Blood in the placenta during pregnancy
Placental Abruption | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is placental abruption?
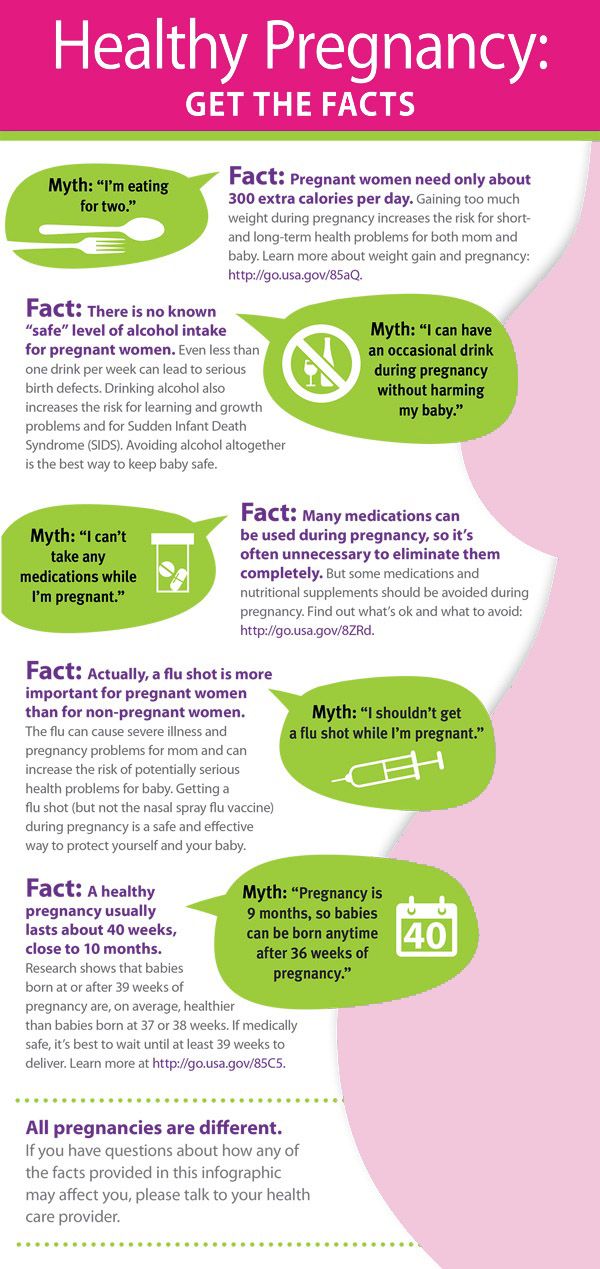
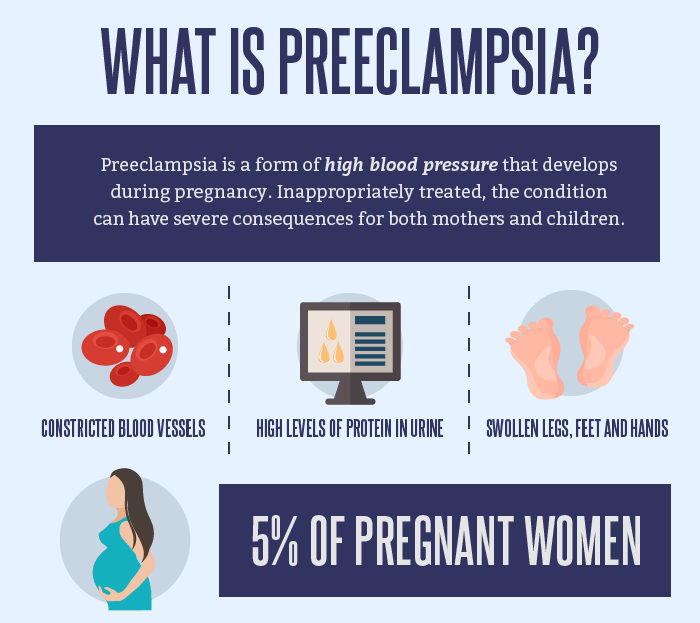
Bleeding can happen at any time during pregnancy. Placental abruption can cause bleeding late in pregnancy. This means after about 20 weeks.
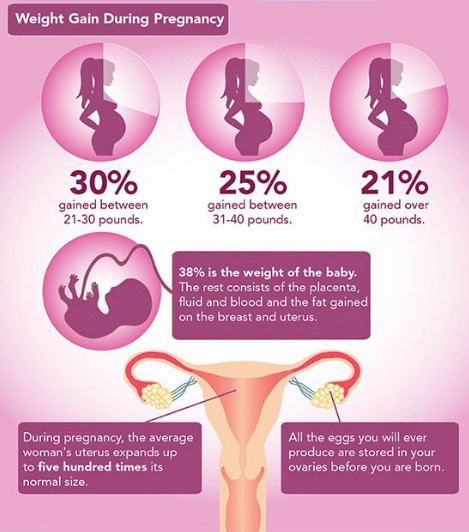
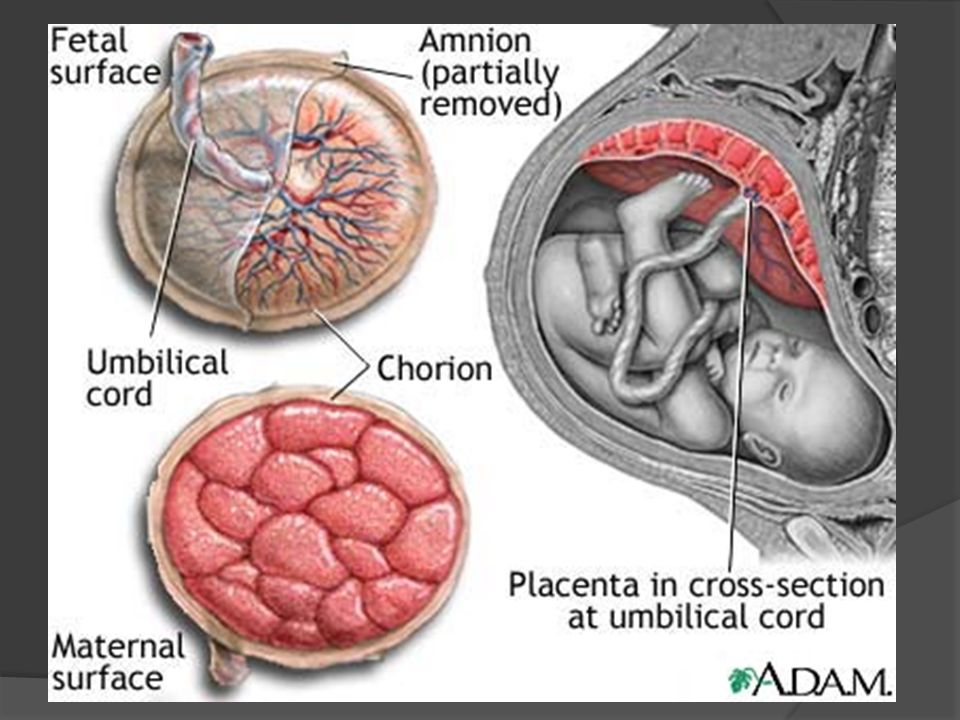
Placental abruption is when the placenta pulls away from where it's attached to the uterus. The placenta has many blood vessels that bring the nutrients from the mother to the developing baby. If the placenta starts to pull away during pregnancy, these blood vessels bleed. The larger the area that pulls away, the greater the amount of bleeding.
What causes placental abruption?
A direct blow to the uterus can cause placental abruption. For instance, this could happen during a car crash. Healthcare providers don’t know what causes it in other cases. You may be at higher risk if:
- You had a placental abruption with a previous pregnancy
- Your water breaks before 37 weeks of pregnancy (called preterm premature rupture of membranes or PPROM)
- You have high blood pressure
- You smoke cigarettes
- You're pregnant with twins or more (multiple pregnancy)
- You have sickle cell anemia, a disorder with abnormally shaped red blood cells
What are the symptoms of placental abruption?
The most common symptom of placental abruption is painful, dark red bleeding from the vagina. It happens during the third trimester of pregnancy. It also can occur during labor. Some women may not have vaginal bleeding that can be seen, but there may be bleeding inside the uterus.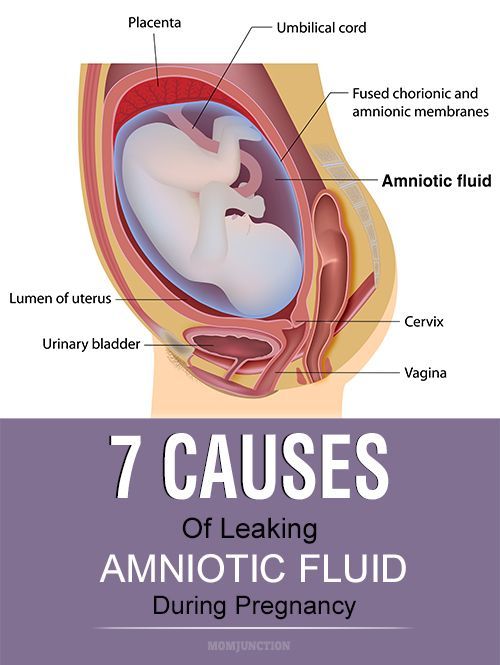 Symptoms of placental abruption may include:
Symptoms of placental abruption may include:
- Vaginal bleeding
- Pain in the belly (abdomen)
- Back pain
- Labor pains (uterine contractions) that don't relax
- Blood in the bag of water (amniotic fluid)
- Feeling faint
- Not feeling the baby move as much as before
These symptoms may be caused by other health conditions. Always see your healthcare provider for a diagnosis.
How is placental abruption diagnosed?
Your healthcare provider can diagnose placental abruption based on your symptoms. These include the amount of bleeding and pain. You will likely need an ultrasound. This test will show where the bleeding is. The provider will also check on your developing baby.
There are 3 grades of placental abruption:
- Grade 1.
 Small amount of vaginal bleeding and some uterine contractions. But no signs of fetal distress or low blood pressure in the mother.
Small amount of vaginal bleeding and some uterine contractions. But no signs of fetal distress or low blood pressure in the mother. - Grade 2. Mild to medium amount of bleeding and uterine contractions. The baby's heart rate may show signs of distress.
- Grade 3.Medium to severe bleeding or hidden bleeding. Also uterine contractions that don't relax, belly pain, low blood pressure, and the death of the baby.
Sometimes placental abruption isn't found until after delivery, when an area of clotted blood is found behind the placenta.
How is placental abruption treated?
There is no treatment to stop placental abruption or reattach the placenta.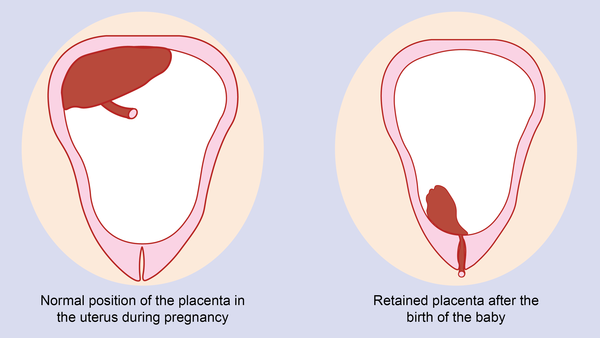 Your care depends on how much bleeding you have, how far along your pregnancy is, and how healthy your developing baby is. You may be able to have a vaginal delivery. Or you may need a cesarean section delivery if you have severe bleeding or if you or your baby are in danger. You may need a blood transfusion if you lose a lot of blood.
Your care depends on how much bleeding you have, how far along your pregnancy is, and how healthy your developing baby is. You may be able to have a vaginal delivery. Or you may need a cesarean section delivery if you have severe bleeding or if you or your baby are in danger. You may need a blood transfusion if you lose a lot of blood.
What are possible complications of placental abruption?
Placental abruption is dangerous because of the risk of uncontrolled bleeding (hemorrhage). This can mean less oxygen and nutrients going to the developing baby. Severe placental abruption is rare. Other complications may include:
- Uncontrolled bleeding (hemorrhage) and shock
- Disseminated intravascular coagulation (DIC). This is a serious blood clotting problem.
- Poor blood flow and damage to kidneys or brain
- The baby dies in the uterus (stillbirth)
When should I call my healthcare provider?
Call your healthcare provider about any bleeding you have while pregnant. Bleeding during pregnancy may not be serious. If the bleeding is medium to severe, or you have pain, contact your healthcare provider right away.
Bleeding during pregnancy may not be serious. If the bleeding is medium to severe, or you have pain, contact your healthcare provider right away.
Key points about placental abruption
- Placental abruption causes bleeding when the placenta starts to pull away too early from the uterus.
- This condition is often painful.
- If you have placental abruption, you may need to deliver your baby early and may need a cesarean section delivery.
- Report any bleeding in pregnancy to your healthcare provider.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Medical Reviewer: Irina Burd MD PhD
Medical Reviewer: Donna Freeborn PhD CNM FNP
Medical Reviewer: Heather M Trevino BSN RNC
© 2000-2022 The StayWell Company, LLC.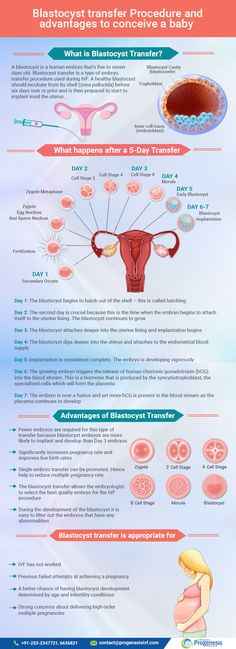 All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Symptoms, Causes & Effects On Baby
Overview
What is a placental abruption?
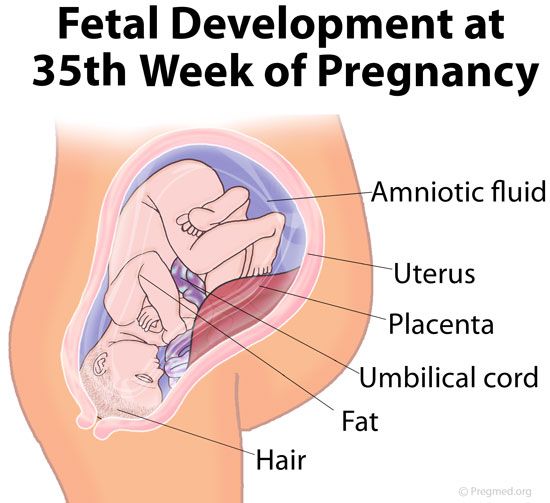
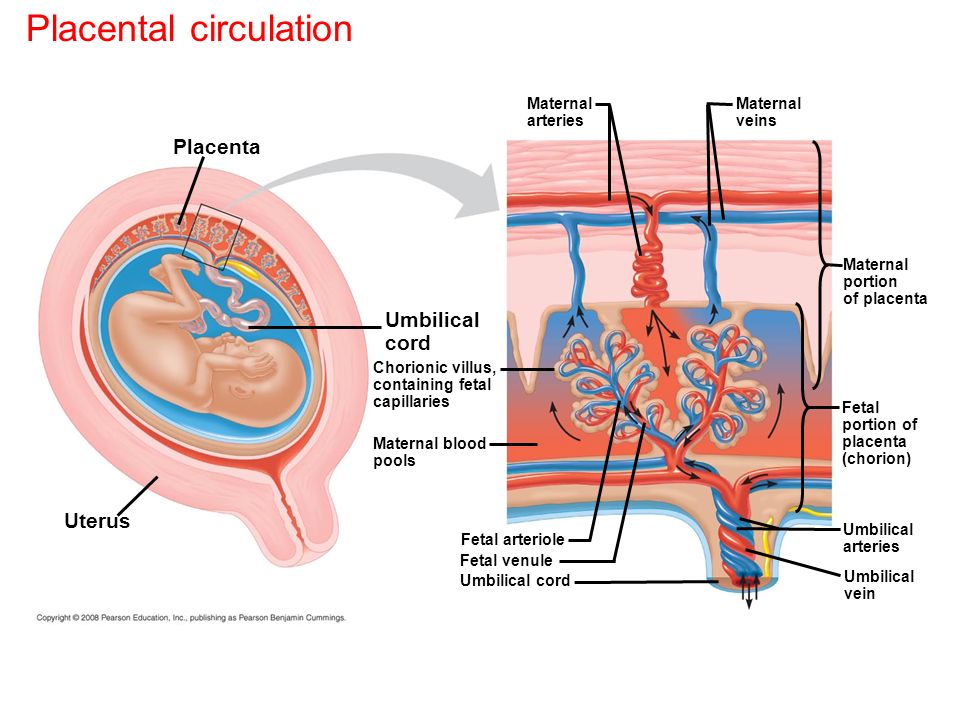
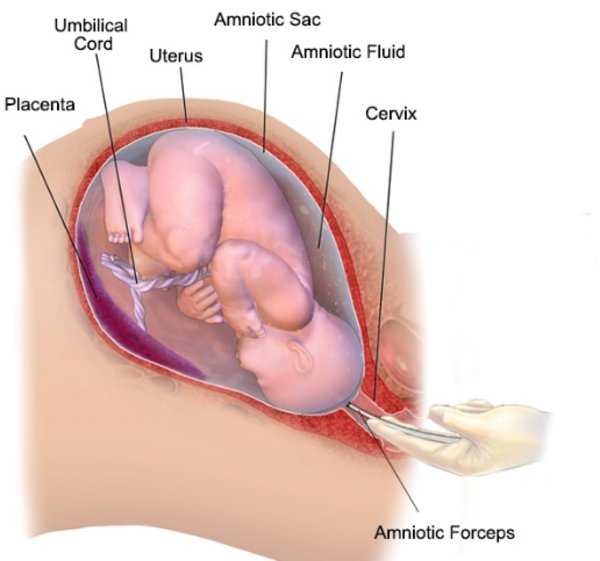
Placental abruption is a complication of pregnancy that happens when the placenta separates from your uterus before delivery. The placenta is a temporary organ that connects a growing fetus to your uterus during pregnancy. It attaches to the wall of your uterus, usually on the top or side and acts as a lifeline that gives nutrients and oxygen to the fetus through the umbilical cord. The placenta also removes waste from the fetus's blood.
In placental abruption, the placenta may completely detach or partially detach. This can decrease the amount of oxygen and nutrients to the fetus and cause heavy bleeding in the birthing parent. Placental abruption is a serious condition that requires medical treatment.
What are the different types of placental abruption?
- A partial placental abruption occurs when the placenta does not completely detach from the uterine wall.
- A complete or total placental abruption occurs when the placenta completely detaches from the uterine wall. There is usually more vaginal bleeding associated with this type of abruption.
- Revealed placental abruptions have moderate to severe vaginal bleeding that you can see.
- Concealed placental abruptions have little or no visible vaginal bleeding. Blood is trapped between the placenta and uterine wall.
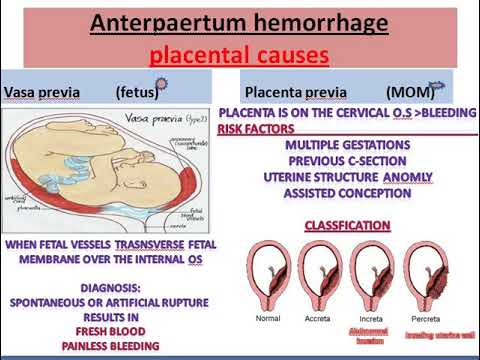
What is the difference between placental abruption and placenta previa?
In placenta previa, the placenta is covering all or part of the birthing parent's cervix. It's also called low-lying placenta. Think of it as an obstacle that’s blocking the exit from the uterus. Even though the placenta is in a complicated position, it’s still attached to the uterus. When the placenta detaches from the uterus, this is a placental abruption. Both conditions can cause vaginal bleeding during pregnancy and labor.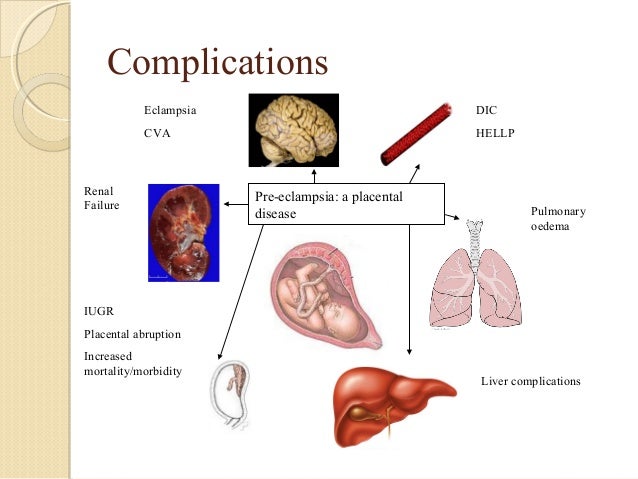
How common is a placental abruption?
About 1 out of 100 pregnancies has placental abruption. This condition is usually seen in the third trimester, but it can happen any time after 20 weeks of pregnancy up until delivery.
What are the effects of placental abruption?
Placental abruption can be life-threatening to the fetus and sometimes to you. Complications from a placental abruption include:
For baby:
- Premature birth.
- Low birth weight.
- Growth problems.
- Brain injury from lack of oxygen.
- Stillbirth.
For birthing parent:
- Blood loss.
- Blood clotting issues.
- Blood transfusion.
- Hemorrhage.
- Kidney failure.
Symptoms and Causes
What causes placental abruption?
The cause of placental abruption is often unknown. Certain lifestyle choices or abdominal trauma can increase your risk for placental abruption.
What are the risk factors for placental abruption?
You are at higher risk for placental abruptions if you have any of the following:
- Trauma or injury to your uterus (like a car accident, fall or blow to the stomach).
- Previous placental abruption.
- Multiple gestations (twins or triplets).
- High blood pressure (hypertension), gestational diabetes or preeclampsia.
- If you smoke or have a history of drug use.
- Short umbilical cord.
- Maternal age 35 or greater.
- Uterine fibroids.
- Thrombophilia (a blood clotting disorder).
- Premature rupture of membranes (the water breaks before the fetus is full term).
- Rapid loss of the amniotic fluid.
What are the signs and symptoms of placental abruption?
Each person can have different symptoms of placental abruption. However, the most common symptom is vaginal bleeding with cramping during the third trimester of pregnancy. Symptoms or signs can also include:
- Abdominal pain.
- Uterine contractions that are longer and more intense than average labor contractions.
- Uterine tenderness.
- Backache or back pain.
- Decreased fetal movement.
Vaginal bleeding can vary and is not an indication of how much the placenta has separated. In some instances, there could be no visible bleeding because the blood is trapped between the placenta and the uterine wall. Pain can range from mild cramping to strong contractions and often begins suddenly.
These symptoms can resemble other pregnancy conditions. Always consult with your healthcare provider for a diagnosis.
Do you always bleed during a placental abruption?
Most of the time, you will see some blood during a placental abruption. In the event of a concealed abruption, the blood will be behind the placenta. In that case, there will be no bleeding. In other cases, the abruption develops slowly, which can cause occasional, light bleeding.
Talk to your healthcare provider about any vaginal bleeding you experience during your pregnancy.
What does placental abruption feel like?
You may experience sudden or sharp pain, cramping, or tenderness in your lower pelvic region or back during a placental abruption.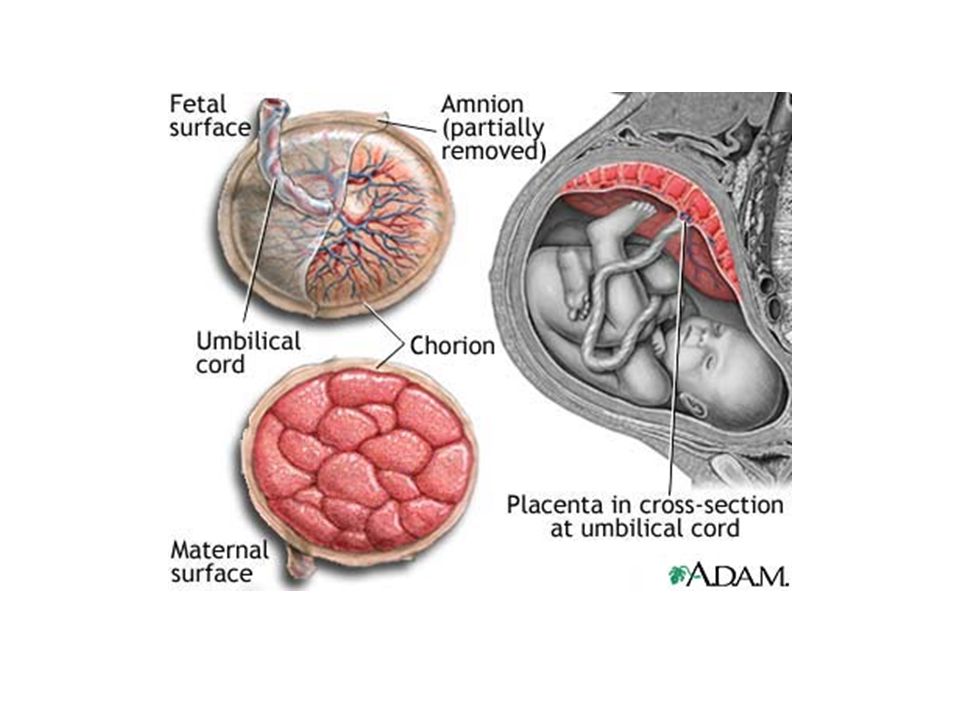 You could also feel less movement from the fetus. You should discuss these symptoms with your healthcare provider immediately.
You could also feel less movement from the fetus. You should discuss these symptoms with your healthcare provider immediately.
What are the first signs of a placental abruption?
The most common symptom of a placental abruption is vaginal bleeding, although you will not always bleed. You may also have sudden, ongoing pain in your abdomen or back.
Diagnosis and Tests
How is a placental abruption diagnosed?
Placental abruption is diagnosed through an exam and monitoring. You may be admitted to the hospital depending on the severity of the abruption or you may be able to rest at home. Your healthcare provider will:
- Ask how much bleeding has occurred.
- Ask where you feel pain and how intense the pain is.
- Ask when symptoms started.
- Monitor your blood pressure.
- Monitor the fetal heart rate and movement.
- Monitor your contractions.
- Use ultrasound to locate the bleeding and to check the fetus.
- Recommend blood or urine tests.
There are typically three grades of placental abruption a healthcare provider will diagnose:
- Grade 1: Small amount of bleeding, some uterine contractions, and no signs of stress to you or the fetus.
- Grade 2: Mild to moderate amount of bleeding, some uterine contractions, and signs of fetal stress.
- Grade 3: Moderate to severe bleeding or concealed bleeding, uterine contractions that do not relax, abdominal pain, low blood pressure, and fetal death.
It is important to discuss any symptoms or changes in symptoms with your healthcare provider.
Management and Treatment
How is a placental abruption treated?
Once the placenta has separated from the uterus, it cannot be reconnected or repaired. A healthcare provider will recommend treatment based on:
- The severity of the abruption.
- How long the pregnancy is/gestational age of the fetus.
- Signs of distress from the fetus.
- Amount of blood you've lost.
Generally, the severity of the abruption and gestational age of the fetus are the two most important factors:
If the fetus isn't close to full term:
- If it's too soon for your baby to be born and your abruption is mild, you will be closely monitored until you reach 34 weeks of pregnancy. If the fetal heart rate is normal and you're not bleeding, your healthcare provider may allow you to go home to rest. They may give you medication to help with fetal lung development.
- If your abruption is severe and the health of you or the fetus are at risk, immediate delivery may be necessary.
If the fetus is near full term:
- If your abruption is mild and the fetal heart rate is stable, a closely monitored vaginal delivery is possible. This is generally determined around 34 weeks of pregnancy.
- If the abruption gets worse or you or the fetus are in danger at any time, the baby will be delivered via emergency Cesarean section.

Prevention
Can I prevent a placental abruption?
Placental abruptions are typically unpreventable. You can reduce your risk by:
- Not smoking or using drugs.
- Keeping your blood pressure at a healthy level.
- Managing diabetes.
- Taking health and safety precautions like wearing a seat belt.
- Reporting any abdominal trauma to your healthcare provider.
- Talking to your healthcare provider about any vaginal bleeding.
Outlook / Prognosis
What can I expect if I have a placental abruption?
This can vary depending on the severity of your symptoms and how far along you are in your pregnancy. You can expect to be monitored closely and often. Watch for any changes in symptoms and discuss them with your healthcare provider immediately.
What is my baby’s survival rate after a placental abruption?
The two factors that affect survival rate are gestational age at birth and the severity of the abruption.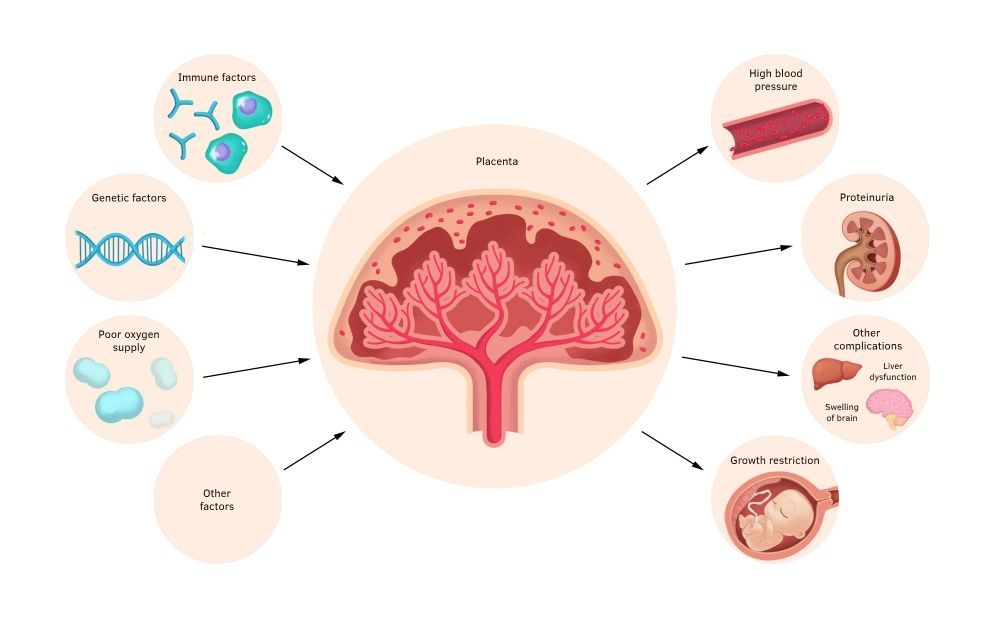 Early detection, close monitoring, and quick treatment can help reduce complications.
Early detection, close monitoring, and quick treatment can help reduce complications.
Can I have another placental abruption?
You have about a 15% chance of having another abruption in a future pregnancy. With two prior abruptions, this chance increases to about 25%. If you have had a previous abruption, please let your healthcare provider know.
What are questions I should ask my healthcare provider?
Your healthcare provider should be able to answer your questions and prepare you for treatment of placental abruption. Here are some questions you might ask:
- Is my baby’s life in danger? Is mine?
- What are my treatment options?
- Can I give birth now?
- How will I know if my abruption is worsening?
- What are potential complications?
- Do I need additional tests?
Frequently Asked Questions
Can sex cause a placental abruption?
Sexual intercourse is not a direct cause of placental abruption.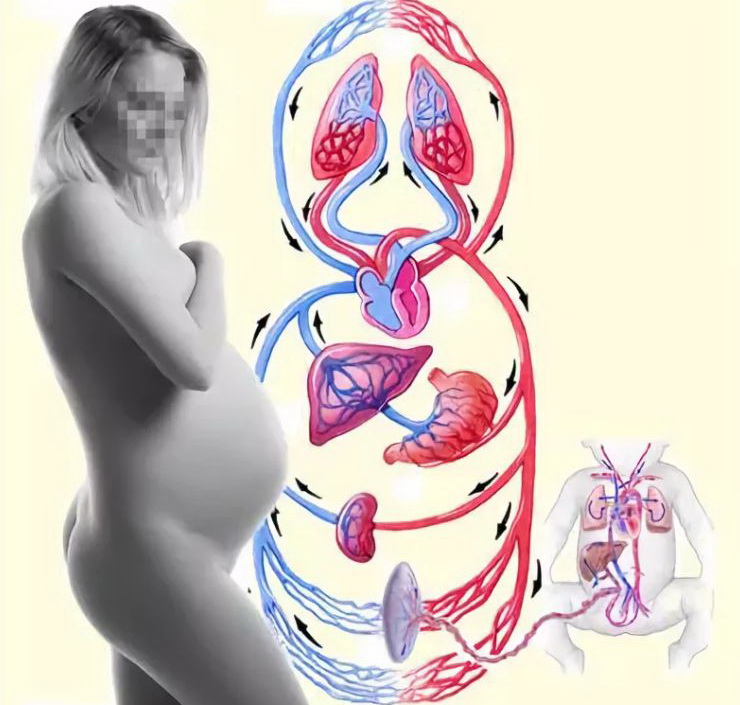 In most cases, it’s perfectly safe to have sex during pregnancy. Activities with a high risk of falling or abdominal trauma should be avoided during pregnancy.
In most cases, it’s perfectly safe to have sex during pregnancy. Activities with a high risk of falling or abdominal trauma should be avoided during pregnancy.
Can sneezing cause a placental abruption?
Sneezing is a normal thing your body does and is not a cause for placental abruption. It can't harm the fetus in any way. If you have any concerns about frequent and forceful sneezing or coughing, reach out to your healthcare provider for guidance.
Can smoking cause a placental abruption?
Smoking can increase your risk of many complications during pregnancy, including placental abruption. Ask your healthcare provider about ways to quit smoking.
When do I call my healthcare provider if I suspect a placental abruption?
Call your healthcare provider immediately if are bleeding, cramping or experience pelvic pain during your pregnancy, especially in the third trimester.
A note from Cleveland Clinic
Placental abruption is an uncommon, yet serious condition people can experience during pregnancy. Talk to your healthcare provider if you experience vaginal bleeding, pelvic pain or cramping. Placental abruption should be diagnosed and treated promptly to ensure you and your baby are healthy.
Talk to your healthcare provider if you experience vaginal bleeding, pelvic pain or cramping. Placental abruption should be diagnosed and treated promptly to ensure you and your baby are healthy.
Premature placental abruption: what a future mother needs to know and how not to miss its signs | Blog
First, let's talk about what is the placenta?
The placenta is the embryonic organ that connects the body of mother and child. Its uniqueness lies in the fact that it is the only "disposable" organ. The placenta begins to develop from the 2nd week of pregnancy, forms up to 15-16 weeks and reaches full functional maturity by 36 weeks. And after the birth of the fetus (in the third stage of childbirth), it separates and leaves the mother's body, starting the process of lactation at the endocrinological level. nine0005
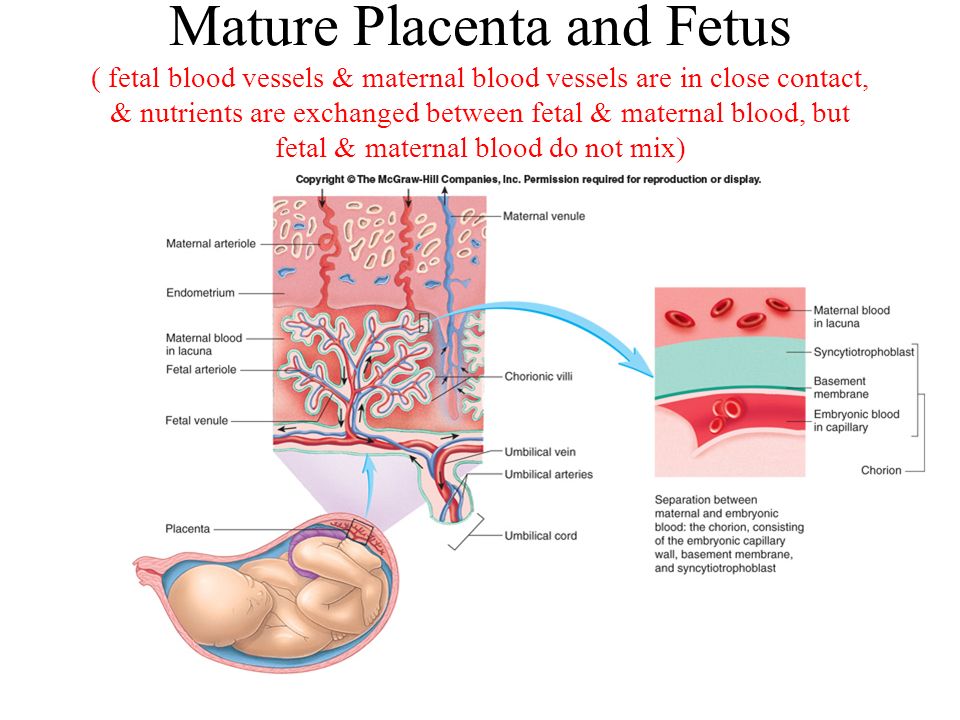
The placenta performs important functions such as gas exchange, nutrient exchange between the mother and the child, provides immunological protection and works as an endocrine gland, producing hormones necessary for the development of the fetus and the normal course of pregnancy. Every minute, about 500 ml of blood enters the placenta, but at the same time it is a kind of barrier that does not allow the blood of the mother and child to mix, and also prevents many toxic substances from entering the bloodstream of the baby. nine0005
Every minute, about 500 ml of blood enters the placenta, but at the same time it is a kind of barrier that does not allow the blood of the mother and child to mix, and also prevents many toxic substances from entering the bloodstream of the baby. nine0005
In this article we will talk about placental abruption.
This condition is quite rare (up to 1.5% of all pregnancies), but causes such threatening complications as massive bleeding and hemorrhagic shock, fetal distress, which in some cases can cause fetal death. Normally, the detachment of the placenta from the inner wall of the uterus occurs only after the birth of the fetus. If this happens before the onset of labor, as well as in the first or second stage of labor, this is the premature detachment of a normally located placenta. This condition is a very dangerous pathology that requires immediate diagnosis and decision of further medical tactics in the near future. nine0005
Causes of premature placental abruption
The only cause of premature placental abruption, unfortunately, has not been established to date.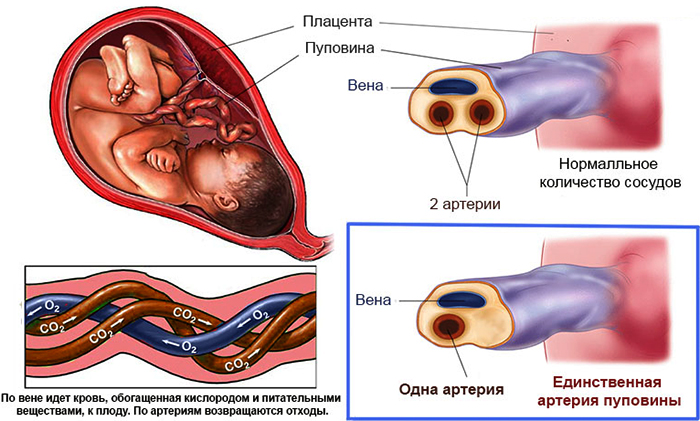 There are many theories, but in general, the occurrence of this condition is associated with many provoking factors.
There are many theories, but in general, the occurrence of this condition is associated with many provoking factors.
Major risk factors include:
- arterial hypertension,
- diabetes mellitus
- pregnant age over 40
- multiple pregnancy
- polyhydramnios
- postterm pregnancy and large fetus
- past uterine surgery
- blood clotting disorder,
- autoimmune diseases
- kidney disease
- bad habits such as smoking and drug use
- inflammatory diseases of the uterus and placenta, abnormal development of the uterus.
Causes that can provoke placental abruption: physical trauma of a pregnant woman (accident, fall, blow to the stomach), disruption of the contractile activity of the uterus, stress, gross obstetric manipulations. nine0005
Types of placental abruption
There are the following types of placental abruption: partial and complete.
Partial detachment, in turn, can be central and marginal.
Why is this classification so important? And because both the clinical picture and medical tactics depend on the place and volume of the detachment. Partial detachment can be progressive or non-progressive.
Non-progressive detachment has a significantly better prognosis for a pregnant woman, because in this case, conservative treatment is possible with preservation of pregnancy. nine0005
Symptoms of placental abruption:
Here is a triad of main symptoms that may be a sign of placental abruption:
- abdominal pain, feeling of increased uterine tone;
- bleeding from the genital tract;
- violation of the fetal heartbeat, indicating fetal distress.
Also, a woman can feel the baby's reaction to a decrease in the amount of oxygen supplied to him due to placental abruption - he begins to move more actively, reacting to hypoxia. nine0005
These symptoms do not always appear at the same time! For example, with marginal abruption of the placenta, blood flows into the vagina, which means that the woman sees signs of bleeding. With central detachment, a retroplacental hematoma is formed. Bleeding is internal, which means that a pregnant woman may not notice its signs. The appearance of an accelerated heartbeat in a woman, a decrease in blood pressure, nausea, dizziness, and severe weakness may indicate internal bleeding.
With central detachment, a retroplacental hematoma is formed. Bleeding is internal, which means that a pregnant woman may not notice its signs. The appearance of an accelerated heartbeat in a woman, a decrease in blood pressure, nausea, dizziness, and severe weakness may indicate internal bleeding.
However, with central placental abruption, blood accumulates in front of the placenta and begins to “press” on nearby tissues. As a result, a pronounced pain syndrome occurs.
It must be emphasized that if at least one of the symptoms appears, it is necessary to immediately inform the doctor about this! This condition can be very dangerous for you and your baby, so it is important to diagnose it in a timely manner.
Diagnosis of placental abruption
Diagnosis of placental abruption is based not only on clinical symptoms and gynecological examination. Ultrasound diagnostics is the main method that allows you to accurately assess the location and area of the exfoliated area of the placenta and see the presence or absence of a hematoma. Also, ultrasound can distinguish premature detachment from placenta previa (its abnormal location, in which it overlaps the internal pharynx of the cervix). This condition can have similar symptoms, as it is often accompanied by bleeding. The condition of the fetus and the degree of its hypoxia will be determined using cardiotocography, and Dopplerography, in turn, assesses violations of the uteroplacental circulation. Based on these examination results, the obstetrician-gynecologist, and more often a council of doctors, decides on the type of further medical tactics. nine0005
Also, ultrasound can distinguish premature detachment from placenta previa (its abnormal location, in which it overlaps the internal pharynx of the cervix). This condition can have similar symptoms, as it is often accompanied by bleeding. The condition of the fetus and the degree of its hypoxia will be determined using cardiotocography, and Dopplerography, in turn, assesses violations of the uteroplacental circulation. Based on these examination results, the obstetrician-gynecologist, and more often a council of doctors, decides on the type of further medical tactics. nine0005
Treatment of placental abruption
Treatment of placental abruption always requires hospitalization of the pregnant woman in the maternity hospital for constant monitoring of her condition. In cases of non-progressive mild placental abruption with a stable state of the mother and fetus, conservative tactics with drug therapy and preservation of pregnancy are possible. Progressive detachment, as well as severe detachment, certainly requires an emergency caesarean section. nine0005
nine0005
In case of complete detachment of the placenta, with the rapid progression of this condition, massive bleeding occurs, which threatens the life of both the pregnant woman and the child. In such a situation, surgeons always prioritize the life of a woman and do everything necessary to save her. Some cases may, unfortunately, require even such radical surgical tactics as removal of the uterus. However, at the current level of development of medicine, more and more technologies are emerging that, with timely assistance, can save not only the life of the mother and child, but also the reproductive functions of a woman. In particular, our obstetrician-gynecologists and anesthesiologists use up-to-date international medical protocols to ensure the safest possible delivery. Appropriate algorithms have also been developed for surgical interventions with a high risk of bleeding. Thanks to the latest technologies in vascular surgery with X-ray and ultrasound control, massive bleeding can be quickly and safely stopped. That is why we make sure that our maternity hospital always has the necessary amount of blood products and all the necessary modern equipment that may be needed in critical situations. nine0005
That is why we make sure that our maternity hospital always has the necessary amount of blood products and all the necessary modern equipment that may be needed in critical situations. nine0005
Quite often, expectant mothers ask about the prevention of such complications as placental abruption.
We advise you to adhere to the following recommendations:
- avoid stressful situations, excessive physical activity, factors that can lead to physical injury,
- do not smoke or use drugs
- control your blood pressure during pregnancy. nine0045
And of course, our patients who have certain chronic diseases require special attention. They need to undergo all the necessary examinations in a timely manner and adhere to the prescribed treatment and recommendations.
If you still have questions about this topic, please contact our specialists! Take care of yourself and be attentive to your well-being!
I wish your pregnancy to be a source of only positive emotions!
Save at all costs: reasons for abortion
January 17, 2017 Articles on gynecology
According to Wikipedia, 15-20% of clinically diagnosed pregnancies end in spontaneous abortion. These numbers are a lower estimate, as many miscarriages occur in the early stages, before the woman knows she is pregnant. After all, often the clinical signs of a miscarriage are mistaken for heavy periods or for their delay. nine0005
These numbers are a lower estimate, as many miscarriages occur in the early stages, before the woman knows she is pregnant. After all, often the clinical signs of a miscarriage are mistaken for heavy periods or for their delay. nine0005
What are the reasons for termination of pregnancy at different stages? How to prepare for pregnancy after a bad experience that ended in a miscarriage? These questions were answered by an obstetrician-gynecologist of the highest category at Bullfinch Medical Center ALEXANDER GIL.
- Alexander Vadimovich, most miscarriages happen at the beginning of pregnancy, and many women are perplexed: why could this happen?
- The main cause of miscarriages before 6 weeks is natural selection. There is a laying of pregnancy with congenital malformations of the embryo, which is no longer viable - thus, natural selection is carried out, in which we cannot interfere. nine0005
You will never know the exact cause of a miscarriage at this time, even if after abrasion (curettage of the uterine mucosa), the contents are sent for research.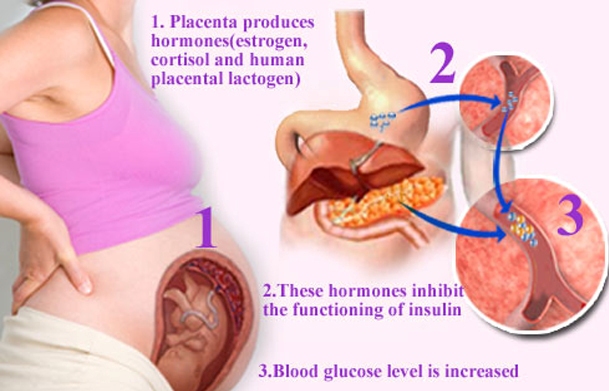 As a rule, the answer comes: “short-term pregnancy” and nothing more.
As a rule, the answer comes: “short-term pregnancy” and nothing more.
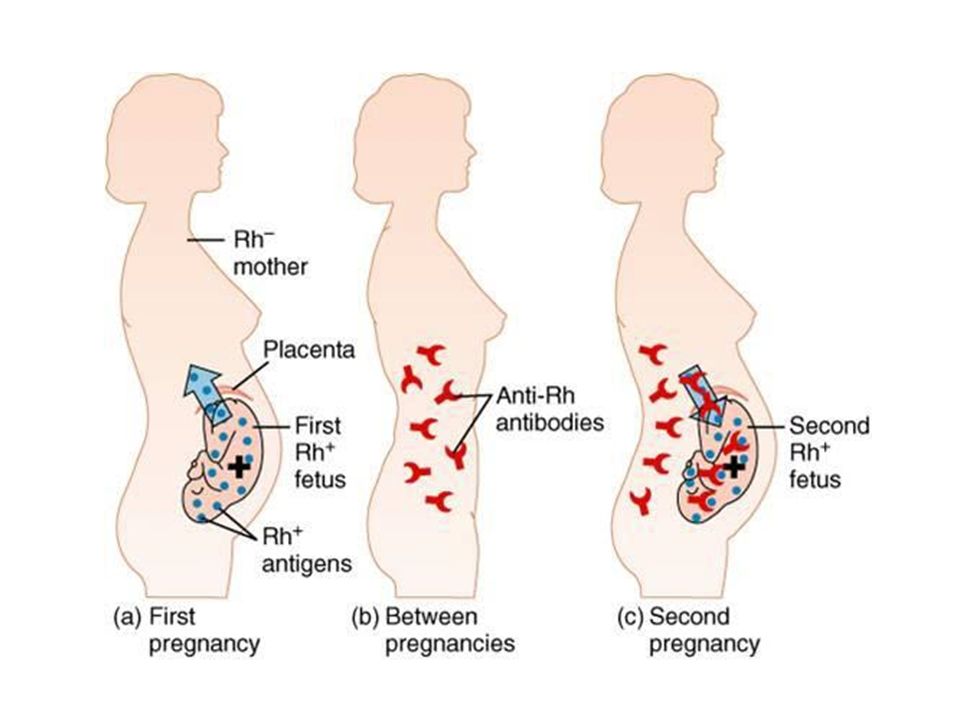
There is another reason for termination of pregnancy, especially if it is not the first one - Rh-conflict (when a woman has Rh-negative blood, and men - Rh-positive). But in our country, effective prevention of the Rh conflict is used, so that troubles can be avoided at the stage of pregnancy planning. nine0005
In the structure of early termination of pregnancy, no one excludes infections and problems associated with hormones. At a period of 6-8 weeks, promising pregnancies are often interrupted due to a lack of hormones. During normal pregnancy, a woman has a so-called corpus luteum in one of the ovaries, which produces endogenous progesterone.
Unfortunately, the functioning of the corpus luteum ends by about 7 weeks of pregnancy, and if initially there was not enough endogenous progesterone, the pregnancy stops developing: the fetal egg detaches and the so-called missed pregnancy occurs. nine0005
In some cases, with detachment of the fetal egg, pregnancy can be saved, the main thing is to contact a specialist in time.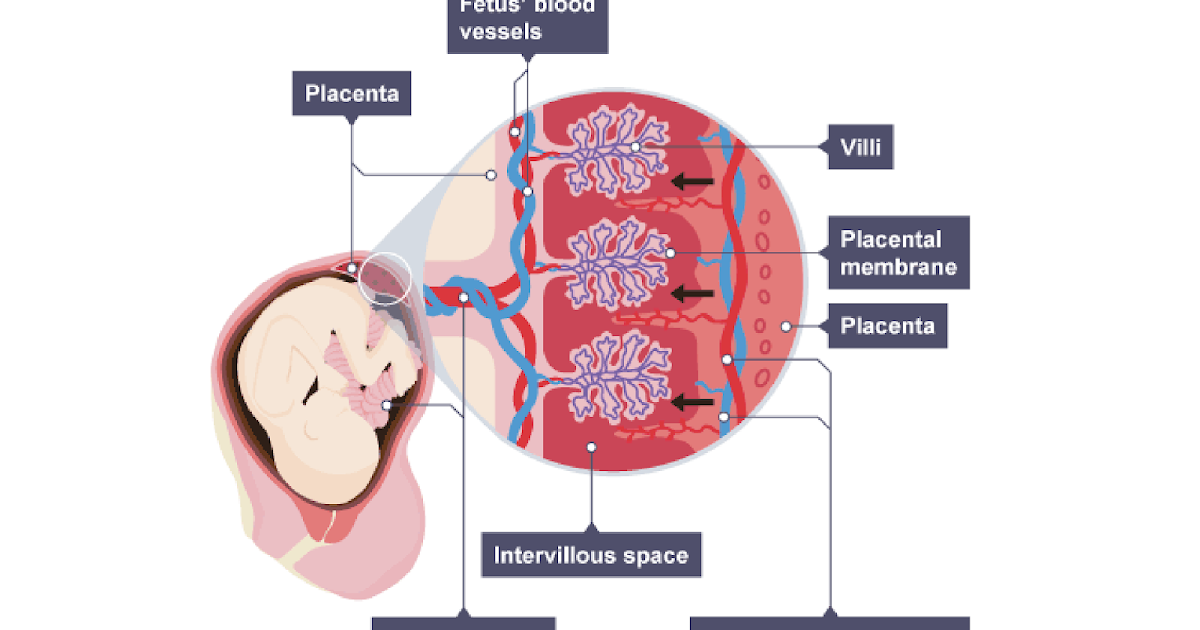 If, according to the results of ultrasound studies, the doctor sees that the embryo is still alive, pregnant women are prescribed exogenous progesterone in tablets or suppositories. This hormone also exists in the form of injections - it is used to saturate the body faster and prevent miscarriage.
If, according to the results of ultrasound studies, the doctor sees that the embryo is still alive, pregnant women are prescribed exogenous progesterone in tablets or suppositories. This hormone also exists in the form of injections - it is used to saturate the body faster and prevent miscarriage.
- Agree, when a woman becomes pregnant, she cannot suspect that she does not have enough progesterone in her body. What should be her concern? What signs indicate this? nine0005
- Any discharge from scanty dark brown to more profuse bloody is a bad sign. You should not hesitate to contact a gynecologist.
If spotting appears, an ultrasound examination, a blood test for progesterone is indicated.
I want to say that lack of progesterone can cause miscarriage up to 15 weeks. At 15-16 weeks, the placenta is finally formed, which will secrete (produce) this hormone. nine0005
nine0005
- Alexander Vadimovich, what problems can arise with the placenta during pregnancy?
- In the early stages, the chorion (unformed placenta) can block the internal os, maybe its marginal location - this is a big risk of abortion. In this case, the woman is admitted to the hospital and observed for up to 16 weeks - by this time, the chorion, as a rule, rises. But there remains a percentage of pregnant women in whom the placenta overlaps the cervix of the uterus - this is called the "central location of the placenta." To maintain pregnancy, such women, as a rule, must be in the clinic and under observation all the time. nine0005
— What is the treatment for infections that appear during pregnancy?
- Infections can occur even in women who were carefully examined before pregnancy. Often this problem occurs due to spotting - this is a favorable environment for the development of infections.
Ectopia (erosion) of the cervix is also an infection that is a clear threat to pregnancy.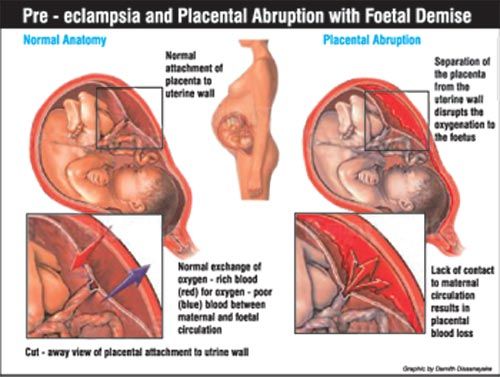 Therefore, it is so important to undergo a colposcopy before conception and be treated for ectopia, if it is detected. nine0005
Therefore, it is so important to undergo a colposcopy before conception and be treated for ectopia, if it is detected. nine0005
Infection by the ascending route can penetrate in utero and adversely affect the health of the fetus. There is such a complication as intrauterine fetal pneumonia, which is treated very poorly and occupies a large percentage in the structure of infant mortality.
And we treat infections whenever possible in any way that is prescribed in the protocol. There is such a tactic, which is to take antibiotics. There is no need to be afraid of them, as the doctor will prescribe only medicines approved for pregnant women. Sometimes you have to use those drugs, the benefits of which are greater than the risk of adverse reactions. nine0005
— What threats can affect a mid-term pregnancy?
— Among the many causes that lead to spontaneous miscarriages is isthmic-cervical insufficiency. This is a condition in which the isthmus and cervix cannot cope with the increasing load (growing fetus, amniotic fluid), begin to open - and the baby is born prematurely.
There are indications for the prevention of this condition - the imposition of a circular submucosal suture on the cervix. The best time is 16-17 weeks. You can do this procedure after 20 weeks, but the effect will be less. nine0005
In the middle of pregnancy, a placental abruption can occur in a woman. In some cases, pregnancy can be saved with the help of drugs that affect blood clotting. But often doctors are forced to resort to a small caesarean section. As a rule, childbirth before 22 weeks ends in the death of the fetus, and here we are already talking about saving the life of the mother.
I encourage pregnant women to refrain from flying. In my medical practice, there have been several cases where placental abruption in patients occurred during a flight. Who will provide you with qualified assistance in this case? I advise you not to take risks. nine0005
In Belarus, as in other European countries, labor begins at 22 weeks, but it is considered premature.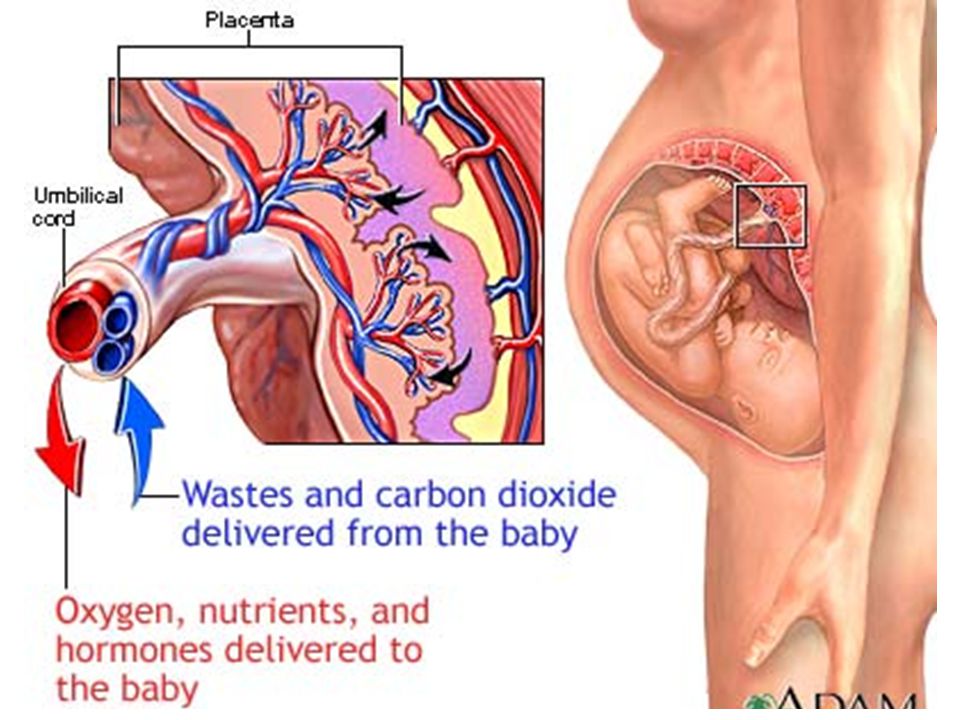 Doctors are doing everything possible to save a promising pregnancy by any means. The main thing is to always be under the supervision of a specialist and follow all his recommendations.
Doctors are doing everything possible to save a promising pregnancy by any means. The main thing is to always be under the supervision of a specialist and follow all his recommendations.
- Alexander Vadimovich, unauthorized termination of a desired pregnancy is always a great psychological trauma for a woman. No one wants to experience this again. What are the features of preparing for the next pregnancy after a miscarriage? nine0005
— Before thinking about a second pregnancy, it is advisable for women who experience mental anguish to undergo a course of psychotherapy. This is very important, because mental problems can be very serious, especially in women after unsuccessful in vitro fertilization (IVF).
The main rule: do not get pregnant after a miscarriage for 6 months. It is best to protect yourself at this time with oral contraceptives, which the doctor will prescribe. This is necessary in order to restore normal reproductive function. nine0005
A set of examinations for women who have had a miscarriage is ordered individually.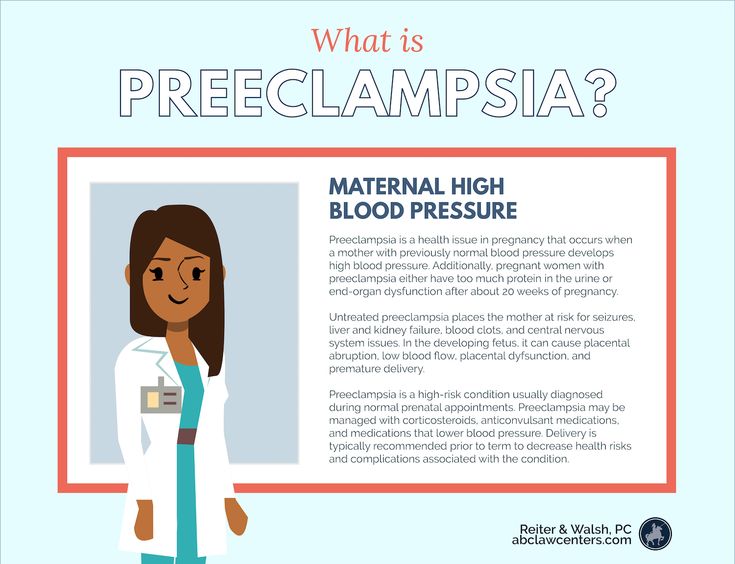 But the general recommendations are:
But the general recommendations are:
1. Diagnosis of sexually transmitted infections: mycoplasmosis, ureaplasmosis, chlamydia, herpes simplex virus, human papillomavirus (HPV).
You should also be screened for infections that may have caused a miscarriage in a previous pregnancy.
2. Test for sex hormones - if prescribed by a doctor.
3. Thyroid hormones (TSH, T4 free, ATPO), ultrasound of the thyroid gland, consultation with an endocrinologist. nine0177 4. If necessary, consultation of a therapist and other specialists, a blood test for sugar, syphilis, HIV.
5. Ultrasound of the abdomen and kidneys. During pregnancy, many chronic diseases are exacerbated, incl. and kidney disease. You need to be treated before conception.
6. Colposcopy (examination of the cervix under a microscope).
7. Partner semen analysis.
An examination by a geneticist is indicated if, when planning a pregnancy, a woman is 36 years old, and a man is 45 years old and over.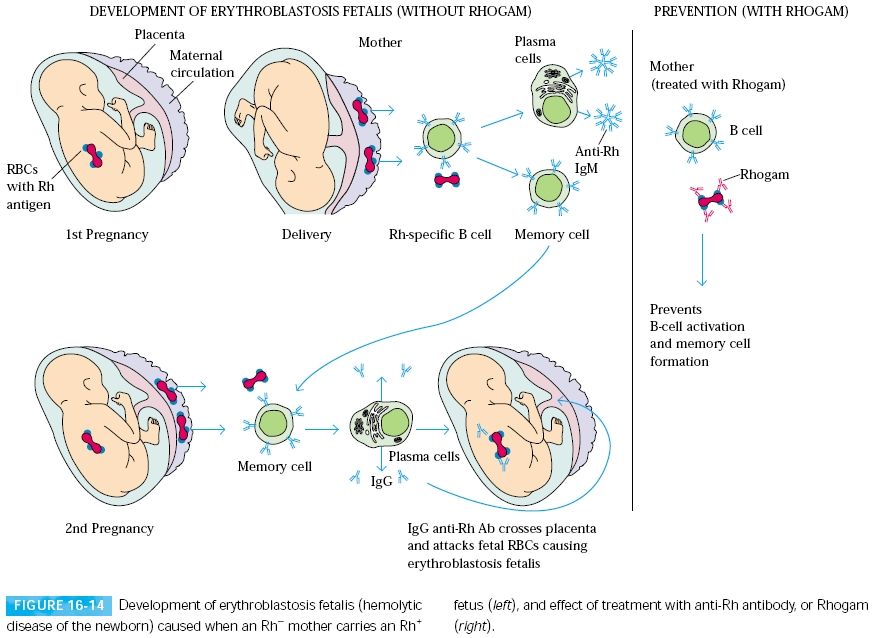 Also, this doctor should be visited by a couple who had two non-developing early pregnancies in a row. nine0005
Also, this doctor should be visited by a couple who had two non-developing early pregnancies in a row. nine0005
Another tip from practice. Many women, having barely become pregnant, rush to confirm this on an ultrasound. Of course, there is no direct evidence that such research is harmful to the fetus, but there is also no evidence to the contrary that it is absolutely harmless. Since you so desire this pregnancy, it’s not worth the risk, and a competent doctor will definitely warn a woman against doing an early ultrasound without any special indications.
Pregnancy and its prospects can be determined using a blood test for hCG (human chorionic gonadotropin), or, more simply, the pregnancy hormone. It is absolutely harmless for pregnancy. It is advisable to donate blood at the beginning of the delay, a week later - again. If the increase in hCG is normal, then the pregnancy is promising, not ectopic - and there are no indications for ultrasound. nine0005
For the first time, a woman should come for ultrasound diagnostics at 11-12 weeks of pregnancy.