Belly button cover
How To Clean Your Baby's Belly Button, Because It's Not Exactly Ready For Bathing
By Elizabeth Helen Spencer
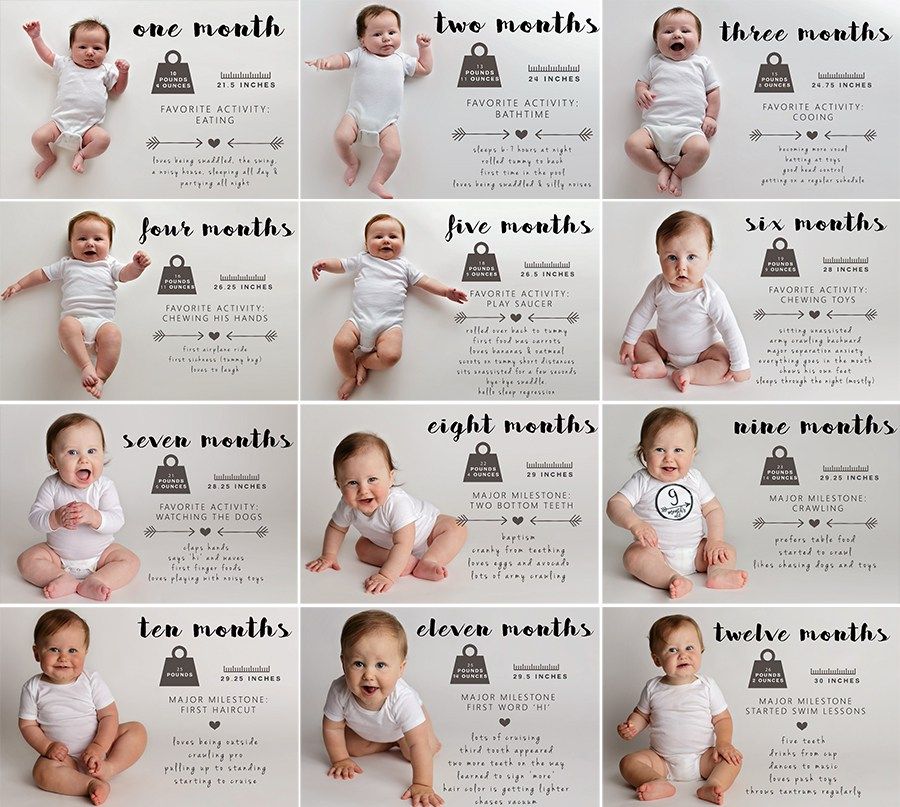
For 40 weeks or so of pregnancy, you planned and anticipated. Now the picture in your mind is a living and breathing newborn. After a short hospital stay that often feels too brief, you get to take baby home and care for them without the assistance of the nursing team. For many new parents, this transition is a shock, regardless of how many books you read. There's so much to do and newborn belly button care is no small part of your to-do list. Knowing how to clean your baby's belly button is important and honestly, you're probably too sleep deprived to remember the instructions from the hospital. Both the World Health Organization (WHO) and the American Academy of Pediatrics (AAP) recommend a dry approach to belly button care until the umbilical cord stump falls off within the first one to two weeks of life.
What does "dry care" mean when it comes to your baby's belly button? "Simply keeping the umbilical cord clean and dry," Catherine Gritchen, a pediatrician at Miller Children's and Women's Hospital in Long Beach, California, tells Romper over email. Before 1998, when WHO changed its recommendation to dry care, the standard approach to belly button care was to apply antibacterial or antiseptic topical care to the cord stump. However, explains Gritchen, "Using any type of antibacterial application (such as alcohol or triple dye) actually tends to delay the cord separation because it kills off the beneficial bacteria that help with separation. Also, it can select for opportunistic 'bad' bacteria, actually increasing the chance of infection." In poorer countries where clean water and hygiene are not guaranteed, this "wet" approach is still used, but it is no longer necessary or considered best practice in the United States.
While we commonly think and refer to it as a belly button, it's important to keep in mind that a newborn doesn't really have a belly button until their umbilical cord stump falls off. Until then, "the umbilical cord stump is a healing tissue from the placenta," explains Trung Tristan Truong, MD a pediatrician at MemorialCare Saddleback Medical Center in Laguna Hills, California. This is why infection (called omphalitis), if it occurs, can be serious. Babies need to receive intravenous antibiotic therapy in the hospital if they contract omphalitis.
This is why infection (called omphalitis), if it occurs, can be serious. Babies need to receive intravenous antibiotic therapy in the hospital if they contract omphalitis.
As part of baby's daily routine until the cord stump falls off, "you should keep the umbilical cord dry and fold the diaper down below the cord so that it doesn’t get wet from urine," Gina Posner, a pediatrician at Orange Coast Medical Center in Fountain Valley, California, tells Romper over email. This means no immersive bathing (sponge baths are okay) during the period of cord stump care. "If the cord stump comes into contact with urine or fecal matter, just clean it with water," adds Truong.
"After the cord falls off, the stump may be moist and have bit of bleeding around the edges," says Gritchen. You can "simply wash with soap and water and pat dry," she adds. After the belly button area is completely healed and dry, you can begin a normal bath rountine for your baby.
Luckily, all three doctors say the instructions for belly button cleaning and care are the same whether you're one month old or an adult: treat it like any other creased or folded area of skin. Don't rub too hard, be gentle, and use a Q-tip if you need to remove debris or water. Everyone’s belly button scar is unique, and beyond the inner/outie dichotomy, some navals are deeper or more folded than others. As your newborn grows into an older baby and young toddler, belly buttons (theirs, yours, the whole family's) become a source of amusement. You'll hardly remember struggling to get the plastic clamp off all those months ago.
Don't rub too hard, be gentle, and use a Q-tip if you need to remove debris or water. Everyone’s belly button scar is unique, and beyond the inner/outie dichotomy, some navals are deeper or more folded than others. As your newborn grows into an older baby and young toddler, belly buttons (theirs, yours, the whole family's) become a source of amusement. You'll hardly remember struggling to get the plastic clamp off all those months ago.
Tags
Wellness Care
Article
Watch Out for Hidden Sugars
Read More arrow-rightArticle
Travel Safety
Read More arrow-rightArticle
Protecting Your Skin Through Summer
Read More arrow-rightOutie Belly Button Cause for Concern? What You Need to Know
Belly buttons come in all shapes and sizes. There are innies and outies. Pregnant women often have their innie become an outie temporarily when their bellies grow. A few people don’t even have a belly button to speak of. The majority of belly buttons are innies. This doesn’t mean that having an outie is a cause for concern, though.
A few people don’t even have a belly button to speak of. The majority of belly buttons are innies. This doesn’t mean that having an outie is a cause for concern, though.
Almost immediately after birth, a baby’s umbilical cord is clamped and cut, leaving an umbilical stump. Within one to three weeks, the stump dries and shrivels up, eventually falling off. The baby is sometimes left with scar tissue, some more than others. The amount of space between the skin and abdominal wall may also have something to do with how much of the stump remains visible or tucks away. Contrary to popular belief, it has nothing to do with how the cord was cut or the competence of your doctor or midwife.
How a baby’s umbilical cord is clamped or cut has nothing to do with baby ending up with an outie. An outie is normal and not usually a medical concern, only a cosmetic one for some.
For some infants, the cause of an outie belly button may be an umbilical hernia or granuloma.
Umbilical hernia
Most umbilical hernias are harmless. They occur when part of the intestine bulges through the umbilical opening in the abdominal muscles. This creates a soft bulge or swelling near the navel that might become more noticeable when the baby cries or strains. They are more common in premature babies, low birth weight babies, and Black infants.
They occur when part of the intestine bulges through the umbilical opening in the abdominal muscles. This creates a soft bulge or swelling near the navel that might become more noticeable when the baby cries or strains. They are more common in premature babies, low birth weight babies, and Black infants.
Umbilical hernias usually close on their own without treatment before the age of 2. They’re usually painless and don’t produce any symptoms in babies and children. Hernias that don’t disappear by the age of 4 may need to be surgically repaired to prevent complications. Rarely, the abdominal tissue can become trapped, reducing blood supply. This can cause pain and increase the risk for tissue damage and infection.
If you believe your baby has an umbilical hernia, speak to a pediatrician. Get emergency medical care if:
- the bulge becomes swollen or discolored
- your baby is in pain
- the bulge is painful to the touch
- your baby begins to vomit
Umbilical granuloma
An umbilical granuloma is a small growth of tissue that forms in the belly button in the weeks after the umbilical cord is cut and the stump falls off. It appears as a small pink or red lump and may be covered in a clear or yellow discharge. It doesn’t usually bother the baby, but it can occasionally become infected and cause symptoms such as skin irritation and fever. It will often go away on its own within a week or two. If it doesn’t, treatment may be required to prevent infection.
It appears as a small pink or red lump and may be covered in a clear or yellow discharge. It doesn’t usually bother the baby, but it can occasionally become infected and cause symptoms such as skin irritation and fever. It will often go away on its own within a week or two. If it doesn’t, treatment may be required to prevent infection.
Once your pediatrician has diagnosed an umbilical granuloma, if there are no signs of infection, it may be treated at home using table salt. To use this method:
- Expose the center of the umbilicus by gently pressing on the surrounding area.
- Apply a small pinch of table salt over the granuloma. Too much can damage the skin.
- Cover with a clean piece of gauze for 30 minutes.
- Clean the area using clean gauze soaked in warm water.
- Repeat twice a day for three days.
If this doesn’t work or if there are signs of infection, the granuloma can be treated in a doctor’s office using silver nitrate to cauterize the granuloma. Topical steroids have been suggested as another treatment.
Topical steroids have been suggested as another treatment.
An outie is harmless and there’s no need to see a doctor. If you’re concerned about a hernia, bring it up at your baby’s next checkup. A doctor can spot a hernia easily and will likely suggest a “watch and wait” approach. There’s no danger to your baby’s health and it will likely resolve on its own over time.
The only time an outie poses a risk is if the intestine becomes trapped.
Chances are you’ve heard the myth that you can prevent an outie by strapping something across a baby’s belly or taping a coin over it. This is pure folklore with no medical merit. Not only will this not change the shape or size of your baby’s belly button, but it could actually be harmful. The coin and tape could irritate your baby’s skin and cause an infection. It’s also a choking hazard should the coin come loose.
An outie belly button is a cosmetic issue and doesn’t require surgery. Granulomas need to be treated to avoid infection. Hernias usually disappear on their own and those that don’t can be treated with a simple surgical procedure after the age of 4 or 5.
Hernias usually disappear on their own and those that don’t can be treated with a simple surgical procedure after the age of 4 or 5.
If your child is bothered by their outie when they get older, speak to their doctor.
To avoid irritation or infection, you’ll need to keep the stump clean and dry until it falls off.
To do this:
- give your baby sponge baths instead of submersing them in a tub
- don’t cover the belly button with their diaper
- use mild soap and water
Call your doctor if the stump hasn’t fallen off in two months or if you notice:
- a foul-smelling discharge
- redness
- signs of tenderness when you touch it or the surrounding skin
- bleeding
An outie belly button isn’t a medical issue. If you’re concerned about a hernia or granuloma, or if your baby appears to be in pain and is showing signs of infection, see your doctor. Otherwise, an outie belly button is just that — a belly button that sticks out — and shouldn’t be a cause for concern.
How to self-administer a hypodermic injection using a pre-filled syringe
Share
Time to read: Approximately 6 min.
This information will help you learn how to give yourself a hypodermic injection (shot) using a pre-filled syringe. A subcutaneous injection is an injection that is given under the skin. A pre-filled syringe is a syringe that is sold with medication already inside.
The health worker will show you how to give the injection yourself. You can use the information in this resource as a reminder when you inject at home.
back to top of pageHow to store pre-filled syringes
How pre-filled syringes are stored depends on the type of medicine they contain. Most medicines are stored at room temperature, but some should be refrigerated. Your healthcare provider will tell you how to store your syringes. Do not store pre-filled syringes in the freezer or expose them to the sun.
If you have questions about storing or transporting pre-filled syringes while traveling, ask your healthcare provider.
What to do if the medicine is frozen
If the medicine inside the syringe is frozen, place it near the front of the refrigerator or on a shelf in the refrigerator door to thaw. Do not use the medicine if it has been frozen more than once. Call your health care provider for further instructions.
back to top of pageHow to self-administer a hypodermic injection
Prepare supplies
Place supplies on a clean, flat surface (such as a dining table or kitchen worktop). You will need:
- 1 alcohol wipe
- 1 small gauze or cotton swab, unless you inject yourself with enoxaparin (Lovenox ® ) or heparin
- 1 dressing (e.g. Band-Aid ® )
- Sturdy container for syringe and needle disposal (e.g. plastic bottle with cap for liquid laundry detergent)
- Read the resource Storage and Disposal of Household Medical Needles for information on selecting a sharps container.
- Read the resource Storage and Disposal of Household Medical Needles for information on selecting a sharps container.
- 1 pre-filled syringe with needle cap
- If you store pre-filled syringes in the refrigerator, remove one syringe 30 minutes before injection. When you inject, the medicine should be at room temperature.
- Do not shake the syringe. Shaking may spoil the medicine in it.
Check the pre-filled syringe
Check the following drug information:
- Name. Make sure it matches the one assigned to you by your healthcare provider.
- Dose. Make sure it matches the one assigned to you by your healthcare provider.
- Expiration date. Check that the expiration date has not expired.
- Colour. Check that the medicine in the syringe is clear and colorless. Do not use if it is foamy, discolored, cloudy or has crystals.
If the drug name or dose does not match what your healthcare provider ordered, if the drug has expired, or if the drug is foaming, discolored, cloudy, or has crystals in it, do not use the syringe. If you have another syringe, use it. Then contact your healthcare professional or pharmacist and let them know. You may be able to bring a full syringe to the pharmacy to have it replaced.
If you have another syringe, use it. Then contact your healthcare professional or pharmacist and let them know. You may be able to bring a full syringe to the pharmacy to have it replaced.
Prepare injection site
Select an injection site on the body where the skin can be pulled back 1 to 2 inches (2.5 to 5 cm). It is best to choose one of the following sites (see picture 1):
- abdomen (abdomen), except for a 2 inch (5 cm) area around the navel;
- middle of anterior or middle of outer thigh;
- upper buttocks;
- back of the upper arm if another person gives you the injection.
If your healthcare provider has asked you to inject at a specific site, follow these guidelines. Some medicines work better when given in certain places. Do not inject into areas that are painful, red, bruised, hard, or have scars or stretch marks.
Figure 1. Injection sites
Give each subsequent injection at a different site. To keep track of places, it is convenient to use a notepad or calendar. The introduction of the drug in the same place leads to the formation of scar tissue. This may cause the medicine to stop working as it should. This will also make it difficult to insert the needle into the skin.
To keep track of places, it is convenient to use a notepad or calendar. The introduction of the drug in the same place leads to the formation of scar tissue. This may cause the medicine to stop working as it should. This will also make it difficult to insert the needle into the skin.
After selecting the injection site, follow the instructions below.
- Wash hands thoroughly with soap and water or use alcohol-based hand rub.
- If you wash your hands with soap and water, wet them, lather them, rub them together thoroughly for 20 seconds, then rinse. Dry your hands with a disposable towel and turn off the faucet with the same towel.
- When using alcohol-based hand rub, be sure to apply it to your hands and rub your hands together until it dries completely.
- Tuck in clothing covering the injection site.
- Open the alcohol pad. Wipe the skin at the injection site with a tissue, pressing it firmly against the skin. Start in the center of the selected area and move to the outer edges in a circular motion.

- Let the leather dry. Do not fan this place and do not blow on it.
Inject yourself
- Take the syringe out of the package.
- If you are injecting Lovenox, make sure there is an air bubble in the syringe. If there is no vial, put this syringe aside and use another one. After you give yourself an injection, contact your healthcare provider or pharmacist and let them know. You may be able to bring a full syringe to the pharmacy to have it replaced.
- With your dominant hand (the hand you use to write), grasp the middle of the syringe like a pen or a darts.
- Carefully remove the cap from the needle (see Figure 2). After removing the cap from the needle, do not put the syringe. Take care not to let anything, not even your fingers, touch the needle. If anything touches the needle, place the syringe in a sharps container. Start the procedure again with a new syringe. After you inject yourself, contact your healthcare provider and let them know.

Figure 2 Remove the cap from the needle
- If you are injecting yourself with a medicine other than Lovenox, check the syringe for air bubbles. If there is a bubble in the syringe, hold the syringe with the needle pointing up. Gently tap the syringe with your fingers so that air bubbles rise to the top of the syringe, closer to the needle. Slowly press the plunger to release air bubbles from the syringe. Do not do this with Lovenox.
- Make sure you continue to hold the syringe in the middle as you would a pen or a dart. Use your free hand to pull back the skin at the injection site.
- In one even and quick motion, fully insert the needle at a right angle into the skin (see Figure 3). Don't put your thumb on the piston just yet.
Figure 3. Figure 3. Insert the needle into the skin
- Stop pulling the skin. Slowly press down on the plunger with your thumb and lower it all the way down until all of the medicine has been injected (see Figure 4).
 You can use the thumb of either hand for your convenience.
You can use the thumb of either hand for your convenience. Figure 4. Push piston all the way down
- When the syringe is empty, pull the needle straight up from the skin.
- Do not put pressure on the injection site if you have injected yourself with Lovenox or heparin. If necessary, apply a bandage to the injection site.
- If you have injected yourself with any other medicine other than Lovenox and heparin, place a cotton swab or gauze over the injection site and hold it down for a few seconds. If necessary, apply a bandage to the injection site.
- Attach the needle guard.
- If you have injected yourself with Lovenox, push the plunger down hard and push it all the way down. The protective cap should sit on its own in the right place.
- If you are injecting any medication other than Lovenox, grasp the clear plastic finger rests on the sides of the syringe with one hand.
 Grab the guard with your other hand (see figure 5). Slide the needle guard over the needle until the needle is completely covered (see Figure 6). You will hear a click when the guard snaps into place.
Grab the guard with your other hand (see figure 5). Slide the needle guard over the needle until the needle is completely covered (see Figure 6). You will hear a click when the guard snaps into place. Figure 5. Take the protective cap
Figure 6. Slide on the guard
- Discard the syringe in a sharps container. Do not reuse a pre-filled syringe.
For information on how to choose a sharps container and dispose of used syringes and other household medical needles, see our resource Storing and Disposing of Household Medical Needles.
back to top of pageWhen should you contact your healthcare provider?
Call your healthcare provider if you have any of the following symptoms:
- The injection site does not stop bleeding.
- You are in very severe pain.
- You injected the medicine in the wrong place.
- You have a fever of 100.4°F (38°C) or higher.
- You have signs of an allergic reaction, such as swelling, redness, itching, or a rash.

- You cannot use the syringe because the medicine has expired, the medicine is foamy, discolored, cloudy, or has crystals in it.
- You cannot use the syringe because you touched something with the needle before you injected.
- You cannot use a pre-filled Lovenox syringe because it does not contain an air bubble.
- You have difficulty getting an injection.
You must have JavaScript enabled to use this form.
Share your opinion
Give us your feedback
Your feedback will help us improve the information we provide to patients and caregivers.
Questions
| Questions | Yes | To some extent | No |
|---|---|---|---|
| Was this information easy for you to understand? | Yes | To some extent | No |
What should be explained in more detail?
Date last updated
Can the navel untie | Cuprum
We use cookies
to improve our experience!
Good
Author: Valeria Zhukova
August 24, 2022
597 views
“Don't overstrain, otherwise the navel will untie”, familiar phrase? As children, we understood it literally, and when we grew up, we realized that . .. Although wait a minute, the question of why the navel should be untied was still open.
.. Although wait a minute, the question of why the navel should be untied was still open.
The navel is just a scar where the umbilical cord was cut. Therefore, the navel cannot be untied.
The appearance of the navel begins to take shape during the healing process. Navels are different: convex and sunken - round, almond-shaped, horizontal, spiral shape. Any form is perfectly normal. Therefore, the appearance of the navel is just another unique feature of a person.
But in the case of a protruding navel, there is something to watch out for. This shape may be a sign that a person has an umbilical hernia.
Hernias occur when an internal organ protrudes through the wall of a muscle or other tissue. An umbilical hernia occurs when fatty tissue or part of the intestine bulges near the navel.
Umbilical hernias can occur in both newborns and adults. In infants, they appear in 10-20% of cases, in adults - in 3-10%.
In infants, they appear in 10-20% of cases, in adults - in 3-10%.
There are several reasons for an umbilical hernia:
- When a baby is in the womb, he receives all the necessary nutrients from his mother through the umbilical cord. It passes through the muscles of the anterior abdominal wall, creating an area that usually tightens after birth. If this does not happen, a hernia may form in this place.
- An adult can "earn" a hernia when there is a lot of tension in the abdomen, for example due to constant constipation, being overweight, after childbirth, or even with frequent severe coughing.
An umbilical hernia usually does not cause discomfort or pain. You can determine a hernia when a person is sitting, laughing, coughing or sneezing - with tension in the abdominal muscles. In the supine position, it becomes invisible.
If you suspect that you have an umbilical hernia, you should see your doctor. He will conduct an examination, and in some cases recommend a CT scan.
Most pediatric umbilical hernias resolve without intervention by 3-4 years of age. If the hernia is more than two centimeters, there is a risk of infringement (compression), which means that the child may need surgery.
After the operation, the doctor will prescribe painkillers and give advice on care:
- The child should not take a bath for several days. To help him maintain hygiene, use a damp sponge. Do not wet the operated area, with light movements, blotting, wash the baby.
- Sports activities, active play such as cycling should be avoided. The doctor will tell you when you can return to the usual rhythm of life.
- Diet: Eat vegetables, fruits, high fiber foods, and drink plenty of water.
 Diet is needed to avoid constipation.
Diet is needed to avoid constipation.
The incision site should heal within four to six weeks. The skin will be delicate, so it needs to be protected from the sun. Also, do not wear scratchy and uncomfortable clothing that can rub.
If an umbilical hernia is found in an adult , then it will not disappear by itself. Surgery is most often recommended to avoid complications.
After the examination, the surgeon will recommend the most suitable type of surgery:
- Laparotomy surgery. An incision is made at the location of the hernia, the protruding tissues are returned to their place, the muscles are sutured. In some cases, a mesh is implanted for additional support.
- Laparoscopic surgery. Similar to laparotomy, but instead of an incision, small incisions are made to insert surgical instruments.

- Robotic hernioplasty. The operation is done through a small incision, the surgeon sits at the console and controls the robotic system.
Unlike babies, a hernia in an adult will not go away on its own. Over time, it can increase in size, start to hurt and cause complications:
- Infringement. Part of the intestine gets stuck in the muscles, as a result, a person feels severe sharp pain, nausea and vomiting appear.
- Violation of the blood supply. A hernia occludes part of the intestine in such a way that it cuts off blood flow in it. In this case, an emergency operation is necessary in order to prevent tissue death.
Hernia is preventable:
- Exercise and eat healthy. Include fruits, vegetables, and whole grains in your diet.
- Do not lift heavy objects.