Hepatitis b pregnant
Hepatitis B Foundation: Pregnancy and Hepatitis B
Babies born to a mother with hepatitis B have a greater than 90% chance of developing chronic hepatitis B if they are not properly treated at birth. It is very important that pregnant people know their hepatitis B status in order to prevent passing the virus on to their newborn baby during delivery. If your doctor is aware that you have hepatitis B, he or she can ensure hep B transmission to your baby is prevented by taking the right steps based on blood tests results and to make arrangements to have the proper medications in the delivery room to prevent your baby from being infected.
ALL pregnant people should be tested for hepatitis B. Testing is especially important for people who fall into high-risk groups such as health care workers, people from ethnic communities or countries where hepatitis B is common, spouses or partners living with an infected person, etc. If you are pregnant, be sure your doctor tests you for hepatitis B before your baby is born, ideally as early as possible during the first trimester.
If you test positive for hepatitis B infection, then your newborn must be given proper prevention immediately in the delivery room, clinic or bedside:
- first dose (called "birth dose") of the hepatitis B vaccine
- one dose of the Hepatitis B Immune Globulin (HBIG).*
* Note: HBIG is recommended by U.S. CDC. HBIG is not recommended by WHO and may not be available in all countries. What is most important is to make sure the hepatitis B vaccine birth dose is given as soon as possible!
If these two medications are given correctly, a newborn born to a person with hepatitis B has more than a 90% chance of being protected from a hepatitis B infection. You must make sure your baby receives the remaining shots of the vaccine series according to schedule to ensure complete protection.
Although the U.S. CDC states that the medications can be given within the first 12 hours of life and the WHO states vaccine birth dose can be given within 24 hours, there is no second chance to protect an infant once this window of opportunity is missed. Therefore, the Hepatitis B Foundation strongly recommends that health care professionals properly administer the birth dose of the hepatitis B vaccine immediately in the delivery room to avoid any delays or mistakes.
Therefore, the Hepatitis B Foundation strongly recommends that health care professionals properly administer the birth dose of the hepatitis B vaccine immediately in the delivery room to avoid any delays or mistakes.
If you test positive for hepatitis B infection while pregnant, your doctor also should do a hepatitis B viral load blood test (HBV DNA) during your pregnancy. In some cases, the laboratory test results may show a very high viral load. In these cases, your physician may recommend that you take an oral antiviral drug in your third trimester to reduce the risk of infecting your newborn at birth. If the hepatitis B viral load test is not available, WHO recommends that pregnant women are tested for the hepatitis B e-antigen (HBeAg), and if positive, an antiviral is recommended during the last trimester. Regardless of viral load levels or HBeAg status, the hepatitis B vaccine birth dose and completion of the vaccine series is essential to protect your infant from infection with the hepatitis B virus.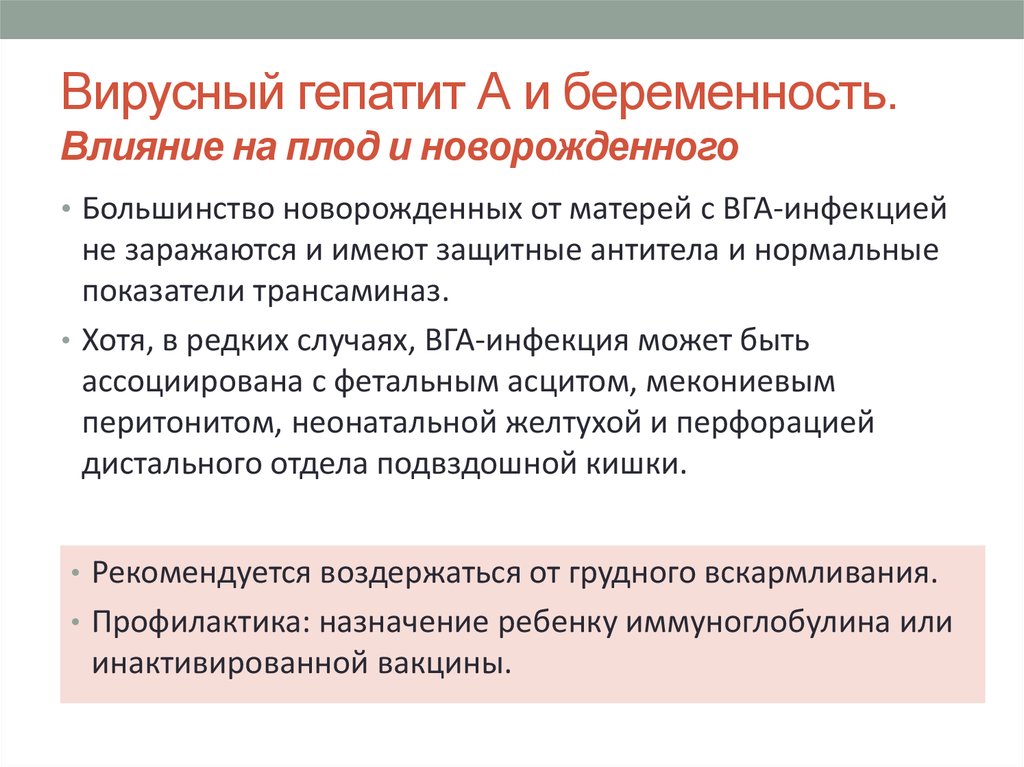
Additional Resource Links:
U.S.: Centers for Disease Control and Prevention: Viral Hepatitis, Perinatal Transmission (2022)
EU/EEA: Antenatal Screening for HIV, Hepatitis B, Syphilis and Rubella Susceptibility in the EU/EEA (2016)
Globally: WHO Prevention of Mother-To-Child Transmission of Hepatitis B Virus: Guidelines on Antiviral Prophylaxis in Pregnancy (2020)
Page updated September 2020.
Hepatitis B Foundation: Treatment During Pregnancy
A hepatitis B virus infection should not cause any problems for you or your unborn baby during your pregnancy if you take the correct precautions. It is important for your doctor to be aware of your hepatitis B infection so that he or she can run appropriate tests and evaluate and monitor the health of your liver, and so your baby can be protected from infection with hepatitis B when it is born. The U.S. CDC and WHO recommend that ALL pregnant people are tested for hepatitis B.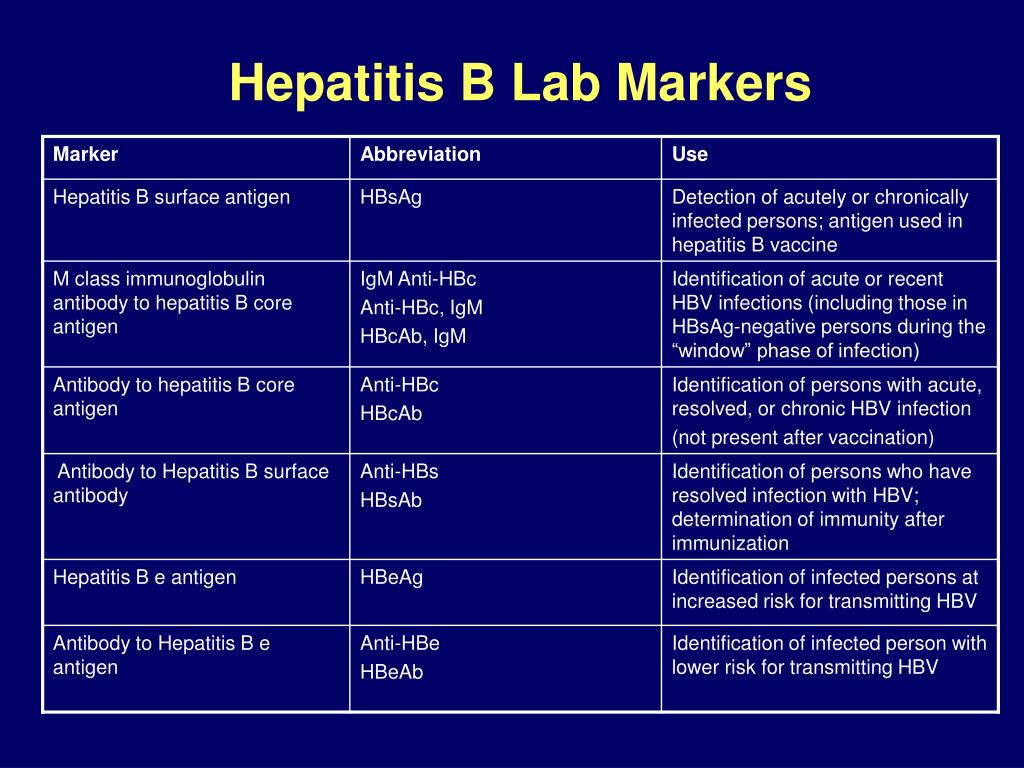 Please ask your doctor to test you for hepatitis B early in your pregnancy!
Please ask your doctor to test you for hepatitis B early in your pregnancy!
The birth dose of the hepatitis B vaccine and hepatitis B immune globulin (HBIG, if recommended and available) can sometimes fail to prevent transmission to newborns. This typically occurs in pregnant people who are HBeAg positive and have a very high viral load, allowing for the transmission of hepatitis B to your baby. Fortunately, there is a way to prevent transmission even if you are a person with a high viral load.
All people who are diagnosed with hepatitis B in pregnancy should be referred for follow up care with a physician skilled at managing hepatitis B infection. Your physician should perform additional laboratory testing, including HBV DNA level (viral load), and should be checked to see if there is evidence of cirrhosis (extensive liver damage). (click here for a detailed description of these tests).
An HBV DNA level greater than 200,000 IU/mL or 1 million cp/ml indicates a level where the combination of the birth dose of the hepatitis B vaccine (and HBIG) will fail. First-line, antiviral therapy with tenofovir (TDF/viread) is recommended starting from week 28 of pregnancy until delivery but may continue 3 months postpartum. Please talk to your doctor about your own test results.
First-line, antiviral therapy with tenofovir (TDF/viread) is recommended starting from week 28 of pregnancy until delivery but may continue 3 months postpartum. Please talk to your doctor about your own test results.
If the HBV DNA (viral load) blood test is not available or is cost prohibitive, then pregnant people should be tested for HBeAg (a blood test). A “positive” HBeAg test result can indicate a high virus level. Antiviral treatment with tenofovir (TDF) during the last trimester would be recommended for women who test HBeAg positive. TDF Treatment may be discontinued after delivery or 3-months postpartum.
All babies born to people with hepatitis B should receive a birth dose of the hepatitis B vaccine within 24 hours of delivery whether they receive treatment with an antiviral or not.
All people who are diagnosed with hepatitis B should be referred to care with a knowledgeable doctor. Some may require continued treatment with an antiviral, many will not. All people need regular monitoring throughout their life since hepatitis B infection and the health of the liver can change over time.
Additional Resource Links:
U.S.:
Centers for Disease Control and Prevention: Viral Hepatitis, Perinatal Transmission (2018)
EU/EEA:
Antenatal Screening for HIV, Hepatitis B, Syphilis and Rubella Susceptibility in the EU/EEA (2016)
Globally:
WHO Prevention of Mother-To-Child Transmission of Hepatitis B Virus: Guidelines on Antiviral Prophylaxis in Pregnancy (2020)
Page updated September 2020
What to do if hepatitis B or C viruses are detected during pregnancy, preparation for pregnancy or IVF procedure
Hepatit.ru
Specialized scientific hepatological center Academicians of RAMS
V.I. Pokrovsky and Yu.M. Lopukhin
Park Kultury
How to get there in 30 seconds
Moscow, Zubovsky boulevard, 13
+7 (495) 255-10-60
PRE-BOOKING
DAILY: 9:00-21:00
In 22 years, 32487 patients were successfully treated. New drugs give a guarantee of up to 99%!
New drugs give a guarantee of up to 99%!
Schedule of the Clinic on New Year's holidays: December 30 - January 3 non-working days
January 4, 5, 6 working days from 10:00
January 7-9 non-working days
- Home
- You have been diagnosed with hepatitis B or C virus while preparing for pregnancy or IVF
In preparation for pregnancy, you passed tests, including those for hepatitis. If, according to the results of these tests, markers of viral hepatitis are found in you (HBs-Ag - positive, or HCV - positive), then you will need to contact a hepatologist to confirm the diagnosis and advise on your next steps in confirming the diagnosis of hepatitis. In our center there is a specialist who has extensive experience in accompanying pregnancy with viral hepatitis - this is Nelli Nikolaevna Tsurikova, Candidate of Medical Sciences. nine0003
Hepatitis B and C are not a contraindication to pregnancy. You have a real opportunity to give birth to a healthy child.
The hepatitis C virus does not cross the placenta and can be transmitted to the baby in extremely rare cases. Much more contagious is the hepatitis B virus, which can be transmitted to a child in about 30-40% of cases. In this regard, with hepatitis C, childbirth can be carried out in a general maternity hospital, and with hepatitis B, preferably in a specialized department, where specialists have the opportunity to take all the necessary measures for the child in order to exclude the transmission of the virus during childbirth, and also immediately after birth to introduce drugs in case of infection during pregnancy, preventing the development of infection. In addition, the child is vaccinated according to a special scheme for children born to an infected mother. nine0003
It should be borne in mind that pregnancy is an additional burden for the liver. Therefore, if you have viral hepatitis, then first of all it is necessary to find out with a hepatologist the condition of the liver, the degree of its damage by the virus.
During pregnancy, it is desirable to be under the control of a hepatologist, since it is possible to exacerbate the process and worsen the mother's condition.
Hepatologist's consultation
until December 24 free of charge
Important to know
- What is hepatitis B
- Hepatitis B treatment
- What is Hepatitis C
- Hepatitis C treatment
- Treatment of hepatitis C with new drugs
- alcoholic liver disease
- Fatty hepatosis
- Cirrhosis of the liver
- What is liver elastometry (fibroscan)
- Analyzes and examinations
Do you have a reason to see a hepatologist? nine0011
1) Do you have heaviness in your right side?yes no
2) Have you visited a dentist in the last 5 years?
yes no
3) Have you had surgery or tattoos?
yes no
4) Do you often feel tired?
yes no
5) Is your waist larger than 90 cm?
yes no
Patient reviews View all reviews
Gratitude from Channel One for help in preparation and participation in the program "Male and Female" nine0003
hepatology center in Moscow —
"HEPATIT. RU" © 2001 - 2022
RU" © 2001 - 2022
Clinic on Sadovy
119021 Moscow, Zubovsky boulevard, 13
+7 (495) 255-10-60
Appointment for consultation daily: 9:00 - 21:00
Thank you, your application has been received
Viral hepatitis B and pregnancy
06/01/2018
Viral hepatitis B should not be in our children. There are all means for this in the modern world. There are effective and safe recombinant vaccines, and the control of protective antibody levels is simple and cheap. All that is required of us is to vaccinate the child and periodically assess the level of antibodies to the HBs antigen of the hepatitis B virus (Anti-HBs), if necessary, re-vaccinate. How often should antibodies be monitored? Not very often, once every few years is more than enough. We all periodically donate blood for certain tests, and taking an additional sample on occasion will not be difficult. Naturally, not only children, but also all adults should be vaccinated. You don't need to weigh the risks of catching hepatitis B, you just need to be vaccinated. nine0005
You don't need to weigh the risks of catching hepatitis B, you just need to be vaccinated. nine0005
However, some of us are already living with hepatitis B, including mothers-to-be. Mothers whose blood contains HBsAg and HBeAg - we are talking about certain viral proteins - transmit the virus to their children in 70-90% of cases, HBeAg-positive and HBsAg-negative mothers transmit the virus to their child in 10-40% of cases. If vertical transmission of the virus from mother to child has been realized, then the probability of chronic hepatitis B in a child is about 90%, with very sad, albeit distant, prospects. nine0003
Transmission of the virus in utero is a very small percentage of cases, according to some estimates, no more than 4%, the main risk area is childbirth. The complex of active immunoprophylaxis - an immunoglobulin such as HBIG, and a passive one - a hepatitis B vaccine, literally in the first hours after childbirth, can significantly reduce the risks of vertical transmission to about 3%. And all cases of vertical transmission with adequate prophylaxis are associated with a high viral load and the presence of HBeAg.
And all cases of vertical transmission with adequate prophylaxis are associated with a high viral load and the presence of HBeAg.
And this unfavorable factor can also be eliminated or minimized as much as possible today. Viral load, if indicated, can be effectively suppressed by using quite safe antiretroviral drugs in the third trimester of pregnancy. The drug of choice here is tenofovir, the alternative solution is telbivudine. This should be done, of course, under the supervision of a qualified doctor who is very well versed in the matter.
Caesarean section, and even more so the use of HBIG during pregnancy, are not recommended, these measures have not been shown to be effective. It is worth noting that there are some reasonable doubts about the effectiveness of HBIG even after childbirth, but since it is safe, and data on effectiveness, albeit of low quality, are available, this option is considered relevant today. nine0003
Breastfeeding in the presence of hepatitis B is not contraindicated, even for unvaccinated children it does not carry serious risks, however, we repeat - there should not be those who are not vaccinated against hepatitis B.