Baby sticky eye or conjunctivitis
Sticky eye | Pregnancy Birth and Baby
Sticky eye | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is sticky eye?
If your baby's eye is very watery and there is some discharge, it's probably a blocked tear duct. This is also known as 'sticky eye'. This condition usually gets better by itself, but it's still wise to check with your doctor. There are things you can do to help it get better and avoid infection.
What causes sticky eye?
Glands inside the upper eyelids produce tears. The tears flow over the surface of the eye. They drain away through small openings in the inside corner of the upper and lower eyelids. The tears then flow through the tear duct to the nose.
About 1 in 20 babies is born with tear ducts that are too narrow or blocked completely. Sometimes the tear duct (tube) is blocked by a plug of mucus or cells that developed before the baby was born. This means their tears can't drain away and their eyes are wet all the time.
Is it sticky eye?
If your baby has sticky eye, their eye or eyes will water a lot. They may have tears running down their cheeks. Sometimes there may be swelling and a sticky yellow or green discharge. Sticky eye is not an infection and should not cause your child pain.
Other symptoms may mean the eye is infected, such as red, swollen, or sore eyes. Your baby may also have a fever or be fussier than usual.
Eye infections include conjunctivitis and dacryocystitis. You should always see your doctor if you think your baby has an eye infection.
You should also see your doctor if:
- your baby seems sensitive to light
- they have large amounts of eye discharge
- they are constantly squeezing their eyes shut
- the side of their nose seems swollen, red, and painful
- the tear duct is still blocked by the time they reach 1 year of age
How is sticky eye treated?
Sticky eye normally clears up by the time your baby is 12 months. If there is any sign of infection, your doctor might give your baby some antibiotic eye drops or ointment.
If there is any sign of infection, your doctor might give your baby some antibiotic eye drops or ointment.
Some babies will need surgery if the blocked tear duct doesn't improve. This is done with a general anaesthetic, so the doctor can open the tear duct with a probe.
How do I manage my baby’s sticky eye?
There are ways for you to help manage and treat your baby’s sticky eye.
To help the blocked tear duct, your doctor may teach you a special massage.
If your baby has sticky eye, it is important to keep their eyes clean. This will help prevent infection.
Wash the affected eye or eyes as needed, following the directions below:
- Wash your hands thoroughly with soap and water.
- Pat the eye dry with a clean (or disposable) towel.
- Gently wipe each eye with a disposable cotton swab soaked in water or a weak saline solution, making sure to wipe from the inside corner of the eye to the outside corner.
- Do not touch the eye itself or clean inside the eyelid because you may damage the eye.
- Use a new cotton swab for each eye.
- Wash your hands again.
You can make saline solution by dissolving:
- 1 teaspoon of salt
- 1 cup (250ml) of boiling water
Make sure that the solution has cooled to room temperature before using.
There is also evidence to support using breastmilk to clean your baby's eye. This will not cause any harm to your baby.
If you see signs of an infection, you should see your doctor.
Sources:
Children's Health Queensland Hospital and Health Service (Blocked tear duct (nasolacrimal duct obstruction)), Royal Australian College of General Practitioners (RACGP) (Acute red eye in children), The Royal Hospital for Women (Sticky eye care for a neonate), Perth Children’s Hospital (Blocked tear duct (Nasolacrimal duct obstruction)), International Ophthalmology (The natural process of congenital nasolacrimal duct obstruction and effect of lacrimal sac massage)Learn more here about the development and quality assurance of healthdirect content.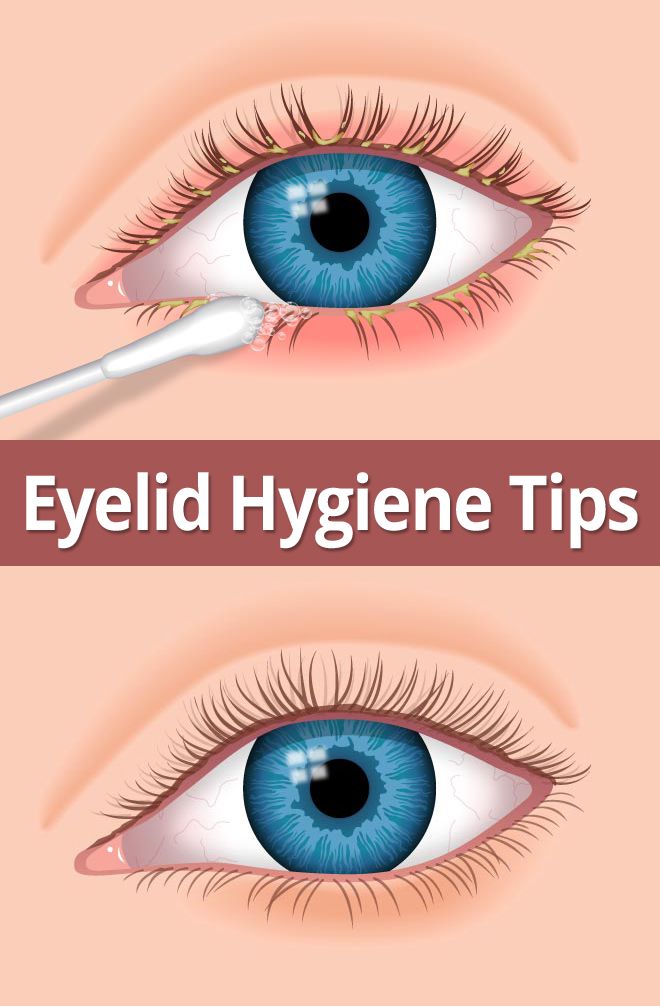
Last reviewed: July 2022
Back To Top
Related pages
- Conjunctivitis
- Cleaning your baby's ears, eyes and nose
Need more information?
Conjunctivitis | SA Health
Conjunctivitis is an inflammation of the lining of the eye and eyelid caused by bacteria, viruses, chemicals or allergies.
Read more on SA Health website
Conjunctivitis
Conjunctivitis is an inflammation of the surface of the eye. It is very common in young children and it can be highly contagious. Learn more here.
Read more on Pregnancy, Birth & Baby website
Pollen - a trigger for hay fever - National Asthma Council Australia
Plant pollen is well known as a trigger for seasonal allergic rhinitis (hay fever) and seasonal allergic conjunctivitis.
Read more on National Asthma Council Australia website
Conjunctivitis in babies, children & teens | Raising Children Network
Conjunctivitis is a type of eye infection. It’s very common and can be very contagious. Your child needs to see a GP for the right conjunctivitis treatment.
Read more on raisingchildren.net.au website
Other Allergic Conditions - Allergy & Anaphylaxis Australia
Other Allergic Conditions included: Urticaria (Hives), Eczema (Atopic Dermatitis), Allergic Conjunctivitis, Allergic Rhinitis (hayfever), Sinusitis
Read more on Allergy and Anaphylaxis Australia website
Conjunctivitis - MyDr.com.
 au
au Conjunctivitis is an inflammation of the eye's conjunctiva and may be contagious. Treatment depends on the cause.
Read more on myDr website
Conjunctivitis: self-care - MyDr.com.au
A major cause of eye problems is allergic, bacterial or viral conjunctivitis (inflammation of the 'wet' surfaces of the eye). Find out what products are available for conjunctivitis.
Read more on myDr website
Conjunctivitis - Better Health Channel
Conjunctivitis is an eye infection caused by a bacteria or virus. Symptoms include eye redness, a discharge and swollen lids. Conjunctivitis is treated with antibacterial eye drops or ointment. Children must not attend school or child care if they have conjunctivitis.
Read more on Better Health Channel website
Allergic conjunctivitis - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Allergic conjunctivitis usually causes mild to moderate symptoms, including redness, which respond to non medicated treatment. However, sometimes symptoms can be extremely severe and debilitating with swelling of the eyelids and conjunctivae and a sensation of grittiness and burning.
However, sometimes symptoms can be extremely severe and debilitating with swelling of the eyelids and conjunctivae and a sensation of grittiness and burning.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Blocked tear duct: babies & toddlers | Raising Children Network
Many babies get a blocked tear duct. Symptoms include watering eyes and discharge. Blocked tear ducts mostly fix themselves, but it’s good to see a GP.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Is My Baby’s Eye Discharge Normal?
Written by Nicole Blades
In this Article
- What’s Normal?
- When It’s Conjunctivitis
- When Treatment Is Needed
As the parent of a newborn, nothing beats staring lovingly into your sweet little bundle’s eyes. (Well, watching your baby sleeping soundly comes pretty close!) But what if when you look into your child’s eyes, you see that they have goopy, sticky discharge? Is it something to be concerned about?
What’s Normal?
First of all, take a breath, because sticky eye discharge in newborns is very common.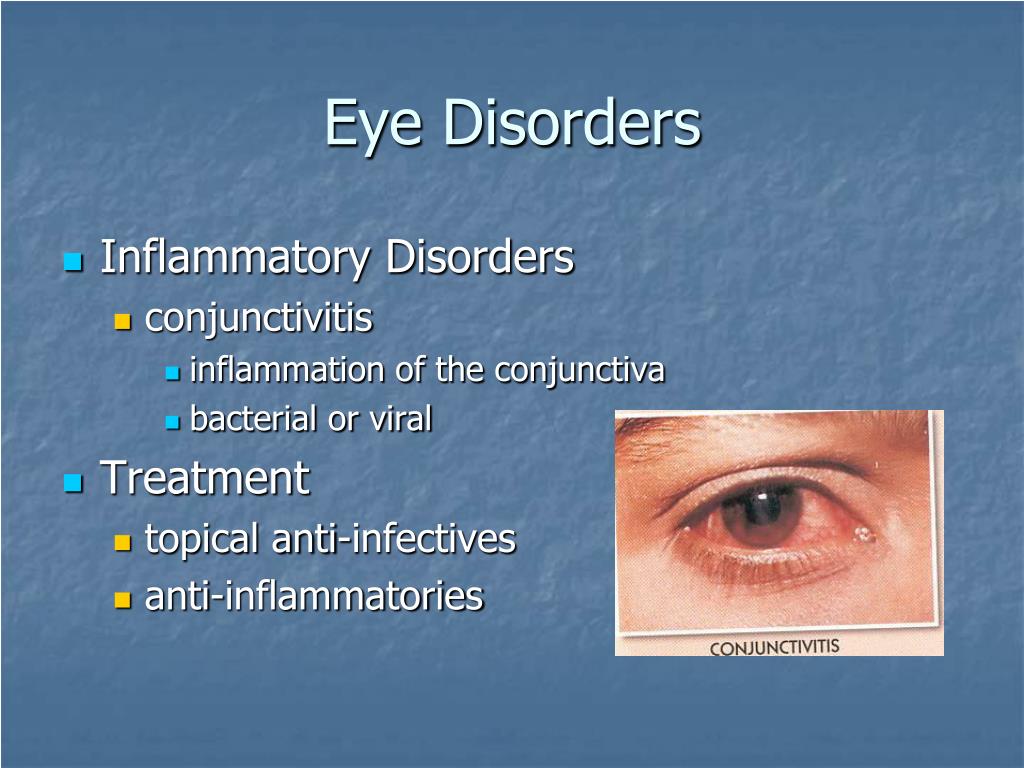 If the white part of your baby’s eye -- the sclera -- is clear and there is no redness, but there is discharge, it’s most likely a blocked tear duct.
If the white part of your baby’s eye -- the sclera -- is clear and there is no redness, but there is discharge, it’s most likely a blocked tear duct.
About 1 in 5 babies are born with tear ducts that haven’t fully developed. The blockage is usually in one eye but can be in both. It often clears up on its own. A warm compress can help, but if it lasts a long time, it might need surgery.
When It’s Conjunctivitis
Since a newborn hasn’t been around that long -- under 2 months -- it’s not common for them to get a lot of viral infections. But sometimes their clogged tear duct can lead to an infection such as conjunctivitis.
This happens when there is inflammation of the thin layer of tissue (conjunctiva) that covers the sclera. Symptoms are similar to the sticky, watery eyes that come with a blocked tear duct. But with conjunctivitis, there is more swelling, tenderness, and redness of the eye area, and the whites of the eye will be pink or red. Your baby’s eyelid might be red, sticky, and itchy, and the discharge takes on a yellowish color.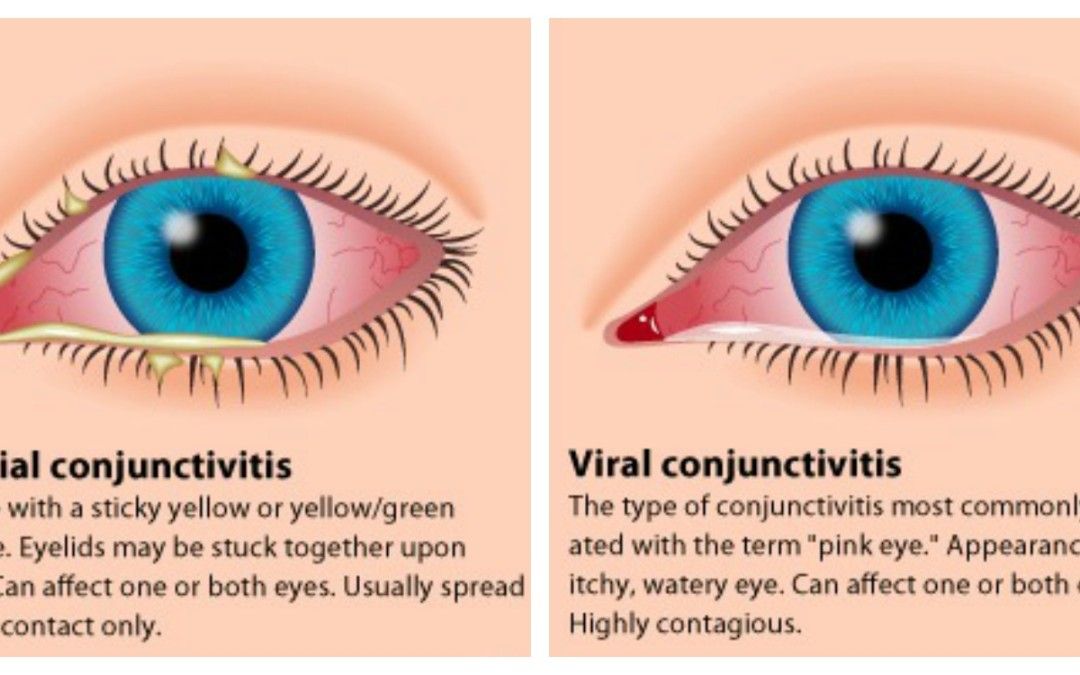 Also, their eyes might be more watery than usual. The infection often starts in one eye and spreads to the other.
Also, their eyes might be more watery than usual. The infection often starts in one eye and spreads to the other.
Chemical conjunctivitis can happen when eye drops and ointments, typically used on newborns at birth to help prevent infection, actually cause the irritation. It can show up as mildly red eyes and some puffiness in the eyelids.
It’s rare, but red, angry, itchy eyes with swollen eyelids and discharging pus could mean ophthalmia neonatorum (ON).This is a bacterial infection that can happen during childbirth if the baby passes through a birth canal infected with chlamydia. The symptoms usually show up 5-12 days after birth. Among newborns with ON, half also have the infection other areas of their bodies.
Call the doctor if the baby has a fever and:
- Your baby cannot open their eyes or you cannot see the eye
- The area is tender to touch and the skin around the eye is red
- There is a lot of eye discharge
These may be signs of a bacterial infection of the sclera.
When Treatment Is Needed
Doctors usually recommend a wait-and-see approach, as this issue often clears up on its own. You can also apply a warm compress to the bothered eye.
If the tear duct is still blocked and the eye discharge continues up to the baby’s first birthday, you should see your child’s doctor. They may refer you to a pediatric eye specialist, as it may need surgery.
To treat conjunctivitis caused by the blocked tear duct, try a gentle warm massage with your clean hand between your baby’s eye and nasal area. For chemical conjunctivitis, the symptoms usually only last for 1-3 days after birth, so no treatment is needed. And if it’s ON, doctors usually treat that with oral antibiotics.
Conjunctivitis: symptoms, causes, treatment of viral, allergic, bacterial conjunctivitis.
From All About Vision
- Causes
- Symptoms
- Treatment
What is conjunctivitis?
Conjunctivitis is an inflammation of the thin, clear membrane that covers the whites of the eye and the inside of the eyelids (conjunctiva). nine0003
nine0003
Conjunctivitis may sound daunting, but this common eye problem is easy to treat. In addition, with a few simple precautions, conjunctivitis can often be prevented. However, there is one type of conjunctivitis that can cause serious vision problems if left untreated. See an eye doctor if you have concerns about conjunctivitis.
Anyone can get conjunctivitis, but office workers, shop workers, preschoolers, schoolchildren, university students, teachers, and childcare workers are particularly at risk of contagious conjunctivitis because they work in close contact with other people. nine0003
Here's what you need to know about conjunctivitis:
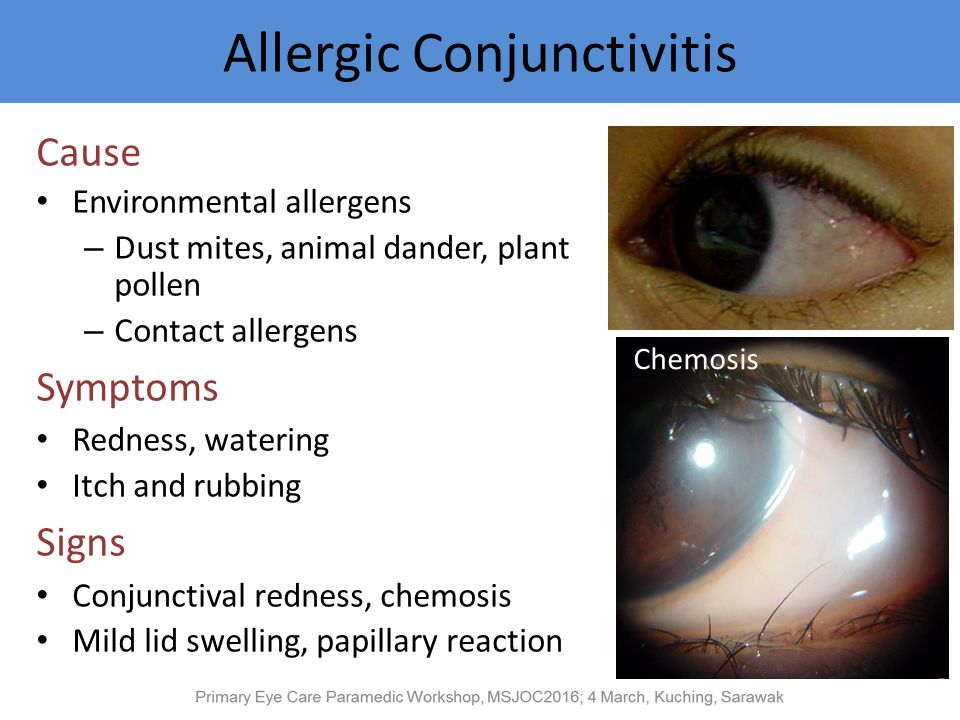
What causes conjunctivitis?
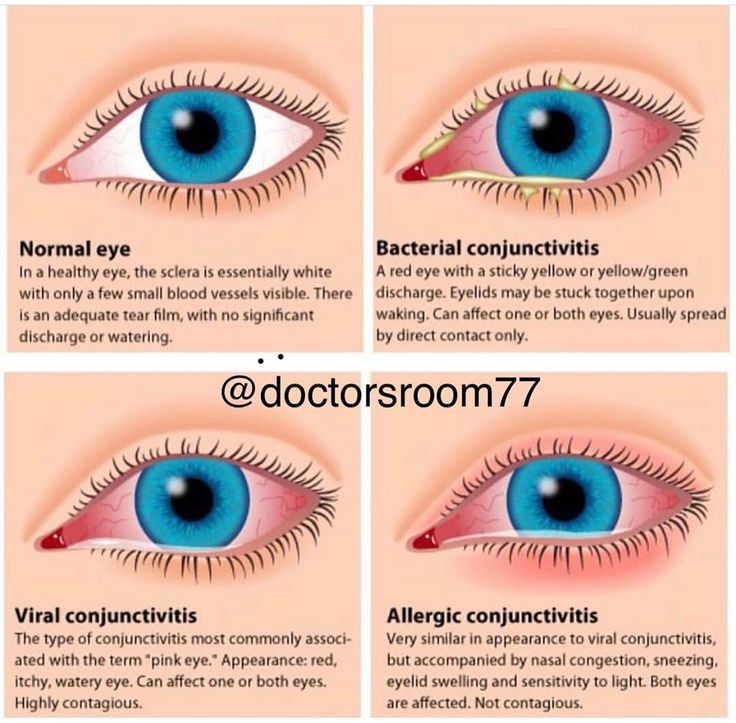
The main types of conjunctivitis, depending on the cause, include:
-
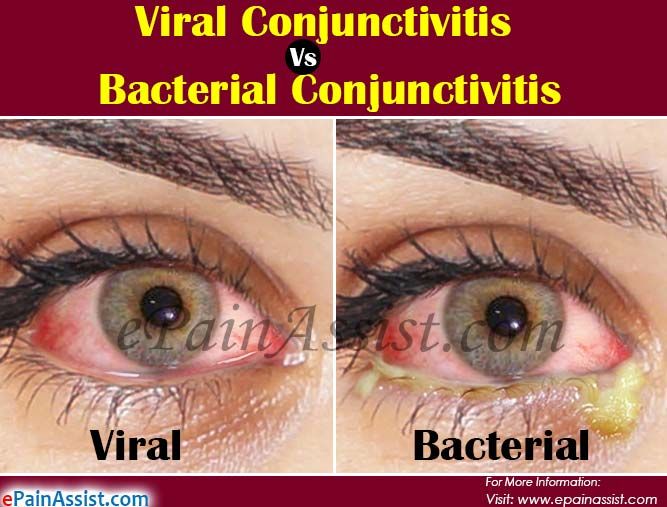
Viral conjunctivitis. Caused by a virus, such as a viral infection of the upper respiratory tract. This type of conjunctivitis is highly contagious but usually goes away on its own within a few days without treatment.
-
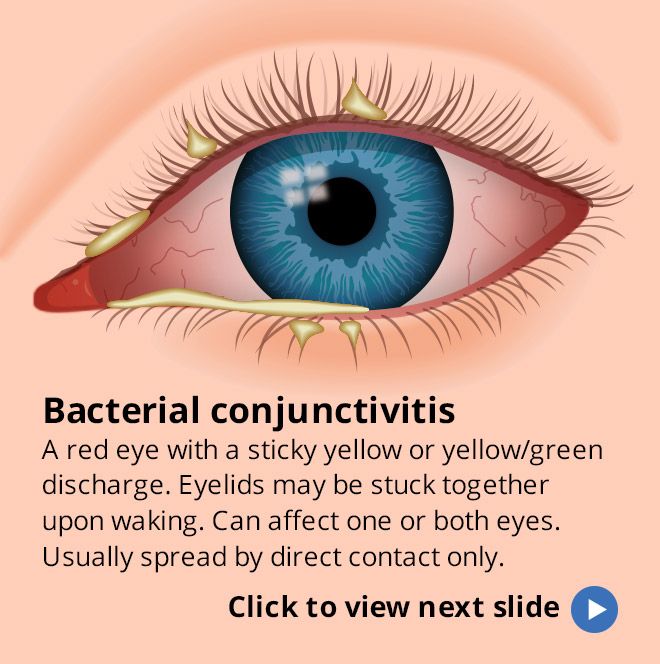
Bacterial conjunctivitis. Caused by bacteria; this type of conjunctivitis can cause serious damage to the eye if left untreated. nine0003
-
Allergic conjunctivitis. This type of conjunctivitis is caused by eye irritants such as pollen, dust and animal dander in susceptible individuals. Allergic conjunctivitis can be seasonal (pollen) or year-round (dust; pet dander).
Symptoms of conjunctivitis
The main symptom of conjunctivitis is the pink color of the eye. Other symptoms of conjunctivitis depend on the type of conjunctivitis:
-
Bacterial conjunctivitis has symptoms such as sticky, yellow or greenish-yellow discharge at the corner of the eye. In some cases, these secretions can be strong enough that the eyelids stick together in the morning after sleep. One or both eyes may be affected. Bacterial conjunctivitis is contagious and is usually spread by direct contact, that is, by touching the eyes with infected hands or objects.

-
Symptoms of allergic conjunctivitis include tearing, burning, itchy eyes, and are often accompanied by nasal congestion and runny nose, and sensitivity to light. Allergic conjunctivitis affects both eyes, but this type of conjunctivitis is not contagious.
Ways to treat conjunctivitis
As you might expect, the treatment of conjunctivitis depends on the type of conjunctivitis you have:
-
Treating viral conjunctivitis
In most cases, viral conjunctivitis lasts for several days and does not require any medical treatment. Applying a cold, damp flannel cloth to your eyes several times a day can relieve the symptoms of viral conjunctivitis.
-
Treating bacterial conjunctivitis
Your doctor will usually prescribe antibiotic eye drops or ointment to treat bacterial conjunctivitis. nine0003
It can often be difficult to tell by symptoms alone what type of conjunctivitis you have (or if you have other eye conditions and health problems that cause similar symptoms).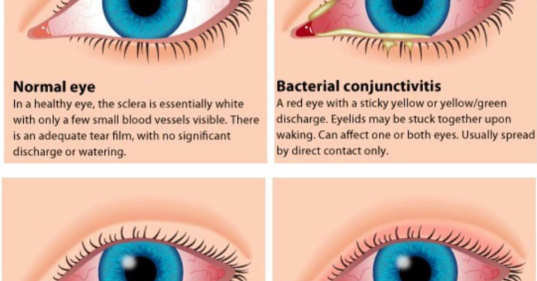
Conjunctivitis can also cause dry eyes. In addition, bacterial conjunctivitis can sometimes lead to very serious eye problems, including permanent loss of vision.
For these reasons, whenever redness and irritation of the eyes occurs, you should immediately call the optometrist and make an appointment for an eye examination. nine0003
If you wear contact lenses and you develop redness and irritation in your eyes, remove your lenses and wear only glasses until your eye has been examined by an optometrist.
9 Tips for Preventing Conjunctivitis
Now that you have a basic understanding of viral conjunctivitis and other forms of conjunctivitis, what can you do to protect yourself and your children from it?
Here are nine simple precautions you can take to significantly reduce your risk of conjunctivitis:
-
Never share personal items such as facial sponges, hand towels or tissues.
-
Cover your nose and mouth when coughing or sneezing, avoid rubbing your eyes and avoid touching your eyes.
-
Wash your hands frequently especially when you are at school or other public places.
-
Keep hand sanitizer nearby and use frequently. nine0003
-
Frequently wipe surfaces such as countertops, bathroom surfaces, faucet handles and phones in common use with an antiseptic.
-
If you know you have seasonal allergies , ask your doctor what you can do to minimize your symptoms before they occur.
-
If you wear contact lenses, follow your optometrist's instructions for lens care and replacement timing, and use contact lens solutions appropriately or consider switching to disposable daily contact lenses. nine0003
-
When swimming , wear swimming goggles to protect yourself from bacteria and other micro-organisms in the water that can cause conjunctivitis.
-
Remove your contact lenses before showering to prevent bacteria from getting between your eyes and lenses.
Wash your hands frequently to prevent the spread of viral conjunctivitis.
Despite these precautions, you or your child can still develop conjunctivitis. nine0003
If your child develops conjunctivitis, inform caregivers/teachers of the infection so that they can take extra sanitization measures in the classroom or in the daycare group. The child should remain at home until the contagious stage has passed.
Your optometrist will tell you when you or your child can go back to public places without the risk of spreading conjunctivitis, usually about three to five days after diagnosis. nine0003
If conjunctivitis persists, or because red or pink eyes can be a symptom of many different eye conditions - some of which can be quite serious - see an optometrist.
Page published on Thursday, November 12, 2020
Allergic conjunctivitis in children. What is allergic conjunctivitis in children?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment.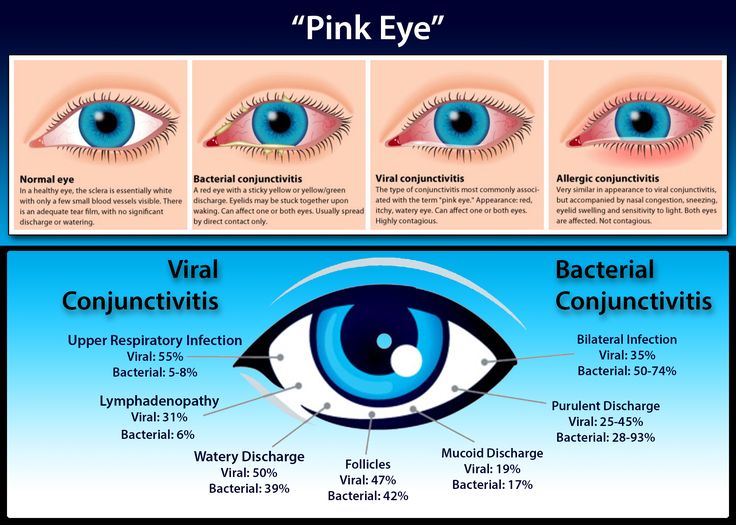 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0003
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0003
Allergic conjunctivitis in children is an inflammatory process in the conjunctival membrane of the eye, which is a reaction to a particular antigen that sensitizes the body. The development of allergic conjunctivitis in children is accompanied by local swelling, itching and redness of the eyes, lacrimation, and photophobia. Diagnosis of allergic conjunctivitis in children is carried out by a pediatric ophthalmologist and allergist; includes microscopic examination of the lacrimal fluid, total IgE, KLA, skin tests. Therapy of allergic conjunctivitis in children requires the elimination of contact with the allergen, the appointment of antihistamines in the form of eye drops and orally, and specific immunotherapy. nine0003
ICD-10
h20.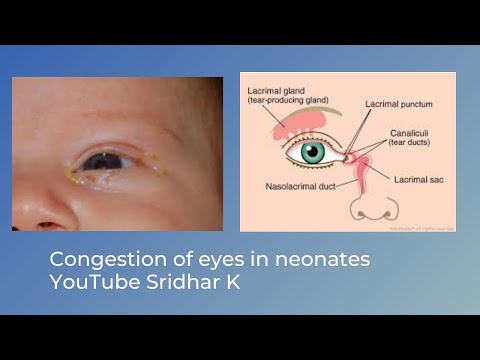 1 Acute atopic conjunctivitis
1 Acute atopic conjunctivitis
- Causes
- Classification
- Symptoms
- Diagnostics
- Treatment of allergic conjunctivitis in children
- Prognosis and prevention
- Prices for treatment
General
Allergic conjunctivitis in children is a common disease in modern pediatrics, which is the subject of study in pediatric ophthalmology and allergology. Allergic conjunctivitis is characterized by inflammation of the mucous membrane covering the sclera and the inner surface of the eyelid, due to the body's hypersensitivity to any allergen. In most cases, the manifestation of allergic conjunctivitis in children occurs at the age of 3-4 years. Among school-age children, allergic conjunctivitis occurs in 3-5% of cases. Allergic conjunctivitis in children usually accompanies other allergic manifestations: allergic rhinitis, hay fever, atopic dermatitis, bronchial asthma, etc. nine0003
Allergic conjunctivitis in children
Causes
The basis of allergic conjunctivitis in children is an increased individual sensitivity to certain environmental factors - allergens.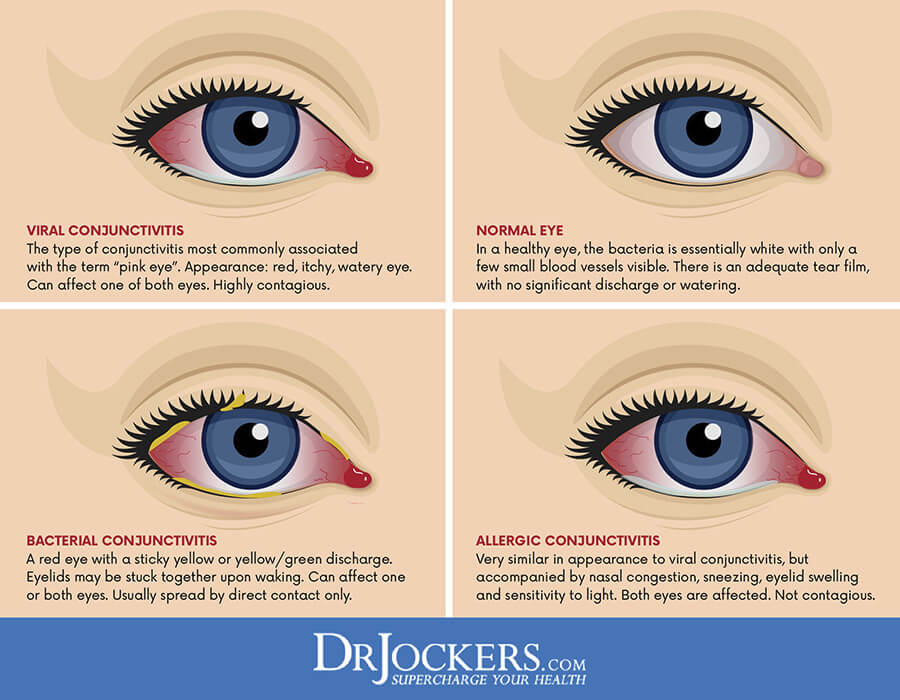 Such exogenous factors can be allergens: household (household and library dust, mites, pillow feathers, household chemicals), pollen (pollen of flowering trees and grasses), epidermal (dandruff and animal hair, pet food), food (food - citrus fruits, chocolate, honey, berries, etc.), medicinal (medicines). nine0003
Such exogenous factors can be allergens: household (household and library dust, mites, pillow feathers, household chemicals), pollen (pollen of flowering trees and grasses), epidermal (dandruff and animal hair, pet food), food (food - citrus fruits, chocolate, honey, berries, etc.), medicinal (medicines). nine0003
In some cases, foreign bodies of the eye, as well as allergens of bacterial, viral, fungal and parasitic origin, become the cause of the development of allergic conjunctivitis in children. It has been established that allergic eye diseases in young children are more often caused by genetic and social factors, and in older children - by previous household, food, epidermal sensitization, the severity of which largely determines the severity of allergic conjunctivitis. nine0003
Classification
Taking into account the etiopathogenetic mechanisms, the following forms of allergic conjunctivitis in children are distinguished: hay (hay fever), macropapillary (hyperpapillary), medicinal, tuberculosis-allergic, infectious-allergic and spring catarrh.
- Pollinous conjunctivitis in children is an allergic eye disease caused by the pollen of grasses, cereals, trees. It has a seasonal dependence, occurs during the flowering of those plants to the pollen of which the body is sensitized. With hay fever, pollinous conjunctivitis in children is combined with urticaria, asthmatic bronchitis, atopic or contact dermatitis, Quincke's edema, dyspeptic disorders, headaches. nine0008
- Spring conjunctivitis. It most often occurs in boys aged 5-12 years. Spring conjunctivitis in children has a persistent chronic course; exacerbations occur mainly in the sunny season. Spring catarrh can occur in conjunctival, limbal and mixed forms.
- Hyperpapillary conjunctivitis. The occurrence of hyperpapillary conjunctivitis is associated with contact irritation of the conjunctiva by foreign bodies (contact lenses, eye prostheses, sutures). On the conjunctiva of the upper eyelid, on examination, giant papillae (from 1 mm or more) are revealed.
 nine0008
nine0008 - Drug allergic conjunctivitis in children develops against the background of the use of various eye drops. An allergy can occur both to the main active ingredient and to the preservatives used in the drops; especially often, allergic conjunctivitis in children occurs with the instillation of antibacterial eye drops and anesthetics.
- Infectious-allergic conjunctivitis in children is associated with sensitization of the body to microbial allergens: bacterial, viral, fungal exotoxins. At the same time, the pathogen itself is not detected in the conjunctiva of the eye. nine0008
- Tuberculous-allergic eye damage proceeds according to the type of keratoconjunctivitis, with simultaneous damage to the conjunctiva and cornea. This form of allergy is the result of an allergic reaction to the waste products of Mycobacterium tuberculosis circulating in the blood.
Symptoms
Usually, the symptoms of allergic conjunctivitis in a child develop within a few minutes or one day after exposure to the allergen.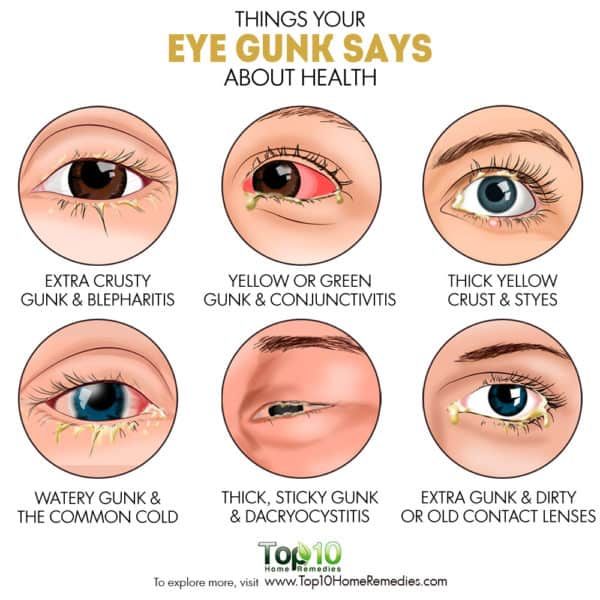 In this case, both eyes are immediately involved in reactive inflammation. The eyelids of the child swell, the conjunctiva becomes hyperemic and edematous, lacrimation occurs, and with severe conjunctivitis - photophobia. nine0003
In this case, both eyes are immediately involved in reactive inflammation. The eyelids of the child swell, the conjunctiva becomes hyperemic and edematous, lacrimation occurs, and with severe conjunctivitis - photophobia. nine0003
The leading subjective symptom of allergic conjunctivitis in children is intense itching, which makes the child constantly scratch his eyes, further intensifying all manifestations of the disease. In the conjunctival cavity, a transparent (sometimes sticky or membranous) discharge constantly accumulates. Purulent discharge in uncomplicated allergic conjunctivitis in children is usually absent, and occurs only when an infectious component is added.
Allergic conjunctivitis in children can be acute (with a quick onset and a quick end) or chronic (long, sluggish, with periodic exacerbations). The nature of the course is determined by the causally significant allergen and the frequency of contact with it. nine0003
Diagnostics
Diagnosis of allergic conjunctivitis in children is carried out by a pediatric ophthalmologist and an allergist-immunologist.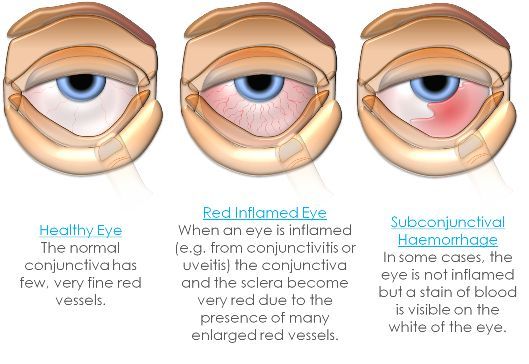 Reliable diagnostic criteria for allergic conjunctivitis in children include: the presence of an allergic history, the relationship of the onset of the disease with certain external factors (flowering, contact with animals, the use of certain foods, etc.), characteristic clinical symptoms.
Reliable diagnostic criteria for allergic conjunctivitis in children include: the presence of an allergic history, the relationship of the onset of the disease with certain external factors (flowering, contact with animals, the use of certain foods, etc.), characteristic clinical symptoms.
To confirm the diagnosis, a microscopic examination of the lacrimal fluid is performed, where, with allergic conjunctivitis in children, more than 10% of eosinophils are found. With the allergic nature of the disease, an increased level of total IgE, eosinophilia, is also detected compared to the age norm. In the presence of a purulent secret, a bacteriological examination of the discharge from the conjunctival cavity is performed. The manifestation of a systemic allergic reaction necessitates examination of the child's gastrointestinal tract, analysis of feces for helminth eggs, and scraping for enterobiasis. nine0003
The direct cause of allergic conjunctivitis in children can be identified by skin allergy tests and a blood test for specific IgE.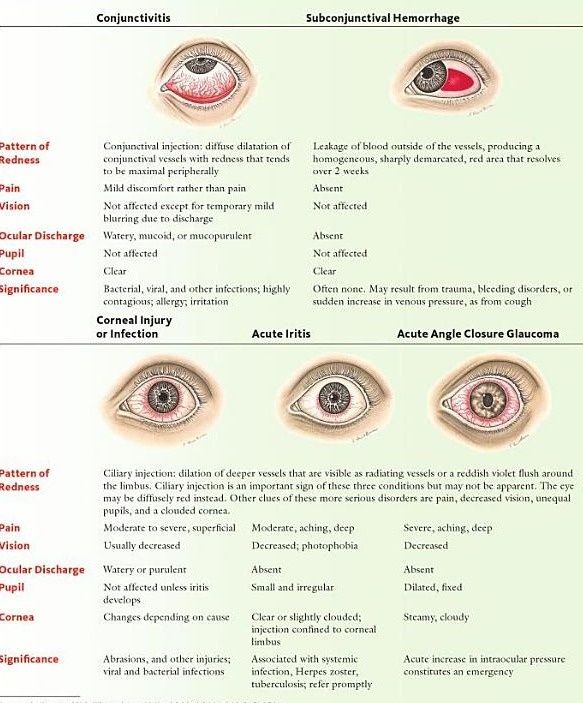 Differential diagnosis of allergic conjunctivitis in children is carried out with demodicosis, fungal, bacterial, autoimmune conjunctivitis.
Differential diagnosis of allergic conjunctivitis in children is carried out with demodicosis, fungal, bacterial, autoimmune conjunctivitis.
Treatment of allergic conjunctivitis in children
An indispensable condition for successful therapy is elimination measures that involve the exclusion of contact with the allergen. The pathogenetic basis for the treatment of allergic conjunctivitis in children is antihistamines in the form of tablets and instillations of eye drops in age-specific dosages and concentrations. In the persistent course of the disease, topical NSAIDs and corticosteroids are prescribed. nine0003
It is possible to carry out allergen-specific therapy, which is most effective in children. It involves the introduction of small doses of the allergen in increasing concentrations, which is accompanied by a gradual addiction to this allergen, a decrease or disappearance of the symptoms of allergic conjunctivitis in children.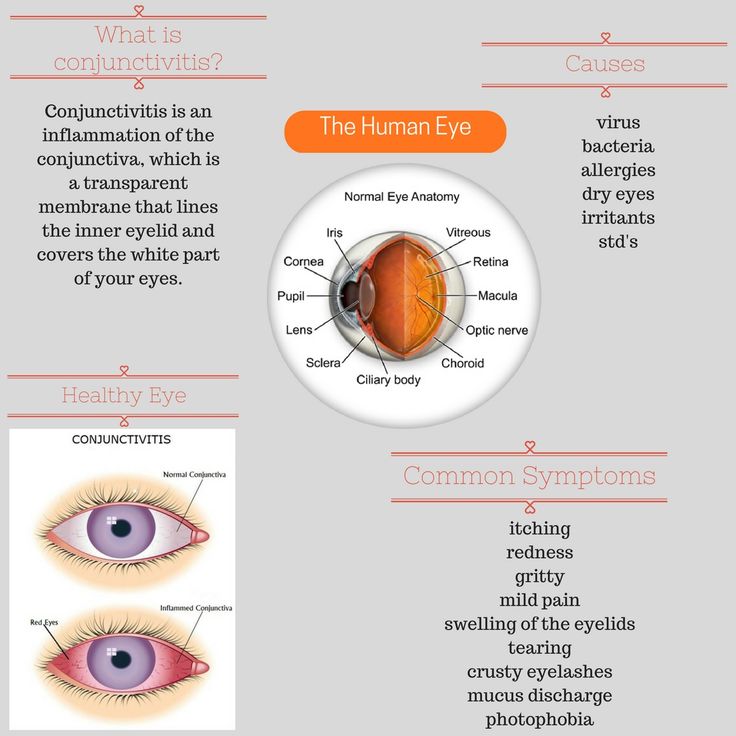
Prognosis and prevention
With untimely diagnosis of allergic conjunctivitis in children, the cornea and other eye tissues may be involved in the inflammatory process, which is fraught with a decrease in visual acuity and the development of forms of eye diseases that are difficult to treat (keratitis, corneal ulcers). Identification and elimination of the allergen, as well as specific immunotherapy, can prevent recurrence of allergies. Specific prevention of allergic conjunctivitis in children has not been developed. Attention should be paid to strengthening the general immunity of the child, to conduct preventive courses of desensitizing therapy during the seasons of exacerbation of the disease, to avoid contact with known allergens. nine0003
You can share your medical history, what helped you in the treatment of allergic conjunctivitis in children.
You can get advice from an ophthalmologist and an allergist-immunologist in Volgograd, Volzhsky and Mikhailovka at DIALINE clinics.