Breast milk for cold sores
Breastfeeding and herpes | BabyCenter
- Community
- Getting Pregnant
- Pregnancy
- Baby names
- Baby
- Toddler
- Child
- Health
- Family
- Courses
- Registry Builder
- Baby Products
Advertisement
Condition
Herpes simplex type 1 (HSV-1), herpes simplex type 2 (HSV-2)
The potential problem
HSV-1 is a virus that usually causes cold sores or fever blisters around the mouth, but it can also cause similar blisters anywhere on the body above the waist. HSV-2, also a virus, usually causes genital sores or blisters.
Both forms of herpes can be passed on during skin-to-skin contact. In the United States, nearly 80 million people have some form of herpes. Herpes can cause serious infections in newborns because their immune systems are still developing.
Can I breastfeed?
Yes, with care. The herpes virus is not transmitted through breast milk. However, your baby could get infected by touching a blister or sore on your breast, mouth, or other area of your body.
Solution
To avoid spreading the virus, always keep clean clothing between your baby and any affected area of skin. Thoroughly wash your hands after using the toilet or touching a sore, and wash your hands and lay a clean towel or receiving blanket on your lap before holding your baby.
If you have a blister on or around your mouth, do not kiss your baby until the sore has completely disappeared. And don't let your baby touch – with her mouth, nose, hands, or other body part – any blisters on your skin.
If you have a herpes blister on your breast that's close to your nipple or areola, don't nurse from that side until the area has completely cleared up. Instead, express or pump your milk from that breast. If you can pump milk from the infected breast without letting your hands or any pump parts touch the sore, you can use the pumped milk to feed your baby. Otherwise, you must discard it. You may need to supplement your breast milk with formula or donor milk during these times. You can continue to nurse from the unaffected breast.
Otherwise, you must discard it. You may need to supplement your breast milk with formula or donor milk during these times. You can continue to nurse from the unaffected breast.
Your healthcare provider may prescribe antiviral medications such as acyclovir or vidarabine (which is sold in eyedrop form) to fight the herpes infection and help prevent future outbreaks. These drugs are generally considered safe during breastfeeding, but consult with your baby's doctor about taking them while nursing. Or check Lactmed, the drugs and lactation database of the National Institutes of Health.
Read about herpes during pregnancy.
Advertisement | page continues below
Was this article helpful?
Yes
No
Karen Miles
Karen Miles is a writer and an expert on pregnancy and parenting who has contributed to BabyCenter for more than 20 years. She's passionate about bringing up-to-date, useful information to parents so they can make good decisions for their families.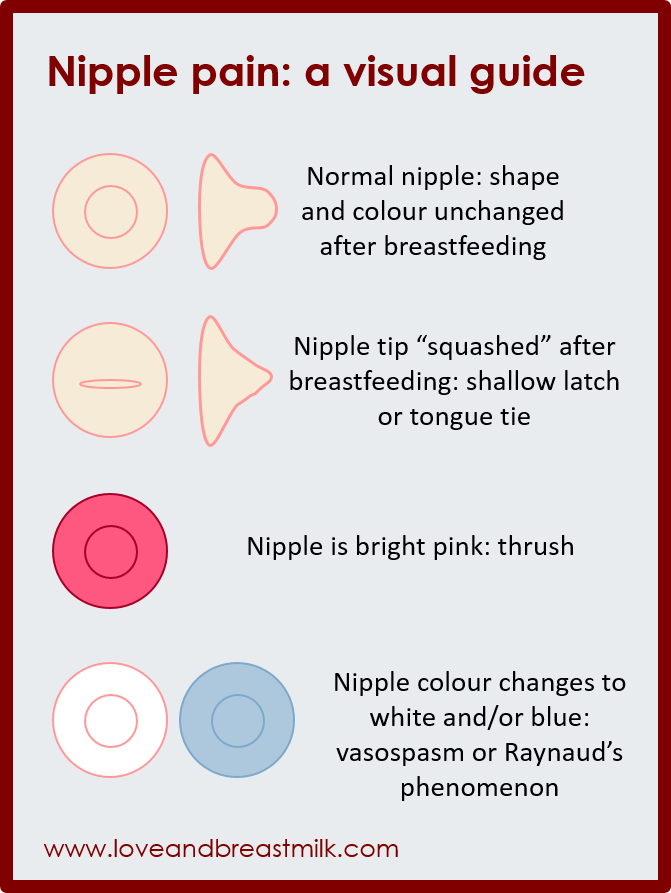 Her favorite gig of all is being "Mama Karen" to four grown children and "Nana" to nine grandkids.
Her favorite gig of all is being "Mama Karen" to four grown children and "Nana" to nine grandkids.
Herpes Simplex Virus (HSV) | Breastfeeding
Herpes simplex virus (HSV) in infants can be severe. Mothers with HSV can continue to breastfeed if no lesions are present on the breasts and if lesions elsewhere on the body are carefully and fully covered. Mothers with active lesions on the breast should temporarily stop breastfeeding from the affected breast and should not feed expressed breast milk from the affected breast.
Herpes simplex virus (HSV) is a lifelong virus that is categorized into two distinct herpesvirus species, herpes simplex virus 1 (HSV-1) and herpes simplex virus 2 (HSV-2). HSV-1 is typically transmitted by oral-oral contact to cause oral herpes but can also cause genital herpes through oral-genital contact. HSV-2 is typically sexually transmitted and causes genital herpes but can also cause infections in the mouth. Importantly, both types of virus can cause herpes disease in newborns and infants and can appear anywhere on the body.
In newborn infants, HSV infections are often severe and result in high rates of mortality and morbidity. Every precaution needs to be taken to prevent infants from being exposed to the herpes virus and appropriate hand hygiene should be done before holding the infant.
Is it safe for a mother to breastfeed if she has active herpetic lesions?
Maybe. Women with herpetic lesions may transmit HSV to their infants by direct or indirect contact with the lesions. Breastfeeding is acceptable if no lesions are present on the breasts and if active lesions elsewhere on the mother are carefully and fully covered. In cases where a mother has herpetic lesions on her breast, the mother should temporarily refrain from breastfeeding her infant from the affected breast or feeding her infant expressed breast milk from the affected breast. She should discard expressed breast milk from the affected side until the lesions have healed. A mother may breastfeed her infant or express milk from the unaffected breast but should ensure that the lesions on the affected breast are completely covered to avoid transmission. Mothers should also follow appropriate hand hygiene practices to avoid transmission of herpes to her infant.
Mothers should also follow appropriate hand hygiene practices to avoid transmission of herpes to her infant.
Providers: Lesions on the breast could easily be mistaken for impetigo or eczema. Questionable lesions should be tested promptly for HSV so that if positive, acyclovir (safe to use while breastfeeding) can be administered quickly and breastfeeding can be discontinued until the lesion has healed.
Some mothers may need additional support to maintain their milk production and/or supplement with their expressed human milk (previously expressed milk or expressed milk from the unaffected breast) or formula while herpetic lesions on the breast are healing. Mothers should talk with their physicians to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
Is it safe for a mother to give her infant hand expressed or pumped breast milk if she has active herpetic lesions on her breast?
No. Breast milk can be contaminated if it comes in contact with active herpetic lesions through touching the breast during hand expression or via the pump. Therefore, if a mother has herpetic lesions on her breast, she should discard expressed breast milk from the affected side until the lesions have healed. Expressing breast milk will be important for maintaining milk production while not directly breastfeeding from the affected breast. Mothers should be vigilant about practicing appropriate hand hygiene and cleaning the pump parts thoroughly. Mothers should talk with their healthcare provider to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
Breast milk can be contaminated if it comes in contact with active herpetic lesions through touching the breast during hand expression or via the pump. Therefore, if a mother has herpetic lesions on her breast, she should discard expressed breast milk from the affected side until the lesions have healed. Expressing breast milk will be important for maintaining milk production while not directly breastfeeding from the affected breast. Mothers should be vigilant about practicing appropriate hand hygiene and cleaning the pump parts thoroughly. Mothers should talk with their healthcare provider to determine if their lesions have healed and they can resume breastfeeding or expressing milk from the affected breast.
It is safe to use expressed breast milk from the unaffected breast, as long as the mother ensures that the lesions on the affected breast are completely covered to avoid transmission. Appropriate hand hygiene and cleaning the pump parts thoroughly are still important.
For more information about managing breastfeeding with specific medical conditions, read Lawrence RA, Lawrence R. (2016) Breastfeeding: A guide for the medical profession, 8th Edition.
Feeding when sick | Medela
If you or your baby are unwell, you may wonder if it is safe to breastfeed. The great news is that breastfeeding when you're sick is most often good for both of you. Read more about this in our article.
Share this information
Did you know that a breastfed baby is usually much less prone to illness? Although it is impossible to avoid them completely, the protective properties of breast milk help babies get sick less often 1 and recover faster than formula-fed babies.
Breast milk contains antibacterial and antiviral agents. 2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the use of breast milk to treat everything from conjunctivitis to cancer. 3.4
1 Scientists are already exploring the use of breast milk to treat everything from conjunctivitis to cancer. 3.4
Should a sick baby be breastfed? nine0021
Yes. Breastfeeding promotes recovery and also helps to calm the baby. Breast milk contains antibodies, white blood cells, stem cells, and protective enzymes that help fight infections and help your baby recover faster. 1,5,6 In addition, the composition of breast milk (the balance of vitamins and nutrients) is constantly adjusted to the baby's body to help him recover as soon as possible. Thus, you will spend less time on sick leave and visit the doctor less often. nine0009 7
“Breastfeeding gives the baby everything she needs when she is sick. This is his medicine, food, drink and comfort. For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
Surprisingly, when a child becomes ill, the composition of breast milk changes. When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. nine0009 8 When your baby is sick, your milk also spikes in immune-boosting cells (white blood cells). 5
When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. nine0009 8 When your baby is sick, your milk also spikes in immune-boosting cells (white blood cells). 5
In addition, breast milk is very easy to digest, making it ideal for babies with indigestion.
“At 12 months my daughter contracted norovirus and could only breastfeed,” recalls Maya, a mother of two in Spain. produce more milk. It was amazing. After 48 hours, I was able to meet the daily requirement for milk. It saved my baby from a drip." nine0003
It should be taken into account that sometimes during an illness it is necessary to change the habitual breastfeeding regimen. For example, with a cold, a baby may want to eat more often, but little by little, both to calm down and because of nasal congestion, which makes it difficult to apply to the chest for a long time. If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
What should I do if my baby is seriously unwell and cannot breastfeed? nine0021
Occasionally, if a child feels unwell, they may not have an appetite or the strength to feed. If your baby is not eating well, seek advice from your healthcare provider, nurse practitioner, or lactation consultant to help prevent dehydration.
You may be asked to express milk to feed your baby with a bottle, a Soft Cup*, or other suitable method that requires minimal effort from the baby. Pumping on a regular breastfeeding schedule will also help keep your milk supply stable. nine0003
You can express milk with one of our convenient breast pumps, such as the modern electronic Swing Flex** or the Harmony** manual breast pump. Rest assured, freshly expressed breast milk is just as good as breast milk, so your baby will get all the protection and support it needs.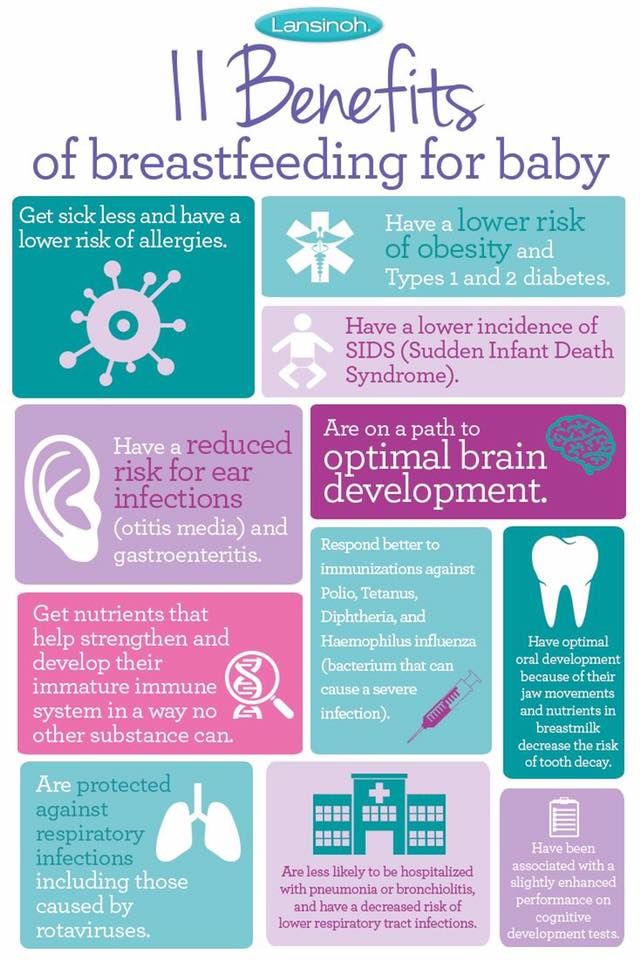
If you have concerns about your baby's health or how much milk they are drinking, see your doctor as soon as possible.
Can I continue to breastfeed if I become ill myself? nine0021
You may not want to do this if you feel unwell, but in most cases it is best to continue breastfeeding. If you have a cold, runny nose, diarrhoea, vomiting, or mastitis, continue breastfeeding as normal with your doctor's approval. The baby is unlikely to become infected through breast milk. What's more, the antibodies in your milk will help reduce your baby's risk of contracting the same 13 virus.
“Breastfeeding when sick is not only safe most of the time, but also beneficial. Your baby is the least at risk of catching your upset stomach or cold, as he is already in close contact with you and receives a daily dose of protective antibodies from milk, ”says Sarah Beeson. nine0003
If there is a risk of contracting a viral infection by airborne droplets, it is advisable to temporarily switch to expressing breast milk and bottle feeding.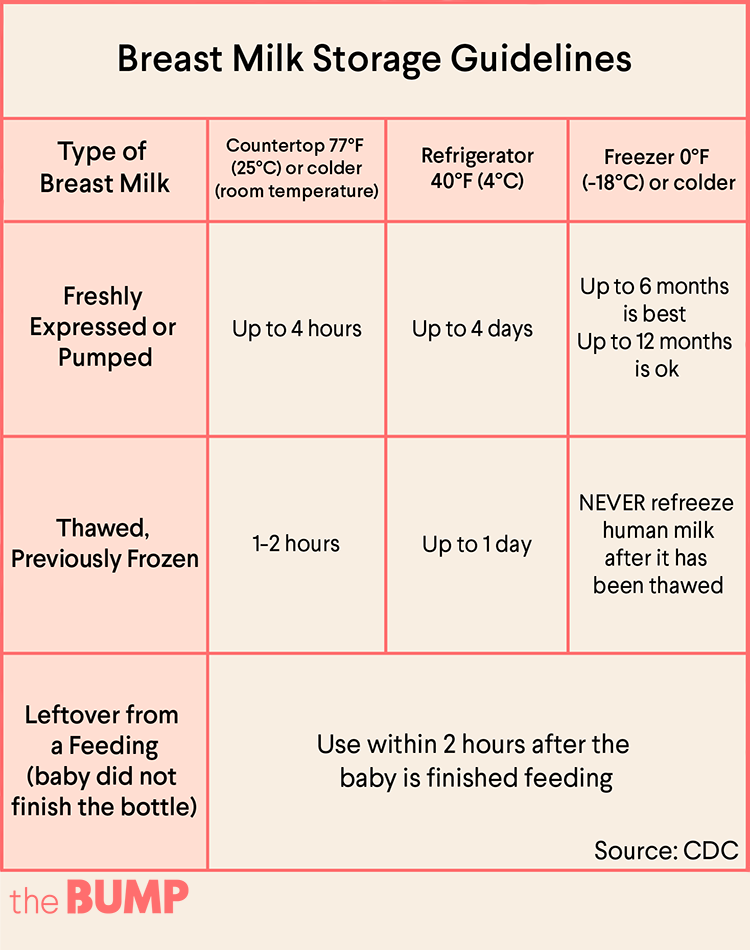
In order not to lose the amount of milk produced when the body is still weakened by the disease, it is best to use the Swing Maxi Flex ** double breast pump, which helps to stimulate lactation, increase the amount of milk (by 18% on average) and increase its fat content (+1% ) 14 .
However, breastfeeding and pumping when sick can be very tiring. You need to take care of yourself so that you can take care of the baby. Try to drink more fluids, eat when you can, and get plenty of rest. Crawl under the covers for a few days and ask family or friends to help care for your baby if possible, so you can put all your energy into recovery. nine0003
“Don't worry about your milk supply, it will last. Most importantly, do not stop breastfeeding abruptly so that mastitis does not develop, ”adds Sarah.
Proper hygiene is very important to reduce the risk of spreading the disease. Wash your hands with soap and water before and after breastfeeding and pumping, preparing and eating food, using the toilet and changing diapers. Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose. nine0003
Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose. nine0003
Can I take medication while breastfeeding?
In agreement with the attending physician and compliance with the dosage, certain medications are allowed. 9.10
.
“When talking to a doctor or pharmacist for any reason, always state that you are breastfeeding,” she continues. nine0003
What about long-term treatment?
If you are on long-term treatment for diabetes, asthma, depression, or other chronic conditions, the benefits of breastfeeding may outweigh the risks. “Breastfeeding is often possible for almost any disease, with the exception of some very rare conditions,” Sarah says, “you will be very familiar with the drugs you are taking, and during pregnancy you can discuss them with your doctor or other specialist. There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor. nine0003
There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor. nine0003
“I was on high doses of epilepsy medication, but I was still able to breastfeed,” recalls Nicola, a mother from the UK. “I saw a neurologist to ensure my son was safe and to minimize the risk of a seizure. Seizures can happen due to lack of sleep, and I fed day and night, but I took good care of myself, and my husband supported me. It was a positive experience."
What if I have to go to the hospital?
If you need to be hospitalized or urgently hospitalized, there are different ways to continue feeding your baby healthy breast milk so that you can return to normal breastfeeding after you are discharged. nine0003
“Express and freeze breast milk so that the caregiver can feed the baby. Practice at home ahead of time and be sure to let your doctors know that you are a breastfeeding mother, both before entering the hospital and while in it, ”recommends Sarah.
“If the baby is very small, you may be allowed to take him with you. Find out if the hospital has a supervising doctor or lactation consultant to contact. This specialist will support you, especially if you are in a general ward. If hospitalization is urgent, warn the doctors that you have a baby so that they take this into account. nine0003
Surgery under local or general anesthesia does not necessarily mean that breastfeeding will have to be stopped, or milk will need to be pumped and discarded. By the time you recover from surgery and can hold your baby, the amount of anesthetic in your breast milk will be minimal, so breastfeeding will be safe in most cases. 10 However, it is always best to consult your doctor or attending physician beforehand. nine0003
To ensure that the situation of treatment or departure does not affect the baby's diet, it is advisable to create a breast milk bank. This should be done daily by expressing one extra serving and freezing it in the handy, durable Medela Breast Milk Storage Bags. Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
For hygienic and easy pumping, use a breast pump with 2-Phase Expression technology for a fast, full flow of milk. For example, the ultra-comfortable Swing Flex** breastpump that adapts to the shape of your breasts and allows you to pump milk in a comfortable position, even lying back on the pillows 15 .
Don't forget to sterilize your breast pump with the Quick Clean microwave bags. Medela milk storage bags do not need to be handled as they are aseptically packaged and ready to use immediately.
Are there times when breastfeeding is not allowed?
In some cases, for the safety of the baby, breastfeeding should be stopped for a while, and instead, milk should be expressed and discarded to maintain milk production until the end of treatment. This includes radiotherapy and chemotherapy for cancer, herpes sores on the chest, and infections such as tuberculosis, measles, or blood poisoning that can be transmitted through breast milk. nine0009 11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
nine0009 11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
For quality lactation support during this period, you can use the dual electronic breast pump with innovative Flex technology or rent a Symphony Clinical Breast Pump** if possible. A list of cities where you can rent a breast pump can be found on the "Rent a Medela Clinical Breast Pump" page. nine0003
Literature
1 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet . 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
2 Lönnerdal B. Bioactive proteins in breast milk. J Pediatric Child Health. nine0120 2013;49 Suppl 1:1-7. - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Australian Breastfeeding Association [Internet]. Topical treatment with breastmilk: randomized trials. [ cited 2018 Apr 4]. Available from https://www.breastfeeding.asn.au - Australian Breastfeeding Association [Internet]. "Topical treatment with breast milk: a randomized trial". [cited 4 April 2018] See article at https://www.breastfeeding.asn.au
4 Ho JCS et al. HAMLET–A protein-lipid complex with broad tumoricidal activity. Biochem Biophys Res Commun. 2017;482(3):454-458. - Ho J.S.S. et al., "HAMLET - a protein-lipid complex with extensive antitumor activity". Biochem Biophys Res Comm. 2017;482(3):454-458. nine0120
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Hassiotou F, Hartmann PE. At the dawn of a new discovery: the potential of breast milk stem cells . Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv. 2014;5(6):770-778.
7 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child. 2010;95(12):1004-1008.
" Arch Dis Child. 2010;95(12):1004-1008.
8 Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol . 1998;81(6):523-533. — Hanson, L.A., "Breastfeeding provides passive and likely long-term active protection against disease." Ann Allergy Asthma Immunol. 1998;81(6):523-533.
9 Hale TW, Rowe HE. Medications and Mothers' Milk 2017. 17th ed. New York, USA: Springer Publishing Company; 2017. 1095 p . — Hale T.W., Rowe H.I., Medications and Breast Milk 2017. 17th edition. New York, USA: Publishing House Springer Publishing Company ; 2017. p. 1095.
10 Reece-Stremtan S et al. ABM Clinical Protocol# 15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017.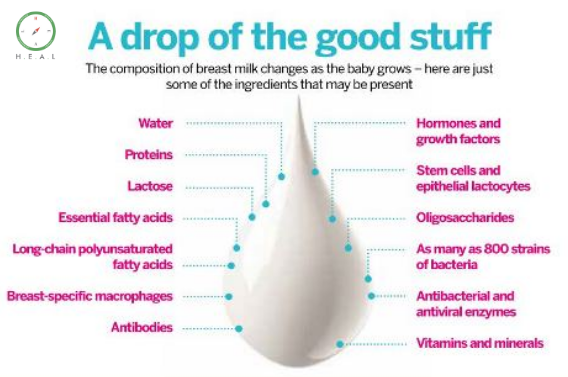 Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). nine0120 2017;12(9):500-506.
Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). nine0120 2017;12(9):500-506.
11 Lamounier JA et al. Recommendations for breastfeeding during maternal infections. J Pediatr 2004;80(5 Suppl ):181-188. - Lamunier J.A. et al., Guidelines for Breastfeeding during Maternal Infectious Diseases. J Pediatrician (Journal of Pediatrics) (Rio J). 2004;80(5 Suppl):181-188. nine0120
12 Hema M et al., Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledge. Indian J Med Res . 2014;140(1):32-39. - Hema M. et al., "Working with the Infant Born to a Mother with Tuberculosis: Current Recommendations and Gaps". Indian W Med Res. 2014;140(1):32-39.
Indian W Med Res. 2014;140(1):32-39.
13 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am JClin Nutr. 2003;77(6):1537S-1543S. Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7
14 Prime et al., Simultaneous Breast Expression in Breastfeeding Women Is More Efficacious Than Sequential Breast Expression, Breastfeed Med. Dec 2012; 7(6): 442–447. Prime DK and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447. nine0120
15 ClinicalTrials.gov [Internet]. Bethesda MD: National Library of Medicine, USA, data on file: NCT03091985. Clinical Research.gov [Internet]. Bethesda MD: National Library of Medicine, USA, data on file: NCT03091985.
Check out the instructions, consult with a specialist
* Ru FSZ 2010/07353 dated 07/19/10
** RU No. FCZ 2010/06525 dated 17/03/2021
FCZ 2010/06525 dated 17/03/2021
9000 9000 9000 9000 9000
000 Use and safety Acyclovir for pregnant and lactating women: can it be taken during pregnancy and breastfeeding
Can acyclovir be used during pregnancy to treat herpes and possible risks to the fetus
Acyclovir belongs to a class of antiviral drugs called synthetic nucleoside analogues. It works by stopping the spread of the herpes virus in the body. Used to reduce pain and speed up the healing of sores or blisters in people with chickenpox (chickenpox), shingles, a rash that can occur in people who have had chickenpox in the past, and outbreaks of genital herpes (occasionally causes ulcers around genitals and rectum). nine0003
In a study by the Centers for Disease Control and Prevention (CDC), aciclovir was found to cross the placenta, but teratogenicity (birth defects) was not observed, but there is still insufficient data to assess the risk of less common defects or to obtain reliable or final conclusions regarding the safety of this drug during pregnancy.
According to research by the Food and Drug Administration (FDA), it was noted that women taking acyclovir for the treatment of herpes simplex, even during the first trimester of pregnancy, did not demonstrate a risk to the fetus. nine0003
The Australian Medicines Administration (AU TGA) has studied a limited number of pregnant women and women of childbearing age who have taken oral acyclovir and found that it did not increase the incidence of malformations or other direct or indirect harmful effects on the mother's fetus. Animal studies have shown an increased incidence of fetal injury, the significance of which in humans is uncertain.
The American College of Obstetricians and Gynecologists (ACOG) recommends taking aciclovir for the treatment of genital herpes, especially recurrent ones, from the 36th week of pregnancy to avoid infection of the newborn baby. But since, as a result of not multiple studies, little information has been provided about it, it is advised to use it with extreme caution, strictly according to the doctor's prescription in the exact minimum dosage indicated as soon as possible. nine0003
nine0003
Information was also provided to ACOG that suppressive therapy in late pregnancy reduces the rate of caesarean section in women with recurrent genital herpes by reducing the rate of relapse during pregnancy, but such treatment may not protect against transmission of the viral infection to the newborn in all cases .
The Centers for Disease Control and Prevention (CDC) in 2015 concluded that this drug can be used to treat herpetic lesions in women at all stages of pregnancy, but under the strict supervision of a doctor, following all his prescriptions for prescribed doses, frequency and duration of administration, as well as in case of the most urgent need and, as a rule, the benefit to the mother should exceed the risk to the fetus. nine0003
Breastfeeding use of acyclovir and exposure to infants
Food and Drug Administration (FDA) studies of the use of acyclovir in women during breastfeeding found that it passes into breast milk, but even at the most At high maternal doses, the concentration of acyclovir in milk is only about 1% of the typical pediatric dose and is not expected to cause any side effects in breastfed infants. Local application of acyclovir to small areas of the mother's body away from the breast does not pose a risk to the infant. nine0003
Local application of acyclovir to small areas of the mother's body away from the breast does not pose a risk to the infant. nine0003
As a result of maternal herpesvirus infection of the infant during pregnancy, newborns are given aciclovir at doses of 20 to 30 mg/kg IV daily according to the CDC. Dosages obtained in breast milk at high maternal doses are only about 3-5% of this dose. Because the infant receives oral doses of breast milk and aciclovir is only about 20% orally bioavailable, the systemic dose received by the nursing infant is 1% or less of the typical pediatric dose, resulting in no reported adverse reactions in infants. nine0003
Several cases of oral aciclovir in breastfeeding mothers have also been reported to the CDC and FDA:
-
The mother of a 4-month-old infant did not notice any side effects in her breastfed infant when she took aciclovir 800 mg orally 5 times a day;
- 90,002 women who were 6 weeks postpartum received acyclovir 300 mg (5 mg/kg) intravenously three times a day for 5 days.