Black dry patches on skin
Acanthosis nigricans - NHS
Acanthosis nigricans is the name for dry, dark patches of skin that usually appear in the armpits, neck or groin. It could be a sign of an underlying condition, so it needs to be checked by a GP.
Check if you have acanthosis nigricans
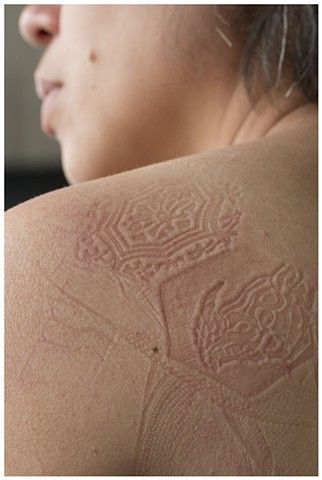
The main symptom of acanthosis nigricans is patches of skin that are darker and thicker than usual.
They can appear anywhere on the body.
The patches are dry and feel similar to velvet.Credit:
Benedicte Desrus / Alamy Stock Photo https://www.alamy.com/stock-photo-childhood-obesity-in-mexico-37878235.html?pv=1&stamp=2&imageid=D82F3D1E-88DD-48FC-8591-AE73FADBC974&p=68490&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3dbar%26st%3d0%26pn%3d1%26ps%3d100%26sortby%3d2%26resultview%3dsortbyPopular%26npgs%3d0%26qt%3dC5HE23%26qt_raw%3dC5HE23%26lic%3d3%26mr%3d0%26pr%3d0%26ot%3d0%26creative%3d%26ag%3d0%26hc%3d0%26pc%3d%26blackwhite%3d%26cutout%3d%26tbar%3d1%26et%3d0x000000000000000000000%26vp%3d0%26loc%3d0%26imgt%3d0%26dtfr%3d%26dtto%3d%26size%3d0xFF%26archive%3d1%26groupid%3d%26pseudoid%3d%26a%3d%26cdid%3d%26cdsrt%3d%26name%3d%26qn%3d%26apalib%3d%26apalic%3d%26lightbox%3d%26gname%3d%26gtype%3d%26xstx%3d0%26simid%3d%26saveQry%3d%26editorial%3d1%26nu%3d%26t%3d%26edoptin%3d%26customgeoip%3d%26cap%3d1%26cbstore%3d1%26vd%3d0%26lb%3d%26fi%3d2%26edrf%3d0%26ispremium%3d1%26flip%3d0%26pl%3d
They're most common in skin folds, such as the armpits, neck or groin.Credit:
CID, ISM /SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/459432/view
Some people also have tiny growths (skin tags) on the patches.Credit:
ANDRE LABBE, ISM/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/886025/view
The patches often appear gradually without any other symptoms.
Sometimes the skin may be itchy.
Non-urgent advice: See a GP if you have:
- new dark patches on your skin
- any skin changes you're unsure about
What happens at your appointment
Although acanthosis nigricans is usually harmless, it's best to get any skin changes checked out.
Rarely, it can be a sign of something more serious, such as cancer.
A GP can usually tell if it's acanthosis nigricans by looking at your skin.
You may need some tests to find out what's causing the patches.
Causes of acanthosis nigricans
The most common cause of acanthosis nigricans is being very overweight.
Other causes include:
- type 2 diabetes
- conditions that affect hormone levels – such as Cushing's syndrome, polycystic ovary syndrome or an underactive thyroid
- taking certain medicines – including steroids or hormone treatments like the contraceptive pill
- rarely, cancer – usually stomach cancer
- rarely, a faulty gene inherited from your parents
Sometimes healthy people with no other conditions get acanthosis nigricans. This is more common in people with black or brown skin.
This is more common in people with black or brown skin.
Treating acanthosis nigricans
Once a GP knows what's causing acanthosis nigricans, they can recommend the best treatment.
The patches should fade over time once the cause is treated.
If you're very overweight, a GP may recommend losing weight.
Depending on the cause, they may also recommend:
- medicine to balance your hormones
- medicine to balance your insulin levels
- changing your medicine to one that does not cause the patches
There's no specific treatment for the patches themselves. A skin specialist (dermatologist) may be able to suggest treatments to improve their appearance, but finding and treating the cause is usually recommended first.
Page last reviewed: 20 June 2021
Next review due: 20 June 2024
Skin Discoloration: Causes, Pictures, and Treatment
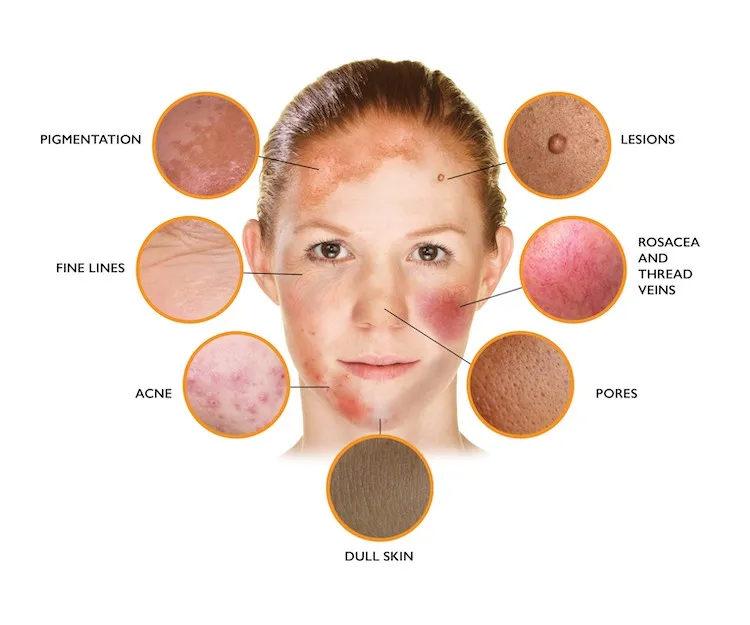
Skin discoloration is a broad term that describes any change in your skin that differs from your natural skin tone. These areas of discolored skin can range in color and may be:
- red
- pink
- purple
- tan
- brown
- black
- blue
While there are many harmless causes of skin discoloration, such as birthmarks, some cases of discolored skin may develop from an underlying medical condition that requires diagnosis and treatment.
Discolored skin patches may also commonly develop on certain body parts due to a difference in melanin levels. Melanin is the substance that provides color to the skin and protects it from the sun. When there’s an overproduction of melanin, it can cause differences in skin tone.
Another possibility is skin cancer, which must be addressed with a dermatologist right away.
In this article, we cover several possible causes of skin discoloration along with pictures so you can discuss any concerns you have with your doctor.
There are many potential causes of skin discoloration, ranging from minor problems to more serious medical conditions. These may include:
- birthmarks, which are discolored skin spots that may be present at, or shortly after, birth
- pigmentation disorders, such as melasma, albinism and vitiligo
- medical conditions, such as rosacea, psoriasis, and Graves‘ disease
- infections from harmful bacteria, viruses, or fungi
- allergies, which may lead to hives or eczema rashes
- skin cancer, which develops from damaged skin cells that become malignant (cancerous)
- other causes, such as burns and medication side effects
Let’s look at these potential causes of skin discoloration in more detail.
Birthmarks
Birthmarks are discolored skin spots that can develop at birth or soon after birth. They are typically harmless and don’t require treatment unless they become bothersome or painful.
Some common types of birthmarks include:
- Moles. Moles can appear on the skin at birth. They can range in color from tan, brown, or black, to red, purple, and blue. Some moles may even be the same color as your skin. Most moles aren’t a cause for concern, but any changes in the size or shape of a mole can signal trouble and should be checked by a healthcare professional.
- Dermal melanocytosis (formerly Mongolian blue spots). Bluish patches that can appear on the backs of babies and young children, usually in those of Asian descent. These blue spots are harmless and often fade over time.
- Port-wine marks. Port-wine marks are flat patches that appear pink or red on lighter skin tones, dark-purple or violet-red on darker skin tones.
 They are caused by swollen blood vessels under the skin.
They are caused by swollen blood vessels under the skin. - Salmon patches. Salmon, red, or pink-colored patches that may develop on a baby’s face or neck. This birthmark tends to go away on its own by ages 1 to 3.
- Strawberry nevus (hemangioma). A red birthmark that’s common in young children and infants. This birthmark usually fades by age 10.
- Deep hemangioma. This type of birthmark also tends to disappear by age 10. It appears as a purple- or blue-tinted lump under the skin that may require treatment if it’s painful or if it breaks open and bleeds.
- Hypopigmented macule. A spot of skin that’s lighter than the rest of your body and tends to go away over time.
- Café au lait spots. Spots of skin that are much darker than the rest of the body. Unlike a hypopigmented macule, this type of birthmark remains for life.
Pigmentation disorders
Pigmentation disorders can cause changes in your skin that are either lighter (hypopigmentation) or darker (hyperpigmentation) than your natural skin tone. While usually harmless, more extensive pigmentation changes may lead someone to get aesthetic treatments.
While usually harmless, more extensive pigmentation changes may lead someone to get aesthetic treatments.
Common pigmentation disorders include:
- Vitiligo. This chronic (long-term) condition causes large patches of hypopigmentation on your skin. While vitiligo can develop at any age, it typically begins before age 20.
- Albinism. Albinism is an inherited condition that leads to the development of extremely light skin, eyes, and hair due to a lack of melanin.
- Melasma. Nicknamed “the mask of pregnancy” due to the involvement of progesterone and estrogen, melasma is a type of hyperpigmentation that causes darker spots of skin on the face and abdomen. It usually fades and gets lighter once you stop taking birth control pills or after pregnancy. Certain amounts of sun exposure can cause it to return.
- Age or “liver“ spots (lentigo). These are common hyperpigmentation spots caused by sun damage.
 Age spots can develop anywhere on the body, but they tend to affect sun-exposed areas, such as your hands, chest, and face.
Age spots can develop anywhere on the body, but they tend to affect sun-exposed areas, such as your hands, chest, and face.
Medical conditions
The immune system normally works to keep the body healthy by fighting off harmful agents that can cause infection and disease.
In people with autoimmune diseases, however, the immune system confuses healthy cells for something foreign and attacks them by mistake. This triggers inflammation throughout the body, resulting in various symptoms, including swelling and redness.
Some autoimmune diseases and other medical conditions that may lead to symptoms of skin discoloration include:
- Psoriasis. Psoriasis is a chronic skin condition characterized by itchy patches of red to silvery scales that are caused by an increase in skin cell turnover.
- Rosacea. This condition may cause skin flushing and redness. Some types of rosacea may also cause acne pustules, ocular (eye) symptoms, and thickened skin.
- Lupus. Lupus can affect the skin as well as other areas in your body, including your joints and major organs.
- Stasis ulcer. A type of leg ulcer that often coincides with varicose veins and venous insufficiency, leading to redness, swelling, and pain.
- Graves’ disease. A type of thyroid disease that causes your body to produce too many thyroid hormones. Related skin symptoms may include areas of rough, thickened, red skin.
- Addison’s disease. This adrenal insufficiency condition may cause areas of hyperpigmentation in the skin. You may also be at an increased risk of developing vitiligo.
- Scleroderma. Scleroderma is a rare autoimmune disorder that may cause patches of thick, discolored skin, as well as problems with connective tissues.
Infections
Various infections can cause changes in skin color in the affected area.
Infections that may lead to discolored skin include:
- Bacterial infections.
 Cuts, scrapes, and other wounds may become infected when bacteria enter, resulting in changes in the texture of your skin. The surrounding area may also turn red or white, and the wound itself may have discharge. Topical or oral antibiotics may be prescribed for these types of skin infections.
Cuts, scrapes, and other wounds may become infected when bacteria enter, resulting in changes in the texture of your skin. The surrounding area may also turn red or white, and the wound itself may have discharge. Topical or oral antibiotics may be prescribed for these types of skin infections. - Fungal infections. Fungal infections, such as ringworm, tinea versicolor, and candida, can also trigger discolored skin patches on various parts of the body. Topical or oral fungal treatments may be used for these conditions.
- Viral infections. Viral infections, such as shingles, cold sores, and warts, may lead to red, purple, or brown bumps or sores. Antiviral treatments may be used for certain types of infections.
Rashes and allergies
Allergic reactions to foods, plants, or irritants can also result in discolored skin patches in various areas of the body. These changes may appear as rashes or raised bumps that itch or burn and can occur in the following:
- Eczema (atopic dermatitis).
 Like certain autoimmune diseases, eczema triggers an immune reaction that attacks the skin. The condition can cause scaly patches and red bumps that ooze or crust over.
Like certain autoimmune diseases, eczema triggers an immune reaction that attacks the skin. The condition can cause scaly patches and red bumps that ooze or crust over. - Contact dermatitis. Contact dermatitis is another type of allergic skin rash that can develop when you come into contact with fragrances, skin care products, metals, or clothing that irritates your skin. Contact dermatitis rashes are often itchy and sometimes even painful.
- Hives (urticaria). These raised, itchy bumps on the skin are the result of inflammation from your body releasing histamine (a compound involved in immune responses) in response to an allergen. While usually acute, some cases of hives can be chronic, lasting for months or even years.
Skin cancer
Cancer can change the skin’s color or texture. Skin cancer may occur when the genetic material in skin cells becomes damaged, often from long-term sun damage or exposure to chemicals. The damage may cause the cells to grow out of control and form a mass of cancer cells.
The damage may cause the cells to grow out of control and form a mass of cancer cells.
There are several types of skin cancer, all of which require treatment:
- Actinic keratosis. A precancerous skin condition characterized by scaly, crusty spots on the hands, arms, or face. These spots are typically brown, gray, or pink. The affected area may itch or burn.
- Basal cell carcinoma. The most common form of skin cancer, basal cell carcinoma affects the top layer of skin. It most often appears in sun-exposed areas. In the early stages, it produces lesions that bleed. The associated bumps may be discolored, shiny and pearly, or scar-like. They can look like open sores and often have slightly higher edges with an indentation in the middle.
- Squamous cell carcinoma. A type of skin cancer that begins in the squamous cells. These cells make up the outermost layer of skin. This condition causes scaly, red patches and raised sores, which are also often seen on sun-exposed areas of the skin.

- Melanoma. This is the least common but most serious form of skin cancer. Melanoma begins as an atypical mole. Cancerous moles are often asymmetrical, multicolored, and large. They can appear anywhere on the body, but they usually first appear on the chest or back in people assigned male at birth and on the legs in people assigned female at birth.
Most discolored skin patches aren’t caused by skin cancer. However, you should ask a healthcare professional to examine any misshapen moles or other rapidly changing skin lesions.
Other causes of skin discoloration
Other conditions and medical treatments that can cause skin discoloration include:
- Bleeding into the skin. This happens when blood vessels burst due to injury, bruising, or an allergic reaction.
- Radiation therapy. Radiation therapy is a cancer treatment that can cause the skin to blister, itch, and peel.
- Spider veins.
 Damaged veins that can appear as clusters of red, blue, or purple lines underneath your skin, particularly in your legs.
Damaged veins that can appear as clusters of red, blue, or purple lines underneath your skin, particularly in your legs. - Hormonal changes. Hormonal changes may cause the development of melasma hyperpigmentation.
- Burns. Skin discoloration can occur from burns such as those associated with injuries and sunburns.
- Medication side effects. Drug-induced hyperpigmentation may occur in some people taking antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and other drugs.
You should schedule an appointment with a doctor if you:
- have any lasting changes in your skin color
- notice a new mole or growth on your skin
- have an existing mole or growth that changed in size or appearance
- have any other concerning symptoms, such as pain, inflammation, or discharge
At your appointment, your doctor will first take a look at areas of skin discoloration and ask you about any changes you’ve noticed. They will also ask about other symptoms you may be experiencing.
They will also ask about other symptoms you may be experiencing.
Depending on your doctor’s findings during the physical exam, they may order further diagnostic testing to determine the cause of skin discoloration. While the exact tests may vary with each potential cause of discolored skin, the options may include:
- blood tests to check for conditions that may cause changes in skin color
- a Wood’s lamp examination to identify possible fungal or bacterial infections
- a skin biopsy to examine a small sample of the affected skin under a microscope for the presence of abnormal cells
Treatment for discolored skin patches depends on the underlying cause. If a healthcare professional finds an underlying health condition, they will attempt to treat that particular condition first.
Any active infection must be treated with the appropriate class of drugs. For example, antibiotics can treat bacterial infections, while antifungal medications treat fungal infections.
If you choose to seek treatment for cosmetic reasons, a dermatologist may recommend over-the-counter or prescription topical treatments to reduce signs of skin discoloration. Professional treatments, such as chemical peels or microdermabrasion, may also be used to help reduce hyperpigmentation, but these aren’t usually covered by insurance.
It’s important to ask your doctor before trying any topical treatments or home remedies that supposedly treat skin discoloration. You should always get a correct diagnosis first.
While many cases of skin discoloration are harmless, any unusual changes in your skin can be concerning. Some causes of discolored skin patches are fairly minor conditions that only need simple treatments. Other causes may be more severe and require ongoing treatment.
It’s important to speak with a doctor about any skin changes that are unusual or bothersome, especially if you notice sudden symptoms or rapid changes in your skin. These could be an indication of a more serious condition.
Your doctor will diagnose the cause of your discolored skin and recommend treatments as appropriate. If skin discoloration is linked to an underlying medical condition, keep in mind that skin symptoms may not go away until the medical condition is first addressed.
Dry spots on the skin: three common dermatological diseases
July 5, 2020
Dry spots on the skin are a common dermatological symptom that can indicate both a temporary failure and a violation of the barrier functions of the epidermis, and a skin disease. It all depends on the size of the spots, the clarity of their boundaries, as well as the duration of their presence on the skin.
The causes of dryness can be divided into two large groups:
- non-specific - allergic reactions to household chemicals, laundry soap, cosmetic products, dehydration due to cold and wind;
- specific - then the spots become a manifestation of dermatological diseases.

Sometimes a person may notice that dry spots appear on his skin after a certain event occurs, for example, after washing clothes with his hands. Then the reason is obvious and easy to eliminate. But if dry spots on the skin do not go away, itch, peel off, you should consult a doctor.
Dry spots with scales
Pink raised dry spots on the body and head may indicate psoriasis. With this dermatological pathology in humans, raised plaques appear on the skin - psoriatic papules. They protrude above the surface of the skin, cause intense itching and flake, tend to spread and merge.
Psoriasis is a chronic autoimmune disease in which rashes are most often localized on the elbows, head, knees and groin. Dry pink spots covered with white scales are foci of chronic inflammation. Under the influence of internal autoimmune processes, epidermal cells divide several times faster than necessary. As a result, small scales are constantly separated from dying skin cells.
Atopic dermatitis and its differences from psoriasis
Atopic dermatitis can also cause dry patches on the body. And as with psoriasis, they cause itching. Due to the increased sensitivity of the skin to environmental factors, the mechanisms of its self-regulation are violated, including the barrier function. That is, an allergy is a trigger for atopic dermatitis, but the tendency to such a skin reaction is genetically laid down.
Most often, atopic dermatitis occurs in children. The disease has a chronic course, when exacerbations are replaced by periods of remission. Here are the typical signs of atopic dermatitis:
- dry skin;
- peeling and redness of the eyelids;
- dry skin-colored plaques on the trunk and extensor areas of the body;
- cracks.
It is difficult for a person who does not have a medical education to distinguish psoriasis from atopic dermatitis, but a doctor can easily make a differential diagnosis. There are several differences that may speak in favor of a particular pathology. Atopic dermatitis often affects children, psoriasis can debut in adulthood. Psoriatic plaques are raised above the skin, and scales can be seen. Dry spots in atopic dermatitis are flat. It is also important to consider typical localization.
There are several differences that may speak in favor of a particular pathology. Atopic dermatitis often affects children, psoriasis can debut in adulthood. Psoriatic plaques are raised above the skin, and scales can be seen. Dry spots in atopic dermatitis are flat. It is also important to consider typical localization.
Useful links: State Center of Urology in Moscow - Clinic of Urology named after R. M. Fronshtein of the First Moscow State Medical University named after I.M. Sechenov
Dry eczema
Sometimes white, dry, scaly patches on the skin of the legs can indicate dry eczema. With this disease, dryness and tightness of the skin first occurs, then peeling and unbearable itching join, cracks may occur. In addition to the legs, the hands, the space between the fingers, and even the face are often affected.
Dry eczema can be caused by bacterial and fungal infections, allergens, synthetic clothing, poor hygiene, and other factors.
As you can see, the appearance of dry spots on the skin can be due to a variety of reasons. An important role is played by the features of the immune system and the tendency to allergic reactions. But in any case, when dry spots appear, it is important to contact a dermatologist and establish the cause of this skin condition.
July 5, 2020
Author of the article: dermatologist Mak Vladimir Fedorovich
ask a question make an appointment
Plaques on the skin - causes, what diseases it occurs in, diagnosis and treatment
- INVITRO
- Library
- Symptoms
Fungus
Allergy
Psoriasis
Keratoma
Mycosis
Nevus
Melanoma
4164 November 16
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment.
 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. Plaques on the skin: the causes of occurrence, in what diseases they occur, diagnosis and methods of treatment.
Definition
A plaque is a pathological element with clear edges that rises above the skin surface or merges with it, more than 5 mm in size.In dermatology, many types of plaques are distinguished - about 70 diseases occur with the formation of these elements, which makes the plaque one of the most common rashes.
Plaque varieties
The shape of the plaques are round, oval and irregular in shape. Over time, the shape, surface and appearance of this element may change.Due to the occurrence of plaques, they can be both a manifestation of skin diseases and a symptom of diseases of internal organs and systems (autoimmune reactions, liver diseases, oncological processes, allergic reactions).

Plaques are dry, smooth, red, brown, gray-white, etc.
Possible causes of plaques
Dry plaques on the skin in adults can be a manifestation of the following diseases:
- Fungal infection of the skin, accompanied by plaques with severe itching.
- Allergic reactions are characterized by the appearance on the skin of smooth dry plaques, pink spots, blisters, which are very itchy and cause severe discomfort. They can develop both when the skin comes into contact with the allergen, and when it gets on the mucous membranes (for example, with urticaria, hay fever, food and contact allergies).
- Psoriasis is a chronic non-infectious skin disease in which scaly dry plaques form on the elbows, knees, scalp, prone to fusion and accompanied by mild itching.
- Dry plaques form on the skin if it is exposed to stress for a long time with the loss of its protective functions.
- Diseases of the digestive tract, accompanied by malabsorption syndrome (impaired absorption of vitamins and trace elements in the small intestine), chronic diseases of the liver and other organs, in which substances that are not normally present in the dermis accumulate, also lead to the appearance of dry plaques.
- Solar keratoma is a precancerous condition, which is characterized by the presence of many light grayish plaques on the skin.
The appearance of red plaques on the skin indicates their good blood supply. Possible causes of this condition may be the following nosologies:
- Drug toxidermia is an allergic reaction accompanied by the appearance of elements in the form of plaques on the skin. In severe cases, Lyell's syndrome or Stevens-Johnson syndrome, toxic epidermal necrolysis, may develop.
- Dühring's dermatitis (herpetiformis) is a chronic skin disease without an established etiology, which is characterized by recurrent appearance of a rash of various morphologies on the skin, accompanied by severe skin itching and burning.

- Mycosis fungoides is a primary T-cell lymphoma of the skin, a malignant lymphoid lesion, primarily of the skin. Itchy red plaques appear on the skin, resembling eczema. In the initial stages, they respond well to treatment with hormonal ointments, but the disease itself requires more complex therapy.
- In children, the appearance of red spots and plaques on the skin is most often associated with an allergic reaction to food.
Brown plaques occur when melanin is deposited in the affected area of the dermis, which causes a brown (dark) color. Possible causes may be the following diseases:
- Becker's nevus is an anomaly in the development of the dermis, when dark plaques with an uneven surface appear on the skin, on which hair can begin to grow over time.
- Pigmentary nevus - "birthmark", may rise above the skin, has a brown or dark color.
- Melanoma is the most malignant skin tumor characterized by rapid metastasis.
 It develops mainly from nevi and moles. If the nature of the surface, the boundaries of the mole change, its size increases, bleeding occurs, you should immediately contact a dermatologist or oncologist to exclude the development of melanoma.
It develops mainly from nevi and moles. If the nature of the surface, the boundaries of the mole change, its size increases, bleeding occurs, you should immediately contact a dermatologist or oncologist to exclude the development of melanoma. - Basal cell skin cancer is more often localized on the head, face, neck, does not metastasize, is characterized by slow growth.
- Senile keratoma occurs in the elderly, most likely due to a lack of vitamins, an abundance of animal fats consumed, skin sensitivity to ultraviolet radiation due to a violation of its protective functions. Typical localization - face, neck, open areas of the body.
- Seborrheic keratoma is a yellowish plaque on the skin that, over time, transforms into a dark brown growth that tends to flake off, itch severely, crack, bleed, and can serve as an entrance gate for infection.
Which doctors to contact
With the formation of plaques on the skin, it is necessary to contact a dermatologist to determine the causes of the appearance of this element of the rash.

Diagnostics and examinations for plaques
For the diagnosis of fungal skin lesions, scraping from the affected area is used for subsequent microscopic examination.The development of an allergic reaction requires seeking medical help to identify the allergen, prescribing antihistamines, and sometimes hormonal drugs. In clinical cases of allergy, along with skin tests, analyzes are performed using various sets of common allergens and triggers: a panel for respiratory allergens, for food allergens, and for a combination of both.
Respiratory Panel
Synonyms: Comprehensive Respiratory Allergen Test Panel; Respiratory allergens panel, Allergen respiratory profile, Allergy testing. Brief description of the study "Panel respira...
Up to 5 business days
Available with home visit
5 515 RUB
Add to cart
Food Panel, IgE
Food Allergen Panel: hazelnut, peanut, Walnut, almond, cow's milk, egg white, egg .
 ..
.. Up to 5 working days
Available with home visit
5 515 RUB
Add to cart
Food and Respiratory Panel
Panel different allergens: A mixture of grass allergens: fragrant spikelet; perennial rye; timothy; rye cultivated; Woolly buckthorn (GP3) IgE ...
Up to 5 business days
Available with home visit
5 515 RUB
Add to cart
In psoriasis, a visit to a dermatologist and rheumatologist will help reduce the severity of the manifestations of the disease, if appropriate therapy is prescribed.
 For the diagnosis, it is usually sufficient to examine, determine, the skin manifestations of psoriasis are so characteristic, but if necessary, a differential diagnosis is carried out, including a clinical blood test, feces for the presence of worm eggs and protozoa, and a histological examination of the skin.
For the diagnosis, it is usually sufficient to examine, determine, the skin manifestations of psoriasis are so characteristic, but if necessary, a differential diagnosis is carried out, including a clinical blood test, feces for the presence of worm eggs and protozoa, and a histological examination of the skin. Clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes)
Synonyms: Complete blood count, UAC. Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram. Brief description of the study CBC: general...
Up to 1 business day
Available with house call
RUB 810
Add to cart
Fecal analysis for helminth eggs (helminth eggs)
Synonyms: Feces on worm eggs; Analysis of feces for eggs of worms.
 Ova and Parasite Exam; O&P; Stool O&P test. Brief description of the study "Analysis of feces for eggs of helminths&ra...
Ova and Parasite Exam; O&P; Stool O&P test. Brief description of the study "Analysis of feces for eggs of helminths&ra... Up to 1 business day
Available with home visit
RUB 570
Add to cart
Fecal analysis for protozoa (PRO stool)
Synonyms: Analysis of faeces for protozoa. Parasite Exam, feces; Parasitic Examination, fecal. Brief description of the study "Analysis of feces for protozoa" Analysis of feces for cis...
Up to 1 business day
Available with home visit
RUB 570
Add to cart
Histological examination of biopsy material and material obtained during surgical interventions (endoscopic material; tissues of the female reproductive system; skin, soft tissues; hematopoietic and lymphoid tissue; bone and cartilage tissue)
Taking biomaterial is paid separately.
 According to the requirements of clause 17 of the Rules for conducting pathological and anatomical studies, approved. Order of the Ministry of Health of Russia...
According to the requirements of clause 17 of the Rules for conducting pathological and anatomical studies, approved. Order of the Ministry of Health of Russia... Up to 5 business days
Available with home visit
2 880 RUB
Add to cart
Diseases of the stomach and intestines can also lead to plaque formation on the skin. To identify the pathology of the gastrointestinal tract, it is enough to refer to therapist or gastroenterologist, conduct a number of endoscopic examinations (gastroscopy, and, if necessary, colonoscopy), ultrasound of the abdominal organs, perform some screening blood tests for diseases of the liver, intestines, stomach.
Gastroscopy
Examination of the mucosa of the upper gastrointestinal tract with the possibility of biopsy or endoscopic removal of small pathological .
 ..
.. RUB 4,440 Sign up
Colonoscopy
Endoscopic examination of the large intestine to look for abnormalities, perform biopsies, and remove small polyps and tumors.
RUB 5,740 Sign up
Comprehensive ultrasound examination of the abdominal organs (liver, gallbladder, pancreas, spleen)
Scanning of the internal organs of the abdominal cavity to assess its functional state and the presence of pathology.
RUB 2,890 Sign up
Liver function tests: screening
Up to 1 business day
Available with home visit
RUB 1,935
Add to cart
Diagnosis of celiac disease: intolerance to cereal proteins (gluten)
Up to 8 business days
Available with home visit
7 520 RUB
Add to cart
Gastropanel
Up to 9 business days
Available with home visit
RUB 4,760
Add to cart
To clarify the diagnosis of keratoma, a skin biopsy is performed and an epithelium scraping is performed, followed by microscopic and histochemical examination.

Histological examination of biopsy material and material obtained during surgical interventions (endoscopic material; tissues of the female reproductive system; skin, soft tissues; hematopoietic and lymphoid tissue; bone and cartilage tissue)
Taking biomaterial is paid separately. According to the requirements of clause 17 of the Rules for conducting pathological and anatomical studies, approved. Order of the Ministry of Health of Russia...
Up to 5 working days
Available with home visit
2 880 RUB
Add to cart
Examination of scrapings and impressions of tumors and tumor-like formations
Material for research.
 Imprints and scrapings are obtained from pathological lesions of the skin and mucous membranes (except for the cervix and cervical canal). Relative to test...
Imprints and scrapings are obtained from pathological lesions of the skin and mucous membranes (except for the cervix and cervical canal). Relative to test... Up to 2 working days
Available with home visit
RUB 1,030
Add to cart
If atypical cells are found in scrapings or biopsies, contact the oncologist.
If xanthomas appear on the skin, it is recommended to consult a cardiologist, take blood tests for lipid profile and blood glucose levels, and screen for diabetes.
Lipid profile screening
Up to 1 business day
Available with home visit
1 355 RUB
Add to cart
Glucose (in the blood) (Glucose)
Research material Serum or blood plasma.
 If it is not possible to centrifuge the sample 30 minutes after collection for serum/plasma separation...
If it is not possible to centrifuge the sample 30 minutes after collection for serum/plasma separation... Up to 1 business day
Available with home visit
335 RUB
Add to cart
Diabetes management: advanced
Up to 1 business day
Available with house call
RUB 5 820
Add to cart
What should I do if plaques appear on the skin?
Any newly appeared neoplasms should be shown to a dermatologist. Their cosmetic removal without prior consultation with a specialist is fraught with serious consequences.
Their cosmetic removal without prior consultation with a specialist is fraught with serious consequences. In addition, there are symptoms that require immediate medical attention:
- change in the shape of the plaque - the edges have become uneven;
- change in the surface of the plaque - cracks, ulcerations appeared;
- change in the size of the plaque - it began to grow rapidly above the surface of the skin or actively spread over it;
- discoloration of the plaque - in cases of malignancy, an uneven color of the formation is usually observed with areas of darker and lighter shades;
- the appearance of bleeding - both contact and spontaneous;
- enlargement of regional (nearby) lymph nodes.
Plaque treatment
When plaques of an allergic nature appear on the skin, antihistamines are prescribed, in cases of a severe course of the disease, glucocorticosteroids. In addition, it is important to follow a hypoallergenic diet.
In addition, it is important to follow a hypoallergenic diet. Mycotic plaques require antifungal drugs, both local (ointments, creams) and systemic (tablets). Taking these drugs is associated with a high risk of side effects, and therefore it is possible only after consulting a doctor, accurate verification of the diagnosis and confirmation of the etiology of the disease.
Treatment of psoriasis is multi-stage and complex, it involves constant monitoring by a rheumatologist, taking cytostatics and other drugs, using ointments and shampoos to improve skin condition, using antihistamines to reduce itching, including physiotherapy and a hypoallergenic diet in the treatment regimen.
When confirming the presence of diseases of the gastrointestinal tract, properly selected therapy can stop the appearance of new plaques on the skin, as well as prevent the development of complications of the underlying disease.
Sources:
- Clinical guidelines.
 Dermatitis herpetiformis // Russian Society of Dermatovenerologists and Cosmetologists. 2016.
Dermatitis herpetiformis // Russian Society of Dermatovenerologists and Cosmetologists. 2016. - Clinical guidelines. Urticaria in children // Union of Pediatricians of Russia; Russian Association of Allergists and Clinical Immunologists. 2018.
- Clinical guidelines. Toxidermia // Russian Society of Dermatovenerologists and Cosmetologists. 2016.
- Clinical guidelines. Familial hypercholesterolemia // National Society for the Study of Atherosclerosis. 2018.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Recommendations
-
Gastrointestinal bleeding
405 29September
-
Intestinal colic
4235 28 September
-
Exanthema
4238 12-th of September
Show more
Fungus
Allergy
Diabetes mellitus
Itching of the scalp
Itching of the scalp: causes, in which diseases it occurs, diagnosis and methods of treatment.

More
Allergy
Iron deficiency
Fungus
Rash
Neurodermatitis
Seborrhea
Eczema
Colic
Urticaria
Erythema
Diathesis
Diathesis: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.
More
Allergy
Adenoids
Nasal polyps
Apnea
Tumor
Rhinitis
Acromegaly
Snoring
Snoring: causes, diseases, diagnosis and treatment.
More
Allergy
Roseola
Papule
Scar
Hyperpigmentation
Depigmentation
Pustule
Rash
Erythema
Blister
Erosion
Ulcer
Dermatitis
Urticaria
Exanthema
Exanthema: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.