Baby fussy after switching whole milk
Does Your Child Cry Over Milk Protein Allergy?
- Digestive Health
Women. Wisdom. Wellness. Jun 29, 2018
It's easy to get the care you need.
See a Premier Physician Network provider near you.
Schedule Now
If your baby’s fussy, one of the possible reasons could be that she’s allergic to cow’s milk protein. A milk protein allergy can cause digestive discomfort and frequent spitting up.
An allergy to the protein in cow’s milk affects 2 to 3 percent of children under age 3. If your child is allergic to cow’s milk, her body’s immune system has an abnormal reaction to the milk protein.
This is different than lactose intolerance, a condition you may be more aware of.
Your doctor can help determine if your child has a cow’s milk allergy, if he’s lactose intolerant, or if something else is causing symptoms.
The good news: About 80 percent of children outgrow the milk protein allergy by the time they are 16.
Cow’s Milk Allergy vs. Lactose Intolerance
An allergy to cow’s milk and lactose intolerance affect different body systems and cause different symptoms.
Milk allergy. If your child has a milk allergy, his immune system attacks the milk protein, releasing histamines and other chemicals that cause allergic reactions in the skin, such as hives, and/or the gastrointestinal system. Breastfed babies with a milk allergy react to dairy products eaten by the mother. Formula-fed babies react to the cow’s milk protein in the formula.
Symptoms of a milk allergy include:
- Frequent spitting up
- Vomiting
- Abdominal pain
- Crying and irritability after feeding
- Diarrhea
- Blood in stool
- Not gaining weight
- Hives
- Scaly skin rash
- Coughing or wheezing
- Watering eyes and stuffy nose
- Anaphylaxis (extreme allergic reaction that affects breathing)
There are two types of cow’s milk allergies – one with an immediate reaction and the other, delayed:
- IgE mediated milk allergy causes a reaction within two hours of exposure to cow’s milk protein.
 IgE, or immunoglobulin E, is a human antibody that causes allergy symptoms like hives, rashes and wheezing.
IgE, or immunoglobulin E, is a human antibody that causes allergy symptoms like hives, rashes and wheezing. - Non-IgE mediated milk allergy carries a delayed response, with symptoms appearing 48 hours to a week after exposure to cow’s milk protein.
Milk (lactose) intolerance. If your child is lactose intolerant, she cannot digest the sugar in milk called lactose. Babies are rarely born with lactose intolerance. The condition more commonly develops in older children and adults. People who are lactose intolerant do not have enough lactase. Lactase is an enzyme produced in the small intestine and is needed to digest lactose.
Symptoms include:
- Gas
- Diarrhea
- Bloated stomach
- Abdominal cramps
- Irritability, crying
- Eczema
- Failure to thrive and gain weight
If your child shows signs of milk allergy or milk intolerance, talk with your doctor right away.
Who’s at Risk for a Milk Allergy?
Cow’s milk is one of eight food allergens that make up most cases of food allergies in the U. S. The others are eggs, fish, peanuts, shellfish, soy, tree nuts and wheat.
S. The others are eggs, fish, peanuts, shellfish, soy, tree nuts and wheat.
Children with a parent or sibling who has asthma, eczema or seasonal allergies may be more likely to develop a milk allergy.
The following symptoms of milk allergy require immediate medical attention:
- Difficulty breathing (anaphylaxis)
- Turning blue
- Lethargy, extreme weakness
- Generalized hives
- Fever
- Bloody diarrhea
- Swelling in area of head and neck
In the case of severe symptoms or anaphylaxis, be prepared to use an EpiPen, which contains an injectable dose of epinephrine, the only medicine that can reverse the symptoms of anaphylaxis.
The good news: About 80 percent of children outgrow the milk protein allergy by the time they are 16.
Diagnosis and Treatment
To diagnose a cow’s milk allergy, your doctor will talk with you about your child’s medical and family history and symptoms. The doctor may perform tests, such as:
The doctor may perform tests, such as:
- A skin-prick test
- A serum IgE blood test
- Checking the stool
If your baby has a milk allergy, he must avoid milk, other dairy products and products containing milk protein. And if you breastfeed, these restrictions apply to you, too.
Babies taking formula should switch to a hypoallergenic version recommended by your doctor. It is best to avoid soy-based formula because many children who are allergic to cow’s milk are also sensitive to soy.
If you have children age 1 and older who are allergic to cow’s milk protein, remove milk and milk products from their diet, including:
- Milk
- Cheese
- Ice cream
- Yogurt
Read labels carefully. That’s because two kinds of milk proteins are found in many foods:
- Casein is the solid part of milk and makes up 80 percent of milk protein.
- Whey is in the liquid part of milk, making up the rest.
Milk protein can be found in:
- Canned tuna
- Sausage and other meats
- Beverage mixes
- Body-building and energy drinks
- Chewing gum
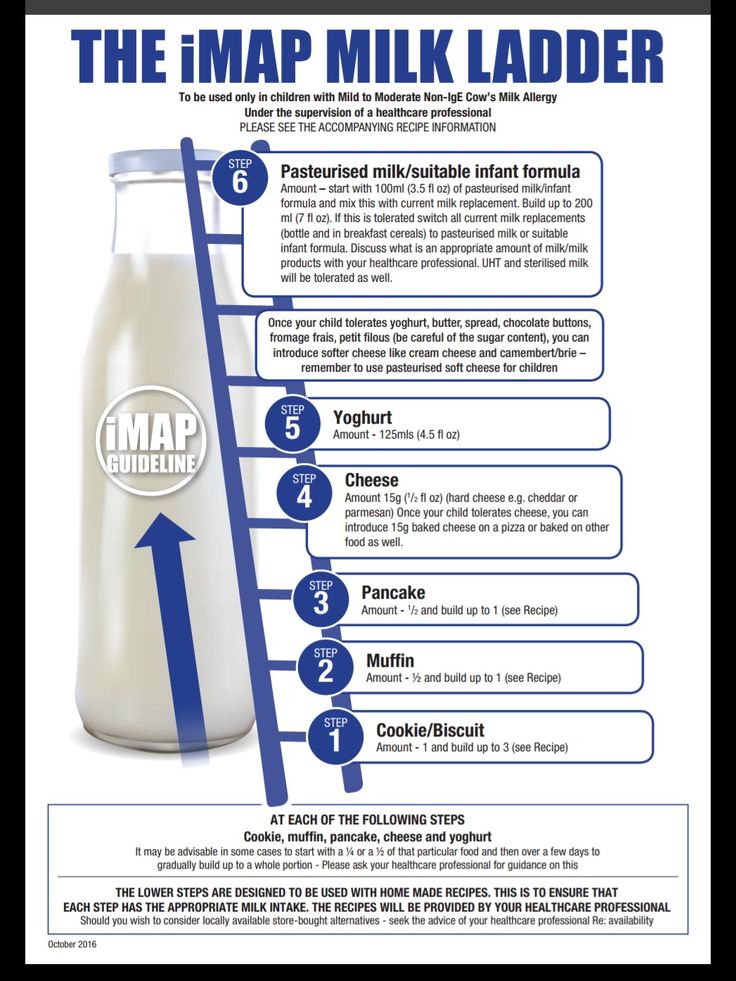
Some people with a milk protein allergy can eat foods with milk that has been extensively heated, like in a muffin.
You may ask your health care provider about meeting with a nutritionist to help ensure that you, as a nursing mother, and your children with milk protein allergies receive proper nutrition while avoiding cow’s milk protein. Cow’s milk provides calcium, vitamin D and potassium.
Preventing and Outgrowing a Milk Allergy
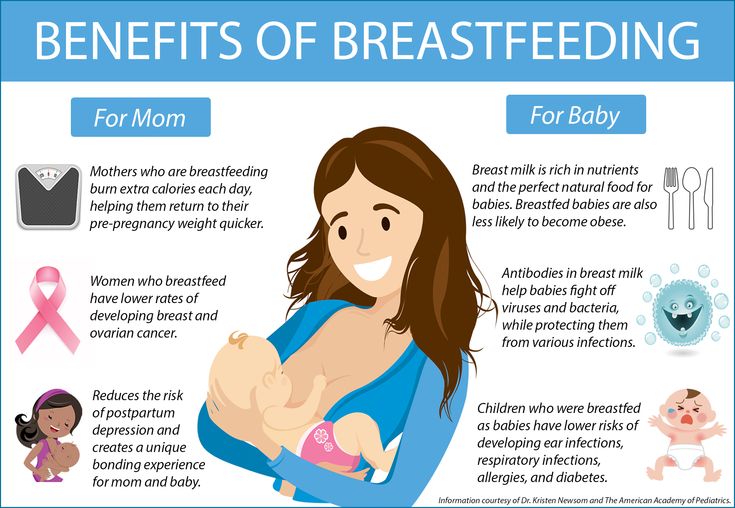
Breastfeeding appears to reduce the development of cow’s milk allergy. Doctors recommend moms breastfeed their babies for at least four months to get the most preventive benefit.
Most children with a cow’s milk allergy outgrow the condition between the ages of 2 and 5, and the allergy rarely lasts into the teen years.
If your child is diagnosed with a cow’s milk allergy, be sure to follow up with your doctor for repeat testing.
Over time, dairy foods can be reintroduced into your child’s diet under the guidance of a doctor or nutritionist. You’ll want to watch for symptoms, as you reintroduce each dairy food.
It's easy to get the care you need.
See a Premier Physician Network provider near you.
Schedule Now
Source: American Academy of Allergy, Asthma and Immunology, WhatToExpect.com, North American Society for Pediatric Gastroenterology, Hepatology and Nutrition, National Dairy Council
Small Steps: Keep Your Food Pipe Healthy
Ask your doctor about medication for controlling acid reflux to reduce wear and tear on your esophagus.
Baby Poop Is Hard After Switching To Milk (Plus What Else To Expect!)
Changing our baby’s diapers is a big part of our responsibilities as parents and, if we’re honest, is often our least favorite job. But even worse than changing yet another poopy diaper, is the concern and worry parents feel after they leave breastmilk or formula behind and we notice that their diapers suddenly contain hard poop. Is it normal for our baby’s poop to be so hard after we transition them to whole milk?
But even worse than changing yet another poopy diaper, is the concern and worry parents feel after they leave breastmilk or formula behind and we notice that their diapers suddenly contain hard poop. Is it normal for our baby’s poop to be so hard after we transition them to whole milk?
It is common to find that your baby’s poop is harder than usual after they make the switch to cow milk from breastmilk or formula. This mild constipation is due to their digestive tract adapting to the higher amount of protein compared to what they are used to. However, if it is accompanied by a fever or other symptoms is a cause for concern.
Keep reading for more information about why your baby’s poop changes when transitioning to whole milk and why it may have become hard after switching to milk from breastmilk or formula. We’ll also cover what other changes you might notice in the color and consistency of their poop. Plus, answers to your questions about what you can do to help ease the transition for your baby, and how to know if the changes you are noticing require a trip to the pediatrician.
Table of Contents
How poop changes when transitioning to whole milkAccording to the American Academy of Family Physicians, you should wait to introduce whole cow’s milk until your baby is at least twelve months old. But what should you do when you introduce your one-year-old baby to milk and notice that your baby’s poop is hard after switching to milk?
The contents of your baby’s diaper may be perfectly normal, just different from what you are used to seeing there. If you breastfed your baby before changing to whole milk, you are probably used to your baby’s poops being runny and green, brown, or mustard yellow in color and looking seedy in texture. If your baby was formula-fed, you are likely used to changing more frequent poops that are yellow, light brown, or orange in color with a consistency similar to peanut butter. Transitioning your baby from breast milk or formula to whole milk can result in changes to the color, size, and consistency of your baby’s poop.
Cow’s milk has higher levels of fat, minerals, and protein as compared to breast milk, which is easier for your baby to digest. Also, formula is often made with processed skim milk which contains less fat and protein than whole milk. When a baby first starts drinking whole milk, their poop may look hard, pale, and tan in color as their bodies adjust to the change of proteins in the milk.
Can switching to whole milk cause hard stools or constipation?Hard poop is common and normal after switching your baby to whole milk from breast milk and formula.
That hard poop you found in your baby’s diaper is likely a sign of milk protein intolerance constipation, as their digestive system is adjusting to breaking down the proteins in cow’s milk.
However, extremely firm, pebble-like stools could be a sign of dehydration and extreme constipation and require a trip to your baby’s doctor.
Can babies get diarrhea when switching to whole milk?If you have just added whole cow’s milk to your baby’s diet, a mild and short-lived case of diarrhea may be a sign of their body adjusting to the changes of more protein in their digestive system and is not normally a cause to be overly concerned.
But if you are changing blow-out diarrhea diapers frequently after introducing milk to your baby’s diet, that is not normal or healthy for your baby and you should contact your pediatrician.
It is possible that your baby has a milk allergy, which is rare, or a virus or illness unrelated to the milk, especially if they are running a fever or show other signs and symptoms of illness.
White or yellow poop after switching baby to whole milkAs parents, we spent a shocking amount of time examining our little one’s poop frequency, consistency, and color.
White poop is uncommon in babies and warrants a trip to the pediatrician, but there are a variety of conditions ranging from normal to severe that could cause your baby’s stool to be yellow in color.
If your baby has chalky white poop, it may indicate a lack of bile in your baby’s liver. White poop can be a sign that your baby is not properly digesting their food which is cause for alarm.
Yellow baby poop can be perfectly normal and healthy if you are still breastfeeding your baby or giving them formula. However, if your baby is pooping frequently and the poop is yellow, very runny, or contains mucus, your baby should be seen by a doctor. Bright yellow poop is also not a normal color for poop and can be caused by serious illness, it too should be evaluated by a doctor. Another possible cause of yellow poop is an intestinal infection which will require a trip to the doctor for a diagnosis. If your baby has an intestinal infection you would likely see other signs of illness, such as abdominal pain and diarrhea.
Baby poop color change after whole milk changeThere are a wide array of colors that can be normal and healthy when it comes to your baby’s poop after introducing whole milk, and the color of your baby’s poop can vary temporarily.
After making the change to whole milk, your baby’s poop may look pale and tan in color. If you have also recently introduced your baby to some new solid food, the presence of undigested food can cause color changes in your baby’s poop.
Healthy baby poop can be various shades of yellow, orange, brown, or green.
Undigested milk in baby stoolIf your baby is not digesting milk properly, your baby will likely have watery diarrhea after consuming milk.
Introducing your baby to whole milk for the first time also means they are consuming a different amount of lactose than they are used to. If your baby cannot digest lactose, you may also notice other signs of intolerance, such as gas, bloating, and an upset stomach.
An intolerance to lactose is not the only cause of diarrhea and you should seek an evaluation by a doctor if it continues.
What does baby poop look like with a milk allergy?The signs and symptoms of a milk allergy can range anywhere from extremely severe to mild and should be evaluated by a doctor.
If your baby has a milk allergy, he or she may have either black or red diarrhea caused by inflammation in your baby’s gut from the milk. If the poop is red and bloody, the inflammation is likely in the lower part of your baby’s gut. If it is black, it is likely from the higher part.
If the poop is red and bloody, the inflammation is likely in the lower part of your baby’s gut. If it is black, it is likely from the higher part.
Signs and symptoms of a milk allergy include:
- Vomiting
- Wheezing
- Hives
- Itching around the mouth
- Swelling of your baby’s lips, tongue, and/or throat
- Coughing
- Shortness of breath
- Diarrhea
- Watery eyes & nose
- Colic
If you notice symptoms of severe allergic reaction immediately after introducing your baby to cow’s milk, you should call an ambulance or take your baby to the hospital immediately.
How to help baby transition to milkThere are several things that we parents can do to help ease the transition to milk for our babies.
Here are some ways to help your baby transition to milk:
- Wait until your baby’s first birthday.

- Take it slowly, when you do – you can mix whole milk with equal parts breastmilk or formula and then gradually increase the ratio of whole milk to breastmilk or formula.
- Give milk as a beverage, not as a meal.
- Serve the milk warm, similar to how you would give them a bottle (or the temperature of fresh breastmilk).
Babies are fussy by nature.
After switching them to milk, it is common for babies to have to strain a little when pooping, and you may see them scrunch up their little faces in frustration when making the effort.
Excessive fussiness and frequent crying after switching to milk are not normal. Talk to your baby’s doctor about your baby starting milk and rule out other possible causes.
How long does it take for a baby to adjust to whole milk?There is no one timetable for how long a baby may take to adjust to drinking milk. Plan on giving your baby time to adjust to the change.
Plan on giving your baby time to adjust to the change.
How long it takes can vary depending on the amount they drink, how often, and how well your baby’s body is responding to it.
As long as you are following the recommendations of your baby’s pediatrician, and keeping a lookout for any symptoms of possible illness or allergy when making the switch, your baby is likely healthy and benefiting from the addition of milk to their diet.
Allergy to cow's milk protein in children
Food allergy is a food-induced adverse (pathological) reaction based on immune mechanisms. In children under one year of age, the most common cause of food allergy is cow's milk protein (CMP).
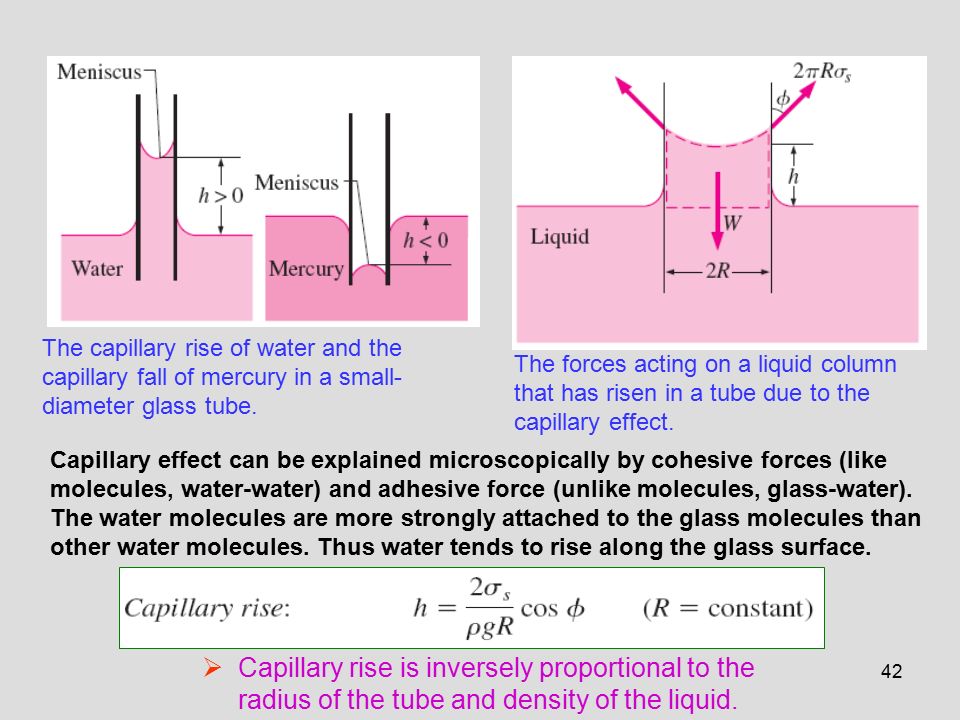
A distinction is made between cow's milk protein allergy and cow's milk protein intolerance. In the first case immune mechanisms are involved, in the second - the baby simply does not have enough enzymes to digest cow's milk protein (for example, lactase deficiency).
There are only 36 cow's milk protein allergens, but 4 of them most often cause food allergies.
Casein is 80% BCM, it is heat stable (does not break down when boiled) and is not a species-specific protein. This means that if you are allergic to it, you may be allergic to the milk of other animal species. nine0015
β - lactoglobulin has the highest allergenic activity, species-specific, not destroyed by boiling. This protein is not found in human milk.
α - lactalbumin is destroyed by boiling, species-specific.
Bovine serum albumin is not destroyed by boiling, if an allergy to this cow's milk protein is detected, the child may also react to beef and veal meat.
It should be noted that mainly children who are formula-fed formulas based on cow's milk protein suffer from allergy to cow's milk protein. nine0015
This type of allergy can also develop in children who are breastfed - if the diet of a nursing mother contains products containing cow's milk protein (milk, cheese, cottage cheese, sour cream, butter, fermented milk products), especially in large quantities.
What symptoms suggest that the baby may be allergic to CMP:
- Skin manifestations (dry skin, dry nummular rashes, skin itching). nine0060
- Gastrointestinal manifestations (bloating, regurgitation, vomiting, loose stools, possibly stools with mucus and blood streaks).
- Respiratory manifestations (itchy eyes, cough, nasal congestion and even urticaria and Quincke's edema). These symptoms are rare in toddlers, but still possible.
Diagnosis
I must say that if the first manifestations of a food allergy in a baby appeared after switching to artificial feeding with a "regular" adapted formula based on cow's milk, then this is a reason to suspect cow's milk proteins as an allergen. nine0015
nine0015
The next thing is correct history taking : the doctor will definitely find out if anyone in your family suffers from allergic diseases (bronchial asthma, allergic rhinitis, atopic dermatitis, hay fever). If the family has these diseases, the risk of developing allergies in the baby increases.
At the discretion of the doctor, it is possible to take blood from a child for the presence of immunoglobulin E (IgE) antibodies to cow's milk proteins, which were mentioned above. In the presence of IgE antibodies to CMP in the baby's blood, almost 100% confirms that he has an allergy. Paradoxically, the absence of these antibodies does not rule out an allergy to cow's milk proteins, but only indicates that the allergy proceeds through a different type of allergic reaction. nine0015
And the simplest, most important and affordable method is the diagnostic diet with the exclusion of products from the child's diet (or from the mother's diet during breastfeeding) containing CMP.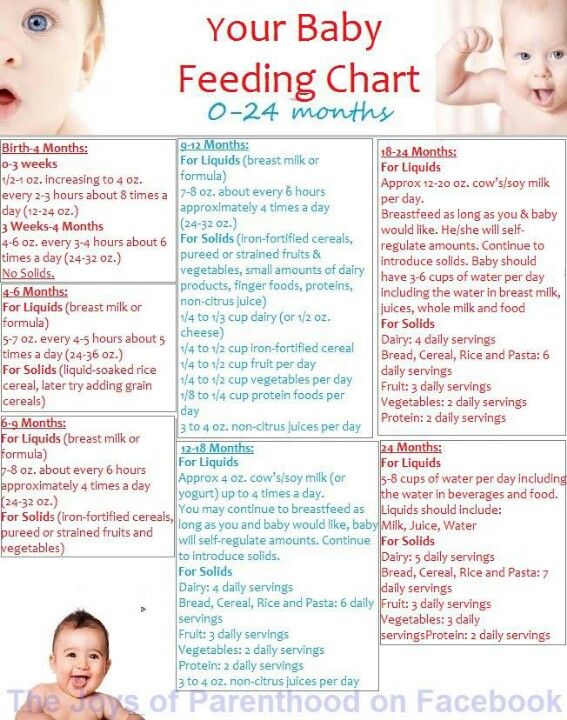 The duration of this diet is from 1-2 to 4 weeks. If during these periods there is no improvement in the condition of the baby, then an allergy to CMP is unlikely.
The duration of this diet is from 1-2 to 4 weeks. If during these periods there is no improvement in the condition of the baby, then an allergy to CMP is unlikely.
If the child's condition improves, you may need challenge test . This means the introduction of dairy products into the child's diet again. And if the manifestations of allergies return, this will prove an allergy to BCM. This test is carried out under strict medical supervision. nine0015
In children who are fed exclusively with breast milk, it is necessary to exclude products containing CMP from the mother's diet .
There are 3 types of mixtures:
- based on the hydrolysis of whey proteins;
- based on the hydrolysis of the casein fraction;
- based on amino acids.
Allergy is possible for the first two options, the reaction is very unlikely for the third option.
If the baby is bottle-fed, then it must be transferred to amino acid blend or highly hydrolyzed blend. Most infant formulas are made with whole proteins and are therefore not suitable for babies allergic to CMP. They also do not recommend hypoallergenic mixtures, since the protein in them is not sufficiently split and mixtures in goat's milk (cross-reactions).
Most infant formulas are made with whole proteins and are therefore not suitable for babies allergic to CMP. They also do not recommend hypoallergenic mixtures, since the protein in them is not sufficiently split and mixtures in goat's milk (cross-reactions).
Usually, allergists first transfer children to mixtures based on complete hydrolysis of BCM or casein, if there is no proper effect within 2-3 weeks, it is recommended to transfer the baby to an amino acid mixture. nine0015
Perhaps, if the child has severe manifestations of food allergies, the doctor will advise you to immediately transfer the baby to an amino acid mixture. By agreement with the doctor, it is possible to transfer the child to a mixture based on soy protein isolate (from 6 months).
Amino acid mixtures are more easily tolerated by children with various forms of food allergies, as they do not have the bitter taste characteristic of mixtures with a high degree of protein hydrolysis.
Amino acid mixtures can be used both for the short term diagnosis of CMP allergy and as a dietary base for long term use in children with food allergies. nine0015
Diet duration — at least 6 months . Then the issue of transferring the baby to a hypoallergenic mixture is decided. In case of recurrence of symptoms, the introduction of dairy products is postponed for another 6 months.
The prognosis for CMP allergy in infants and young children with the correct management of patients is favorable.
Approximately 50% of children by the age of 1 year can be introduced into the diet of foods that include CMP. More than 75% of children by age 3 or older 90% of children by the age of 6 do not show allergic reactions to CMP.
The introduction of complementary foods "Persona Childhood"
The most difficult and controversial issue for young parents is the introduction of complementary foods. Special journals keep returning to this topic, Internet conferences are full of questions: when, what, how and why?
Domestic and foreign pediatricians are no less actively discussing the topic of complementary foods.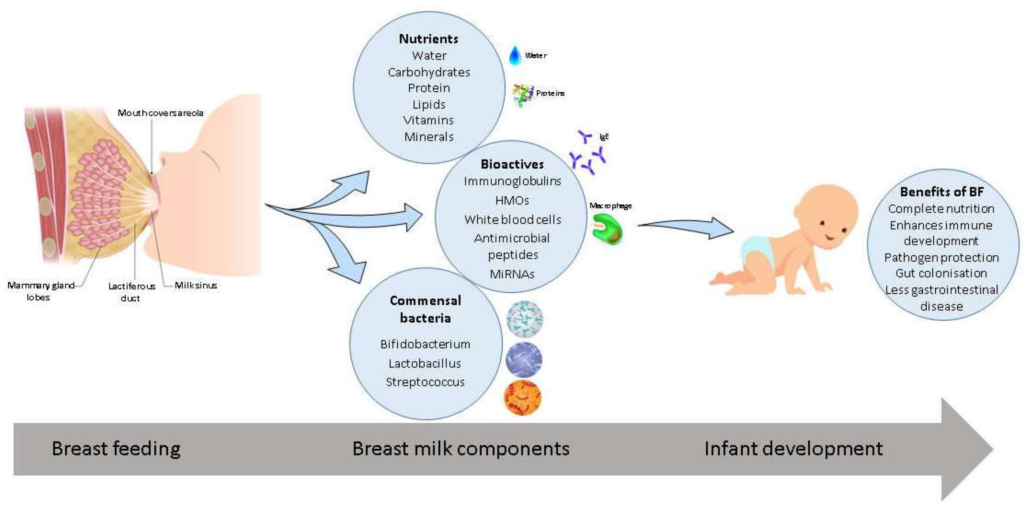 Unresolved questions remain about the timing of the start of complementary foods, and the order of introduction of certain foods. Recently, doctors in most developed countries have abandoned the practice of early introduction of complementary foods. From these positions, the timing of the introduction of complementary foods in Russia was also revised (see table). The proposed scheme is only suitable for healthy children who are breastfed. nine0015
Unresolved questions remain about the timing of the start of complementary foods, and the order of introduction of certain foods. Recently, doctors in most developed countries have abandoned the practice of early introduction of complementary foods. From these positions, the timing of the introduction of complementary foods in Russia was also revised (see table). The proposed scheme is only suitable for healthy children who are breastfed. nine0015
After 4-6 months of breastfeeding, the nutritional value of milk gradually decreases, and the baby's appetite increases, and his need for basic nutrients is unmet. Sometimes mothers note that a 4-6-month-old baby, even after sucking out enough milk before, begins to act up, show anxiety, wake up at night shortly after feeding. At the age of six months, the baby shows interest in the "adult table": the child's body needs additional sources of nutrition. By this time, the teeth usually begin to cut, and the baby's gastrointestinal tract is fully prepared for the perception of new types of food. nine0015
nine0015
The period of transitional nutrition, that is, the introduction of complementary foods, is the time of a gradual transition from mother's milk to the type of complex nutrition that will support the body of a child, and then an adult, for all subsequent years. This is a very important stage in the life of a baby, because in order to develop mature feeding skills, he must move from breast sucking to more and more complex work: learn to roll food with his tongue, swallow thick food, chew, bite off a large piece. If the child is not taught this in time, then he may have problems in the assimilation of "adult" food, against which even functional disorders in the gastrointestinal tract are possible. We can say that the period of introduction of complementary foods is the first step towards growing up a baby. nine0015
Basic rules for the introduction of complementary foods
1. The timing and sequence of introduction of complementary foods depends on the characteristics of the child's development, so it is better to discuss them with a nutritionist or pediatrician.
2. Any new product should be introduced little by little (starting with 5-10 g). With good swallowing and assimilation of complementary foods, the absence of an allergic reaction to the product, it can be offered regularly, gradually increasing the volume to the recommended dose in 1-2 weeks. nine0015
3. Complementary foods should be given before breastfeeding (with the exception of fruit juices).
4. It is better to use commercially produced baby food, as it is prepared from clean, environmentally friendly products and enriched with vitamin and mineral complexes.
5. You should not enter puree or cereals from several components at once. To begin with, it is better to adhere to the principle of monocomponent, so that, if necessary, it is easier to identify the cause of an allergic reaction. Gradually, the child's diet can be expanded by adding each new component within 4-5 days. nine0015
If the child does not have food allergies and intestinal problems, then the first food supplement may be fruit juice . At first they offer, as a rule, apple juice, starting with a few drops. If you prefer homemade juices, use only green apples. Dilute natural juice with boiled water in a ratio of 1:1. Any juice is best given during or after feeding.
When choosing juices, consider their specific properties. Cherry, pomegranate, blackcurrant, blueberry juices contain tannins and have a fixing effect. They can be used if the baby has an unstable stool. For crumbs with a tendency to constipation, carrot, beetroot, apricot, plum juices are useful. It is better not to give grape juice at all, because it contains a lot of sugar, which enhances the fermentation processes in the intestines. You should also be careful with strawberry and citrus juices: they often cause an allergic reaction. nine0015
Approximate scheme for the introduction of products and dishes of complementary foods during breastfeeding of children of the first year of life
| Name of products and dishes | Age, months | |||||||
| 0-3 | 3 | 4 | five | 6 | 7 nine0184 | 8-9 | 9-12 | |
| Fruit juice, ml | - | 5-30 | 40-50 | 50-60 | 60 | 70 | 80 | 90-100 |
| Fruit puree, g nine0184 | - | 5-30 | 40-50 | 50-60 | 60 | 70 | 80 | 90-100 |
| Vegetable puree, g | - | - | 10-100 nine0184 | 150 | 150 | 170 | 180 | 200 |
| Milk porridge, g | - | - | - | 50-100 | 150 | 150 nine0184 | 180 | 200 |
| Curd, g | - | - | - | 10-30 | 40 | 40 | 40 | fifty |
Yolk, pcs. nine0184 nine0184 | - | - | - | - | 0.25 | 0.25 | 0.25 | 0.5 |
| Meat puree, g | - | - | - | nine0189 -- | 5-30 | fifty | 60 | |
| Fish puree, g | - | - | - | - | - | - | 5-30 nine0184 | 30-60 |
| Kefir, other fermented milk products, "follow-up mixtures", ml | - | - | - | - | - | 200 | 200 | 400-500 |
| Whole milk, ml nine0184 | - | - | 100 | 200 | 200 | 200 | 200 | 200 |
| Crackers, cookies, g | - | - | - | nine0189 -3-5 | five | five | 10-15 | |
| Wheat bread, premium, g | - | - | - | - | - | five | five nine0184 | 10 |
| Vegetable oil, g | - | - | 1-3 | 3 | 3 | five | five | 6 |
| Butter, g | - | - | - | 1-4 | 4 | 4 | five | 6 |
Fruit puree is offered two weeks after fruit juice administration.
Of the vegetables , it is better to prefer zucchini or cauliflower to begin with. If you are making your own puree, you need to be sure that the products are safe. When the child gets used to the first products, the assortment of vegetables should be expanded, gradually introducing carrots, potatoes, pumpkins, turnips, and beets. In vegetable puree, depending on age, it is good to add yolk, vegetable oil, milk, meat puree. For a week, the amount of vegetable puree can be increased to 100-150 g per day, replacing one of the breastfeedings with it. At the age when vegetable complementary foods begin (4.5-5.5 months), the child usually switches to a five-time diet. nine0015
Another breastfeeding is gradually replaced with the start of porridge . Cereals from various cereals contain a large amount of a substance called gluten (gluten). The intestinal microflora in an infant is not yet fully formed, it may lack an enzyme that breaks down gluten. Products of incomplete breakdown of gluten have a toxic effect on the intestinal walls, so preference should be given to cereals that do not contain gluten - rice, buckwheat, corn. Later, you can introduce both wheat (semolina) and oatmeal porridge. In the finished dish you need to add butter. If you are allergic to cow's milk, cook cereals in vegetable broth or dilute them with a special mixture (soy or based on milk protein hydrolyzate). nine0015
Products of incomplete breakdown of gluten have a toxic effect on the intestinal walls, so preference should be given to cereals that do not contain gluten - rice, buckwheat, corn. Later, you can introduce both wheat (semolina) and oatmeal porridge. In the finished dish you need to add butter. If you are allergic to cow's milk, cook cereals in vegetable broth or dilute them with a special mixture (soy or based on milk protein hydrolyzate). nine0015
The introduction of meat puree is also best to start with one type of meat. It is advisable to buy meat puree of industrial production without vegetable additives in order to know exactly the amount of meat eaten by the child. If mashed potatoes are prepared at home, the meat should be subjected to double digestion: boil for 20 minutes, then drain the broth, pour hot water over the meat again and cook until tender. Meat Broth is not recommended for children under 2 years of age.
Approximately one month after the introduction of meat puree into the child’s diet, you can start giving him fish (puree).