Big blood clots after miscarriage
Miscarriage - Better Health Channel
What is a miscarriage?
A miscarriage is defined as the loss of a pregnancy before 20 weeks gestation. Miscarriage happens when a pregnancy stops growing. Eventually, the pregnancy tissue will pass out of the body. Some women will feel crampy, period-like pain and in most cases there will be vaginal bleeding.
Most spontaneous miscarriages (75 to 80 per cent) occur in the first 12 weeks of pregnancy. It is estimated that 1 in 4 pregnancies end in miscarriage. Many miscarriages are unreported or go unrecognised because they occur very early in the pregnancy.
Causes of a miscarriage
A miscarriage usually occurs because the pregnancy is not developing properly. The development of a baby from a female and a male cell is a very complicated process. If something goes wrong with the process, the pregnancy will stop developing. Miscarriages are more common in older women than younger women, largely because chromosomal abnormalities are more common with increasing age.
Another cause of miscarriage may be that the developing pregnancy did not embed itself properly into the lining of the uterus (womb). The natural reaction of the uterus is to expel the non-viable pregnancy.
Symptoms of a miscarriage
Pain and bleeding in early pregnancy can mean that you are having a miscarriage, but not always. Bleeding is very common in early pregnancy, affecting about one in four women, many of whom will go on to have a healthy baby. Early bleeding that does not lead to miscarriage will not have caused your baby any harm.
If the bleeding is being caused by a miscarriage, there is no treatment or therapy that can stop the miscarriage from occurring. However, it is still very important that you see a health professional.
Treatment for a miscarriage
Nothing can be done to stop a miscarriage once it has begun. Treatment is aimed at avoiding heavy bleeding and infection. It is also aimed at looking after you, physically and emotionally.
You may need to wait a short period of time before treatments begin. If you experience heavy bleeding with clots and crampy pain in that time, it is likely that you are passing the pregnancy tissue. The bleeding, clots and pain will usually settle when most of the pregnancy tissue has been passed.
Sometimes, the bleeding will continue to be heavy and you may need further treatment. If you think you are having, or have had, a miscarriage, you should see a doctor or go to an emergency department.
You should go to your nearest emergency department if you have:
- increased bleeding – for instance, soaking 2 pads per hour or passing golf ball-sized clots
- severe abdominal pain or shoulder pain
- fever or chills
- dizziness or fainting
- vaginal discharge that smells unpleasant
- diarrhoea or pain when you open your bowels.
Types of miscarriage
The types of miscarriage that can occur include:
- Missed abortion– occurs when the pregnancy has failed, although there has not been any bleeding or other signs.
 Occasionally, the aborted pregnancy may remain in the uterus for weeks or even months until bleeding commences. Missed abortion is suspected when pregnancy symptoms disappear and the uterus stops growing. It is diagnosed by an ultrasound examination.
Occasionally, the aborted pregnancy may remain in the uterus for weeks or even months until bleeding commences. Missed abortion is suspected when pregnancy symptoms disappear and the uterus stops growing. It is diagnosed by an ultrasound examination. - Blighted ovum– this occurs when a pregnancy sac is formed, but there is no developing baby within the sac. This is diagnosed by ultrasound, usually after some bleeding.
- Ectopic pregnancy– this occurs when the developing pregnancy implants in the fallopian tubes rather than in the uterus. One to two per cent of all pregnancies are ectopic and without treatment, an ectopic pregnancy can seriously impact on your health and fertility.
Reactions to miscarriage
There is no ‘right way’ to feel after a miscarriage. A range of feelings is normal, and they often linger for some time after the miscarriage. Reactions may include feelings of:
- emptiness
- anger and disbelief
- disappointment
- sadness and a sense of isolation.
Some degree of grief is very common, even if the pregnancy wasn’t planned. Partners may react quite differently, just as people can respond differently to a continuing pregnancy. Try to take it a day at a time and acknowledge your feelings and reactions as they arise.
In addition to the grief you may feel, your body will be undergoing many hormonal changes, which may make you feel very emotional. Family or close friends can be a great source of support at these times. Alternatively, you may choose to seek professional support.
Don’t blame yourself for a miscarriage
Pathology tests are sometimes performed after a miscarriage, but usually, no cause can be identified. This can add to feelings of distress and disbelief, and may lead to feelings of guilt. However, doctors agree that a miscarriage is rarely caused by anything the mother did – or didn’t – do (for example, drank a glass of wine, ate a particular food, had sex or did not rest enough). In the majority of cases, the next pregnancy proceeds to full term.
After a miscarriage
Often, some of the pregnancy tissue remains in the uterus after a miscarriage. If it is not removed by scraping the uterus with a curette (a spoon-shaped instrument), you may bleed for a long time or develop an infection. Unless all the pregnancy tissue has been passed, your doctor will usually recommend that a curette (also called a ‘D&C’ – dilation and curettage) be performed. This is done under a light general anaesthetic and you can usually go home later the same day. A sample of tissue is usually sent for pathology tests.
After the curette
Most women bleed for 5 to 10 days following a curette. Contact your doctor if you experience:
- prolonged or heavy bleeding
- blood clots or strong abdominal pain
- changes in your vaginal discharge
- fever or flu-like symptoms.
Your next period after a miscarriage
Your ovaries will usually produce an egg about 2 weeks after your miscarriage. Your first period should occur within 4 to 6 weeks. You should have a check-up with your doctor 6 weeks after your miscarriage to make sure there are no problems and to ensure your uterus has returned to normal size. You can also ask any questions about your miscarriage at this time, including the results of any pathology tests.
You should have a check-up with your doctor 6 weeks after your miscarriage to make sure there are no problems and to ensure your uterus has returned to normal size. You can also ask any questions about your miscarriage at this time, including the results of any pathology tests.
The effect of miscarriage on future pregnancies
Most of the problems that cause miscarriage happen by chance and are not likely to happen again. One miscarriage does not significantly increase the risk of the same thing happening with your next pregnancy, as long as no specific cause has been found. Testing is not usually offered to women who have miscarried once or twice because it is very unlikely that anything would be found.
However, women who have had 3 consecutive miscarriages are at risk of miscarrying again. If you fall into this category, you can attend the Recurrent Miscarriage Clinic at The Royal Women’s Hospital for further investigations, counselling and management of future pregnancies.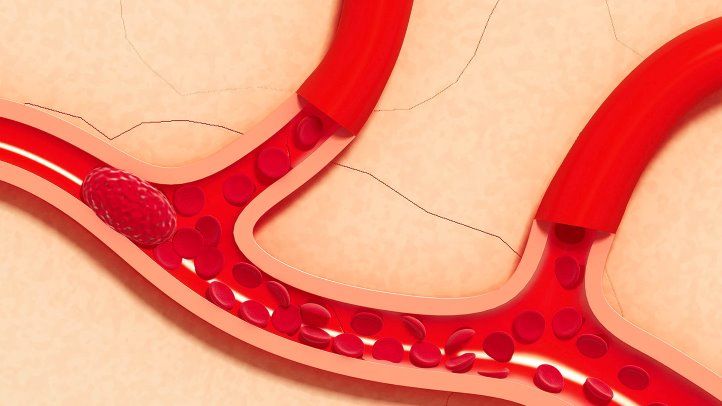
Trying for another pregnancy after miscarriage
There is no right time to try for another pregnancy. Some people decide they need time to adjust to their loss, while others want to try again right away. It is usually suggested you wait until after your next period before trying again. As it is possible to become pregnant again straight away, it is important to use contraception until you are ready to try again.
If you are Rh (Rhesus) negative
If you have an Rh negative blood group, you will require an injection of anti-D immunoglobulin following a miscarriage. This will prevent problems with the Rh factor in future pregnancies. Your doctor will discuss this with you further.
Preparing for another pregnancy after a miscarriage
Although the common reasons for miscarriage cannot be prevented, you can improve your chances for long-term fertility and a successful pregnancy by:
- stopping smoking
- taking regular exercise and having a balanced diet
- reducing stress
- maintaining your weight within recommended limits.

Take folic acid
It is recommended that all women planning a pregnancy take folic acid as it helps promote the normal development of a baby’s nervous system. You will need to take 0.5 mg per day for one month prior to pregnancy and up to 12 weeks gestation.
Where to get help
- In an emergency, call 000 for an ambulance
- Your GP (doctor)
- The Royal Women’s Hospital Tel. (03) 8345 2000
- Miscarriage Australia are researchers and clinicians who aim to help all affected by miscarriage.
- Recurrent Miscarriage Clinic, The Royal Women’s Hospital Tel. (03) 8345 2000
- Stillbirth and Neonatal Death Support (SANDS) Tel. (03) 9899 0218
Miscarriage - Atlanta Gynecology and Obstetrics
Loss of pregnancy before 20 weeks is called a miscarriage. Spontaneous miscarriage is the most common complication of early pregnancy and the rate decreases as the pregnancy progresses.
Miscarriages occur in 8-20% of clinically-recognized pregnancies:
- 80% of these happen in the first 12 weeks of pregnancy
- The rate of loss for unrecognized or “chemical pregnancies” is 13-26%
- The overall risk of loss after 15 weeks is relatively low
Causes of miscarriage
Though it is difficult to identify what causes all miscarriages, most pregnancy losses are thought to be due to chromosomal defects.
- Chromosomal Abnormalities > 60%
- Maternal: Structural Abnormalities
- Uterine Fibroids, Septums, and Adhesions
- Trauma
- Acute Infections
- Blood Disorders (Thrombophilia)
- Unexplained
Loss of viability of the pregnancy usually occurs between 6-12 weeks. Recognition may not occur until weeks later. The course of treatment that you take will depend on your current condition, your desires, the size of your pregnancy, and your provider recommendations.
Factors associated with miscarriage
There can be many factors that affect the probability of having a miscarriage. In many cases, there is more than one factor that comes into play. If you know what these factors are, you can be more cautious.
- Age: Miscarriage risk increases with age. The risk can be as high as 40% at 40 years old and 80% after 45 years old
- Previous miscarriage: The rate of miscarriage increases with the number of previous miscarriages: 20% after one, 28% after two consecutive, and 43% after three or more consecutive losses
- Smoking: Increases the risk of loss
- Alcohol use: Studies have been inconsistent in proving that alcohol can cause an increased rate of pregnancy loss.
 One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day
One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day - Cocaine use
- Non-steroid anti-inflammatories (NSAIDs: Ibuprofen, Advil, Motrin): May be associated with an increased risk of miscarriage if used around the time of conception. The prostaglandin in NSAIDs may interfere with proper implantation
- Caffeine: The risks of miscarriage increase with high levels of consumption (>300mg /day)
Miscarriage at home
You may first note mild vaginal spotting and/or cramping. This bleeding and cramping will increase, at which point you may expel the tissue of the pregnancy. During the miscarriage, you may bleed heavily with large clots, soaking a pad every 10-20 minutes. The cramping may be significant. Tylenol and a heating pad are okay to use at this time. You should call the office or the on-call doctor if the heavy bleeding does not improve after two hours.
Once you have passed the pregnancy tissue, you will notice a decrease in bleeding and cramping. You may collect the passed tissue and store it in a clean and dry container and bring it to the office so that it may be sent out for pathological identification. You may call the office or the on-call doctor at any time for direction and advice.
Office Number: 404-299-9724 | After Hours Number: 404-487-2450
D&C at the hospital
A D&C is a surgical procedure performed under anesthesia to remove tissue from the uterus that has not started to or that has not entirely come out.
A D&C is an outpatient procedure that lasts for about 15-20 minutes. You usually go home about 1-2 hours after the procedure is completed. Most women return to light duties and activity the next day. Cramping and bleeding are common after a D&C. You may have bleeding for up to 2 weeks after your procedure.
Alternatively, we offer appropriate candidates a procedure called a Mechanical Vacuum Aspiration (MVA).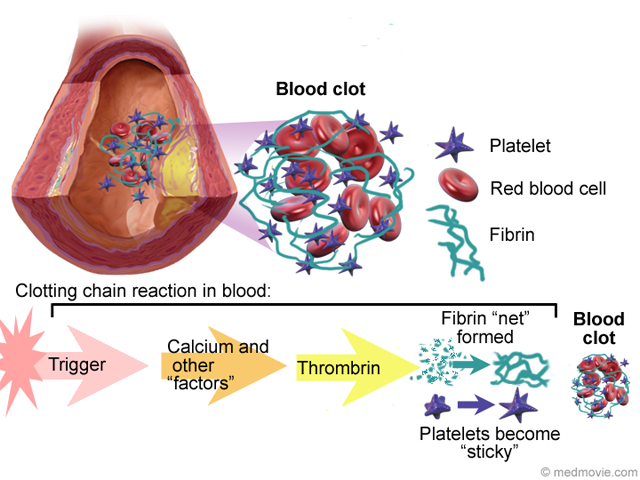 This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
With either of these procedures, we recommend that you do not put anything in the vagina (no tampons, douching, or intercourse) until you are seen again in the office.
Warning signs after a miscarriage or D&C
Call the office if you have:
- Temperature > 100.4
- Nausea and vomiting for > 12 hours
- Increasing pain or bleeding
- Foul-smelling vaginal discharge
Coping with the loss of pregnancy
Emotional healing can take longer than physical healing. Grief after a pregnancy loss is a normal response. In the days and weeks after your pregnancy loss, you may experience a loss of appetite, emotional changes, irritability, sleep disturbances, and inability to focus on daily tasks. This is all normal and should resolve in a few weeks or months.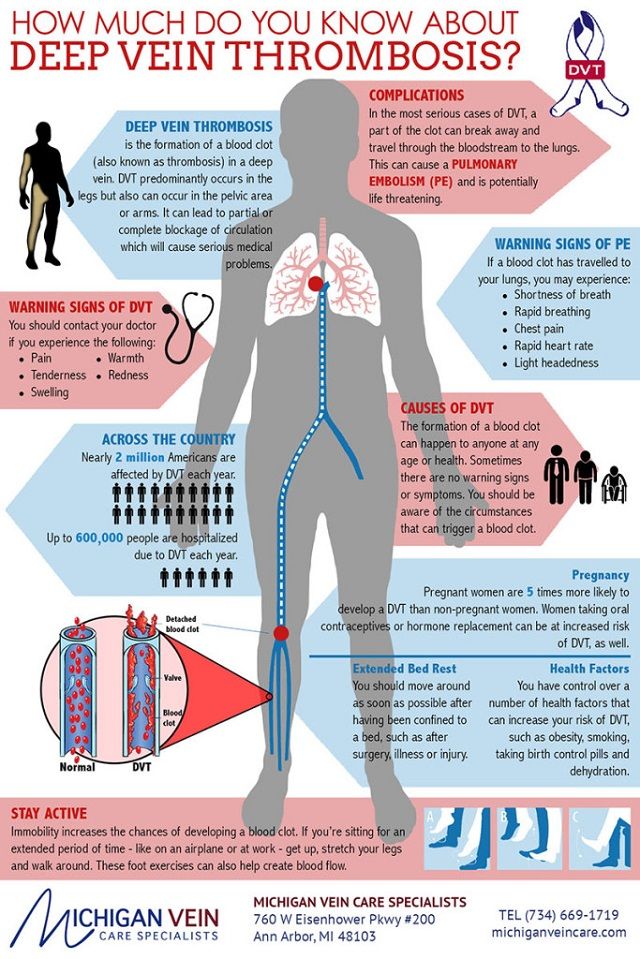 If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
The next pregnancy
Your next period should come within 4-6 weeks after your miscarriage. We recommend that you use contraception until after you have had a normal period. You may continue prenatal vitamins during and after this time. You may also discuss birth control at your post-miscarriage visit if you do not desire to become pregnant again.
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies.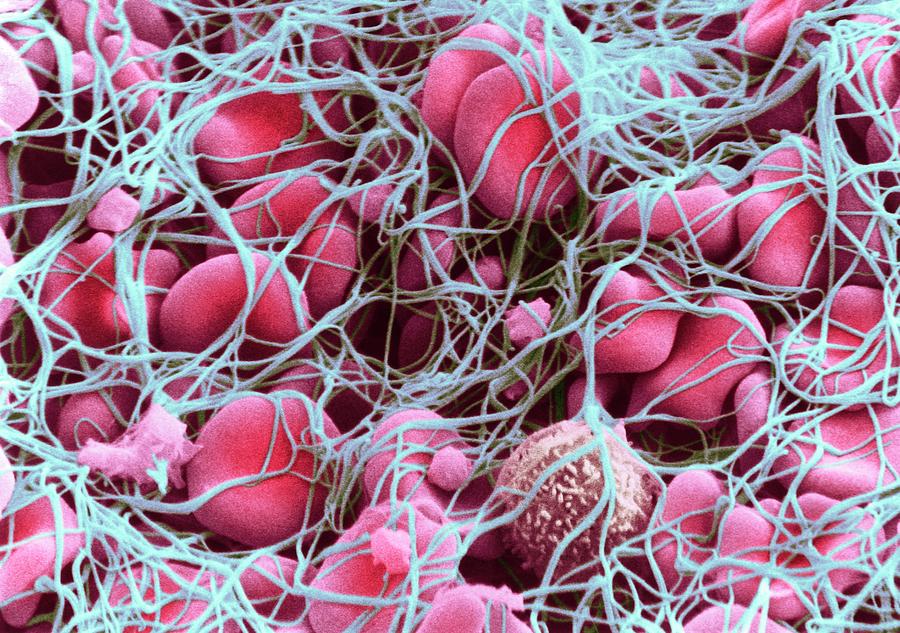 You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.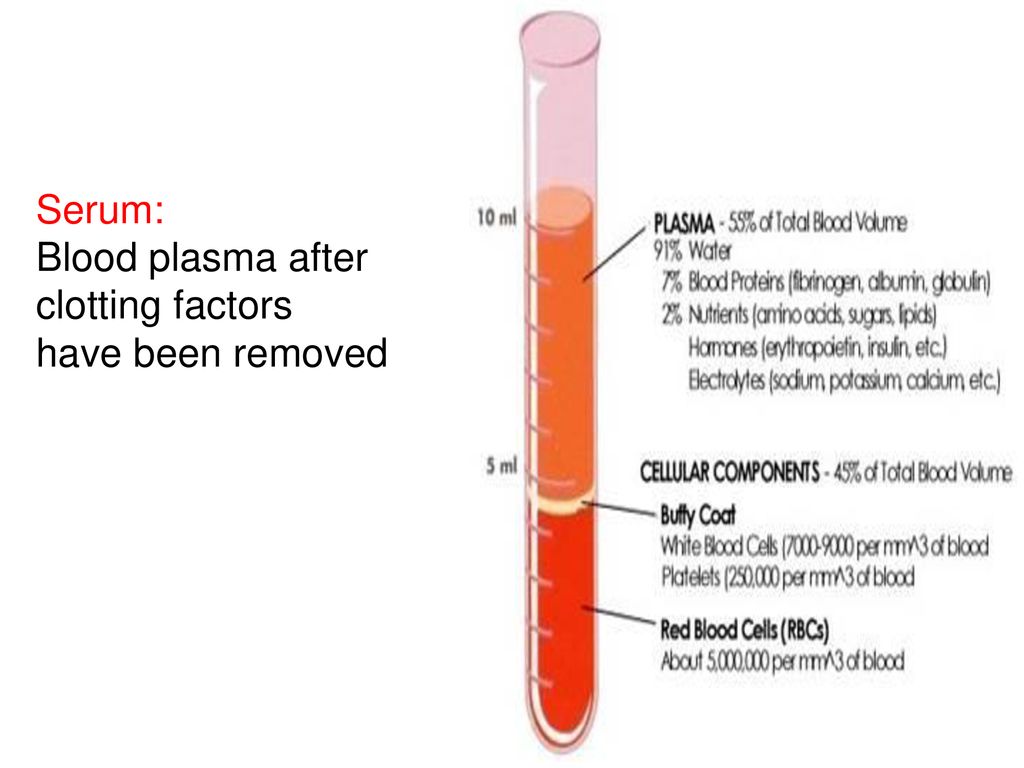
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late.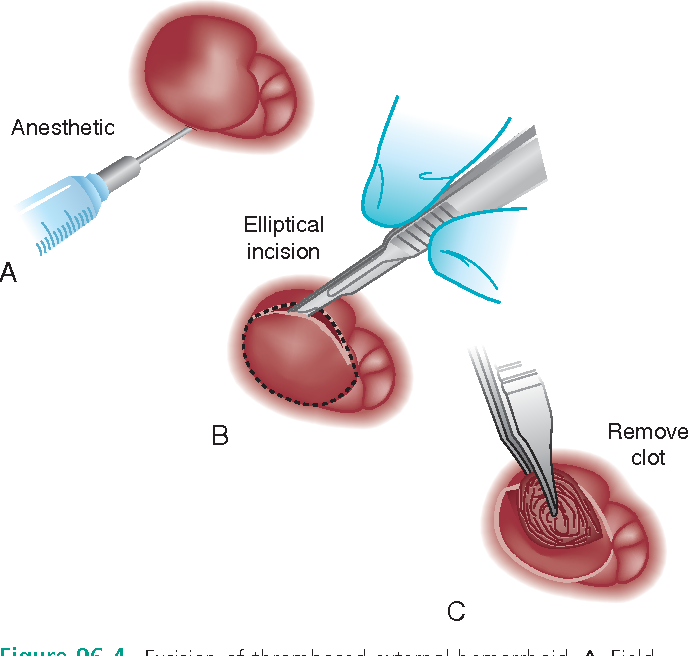 Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina.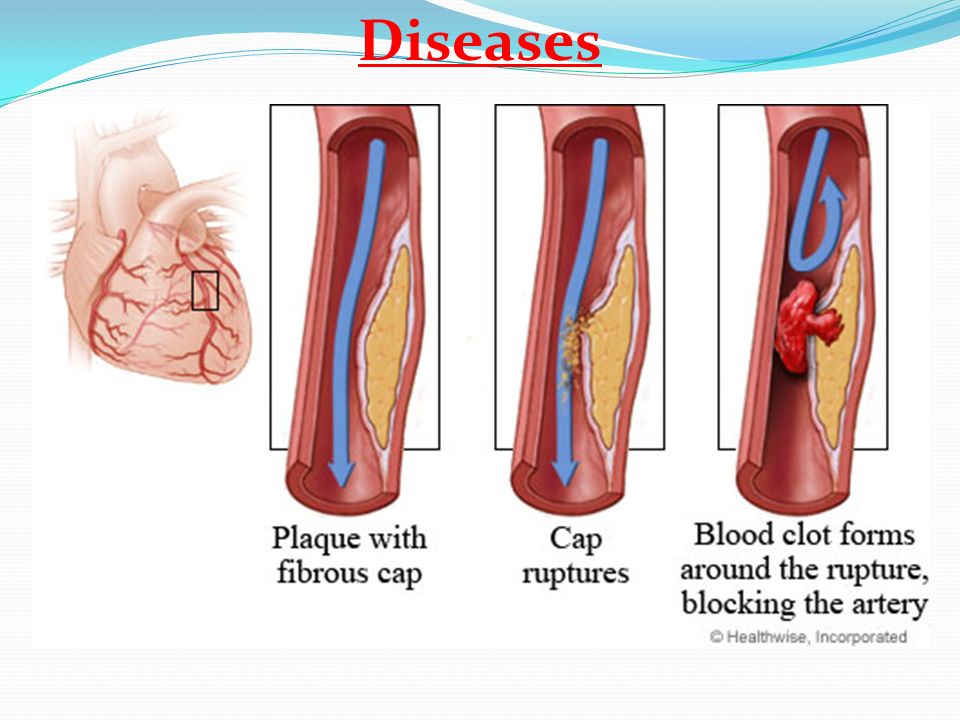 The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
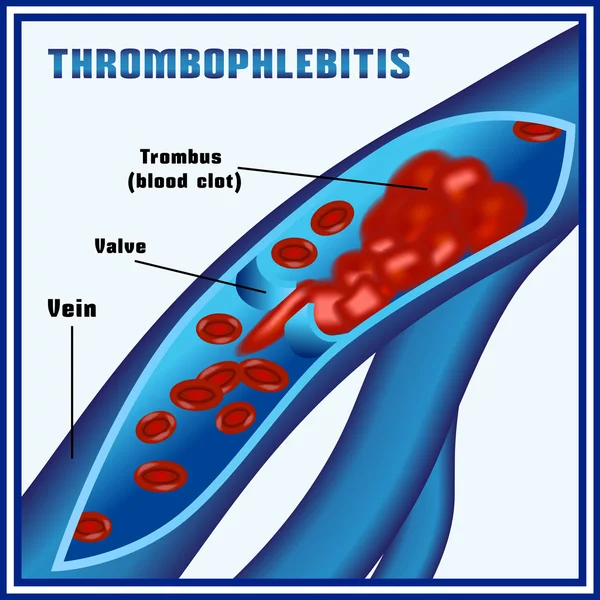
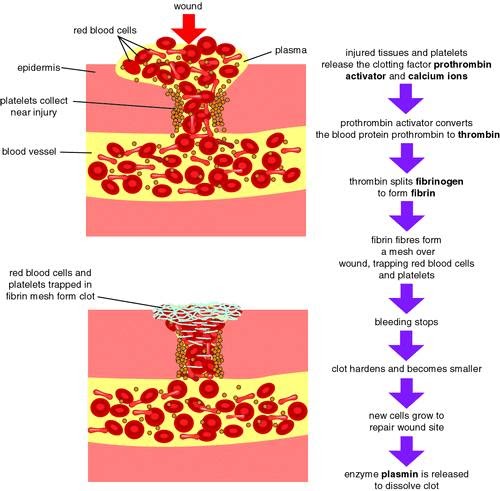
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be started.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
Lower extremity vein thrombosis in obstetric practice
During pregnancy, the incidence of venous thromboembolic complications (VTEC) is 0. 2–1% [1–3], and the risk of thrombosis increases by 5–6 times [2]. And during a physiologically proceeding pregnancy, there are components of the triad described by R. Virchow - changes in the properties of the blood that create favorable conditions for thrombosis, a decrease in blood flow, a change in the vascular wall. During pregnancy, hypercoagulability develops due to an increase in the level of coagulation and platelet aggregation factors and a decrease in the activity of the fibrinolysis system [3, 4]. The concentration of physiological anticoagulants, in particular soluble protein S, decreases [5]. Compression of the inferior vena cava that occurs and progresses as pregnancy progresses leads to an increase in hydrodynamic pressure in its system and an increase in the diameter of deep veins in the lower extremities against the background of a decrease in blood flow in them [6, 7]. In pregnant women, concomitant autoimmune diseases, an increased concentration of circulating estrogens, and viral infections may be a factor that damages the internal lining of the veins [7].
2–1% [1–3], and the risk of thrombosis increases by 5–6 times [2]. And during a physiologically proceeding pregnancy, there are components of the triad described by R. Virchow - changes in the properties of the blood that create favorable conditions for thrombosis, a decrease in blood flow, a change in the vascular wall. During pregnancy, hypercoagulability develops due to an increase in the level of coagulation and platelet aggregation factors and a decrease in the activity of the fibrinolysis system [3, 4]. The concentration of physiological anticoagulants, in particular soluble protein S, decreases [5]. Compression of the inferior vena cava that occurs and progresses as pregnancy progresses leads to an increase in hydrodynamic pressure in its system and an increase in the diameter of deep veins in the lower extremities against the background of a decrease in blood flow in them [6, 7]. In pregnant women, concomitant autoimmune diseases, an increased concentration of circulating estrogens, and viral infections may be a factor that damages the internal lining of the veins [7]. The prerequisites for thrombus formation persist in the postpartum period - the pelvic veins are overstretched, the blood flow in the uterus is sharply reduced, which leads to the formation of venous stasis. The probability of VTEC in the postpartum period increases in 2-9times [7].
The prerequisites for thrombus formation persist in the postpartum period - the pelvic veins are overstretched, the blood flow in the uterus is sharply reduced, which leads to the formation of venous stasis. The probability of VTEC in the postpartum period increases in 2-9times [7].
In obstetrics, there are groups of very high, high and moderate risk of developing VTEC [8, 9]. Groups of very high and high risk are pregnant women with various forms of thrombophilia and with a history of VTEC - relapse during pregnancy was noted in 2-10% of those who had previously undergone VTEC [10]. In a number of thrombophilic conditions, the risk of venous thrombosis increases by more than 100 times, especially in the presence of homozygous, multigenic forms of thrombophilia or combined forms - a combination of antiphospholipid syndrome (APLS) with genetic thrombophilia [2]. The group of moderate risk of developing VTEC includes pregnant women without thrombosis in the past, but with additional factors - pregnancy complications associated with hypercoagulability: severe early toxicosis with dehydration, preeclampsia, somatic pathology (rheumatic heart disease, operated heart, systemic diseases, nephrotic syndrome, obesity), operative delivery, acute and chronic infections.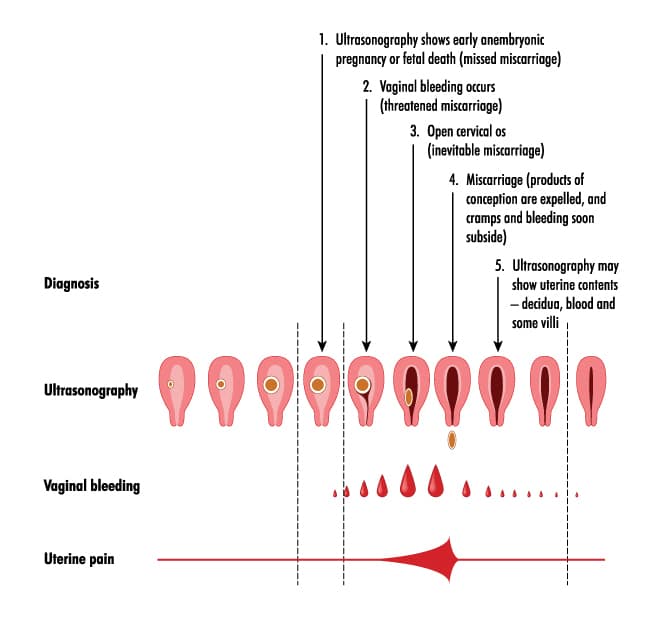 A significant role of immobilization during pregnancy is highlighted [11]. The group of moderate risk should also include pregnant women with varicose veins of the saphenous veins of the lower extremities, which affects from 25 to 33% of women, and with chronic venous insufficiency, which, according to various sources [12], is present in 3.7–15% of women. 50-95% of women with venous pathology developed the disease for the first time during pregnancy [13, 14]. Chronic venous insufficiency, in addition to creating conditions for thrombosis, can contribute to the disruption of the uteroplacental, and then the fetal-placental blood flow, worsening the perinatal prognosis [15]. Long-term static exercise and obesity increase the risk of thromboembolic complications [10, 11].
A significant role of immobilization during pregnancy is highlighted [11]. The group of moderate risk should also include pregnant women with varicose veins of the saphenous veins of the lower extremities, which affects from 25 to 33% of women, and with chronic venous insufficiency, which, according to various sources [12], is present in 3.7–15% of women. 50-95% of women with venous pathology developed the disease for the first time during pregnancy [13, 14]. Chronic venous insufficiency, in addition to creating conditions for thrombosis, can contribute to the disruption of the uteroplacental, and then the fetal-placental blood flow, worsening the perinatal prognosis [15]. Long-term static exercise and obesity increase the risk of thromboembolic complications [10, 11].
The clinical manifestations of thrombosis, regardless of its location, are usually represented by general, painful symptoms and symptoms of congestion. Diagnosis of deep vein thrombosis during pregnancy is complicated by initial venous hypertension in the lower extremities with lymphovenous insufficiency, especially on the left, as well as redistribution of pain impulses due to pregnancy.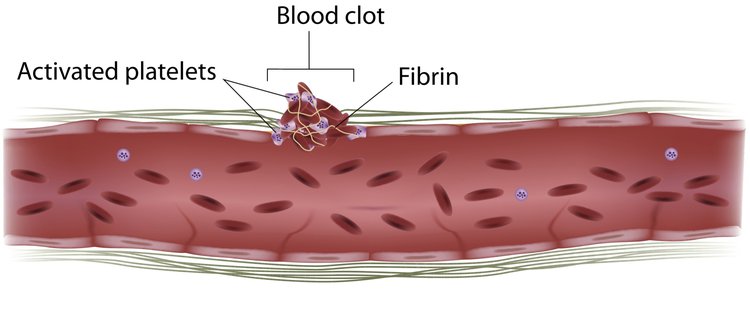 Differential diagnosis can be difficult if vascular pathology develops against the background of other complications of pregnancy — threatening miscarriage, preeclampsia, polyhydramnios [6].
Differential diagnosis can be difficult if vascular pathology develops against the background of other complications of pregnancy — threatening miscarriage, preeclampsia, polyhydramnios [6].
The main method for diagnosing venous thrombosis is compression ultrasound duplex angioscanning (USAS), with negative results - determination of D-dimer and repeated ultrasound in dynamics. If it is suspected that thrombosis has spread to the iliocaval segment and it is impossible to determine its proximal border and nature, computed tomography (CT), magnetic resonance imaging (MRI) is recommended [8, 16]. The D-dimer test is considered during pregnancy as an auxiliary method, since the level of D-dimer increases during physiological pregnancy as the gestation period increases, as well as in the presence of obstetric complications that occur with the development of DIC [16]. An increase in the level of D-dimer was noted in preeclampsia [17] and gestational diabetes mellitus [18]. There is an opinion that the D-dimer indicator is informative for assessing prothrombotic readiness before the appointment of low molecular weight heparins (LMWH), but is less indicative in the process of monitoring the effectiveness of prescribed therapy [19].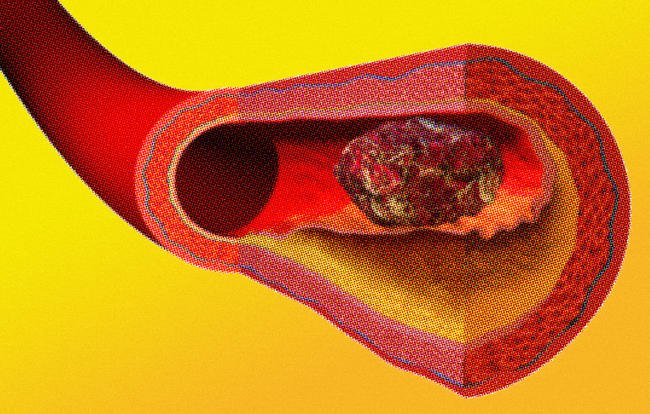
The aim of the study was to analyze 10 years of experience in the treatment and delivery of pregnant women with lower limb vein thrombosis to assess the choice of treatment tactics.
Material and methods
The material of this study was the results of the examination, treatment, follow-up and pregnancy outcome of 96 women with lower extremity vein thrombosis who were treated in a multidisciplinary hospital in Saratov. The structure of the medical institution, among other departments, includes a maternity hospital, gynecological departments, a radiology department and a vascular surgery department.
All patients were divided into three groups according to the trimester of pregnancy in which the disease began: group 1 ( n = 24.25%) - I trimester, group 2 ( n = 26.27%) - II trimester, 3rd group ( n = 46, 47.9%) - III trimester.
Features of the management of pregnant women with VTEC are due to the need to minimize the negative impact on the fetus and careful constant monitoring of its condition. Prior to establishing the diagnosis, the patients were hospitalized in the intensive care unit for joint observation by obstetrician-gynecologists and angiosurgeons until the nature of thrombosis was clarified. Urgently performed ultrasound duplex angioscanning (USAS) of the veins of the lower extremities, the study of hemostasis, the determination of D-dimer. In a number of observations, magnetic resonance imaging was prescribed (II, III trimesters). An obstetric examination was carried out with echographic examination of the uterus and fetus with dopplerometry and cardiotocography. After clarification of the location and nature of thrombosis and the condition of the fetus, tactics were chosen - surgical or conservative. With the exclusion of embologenic thrombosis and the achievement of positive dynamics in the state of hemostasis, the pregnant women continued treatment in the vascular department or, if indicated, in the obstetric or gynecological department, depending on the gestational age.
Prior to establishing the diagnosis, the patients were hospitalized in the intensive care unit for joint observation by obstetrician-gynecologists and angiosurgeons until the nature of thrombosis was clarified. Urgently performed ultrasound duplex angioscanning (USAS) of the veins of the lower extremities, the study of hemostasis, the determination of D-dimer. In a number of observations, magnetic resonance imaging was prescribed (II, III trimesters). An obstetric examination was carried out with echographic examination of the uterus and fetus with dopplerometry and cardiotocography. After clarification of the location and nature of thrombosis and the condition of the fetus, tactics were chosen - surgical or conservative. With the exclusion of embologenic thrombosis and the achievement of positive dynamics in the state of hemostasis, the pregnant women continued treatment in the vascular department or, if indicated, in the obstetric or gynecological department, depending on the gestational age.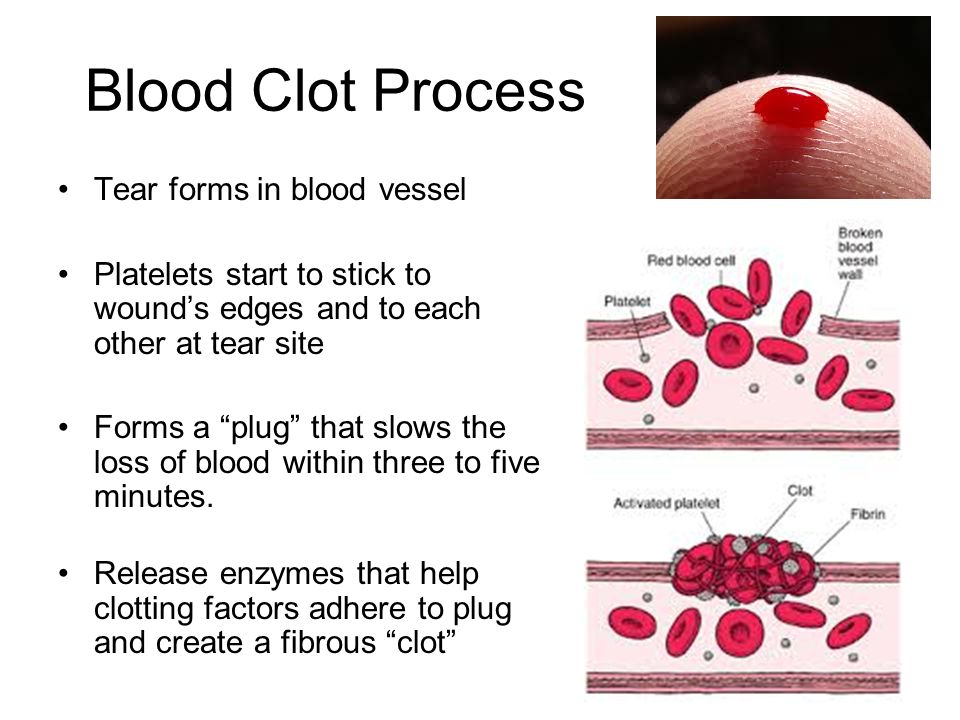 Patients were prescribed compression - the use of compression stockings of the 2nd-3rd class or bandaging with an elastic bandage. Anticoagulant therapy was carried out with therapeutic doses of LMWH. In recent years, we have been successfully using enoxaparin sodium — enixum at doses recommended for treatment during pregnancy [8, 9]. The drug was administered at a therapeutic dose of 1 mg/kg every 12 hours. When positive dynamics were achieved during the thrombotic process, the dose was reduced to a prophylactic dose, depending on body weight, at 40–60 mg/day until delivery. Subcutaneous administration of the drug was stopped at least 24 hours before the planned end of pregnancy - termination of pregnancy, caesarean section or labor induction. Anticoagulant therapy was resumed 6-12 hours after intervention or delivery. After discharge from the hospital, all patients are recommended to wear compression stockings and prolonged use of LMWH (enoxaparin) - for pregnant women before delivery, for puerperas - up to 4-6 weeks of the postpartum period, depending on the presence of factors predisposing to relapse.
Patients were prescribed compression - the use of compression stockings of the 2nd-3rd class or bandaging with an elastic bandage. Anticoagulant therapy was carried out with therapeutic doses of LMWH. In recent years, we have been successfully using enoxaparin sodium — enixum at doses recommended for treatment during pregnancy [8, 9]. The drug was administered at a therapeutic dose of 1 mg/kg every 12 hours. When positive dynamics were achieved during the thrombotic process, the dose was reduced to a prophylactic dose, depending on body weight, at 40–60 mg/day until delivery. Subcutaneous administration of the drug was stopped at least 24 hours before the planned end of pregnancy - termination of pregnancy, caesarean section or labor induction. Anticoagulant therapy was resumed 6-12 hours after intervention or delivery. After discharge from the hospital, all patients are recommended to wear compression stockings and prolonged use of LMWH (enoxaparin) - for pregnant women before delivery, for puerperas - up to 4-6 weeks of the postpartum period, depending on the presence of factors predisposing to relapse.
Results and discussion
Most of our patients — 72 (76%) of 96 had 2 or more risk factors for the development of VTEC and were in the moderate risk group. 59 patients had varicose veins of the lower extremities (Fig. 1). 1. Risk factors for the development of thrombophlebitis complications. 21 patients had impaired lipid metabolism of the II—III degree, 17 pregnant women suffered from arterial hypertension, 2 had diabetes mellitus. 9 patients smoked before and during pregnancy, in 5 patients professional duties were ) patients in the II trimester of pregnancy were operated on for phlegmonous appendicitis, 4 (4.16%) pregnant women in the past received conservative therapy for superficial thrombosis ( n =3) and deep ( n =1) veins of the lower extremities, judging by the anamnestic data, not provoked by anything. The last 6 patients were at high risk of developing thromboembolic complications (see Fig. 1). There were no pregnant women with thrombophilia among our patients, while according to statistical data, 15% of all cases of deep vein thrombosis of the lower extremities are due to APS [20].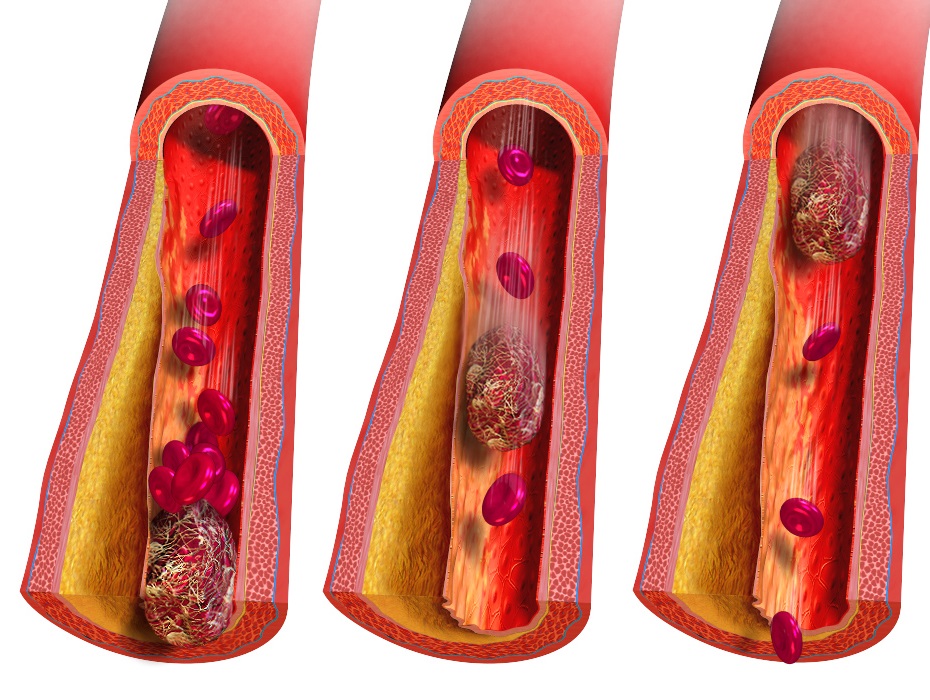
In 30 (31.25%) pregnant women, the pathological process was localized in the superficial, in 66 (68.75%) - in the deep veins of the lower extremities (Fig. 2). Rice. 2. The incidence of deep and superficial thrombosis of the lower extremities in different trimesters of pregnancy.
In 56 (58.4%) cases thrombosis was proximal, in 40 (41.6%) cases it was distal (Fig. 3). Rice. 3. The frequency of occurrence of distal and proximal thrombosis of the lower extremities in different trimesters of pregnancy.
24 (25%) patients of the 1st group were hospitalized in the first trimester of pregnancy (Fig. 4). Rice. 4. Distribution of patients by trimesters of pregnancy (n=96). In this group, in 15 (62.5%) cases, thrombophlebitis of the superficial veins of the lower leg and thigh, combined with varicose veins, occurred. Crossectomy (ligation of the great saphenous vein and its small branches) was performed in 6 (25%) patients with the proximal border of thrombosis of the great saphenous vein at the level of the upper third of the thigh, the rest received conservative therapy.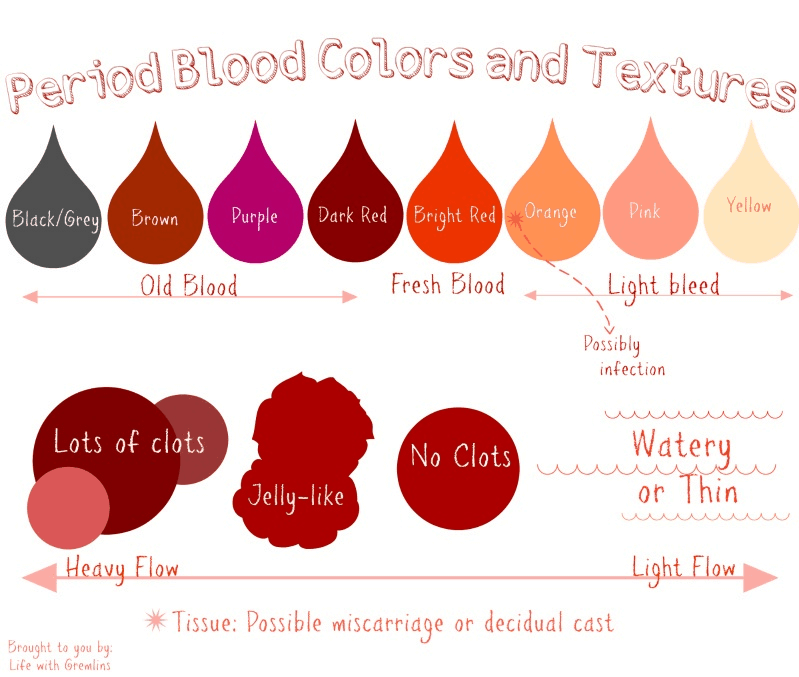 9(37.5%) of patients hospitalized in the first trimester, proximal non-embologenic deep vein thrombosis was diagnosed. Conducted conservative therapy was effective. 5 patients hospitalized in the first trimester and who wished to terminate the pregnancy had an induced abortion. In addition, non-developing pregnancy was diagnosed in 2 cases, which required the emptying of the uterus. Intrauterine intervention was performed after achieving positive dynamics of hemostasis indicators against the background of anticoagulant therapy continued after surgery. The remaining 17 (70.8%) patients of the 1st group successfully reported pregnancy (see table). The outcome of pregnancy in thrombosis of the veins of the lower extremities They did not have repeated episodes of thrombosis before delivery. In 2 cases in the early postpartum period, a manual examination of the walls of the uterine cavity was performed due to hypotonic bleeding. Only one pregnant woman was delivered abdominally due to premature detachment of the placenta at a gestational age of 36-37 weeks.
9(37.5%) of patients hospitalized in the first trimester, proximal non-embologenic deep vein thrombosis was diagnosed. Conducted conservative therapy was effective. 5 patients hospitalized in the first trimester and who wished to terminate the pregnancy had an induced abortion. In addition, non-developing pregnancy was diagnosed in 2 cases, which required the emptying of the uterus. Intrauterine intervention was performed after achieving positive dynamics of hemostasis indicators against the background of anticoagulant therapy continued after surgery. The remaining 17 (70.8%) patients of the 1st group successfully reported pregnancy (see table). The outcome of pregnancy in thrombosis of the veins of the lower extremities They did not have repeated episodes of thrombosis before delivery. In 2 cases in the early postpartum period, a manual examination of the walls of the uterine cavity was performed due to hypotonic bleeding. Only one pregnant woman was delivered abdominally due to premature detachment of the placenta at a gestational age of 36-37 weeks.
In 26 (27.1%) patients (group 2) thrombosis of the veins of the lower extremities developed in the second trimester of pregnancy. In 10 (38.5%) cases the process was localized in the superficial veins, in 16 (61.5%) cases it was in the deep veins. 15 (57.7%) pregnant women hospitalized in the second trimester with non-embologenic thrombosis received conservative therapy. The treatment was effective, the pregnancies were prolonged to full term. Spontaneous, uncomplicated delivery occurred in 12 patients, in 3 cases a caesarean section was performed for obstetric indications - acute fetal distress (2), preeclampsia (1). Crossectomy was performed in 3 (11.5%) pregnant women with thrombosis of the great saphenous vein in the second trimester. In these observations, the pregnancies were prolonged and ended in childbirth through the natural birth canal without complications. In 6 (23%) cases, an embolism-prone nature of deep vein thrombosis of the thigh (floating thrombus) was revealed, which was an indication for surgical intervention — vein plication (1-3 U-shaped sutures involving both walls of the vein) at the level of the upper third of the thigh ( Fig.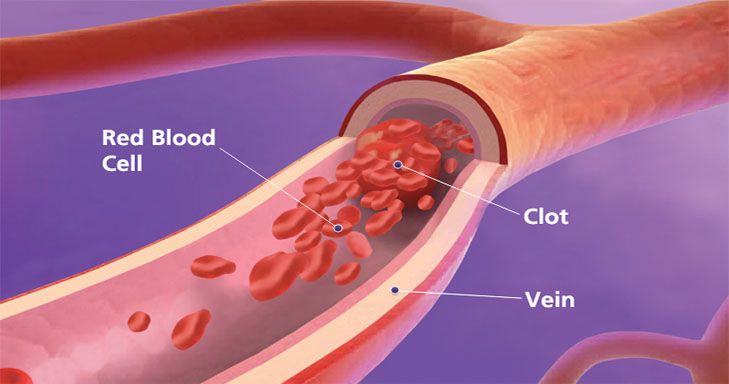 5). Rice. 5. Ultrasound scans, B-mode. a - longitudinal section, b - transverse section. Floating thrombus in the femoral vein (indicated by arrows).
5). Rice. 5. Ultrasound scans, B-mode. a - longitudinal section, b - transverse section. Floating thrombus in the femoral vein (indicated by arrows).
Patients were discharged from the hospital in a satisfactory condition with progressing pregnancy, two of them were delivered abdominally at 37-38 weeks of pregnancy due to vascular pathology. 4 had arbitrary urgent delivery without complications. The pregnancy in the patient, whose plication was performed against the background of infarct pneumonia, ended unfavorably — on the 6th day after the operation, a late miscarriage occurred. One patient underwent hysterectomy in parallel with plication, the indication for which was a non-developing pregnancy at 18 weeks in combination with large uterine fibromyoma.
Out of 46 (47.9%) pregnant women of the 3rd group hospitalized in the third trimester, the process was localized in the superficial veins of the lower leg and thigh in 5 (10.9%) patients. In 17 (36.1%) thrombosis occurred in the deep veins of the leg and was not of a floating nature. These 22 pregnant women received anticoagulant therapy. Of these, 17 (77.3%) gave birth spontaneously, in 2 patients of this group, childbirth was complicated by hypotonic bleeding. Cesarean section was performed in 5 (22.7%) at full-term pregnancy for obstetric indications (preeclampsia - 2 cases, fetoplacental insufficiency in combination with fetal growth retardation - 2, impaired contractile activity of the uterus - 1) with a favorable perinatal outcome. Deep vein thrombosis of the thigh was diagnosed in 24 (52%) pregnant women of the 3rd group. AT 9observations revealed a floating thrombus, which required emergency surgical intervention. Six pregnant women with a gestational age of 35-36 weeks underwent caesarean section and the surgical stage of the operation - plication of the femoral vein proximal to the site of thrombosis. Premature babies were born with an Apgar score of 6-7 points, 2 children were subsequently transferred to the 2nd stage of nursing with subsequent discharge from the hospital.
These 22 pregnant women received anticoagulant therapy. Of these, 17 (77.3%) gave birth spontaneously, in 2 patients of this group, childbirth was complicated by hypotonic bleeding. Cesarean section was performed in 5 (22.7%) at full-term pregnancy for obstetric indications (preeclampsia - 2 cases, fetoplacental insufficiency in combination with fetal growth retardation - 2, impaired contractile activity of the uterus - 1) with a favorable perinatal outcome. Deep vein thrombosis of the thigh was diagnosed in 24 (52%) pregnant women of the 3rd group. AT 9observations revealed a floating thrombus, which required emergency surgical intervention. Six pregnant women with a gestational age of 35-36 weeks underwent caesarean section and the surgical stage of the operation - plication of the femoral vein proximal to the site of thrombosis. Premature babies were born with an Apgar score of 6-7 points, 2 children were subsequently transferred to the 2nd stage of nursing with subsequent discharge from the hospital. In 3 cases, floating deep vein thrombosis was diagnosed at 26, 28, and 31 weeks of gestation, which did not allow us to confidently count on a good perinatal outcome. Therefore, only vein plication was performed, followed by conservative therapy. These pregnant women after completion of treatment in the Department of Vascular Surgery were under the supervision of obstetricians until 37-38 weeks of pregnancy and were delivered in a planned manner abdominally. A caesarean section ended the pregnancy in 15 women with non-embologenic thrombosis that developed after 34 weeks of pregnancy. They underwent anticoagulant therapy until the gestational age of 37–38 weeks, after which a caesarean section was performed with continuation of anticoagulant therapy in the postpartum period. There were no cases of massive blood loss during childbirth. There were no cases of perinatal death. After delivery, anticoagulant therapy continued in combination with early activation of puerperas and the use of compression stockings.
In 3 cases, floating deep vein thrombosis was diagnosed at 26, 28, and 31 weeks of gestation, which did not allow us to confidently count on a good perinatal outcome. Therefore, only vein plication was performed, followed by conservative therapy. These pregnant women after completion of treatment in the Department of Vascular Surgery were under the supervision of obstetricians until 37-38 weeks of pregnancy and were delivered in a planned manner abdominally. A caesarean section ended the pregnancy in 15 women with non-embologenic thrombosis that developed after 34 weeks of pregnancy. They underwent anticoagulant therapy until the gestational age of 37–38 weeks, after which a caesarean section was performed with continuation of anticoagulant therapy in the postpartum period. There were no cases of massive blood loss during childbirth. There were no cases of perinatal death. After delivery, anticoagulant therapy continued in combination with early activation of puerperas and the use of compression stockings.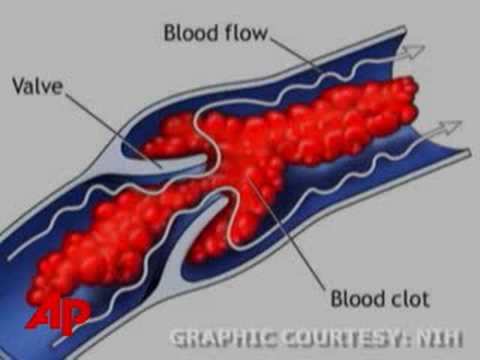 It is believed that in cases where acute thrombosis events were not completely stopped by the time of delivery, it is safer to perform a caesarean section, since active labor can lead to thrombus fragmentation and its proximal migration [6].
It is believed that in cases where acute thrombosis events were not completely stopped by the time of delivery, it is safer to perform a caesarean section, since active labor can lead to thrombus fragmentation and its proximal migration [6].
On days 1–2 after vaginal delivery, deep vein thrombosis of the lower extremity recurred in 3 (3.1%) of our patients. These women had varicose veins of the lower extremities and other risk factors (impaired fat metabolism, moderate preeclampsia) and suffered deep vein thrombosis in the second trimester of pregnancy. The recommended prenatal anticoagulant therapy was carried out haphazardly. After conservative therapy, the puerperas were discharged from the Department of Vascular Surgery in a satisfactory condition.
Thus, the most thromboprone period during pregnancy is its third trimester. Surgical treatment for venous pathology was transferred to 25% of pregnant women, the rest received conservative therapy with a good effect. Pregnancy ended successfully in 87 (90.6%) patients, of which 35 (40.2%) pregnant women were delivered abdominally. The indication for caesarean section in 9 cases was obstetric pathology, in 26 cases operative delivery was undertaken due to vascular pathology.
Pregnancy ended successfully in 87 (90.6%) patients, of which 35 (40.2%) pregnant women were delivered abdominally. The indication for caesarean section in 9 cases was obstetric pathology, in 26 cases operative delivery was undertaken due to vascular pathology.
The choice of method and timing of resolution is determined by the characteristics of the thrombotic process and the obstetric situation [20]. Such tactics made it possible to avoid not only maternal and perinatal mortality, but also serious complications.
Terminals
1. The most thromboprone period during pregnancy is its III trimester - almost 48% of the examined patients were hospitalized in the III trimester.
2. Embolic thrombosis requiring surgical intervention occurred in 25% of pregnant women.
3. In the absence of a threat of dangerous complications and a stable condition of a viable fetus in VTEC in pregnant women, conservative treatment is indicated.
4. Conservative therapy based on LMWH (in recent years enixum) gave a good result in 75% of patients.
5. The chosen treatment tactics contributed to the successful completion of the desired pregnancy in 95.6% of cases; abdominal delivery was performed in 40.23% of pregnant women. In most cases (26 out of 35), caesarean section was performed taking into account the nature of the vascular pathology. Thrombosis of the veins of the lower extremities during pregnancy significantly increases the number of abdominal deliveries.
Credits
Salov Igor Arkadievich - Doctor of Science honey. sciences, prof., head. Department of Obstetrics and Gynecology, Faculty of Medicine, Saratov State Medical University. 410012, Saratov, st. Bolshaya Cossack, 112. Honored. doctor of Russia, chief physician of the City Clinical Hospital No. 1 of Saratov. 410017, Saratov st. them. Kholzunova, 19; e-mail: [email protected]; https://orcid.org/0000-0002-1926-5418
Turlupova Tatyana Ivanovna — Candidate of Medical Sciences, Associate Professor, Department of Obstetrics and Gynecology, Faculty of Medicine, Saratov State Medical University.