Breast pigmentation during pregnancy
Extensive hyperpigmentation during pregnancy: a case report
- Journal List
- J Med Case Reports
- v.5; 2011
- PMC3183040
J Med Case Reports. 2011; 5: 464.
Published online 2011 Sep 19. doi: 10.1186/1752-1947-5-464
,1,2 and 1
Author information Article notes Copyright and License information Disclaimer
Introduction
Skin hyperpigmentation is common during pregnancy and often is due to endocrinological changes. Usual patterns include linea nigra, darkening of areola and melasma. We report a rare diffused hyperpigmentation condition in a pregnant woman of dark colored skin.
Case presentation
A 19-year-old Tanzanian primigravida at 32 weeks gestation presented at our antenatal clinic concerned about an insidious but progressive onset of unusual darkening of her abdominal skin and both breasts. Her antenatal record was unremarkable except for this unusual onset of abnormal skin color. Findings from her physical examination were unremarkable, and she had a normal blood pressure of 120/70 mmHg. Her abdomen was distended with a uterine fundus of 34 weeks. Almost her entire abdominal skin had darkly colored diffuse deep hyperpigmentation extending cephalad from both iliac fossae to involve both breasts to 2-3 cm beyond the areolae circumferentially. She had a fetus in longitudinal lie and cephalic presentation, with a normal fetal heart rate of 140 beats per minute. Other examination findings were unremarkable. The impression at this stage was exaggerated pigmentation of pregnancy. No medical treatment was offered but she was counseled that she might need medical treatment after delivery. She progressed well and had spontaneous labor and normal delivery at 38 weeks gestation. She was lost to follow up.
She progressed well and had spontaneous labor and normal delivery at 38 weeks gestation. She was lost to follow up.
Conclusion
Unusual pregnancy-related skin hyperpigmentation can occur with no adverse consequences to pregnancy, although may worry a pregnant woman. Reassurance and conservative management may be all that is required to allay a patient's concerns.
Hyperpigmentation during pregnancy is commonly due to endocrinological changes. The usual pattern will be seen as linea nigra, melasma and darkening of areola, axillae and medial thighs [1-3]. Extensive hyperpigmentation, however, is unusual, especially in people with dark colored skin [4,5]. Such hyperpigmentation may sometimes be associated with hyperthyroidism [1,5]. We present a case of an unusual pattern of pigmentation in a primigravida seen in her mid-third trimester, who had an unremarkable pregnancy, labor, delivery and postpartum period.
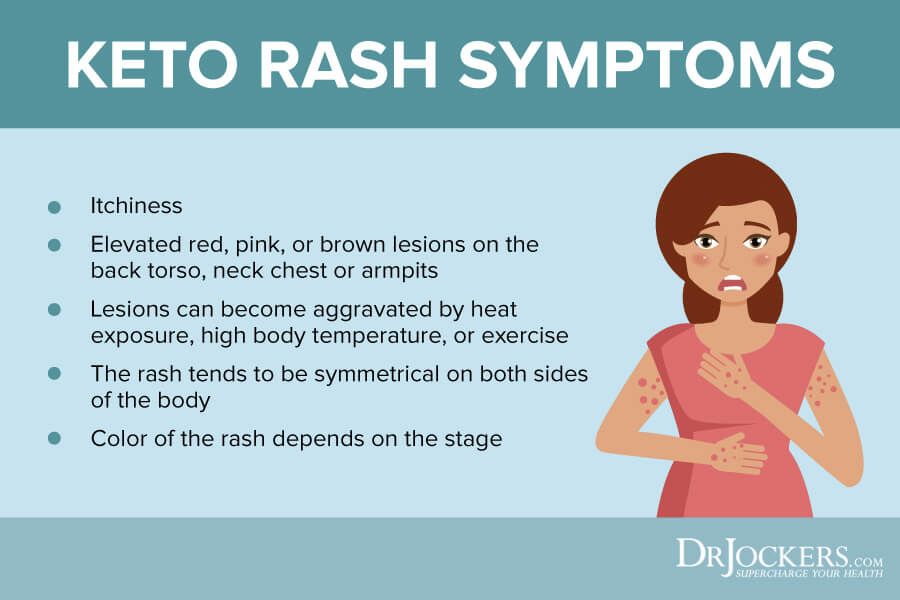
A 19-year-old Tanzanian primigravida at 32 weeks of gestation sought care at a tertiary hospital antenatal clinic. She presented with concerns of an insidious but progressive onset of an unusual darkening of her abdominal skin and both breasts. The darkening was not associated with itching or irritation of the skin.
She presented with concerns of an insidious but progressive onset of an unusual darkening of her abdominal skin and both breasts. The darkening was not associated with itching or irritation of the skin.
She booked for antenatal care at a peripheral clinic and her progress had been unremarkable except for this unusual onset of abnormal skin color. She had no previous history of allergies or family history of skin condition. She was not on any medication except for prescribed iron and folic acid tablets given during antenatal consultations. Her past medical history was unremarkable with no history suggestive of goiter or hyperthyroidism.
On physical examination, her general condition was fair. She was not pale and had no lower limb edema. She had a pulse rate of 70 beats per minute that was regular. Her blood pressure was 120/70 mmHg. Her abdomen was distended with a uterine fundus of 34 weeks. A linea nigra was clearly seen, but in addition almost the entire abdominal skin had dark colored diffuse deep hyperpigmentation, extending from both iliac fossae to involve both breasts (nipples and areolae) to about 2-3 cm beyond the areolae circumferentially (Figure ). She had a fetus in longitudinal lie, cephalic presentation with a normal fetal heart rate of 140 beats per minute. Other system examination findings were unremarkable.
She had a fetus in longitudinal lie, cephalic presentation with a normal fetal heart rate of 140 beats per minute. Other system examination findings were unremarkable.
Open in a separate window
Exaggerated hyperpigmentation of pregnancy. Extensive hyperpigmentation of pregnancy involving both breast and abdominal skin.
The impression at this stage was exaggerated pigmentation of pregnancy. No medications were prescribed, but she was reassured that the condition should have no effect on her pregnancy and its outcome. She continued attending antenatal care regularly. She had spontaneous onset of labor and normal delivery of a baby girl weighing 3200 g with an Apgar score of 9 and 10 at the first and fifth minutes respectively at 38 weeks gestation.
Our patient did not return for follow-up during her postpartum period. She was contacted by phone three months after delivery and she reported that her skin condition had not resolved. We lost contact with her thereafter.
Skin hyperpigmentation is common in pregnancy and often is well described and completely benign in nature [2,5]. The physiology of hyperpigmentation appears to be related to the increased production of estrogens, and perhaps to increased levels of progesterone or a melanocyte-stimulating hormone [1-3,5]. In selected areas of the body such as the linea alba and areola, hyperpigmentation is probably related to the distribution of melanocytes, but extension of these cells beyond these parts may explain unusual patterns of distribution, as in this case [2,3,6].
The intensity of the hyperpigmentation, however, may be related to environmental factors or even intake of some drugs, although other causes may include pre-existing conditions, such as hyperthyroidism, and a genetic predisposition [1,3,5]. Nevoid hyperkeratosis of the nipple and areola should be considered in the absence of abdominal involvement. Dermal melanocytosis is another rare condition that could present similarly to our case; in this condition pregnancy and sun-exposure are thought to be the triggering factors [5].
Most pregnancy-related skin hyperpigmentation is benign and is usually resolved after delivery (usually within a year), although women may be concerned [1,2,5]. Medical treatment is rarely required. In cases where the condition persists, bleaching agents may be used [1,3,5], although at times their effectiveness may be unsatisfactory [5]. Proper counseling and assurance is the only reliable alternative in such cases [5].
Although skin hyperpigmentation is common in pregnancy, extensive pigmentation, as in this case, is rare. Patients may be cosmetically concerned, but all that is required from the health professional is reassurance that the condition has no adverse affect on pregnancy outcome.
Written informed consent was obtained from the patient for publication of this case report and accompanying image. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
The authors declare that they have no competing interests.
AM managed the patient and wrote the initial manuscript. ST performed the initial literature search. Both ST and MM reviewed the subsequent manuscripts and approved the final manuscript.
ST performed the initial literature search. Both ST and MM reviewed the subsequent manuscripts and approved the final manuscript.
- Wade TR, Wade SL, Jones HE. Skin changes and diseases associated with pregnancy. Obstet Gynecol. 1978;52(2):233–242. [PubMed] [Google Scholar]
- Elling SV, Powell FC. Physiological changes in the skin during pregnancy. Clin Dermatol. 1997;15(1):35–43. doi: 10.1016/S0738-081X(96)00108-3. [PubMed] [CrossRef] [Google Scholar]
- Blereau RP. Three cases of hyperpigmentation of pregnancy. Consultantlive. 2002;42(10) [Google Scholar]
- Tunzi M, Gray GR. Common skin conditions during pregnancy. Am Fam Physician. 2007;75(2):211–218. [PubMed] [Google Scholar]
- Ingber A. In: Obstetric Dermatology. Lebwohl M, editor. Jerusalem: Springer; 2009. hyperpigmentation and melasma; pp. 7–17. [Google Scholar]
- Szabo G. The number of melanocytes in human epidermis. Br Med J. 1954;1(4869):1016–1017. doi: 10.1136/bmj.1.4869.1016. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Articles from Journal of Medical Case Reports are provided here courtesy of BioMed Central
Changes to your skin during pregnancy
beginning of content3-minute read
Listen
As your pregnancy develops, you may find that you experience changes to your skin and hair. Some women can develop dark patches on their face and hormonal changes can make your skin a little darker.
Some women can develop dark patches on their face and hormonal changes can make your skin a little darker.
You may also develop stretch marks on your body, particularly around your stomach where your skin is stretching to accommodate your growing baby.
Chloasma - dark patches on the face
Some pregnant women develop dark irregular patches on their face most commonly on the upper cheek, nose, lips, and forehead. This is called 'chloasma'. It is also sometimes known as 'melasma' or the 'mask of pregnancy'.
Chloasma is thought to be due to stimulation of pigment-producing cells by female sex hormones so that they produce more melanin pigments (dark coloured pigments) when the skin is exposed to sun. Some women develop these patches when they take oral contraceptives (the pill).
Women with a light brown skin type who are living in regions with intense sun exposure are more likely to develop these patches. The patches usually fade over a period of several months after giving birth, though they may last for several years for some women.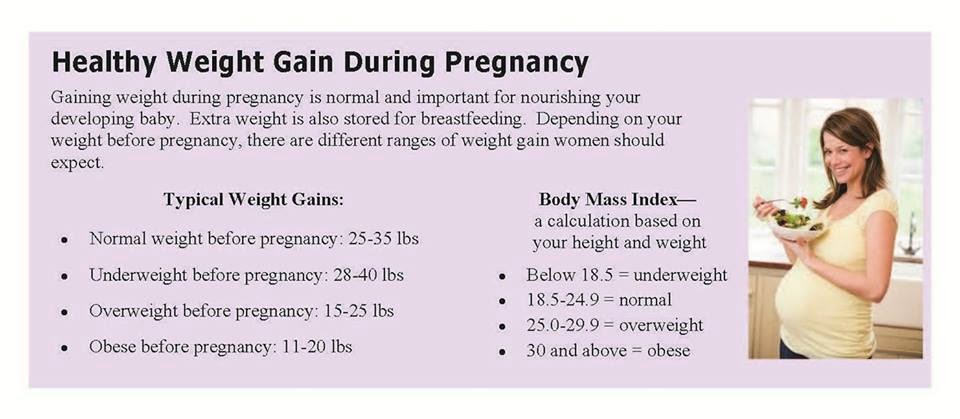
Careful protection of the skin using broad spectrum sunscreens every day during pregnancy and while taking the pill may make it less likely that chloasma will develop. It is necessary to continue to use sunscreen after pregnancy as sun exposure may cause the patches to reappear. Some creams that need to be prescribed by doctors may help to fade the patches.
Skin and hair changes
Hormonal changes taking place in pregnancy will make your nipples and the area around them go darker. Your skin colour may also darken a little, either in patches or all over. Birthmarks, moles and freckles may also darken. Some women develop a dark line down the middle of their stomach, called 'linea nigra'. These changes will gradually fade after the baby is born, although your nipples may remain a little darker.
If you sunbathe while you are pregnant, you may burn more easily. Protect your skin with a good high-factor sunscreen and don't stay in the sun for a long time.
Hair growth can also increase in pregnancy, and your hair may be greasier. After the baby is born, it may seem as if you are losing a lot of hair but you are simply losing the extra hair.
Stretch marks
Many women develop stretch marks during their pregnancy, usually in the last 3 months.
They usually appear on your stomach or sometimes on your upper thighs or breasts. Stretch marks are not harmful and over time, your skin will shrink and the stretch marks will fade into white-coloured scars.
Find out more on stretch marks.
Sources:
Royal Women's Hospital Victoria (Common concerns in early pregnancy - itching and skin), The Australasian College of Dermatologists (Striae), The Australasian College of Dermatologists (Melasma)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2020
Back To Top
Related pages
- Common discomforts during pregnancy
- Stretch marks
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Some features, tools or interaction may not work correctly.
Pigmentation during pregnancy is not a disease
Waiting for a little baby is the most magical and unique period in a woman's life. The expectant mother becomes mysterious, sensitive, caring and unhurried.
The body of a pregnant woman changes every day, and this is natural - after all, a small defenseless little man grows under her heart, whose life and health largely depends on her mother.
A woman already from the first weeks of pregnancy notices changes in her body: the shape is rounded, the breast becomes one size larger and more sensitive than before.
Pigmentation is a fairly common phenomenon during an interesting situation. The appearance of pigmentation on the face and body worries many women.
Some of them are interested in the causes of pigmentation on the skin, while others are trying to find ways to get rid of it. Pigment is a brown coloring matter. Pigmentation is more common in brunettes and dark-skinned women.
There is a popular belief that if a woman's skin deteriorates during pregnancy and age spots become noticeable, she will be a girl! But it is hardly possible to believe in it one hundred percent. Skin pigmentation is a temporary phenomenon, like pregnancy itself, and age spots also happen with boys in the tummy.
Brown spots in pregnant women are called differently: chloasma, mask, hyperpigmentation of the skin. Pigmentation most often appears on a woman's forehead, cheeks, chin, and also happens above the upper lip. A woman can also notice pigmented areas of skin with sharply defined edges on the neck, chest and tummy in the form of a thin strip. If earlier, with the beginning of spring, you had freckles on your face, then most likely their appearance will intensify during pregnancy as a kind of manifestation of pigmentation.
What causes pigmentation during pregnancy? Of course, this is a hormonal restructuring of the body of the woman herself, changes in the work of all organs, primarily the adrenal cortex and pituitary gland. There are opinions that pigmentation is a genetic phenomenon, and also takes place in case of a lack of folic acid in a woman's body.
There are opinions that pigmentation is a genetic phenomenon, and also takes place in case of a lack of folic acid in a woman's body.
In order to prevent and prevent the appearance of pigmented areas of the skin, pregnant women are advised to take quite affordable preventive measures:
- reduce sun exposure. Bright sunlight has beneficial properties, thanks to which vitamin D is constantly produced in the body, but even a short stay in the open sun can provoke pigmentation. If possible, wear light clothing that covers the body, as well as use sunscreen for children with a sufficiently high degree of protection;
- carefully monitor your own health, avoid hypothermia and colds;
- limit the use of cosmetics as much as possible in the summer to avoid the appearance of pigmentation and allergies;
- take complex vitamins specially formulated for pregnant women, especially folic acid;
- eat right, include more vegetables, fruits, cereals and dairy products in your menu;
- avoid stressful situations, do not get nervous and do not "wind" yourself over trifles.

Experts believe that when pigmentation appears while expecting a child, a woman should not take measures to remove them and especially worry about this, she should try to calmly accept these changes in the body, because the spots disappear, as a rule, on their own within two months after childbirth. But for a woman in an interesting position, even such harmless spots can ruin her mood and bring her to tears.
You always want to be beautiful and well-groomed!
If during pregnancy you were “lucky” to become a carrier of specific age spots, then here are some tips to make them less noticeable:
- You can prepare a mask of kefir and lemon juice. Apply such a mask to the skin, hold for about 15-20 minutes, then rinse thoroughly with warm water;
- gentle curd mask is a reliable assistant in the fight against age spots: mix cottage cheese with curdled milk, apply this mixture on your face for 15 minutes, then rinse thoroughly with boiled water;
- cucumber mask is good for whitening age spots.
 To prepare it, you need to grate the cucumber and apply on the face for 15 minutes, then remove with a cotton swab;
To prepare it, you need to grate the cucumber and apply on the face for 15 minutes, then remove with a cotton swab; - recommend freshly squeezed grapefruit juice and parsley juice to lighten age spots, which are applied to spots and washed off with water after 15-20 minutes. For the best effect, you need to repeat these procedures for at least one week.
In the fight against pigmentation, it is necessary to use only "folk" natural remedies that are very useful for the expectant mother and will not harm the baby.
And remember, characteristic skin changes during pregnancy are not a disease, but a natural phenomenon, just like the desire for something salty or sweet...
With the birth of a long-awaited baby, the spots will disappear and your beauty will return to you!
Consult a dermatologist. Consultation free of charge, appointment by phone: +7 (499) 608-88-08
Breast changes from the beginning of pregnancy to the end of breastfeeding
Medela experts tell you what changes occur in the breast from the beginning of pregnancy to the end of breastfeeding, and also share tips for breast care throughout this period.
Share this information
From the moment of conception, your body begins to prepare for the birth of your baby. This applies not only to the uterus - the anatomy of the breast also changes radically. This article will tell you what to expect in each trimester, during and after breastfeeding.
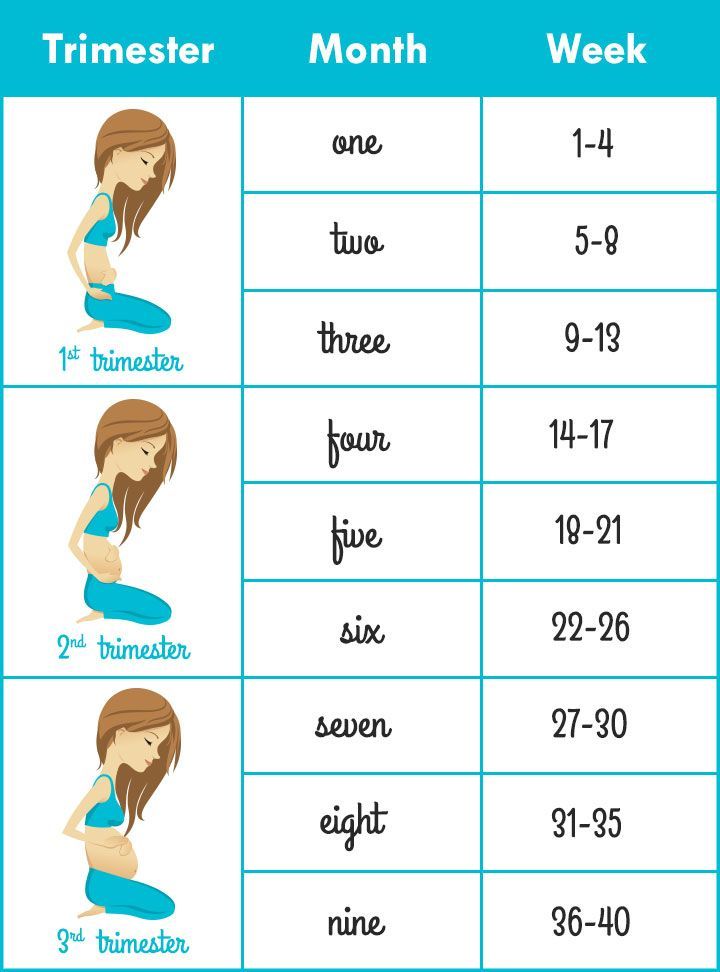
Breast changes in the first trimester
Early in pregnancy, many women notice changes in their breasts. Moreover, often they become the first signs of pregnancy. Fluctuations in hormone levels and changes in the structure of the mammary glands can cause increased sensitivity and soreness of the nipples and breasts as early as the third or fourth week. For some pregnant women, breast tenderness persists until childbirth, but for most it goes away after the first trimester.
“Sometimes during pregnancy, breasts grow very quickly in the first weeks, and sometimes their size increases gradually,” says Dr. Jacqueline Kent, a leading lactation specialist at the University of Western Australia. “All women are different. For some, breast size may not change much until childbirth or even after them. In general, we can say that by the time the milk arrives, the breast will most likely become one and a half times larger than before pregnancy! 1
“All women are different. For some, breast size may not change much until childbirth or even after them. In general, we can say that by the time the milk arrives, the breast will most likely become one and a half times larger than before pregnancy! 1
As soon as your regular bras start to feel tight (usually around 12 weeks), it's time to buy a maternity bra. The most comfortable, according to many women, are seamless models with wide straps made of soft, breathable fabric. It is best to avoid underwired bras as they can put pressure on the developing milk ducts.
It is important to take your measurements correctly in order to find the right bra with a good fit. Take measurements every couple of months, as you may need a different size bra as your baby grows and your breasts get bigger.
Breast changes in the second trimester
From about the 15th week of pregnancy, newly formed cells that produce milk are activated in the breast, and by about the 22nd week, milk production starts. 1 But don't worry - most of this milk will be absorbed by the body without going out, as pregnancy hormones prevent it from being overproduced or excreted.
1 But don't worry - most of this milk will be absorbed by the body without going out, as pregnancy hormones prevent it from being overproduced or excreted.
“During the second trimester, you may notice that the nipples and areolas (the areas of skin around the nipples) become darker and larger,” says Dr. Daniel Prime, Medical Research Associate at Medela. tubercles - the so-called glands of Montgomery. They secrete oil that moisturizes the nipples and will protect them from inflammation and infection when you start to feed. Scientists believe that the smell of this fat is similar to the smell of amniotic fluid and helps the newborn baby find the nipple.” 2
Do not use harsh soap for breast hygiene and do not rub hard with a towel as this can damage this natural lubricant. Just wash your breasts with warm water and pat dry. And if someone tells you to pinch or rub your nipples to prepare them for breastfeeding, don't listen to them!
If you have flat or inverted nipples, your pregnancy is over 32 weeks, and your pregnancy is normal, you can try inserting special nipple formers* into your bra in consultation with your doctor. They help to gently pull out the nipples so that it is easier for the newborn to grasp them. Consult your healthcare professional or read our article on flat and inverted nipples to learn more.
They help to gently pull out the nipples so that it is easier for the newborn to grasp them. Consult your healthcare professional or read our article on flat and inverted nipples to learn more.
If breast size increases dramatically during pregnancy, breast skin may itch and stretch marks may appear on it. A good moisturizer can help soothe itching. The appearance of stretch marks usually depends on genetics and skin type. If you have a predisposition to stretch marks, it is unlikely that you will be able to prevent them, but, fortunately, over time they will become lighter and less noticeable.
Breast changes in the third trimester
In the last trimester, you may again experience soreness and heaviness in your chest. A sleep bra will keep you comfortable at night, while a supportive sports bra will help you avoid soreness and ligament damage during exercise.
Don't forget to buy a pair of nursing bras one month before your baby is born. If possible, consult a specialist in the store or study the online guide to select the appropriate model and size. Every woman is different, but usually cups of a nursing bra are chosen one or two sizes larger than before pregnancy. The underbust girth may also increase as the ribcage expands to provide enough room for the baby. The sales assistant should choose the size of your bra, taking into account the appearance of milk after childbirth. Models with fasteners that can be unfastened with one hand make it easier to attach the baby to the breast.
Every woman is different, but usually cups of a nursing bra are chosen one or two sizes larger than before pregnancy. The underbust girth may also increase as the ribcage expands to provide enough room for the baby. The sales assistant should choose the size of your bra, taking into account the appearance of milk after childbirth. Models with fasteners that can be unfastened with one hand make it easier to attach the baby to the breast.
Surprising but true: milk appears in the breast even before the baby is born. This is why your nipples may start to produce some colostrum (the first breast milk), which will be quite thick and sticky. Sometimes this happens as early as 14 weeks, but more often it still happens in late pregnancy. To avoid the appearance of stains and smudges on clothes, you can use special bra pads.
“If you have diabetes or have been diagnosed with gestational diabetes, your doctor may tell you to express some colostrum by hand and freeze it. A recent study showed that after the 36th week it is quite safe if the pregnancy does not have other complications, 3 , says Dr. Prime, “Storing colostrum can come in handy because babies with diabetic mothers are at higher risk of hypoglycaemia (low blood sugar), and frequent colostrum feeding is the best remedy. . However, be prepared for the fact that there will be very little colostrum. You may only be able to express a few drops at first, and that’s perfectly fine.”
Prime, “Storing colostrum can come in handy because babies with diabetic mothers are at higher risk of hypoglycaemia (low blood sugar), and frequent colostrum feeding is the best remedy. . However, be prepared for the fact that there will be very little colostrum. You may only be able to express a few drops at first, and that’s perfectly fine.”
What happens to the breast after childbirth
Approximately two to four days after the baby is born (sometimes later if there was a caesarean section or a traumatic delivery), you will feel your breasts getting heavier and firmer - this means that the milk has come. 4
“This breast fullness is not only due to excessive milk production, there is also an increase in the amount of blood circulating around the breast and the volume of lymphatic fluid,” explains Dr. Prime, “All this is the result of a gradual decrease in the level of pregnancy hormones that began after the birth of a child and which allows the hormones responsible for the production of milk to enter into work.
During this period, you may experience soreness and discomfort in your breasts, a condition called breast swelling. This is quite common and usually resolves after a few days, during which time breastfeeding must continue. Read on for our tips on how to relieve swelling and discomfort, and if the problem persists, see a lactation consultant or healthcare provider.
What happens to the breast during lactation
For about the first three months of breastfeeding, your breasts are likely to fill up a lot before feeding. Over time, you may notice that your breasts become less full, but this does not mean at all that your milk production has decreased. If you are breastfeeding your baby exclusively and on demand, and at the same time he is growing well, then everything is in order with the amount of milk.
“Be prepared for the fact that after six months of breastfeeding, your breast size will begin to decrease,” Dr. Kent explains, “This is not a sign that your body is producing less milk.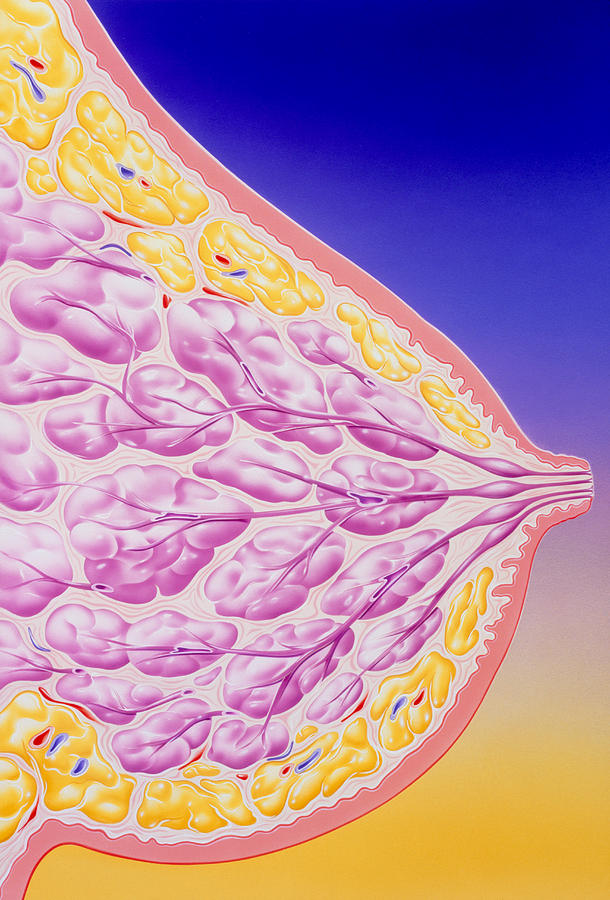 Most likely, the amount of adipose tissue in the breast simply decreased. By the time your baby is 15 months old, your breasts may be back to their pre-pregnancy size, but not smaller. However, whether you continue breastfeeding or not, you may still produce 100 to 300 ml of milk per day.”
Most likely, the amount of adipose tissue in the breast simply decreased. By the time your baby is 15 months old, your breasts may be back to their pre-pregnancy size, but not smaller. However, whether you continue breastfeeding or not, you may still produce 100 to 300 ml of milk per day.”
This may be due to the start of more efficient milk production after six months of breastfeeding, which, according to Dr. Kent's research, may be the result of redistribution of breast tissue. 5
How your breasts change after you stop breastfeeding
When you finally stop breastfeeding—whether after three weeks, three months, or three years—the lactation-related breast changes disappear. “After the complete cessation of breastfeeding, the breasts, as a rule, return to the size that they were before pregnancy. This usually happens in about three months, and for someone else while breastfeeding,” Dr. Kent explains, “If you get pregnant again, the whole process starts all over again. ”
”
Literature
1 Cox DB et al. Breast growth and the urinary excretion of lactose during human pregnancy and early lactation: endocrine relationship. Exp Physiol . 1999;84(2):421-434. - Cox D.B. et al., "Breast growth and urinary lactose excretion during pregnancy and lactation: an endocrine relationship." Exp Physiol. 1999;84(2):421-434.
2 Doucet S et al. The secretion of areolar (Montgomery’s) glands from lactating women elicits selective, unconditional responses in neonates.PLoS One . 2009;4(10): e 7579. - Doucet S. et al., "Papillary circle gland secretion (Montgomery's glands) in lactating women induces a selective unconditioned response in the newborn." PLOS One. 2009;4(10):e7579.
3 Forster DA et al. Advising women with diabetes in pregnancy to express breastmilk in late pregnancy (Diabetes and Antenatal Milk Expressing [DAME]): a multicentre, unblinded, randomized controlled trial.