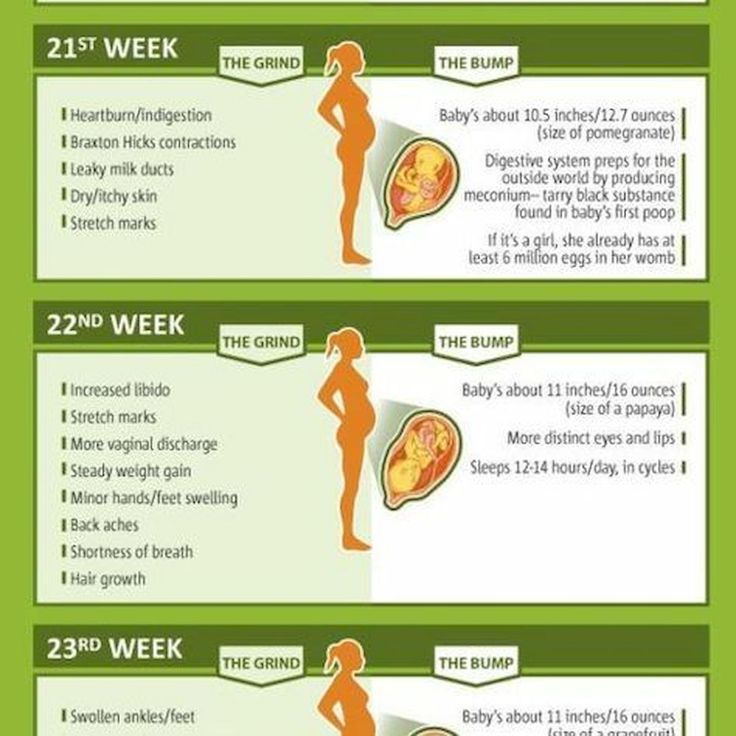
When do you start making breastmilk?
The first milk your breasts produce is called colostrum. It’s a highly nutritious first milk that your body begins making in pregnancy. Colostrum transitions to breast milk after three to five days. Engorgement tends to occur during this time because your milk production is ramping up. Your breasts will be fuller, firmer, swollen and tender to the touch. After several days, the pain and discomfort should gradually subside.
When does engorgement start?
The exact timing varies, but the most common time is between three and five days after you give birth. It may start later if you’ve had a cesarean birth (C-section). The degree of swelling and pain you feel can also vary. Some people are severely engorged, while others feel minor side effects of breast engorgement.
Some people are severely engorged, while others feel minor side effects of breast engorgement.
How long does it take for engorgement to go away?
There’s no set time for engorgement to subside. The engorgement you feel after giving birth is usually the most severe. Most people stop feeling engorged within 10 days; however, feeling “full” can last several weeks. Breast engorgement can come back as long as you breastfeed, chestfeed or pump breast milk.
Possible Causes
What causes breast engorgement?
Your breasts become engorged anytime they’re overly full of milk. It happens the first time within a few days of giving birth and can last several weeks. You can get engorged breasts for as long as you’re making milk.
Reasons your breasts may become overly full are:
- Your milk is transitioning from colostrum to mature breast milk.
- You miss or skip feedings or pumping sessions.
- Your baby sleeps through the night or starts eating solid food.

- You supplement feedings with formula.
- Your baby doesn’t eat as much due to illness.
- Your baby isn’t latching correctly and fully emptying the breast.
What are symptoms of breast engorgement?
No two people will have the same symptoms. People describe their engorged breasts as being:
- Fuller and larger than usual (up to a few cup sizes).
- Swollen.
- Painful.
- Hard and firm.
- Tender and sensitive to touch.
- Lopsided or rocky (hard lumps).
The swelling can also extend up into your armpit and across to your sternum (breast bone). This is because breast tissue extends to these areas. Your nipples may change from being soft and flexible to flat and firm.
Some people also experience a low fever (called milk fever) when they’re engorged. This is typically OK. Call your healthcare provider if your fever increases or lasts several days as it could be a sign of infection.
What does breast engorgement feel like?
Engorged breasts feel like they’re ready to burst. They may feel hard like rocks and so tender that it hurts to walk or change your clothes. Your breasts will feel heavier, and simple things like snuggling your baby may be extremely painful.
They may feel hard like rocks and so tender that it hurts to walk or change your clothes. Your breasts will feel heavier, and simple things like snuggling your baby may be extremely painful.
What do engorged breasts look like?
Engorged breasts look several sizes bigger than their normal size. Most people will see their veins protruding visibly under the skin of their breasts. The skin of your breasts may appear shiny from being stretched. Your breasts will likely have an uneven shape, and you may see visible lumps or hard spots.
Care and Treatment
How do you relieve breast engorgement?
Most people can relieve breast engorgement at home within a few days. Some common treatments for engorged breasts are:
- Using a warm compress or taking a hot shower before feedings to soften your breasts and encourage milk flow.
- Massaging your breasts while nursing or pumping.
- Hand expressing or pumping a small amount of milk between feedings to relieve pressure.

- Applying a cold compress or ice pack to your breasts between feedings to help with swelling.
- Taking ibuprofen or acetaminophen for pain.
- Feeding your baby or expressing milk every two to three hours.
- Letting your baby completely drain your breasts.
Should I pump to relieve engorgement?
Yes, you can pump a little bit of milk to relieve engorgement. Try to pump just enough to feel relief —around 1 to 2 ounces. Remember, producing milk is a supply and demand process. If you pump too much milk, your body will just produce more to make up for it.
How do I stop getting engorged at night?
It’s normal for your breasts to become engorged once your baby starts sleeping longer at night. It may take your milk supply a few days to adapt to your baby’s new pattern. If your breasts are overly filled, it’s OK to remove some milk. You should only remove a little milk – enough to provide some relief so you can get back to sleep.
This can happen anytime your baby goes longer without feedings. If you experience pain or fullness because your baby is going longer stretches between meals, pumping or hand-expressing a little bit of milk is fine.
If you experience pain or fullness because your baby is going longer stretches between meals, pumping or hand-expressing a little bit of milk is fine.
What do I do for engorgement if I don’t want to breastfeed or chestfeed?
You’ll have engorged breasts even if you choose not to breastfeed or chestfeed. However, milk production will eventually stop. Your body will recognize that you don’t need milk, and your supply will dry up. Don’t pump for relief. This will only prolong the process of ending your milk production. Instead, try some of the following treatments until your pain subsides:
- Take an over-the-counter (OTC) pain reliever for pain and swelling.
- Wear a tight-fitting and supportive bra.
- Apply cold compresses to your breasts several times a day.
When to Call the Doctor
What can happen if my breasts get too engorged?
Engorged breasts can make it hard for your baby to feed. Relieving engorgement and softening your breasts and nipples can help with your baby’s latch (the way your baby attaches to your nipple).
Some of the most common feeding issues caused by engorged breasts are:
- Your baby can’t latch to your nipple because it’s too flat and stretched.
- Your nipples become sore and cracked because your baby isn’t latching correctly.
- You feed your baby less because it’s too painful. This can lower your milk supply.
- Overactive let-down or fast milk flow. This can lead to your baby gagging or choking on milk.
- Your baby is unable to empty your breast fully. This can cause clogged milk ducts.
Breast engorgement can also lead to complications like clogged milk ducts and mastitis.
What’s a clogged milk duct?
Milk ducts are a part of breast anatomy that carry milk to the nipples. When one of these ducts gets clogged with milk, you may feel a lump in your breast. Removing the clog as soon as possible can prevent it from becoming infected. To unclog a milk duct, apply heat to the area and gently massage the lump toward your nipple while nursing or pumping.
What’s mastitis?
Mastitis is an infection in your breast tissue. It happens when milk gets trapped in the breast. Bacteria grow in the trapped milk, leading to infection. Your healthcare provider will treat mastitis with antibiotics. You will also be encouraged to gently massage your breast, nurse or pump, and use medication to bring down any fever you may have.
When do I call my doctor?
Contact your healthcare provider, pediatrician or lactation consultant if:
- Your breasts are engorged longer than a few weeks.
- You develop symptoms of mastitis. Signs include a red spot on your breast, a fever, a painful spot on your breast or chills.
- Your baby has a poor latch or issues with breastfeeding/chesfeeding.
- You think you have low milk supply or your baby isn’t eating enough.
Don’t be ashamed to ask for help. Struggling with breastfeeding, chestfeeding or feeding your baby pumped milk is a common struggle. Healthcare providers can help you.
Frequently Asked Questions
Can you prevent breast engorgement?
No, you can’t prevent breast engorgement. It’s a natural part of childbirth. However, you can manage your symptoms so you’re more comfortable. Remember, it will subside once your milk supply is under control. When your milk comes in and your supply is regulated, you can prevent future breast engorgement by:
- Not skipping feeding or pumping sessions.
- Making sure your baby maintains a good latch on your breast.
- Weaning your baby from breast milk slowly.
- Emptying your breasts at each feeding.
A note from Cleveland Clinic
Engorged breasts are hard, swollen and extremely painful. Some engorgement is unavoidable – like when your milk comes in after giving birth. It’s good to learn how to manage breast engorgement and treat it quickly. Remember, engorged breasts are only temporary, and you can take steps to ease the discomfort by removing some milk, softening your breasts before nursing or using ice packs. Call your healthcare provider if your engorgement lasts longer than a few weeks or if you develop signs of mastitis.
Call your healthcare provider if your engorgement lasts longer than a few weeks or if you develop signs of mastitis.
What is breast swelling? | Breast swelling
Some mothers experience breast swelling when milk begins to flow in the first days after childbirth. Usually this phenomenon is temporary and easily eliminated. Read our article to find out how to help yourself.
Share this information
Sioned Hilton, health visitor, neonatal nurse and lactation consultant:
Schoned, a mother of three, has been supporting families with newborns and young children for over 30 years. She provides advice on breastfeeding and pumping, both in clinics and at home. In addition, Schoned writes articles for parenting magazines, attends conferences, and conducts seminars for attending physicians.
When you start breastfeeding, you first produce a small amount of colostrum, which gradually increases over the first few days. After about two to four days, production increases significantly. This phenomenon is called the "arrival" of milk. nine0012 1
This phenomenon is called the "arrival" of milk. nine0012 1
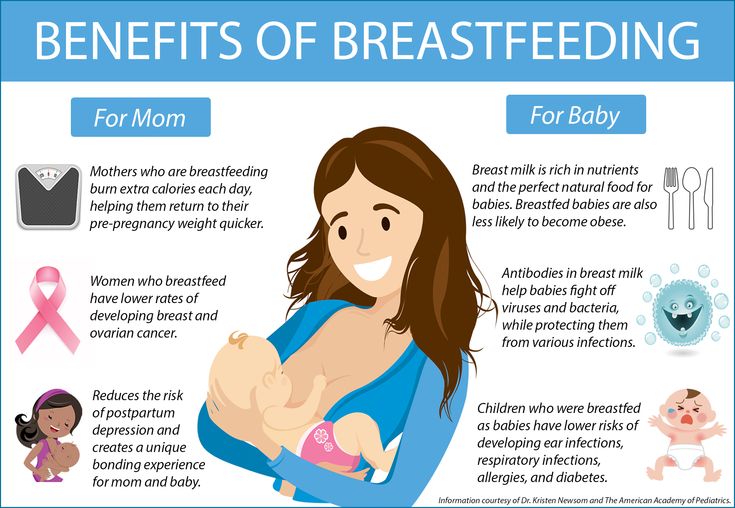
One of the signs that milk is starting to come in is a change in the breast - it fills up and becomes firmer. This is due not only to an increase in the amount of milk, but also to increased blood flow and additional lymphatic fluid to the breast tissues. 2
If the child eats well and often, then for most mothers this feeling of heaviness disappears over time without any complications. However, some women produce so much milk that their breasts fill up and become painful and very hard. This condition is called breast swelling. And although everything usually passes in a day or two, this period can be quite painful. nine0003
How does breast swelling manifest itself?
Swelling may affect one or both breasts. It can cause swelling, sometimes down to the armpits, and a throbbing sensation. The chest becomes quite hot, sometimes lumps are felt in it. All this is due to the fact that a huge number of processes take place inside.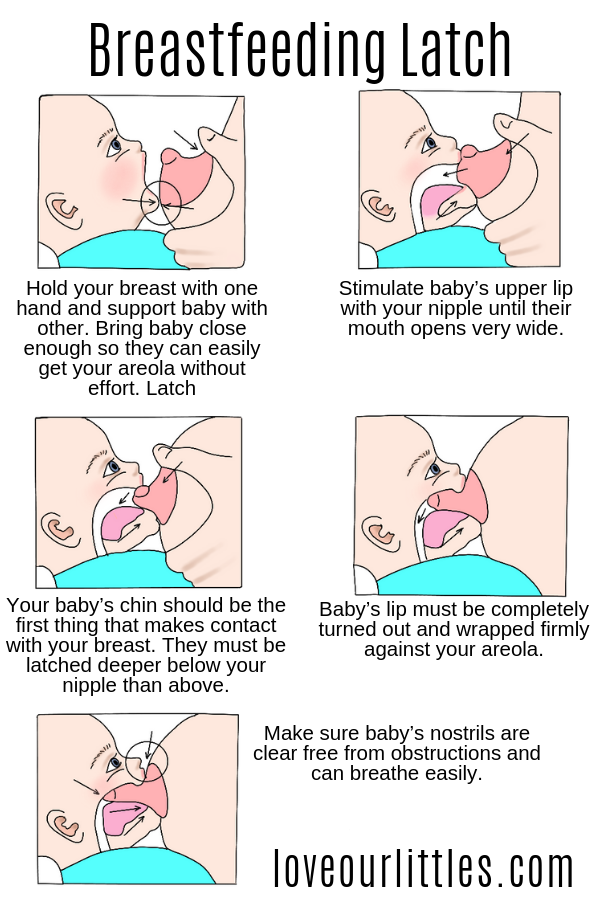 You may also notice other symptoms, such as the skin on your breasts becoming shiny and tight, and your nipples becoming hard and flat. Swelling of the mammary glands can even cause a temperature to rise to 37.5–38.3°C (99–101°F). 3
You may also notice other symptoms, such as the skin on your breasts becoming shiny and tight, and your nipples becoming hard and flat. Swelling of the mammary glands can even cause a temperature to rise to 37.5–38.3°C (99–101°F). 3
In addition to painful sensations, breast swelling is also dangerous because it can make breastfeeding difficult, and this, in turn, will worsen the situation even more. If the baby finds it difficult to latch on because the nipples have become flat and the breast tissue is firmer, nipples may become inflamed. In addition, in the event of a poor grip, he will not be able to completely empty the chest. Thus, if left untreated, swelling of the mammary glands can lead to blockage of the milk ducts, mastitis, and reduced milk production. nine0003
What causes breast swelling?
Usually breast swelling is due to the fact that the child does not feed often enough (less than eight times a day). In principle, this can happen to any mother, but women who have undergone various breast surgeries, including breast augmentation, are more prone to swelling of the mammary glands. 2 Wearing a bra that is the wrong size or that is too tight can increase discomfort and lead to clogged milk ducts and even mastitis. nine0003
2 Wearing a bra that is the wrong size or that is too tight can increase discomfort and lead to clogged milk ducts and even mastitis. nine0003
Breast swelling can occur in both breastfeeding mothers and mothers who are not or cannot breastfeed. The hormonal changes that occur after the birth of a baby and the release of the placenta and increase milk production are independent of whether you are breastfeeding or not. Swelling can also occur if the number of feedings is drastically reduced, for example, if the child becomes ill, sleeps longer, starts eating solid foods, or goes to nursery.
How to treat breast swelling? nine0012 2
The best cure for swollen breasts is a hungry baby! Try to empty your breasts as much and as often as possible to facilitate the release of milk. To do this, feed your baby on demand, preferably eight to twelve times a day.
Maintain skin-to-skin contact with your baby, cuddling as often as possible during the day and at night when you are awake. This will allow him to smell the attractive smell of your milk and have easy access to the breast, and you will be able to better monitor signs that he is hungry and, accordingly, feed more often. Let the baby eat enough from one breast before offering the second. nine0003
This will allow him to smell the attractive smell of your milk and have easy access to the breast, and you will be able to better monitor signs that he is hungry and, accordingly, feed more often. Let the baby eat enough from one breast before offering the second. nine0003
It's a good idea to see a lactation consultant or specialist to check if your baby is properly grasped and positioned. It depends on how well he will eat and empty his chest. The tips below will also help you relieve the symptoms of breast swelling.
Tips for relief of breast swelling 2
- Breastfeed at least eight times a day.
- Make sure your baby is latching on well. nine0055
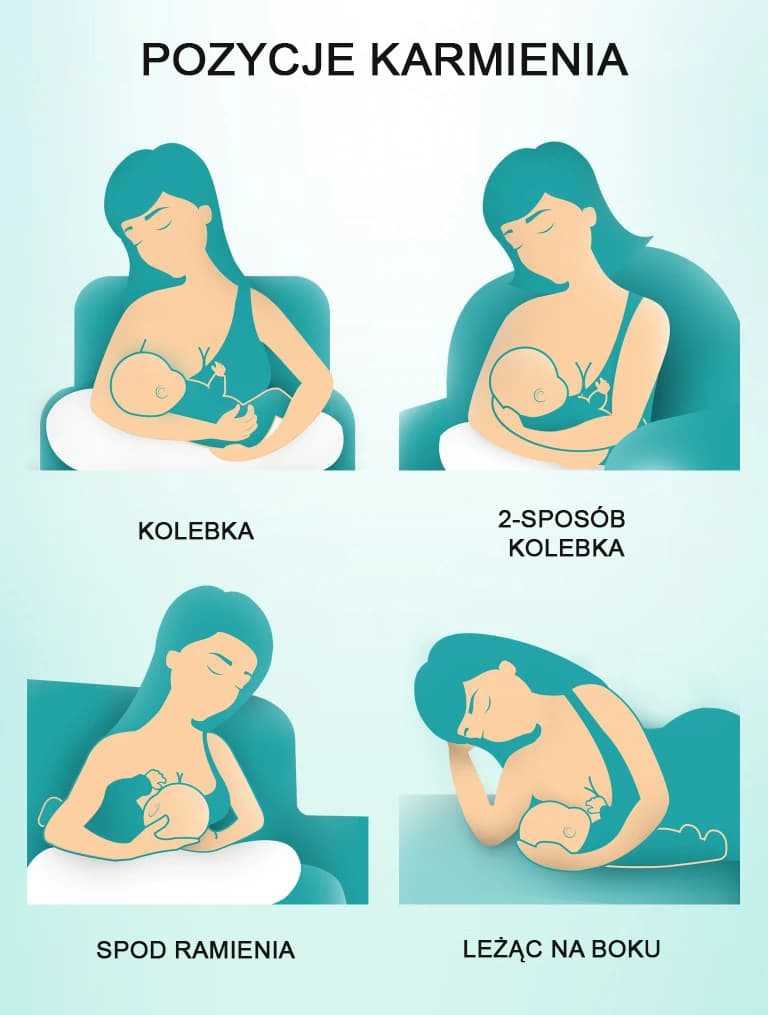
- Try other feeding positions.
- Gently massage your breasts during feeding to improve the flow of milk.
- Express some milk by hand or with a breast pump before feeding to soften the nipple and make it easier for your baby to latch on.
- If your breasts are still firm and full after a feed, pump more until you feel better.
- If your baby cannot breastfeed, express milk for him. Pumping must be continued until the breast becomes softer, and do this at least eight times a day. nine0055
- Try the areola pressure softening technique. This helps to remove excess fluid from the breast. A lactation consultant or specialist will show you how to do this.
- If milk leaks, try taking warm showers or applying warm flannel to your breasts just before feeding or pumping to soften your breasts and make it easier for your milk to flow. You should not, however, warm the chest for more than two minutes, as this can only increase swelling. nine0055
- If your milk isn't leaking, try applying cold compresses, chilled gel pads, or even frozen green peas wrapped in a towel for ten minutes after feeding to reduce swelling and relieve pain.
- Put clean cabbage leaves in your bra. Yes Yes! For many moms, it really helps reduce swelling and discomfort, and there are scientific explanations for this.
 4
4 - Take an anti-inflammatory pain reliever. While breastfeeding, you can take some medications, in consultation with your doctor. Always consult your doctor, follow the drug manufacturer's instructions and the pharmacist's recommendations. To learn more about medications and breastfeeding, read our article on breastfeeding when sick. nine0055
- Wear an appropriately sized and comfortable nursing bra, avoid underwire or no bra at all.
- Do not skip feedings or stop breastfeeding abruptly as this may increase breast swelling.
Seek medical advice if your 5 temperature rises above 38 °C or if your baby is unable to suckle due to breast swelling.
And in any case, try to remain calm. Your body is just getting used to producing milk and feeding your baby. Breast swelling should go away on its own soon after you both get comfortable with breastfeeding. nine0003
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Berens P, Brodribb W. ABM Clinical Protocol# 20: Engorgement, Revised 2016. Breastfeed Med . 2016;11(4):159-163. - Behrens P, Brodrhibb W, "AVM Clinical Protocol #20: Engorgement, 2016 edition". Brestfeed Med (Breastfeeding Medicine). 2016;11(4):159-163.
3 Affronti M Low-grade fever: how to distinguish organic from non-organic forms. Int J Clin Pract. 2010;64(3):316-321. - Affronti M. et al., "Subfebrile temperature: how to distinguish organic from non-organic cases." Int Zh Klin Prakt. 2010;64(3):316-321.
4 Boi B et al. The effectiveness of cabbage leaf application (treatment) on pain and hardness in breast engorgement and its effect on the duration of breastfeeding. JBI Libr Syst Rev . 2012;10(20):1185-1213. - Boys B. et al., "Effectiveness of cabbage leaf (as a drug) for breast pain and engorgement, and its effect on the duration of breastfeeding." nine0095 JBAi Libr Sist Rev. 2012;10(20):1185-1213.
JBI Libr Syst Rev . 2012;10(20):1185-1213. - Boys B. et al., "Effectiveness of cabbage leaf (as a drug) for breast pain and engorgement, and its effect on the duration of breastfeeding." nine0095 JBAi Libr Sist Rev. 2012;10(20):1185-1213.
5 NHS Choices. How do I take someone's temperature? [Internet]. UK: NHS Choices; updated 2016 June 29. Available from : www.nhs.uk/chq/pages/1065.aspx?categoryid=72 - NHS Choice. "How to measure the temperature?" [Internet]. United Kingdom: NHS Choice, 29 June 2016 edition Article linked: www.nhs.uk/chq/pages/1065.aspx?categoryid=72
Solving nine breastfeeding problems in the first month
Expert advice on solving major breastfeeding problems in the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home.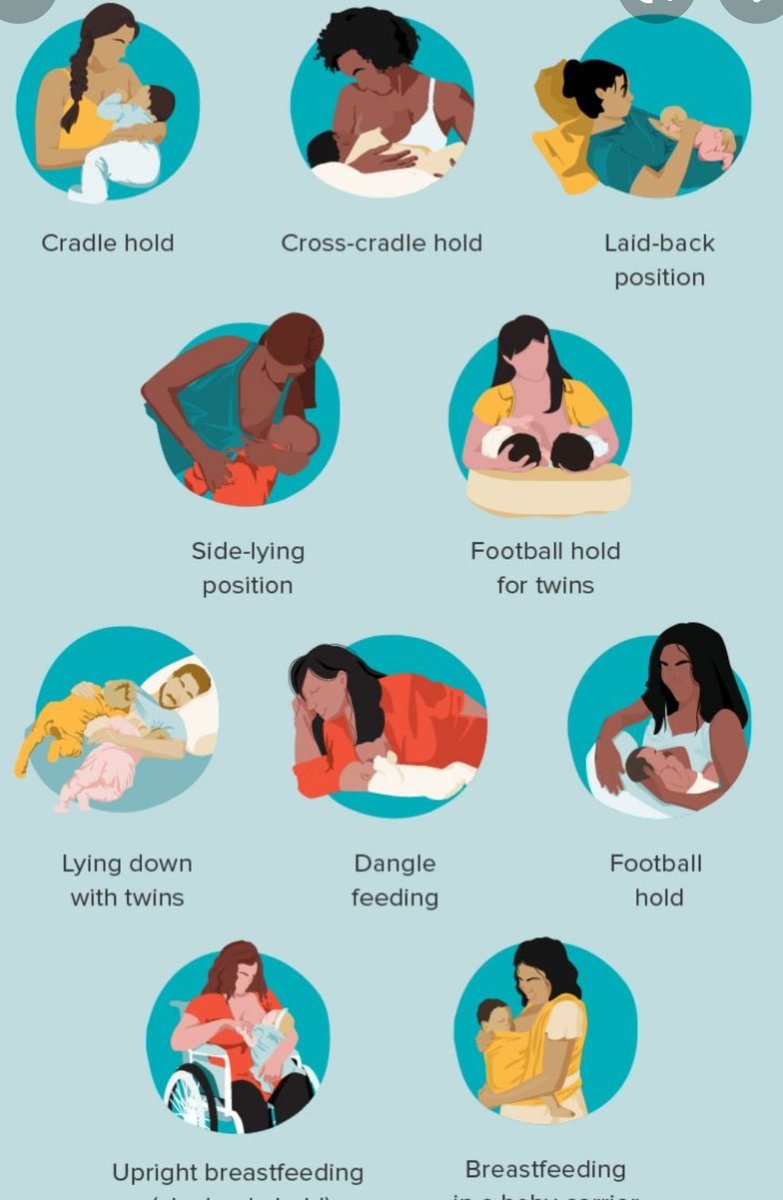 Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences. nine0003
Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences. nine0003
Breastfeeding is as much a skill as driving a car, and in the first month mother and baby may encounter some obstacles along the way. It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps to establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding challenges that mothers often face from the end of the first week to the end of the first month after giving birth. nine0003
Problem #1. A painful lump appeared in the breast
Lumps and bumps in the breast of a nursing woman can appear for various reasons. One of the most common is blockage of the milk ducts, which results in a hard and painful lump that can become inflamed.
Solutions 1–3
- Massage the inflamed area, especially while breastfeeding or expressing, to clear the blockage.
 nine0055
nine0055 - Gently place warm flannel on your breast or take a warm shower before feeding to relieve discomfort.
- Continue breastfeeding as usual to avoid milk accumulation that can cause mastitis.
- Try to express milk from the inflamed breast after feeding to ensure that it is completely emptied. This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you. nine0055
- Try ultrasound therapy. If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist.
- Call your healthcare provider, if you notice signs of infection (breast redness and tenderness or flu-like symptoms such as fever, aches, malaise and headache), or if you think the lump is not related to breastfeeding .
 nine0055
nine0055
Problem #2. The breast is red and sore
If one or both mammary glands are red and sore, and this is not due to blockage of the ducts, mastitis, that is, inflammation of the breast tissue, is not excluded. Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. nine0012 3
Mastitis can be caused by the following causes:
- no treatment for blocked ducts,
- Bacteria entering the breast through cracked and damaged nipples,
- improper attachment of the child to the breast,
- long periods between feedings,
- breasts too full,
- wearing a bra that is too tight or that cuts into the skin,
- Abrupt weaning,
- excess milk.
Solutions 3
In addition to seeking medical attention:
- Continue to breastfeed or express milk frequently. Your milk is still safe for your baby. Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk. nine0054 Give the child the inflamed breast first. This way the child can empty it completely. If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one.
- Have a good rest, drink and eat. You need to get enough fluids and good nutrition.
- Massage the sore area under a warm shower or apply a warm flannel or warm pack to clear the blockage and relieve symptoms before breastfeeding or pumping. nine0055
- Apply a cooling pack after feeding, , to reduce inflammation.

Problem #3. My strength is running out
Breastfeeding in the first weeks can be very tiring and seem endless. The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.
Solutions
- Take care of yourself. This may be easier said than done when you have a newborn in your arms, but still try to get as much rest as possible, eat healthy and regular meals, and drink plenty of water. Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it. nine0055
- Feed lying down. This will allow you to relax and reduce stress on sore spots, stitches or c-section scars.
- Do not skip feedings. Your partner may offer to bottle feed your baby while you are resting. However, despite this temptation, it should be remembered that milk production is best established in the first four weeks through breastfeeding.
 When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding. nine0055
When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding. nine0055
Problem #4. How can I increase breast milk production?
It's easy to question whether your breastmilk supply is adequate, especially when your baby has developmental spikes between the third and fourth weeks. It may seem to you that the child asks for breasts more often because he does not have enough milk. However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. nine0012 4
Solutions 4.5
- Do not try to supplement your baby with formula, unless doctors are worried about weight gain or fluid loss.
 Continue breastfeeding your baby. This will help naturally increase breast milk production.
Continue breastfeeding your baby. This will help naturally increase breast milk production. - Do not feed on a schedule. Feed your baby on demand. Thus, the production of breast milk will adapt to his needs. nine0054 Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Problem #5. I have too much milk
Hyperlactation, or too much milk, can also be difficult for you and your baby. You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. nine0012 6
Solutions
- Express some breast milk at the start of a feed to reduce the force of the flush. Don't pump too much as this can aggravate the situation - pump only as much as needed to ease the discomfort. Try hand pumping or use a breast pump (check out the Medela* breast pump range and choose the right one for you).

- Use the towel or pad to soak up excess milk, or place the milk collection pad** on the other breast while you breastfeed first. nine0055
- The child must feel supported. Hold him firmly (this gives a sense of security) and in a comfortable position so that he can turn his head. Talk to the baby during the first rapid flush, then he will not be frightened by surprise and will not push the breast.
- Contact a lactation consultant or health care professional who will monitor you and suggest single-sided feedings or hourly breast changes (“breast duty”) to normalize your milk supply. nine0055
- Be patient . Problems with milk production usually go away after a few weeks.
Problem #6. I have different breasts!
You have noticed that the baby has a preference for one breast, or that one breast produces more milk than the other, and as a result, the mammary glands have acquired different sizes and shapes. This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks. nine0003
This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks. nine0003
Solutions
- Offer less demanded breasts first during feeding as babies usually suckle more vigorously at the beginning of a feed.
- Use the breast pump to increase breast milk production in the smaller breast.
- Don't give up on bigger breasts. Breastfeeding should continue with fuller breasts to avoid blocked ducts and mastitis.
- See a doctor. Sometimes an ear infection is the reason for a baby to latch on only one side. However, some positions may cause him discomfort, so try to keep the child more upright. In addition, a breast infection can change the taste of milk and cause milk to be rejected as well.
Problem #7.
 A blister has appeared on the nipple
A blister has appeared on the nipple With frequent feeding, sometimes painful friction occurs, and a blood bubble may appear on the breast,
nipple or areola. nine0012 7
Solutions
- Ask a lactation consultant or specialist to check the baby's latch on. A shallow grip can cause blistering of the nipples and areolas.
- Talk to your doctor about what medicine you can take to relieve pain if needed.
- Try other feeding positions to avoid pressure on the painful area. nine0055
- Lubricate inflammation with pure lanolin.
- Use Breast Pads** to avoid rubbing your blister with clothing and help it heal faster with air circulation, or try cooling hydrogel pads** to help relieve pain and promote healing.
- Try expressing milk. Using a breast pump can be an alternative way to get breast milk without bladder irritation.
 Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel. nine0055
Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel. nine0055 - Do not pierce the vial as this may lead to infection.
- Seek medical attention, if the problem persists and causes you pain.
Problem #8. Painful white spot on nipple
When the opening of the milk duct is blocked by milk or a thin layer of skin grows over it, a small white or yellowish spot may appear on the tip of the nipple. For some, these blocked ducts, sometimes called milk vesicles or blisters, cause pinpoint pain, especially during feeding or pumping. Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. nine0012 8
Solutions
- Follow the tips above to solve friction bubble problems.
- Remove the blockage, if you see that the milk cork is starting to bulge.
 Try to squeeze it out very gently with clean nails.
Try to squeeze it out very gently with clean nails. - Continue breastfeeding or pumping, to clear the milk duct. If the milk duct clears during feeding, it will not harm the baby in any way. nine0055
- Apply hot wet flannel to the vial just before feeding or pumping. This will help open the blocked duct. You can also try rubbing the area quickly with a clean, damp cloth.
- Manually express some milk before feeding, trying to push out hardened milk clots. If this does not help, feed the baby or express milk as usual. Repeat several times a day.
- Soak a cotton swab with olive oil and place it in the bra, pressing it against the bubble nipple. This will help soften the skin.
- Seek medical attention, if problem persists. Your doctor may remove the plug with a sterile needle. This should be done immediately after feeding, when the bubble is as inflated as possible.

Issue #9. My nipples hurt while breastfeeding
At the start of breastfeeding, my nipples may become more tender, sore, and even inflamed, but this usually goes away after a few days. If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. nine0012 2.7
The following symptoms and signs that appear on one or both breasts during or after feeding may indicate a bacterial infection or thrush:
- burning, itching or moderate to severe pain in the nipples
- pain in nipples aggravated by contact with clothing,
- nipple pain persists despite attempts to attach baby differently,
- nipples hurt to touch, nine0054 stitching, shooting, burning or deep aching pain,
- chest pain during feeding and almost an hour after,
- hot pink nipples,
- discoloration and texture of the areola (hot pink color, darkening, dryness or peeling),
- white rash on chest or areola.

Also check if your child has any of the following symptoms and signs:
- thick white patches or coating on the tongue
- white indelible spots on the cheeks,
- bright red spotted rash on buttocks not helped by diaper rash creams.
Solutions 7
- Seek medical attention. He will most likely suggest testing for infections to make a diagnosis. Bacterial and fungal (yeast) infections are treated differently, so appropriate treatment should be started as soon as possible. There are other reasons that can cause similar nipple pain, such as eczema, psoriasis or vasospasm (narrowing of the blood vessels) in the mother and problems with latch or tongue frenulum in the child. Therefore, it is very important to make an accurate diagnosis. nine0055
- Strict hygiene. Wash hands before and after feeding and applying any medication, and after changing diapers. Change bra pads regularly, wash bras, tank tops and towels in high temperature water, thoroughly wash breast cups and anything your baby puts in her mouth, such as nipples.
- Let the nipples dry after feeding, as all infections love a warm and humid environment. nine0054 See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
Materials on the topic. Breastfeeding: what to expect in the first month
Breastfeeding: what to expect after the first month
Breastfeeding problems after the first month
Literature
1 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.- Breastfeeding Academy Protocol Committee, "AVM Clinical Protocol #20: Breast engorgement." Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
2 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe and Frauenheilkunde . 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. ABM Clinical Protocol# 4: Mastitis , Revized 2014. Breastfe 9009 H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. ABM Clinical Protocol# 4: Mastitis , Revized 2014. Breastfe 9009 H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
4 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". G Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121. nine0095
5 Amir L. Breastfeeding managing ‘supply’ difficulties.