Bladder issues during pregnancy
Incontinence During Pregnancy and After Childbirth
Written by WebMD Editorial Contributors
In this Article
- What Types of Incontinence Are Experienced During and After Pregnancy?
- How Is Urinary Incontinence During Pregnancy Treated?
- What Are Kegel Exercises?
- When Should You See a Health Care Professional About Incontinence?
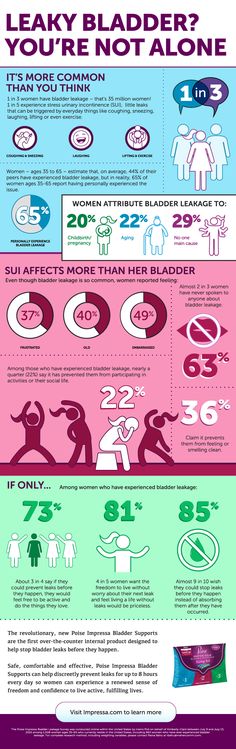
During pregnancy, many women experience at least some degree of urinary incontinence, which is the involuntary loss of urine. The incontinence may be mild and infrequent for some pregnant women. But it can be more severe for others. Age and body mass index are risk factors for pregnancy incontinence, according to one study.
Incontinence can continue after pregnancy and may not be present right after childbirth. Some women do not have bladder problems until they reach their 40s.
What Types of Incontinence Are Experienced During and After Pregnancy?
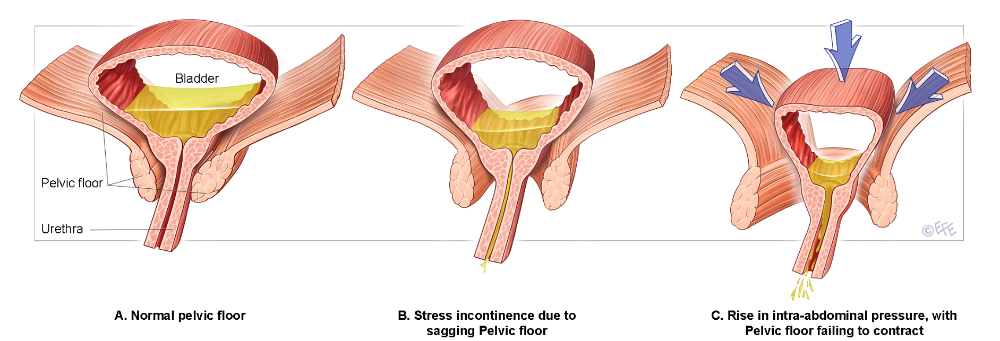
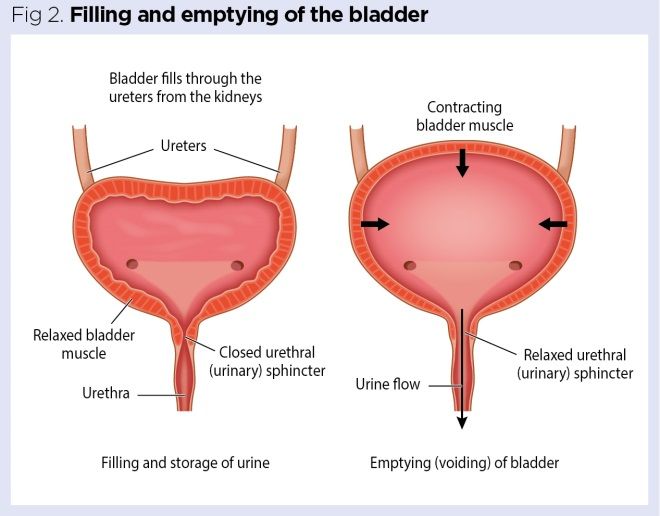
The kind of incontinence experienced during pregnancy is usually stress incontinence (SI). Stress incontinence is the loss of urine caused by increased pressure on the bladder. In stress incontinence, the bladder sphincter does not function well enough to hold in urine.
Urinary incontinence during pregnancy can also be the result of an overactive bladder. Women who have an overactive bladder (OAB) need to urinate more than usual because their bladders have uncontrollable spasms. In addition, the muscles surrounding the urethra -- the tube through which urine passes from the bladder -- can be affected. These muscles are meant to prevent urine from leaving the body, but they may be "overridden" if the bladder has a strong contraction.
The bladder sphincter is a muscular valve that lies at the bottom of the bladder. It works to control the flow of urine. In pregnancy, the expanding uterus puts pressure on the bladder. The muscles in the bladder sphincter and in the pelvic floor can be overwhelmed by the extra stress or pressure on the bladder. Urine may leak out of the bladder when there is additional pressure exerted -- for example, when a pregnant woman coughs or sneezes.
After pregnancy, incontinence problems may continue, because childbirth weakens the pelvic floor muscles, which can cause an overactive bladder. Pregnancy and childbirth also may contribute to bladder control problems because of the following conditions:
- Damage to the nerves that control the bladder
- The fact that the urethra and bladder have moved during pregnancy
- An episiotomy, a cut made in the pelvic floor muscle during delivery of a baby to allow the fetus to come out more easily
How Is Urinary Incontinence During Pregnancy Treated?
Behavioral methods such as timed voiding and bladder training can be helpful in treating urinary incontinence during and after pregnancy. These techniques are often used first and can be done at home. The changes in habits that behavioral methods involve do not have serious side effects.
To practice timed voiding, you use a chart or diary to record the times that you urinate and when you leak urine. This will give you an idea of your leakage "patterns" so that you can avoid leaking in the future by going to the bathroom at those times.
This will give you an idea of your leakage "patterns" so that you can avoid leaking in the future by going to the bathroom at those times.
In bladder training, you "stretch out" the intervals at which you go to the bathroom by waiting a little longer before you go. For instance, to start, you can plan to go to the bathroom once an hour. You follow this pattern for a period of time. Then you change the schedule to going to the bathroom every 90 minutes. Eventually you change it to every two hours and continue to lengthen the time until you are up to three or four hours between bathroom visits.
Another method is to try to postpone a visit to the bathroom for 15 minutes with the first urge. Do this for two weeks and then increase the amount of time to 30 minutes and so on.
In certain cases, a woman may use a pessary, a device to block the urethra or to strengthen the pelvic muscles. In addition, medications also can be helpful in controlling muscle spasms in the bladder or strengthening the muscles in the urethra. Some drugs can help to relax an overactive bladder.
Some drugs can help to relax an overactive bladder.
What Are Kegel Exercises?
Kegel exercises are another method that can be used to help control urinary incontinence. These exercises help tighten and strengthen the muscles in the pelvic floor. Strengthening the pelvic floor muscles can improve the function of the urethra and rectal sphincter.
One way to find the Kegel muscles is to sit on the toilet and begin urinating. Then stop urinating mid-stream. The muscles that you use to stop the flow of urine are the Kegel muscles. Another way to help locate the Kegel muscles is to insert a finger into the vagina and try to make the muscles around your finger tighter.
To perform Kegel exercises, you should:
- Keep your abdominal, thigh, and buttocks muscles relaxed.
- Tighten the pelvic floor muscles.
- Hold the muscles until you count to 10.
- Relax the pelvic floor muscles until you count to 10.
Do 10 Kegel exercises in the morning, afternoon, and at night. They can be done anytime -- while driving or sitting at your desk. Women who do Kegel exercises tend to see results in four to six weeks.
They can be done anytime -- while driving or sitting at your desk. Women who do Kegel exercises tend to see results in four to six weeks.
When Should You See a Health Care Professional About Incontinence?
Talk to your doctor if you still have bladder problems six weeks after delivery. Accidental leaking of urine may mean that you have another medical condition. The loss of bladder control should be treated or it can become a long-term problem.
Tips to prevent involuntary urine leakage (incontinence) during and after pregnancy | Women's Health | Your Pregnancy Matters
Instructions on how to locate pelvic muscles and exercises to strengthen them can help prevent incontinence during and after pregnancy.Friends and family describe stress urinary incontinence (SUI) to pregnant women as if it’s just a fact of life: "After you have a baby, you won't be able to cough, sneeze, or exercise without peeing a little.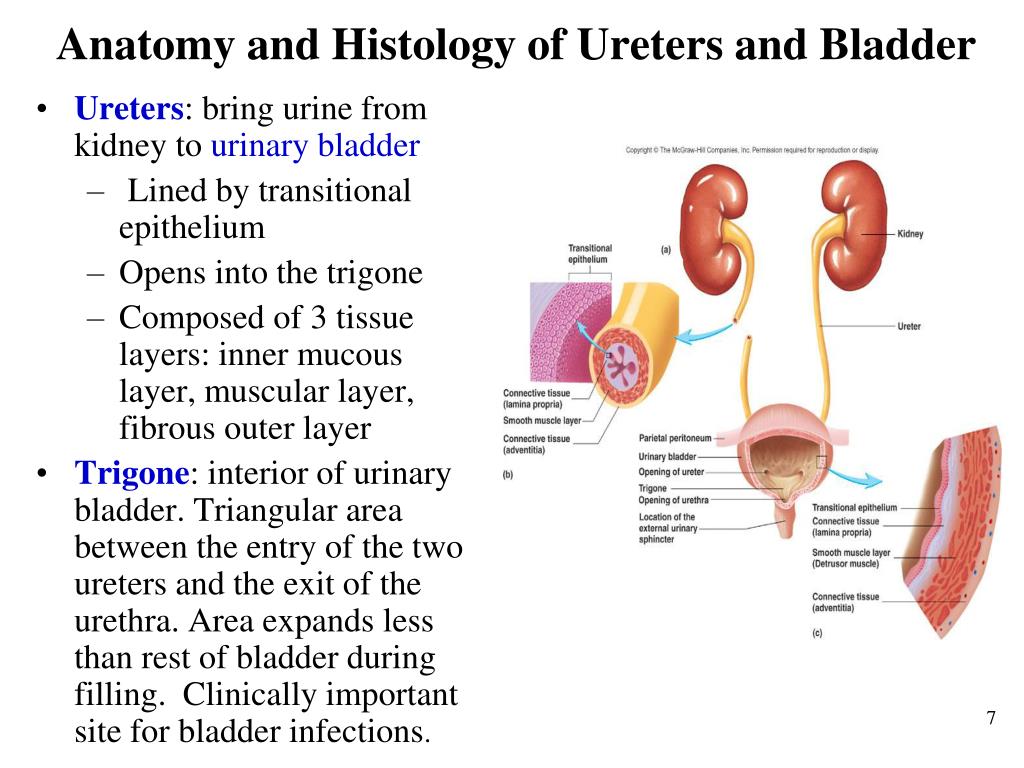 "
"
SUI is the most common type of urinary incontinence associated with pregnancy. More than a third of pregnant women experience involuntary urine leakage during the second and third trimesters, and a third leak during the first three months after delivery.
But you don’t have to just live with urinary incontinence. There are steps you can take to prevent and reduce leakage before, during, and after pregnancy. Interventions can include lifestyle modifications and strengthening your pelvic floor muscles through Kegel exercises.
Unfortunately, not all health care providers make such recommendations. Or they might suggest performing Kegels, but they don't show patients how to do them correctly. There's a lot going on in the pelvic region during pregnancy, and many women don't know how to locate or engage their pelvic floor muscles.
UT Southwestern has one of the largest Female Pelvic Medicine and Reconstructive Surgery divisions in the country. We help patients at all stages of life with strategies and therapies to prevent or treat urinary incontinence.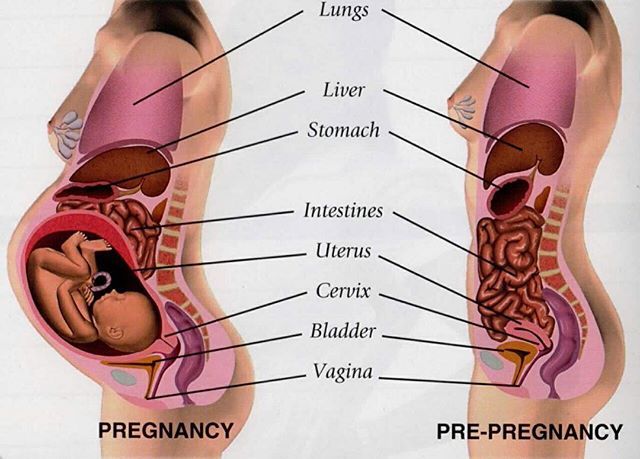
The first step in prevention is education.
Why does urinary incontinence occur with pregnancy?
Pregnancy and childbirth can cause incontinence in several ways:
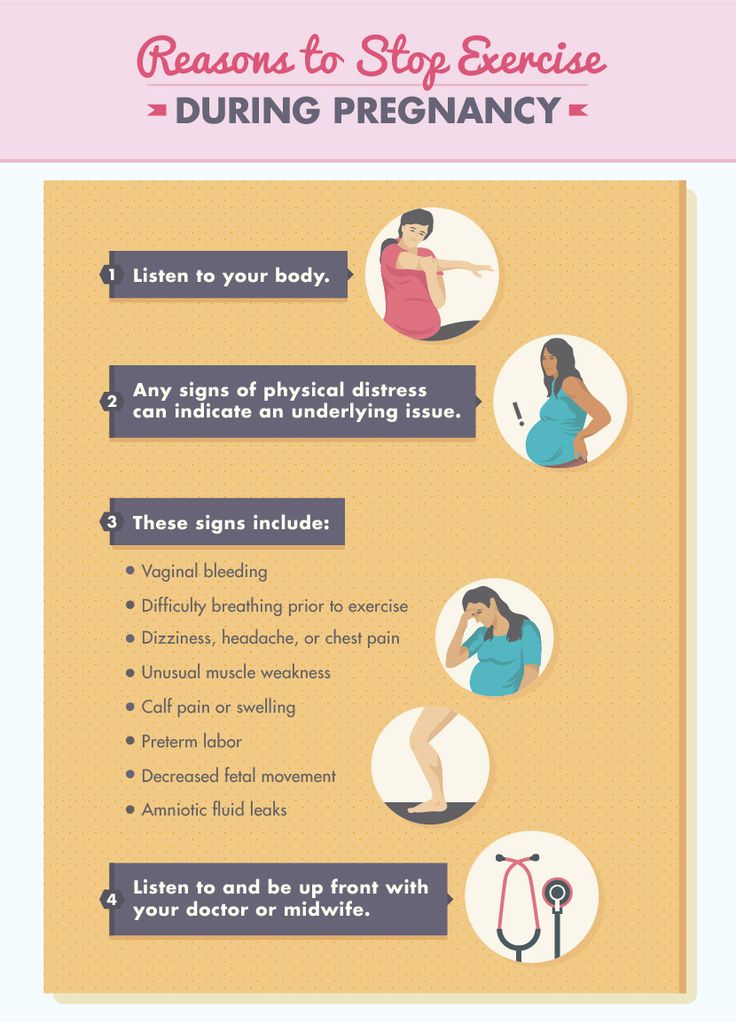
- Your growing baby takes up a lot of room. As the uterus expands, it puts increased pressure on the bladder, urethra, and pelvic floor muscles. This can lead to leakage.
- Changing progesterone levels during pregnancy can weaken the pelvic floor. Increases in this hormone loosen up your ligaments and joints so the belly can expand and so you can deliver. But it can also loosen ligaments in the pelvis that help you hold in urine.
- Childbirth, particularly vaginal delivery, can stretch and weaken the pelvic floor muscles. This can lead to pelvic organ prolapse, in which your bladder, uterus, or rectum droops into the vaginal canal. Prolapse can be associated with urinary incontinence.
- Vaginal delivery also can result in pelvic muscle and nerve injury, which can result in bladder control problems.
If you experience urinary incontinence during pregnancy, you are at higher risk of having a persistent problem after birth. Tell your health care provider about urinary incontinence symptoms as soon as you notice them during pregnancy or at your first postnatal visit.
More than 80% of postpartum women who experience SUI symptoms during pregnancy may continue to experience stress incontinence without treatment.
Related reading: Body after birth: Treating post-pregnancy problems
Where are the pelvic floor muscles?
During initial exam, I often use a clock visual to help women know where their pelvic floor muscles can be palpated. If you lie on your back, imagine the top of the opening of your vagina is 12 o’clock and the bottom of the opening is 6 o’clock.
The pelvic floor muscles are easiest to palpate at the 5 o’clock and 7 o’clock positions– about even with where your legs meet your hips and approximately 3 to 4 centimeters above the vaginal opening.
These are the same muscles you contract when you try to stop the flow of urine midstream or if you were to tighten your vagina around a tampon. And these are the muscles you contract to do Kegel exercises. These pelvic floor muscle exercises were named after Dr. Arnold Kegel, who described them in the 1940s to help patients strengthen their pelvic floor muscles to treat urinary incontinence.
The proper way to Kegel
Verbal or written instructions alone don't necessarily help patients know whether they're doing Kegel exercises properly.
When we see patients for urinary incontinence, we provide education and instruction. We often recommend one to six sessions of supervised Kegel exercises with a female pelvic medicine and reconstructive surgery doctor, a pelvic floor physical therapist, or another provider who has expertise in pelvic floor disorders. While physical therapy or other medical visits usually are not covered by insurance for preventive purposes, they usually are once a problem develops.
In these appointments, your provider will describe how to locate and engage the pelvic floor muscles. The provider will gently press on the pelvic floor muscles with a gloved exam finger inside your vagina and ask you to squeeze the muscles. The muscles will be identified as described. Make sure you’re not squeezing your stomach, legs, or gluteal muscles at the same time, and don’t hold your breath.
Some patients benefit from holding a mirror between the legs to visualize the external anatomy during the exercise. When done properly, you should see the area between your vagina and anus lift toward your upper body.
Doing Kegel exercises regularly is key to strengthening the pelvic floor. We recommend women do 10 repetitions, holding each squeeze for 5 to 10 seconds, three times each day.
You can do the exercises while lying down, sitting, or standing. Many patients find it easier to remember to do Kegels if the exercises become part of a daily routine. Maybe do a set while lying in bed right after you wake up, another as you eat lunch, and another at bedtime.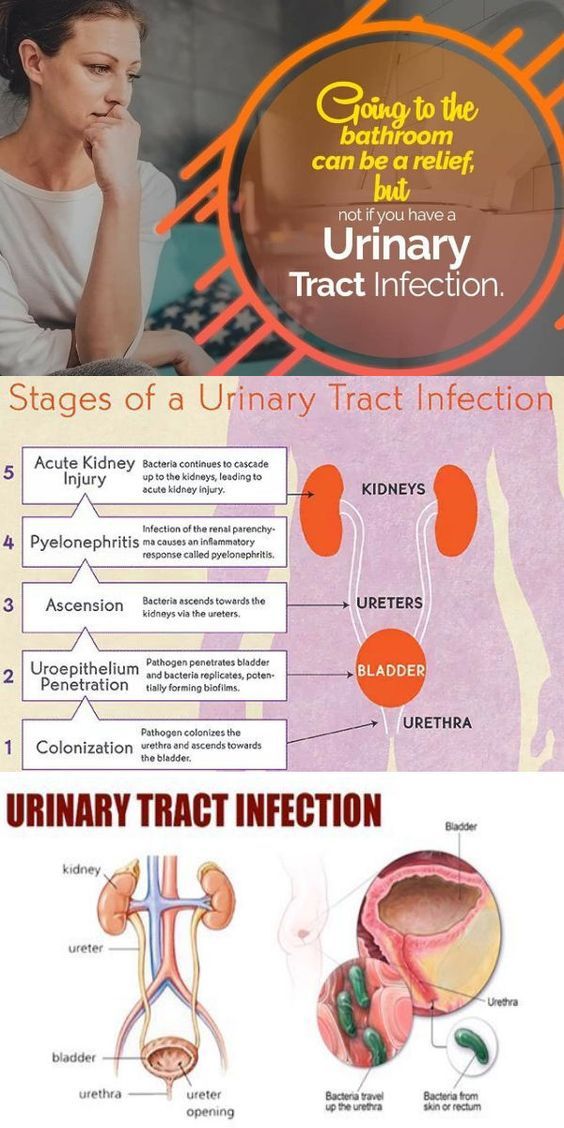
Most women see less frequent urine leakage within a few weeks or months after maintaining a Kegel exercise routine.
Before your big day arrives, get a preview of the accommodations for new moms at UT Southwestern's Clements University Hospital. From the chef-prepared meals to the roomy, high-tech labor and delivery suites, we want to make sure that you, your baby, and your family have the opportunity to bond in a safe and soothing environment.
Lifestyle changes to reduce urinary incontinence
Along with Kegel exercises, there are a few other noninvasive methods to eliminate or reduce the risk of urinary incontinence:
- Lose weight. Excess body weight puts pressure on the bladder.
 Even a 10% reduction in weight can significantly help with urinary incontinence. Work with your doctor to manage your weight gain during pregnancy, and after the birth of your little one, returning to your pre-pregnancy weight will help relieve the pressure on your bladder and pelvic floor.
Even a 10% reduction in weight can significantly help with urinary incontinence. Work with your doctor to manage your weight gain during pregnancy, and after the birth of your little one, returning to your pre-pregnancy weight will help relieve the pressure on your bladder and pelvic floor. - Quit smoking. Smoking has been shown to increase the risk of urinary incontinence as it leads to bladder irritation and chronic coughing.
- Make dietary changes. Some foods and beverages can make incontinence worse. These include caffeine, alcohol, and spicy and acidic foods. This is especially important if you experience urinary frequency and urgency and have trouble making it to the bathroom once you have the urge to urinate. Constipation can worsen symptoms of urine leakage. Stool in the rectum can put pressure on the bladder, urethra, and pelvic floor, so include plenty of higher-fiber foods and fluids in your daily diet.
Other treatments for urinary incontinence
Your doctor may recommend alternative treatment options, such as:
- Electrical stimulation: This therapy can help rehabilitate weak pelvic floor muscles and can be done in conjunction with Kegel exercises.

- Medications: Certain drugs can be used to treat urgency urinary incontinence (UUI) that does not respond to diet and behavioral modification, such as timed voiding to avoid overfilling of the bladder. UUI is associated with a sudden, intense urge to urinate followed by involuntary loss of urine. It is often associated with urinary frequency and urgency. Medications to treat UUI allow the bladder to fill up with more urine before giving the body a signal that it needs to use the bathroom.
- Pessary: This is a plastic insert that supports the vaginal walls. It can be removed, replaced, and cleaned at home.
- Surgical procedures: There are several surgical procedures that can be performed for the treatment of stress urinary incontinence that does not respond to the conservative measures described above. One of the most common and effective surgeries involves placing a synthetic mesh sling between the vagina and the middle portion of the urethra. This supports the urethra like a hammock and helps control urine leakage during activities such as coughing, sneezing, laughing, exercise.
 Other effective surgeries for SUI that do not involve mesh include the Burch colposuspension and the traditional pubovaginal sling with graft material procured from the patient’s own body. Urethral bulking injection is an office procedure that may provide relieve of symptoms in patients who have contraindications for surgery.
Other effective surgeries for SUI that do not involve mesh include the Burch colposuspension and the traditional pubovaginal sling with graft material procured from the patient’s own body. Urethral bulking injection is an office procedure that may provide relieve of symptoms in patients who have contraindications for surgery.
If you are experiencing urinary incontinence during or after pregnancy, know that you’re not alone. Talk with your doctor – we can help you get back to exercising, laughing, and sneezing without worrying about a accidental urine leakage.
To visit with an incontinence expert, call 214-645-8300 or request an appointment online.
Cystitis during pregnancy: description of the disease, causes, symptoms, diagnosis and treatment
What not to do with cystitis in early pregnancy
1. Take antibiotics unless prescribed by a doctor. Self-medication can lead to the development of fetal abnormalities. It is especially forbidden to take tetracycline, ofloxacin, norfloxacin, aminoglycosides.
2. Carrying out instillations. This procedure, during which an antibacterial drug is injected into the bladder, can cause an early miscarriage. nine0005
3. You can not take non-steroidal anti-inflammatory drugs. This refers to the intake of nimesil, diclofenac, analgin, etc. Otherwise, the unborn child may experience severe pathologies.
4. Do not carry out physiotherapy procedures, so as not to provoke a miscarriage.
5. Do not take a hot bath, do not visit the sauna, bath. Avoid overheating to avoid uterine hypertonicity.
How does cystitis manifest during pregnancy?0003
The inflammatory process in the bladder in a pregnant woman is manifested:
-
Frequent urination. This symptom does not always signal the appearance of cystitis. This is normal during pregnancy.
-
The appearance of itching and burning in the urethra. An increase in these symptoms is observed after urine has begun to stand out.
nine0022
-
There is always a feeling that the bladder has not completely emptied.
-
False claims appear. The pregnant woman is in dire need of going to the toilet, but there is no urine output.
-
The stomach hurts, heaviness is felt in the lower part of the abdomen.
-
The color of the urine changes. It is cloudy, reddish in color. This is due to blood impurities. nine0005
-
After emptying the bladder, urine still leaks. The spread of the inflammatory process occurred on the sphincter. In this case, there was a violation of its functioning.
-
A woman observes that a purulent and mucous secretion has begun to be released from the urethra.
-
body intoxication. There is a general weakness, often a headache, body temperature rises, there is no appetite. nine0005
Features of the treatment of cystitis in the later stages
Treatment of the disease in the third trimester of pregnancy is very similar to early treatment. However, there is a decrease in the risk of developing pathologies in the unborn child if the gestational age is more than 24 weeks.
However, there is a decrease in the risk of developing pathologies in the unborn child if the gestational age is more than 24 weeks.
At this time, the formation of the main organs, tissues and systems has already taken place. They just mature and develop. But at this stage of pregnancy, the likelihood of developing cystitis increases, which is dangerous for both the child and the pregnant woman with its complications. nine0005
Those medicines and procedures that were prohibited at an early date may be prescribed at a later date. It must be remembered that only the attending physician can prescribe this. It takes into account all the risks of treatment for the expectant mother and her child.
Exemplary regimen for the treatment of disease in late pregnancy
1. Appointment of antibiotic therapy. They can prescribe amoxicillin, suprax, monural. If the disease is more severe, the doctor prescribes penicillins, macrolipids, and other cephalosporins. nine0005
2. Instillation is carried out. During the procedure, an antibacterial and anti-inflammatory drug is injected into the bladder. This method can be carried out only in late pregnancy and only in the chronic form of the disease. The procedure is carried out in a hospital.
Instillation is carried out. During the procedure, an antibacterial and anti-inflammatory drug is injected into the bladder. This method can be carried out only in late pregnancy and only in the chronic form of the disease. The procedure is carried out in a hospital.
3. Herbal preparations (canephron, urolesan, cystone) are prescribed.
4. Treatment with antispasmodics.
5. Use of physiotherapy. Pregnant women may be prescribed electrophoresis or galvanophoresis with no-shpa or papaverine, calcium chloride, acetylsalicylic acid, antiseptic and antibiotic. These methods are indicated up to 34 weeks of pregnancy. Physiotherapy is in most cases prescribed for chronic cystitis. Contraindication is increased uterine tone, bleeding, preeclampsia, etc. nine0005
6. The use of immunostimulating drugs (flavozid or viferon).
It should be remembered that any therapeutic measures should be prescribed exclusively by a qualified and experienced specialist. With any attempt at self-treatment, the most deplorable consequences for the unborn child can occur.
With any attempt at self-treatment, the most deplorable consequences for the unborn child can occur.
Types of cystitis during pregnancy
Cystitis in early pregnancy can have a different etiology. This means that there is no single method of treating pathology. Drawing up a treatment regimen and prescribing drugs depends on the results of the diagnosis. The disease may be: nine0005
-
Hemorrhagic. The provoking factor is an infectious agent. They mean Escherichia or Pseudomonas aeruginosa, enterobacteria, streptococci. This is the most common form of cystitis. In such a situation, treatment with an antibacterial drug is necessary. The choice of the drug is carried out strictly by the attending physician, since the intake of certain drugs is prohibited in the first trimester of pregnancy.
- nine0004 Interstitial. This type of cystitis is characterized by a non-infectious inflammatory process, that is, the cause of the disease is an allergen or medication.
 To eliminate this form of the disease, an antibiotic is not prescribed. For the treatment of interstitial cystitis, a pregnant woman is shown taking anti-inflammatory, sedative and analgesic drugs.
To eliminate this form of the disease, an antibiotic is not prescribed. For the treatment of interstitial cystitis, a pregnant woman is shown taking anti-inflammatory, sedative and analgesic drugs. -
Luchev. Refers to a rarer occurrence during pregnancy. This is explained by the fact that the conduct of radiation therapy to a woman is prohibited during the bearing of a child. For the treatment of this form of cystitis, antispasmodics, sedatives and drugs are prescribed that help accelerate regenerative processes. nine0005
-
Sexual. An exacerbation of this form of cystitis during pregnancy occurs due to prior infection. Strengthening of the symptoms of the disease is observed after sexual intercourse, if there are no barrier means of protection. This can be easily explained. After intimacy, the microflora changes. If pathogenic or conditionally pathogenic microorganisms have entered the urethra, a woman will notice the appearance of signs of cystitis.
 Genital inflammation of the bladder needs to take antiseptics, sedatives, diuretics. nine0005
Genital inflammation of the bladder needs to take antiseptics, sedatives, diuretics. nine0005
Why does cystitis appear
The development of cystitis during pregnancy occurs under the influence of several factors. An important point is the timely determination of the causes that led to the appearance of cystitis. This is necessary so that the doctor can prescribe effective treatment and draw up a list of medical recommendations that will help the pregnant woman avoid a relapse of the disease. Also, it helps to prevent the transition of the disease into a chronic form. nine0005
There are a number of factors that lead to cystitis:
-
Promiscuous sexual intercourse. The likelihood of infection during sexual contact increases, since the urethra and vagina are located in close proximity. It should be borne in mind that the penetration of infection into the urinary tract can occur, both from the mucous membrane of the vagina and the external genital organ of a woman.
 nine0019
nine0019 -
Prolonged presence of dysbacteriosis or vaginal candidiasis. If the vaginal microflora is disturbed, pathogenic microorganisms multiply much faster. This can cause an inflammatory response. nine0005
-
Impaired immunity. If immunity is lowered or allergic local pathologies are present, a significant decrease in the protective properties of the body occurs. As a result, pathogenic or opportunistic microorganisms enter the bladder without any obstacles.
-
With infrequent urination. It is normal for a woman to empty her bladder at least 4 times a day. During pregnancy, this figure increases. There are various reasons why a timely trip to the toilet is not possible.
 And if it becomes regular, the structure of the urethra and the sphincter anatomically change. As a result of such changes, the normal emptying of the bladder is disrupted. In addition, if urine is in the bladder for a long time, optimal conditions are created for infectious development. nine0005
And if it becomes regular, the structure of the urethra and the sphincter anatomically change. As a result of such changes, the normal emptying of the bladder is disrupted. In addition, if urine is in the bladder for a long time, optimal conditions are created for infectious development. nine0005 -
With regular hypothermia. If the body of a pregnant woman is often supercooled, its local protective properties are weakened, as a result of this, the likelihood of unhindered penetration of the infection into the bladder increases. Damaging factors contribute to the development of an inflammatory reaction in the walls of the bladder, as a result - the appearance of signs of cystitis.
Neglect of hygiene rules. It is necessary to wash the external genital organs daily, to wash after intimacy, to change underwear in a timely manner, to use daily pads. All this helps to reduce the likelihood of infection entering the urinary tract of a woman.
All causes of cystitis are divided into infectious and non-infectious. There are four routes of bladder infection: nine0005
1. Descending - the penetration of the infection occurs from the inflamed organ, that is, the kidney.
2. Ascending - the initial localization of the infection that has entered the bladder is the external environment.
3. Lymphogenic - lymphatic vessels are involved in the movement of the infection. Basically, the focus of infection in the inflamed genital organ.
4. Hematogenous - the spread of infection occurs through the bloodstream from a distant purulent focus. nine0005
Non-infectious causes of cystitis:
-
An allergic reaction, which manifests itself in the form of an inflammatory process of the mucous membrane of the bladder.
-
Disturbed work of the immune system, nervous system.
-
If the lower abdomen or pubis is undergoing radiation therapy.
nine0055 -
regular hypothermia of the body.
-
Constant use of tight underwear.
-
Non-compliance with hygiene rules.
-
Chronic disease of one or another internal organ.
 nine0005
nine0005 -
Overwork, hypovitaminosis.
-
Impaired emptying of the bladder.
-
Reduced protective functions of the body.
-
The presence of a foreign body that is located in the bladder.
- I degree - uncomplicated pyelonephritis that occurred during pregnancy; nine0022
- II degree - chronic uncomplicated pyelonephritis, noted before pregnancy;
- III degree - pyelonephritis with hypertension, azotemia, pyelonephritis of a single kidney.
There are factors in the presence of which increases the likelihood of developing cystitis. This happens when:
Despite the fact that the most common cause of cystitis is a bacterial infection, the inflammatory process in the bladder can begin due to some non-infectious factors. nine0005
Under the influence of certain drugs, especially chemotherapy drugs, an inflammatory process in the bladder can begin. The cause of drug cystitis is the excretion of the decay products of medicines from the body.
With prolonged use of the catheter, there is an increase in susceptibility to bacterial infection. As a result, the likelihood of an inflammatory process increases. This is called foreign body cystitis. nine0005
Some women may be hypersensitive to a particular substance found in personal care or household products.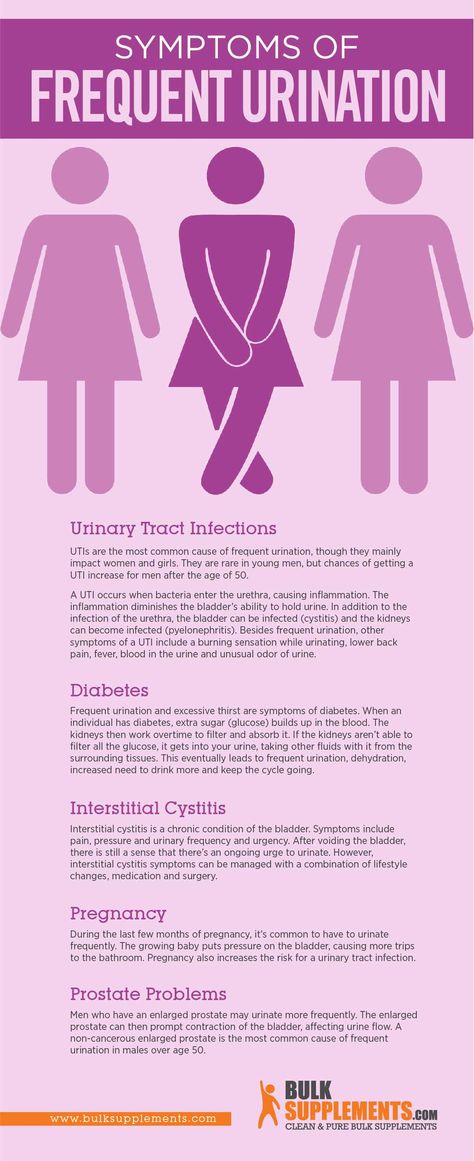 They mean bath foam, feminine hygiene spray, spermicidal gel. In some situations, the inflammatory process is a consequence of the reaction of the body - allergies.
They mean bath foam, feminine hygiene spray, spermicidal gel. In some situations, the inflammatory process is a consequence of the reaction of the body - allergies.
Diagnostic measures
If any signs of cystitis appear, a woman should immediately consult a doctor. At the appointment, the patient is asked about how long ago she noticed the onset of symptoms, whether this happened before, and also what diseases were previously transferred and are present now. The patient must truthfully answer the questions. Otherwise, the doctor will not get a complete picture of what is happening to her. nine0005
To detect cystitis, the doctor sends for a laboratory examination. It consists in the delivery of a general analysis of blood and urine. Thanks to such studies, it is possible to detect inflammation, the level of leukocytes and the immature form of neutrophils, the level of erythrocyte sedimentation rate. In addition, protein in the urine, bacteria are detected. If the result of a general urinalysis showed that the content of leukocytes is increased, the patient is prescribed a urine test according to Nechiporenko.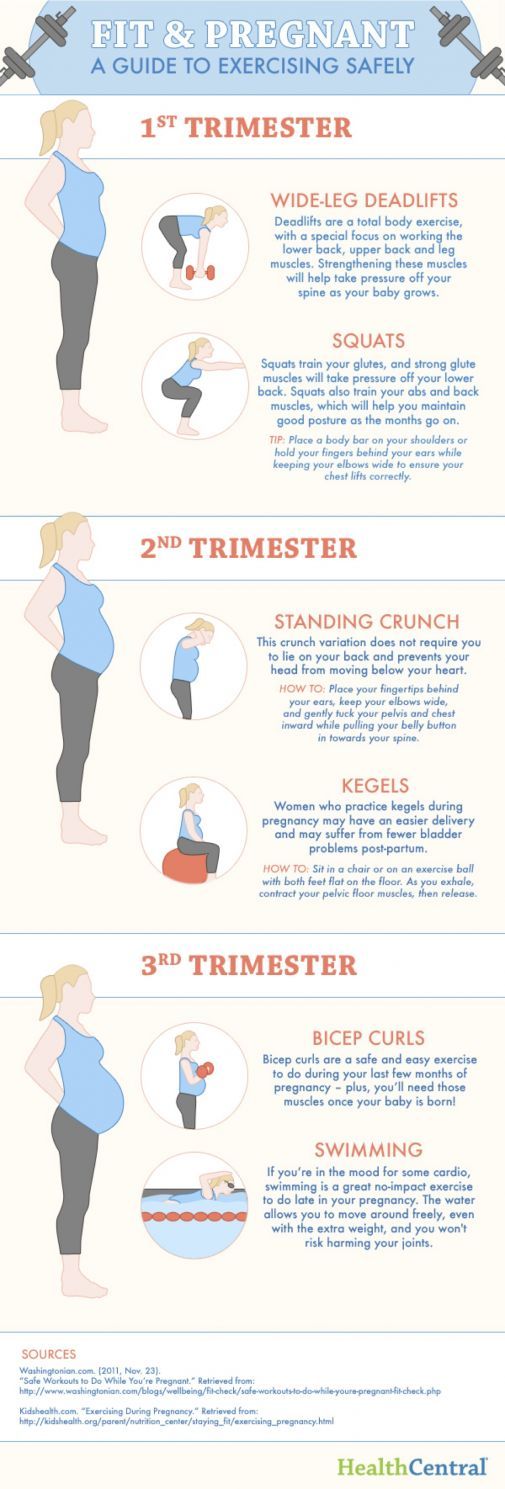
Conducting such a urine test will help determine what was the causative agent of the disease. As a result, more effective treatment is prescribed. With this method of examination, an antibiogram can be performed and the sensitivity of the pathogen to various types of antibacterial drugs can be determined. nine0005
Also, special test strips are used, thanks to which nitrites and leukocytes are determined. Such special strips give a reaction if the products of the activity of pathogenic microorganisms are present in the urine.
Ultrasound examination of the bladder helps to exclude stones in the organ, and also, the doctor assesses the condition of the upper urinary tract and the organs adjacent to the bladder. Ultrasound will allow to exclude a volumetric neoplasm. nine0005
How to prevent the development of cystitis
There are a number of recommendations, subject to which the likelihood of developing the disease decreases.
1. It is necessary to wash every day once a day. For these purposes, use soap, preferably for children. It does not contain fragrances and dyes.
For these purposes, use soap, preferably for children. It does not contain fragrances and dyes.
2. Carefully monitor that the sexual partner observes the basic rules of personal hygiene. He must wash the external genitalia every day. nine0005
3. Before and after sexual intercourse, you should thoroughly wash yourself. Use soap. This rule must be respected by both sexual partners.
4. With stomatitis, tonsillitis, oral candidiasis and other infections, it is not recommended to have oral sex. This rule is easy to explain - with saliva, the infection is transmitted to the external genital organs, and then to the urethra.
5. Always dress for the weather. Hypothermia can cause chronic recurrent cystitis. It should be noted that cystitis is not the most terrible pathology that hypothermia can cause. In addition to cystitis, an inflammatory process develops in nearby organs, which can provoke a miscarriage. nine0005
6. Keep track of the state of your own immunity.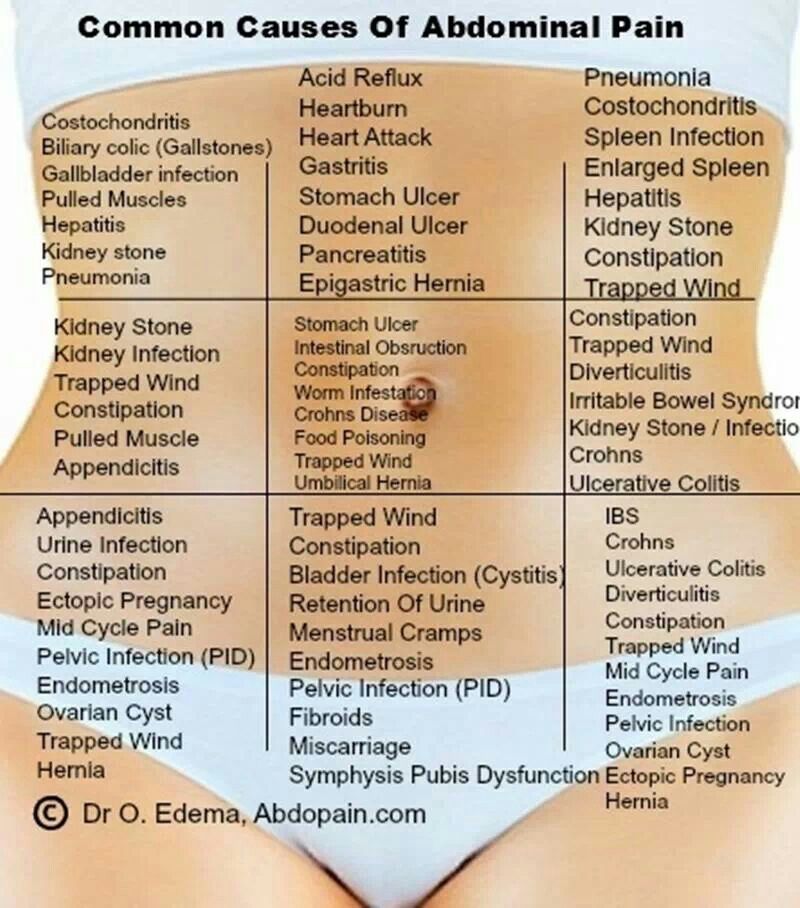 If a woman often has a cold, it can be judged that the work of the immune system is reduced. To restore it, you need to contact a qualified specialist.
If a woman often has a cold, it can be judged that the work of the immune system is reduced. To restore it, you need to contact a qualified specialist.
7. Try as much as possible not to hold back urination. With prolonged retention of urine in the bladder, an infection develops.
8. Drink enough fluids.
9. A man should change his underwear every day. Thanks to this rule, the risk of developing the disease is minimized.
10. After emptying the bowels, wipe from front to back. By no means the other way around. This tactic is easy to explain - if you wipe from back to front, you can transfer intestinal bacteria to the external genitalia. After that, pathogenic microorganisms will reach the urethra.
11. During an exacerbation of the disease, the patient should take about 2.5 liters of fluid per day. It can be both water and fresh natural juices, cranberry juice. Carbonated water and artificial drinks should be excluded from the diet.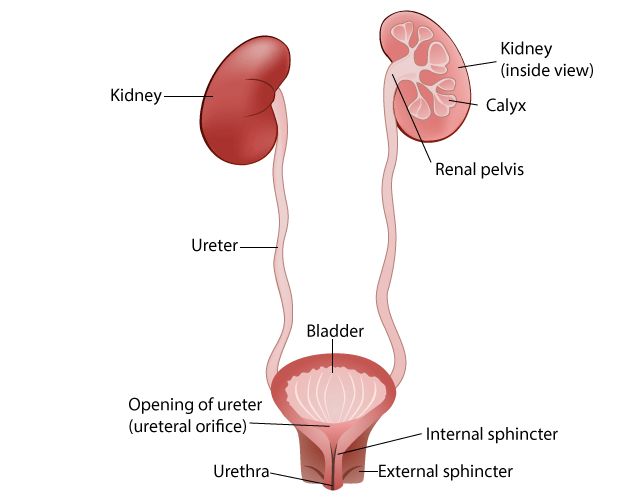 nine0005
nine0005
12. Do not wear tight synthetic underwear.
13. Avoid frequent constipation.
In any case, it is necessary to consult with a qualified specialist who will tell you how a woman should behave during pregnancy. If you do not visit a doctor with symptoms of cystitis, this threatens with dangerous complications not only for the expectant mother, but also for the child, up to the death of the fetus.
Urinary tract infections vs pregnancy: treatment and prevention
Resume. Urinary tract infections are one of the most common complications in pregnant women, which can lead to serious consequences not only for the expectant mother, but also for the child. When managing pregnant women with diseases of the urinary system, it is extremely important to choose the right and, most importantly, safe therapeutic tactics. What drugs are safe during pregnancy? What obstetric and therapeutic tactics are most effective for kidney diseases in pregnant women? What diagnostic methods are best used for asymptomatic bacteriuria, acute cystitis and pyelonephritis? Professor 9 spoke about this in her speech0107 Olga Grishchenko , Head of the Department of Perinatology, Obstetrics and Gynecology of the Kharkiv Medical Academy of Postgraduate Education during the training workshop for gynecologists "Actual Guidelines of Gynecology, Reproductology, Obstetrics", held on March 29, 2019 in Kharkiv. The event was organized by the MedExpert Group of Companies together with the National Medical University named after A.A. Bogomolets and National Medical Academy of Postgraduate Education named after P.L. Shupyk. nine0005
The event was organized by the MedExpert Group of Companies together with the National Medical University named after A.A. Bogomolets and National Medical Academy of Postgraduate Education named after P.L. Shupyk. nine0005
Urgency of the problem
Urinary tract infections (UTIs) are the most common bacterial infections in outpatient practice, they take the 2nd place, second only to respiratory tract infections. According to statistics, 50% of women in the world have an episode of UTI at least once in their lives, of which 25–40% experience a relapse of the disease within 6–12 months. Every year, about 10% of women develop acute cystitis, and pyelonephritis remains the leading cause of hospitalization during pregnancy for non-obstetric indications. nine0005
In the presence of UTIs in pregnant women, the risk of preterm labor and rupture of amniotic fluid, chorioamnionitis increases, premature or functionally immature children are born, and the level of perinatal mortality increases.
In the structure of UTI, asymptomatic bacteriuria is observed in 4-9.5% of pregnant women, acute pyelonephritis - in 12-25%, chronic pyelonephritis - in 33%, glomerulonephritis, urolithiasis - in 0.1-0.2%.
Risk factors and pregnancy
As a rule, infections, self-medication or improper treatment, asymptomatic bacteriuria, frequent UTIs in combination with inflammatory diseases (colpitis), lifestyle and nutrition can affect the occurrence of pathology of the urinary system. nine0005
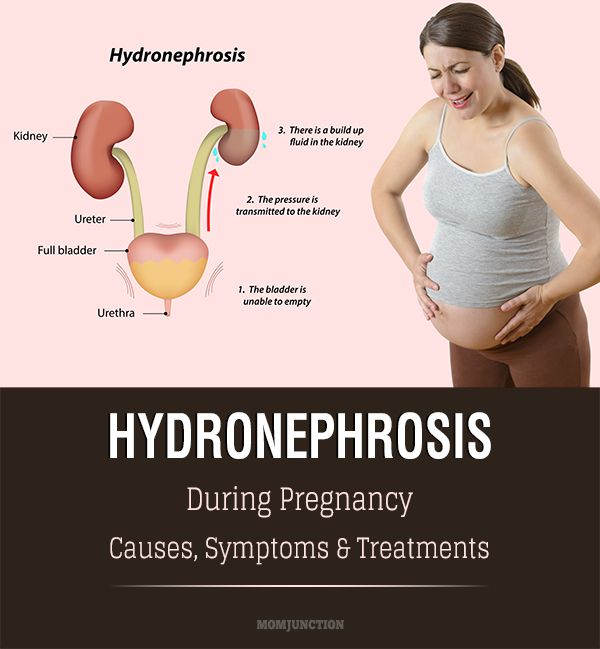
Pregnant women have an increased risk of diseases of the urogenital tract. A high level of progesterone leads to the development of hypotension, hypokinesia, dyskinesia of the ureters and pyelocaliceal system. In turn, the uterus compresses the ureter, high intra-abdominal pressure occurs, especially in primiparas. During pregnancy, the renal pelvis enlarges, the growing uterus squeezes the ureter more and more, the outflow of urine from the kidneys becomes difficult, the urine stagnates, bacteria multiply in it, and inflammation easily occurs. nine0005
nine0005
Infectious agents can enter the bladder by ascending (with inflammatory diseases of the urethra), descending (most often with tuberculous kidney damage), hematogenous (if there is a purulent focus in other parts of the body) and lymphogenic (with diseases of the genital organs) by.
Classification of UTIs in pregnant women
UTIs in pregnant women include asymptomatic bacteriuria, lower urinary tract infections (acute and recurrent cystitis) and upper urinary tract infections (acute pyelonephritis, chronic pyelonephritis in remission, exacerbation, latent course). nine0005
Cystitis in pregnancy: course, diagnosis
Cystitis is an inflammation of the bladder wall, one of the most common urological diseases, as a rule, its cause is an infection. Symptoms of cystitis in women are manifested in the form of frequent urination, cramps and pain when urinating, pulling sensations in the lower abdomen, weakness, fatigue, irritability, blood in the urine, cloudy urine, pus or yellow spots on the underwear.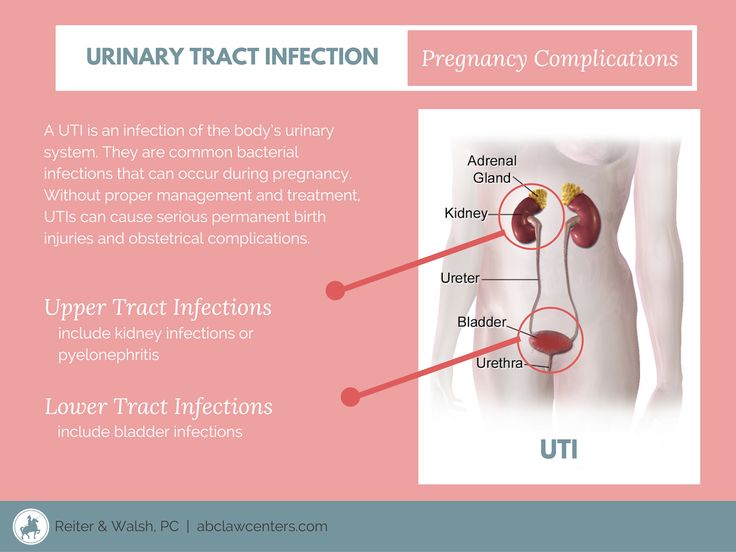
Normally, urination is not accompanied by pain. In women, painful urination can be caused by diseases of the bladder, urethra, or vagina. So, pain in the bladder, as a rule, is felt in the area of the womb, it can increase during urination or, conversely, decrease when the bladder is empty. Urethral pain associated with urination is felt by the patient directly in the urethra and is usually aggravated by urination. Urine entering the vaginal opening can cause pain if it is inflamed. Inflammation of the urethra is most often characterized by a bacterial nature and requires additional examination and treatment. nine0005
Primary diagnosis of cystitis involves an examination by specialized specialists (urologist, nephrologist, gynecologist), as well as taking an anamnesis and establishing possible causes of the disease (hypothermia, unprotected intercourse, taking medications, the presence of concomitant diseases).
Laboratory tests include a urinalysis for Nechiporenko cultures (helps identify the pathogen), a general urinalysis (allows you to identify erythrocytes, leukocytes, protein in the urine; the urine itself may be cloudy with an admixture of blood or pus), a general blood test (allows you to identify a picture inflammatory process, it is possible to increase the erythrocyte sedimentation rate (ESR), leukocytosis). Among instrumental methods, ultrasound examination (ultrasound) of the bladder, ureteroscopy and cystoscopy (in case of violation of the passage of urine) are used. nine0005
Among instrumental methods, ultrasound examination (ultrasound) of the bladder, ureteroscopy and cystoscopy (in case of violation of the passage of urine) are used. nine0005
Asymptomatic bacteriuria during pregnancy
Asymptomatic bacteriuria during pregnancy is dangerous for both the mother and the fetus, against its background, 25% of women develop acute pyelonephritis. According to the World Health Organization, about 8% of women report asymptomatic bacteriuria, 15-57% of women with untreated asymptomatic bacteriuria develop symptoms of UTI (acute cystitis or pyelonephritis). Therapy of this disease during pregnancy reduces the risk of developing acute UTIs, preterm birth, and low birth weight. nine0005
Diagnosis of asymptomatic bacteriuria can be established by detecting 10 5 CFU/ml of one strain of bacteria or 10 2 CFU/ml of uropathogen Escherichia coli in 2 urine samples taken from leukocytes containing >4 h field of view in the absence of clinical manifestations of UTI.
It should be remembered that the risk of this pathology is most real from the 9th to the 17th week of pregnancy. The only reliable method for diagnosing asymptomatic bacteriuria is the method of urine culture. nine0005
In accordance with Ukrainian and international recommendations for asymptomatic bacteriuria, oral antibiotic therapy with a single dose of fosfomycin trometamol is recommended.
Pyelonephritis: diagnosis
Pyelonephritis is an infectious and inflammatory disease of the kidneys of bacterial etiology with a primary and predominant lesion of the interstitium and tubular apparatus. The incidence of pyelonephritis during pregnancy reaches 33%, mortality - 3.5%, maternal mortality from kidney disease in the structure of extragenital pathology is 8-10%, the incidence of gestational pyelonephritis is 11.5%. nine0005
Primary pyelonephritis in pregnant women is difficult to treat, may be accompanied by fever, chills, nausea, vomiting, pain in the lumbar region, the appearance of pyuria, bacteriuria.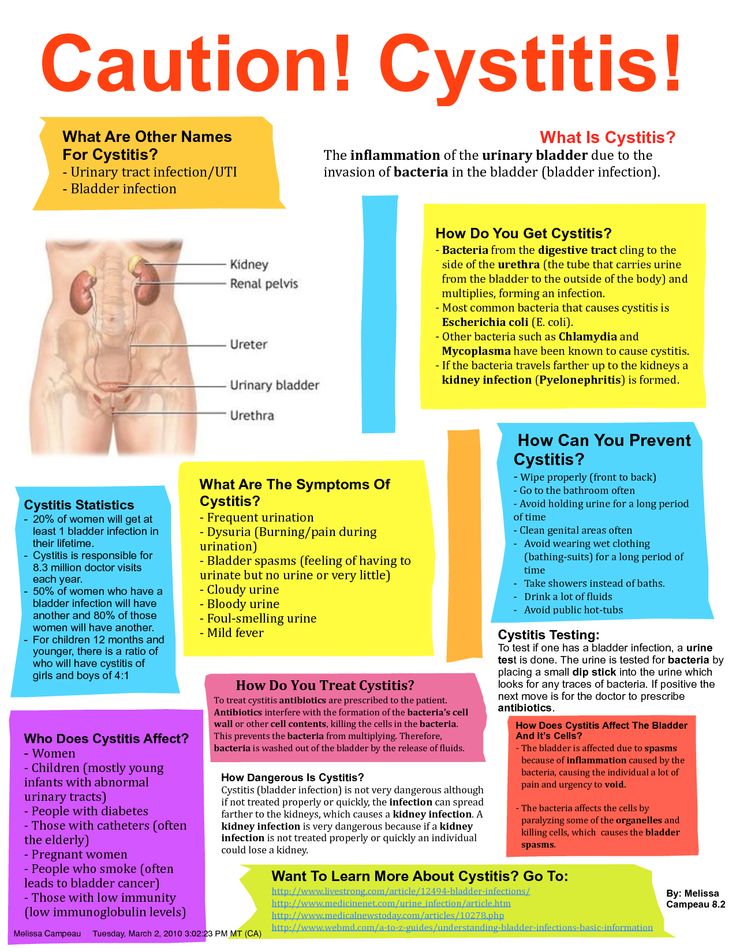 As a rule, the right kidney is affected more often than the left one, with expansion of the pelvicalyceal system (according to ultrasound).
As a rule, the right kidney is affected more often than the left one, with expansion of the pelvicalyceal system (according to ultrasound).
In acute pyelonephritis, the mandatory research methods are a general urinalysis (in 2 portions) 1 time in 7 days, a Nechiporenko urinalysis, a general and biochemical blood test, a bacteriological urinalysis, ultrasound of the kidneys and bladder, daily proteinuria, a biochemical blood test , blood pressure monitoring, urologist consultation. Additional research methods - computed tomography without contrast or excretory urogram, nuclear magnetic resonance imaging - are carried out exclusively for strict, sometimes vital, indications. nine0005
It should be remembered that dysuria in primary acute cystitis with a body temperature of 38 ° C and chills may indicate acute ascending pyelonephritis. A sharp dysuric syndrome is characteristic of the associated cystitis during exacerbation of chronic pyelonephritis. Urinary syndrome (proteinuria, leukocyturia, hematuria, etc. ) may periodically disappear with a unilateral process and ureter occlusion; therefore, serial urine tests are necessary. The degree of leukocyturia does not always correspond to the severity of the inflammatory process. A single urine culture gives at least 20% false positive results. Bacteriuria appears and can be detected 2 days earlier than pyuria. nine0005
) may periodically disappear with a unilateral process and ureter occlusion; therefore, serial urine tests are necessary. The degree of leukocyturia does not always correspond to the severity of the inflammatory process. A single urine culture gives at least 20% false positive results. Bacteriuria appears and can be detected 2 days earlier than pyuria. nine0005
Choice of drugs for the treatment of pregnant women with UTIs
There are certain requirements for antibiotics for the treatment of UTIs in pregnant women. In particular, they must be effective against most pathogenic pathogens, have the ability to create a high concentration in organs - foci of infection, have a long half-life sufficient to maintain a high concentration of the antibiotic in the blood, not have toxic and allergic effects, be well tolerated by patients, be harmless to mother and fetus. nine0005
It has been shown that it is advisable to use antibacterial uroseptics for the treatment of pregnant women with acute cystitis, asymptomatic bacteriuria, acute pyelonephritis. In particular, fosfomycin trometamol has a bactericidal effect associated with blocking the bacterial enzyme involved in the synthesis of the cell wall, as well as an anti-adhesive effect (destroys the fimbria of Escherichia coli, preventing it from fixing on the wall of the urothelium and promoting leaching from the urinary tract). After a single dose of the drug, the therapeutic concentration is observed for 48 hours (this is enough to sterilize urine and recover). nine0005
In particular, fosfomycin trometamol has a bactericidal effect associated with blocking the bacterial enzyme involved in the synthesis of the cell wall, as well as an anti-adhesive effect (destroys the fimbria of Escherichia coli, preventing it from fixing on the wall of the urothelium and promoting leaching from the urinary tract). After a single dose of the drug, the therapeutic concentration is observed for 48 hours (this is enough to sterilize urine and recover). nine0005
An alternative to antibiotics are phytoneering preparations with anti-adhesive and antibacterial activity, as well as anti-inflammatory, antispasmodic, nephroprotective properties.
Organization of care for pregnant women with UTI and prevention
Delivery of pregnant women with UTI (without obstetric pathology) is carried out through the natural birth canal, taking into account the obstetric situation.
There are degrees of risk of pyelonephritis: