Induced labor timeline
Induced labour | Pregnancy Birth and Baby
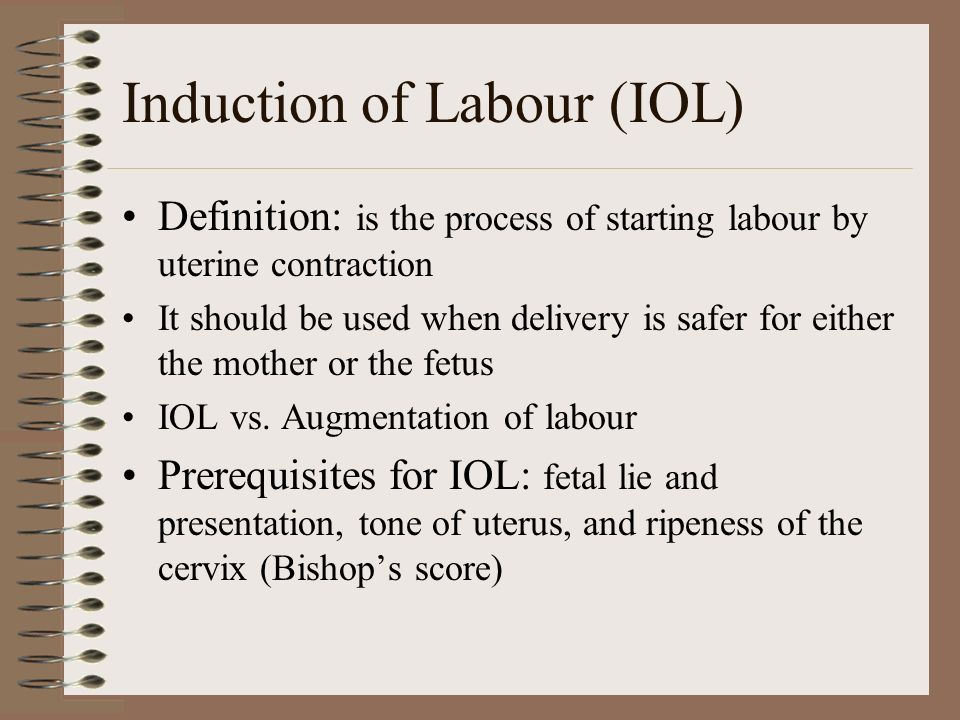
What is an induced labour?
Labour normally starts naturally any time between 37 and 42 weeks of pregnancy. The cervix softens and starts to open, you will get contractions, and your waters break.
In an induced labour, or induction, these labour processes are started artificially. It might involve mechanically opening your cervix, breaking your waters, or using medicine to start off your contractions — or a combination of these methods.
In Australia, about 1 in 3 women has an induced labour.
What are the differences between an induced and a natural labour?
An induced labour can be more painful than a natural labour. In natural labour, the contractions build up slowly, but in induced labour they can start more quickly and be stronger. Because the labour can be more painful, you are more likely to want some type of pain relief.
If your labour is induced, you are also more likely to need other interventions, such as the use of forceps or ventouse (vacuum) to assist with the birth of your baby. You will not be able to move around as much because the baby will be monitored more closely than during a natural labour.
You will only be offered induced labour if there is a risk to you or your baby's health. Your doctor might recommend induced labour if:
- you are overdue (more than 41 weeks pregnant)
- there is a concern the placenta is not working as it should
- you have a health condition, such as diabetes, kidney problems, high blood pressure or pre-eclampsia
- the baby is making fewer movements, showing changes in its heart rate, or not growing well
- your waters have broken, but the contractions have not started naturally
- you are giving birth to more than one baby (twins or multiple birth)
Not everyone can have an induced labour. It is not usually an option if you have had a caesarean section or major abdominal surgery before, if you have placenta praevia, or if your baby is breech or lying sideways.
Can I decide whether to have an induced labour?
If you are overdue, you might decide to wait and see if labour will start naturally. However, if there is a chance you or your baby are at risk of complications, you might need to consider induced labour before your due date.
However, if there is a chance you or your baby are at risk of complications, you might need to consider induced labour before your due date.
When making your decision, discuss the risks and benefits with your doctor. Do not be afraid to ask lots of questions, such as:
- Why do I need an induction?
- How will it affect me and my baby?
- What will happen if I do not have the induction?
- What procedures are involved and how will you care for me and my baby?
You might need to consider several other health concerns. For example, there is a higher risk of stillbirth or other problems if your baby is not born before 42 weeks, and an increased risk of infection if your waters break more than 24 hours before labour starts.
What can I expect with an induced labour?
During the late stages of your pregnancy, your healthcare team will carry out regular checks on your health and your baby's heath. These checks help them decide whether it is better to induce labour or to keep the baby inside. Always tell your doctor or midwife if you notice your baby is moving less than normal.
Always tell your doctor or midwife if you notice your baby is moving less than normal.
If they decide it is medically necessary to induce labour, first your doctor or midwife will do an internal examination by feeling inside your vagina. They will feel your cervix to see if it is ready for labour. This examination will also help them decide on the best method for you.
It can take from a few hours to as long as 2 to 3 days to induce labour. It depends how your body responds to the treatment. It is likely to take longer if this is your first pregnancy or you are less than 37 weeks pregnant.
What options are there to induce labour?
There are different ways to induce labour. Your doctor or midwife will recommend the best method for you when they examine your cervix. You may need a combination of different strategies. You will need to provide written consent for the procedure.
Sweeping the membranes
During a vaginal examination, the midwife or doctor makes circular movements around your cervix with their finger. This action should release a hormone called prostaglandins. You do not need to be admitted to hospital for this procedure and it is often done in the doctor's room. This can be enough to get labour started, meaning you will not need any other methods.
This action should release a hormone called prostaglandins. You do not need to be admitted to hospital for this procedure and it is often done in the doctor's room. This can be enough to get labour started, meaning you will not need any other methods.
Risks: This is a simple and easy procedure; however, it does not always work. It can be a bit uncomfortable, but it does not hurt.
Oxytocin
A synthetic version of the hormone oxytocin is given to you via a drip in your arm to start your contractions. When the contractions start, the amount of oxytocin is adjusted so you keep on having regular contractions until the baby is born. This whole process can take several hours.
Risks: Oxytocin can make contractions stronger, more frequent and more painful than in natural labour, so you are more likely to need pain relief. You will not be able to move around much because of the drip in your arm and you will also have a fetal monitor around your abdomen to monitor your baby.
Sometimes the contractions can come too quickly, which can affect the baby's heart rate. This can be controlled by slowing down the drip or giving you another medicine.
Artificial rupture of membranes ('breaking your waters')
Artificial rupture of membranes (ARM) is used when your waters do not break naturally. Your doctor or midwife inserts a small hook-like instrument through your vagina to make a hole in the membrane sac that is holding the amniotic fluid. This will increase the pressure of your baby's head on your cervix, which may be enough to get labour started. Many women will also need oxytocin to start their contractions.
Risks: ARM can be a bit uncomfortable but not painful. There is a small increased risk of a prolapsed umbilical cord, bleeding or infection.
Prostaglandins
A synthetic version of the hormone prostaglandins is inserted into your vagina to soften your cervix and prepare your body for labour. It can be in the form of a gel, which may be given in several doses (usually every 6 to 8 hours), or a pessary and tape (similar to a tampon), which slowly releases the hormone over 12 to 24 hours. You will need to lie down and stay in hospital after the prostaglandins is inserted. You may also then need ARM if your waters have not broken, or oxytocin to bring on the contractions.
You will need to lie down and stay in hospital after the prostaglandins is inserted. You may also then need ARM if your waters have not broken, or oxytocin to bring on the contractions.
Prostaglandins gel is often the preferred method of inducing labour since it is the closest to natural labour. Tell your midwife or doctor straight away if you start to experience painful, regular contractions 5 minutes apart for your first baby, or 10 minutes apart for subsequent babies, or if your waters break, because these are both signs that your labour is beginning.
Risks: Some women find their vagina is sore after the prostaglandin gel, or they might experience nausea, vomiting or diarrhoea. These side effects are rare and there is no evidence that induction using prostaglandin is any more painful than a natural labour.
Very rarely, the contractions can come too strongly, which can affect the baby's heart rate. This can be controlled by giving you another medicine or removing the pessary.
You need to let your doctor or midwife know immediately if you start bleeding, or if your baby is moving less, because this could be a sign that something is wrong.
Cervical ripening balloon catheter
A cervical ripening balloon catheter is a small tube attached to a balloon that is inserted into your cervix. The balloon is inflated with saline, which usually puts enough pressure on your cervix for it to open. It stays in place for up to 15 hours, and then you will be examined again.
Tell your midwife or doctor straight away if you start to experience painful, regular contractions 5 minutes apart for your first baby, or 10 minutes apart for subsequent babies, or if your waters break, because these are both signs that your labour is beginning.
You may also need ARM or oxytocin if you are using a cervical ripening balloon catheter.
Risks: Inserting the catheter can be a bit uncomfortable but not painful.
You also need to let your doctor or midwife know immediately if you start bleeding, or your baby is moving less, because this could be a sign that something is wrong.
Can I have pain relief during induced labour?
Induced labour is usually more painful than natural labour. Depending on the type of induction you are having, this could range from discomfort with the procedure or more intense and longer lasting contractions as a result of the medication you have been given. Women who have induced labour are more likely to ask for an epidural for relief.
Because inductions are almost always done in hospital, the full range of pain relief should be available to you. There is usually no restriction on the type of pain relief you can have if your labour is induced.
Are there any risks with inducing labour?
There are some increased risks if you have an induced labour. These include that:
- it will not work — in about 1 of 4 cases, women go on to have a caesarean
- your baby will not get enough oxygen and their heart rate is affected
- you or your baby get an infection
- your uterus tears
- you bleed a lot after the birth
What happens if the induction does not work?
Not all induction methods will work for everyone. Your doctor may try another method, or you might need to have a caesarean. Your doctor will discuss all of these options with you.
Your doctor may try another method, or you might need to have a caesarean. Your doctor will discuss all of these options with you.
Learn more here about the development and quality assurance of healthdirect content.
Labor induction - Mayo Clinic
Overview
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).
- An infection in the uterus (chorioamnionitis).
- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).

- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).
- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Risks
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction.
 An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary. - Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.
- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery. Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
An emergency C-section is needed to prevent life-threatening complications.
 The uterus might need to be removed.
The uterus might need to be removed. - Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.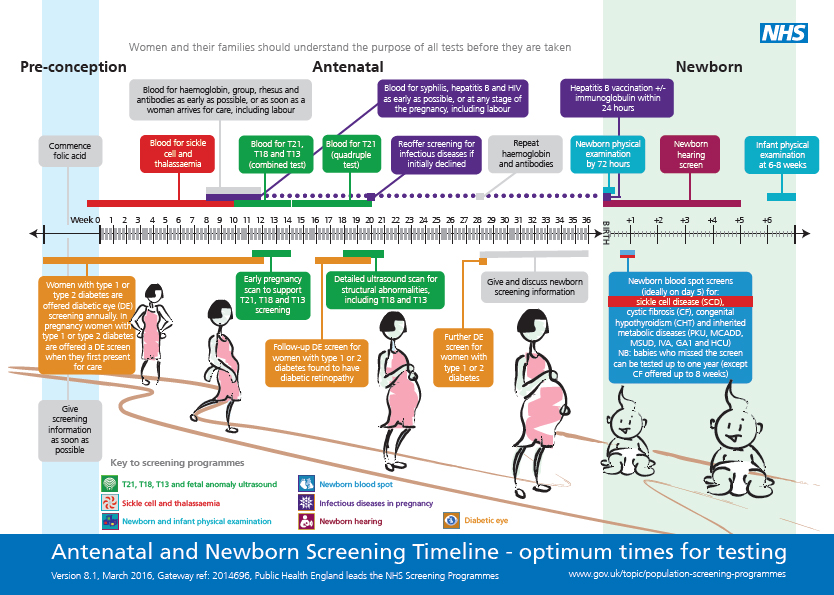
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac. With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus.
 This separates the sac from the cervix and the lower uterine wall, which might help start labor.
This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening. The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
assessment of oxidative status, matrix metalloproteinases and their tissue inhibitors in amniotic fluid
Introduction. Early delivery for medical reasons by the mother and/or fetus in modern obstetrics is the main way to reduce maternal and perinatal mortality. Its frequency is steadily increasing in the structure of all preterm births and averages 30% [1, 2, 3]. Induced preterm labor for medical reasons is most often abdominal. They are performed in situations requiring termination of pregnancy in life-threatening conditions of the mother and/or fetus [4-7]. With sparing operative delivery according to indications from the fetus, the death of children is reduced, but there are serious violations of postnatal adaptation [8, 9]. In conditions of oxygen deficiency and due to anatomical and physiological features in premature newborns, various perinatal injuries, mainly cerebrovascular disorders, often occur. Ischemia of the nervous tissue leads to the activation of lipid peroxidation processes and an increase in the formation of free radicals [10, 11].
In conditions of oxygen deficiency and due to anatomical and physiological features in premature newborns, various perinatal injuries, mainly cerebrovascular disorders, often occur. Ischemia of the nervous tissue leads to the activation of lipid peroxidation processes and an increase in the formation of free radicals [10, 11].
In recent years, the pathogenesis of brain damage during perinatal hypoxia has been associated with dysfunction of the extracellular matrix, since it is less protected from oxidative damage than cells [12, 13]. Under the influence of pathological forms of oxygen, the activity of matrix metalloproteinases (MMP) increases, which are proteolytic enzymes, the main role of which is the degradation of the connective tissue matrix of tissues, which leads to the formation of structural tissue defects and the development of inflammation [14, 15, 16]. The concentration of MMPs and their tissue inhibitors increases in direct proportion to the severity of the resulting disorders [17, 18, 19].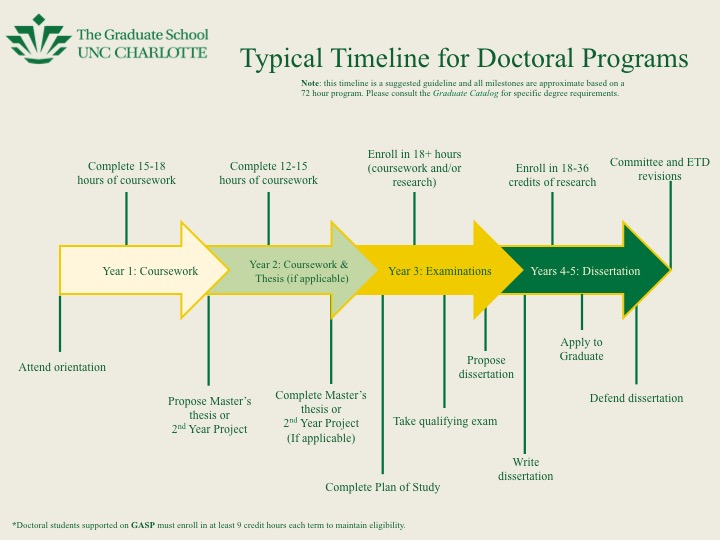
The search for early markers of brain damage and ways to protect against pathogenic agents is recognized as a priority in medical science to reduce mortality and disability in children born with low and very low birth weight.
Purpose of the study. Evaluation of the oxidative status, the concentration of matrix metalloproteinases-1,9 and their tissue inhibitors in the amniotic fluid of fetuses with low body weight during early abdominal delivery.
Materials and research methods. The study included 142 women who were divided into two groups. The main group consisted of 102 women delivered by caesarean section at 28-33.6 weeks of pregnancy in the interests of the mother and/or fetus. Exclusion criteria : antenatal fetal death, congenital malformations of the fetus, multiple pregnancy. The comparison group consisted of 30 patients who did not have severe obstetric and perinatal complications, who were delivered by abdominal route at full term for obstetric indications (uterine scar, aggravated obstetric and gynecological history). nine0005
nine0005
To assess the oxidative status, the concentration of MMP-1, MMP-9 and their tissue inhibitors (TIMP-1) in 64 women, samples of amniotic fluid were taken after an incision on the uterus during abdominal delivery by amniotomy. Amniotic fluid in a volume of 5 ml was taken into a sterile tube with a needle for spinal puncture, and lithium heparinate (14 IU/ml) was added. The samples were centrifuged at 3000 rpm (1200 g) for 15 minutes, and the concentration of thiobarbiturate-reactive products (TBRP) was determined in the supernatant by the photometric method on a KFK-3 spectrophotometer at a wavelength of 532 nm. The concentration of TBRP was estimated from the change in optical density caused by staining with a complex of malondialdehyde (MDA) with thiobarbituric acid in a ratio of 1:2 using a reagent kit from ZeptoMetrix Corporation (USA) cat. No. 0801192. The concentration of matrix metalloproteinases and their tissue inhibitors was determined using a set of reagents from Ray Biotech (USA), cat. No. ELH-MMP9-001 by enzyme immunoassay (sensitivity 10 pg/ml) using a vertical Multiscan photometer from Labsystem (Finland) at a wavelength of 450 nm [20].
Amniotic fluid samples were collected at the Perinatal Center (Clinical) of the Altai Territory (Barnaul) in accordance with the recommendations and requirements of the ethical committee. All patients signed a voluntary informed consent for the collection of biological material. nine0005
Statistical processing of the material was carried out using Microsoft Excel spreadsheets and the IBM SPPS Statistics application software package. Comparison of quantitative values in two independent groups was carried out using the non-parametric Mann-Whitney U-test. The data obtained are presented as median (Me) and interquartile range (25th and 75th percentiles). Qualitative characteristics were evaluated using the criterion χ 2 . Stepwise discriminant analysis was used to construct a mathematical model for predicting the severity of cerebral ischemia in newborns with the derivation of linear equations. The critical level of significance (p) was taken at a value less than 0.05. nine0005
The critical level of significance (p) was taken at a value less than 0.05. nine0005
Results and discussion. Induced preterm labor by caesarean section was performed in patients of the main group according to indications from the mother's side - in 70 (68.6%) cases, from the fetus - in 32 (31.4%) cases. The range of indications for operative delivery is shown in Figure 1.
As can be seen from Figure 1, the main indication for early delivery was severe preeclampsia (38.2%), in every fourth case - progressive placental insufficiency, in third place (17, 6%) - premature detachment of a normally located placenta (PONRP). nine0005
All 102 premature newborns were diagnosed with cerebral ischemia of hypoxic-ischemic origin, and in 44.1% - severe, which was combined with respiratory distress syndrome. Indications for operative delivery in patients of the main group, depending on the severity of cerebral ischemia (CI) of newborns, are shown in Figure 2.
and chronic placental dysfunction - premature detachment of a normally located placenta (p=0.03) and progressive intrauterine fetal hypoxia (p<0.001). On the contrary, mild and moderate CI were more often observed in children whose mothers were delivered early due to severe preeclampsia (p<0.001). During delivery due to worsening of the course of extragenital diseases (EGD) and insolvency of the scar on the uterus, cases of severe CI in premature newborns were not registered. nine0005
The concentration of TBRP in the amniotic fluid taken before the onset of labor immediately after the incision of the lower uterine segment in patients with induced preterm labor was significantly higher compared to that in the comparison group: 14.1±2.7 and 3.9±0 .9 nmol/ml (p<0.001), which reflects the activation of lipid peroxidation processes in fetuses whose mothers were delivered ahead of schedule due to severe obstetric complications in the pregnant woman and/or fetus.
The concentrations of MMP-1,9 and their tissue inhibitors (TIMP-1) in the amniotic fluid of premature fetuses are shown in Table 1.
fetal and newborn brain [15, 17, 18]. As can be seen from Table 1, the activity of MMP-9 in the amniotic fluid of premature fetuses, taken immediately after the incision on the uterus from patients without labor, was higher than in full-term fetuses of the comparison group, which was accompanied by a significant inhibition of TIMP-1 function and a higher ratio MMP-1.9/TIMP-1 (p<0.05).
For the automated diagnosis of severe CI, according to the results of complex studies in premature newborns, we used a step-by-step discriminant analysis. As a result, a classification matrix was obtained for a training sample of newborns with varying degrees of severity of cerebral ischemia who were born surgically. The overall classification accuracy was 81.6%, which can be considered an excellent result (>80%): 69.2% - the proportion of correct classifications for children with severe CI and 88.0% - with mild and moderate CI. nine0005
Two linear equations of discriminant functions were compiled to predict the severity of CI in premature newborns, substituting the values of MMP-9 into each of them, it is possible to assign a newborn to one of the two groups corresponding to the highest value of the function with a probability of 81.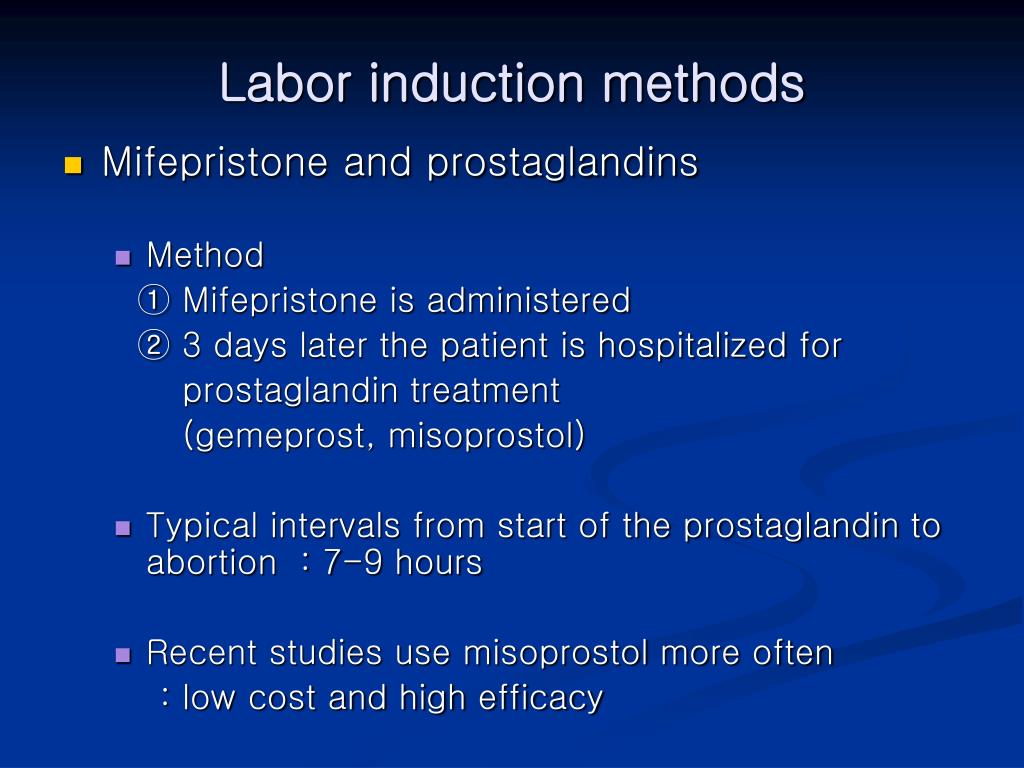 6%.
6%.
Classification equations of discriminant functions:
D 0 (light and medium CI) = -10.29 + 0.064×MMP9
Conclusion. Thus, in fetuses from mothers prematurely delivered by the abdominal route due to life-threatening conditions, oxidative stress occurs. The severity of antenatal hypoxia is confirmed by the high activity of the thiobarbiturate-reactive product - malondialdehyde and the enzyme that destroys type IV collagen - matrix metalloproteinase-9 compared with fetuses during urgent planned abdominal birth. A decrease in the concentration of tissue inhibitors of matrix metalloproteinases, which are the main component of the blood-brain barrier of the fetal brain, can be regarded as inhibition of their function in conditions of severe hypoxia/ischemia in placental insufficiency, which accompanies all severe obstetric complications. nine0005
Prognostic calculation of the severity of cerebral ischemia in the amniotic fluid of the fetus during early abdominal delivery allows you to develop in advance the tactics of managing premature newborns, including rehabilitation measures.
Management of pregnancy resulting from the use of ART. Pregnancy after IVF
The widespread introduction of Assisted Reproductive Technologies (ART) in medicine and the increasing awareness of infertile couples who want to have children have led to a significant increase in the number of pregnant women who become pregnant as a result of the use of ART. nine0005
But what is special about an induced pregnancy? Isn't it all over already? After all, the problem is solved. And I'm finally pregnant! Isn't it time for me to relax and not go anywhere else, not take endless tests ???
Unfortunately, you can't relax. After all, it is known that induced pregnancy is at high risk for the development of a wide variety of obstetric complications. In this regard, there is an urgent need for careful monitoring and examination of pregnant women in order to reduce the incidence of complications, develop tactics for managing pregnancy and childbirth, maintaining the health of the woman and getting a healthy baby. nine0005
nine0005
The peculiarities of the course of pregnancy resulting from IVF include:
- tendency to miscarriage;
- multiple pregnancy;
- high infectious index.
An analysis of the course of induced pregnancy showed that the highest frequency of termination of pregnancy after IVF occurs in the first trimester, in the second and third trimesters, a decrease in the frequency of the threat of termination by 1.5 times is characteristic.
nine0085Pregnancy after ART is characterized by the formation of primary placental insufficiency, which requires early prescription of drugs aimed at its prevention and treatment.
In general, during pregnancy after IVF, the frequency of obstetric complications (the threat of spontaneous abortion, isthmic-cervical insufficiency, preeclampsia, infection of the fetus, bleeding disorders, the formation of placental insufficiency, improper attachment of the placenta) is 2-3 times higher than during pregnancy, occurring naturally.