Back and pelvic pain during pregnancy
Back pain in pregnancy - NHS
It is very common to get backache or back pain during pregnancy, especially in the early stages.
During pregnancy, the ligaments in your body naturally become softer and stretch to prepare you for labour. This can put a strain on the joints of your lower back and pelvis, which can cause back pain.
Avoiding and easing back pain in pregnancy
Try these tips:
- bend your knees and keep your back straight when you lift or pick something up from the floor
- avoid lifting heavy objects
- move your feet when you turn to avoid twisting your spine
- wear flat shoes to evenly distribute your weight
- try to balance the weight between 2 bags when carrying shopping
- keep your back straight and well supported when sitting – look for maternity support pillows
- get enough rest, particularly later in pregnancy
- have a massage or a warm bath
- use a mattress that supports you properly – you can put a piece of hardboard under a soft mattress to make it firmer, if necessary
- go to a group or individual back care class
You can take paracetamol to ease back pain while you are pregnant, unless your GP or midwife says not to. Always follow the instructions on the packet.
When to get help for back pain in pregnancy
If your backache is very painful, talk to your GP or midwife. They may be able to refer you to an obstetric physiotherapist at your hospital, who can give you advice and may suggest some helpful exercises.
Non-urgent advice: Contact your GP or midwife urgently if:
You have back pain and you:
- are in your second or third trimester – this could be a sign of early labour
- also have a fever, bleeding from your vagina or pain when you pee
- have pain in one or more of your sides (under your ribs)
Immediate action required: Call 999 or go to A&E if:
You have back pain and:
- you lose feeling in one or both of your legs, your bum, or your genitals
Exercises to ease back pain in pregnancy
This gentle exercise helps to strengthen stomach (abdominal) muscles, which can ease back pain in pregnancy:
Credit:
Agencja FREE / Alamy Stock Photo https://www. alamy.com/stock-photo-pregnant-woman-doing-exercises-32344372.html?pv=1&stamp=2&imageid=FC98903A-AC65-4C38-BF96-00BB1F4352CB&p=29056&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3dbar%26st%3d0%26pn%3d1%26ps%3d100%26sortby%3d2%26resultview%3dsortbyPopular%26npgs%3d0%26qt%3dBTHBG4%26qt_raw%3dBTHBG4%26lic%3d3%26mr%3d0%26pr%3d0%26ot%3d0%26creative%3d%26ag%3d0%26hc%3d0%26pc%3d%26blackwhite%3d%26cutout%3d%26tbar%3d1%26et%3d0x000000000000000000000%26vp%3d0%26loc%3d0%26imgt%3d0%26dtfr%3d%26dtto%3d%26size%3d0xFF%26archive%3d1%26groupid%3d%26pseudoid%3d387440%26a%3d%26cdid%3d%26cdsrt%3d%26name%3d%26qn%3d%26apalib%3d%26apalic%3d%26lightbox%3d%26gname%3d%26gtype%3d%26xstx%3d0%26simid%3d%26saveQry%3d%26editorial%3d1%26nu%3d%26t%3d%26edoptin%3d%26customgeoip%3d%26cap%3d1%26cbstore%3d1%26vd%3d0%26lb%3d%26fi%3d2%26edrf%3d0%26ispremium%3d1%26flip%3d0%26pl%3d
alamy.com/stock-photo-pregnant-woman-doing-exercises-32344372.html?pv=1&stamp=2&imageid=FC98903A-AC65-4C38-BF96-00BB1F4352CB&p=29056&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3dbar%26st%3d0%26pn%3d1%26ps%3d100%26sortby%3d2%26resultview%3dsortbyPopular%26npgs%3d0%26qt%3dBTHBG4%26qt_raw%3dBTHBG4%26lic%3d3%26mr%3d0%26pr%3d0%26ot%3d0%26creative%3d%26ag%3d0%26hc%3d0%26pc%3d%26blackwhite%3d%26cutout%3d%26tbar%3d1%26et%3d0x000000000000000000000%26vp%3d0%26loc%3d0%26imgt%3d0%26dtfr%3d%26dtto%3d%26size%3d0xFF%26archive%3d1%26groupid%3d%26pseudoid%3d387440%26a%3d%26cdid%3d%26cdsrt%3d%26name%3d%26qn%3d%26apalib%3d%26apalic%3d%26lightbox%3d%26gname%3d%26gtype%3d%26xstx%3d0%26simid%3d%26saveQry%3d%26editorial%3d1%26nu%3d%26t%3d%26edoptin%3d%26customgeoip%3d%26cap%3d1%26cbstore%3d1%26vd%3d0%26lb%3d%26fi%3d2%26edrf%3d0%26ispremium%3d1%26flip%3d0%26pl%3d
1) Start on all fours with knees under hips, hands under shoulders, fingers facing forwards and stomach muscles lifted to keep your back straight.
Credit:
Agencja FREE / Alamy Stock Photo https://www.alamy.com/stock-photo-pregnant-woman-doing-exercises-32344367.html?pv=1&stamp=2&imageid=DA3DDA5D-3D86-471C-9DFB-66A032C21750&p=29056&n=440&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3Dbar%26st%3D0%26sortby%3D3%26qt%3D%2520Pregnant%2520woman%2520doing%2520exercises%26qt_raw%3D%2520Pregnant%2520woman%2520doing%2520exercises%26qn%3D%26lic%3D3%26edrf%3D0%26mr%3D0%26pr%3D0%26aoa%3D1%26creative%3D%26videos%3D%26nu%3D%26ccc%3D%26bespoke%3D4%26apalib%3D%26ag%3D0%26hc%3D0%26et%3D0x000000000000000000000%26vp%3D0%26loc%3D0%26ot%3D0%26imgt%3D0%26dtfr%3D%26dtto%3D%26size%3D0xFF%26blackwhite%3D%26cutout%3D%26archive%3D1%26name%3D%26groupid%3D%26pseudoid%3D%26userid%3D%26id%3D%26a%3D%26xstx%3D0%26cbstore%3D0%26resultview%3DsortbyRelevant%26lightbox%3D%26gname%3D%26gtype%3D%26apalic%3D%26tbar%3D1%26pc%3D%26simid%3D%26cap%3D1%26customgeoip%3DGB%26vd%3D0%26cid%3D%26pe%3D%26so%3D%26lb%3D%26pl%3D0%26plno%3D%26fi%3D0%26langcode%3Den%26upl%3D0%26cufr%3D%26cuto%3D%26howler%3D%26cvrem%3D0%26cvtype%3D0%26cvloc%3D0%26cl%3D0%26upfr%3D%26upto%3D%26primcat%3D%26seccat%3D%26cvcategory%3D*%26restriction%3D%26random%3D%26ispremium%3D1%26flip%3D0%26contributorqt%3D%26plgalleryno%3D%26plpublic%3D0%26viewaspublic%3D0%26isplcurate%3D0%26imageurl%3D%26saveQry%3D%26editorial%3D%26t%3D0%26edoptin%3D%26apaid%3D%7B18B189B6-6A83-41BD-8442-2448A6B7E281%7D%26custspecid%3D14369B5F-24B7-4344-B743-D5DE569A1F46
2) Pull in your stomach muscles and raise your back up towards the ceiling, letting your head and bum relax downwards gently – do not let your elbows lock and only move your back as far as you comfortably can.
Credit:
Agencja FREE / Alamy Stock Photo https://www.alamy.com/stock-photo-pregnant-woman-doing-exercises-32344372.html?pv=1&stamp=2&imageid=FC98903A-AC65-4C38-BF96-00BB1F4352CB&p=29056&n=0&orientation=0&pn=1&searchtype=0&IsFromSearch=1&srch=foo%3dbar%26st%3d0%26pn%3d1%26ps%3d100%26sortby%3d2%26resultview%3dsortbyPopular%26npgs%3d0%26qt%3dBTHBG4%26qt_raw%3dBTHBG4%26lic%3d3%26mr%3d0%26pr%3d0%26ot%3d0%26creative%3d%26ag%3d0%26hc%3d0%26pc%3d%26blackwhite%3d%26cutout%3d%26tbar%3d1%26et%3d0x000000000000000000000%26vp%3d0%26loc%3d0%26imgt%3d0%26dtfr%3d%26dtto%3d%26size%3d0xFF%26archive%3d1%26groupid%3d%26pseudoid%3d387440%26a%3d%26cdid%3d%26cdsrt%3d%26name%3d%26qn%3d%26apalib%3d%26apalic%3d%26lightbox%3d%26gname%3d%26gtype%3d%26xstx%3d0%26simid%3d%26saveQry%3d%26editorial%3d1%26nu%3d%26t%3d%26edoptin%3d%26customgeoip%3d%26cap%3d1%26cbstore%3d1%26vd%3d0%26lb%3d%26fi%3d2%26edrf%3d0%26ispremium%3d1%26flip%3d0%26pl%3d
3) Hold for a few seconds then slowly return to the box position – take care not to hollow your back, it should always return to a straight, neutral position.
4) Do this slowly and rhythmically 10 times, making your muscles work hard and moving your back carefully.
Doing prenatal yoga or aquanatal classes (gentle exercise classes in water) with a qualified instructor can also help build your muscles to better support your back. Ask at your local leisure centre.
Page last reviewed: 15 March 2021
Next review due: 15 March 2024
Pelvic pain in pregnancy - NHS
Some women may develop pelvic pain in pregnancy. This is sometimes called pregnancy-related pelvic girdle pain (PGP) or symphysis pubis dysfunction (SPD).
PGP is a collection of uncomfortable symptoms caused by a stiffness of your pelvic joints or the joints moving unevenly at either the back or front of your pelvis.
Symptoms of PGP
PGP is not harmful to your baby, but it can be painful and make it hard to get around.
Women with PGP may feel pain:
- over the pubic bone at the front in the centre, roughly level with your hips
- across 1 or both sides of your lower back
- in the area between your vagina and anus (perineum)
- spreading to your thighs
Some women may feel or hear a clicking or grinding in the pelvic area.
The pain can be worse when you're:
- walking
- going up or down stairs
- standing on 1 leg (for example, when you're getting dressed)
- turning over in bed
- moving your legs apart (for example, when you get out of a car)
Most women with PGP can have a vaginal birth.
Non-urgent advice: Call your midwife or GP if you have pelvic pain and:
- it's hard for you to move around
- it hurts to get out of a car or turn over in bed
- it's painful going up or down stairs
These can be signs of pregnancy-related pelvic girdle pain.
Treatments for PGP
Getting diagnosed as early as possible can help keep pain to a minimum and avoid long-term discomfort.
You can ask your midwife for a referral to a physiotherapist who specialises in obstetric pelvic joint problems.
Physiotherapy aims to relieve or ease pain, improve muscle function, and improve your pelvic joint position and stability.
This may include:
- manual therapy to make sure the joints of your pelvis, hip and spine move normally
- exercises to strengthen your pelvic floor, stomach, back and hip muscles
- exercises in water
- advice and suggestions, including positions for labour and birth, looking after your baby and positions for sex
- pain relief, such as TENS
- equipment, if necessary, such as crutches or pelvic support belts
These problems tend not to get completely better until the baby is born, but treatment from an experienced practitioner can improve the symptoms during pregnancy.
You can contact the Pelvic Partnership for information and support.
Coping with pelvic pain in pregnancy
Your physiotherapist may recommend a pelvic support belt to help ease your pain, or crutches to help you get around.
It can help to plan your day so you avoid activities that cause you pain. For example, do not go up or down stairs more often than you have to.
The Pelvic, Obstetric & Gynaecological Physiotherapy (POGP) network also offers this advice:
- be as active as possible within your pain limits, and avoid activities that make the pain worse
- rest when you can
- ask your family, friends or partner, if you have one, to help with everyday activities
- wear flat, supportive shoes
- sit down to get dressed – for example, do not stand on 1 leg when putting on jeans
- keep your knees together when getting in and out of the car – a plastic bag on the seat can help you swivel
- sleep in a comfortable position – for example, on your side with a pillow between your legs
- try different ways of turning over in bed – for example, turning over with your knees together and squeezing your buttocks
- take the stairs 1 at a time, or go upstairs backwards or on your bottom
- if you're using crutches, have a small backpack to carry things in
- if you want to have sex, consider different positions, such as kneeling on all fours
POGP suggests that you avoid:
- standing on 1 leg
- bending and twisting to lift, or carrying a baby on 1 hip
- crossing your legs
- sitting on the floor, or sitting twisted
- sitting or standing for long periods
- lifting heavy weights, such as shopping bags, wet washing or a toddler
- vacuuming
- pushing heavy objects, such as a supermarket trolley
- carrying anything in only 1 hand (try using a small backpack)
The physiotherapist should be able to provide advice on coping with the emotional impact of living with chronic pain, such as using relaxation techniques. If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
Download the POGP leaflet Pregnancy-related pelvic girdle pain for mothers-to-be and new mothers.
You can get more information on managing everyday activities with PGP from the Pelvic Partnership.
Labour and birth with pelvic pain
Many women with pelvic pain in pregnancy can have a normal vaginal birth.
Plan ahead and talk about your birth plan with your birth partner and midwife.
Write in your birth plan that you have PGP, so the people supporting you during labour and birth will be aware of your condition.
Think about birth positions that are the most comfortable for you, and write them in your birth plan.
Being in water can take the weight off your joints and allow you to move more easily, so you might want to think about having a water birth. You can discuss this with your midwife.
You can discuss this with your midwife.
Your 'pain-free range of movement'
If you have pain when you open your legs, find out your pain-free range of movement.
To do this, lie on your back or sit on the edge of a chair and open your legs as far as you can without pain.
Your partner or midwife can measure the distance between your knees with a tape measure. This is your pain-free range.
To protect your joints, try not to open your legs wider than this during labour and birth.
This is particularly important if you have an epidural for pain relief in labour, as you won't be feeling the pain that warns you that you're separating your legs too far.
If you have an epidural, make sure your midwife and birth partner are aware of your pain-free range of movement of your legs.
When pushing in the second stage of labour, you may find it beneficial to lie on one side.
This prevents your legs from being separated too much. You can stay in this position for the birth of your baby, if you wish.
Sometimes it might be necessary to open your legs wider than your pain-free range to deliver your baby safely, particularly if you have an assisted delivery (for example, with the vacuum or ventouse).
Even in this case, it's possible to limit the separation of your legs. Make sure your midwife and doctor are aware that you have PGP.
If you go beyond your pain-free range, your physiotherapist should assess you after the birth.
Take extra care until they have assessed and advised you.
Who gets pelvic pain in pregnancy?
It's estimated that PGP affects up to 1 in 5 pregnant women to some degree.
It's not known exactly why pelvic pain affects some women, but it's thought to be linked to a number of issues, including previous damage to the pelvis, pelvic joints moving unevenly, and the weight or position of the baby.
Factors that may make a woman more likely to develop PGP include:
- a history of lower back or pelvic girdle pain
- previous injury to the pelvis (for example, from a fall or accident)
- having PGP in a previous pregnancy
- a physically demanding job
- being overweight
- having a multiple birth pregnancy
healthtalk.org has interviews with women talking about their experiences of pelvic pain in pregnancy.
Read more about coping with common pregnancy problems, including nausea, heartburn, tiredness and constipation.
Find maternity services or physiotherapy services near you.
Community content from HealthUnlockedMethods for the prevention and treatment of pain in the lumbar region and pelvic region during pregnancy
Review question
We were looking for evidence of the effect of any treatment used to prevent or treat low back pain, pelvic pain, or both during pregnancy. We would also like to know if the treatment reduced disability or sick leave, and if the treatment caused any side effects for pregnant women.
We would also like to know if the treatment reduced disability or sick leave, and if the treatment caused any side effects for pregnant women.
Relevance
Pain in the lumbar region, pelvic region, or both is a common complaint during pregnancy, often progressing as the pregnancy progresses. This pain can interfere with the daily activities, work, and sleep of pregnant women. We wanted to find out which treatment or combination of treatment options would be better than conventional prenatal care for pregnant women with these complaints.
Study profile
This evidence is current to 19 January 2015. We included 34 randomized trials with 5,121 pregnant women aged 16 to 45 in this updated review. The women were between 12 and 38 weeks pregnant. Studies have looked at various treatments for pregnant women with low back pain, pelvic pain, or both types of pain. All treatments were added to routine antenatal care and only compared to routine antenatal care in 23 studies. Symptoms in women in the studies were assessed in many ways, from self-reported pain to sick leave with the results of special tests.
Symptoms in women in the studies were assessed in many ways, from self-reported pain to sick leave with the results of special tests.
Main results
Pain in the lumbar region
When we combined the results of seven studies (645 women) that compared any form of physical exercise with routine prenatal care, exercise (lasting five to 20 weeks), we found that women with low back pain improved and disability rates decreased .
Pelvic pain
Less evidence is available for the treatment of pelvic pain. Two studies showed that women who participated in group exercise and received training in pain management reported no difference in pelvic pain compared to women who received routine prenatal care.
Pain in the lumbar region and pelvis
Results from four studies (1,176 women) when combined showed that an 8 to 12 week exercise program reduced the number of women who complained of low back and pelvic pain. In two studies (1,062 women), ground exercises of various formats also reduced sick leave-related low back and pelvic pain.
In two studies (1,062 women), ground exercises of various formats also reduced sick leave-related low back and pelvic pain.
However, two other studies (374 women) found that group exercise and education was no better in preventing pain, both in the pelvic region and in the lumbar region, compared with conventional prenatal care.
There have been a number of separate studies that have evaluated different treatment options. These results confirm that craniosacral therapy, osteomanipulation therapy, or multimodal intervention (manual therapy, exercise, and education) may be beneficial.
When side effects were reported, there were no long-term side effects in any of the studies.
Quality of evidence and conclusions
There is low-quality evidence that exercise reduces pain and disability in women with low back pain, and moderate-quality evidence for the effect of exercise on reducing sick leave and reducing the number of women with both lower back and pelvic pain complaints. The quality of the evidence depends on problems with study design, small numbers of women, and variable results. Ultimately, we believe that future research is likely to change our findings. There is not enough good quality evidence to make confident decisions about the treatment of these complaints.
The quality of the evidence depends on problems with study design, small numbers of women, and variable results. Ultimately, we believe that future research is likely to change our findings. There is not enough good quality evidence to make confident decisions about the treatment of these complaints.
Translation notes:
Translation: Kong Hong Han. Editing: Gamirova Rimma Gabdulbarovna, Ziganshina Lilia Evgenievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center based at Kazan Federal University). For questions related to this translation, please contact us at: [email protected]
Lower back pain and pregnancy
As a result, there are changes in the spine, in the muscles of the abdomen and back and the shape of the lumbar curve of the spine (hyperlordosis), and all this becomes relaxed. Poor posture and poor muscle tone can also affect spinal mechanics.
The lumbar curve of the spine begins to slowly increase as the pelvis begins to move back.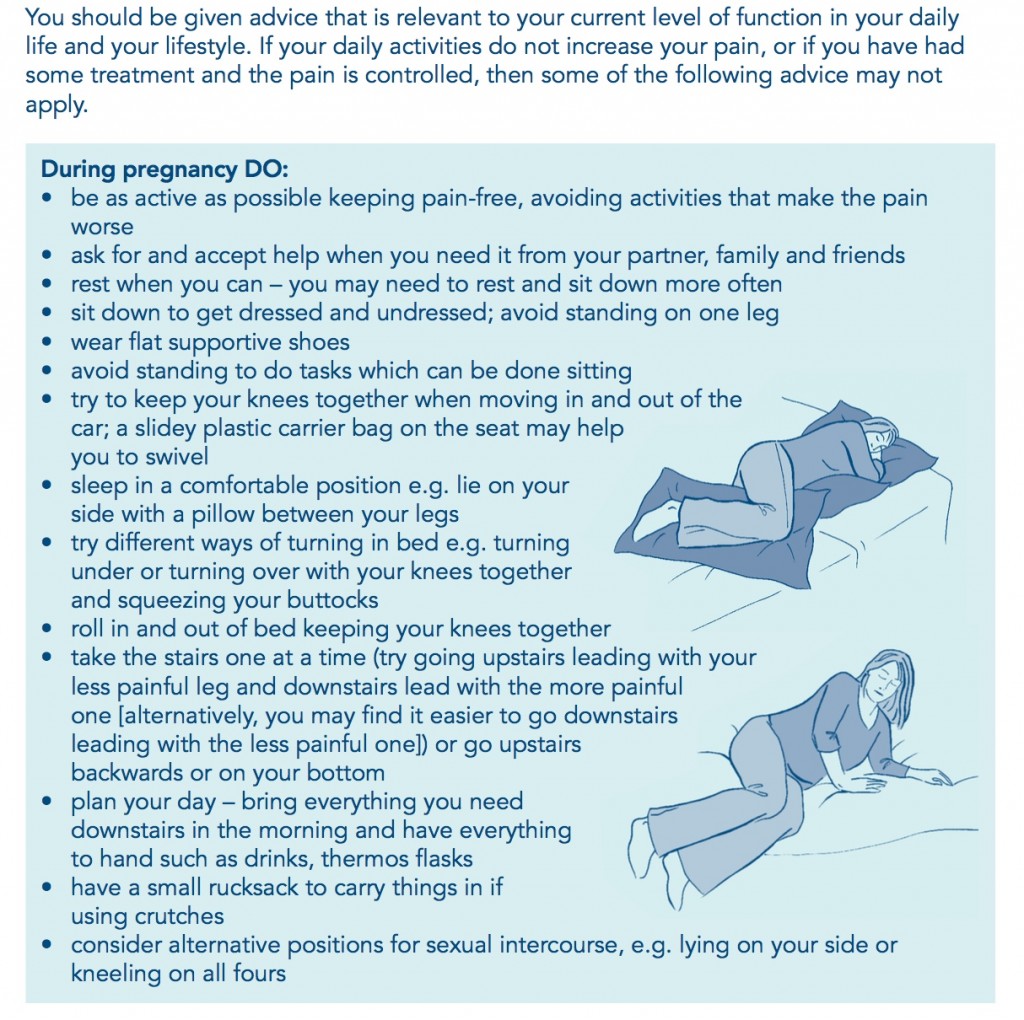 This posture begins to affect the weakened muscles and leads to the accumulation of fatigue in the muscles of the lower back. A woman may experience moderately painful muscle spasms at first, which may be the first sign of the possibility of persistent low back pain as the pregnancy progresses. The growing uterus shifts the center of gravity and weakens the abdominal muscles, changes posture and puts excessive stress on the back. If the uterus affects the nerves, then this can lead to pain. In addition, being overweight during pregnancy puts more stress on the muscles and joints, and therefore, by the end of the day, a pregnant woman may feel discomfort.
This posture begins to affect the weakened muscles and leads to the accumulation of fatigue in the muscles of the lower back. A woman may experience moderately painful muscle spasms at first, which may be the first sign of the possibility of persistent low back pain as the pregnancy progresses. The growing uterus shifts the center of gravity and weakens the abdominal muscles, changes posture and puts excessive stress on the back. If the uterus affects the nerves, then this can lead to pain. In addition, being overweight during pregnancy puts more stress on the muscles and joints, and therefore, by the end of the day, a pregnant woman may feel discomfort.
Experts describe the two most common patterns of low back pain during pregnancy: low back pain that occurs in the area of the lumbar vertebrae in the lower back, and posterior pelvic pain, which is felt in the back of the pelvis. Some women have symptoms of both types of low back pain.
Low back pain is similar to the pain that a woman experienced before pregnancy. Pain is felt in the lower back and around the spine, approximately at waist level. Also, women may experience pain that radiates to the legs. Prolonged sitting or standing can aggravate the pain and, as a rule, the pain tends to increase towards the end of the day. Many more women experience back pelvic pain, which is felt less than lower back pain. The pain may be deep inside the buttocks, on one or both buttocks, or in the back of the thighs. Pain can be triggered by activities such as walking, climbing stairs, getting in and out of the bathroom on a low cabinet, turning in bed, or twisting and lifting heavy objects.
Pain is felt in the lower back and around the spine, approximately at waist level. Also, women may experience pain that radiates to the legs. Prolonged sitting or standing can aggravate the pain and, as a rule, the pain tends to increase towards the end of the day. Many more women experience back pelvic pain, which is felt less than lower back pain. The pain may be deep inside the buttocks, on one or both buttocks, or in the back of the thighs. Pain can be triggered by activities such as walking, climbing stairs, getting in and out of the bathroom on a low cabinet, turning in bed, or twisting and lifting heavy objects.
Positions that involve leaning forward, such as sitting, in a chair, and working at a desk while leaning forward, can exacerbate posterior pelvic pain. Women with posterior pelvic pain are also more likely to experience pain over the pubic bone.
When low back pain radiates to the buttocks and thighs, sciatica is often suspected - although sciatica is not very common in pregnant women. True sciatica, which can be caused by a herniated disc or the presence of a disc protrusion in the lumbar spine, occurs in only 1 percent of pregnant women.
True sciatica, which can be caused by a herniated disc or the presence of a disc protrusion in the lumbar spine, occurs in only 1 percent of pregnant women.
If there is compression and inflammation of the sciatic nerve (herniated disc), then the pain in the legs is more severe than with normal low back pain. Pain can be felt not only in the thigh, but also below the knee or even radiate to the foot. It is also possible the presence of sensory disturbances, such as numbness or tingling sensations.
In severe sciatica, there may be numbness in the groin area, as well as in the genital area. You may also have trouble urinating or defecation. If a pregnant woman has suspicions of sciatica, then she must definitely contact her doctor. If symptoms such as impaired sensation in the legs and weakness in one or both legs or loss of sensation in the groin and impaired urination or defecation appear, then you need to see a doctor urgently! Such symptoms may be evidence of the development of the "cauda equina" syndrome in the presence of a herniated disc in a pregnant woman, and in such cases an emergency operation is necessary.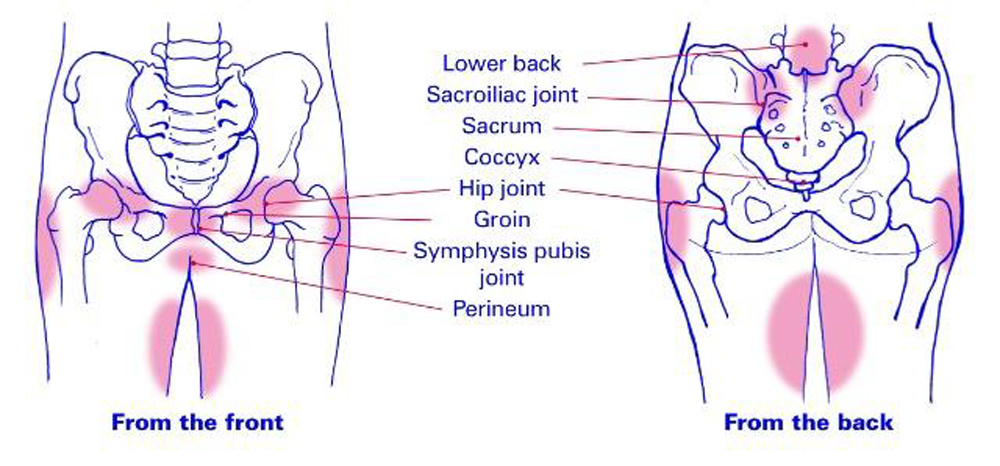
Risk factors for low back pain
It is not surprising that, most likely, low back pain in pregnant women is most likely if there were already pains before pregnancy or there were degenerative changes in the lumbar spine (protrusions, herniated discs). Also at higher risk are pregnant women who led an inactive lifestyle before pregnancy, as a result of which their back muscles are weak, as well as the abdominal muscles. Pregnancy with multiple fetuses (twins) significantly increases the risk of lower back pain. Obesity may also be a risk factor for developing low back pain during pregnancy.
Diagnosis of low back pain.
Examinations such as CT (MSCT) are rarely used to diagnose the causes of low back pain in pregnant women due to possible teratogenic effects on the fetus. MRI is also not recommended, especially in the first trimester of pregnancy. But, if there are clinical indications, then MRI can be performed. Therefore, as a rule, the diagnosis of low back pain in pregnant women is mainly based on physical examination data, symptoms and medical history (for example, the presence of a disc herniation before pregnancy).
Treatment
The use of any medication during pregnancy is a big risk, since all medications will also enter the body of the fetus. Therefore, the usual prescription of painkillers, muscle relaxants, or steroids (NSAIDs) for back pain is contraindicated in pregnant women. In addition, the use of acupuncture physiotherapy is also not recommended. It is possible to use light massage and very gentle manual therapy techniques.
At the forefront of the treatment of back pain in pregnant women is exercise therapy (gymnastics) and certain recommendations for daily activities. Gymnastics can be specialized, such as prenatal yoga. Good effect gives swimming and walking.
Swimming is an excellent choice of exercise for pregnant women because it strengthens the abdominal and lower back muscles, and being in the water relieves stress on joints and ligaments.
Need to maintain proper biomechanics during pregnancy:
- Stand up straight. This becomes more and more difficult to do as the shape of the body changes, but one must try to keep the back straight and the shoulders back.
 Pregnant women tend to drop their shoulders and arch their back as their belly grows, which puts more stress on the spine.
Pregnant women tend to drop their shoulders and arch their back as their belly grows, which puts more stress on the spine. - If it is necessary to sit during the day, then one should sit straight. Leg support (bedside table) can help prevent lower back pain, and you can also put a special pillow under the lower back. Take frequent breaks from sitting. You need to get up and walk for several minutes, at least once an hour.
- It is equally important not to stand too long. If you need to stand all day, then it is advisable to rest while lying on your side during a break, supporting your upper leg and stomach with pillows.
- Avoid movements that increase pain. If there is posterior pelvic pain, then one should try to limit activities such as climbing stairs. It is also advisable to avoid any activity that requires extreme movement of the hips or spine.
- It is important to wear comfortable shoes and avoid high heels. As the abdomen grows, the center of gravity shifts and when wearing shoes with heels, the risk of falls increases.
- Always bend your knees and pick things up from your haunches to minimize stress on your back. Spinal twisting should be avoided and activities such as vacuuming or mopping should be avoided.
- Divide the weight of the items to be carried. For a uniform load, it is necessary to carry the weight in two bags.
With severe pain and weak muscle corset, you can wear a belt.
Particular attention should be paid to pregnant women with herniated discs, as in a certain percentage of cases, it is possible to develop cauda equina syndrome during pregnancy, a very serious neurological condition.
Seek immediate medical attention if any of the following symptoms occur:
- Back pain pain is very severe, persistent, or gradually worsens, or if the pain appears after an injury, or if it is accompanied by a rise in temperature.
- Numbness in one or both legs, or feeling that the legs do not obey
- Loss of sensation in the buttocks, groin, perineum, or impaired bladder and bowel function.