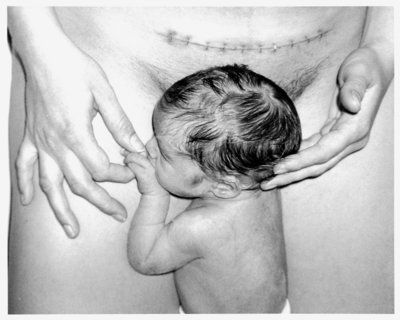
Baby being born vagina
What To Expect, Benefits & Complications
What is a vaginal delivery?
A vaginal delivery is when a person gives birth through their vagina. It's the most common method of childbirth. During a vaginal birth, your uterus contracts to thin and open your cervix and push your baby out through your vagina (or birth canal).
Healthcare providers prefer vaginal deliveries because they're usually safest for the fetus and the birthing person. A vaginal delivery occurs most often between weeks 37 and 42 of pregnancy.
How common are vaginal deliveries?
According to the Centers for Disease Control and Prevention (CDC), there were more than 2.5 million vaginal deliveries in 2020. Vaginal deliveries account for about 68% of all births in the United States and 80% of births worldwide.
What are the types of vaginal delivery?
There are different types of vaginal deliveries: spontaneous, induced and assisted.
- Spontaneous vaginal delivery: A vaginal delivery that happens on its own and without labor-inducing drugs.
- Induced vaginal delivery: Drugs or other techniques initiate labor and prepare your cervix. This is also called labor induction.
- Assisted vaginal delivery: A vaginal birth that occurs with the help of forceps or a vacuum device to get your baby out. Both spontaneous and induced vaginal delivery can be assisted.
What are the stages of a vaginal delivery?
A vaginal delivery can be broken into three stages: labor, birth and delivering the placenta.
Labor
The first stage of labor begins with uterine contractions and ends with your cervix being 10 centimeters dilated and 100% effaced.
Labor can be classified as early labor, active labor and transitional labor.
- Early labor: The time when contractions begin and your cervix starts to open (dilate) and thin (efface). Your cervix may be about 5 centimeters dilated at the end of early labor.
- Active labor: This stage of labor consists of strong contractions that last up to one minute each and happen about three minutes apart.
 Some people request an epidural during this time because contractions can be painful. Healthcare providers may also give you oxytocin (Pitocin®) to speed up labor.
Some people request an epidural during this time because contractions can be painful. Healthcare providers may also give you oxytocin (Pitocin®) to speed up labor. - Transitional labor: This is the time just before your cervix is 10 centimeters dilated. It's a short but intense time when your contractions come very quickly and last longer than one minute. This phase may make you sweat, vomit or feel shaky. It happens just before you begin to push.
Birth
The birthing stage begins when you reach 10 centimeters and ends with the birth of your baby through your vagina. In this stage of labor, you experience strong contractions and begin pushing. You may feel pressure or like you need to poop. Your healthcare provider may coach you through pushing, especially if you've had an epidural and can't feel contractions. This phase can last a few minutes or a few hours. Generally, birth is quicker if you've had a prior vaginal delivery.
Delivering the placenta
The last stage of labor is delivering the placenta (commonly called afterbirth). It begins after your baby is removed from your vagina and ends when your placenta is delivered. Your healthcare provider may ask you for a few more pushes. This stage begins a few minutes after your baby is born and lasts up to 30 minutes.
It begins after your baby is removed from your vagina and ends when your placenta is delivered. Your healthcare provider may ask you for a few more pushes. This stage begins a few minutes after your baby is born and lasts up to 30 minutes.
It's important to remember that labor and childbirth are different for everyone. Certain factors can play a role in your labor being longer or shorter. For example, if you get an epidural, you won't experience the same pain level as a person who doesn't get an epidural. Also, your labor may be longer if it's your first baby. Factors like the size and position of your baby and how quickly you dilate can all affect how long a vaginal delivery takes.
What are the risks of having a vaginal delivery?
Vaginal deliveries generally carry the least risk. The most common complications during a vaginal delivery are:
- Failure to progress: This is when labor slows or stops and your cervix doesn't dilate. Your healthcare provider may give you oxytocin to stimulate contractions and progress labor.

- Irregular fetal heart rate: This is when your baby's heart rate slows down because their head or umbilical cord is compressed.
- Hemorrhage: This is excessive or life-threatening bleeding during or after birth. Sometimes a person doesn't bleed until several hours after delivery (postpartum hemorrhage).
- Vaginal tears: These are tears in the tissue around your vagina and rectum that happen during childbirth.
- Deep vein thrombosis: These are blood clots that develop in your legs or pelvis shortly after delivery.
- Postpartum preeclampsia: This is excessively high blood pressure in a person who has just given birth.
Reasons to avoid vaginal delivery
A vaginal delivery is usually the preferred delivery method. However, certain conditions make a vaginal delivery dangerous. Your healthcare provider may recommend a C-section delivery if:
- Your baby is in a breech position.

- You have placenta previa or a problem with your placenta.
- You have an untreated infection or open genital lesions from herpes simplex virus.
- You have a chronic health condition.
What are the advantages of a vaginal delivery?
A vaginal delivery offers several benefits to both the birthing person and the fetus.
The benefits of vaginal delivery for the birthing person are:
- Shorter recovery time.
- Lactation begins sooner.
- Lower chance of future pregnancy complications.
The benefits of vaginal delivery for the fetus are:
- Lower chance of respiratory conditions.
- Improved immune system function.
- More likely to breastfeed (chest feed).
Is a vaginal delivery painful?
Yes, it can be painful. There are many options to help manage your pain during a vaginal delivery. Some people choose to get an epidural block. An epidural numbs your body from the waist down. Discuss your options for pain relief with your healthcare provider.
Discuss your options for pain relief with your healthcare provider.
What side effects can I expect after a vaginal delivery?
You may have physical and emotional changes after giving birth. It's common to experience:
- Constipation.
- Engorged breasts.
- Pain and soreness in your vagina, especially if you tore.
- Mood swings.
- Vaginal bleeding.
- Hemorrhoids.
- Headaches, hot flashes or sweating (from hormonal changes).
- Cramps.
- Lochia (a type of vaginal discharge).
Some people experience the "baby blues," postpartum depression or postpartum anxiety. Hormonal changes may cause sadness, crying or other emotions within the first few weeks after a vaginal delivery. If you still feel sad, anxious or have mood swings several weeks or months after your baby is born, talk to your healthcare provider.
How long does it take to heal from vaginal delivery?
Recovery time for a vaginal delivery varies. Generally, healing from a vaginal delivery is faster than it is for a C-section. Several factors can influence how quickly you heal. One of those is if your vagina tears and how severe that tear is. If you've torn, you may feel sore for several weeks. Going to the bathroom, sitting and standing or performing everyday tasks may be painful. It's normal to experience swelling and itching around the tear. Most people will have swelling, bruising and general soreness in their vaginal area for a week or two, regardless of vaginal tearing. Putting cold compresses or cooling sanitary pads on your vaginal area may help.
Generally, healing from a vaginal delivery is faster than it is for a C-section. Several factors can influence how quickly you heal. One of those is if your vagina tears and how severe that tear is. If you've torn, you may feel sore for several weeks. Going to the bathroom, sitting and standing or performing everyday tasks may be painful. It's normal to experience swelling and itching around the tear. Most people will have swelling, bruising and general soreness in their vaginal area for a week or two, regardless of vaginal tearing. Putting cold compresses or cooling sanitary pads on your vaginal area may help.
How long do you bleed after a vaginal delivery?
It depends on the person. Some people will bleed for less time than others. It's normal to be bleeding at your postpartum visit several weeks later. Contact your healthcare provider if your bleeding increases over time or you're still filling extra thick sanitary pads after several weeks.
How long after vaginal delivery can you have sex?
Most healthcare providers recommend waiting at least six weeks or until after your postpartum visit to have sex. This gives your body time to heal and allows your provider to examine your vagina to make sure it has healed. Also, consider birth control options and future pregnancies before engaging in sexual intercourse again. Just because you aren’t menstruating and have just given birth doesn't mean you can't get pregnant again.
This gives your body time to heal and allows your provider to examine your vagina to make sure it has healed. Also, consider birth control options and future pregnancies before engaging in sexual intercourse again. Just because you aren’t menstruating and have just given birth doesn't mean you can't get pregnant again.
Can you prepare for a vaginal delivery?
You can try to prepare by creating a birth plan, but there's no way to know what will happen when the time comes. Every labor and delivery is unique. It may help to discuss your wishes with your partner, family, friends and healthcare provider. Asking questions beforehand can also help you know what to expect.
What questions should I ask my healthcare provider about a vaginal delivery?
It's hard to know what to expect from a vaginal delivery, especially if you've never given birth. Even if you've had previous vaginal deliveries, each delivery is unique and different.
Some common questions that people ask their healthcare provider about a vaginal delivery are:
- What are the risks of a vaginal delivery?
- How will I know when to push?
- How can I reduce my risk of vaginal tearing?
- How will I know labor is starting?
- When should I go to the hospital?
- How long will it take to recover from vaginal delivery?
- Is there anything I can do to improve my chances of a normal delivery?
A note from Cleveland Clinic
Giving birth is an exciting and life-altering event. Every pregnancy, labor and delivery is unique. A vaginal delivery is the most common way to give birth. It's hard to know what to expect until you've experienced it, but talking to your healthcare provider and asking questions can help you prepare. Vaginal deliveries are generally low-risk and highly successful. Your healthcare team is trained to manage any complications that arise and help you welcome a healthy baby into the world.
Every pregnancy, labor and delivery is unique. A vaginal delivery is the most common way to give birth. It's hard to know what to expect until you've experienced it, but talking to your healthcare provider and asking questions can help you prepare. Vaginal deliveries are generally low-risk and highly successful. Your healthcare team is trained to manage any complications that arise and help you welcome a healthy baby into the world.
What to Expect During a Vaginal Delivery
What to Expect During a Vaginal DeliveryMedically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI — By The Healthline Editorial Team on April 18, 2018
Choosing a vaginal delivery
Every delivery is as unique and individual as each mother and infant. In addition, women may have completely different experiences with each new labor and delivery. Giving birth is a life-changing event that will leave an impression on you for the rest of your life.
Of course, you’ll want this to be a positive experience and to know what to expect. Here’s some information about what may happen as you’re delivering your baby.
Here’s some information about what may happen as you’re delivering your baby.
Birth plans: Should you have one?
As you approach the latter part of your pregnancy, you may want to write a birth plan. Consider carefully what’s important to you. The overall goal is a healthy mother and baby.
The birth plan outlines your ideal birth and may need to be adjusted as the actual situation unfolds.
Talk with your partner and decide who you want to have attending the birth. Some couples feel that this is a private time and prefer not to have others present.
A birth plan may include other subjects like pain relief during labor, delivery positions, and more.
Early phases of labor
Amniotic sac
The amniotic sac is the fluid-filled membrane surrounding your baby. This sac will almost always rupture before the baby is born, though in some cases it remains intact until delivery. When it ruptures, it’s often described as your “water breaking. ”
”
In most cases, your water will break before you go into labor or at the very beginning of labor. Some women experience their water breaking as a gush of fluid, although it can also be a trickle of fluid. The fluid should be clear and odorless.
When your water breaks, contact your obstetrician gynecologist (ob-gyn) or other obstetric care provider and follow their guidance.
Contractions
Contractions are the tightening and releasing of your uterus. These motions will eventually help your baby push through the cervix. Contractions can feel like heavy cramping or pressure that begins in your back and moves to the front.
Contractions aren’t a reliable indicator of labor. You might already have felt Braxton-Hicks contractions, which may have started as early as your second trimester.
A general rule is that when you are having contractions that last for a minute, are five minutes apart, and have been so for an hour, you’re in true labor.
Cervix dilation
The cervix is the lowest part of the uterus that opens into the vagina. The cervix is a tubular structure approximately 3 to 4 centimeters in length with a passage that connects the uterine cavity to the vagina.
During labor, the role of the cervix must change from maintaining the pregnancy (by keeping the uterus closed) to facilitating delivery of the baby (by dilating, or opening, enough to allow the baby through).
The fundamental changes that occur near the end of the pregnancy result in a softening of the cervical tissue and thinning of the cervix, both of which help prepare the cervix. True, active labor is considered to be underway when the cervix is dilated 3 centimeters or more.
Labor and delivery
Eventually, the cervical canal must open until the cervical opening itself has reached 10 centimeters in diameter and the baby is able to pass into the birth canal.
As the baby enters the vagina, your skin and muscles stretch. The labia and perineum (the area between the vagina and the rectum) eventually reach a point of maximum stretching. At this point, the skin may feel like it’s burning.
The labia and perineum (the area between the vagina and the rectum) eventually reach a point of maximum stretching. At this point, the skin may feel like it’s burning.
Some childbirth educators call this the ring of fire because of the burning sensation felt as the mother’s tissues stretch around the baby’s head. At this time, your healthcare provider may decide to perform an episiotomy.
You may or may not feel the episiotomy because the skin and muscles can lose sensation due to how tightly they’re stretched.
The birth
As the baby’s head emerges, there is a great relief from the pressure, although you’ll probably still feel some discomfort.
Your nurse or doctor will ask you to stop pushing momentarily while the baby’s mouth and nose are suctioned to clear out amniotic fluid and mucus. It’s important to do this before the baby starts to breathe and cry.
Usually the doctor will rotate the baby’s head a quarter of a turn to be in alignment with the baby’s body, which is still inside you. You’ll then be asked to begin pushing again to deliver the shoulders.
You’ll then be asked to begin pushing again to deliver the shoulders.
The top shoulder comes first and then the lower shoulder.
Then, with one last push, you deliver your baby!
Delivering the placenta
The placenta and the amniotic sac that supported and protected the baby for nine months are still in the uterus after the delivery. These need to be delivered, and this can happen spontaneously or it may take as long as half an hour. Your midwife or doctor may rub your abdomen below your belly button to help tighten the uterus and loosen the placenta.
Your uterus is now about the size of a large grapefruit. You may need to push to help deliver the placenta. You may feel some pressure as the placenta is expelled but not nearly as much pressure as when the baby was born.
Your healthcare provider will inspect the delivered placenta to make sure it was delivered in full. On rare occasions, some of the placenta doesn’t release and may remain adhered to the wall of the uterus.
If this happens, your provider will reach into your uterus to remove the leftover pieces in order to prevent heavy bleeding that can result from a torn placenta. If you would like to see the placenta, please ask. Usually, they’ll be happy to show you.
Pain and other sensations during delivery
If you opt for a natural childbirth
If you decide to have a “natural” childbirth (delivery without pain medication), you’ll feel all types of sensations. The two sensations you’ll experience the most are pain and pressure. When you begin to push, some of the pressure will be relieved.
As the baby descends into the birth canal, though, you’ll go from experiencing pressure only during the contractions to experiencing constant and increasing pressure. It will feel something like a strong urge to have a bowel movement as the baby presses down on those same nerves.
If you choose to have an epidural
If you have an epidural, what you feel during labor will depend on the effectiveness of the epidural block. If the medication properly deadens the nerves, you may not feel anything. If it’s moderately effective, you may feel some pressure.
If the medication properly deadens the nerves, you may not feel anything. If it’s moderately effective, you may feel some pressure.
If it’s mildly so, you’ll feel pressure that may or may not be uncomfortable to you. It depends on how well you tolerate pressure sensations. You may not feel the stretching of the vagina, and you probably won’t feel an episiotomy.
Possible tearing
Although significant injuries aren’t common, during the dilation process, the cervix may tear and ultimately require repair.
Vaginal tissues are soft and flexible, but if delivery occurs rapidly or with excessive force, those tissues can tear.
In most cases, lacerations are minor and easily repaired. Occasionally, they may be more serious and result in longer-term problems.
Normal labor and delivery often result in injury to the vagina and/or cervix. Up to 70 percent of women having their first baby will have an episiotomy or some sort of vaginal tear requiring repair.
Fortunately, the vagina and cervix have a rich blood supply. That’s why injuries in these areas heal quickly and leave little or no scarring that could result in long-term problems.
That’s why injuries in these areas heal quickly and leave little or no scarring that could result in long-term problems.
The outlook
It’s not impossible to prepare yourself for labor and delivery, but it’s a famously unpredictable process. Understanding the timeline and hearing about other mothers’ experiences can go a long way to making childbirth less mysterious.
Many expectant mothers find it helpful to write out a birth plan with their partner and share it with their medical team. If you do create a plan, be prepared to change your mind if the necessity arises. Remember that your goal is to have a healthy baby and a healthy, positive experience.
Last medically reviewed on April 18, 2018
- Parenthood
- Postpartum Care
- Post Delivery
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Kettle C, et al. (2010). Absorbable stitches for repair of episiotomy and tears at childbirth.
cochrane.org/CD000006/PREG_absorbable-stitches-for-repair-of-episiotomy-and-tears-at-childbirth - Labor and delivery, postpartum care. (2016).
mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/stages-of-labor/art-20046545b - Stages of labor. (n.d.).
swedish.org/services/pregnancy-and-childbirth/labor-delivery/what-happens-during-delivery/stages-of-labor - When to go to the hospital. (n.d.).
babies.sutterhealth.org/laboranddelivery/labor/ld_when-hosp.html
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Apr 18, 2018
By
The Healthline Editorial Team
Edited By
John Bassham
Medically Reviewed By
Debra Sullivan, PhD, MSN, RN, CNE, COI
Share this article
Medically reviewed by Debra Sullivan, Ph. D., MSN, R.N., CNE, COI — By The Healthline Editorial Team on April 18, 2018
D., MSN, R.N., CNE, COI — By The Healthline Editorial Team on April 18, 2018
related stories
Natural vs. Epidural: What to Expect
Risks of Epidurals During Delivery
The Acupressure Points for Inducing Labor
Cervix Dilation Chart: The Stages of Labor
Is It True? 8 Childbirth Questions You’re Eager to Ask, Answered by Moms
Read this next
Natural vs. Epidural: What to Expect
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
To help make your birthing experience a beautiful one, we tell you what you need to know when it comes to choosing between a natural birth or using an…
READ MORE
Risks of Epidurals During Delivery
Medically reviewed by Karen Gill, M.D.
Epidural blocks and combined spinal-epidural blocks provide relief from the pain of labor.
 However, these techniques aren't risk-free. Get the facts…
However, these techniques aren't risk-free. Get the facts…READ MORE
The Acupressure Points for Inducing Labor
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Are you pregnant and past your due date? Help induce labor naturally by pressing on these acupressure points along the body.
READ MORE
Cervix Dilation Chart: The Stages of Labor
Medically reviewed by Carolyn Kay, M.D.
Ready to deliver and welcome your little one? Here’s a look at the stages of labor.
READ MORE
Is It True? 8 Childbirth Questions You’re Eager to Ask, Answered by Moms
Medically reviewed by Rachel Liberto, R.N.
You've been dying to know whether everything you've heard about childbirth is true. Moms spill the beans, once and for all.

READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.
READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
Does Swaddling Increase the Risk of SIDS?
Medically reviewed by Mia Armstrong, MD
Is swaddling safe, or is it a risk factor for SIDS? Here's what the most recent research says.
READ MORE
The vagina after childbirth - why it stretches, how it changes and recovers
After childbirth, your body may look and feel different ...
After childbirth, everything changes quickly. Your family has grown - now you have a child who needs to be loved and raised, who needs to be taken care of. You can experience joy, surprise, admiration and fear - all at the same time. In addition to the biggest change (in front of you is a completely new person who can’t even hold his head), there are also those that concern you yourself.
Becoming a mother, you face changes - internal and external, physical and psychological. Your body is no longer the same as it was before pregnancy, and that's okay! The vagina also changes after childbirth - this is a completely natural part of the process of bearing a child and childbirth. You may get a few new stretch marks, and your breasts may lose their usual shape. Let's find out more about how the intimate area (vagina, vulva, and bikini area) can change after childbirth, so you know what to expect.
Let's find out more about how the intimate area (vagina, vulva, and bikini area) can change after childbirth, so you know what to expect.
So, what changes happen to the bikini area and vagina after childbirth?
The intimate area, and especially the vagina, changes after childbirth, and this is natural. In order for the baby to pass through the birth canal, the entrance to the vagina must stretch. Its walls move apart and expand, almost like an umbrella. Sometimes the perineum — the area between the entrance to the vagina and the anus — is torn, or the doctor cuts it open to allow the baby to come out. This is called an episiotomy. The very thought of an episiotomy can be daunting, but be aware that you will be asked for consent prior to surgery, offered anesthesia (usually a local anesthetic to numb the area), and then sutured [1].
9 out of 10 women who give birth vaginally for the first time have some kind of tear, incision or episiotomy [2], so this is a common occurrence that most women in labor experience. Although the thought of such traumas can be scary, talking with those who have gone through it will help you reassure yourself that everything will be fine. You can also discuss this with your doctor so you know exactly what to expect and how to deal with it.
Although the thought of such traumas can be scary, talking with those who have gone through it will help you reassure yourself that everything will be fine. You can also discuss this with your doctor so you know exactly what to expect and how to deal with it.
You may feel like your vagina has become wider after childbirth
After the baby has passed through the vagina, it may seem wider than before. It may also feel like the vagina is looser, softer, and “opener” [3]. Also, the vagina after childbirth can be traumatized and swollen, but this will most likely pass in a few days.
And although the vagina is unlikely to be the same as before, this is not surprising, and therefore nothing to worry about. Pelvic floor exercises will help tighten the muscles surrounding the vagina in no time! They can be performed without interruption from everyday activities: in line, while watching TV, when the child is sleeping, driving or on the bus while going on business. It is better to start doing such exercises during pregnancy.
It is better to start doing such exercises during pregnancy.
Pelvic floor exercises are also a great way to reduce urinary incontinence, which many women experience after childbirth. .
You may be worried about vaginal dryness after childbirth
After childbirth, the level of the hormone estrogen in the body decreases compared to what it was during pregnancy. This is why you feel dryness in the vagina after childbirth. If you are breastfeeding, your estrogen levels will be lower than if you are formula feeding.
If vaginal dryness after childbirth bothers you, especially after returning to a regular sex life, use a lubricant and see how much more comfortable you feel! Of course, often sex is far from the main thing that worries after the birth of a child; during this period, reduced libido is completely normal [4]! Talk to your partner - together you will work through your insecurities and figure out how to make sex as comfortable as possible for you when you are ready for it. If dryness continues to bother you or you experience pain, see your doctor for advice.
If dryness continues to bother you or you experience pain, see your doctor for advice.
Vulva pain
Your vulva has been through a lot, especially if your perineum was stitched up after a tear or an episiotomy during childbirth. You may be experiencing pain, but it will likely go away within 6-12 weeks after giving birth. Painkillers can be used, but check with your doctor first if you're breastfeeding. Be patient a little: your condition will improve every day, and, in the end, the pain will be left behind.
While the body is recovering, it is important to maintain intimate hygiene by controlling postpartum discharge. Change your pads frequently, wash your hands before changing them, and bathe or shower regularly. After a while everything should be back to normal.
It is important that a new mother takes care of herself, both physically and mentally.
Ask your partner or loved ones for help to be able to take some time for yourself, even when everything is upside down: turn on pleasant music, light a few candles and relax in the bath.
What does the belly and body look like after childbirth?
Not only the intimate area (vagina, vulva and bikini area) changes after childbirth. Your whole body is being rebuilt: first it was growing life, and now it is adapting to nourish it. Here are a couple of completely natural changes that you can see in the mirror:
What your belly looks like after giving birth This is because the muscles and skin have stretched.
Even if you think you need to get back in shape as soon as possible, it's important to remember that not having a flat abs is completely normal. You've been busy carrying the little man and taking care of him, thank you! Eat right, exercise when you are ready, and you will soon feel healthy and strong, and your stomach will gradually decrease in size. It's not a race, and there's no need to compare yourself to other new moms or Instagram bloggers. Move at your own pace and everything will work out when the time is right.
Stretch marks after pregnancy
Stretch marks appear when the skin is stretched and torn in places. They can be pink, red, brown, black, silver, or even purple depending on skin type, and appear on the abdomen, upper thighs, and chest. This happens to 8 out of 10 pregnant women [5], so you are not alone. Over time, they will become paler, not as noticeable. Think of stretch marks as a great reminder of how strong you are.
Your body is capable of many things - it can change, grow and regenerate to give new life. At first, after childbirth, it will look a little strange, but this is not surprising. Be proud of what you've been through, take care of yourself, take the time to take care of yourself, and don't neglect your health and well-being. Even when your sweet little one is screaming, remember that you can handle everything, and even if everything is falling apart, your partner, friends and family will always come to the rescue.
If you want to know more about what can happen after childbirth, read our articles on postpartum discharge and when to expect your first period after pregnancy.
Medical disclaimer
The medical information contained in this article is for reference only and should not be used for any diagnostic or therapeutic purposes. Consult a doctor about a specific disease
Links:
note-1 [1] https://www.nct.org.uk/labour-birth/you-after-birth/episiotomy-during-childbirth
note-2 [2] https:// www.rcog.org.uk/en/patients/tears/tears-childbirth/
note-3 [3] https://www.nhs.uk/live-well/sexual-health/vagina-changes- after-childbirth/
note-4 [4] https://www.nhs.uk/conditions/loss-of-libido/
note-5 [5] https://www.nhs. uk/conditions/pregnancy-and-baby/stretch-marks-pregnant/
Childbirth perineal incision
why it is needed
In obstetrics, the term "perineum" means a small distance between the vagina and the anus. It is this place that obstetrician-gynecologists mean when they talk about a rupture or incision of the perineum. During childbirth, the baby's head moves through the birth canal and reaches the pelvic floor, stretching the muscles and skin of the perineum. The maximum load on the perineal tissue is experienced during the second stage of labor, when the baby's head erupts. It is at this point that the perineum may rupture. To prevent this from happening, and do episiotomy - surgical incision in the perineum, between the vagina and anus . A surgical incision is always better than a spontaneous rupture, because it has smooth edges and will heal faster than a laceration. In addition, the doctor can control the length of the incision, and a spontaneous rupture runs the risk of stretching both over a long distance and to a great depth.
During childbirth, the baby's head moves through the birth canal and reaches the pelvic floor, stretching the muscles and skin of the perineum. The maximum load on the perineal tissue is experienced during the second stage of labor, when the baby's head erupts. It is at this point that the perineum may rupture. To prevent this from happening, and do episiotomy - surgical incision in the perineum, between the vagina and anus . A surgical incision is always better than a spontaneous rupture, because it has smooth edges and will heal faster than a laceration. In addition, the doctor can control the length of the incision, and a spontaneous rupture runs the risk of stretching both over a long distance and to a great depth.
how it happens
The perineum is cut at the end of the second stage of labor, if there are characteristic signs of an impending rupture - protrusion of the perineum, cyanosis, swelling, pallor of the skin. The incision is about 2–3 cm long, with minimal blood loss. And most importantly - this manipulation is completely painless: at the height of the attempts, the tissues of the perineum are so overstretched that the blood flow in them stops, respectively, pain is not felt . But the incision is sewn under local anesthesia, so again the woman does not feel any severe pain, they do this after the baby and the placenta are born. While the mother is in the maternity hospital, the midwife of the postpartum department treats the stitches with antiseptics every day. Sometimes in the first three days, with swelling in the area of \u200b\u200bthe seams, ice is applied to them.
And most importantly - this manipulation is completely painless: at the height of the attempts, the tissues of the perineum are so overstretched that the blood flow in them stops, respectively, pain is not felt . But the incision is sewn under local anesthesia, so again the woman does not feel any severe pain, they do this after the baby and the placenta are born. While the mother is in the maternity hospital, the midwife of the postpartum department treats the stitches with antiseptics every day. Sometimes in the first three days, with swelling in the area of \u200b\u200bthe seams, ice is applied to them.
and then what?
Women who have had a perineal incision during childbirth will have to follow certain rules. If after a normal birth with an episiotomy, walking is allowed almost immediately (by the end of the first day for sure), then you can’t sit after an episiotomy for two whole weeks - and this is the main inconvenience after this manipulation. It will be necessary to feed the child in a lying position, and she herself will have to stand or lie down. If you still need to sit down (for example, you have to travel in a car), you can use seat pad (sold in pharmacies) or children's inflatable swimming ring. It will be possible to sit down completely when the stitches are completely healed: most often this happens in the first two weeks after childbirth.
It will be necessary to feed the child in a lying position, and she herself will have to stand or lie down. If you still need to sit down (for example, you have to travel in a car), you can use seat pad (sold in pharmacies) or children's inflatable swimming ring. It will be possible to sit down completely when the stitches are completely healed: most often this happens in the first two weeks after childbirth.
In the first few days after childbirth, do not push too hard during a bowel movement, if necessary, you can use a laxative.
taking care of the suture
· At home, you need to continue treating the incision site - even at the maternity hospital, you should ask the doctor what kind of antiseptic is needed and how often the suture should be treated.
· In order for the incision to heal faster and better, it is necessary to change the maternity pads frequently - every 3-4 hours. You can also give yourself air baths once or twice a day.
· After each visit to the toilet, wash the external genitalia and gently pat dry the perineum. In addition to ordinary running water, you can use a solution of chamomile, calendula.
· If there is swelling in the area of the stitches, then you can apply a chilled gel pack, ice to them for a short time.
pay attention
Some time after the episiotomy, there may be some pain in the suture area, burning, discomfort, irritation and swelling of the skin is possible - this is a normal phenomenon: after all, there was a surgical intervention and it takes time for the tissues to recover. In general, the perineal incision heals most often without complications - only a small skin scar remains, which becomes almost invisible over time.
But sometimes healing is delayed or complicated by some kind of inflammation, for example, this happens if a woman has colpitis - inflammation of the vagina. Then the pain, swelling either intensifies, or simply does not go away for a long time, in the area of \u200b\u200bthe seam there is a feeling of pulsation, twitching, bursting, and there may even be purulent discharge. Then you should immediately consult a doctor, he will examine the seam and prescribe treatment.
Then you should immediately consult a doctor, he will examine the seam and prescribe treatment.
how to avoid
Of course, episiotomy during childbirth is not done for everyone, but only according to indications. But still, every woman wants to avoid it. To do this, you need to behave correctly in childbirth: the main thing is not to pinch, you must, on the contrary, try to “open up” as much as possible in order to release the child. How to do this, as well as how to behave in and between contractions, how to breathe, what positions to take, how to reduce labor pain, future parents will be taught at school. Such preparation, as well as an optimistic attitude, will help to endure the birth and, possibly, avoid an incision.
Also, from 36 weeks of pregnancy, perineal massage with oil can be performed daily. And although there are no statistics that such a massage reduces the likelihood of an episiotomy, nevertheless, the perineal tissues will be slightly moistened, stretched, the woman will feel her body better - all this is also a small prevention of surgical manipulation.