Real baby being born
Woman giving birth: Live birth video
Narrator: Samiyyah is the owner of a day spa in Philadelphia. She is 38 weeks pregnant with her second child.
Samiyyah: With the first pregnancy, I delivered in a hospital, and it was very restricting, you know, being confined to the bed, not being able to, you know, move when I felt my body wanted me to do certain things.
Narrator: For her son Safi's birth, she was given pitocin to speed up labor, an epidural for pain management, and an episiotomy (a surgical cut to widen the vaginal opening).
This time, she's planning a natural delivery -- without pain medication and other medical interventions -- at a birth center.
Samiyyah: Yes, I've been told that I am completely crazy for being, you know, for not having the drugs, but I've been there and I didn't like it, so I figured I would try this. It's healthier for the baby; it's healthier for me. So why not? I mean, women, we were designed to do this.
Narrator: Seven days after her due date, Samiyyah's labor kicks into gear. At the birth center in Bryn Mawr, Pennsylvania, Julia Rasch, a licensed nurse/midwife, performs an internal exam and starts an IV line to give Samiyyah a dose of antibiotics, since she's positive for Group B strep.
Samiyyah is 3 centimeters dilated, 100 percent effaced, and her water hasn't broken yet, which is common in the first stage of labor.
Birth centers offer a more relaxed and intimate alternative to hospitals for women expecting uncomplicated births.
It's important to choose a birth center with nearby hospital privileges in case of an emergency.
Helping her through her first natural birth is her husband, Arvan. Her mother-in-law, Irena, and 6-year-old son Safi are there for support.
Samiyyah: We've talked about, you know, what he's gonna see, we've shown him pictures, and I think he'll be okay.
Narrator: As Samiyyah's labor progresses, her baby's heart rate is monitored every 15 minutes.
Samiyyah: My goal is to remain calm and try to stay level-headed.
Narrator: As her contractions pick up, she starts experiencing painful back labor, typically caused by the baby's head pressing against the lower spine.
Samiyyah finds some relief by trying a combination of slow steady breathing, constant deep massaging and counterpressure, spending lots of time in a heated Jacuzzi, and trying different labor positions.
Arvan: She's doing great. She's doing great. She's really pushing through.
Narrator: Her midwife feels it's time to break her water with an amni hook, since she can feel the amniotic sac bulging. This is a common procedure and usually helps speed up the labor process.
Samiyyah: I thought it would be painful, but it wasn't at all. Actually it was like a relief of pressure.
Midwife Julia Rasch: Large amount of clear fluid. Beautiful.
Narrator: Her contractions now intensify as she starts to feel the urge to push. This is called hard labor or transition. The muscles your body uses to contract are transitioning from dilating the cervix to pushing the baby down and out.
Midwife: The intensity of the contractions is increasing, and just a certain force is now really behind that baby coming.
Narrator: Transition can be the most painful part of labor -- but usually the shortest phase.
Narrator: Though most mothers dilate nearly 8 to 10 centimeters before transitioning, Samiyyah is only 5 centimeters dilated and is having trouble resisting the urge to push.
Arvan: Sam, do not push. Fight it. Fight it.
Samiyyah: I'm trying!
Narrator: Her midwife agrees her body is ready to deliver. Pushing before being fully dilated is uncommon. This is why each caregiver has to manage her patient's labor on an individual basis.
Midwife: Okay now, take a breath and do it again.
Narrator: Her midwife uses her fingers to pull back her cervical opening as Samiyyah pushes.
The midwife made the right decision, listening to her body. With just 11 minutes of pushing, Arvan and Samiyyah's baby emerges.
Samiyyah: [screams]
Arvan: Good job! Good job!
Midwife: There's your baby!
Narrator: Sami Sarrajj, a healthy boy, is placed immediately on his mother's chest.
Midwife: You did it! You did it!
Narrator: Dad cuts the umbilical cord, and the midwife collects some of the cord blood for routine testing.
It's not over yet. The midwife helps deliver the placenta, and a nurse presses on the fundus -- the upper part of the uterus -- to check how much the uterus has contracted.
Applying pressure is a common practice used by caregivers to help expel excess blood.
Samiyyah tore along her previous episiotomy line, and her midwife repairs it with stitches, which takes 15 minutes to complete.
Arvan: You did a hell of a job... Yeah!
Narrator: Samiyyah is now breastfeeding and bonding with her baby. Incredibly, in an hour, she is showered up and savoring some well-deserved fettucini Alfredo.
It was a fast delivery, with just four hours and 11 minutes of labor. Samiyyah's natural birth is a success, and she's ready to try it again.
Samiyyah: One more. We're going to try for a girl. (laughs)
Narrator: Everyone played a supportive part on the birth team… Even big brother Safi got to announce the news that his brother was born.
Live birth: C-section surgery | Video
Medically reviewed by Lizellen La Follette, M.D.
Dr. Lizellen La Follette: Oh, good morning, Ryan. Good morning, Melisha. You're thinking positive, kiddo. You're having Boston today?
Melisha: Yeah.
Nurse: What a great name.
Dr. Follette: Right? Is it a great name?
PREPARING FOR THE C-SECTION
Dr. Christopher Hatch: So, I'm Dr. Hatch. I'm going to be your anesthesiologist today.
Melisha: Okay.
Dr. Hatch: Sounds like they weren't able to get an IV in you, so I'm going to take a look at it and see if I can help you out there.
Nurse: Let’s only do this once, okay.
Dr. Hatch: Okay, my dear, on the count of three a pinch. Ready? Get you numb. One, two, and three – big pinch.
Nurse: Deep breaths. Deep breaths.
Deep breaths.
Dr. Hatch: Breath, breath, breath. Burn, burn, burn. So sorry.
Melisha: Ouch.
Dr. Hatch: How's your hand? Is it going numb?
Melisha: Yes.
Dr. Hatch: Deep cleansing breaths. That's what we do. Hang tight. I'm just putting – it's all right. It's in.
Ryan: It's already in.
Nurse: I'll dress it.
Dr. Hatch: Okay. I'll just hold this like this for you while you do it. It's always good to have say. So, there's no more needle in there, okay? Take deep cleansing breaths. This is just a nice big dressing that's going to go on and make sure this wonderful IV doesn't go anywhere. Okay?
Melisha: All right.
Dr. Follette: Here we go. It's a little cold in here, Melisha, but that little step stool is your spot.
Dr. Hatch: No surprises. That's the deal. Okay?
Okay?
Dr. Follette: Here we are.
Dr. Hatch: You're going to do great. Do you know what you're having this time?
Melisha: A boy.
Dr. Hatch: Right on. Okay. Lots of cold soap on your back. Okay?
Melisha: Okay.
Dr. Hatch: I'm not going to sneak up on you, okay? I promise.
Melisha: Okay.
Dr. Hatch: Okay, another drape on your back, a little bit cold, a little bit sticky.
Honestly, your job right now is to just focus on, before you know it, you're going to be seeing this person. And at that point nothing else is really going to matter what's going on.
Does that feel like I'm pushing right over the bones of your back or like I'm pushing right over your spine? Perfect. I'm going to put some local anesthesia in there, it's going to sting a bit. Remember like for the IV? You're going to feel that on the count of three, okay? Take a nice deep breath for me. One, two, and three – big pinch.
One, two, and three – big pinch.
Dr. Follette: Good job.
Dr. Hatch: You're doing great.
Dr. Follette: Wow, awesome, Melisha.
Dr. Hatch: Nice, easy, deep breaths. Okay? Okay, you're doing a great job.
Dr. Follette: It's very hard to get your spine to bend when you have a baby in front. So part of it is just trying to get the spaces for Dr. Hatch.
Dr. Hatch: That's more challenging when you're shorter as well, because everything's a bit more compressed.
Dr. Follette: Still feel pressure.
Dr. Hatch: I think we're just dealing with very tight spaces.
Dr. Follette: Yeah, stay in that same position. You're doing great.
Dr. Hatch: You're doing super great, everything's fine, okay? But I think we're in the right spot now.
Melisha: Okay, okay, okay, okay.
Dr. Follette: Yeah. Nice. Beautiful. Good job.
Dr. Hatch: Okay, just going to hold super still for me. You're going to feel some pressure and some warmth in your back now.
Dr. Follette: Remember the warmth?
Dr. Hatch: Pressure and warmth. You're doing amazing.
Dr. Follette: Wonderful.
Dr. Hatch: Any more pain?
Melisha: No.
Dr. Hatch: Perfect.
Dr. Follette: Done. Okay. I know.
Dr. Hatch: You were super patient with that. Someone could help them with the legs and then we'll just kind of rotate in.
Dr. Follette: Down on your elbow. Just straight down on your elbow. We got your legs.
Melisha: My legs are numb.
Dr. Hatch: I know. It's going to be fun.
Dr. Follette: Yeah, that's it, remember. That was the point, remember?
That was the point, remember?
Dr. Hatch: We make you numb and then we try to make you move, right?
Melisha: Okay.
Dr. Follette: We're going to listen to Boston's heartbeat, and then we're going to put the catheter in, and then we're ready to go. Okay, guys? Are you guys okay for us to scrub?
Melisha: Where's my husband?
THE SURGERY
Dr. Follette: But you shouldn't be able to feel much except for maybe the pressure in your belly.
Dr. Hatch: You might feel a little pressure.
Just keep in mind, you're the center of our universe. Okay? We're all here for you, all right?
You're going for it here. Very good. Sorry dear, it's a way to help them retract, okay?
Dr. Follette: Okay, we're going to go scrub. Okay? We're going to go scrub and then we'll bring Ryan in. Okay, everybody? Okay, we're putting our gloves on, and we're going to put the drape on, and then we'll bring Ryan.
Dr. Hatch: Her vital signs are perfect, she just feels a little yucky right now, which is pretty standard.
Dr. Follette: Okay. You're going to feel some pressure. We're going to get Ryan in, in a second. That'd be nice.
Melisha: I'm feeling better.
Dr. Follette: Good, you should.
Melisha: Oh, God, thank you.
Dr. Follette: All right?
Dr. Hatch: I mean there's nothing fun about that initial feeling.
Dr. Follette: Okay, let's just measure for fun.
Dr. Hatch: What time for the time up then, Jordan?
Jordan: Hold on, I'm getting there right now. Fifty-four. 08:54.
Dr. Follette: It's marked and we're ready to go. Dr. hatch, we are good. Ready? We got Ryan to come?
Dr. Hatch: He's going to be here in two seconds, okay? We're going to step out the door and get him now.
Dr. Follette: We're starting.
Dr. Hatch: What did you all say time-wise? What did your computer say?
Jordan: Get a hold right there.
Dr. Hatch: Thank you.
Ryan: You look great.
Melisha: Okay. Thank you.
Dr. Follette: Getting through all the layers. You can see beautiful layers. Watch out for the knife. Okay. Let's get the Bovie back just for fun. You're doing great, Melisha. We've already started, okay, cutie? We've already started. We're just going through the fascial layers now. All the layers, your beautiful muscles, you'll be pleased to know we're separating them not cutting them.
Okay. We're in the fascial layers now. Everybody's good. We're going through all the layers, okay? Make sure all the layers are all good. Making sure the bladder's out of our way. Metzenbaums again. Thank you. Just going through all the layers. There's some scarring here, so we're just getting a little layers up.
There's some scarring here, so we're just getting a little layers up.
Melisha: Okay. My chest feels tight.
Dr. Hatch: You're just going to feel funky like that. Right now your oxygen saturation is 100 percent. Okay? So that's all good.
Melisha: I'm okay. I'm okay.
Dr. Hatch: You're doing a great job.
Melisha: I trust you. I trust you.
Dr. Follette: Everything's going great.
Melisha: Okay.
Dr. Follette: You're going to feel some pulling.
Melisha: I feel pulling, yes.
Dr. Hatch: Yes. A lot of pulling, a lot of tugging, a lot of pressure. And at some point, honestly, it's going to feel like someone sitting on your chest, okay? That's normal because they're putting a lot of pressure at the top of your belly to help deliver, okay?
Dr. Follette: Alexis retractor. Remember it's two pieces of almost cellophane. It's like a retractor so we don't have to pull and tug. So we bring it in and then we let the uterus come to us when we fold it down. Okay. All right. We ready for uterine incision, everybody? Gonna start here. Uterine.
Remember it's two pieces of almost cellophane. It's like a retractor so we don't have to pull and tug. So we bring it in and then we let the uterus come to us when we fold it down. Okay. All right. We ready for uterine incision, everybody? Gonna start here. Uterine.
Speaker 6: What's your time now?
Speaker 8: 9:01
Dr. Follette: We want to be very careful because everything's nice and thin here, and we would like to stay away from any parts of the baby. Here we go. There's the amniotic sac, so I obviously didn't go underneath the sac, so that's good. Butt is here, so we need to deliver this baby breech. Butt's here.
Melisha: Oh, my chest.
Dr. Hatch: Lots of pressure here. Lots of pressure.
Dr. Follette: Hold on. Hold on. Lots of pressure from us. Here comes the baby's butt. We're coming out butt first. Look at the baby's first. Hi, cutie. Umbilical cord around the body here. Here's an elbow. There's another baby delivering itself. Hi! This is Boston. Let's see if we can show Melisha. Can I show Melisha her cute little boy? Melisha, look. Look at this cutie. Can you see him?
Here's an elbow. There's another baby delivering itself. Hi! This is Boston. Let's see if we can show Melisha. Can I show Melisha her cute little boy? Melisha, look. Look at this cutie. Can you see him?
Ryan: Oh.
Dr. Follette: You got him? Congrats. Hi, Boston. You tell us, buddy. You're nice and loud. You're nice and loud, buddy. Nice and loud. You got him?
Ryan: Buddy. Hey big boy.
POST-OPERATION
Dr. Follette: Placenta is out and doing great. Wiping the uterus clean. Just to make sure, I'll take some rings so we can see all the layers. We'll go and then we'll take a stitch.
Nurse: You can come on over and meet him if you'd like. He's ready for you.
Dr. Follette: We're closing the first layer. We'll have a second layer after this, okay?
Melisha: Hi, baby. Hello. Hi.
Dr. Follette: So what we're trying to do is clamshell the uterus to hide the first layer of stitching by pulling the uterine layer around it so that it hides it and it gives it a second strength layer. So that's called a two-layer closure, which is our normal layer closure that we have for a c-section.
So that's called a two-layer closure, which is our normal layer closure that we have for a c-section.
Everybody's good, Melisha.
Melisha: The baby's okay?
Speaker 6: Yeah, look at him. Oh, he's touching you.
Dr. Hatch: Everything's fine. He's just chilling right now. It's all good. Are you doing okay?
Melisha: Yeah.
Dr. Hatch: Yeah? Good.
Dr. Follette: Tubes and ovaries over here looking good. This side, that looks good on that side, Jackie. We're done. Okay. We're going to put the uterus back in. Okay. In it goes and then we're going to take the retractor out.
I'm going to close this all in one big layer. Trying to stay away from all the vessels and make sure we're fine here. All right. We will close now the fascial layer and then everything's fine up here, Dr. Hatch.
Dr. Hatch: Yeah? Okay, great.
Dr. Follette: It went great. Uterus is closed.
Follette: It went great. Uterus is closed.
Nurse: Let's see how big he is?
Ryan: Ooh. We weren't expecting that one.
Nurse: 36-80. 8 pounds, 2 ounces.
Ryan: 8 pounds, 2 ounces, babe.
Dr. Follette: And that's a big – yeah, no kidding. Eight pounds.
Melisha: I knew he was big.
Dr. Follette: He was, cutie gets some credit for that.
All layers are closed, Melisha, and you will not have any staples or anything to take off. It's all underneath the skin. I know, right?
Congratulations. Boston's born. And thanks, everybody.
Melisha: Thank you for everything.
Dr. Follette: I know, right? Come on. We did it. Hello you, Boston.
Ryan: Thank you. Thank you.
Dr. Follette: Oh my goodness. Look at the chubster.
Ryan: Very happy dad. I'm glad mama's doing okay.
I'm glad mama's doing okay.
Dr. Hatch: Thanks everyone.
Dr. Follette: Thanks, Pauline.
Nurse: Now we're in recovery. Basically you'll be here. We'll be checking on your vitals for the next hour or so, and when everyone is ready to go we'll move you directly to your postpartum room, where you'll be for the next three to four days.
Nurse: Okay. We want to see, can you move your legs now?
Melisha: No.
Nurse: Move your toes?
Melisha: I can't.
Nurse: Okay, so we're going to put your head up a little bit. When I put your head up, if you feel nauseated or dizzy or anything, you tell me immediately.
Melisha: Okay.
Nurse: Okay?
Any questions for me?
Melisha: When can I start nursing?
Nurse: Right now.
Nurse: We're going to go on the side to start with just because you'll be able to use your hand when you need it. I'm going to put him back inside your gown. How does that feel?
Melisha: Fine.
Nurse: I'm going to try to bring his lower lip down just a little bit more. There we go. That's the one. How does it feel?
Melisha: Like he's sucking.
Nurse: Perfect. Not biting?
Melisha: No.
Ryan: Good job, Mama.
Melisha: Thank you. It was not easy. The staff was really helpful, so I'm so grateful for them. I started sobbing because I was so happy and he's so healthy and I think that was the biggest thing. Having a healthy baby at any age is a blessing but especially when you're older. I'm just really grateful. Yeah.
Video production by MEgTV
“His organs and systems are not ready” Why are they trying to save children in Russia who have almost no chance of surviving and being healthy: Society: Russia: Lenta.ru
period (less than 22 weeks) and extremely low weight (less than 500 grams). This happened after a series of criminal cases that the Investigative Committee initiated against obstetricians. So, neonatologist Elina Sushkevich from Kaliningrad was accused of killing a 22-week-old boy. Why are they trying to save 500-gram children in Russia at all today, what are their chances of surviving and whether they can grow up healthy - Lenta.ru learned from the doctor of medical sciences, head of the scientific department of neonatology and pathology of young children at the Research Clinical Institute of Pediatrics named after Yu.E. Veltishchev Elena Keshishyan. nine0003
This happened after a series of criminal cases that the Investigative Committee initiated against obstetricians. So, neonatologist Elina Sushkevich from Kaliningrad was accused of killing a 22-week-old boy. Why are they trying to save 500-gram children in Russia at all today, what are their chances of surviving and whether they can grow up healthy - Lenta.ru learned from the doctor of medical sciences, head of the scientific department of neonatology and pathology of young children at the Research Clinical Institute of Pediatrics named after Yu.E. Veltishchev Elena Keshishyan. nine0003
***
Lenta.ru: Now the minimum criteria for saving premature babies are 22-23 weeks and 500 grams of weight. Why?
Elena Keshishyan : In order to understand what is the limit of possibilities both in technical terms (creation of an environment close to intrauterine), and in terms of the maturity of the child's brain, which is able to develop out of utero, attempts were made in the world to give birth to premature babies of different ages. The greatest successes in this were achieved by the Japanese. They tried out babies born at 20 weeks. That is, the approximate gestational age was five months. The Japanese succeeded, but in isolated cases. And they saw that in children born at this age there is no differentiation of the brain, division into gray and white matter. Roughly speaking, this process determines the ability to think, to feel. This is called higher nervous activity. It is this ability that distinguishes man from animals. nine0003
The greatest successes in this were achieved by the Japanese. They tried out babies born at 20 weeks. That is, the approximate gestational age was five months. The Japanese succeeded, but in isolated cases. And they saw that in children born at this age there is no differentiation of the brain, division into gray and white matter. Roughly speaking, this process determines the ability to think, to feel. This is called higher nervous activity. It is this ability that distinguishes man from animals. nine0003
Therefore, guided by research data and on the basis of a humanistic idea, the World Health Organization has established this limit for human live birth - 23 weeks, which corresponds to approximately 500 grams of weight. This is the minimum age at which the brain can differentiate into gray and white matter. And, accordingly, there is hope that it will already be a human person with mental abilities.
Countries with technological capabilities, including Russia, have agreed that those born at this gestational age can legally be considered human. That is, they have all human rights, including medical care. nine0003
That is, they have all human rights, including medical care. nine0003
Since 2012, Russia has moved to the WHO criteria for nursing premature babies. How many of these children have been saved during this time?
As a percentage of all those born, this is a minuscule amount. I don't have exact numbers. But I want to say that the body of children born almost half prematurely is very immature. And their survival rate, conditionally, is one in a hundred. Still, 22-23 weeks is not childbirth in the full sense. From the point of view of nature, this is a miscarriage, this is a critical situation that may be associated with the health of the mother or the sick child herself. Therefore, the readiness for independent existence in such fruits is close to zero. Even if we assume that the maximum efforts of doctors are thrown to save the child, all the necessary equipment is connected, the chance that he will get out is very small. In such an infant, the kidneys, gastrointestinal tract, heart and other organs may not work. This is a very, very complex, jewelry work of doctors. nine0003
This is a very, very complex, jewelry work of doctors. nine0003
One of the smallest surviving premature babies in the world. Amilya Taylor was born in 2006 in Miami, USA. She spent only 22 weeks in the womb and was born with a weight of 284 grams and a height of 24 centimeters.
Photo: Baptist Health South Florida / Reuters
And dear?
Of course. A day in a well-equipped neonatal intensive care unit costs several thousand dollars. And to leave such a child, months are needed. But I want to emphasize that the number of survivors in this period is minimal. And it is minimal in almost all countries where the WHO criteria apply. nine0003
If these children are not viable, cost too much, then why were these criteria established?
The medical task here is not at all to save without exception all children born at a term of five months. It is clear that there is not a single person who does not understand that this child is at risk of being blind, deaf and immobilized. The task of medicine in this situation is to acquire knowledge and experience.
The task of medicine in this situation is to acquire knowledge and experience.
Obstetricians learn how to prolong pregnancy as much as possible. There is a whole range of activities: prenatal diagnosis of genetic chromosomal diseases, various fetal malformations, identification of risk groups among pregnant women, their special monitoring, prenatal logistics and routing. They also hone the ability to properly take birth at this time. This must be done as carefully as possible and do not forget about the "golden hour". It is necessary to have time to give the child, without waiting until his condition worsens, what he could not get from his mother. That is, even if the child screamed, you need to understand that soon he will stop doing this and will not be able to breathe. The "golden hour" essentially determines whether or not there will be damage to brain cells. This means whether or not a child will have a full life. nine0003
And the qualifications of resuscitators working with such children are growing today. All this led to an important point: the quality of nursing of children born a little later, at 26-28 weeks, has become much better. I see these babies regularly. And I can say that over time, many of them are no different from their peers.
All this led to an important point: the quality of nursing of children born a little later, at 26-28 weeks, has become much better. I see these babies regularly. And I can say that over time, many of them are no different from their peers.
And before?
About 30 years ago, about six or seven out of ten children would have become severely disabled. And today I had three 26-week-old babies at my appointment. And everyone is developing quite well, there is a slight backlog, but they will catch up. These children no longer have those possible malformations that, unfortunately, would have necessarily arisen in past years. nine0003
And this became possible thanks to the experience, the accumulation of knowledge about how such babies develop. There are no small things. This applies to everything - how to evaluate the heartbeat, how to interpret blood tests, and so on. Caring for a premature baby, both in the neonatal period and later, in the first or second year of life, is not the same as managing a normal, full-term baby. But knowledge allows timely adjustment of development, without even waiting for problems.
But knowledge allows timely adjustment of development, without even waiting for problems.
Photo: Science Photo Library / East News
It is important to understand that a premature baby is not a small copy of a normal one. This is a child who is forced to adapt to extrauterine life, when physiologically he should not do this. Its organs and systems are not prepared to function in the new conditions.
"This is painful love at the level of deep depression"
What do such children most often suffer from?
One of the typical pathologies is retinopathy of prematurity. In children, the mechanism that protects the eye from light has not yet matured. And they experience a real shock, suddenly falling into our bright world. Photons of light and the flow of oxygen begin to act on the retina, its vessels begin to grow rapidly, penetrate all the media of the eye, and, ultimately, exfoliate the retina, leading to total blindness. Earlier, even when I was just starting to work, although we knew about such a disease as retinopathy of prematurity, there were few children born and surviving at gestational ages of less than 30 weeks. Therefore, no one knew how to treat this disease. It's scary to remember, but premature babies were in wards with round-the-clock lighting. The light was needed so that doctors and nurses could observe the baby's condition and notice changes in time. At that time, six out of ten children whose birth weight was less than a kilogram went blind. Just then, the borders were opened in Russia, and we were amazed that in Europe, a maximum of two out of ten newborns had blindness. nine0003
Therefore, no one knew how to treat this disease. It's scary to remember, but premature babies were in wards with round-the-clock lighting. The light was needed so that doctors and nurses could observe the baby's condition and notice changes in time. At that time, six out of ten children whose birth weight was less than a kilogram went blind. Just then, the borders were opened in Russia, and we were amazed that in Europe, a maximum of two out of ten newborns had blindness. nine0003
But we started learning very quickly. Now in perinatal centers in all intensive care units for premature babies - twilight. The cuveuses are completely covered with dark blankets. The staff does not need to watch the baby all the time - all readings are automatically recorded by special devices. In good ICUs, nurses who approach babies have headlights. This is to avoid disturbing other children. In many intensive care units, a large “ear” hangs. If the decibel level in the room begins to exceed the allowable limit, the device lights up red. nine0003
nine0003
After the birth of the child, every week they begin to look at the eyes with a special method. If there is proliferation of blood vessels, laser coagulation of the retina is performed. There are specialists in such operations in almost every major city.
Approximately 400-600 babies pass through me every year, born at 26-28 weeks. Over the past few years, not a single blind person has been among them. Although earlier in hospitals for such newborns it was necessary to open entire departments.
Is there any data on how many premature babies later became healthy? nine0003
Now, among premature babies born at five or six months (25-26 weeks of pregnancy), 25-30 percent become disabled. The same is true in developed countries. And even 20-30 years ago there were 75-80 percent of them.
The risks for these children are still very high. They require long-term observation and treatment. But still today they have incommensurably or better chances than before.
Photo: East News
Do unfortunate parents regret insisting on resuscitation at all costs? nine0003
As a doctor, no one has ever told me this. Naturally, the families had very different hopes for childbirth. In the doctor's office they cry, but they don't moan. These children are madly loved. But this is painful love at the level of deep depression. Probably, some of these mothers may think at night what would happen if they knew in advance how everything would turn out. Perhaps they voice this to their mothers, husbands, girlfriends ... But not to doctors. This is where people prefer to stay.
When a child is one or two years old, from a moral point of view, the situation is more difficult than in three days. Newborns are all wonderful bags, it is only then that children begin to differ from each other. These families have a very specific and difficult life. When a child lies at home, does not move, does not swallow, never looks at you, does not speak - this is very difficult. And parents need to be helped to turn their life into at least a relatively social one, not to make them outcasts. nine0003
And parents need to be helped to turn their life into at least a relatively social one, not to make them outcasts. nine0003
What family support can I expect now?
When Russia switched to WHO standards, doctors began to say that if we started caring for such children, there would be a high incidence of cerebral palsy, mental retardation and other pathologies leading to severe disability. Without the development of a specialized service that will help such children, we will inflict enormous damage on a society that will not accept such an increase in the number of people with disabilities. Then a follow-up system for premature babies began to develop, which leads them up to three years. Because in the usual polyclinic network there are not always doctors who understand how a child born with low or extremely low body weight grows and develops. In parallel with this, the system of medical rehabilitation is developing quite rapidly. nine0003
The worst situation is with the social service. Help for these children is minimal. Few people explain to families how to care for such a child, how to develop him, how to maintain motor skills. If in large cities at least some minuscule can be achieved, then what can we say about the province? All this turns one of the parents out of social life. There are no places where it would be possible to transfer such a child at least for a week, a month, so that the parents could have a little rest. Since the state has taken such a step, since we have legally recognized a 500-gram fetus as a person, then they themselves also need to act humanly in the future with his family. nine0003
Help for these children is minimal. Few people explain to families how to care for such a child, how to develop him, how to maintain motor skills. If in large cities at least some minuscule can be achieved, then what can we say about the province? All this turns one of the parents out of social life. There are no places where it would be possible to transfer such a child at least for a week, a month, so that the parents could have a little rest. Since the state has taken such a step, since we have legally recognized a 500-gram fetus as a person, then they themselves also need to act humanly in the future with his family. nine0003
Is there a support system in other countries?
I know that in Europe and in the USA it is built very well. The emphasis is not on medical rehabilitation, but on social rehabilitation. They have social workers who come and relieve these families of a significant part of their worries. Somewhere there are social centers where a child can be taken to a kindergarten. Moreover, they are zoned - parents do not need to go to the other end of the city.
Moreover, they are zoned - parents do not need to go to the other end of the city.
Photo: Alexander Kondratyuk / RIA Novosti
“Even if it is clear that a child has pathologies that are incompatible with life, they must be saved to the last”
You say that some time ago, 1kg premature babies were also considered “non-residents”, but now they are quite promising. Is it possible that in 30-40 years the same can be said about 500-gram ones?
Indeed, even 30-40 years ago, when it was not possible to maintain breathing, children born before seven months of age survived very rarely. nine0003
Then, when some first mechanisms appeared, the bar was raised until the 28th week of pregnancy, which is about six months. But technological progress is always moving forward, and this has allowed us to further gradually reduce the age of survival. We can now at least partially simulate intrauterine conditions. For example, when a child is not born on time, he does not yet have a substance in his lungs, thanks to which he can breathe - surfactants. They can be introduced immediately at birth, start artificial ventilation of the lungs and thereby support gas exchange. It also became possible to give nutritional subsidies not through the gastrointestinal tract, but through a vein with special substances that are already ready for inclusion in metabolism. There are many other adaptations: the creation of a thermal regime, humidity close to intrauterine. nine0003
They can be introduced immediately at birth, start artificial ventilation of the lungs and thereby support gas exchange. It also became possible to give nutritional subsidies not through the gastrointestinal tract, but through a vein with special substances that are already ready for inclusion in metabolism. There are many other adaptations: the creation of a thermal regime, humidity close to intrauterine. nine0003
Technologically, the frontier could move indefinitely. If desired, you can simulate a situation where a woman is not needed at all to bear a child. But I have already said that scientists have established that the age of 22-23 weeks is the minimum period at which the cells of the cerebral cortex can develop postnatally. Still, the main criterion for the normal development of a child is not technological achievements, but the capabilities of the brain.
Is it true that they try to save all 500-gram children only in Russia and Turkey, and in other countries - only if the child has high chances for a normal life? nine0003
This is not true. In all countries where the WHO concept has been adopted, these children are subject to mandatory medical care. But there are nuances. If the baby was born between the 23rd and 25th weeks, parents can refuse resuscitation. To do this, in many countries there is a legal standard, reminiscent of the law on euthanasia.
In all countries where the WHO concept has been adopted, these children are subject to mandatory medical care. But there are nuances. If the baby was born between the 23rd and 25th weeks, parents can refuse resuscitation. To do this, in many countries there is a legal standard, reminiscent of the law on euthanasia.
There is a special service in perinatal centers. When it becomes clear that preterm labor has begun, representatives approach relatives - the father and, if possible, the mother. “We assume that a baby will be born with such and such parameters. In this case, there are such and such development risks ... You have the right to choose either full resuscitation or palliative care. And depending on what the parents decide, the doctors act. nine0003
Photo: Sergey Pyatakov / RIA Novosti
In Russia, you can also choose a palliative today, right?
This is not prescribed by law. Today, even if it is clear that a child has pathologies incompatible with life, they must be saved to the last.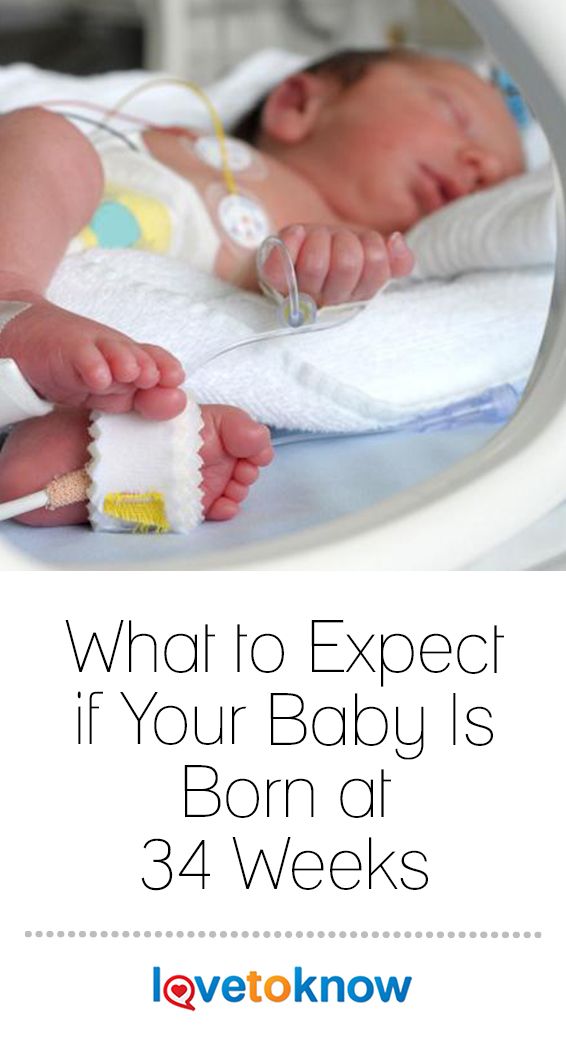 It happens that parents can sign a paper on their own that they would not like resuscitation, but this has no legal force. Parents can say, “Look, he is breathing, breathing. He opened his eyes. Let's revive him now!" And we lost time, which in this case is very important. This child initially has little chance, but it has become even less. And a situation may arise when parents accuse the doctors that their child was not specially treated, “talking teeth”. nine0003
It happens that parents can sign a paper on their own that they would not like resuscitation, but this has no legal force. Parents can say, “Look, he is breathing, breathing. He opened his eyes. Let's revive him now!" And we lost time, which in this case is very important. This child initially has little chance, but it has become even less. And a situation may arise when parents accuse the doctors that their child was not specially treated, “talking teeth”. nine0003
The medical community is very concerned about this ambiguous position of doctors. And we have a number of proposals to solve the problem of their protection.
What exactly is offered?
Legislative initiative to allow parents to independently decide whether resuscitation care is appropriate for a child born between the 23rd and 25th weeks. Naturally, all this should be discussed. It is necessary to involve the public in the discussion: these are lawyers, doctors, patient communities, representatives of religious denominations. nine0003
nine0003
The Ministry of Health has now prepared new criteria for newborns born too early. In particular, it is proposed not to register such a child until he has lived seven days. Maybe this will fix the situation, protect doctors from murder charges?
There are a lot of pitfalls here. In Russia, there was a similar law on kilogram children. They were assisted from birth, but until the age of seven days the child was considered a fetus. If he died, then his mortality already went into other criteria, it was not considered the death of a newborn. nine0003
There are not many children born with extremely low rates, they simply cannot influence the demographic structure in any way. But if there is such a situation that you can not register for up to seven days, it seems to me that even more claims may arise against doctors regarding the failure to provide assistance.
These are very difficult questions. On the one hand, parents can say: you did not save the child. And others, on the contrary, will say: why are you torturing him in vain? And imagine a resuscitator who may be faced with an ethical choice: he has only one ventilator in the hospital, and a 23-week-old baby has been on it for the 40th day. And then a 32-week-old is born in the hospital. He needs help, hold him for three days on the device, and then the baby will cope on his own. In the first case, there will certainly be a disabled person. And in the second - almost healthy. And what should a doctor do? nine0003
And then a 32-week-old is born in the hospital. He needs help, hold him for three days on the device, and then the baby will cope on his own. In the first case, there will certainly be a disabled person. And in the second - almost healthy. And what should a doctor do? nine0003
Are you speaking theoretically now or do such situations occur?
We cannot have this in federal centers. We have enough equipment. I just illustrated with an example that the issue of nursing such children is the most difficult, all aspects are in common in it - from medical to ethical and religious.
Photo: Sergei Krasnoukhov / RIA Novosti
“The issue of infant mortality has always been political”
The issue of infant mortality has recently become political. Perhaps that is why patient scandals associated with maternity hospitals are developing so sharply? nine0003
The issue of infant mortality has always been political. This is a socially significant parameter that determines the position of the country in terms of development. In our country as a whole, infant mortality has significantly decreased over ten years. However, in the last two years the rate of decline has slowed down. Our government says it's bad. From the point of view of doctors, this is not entirely true. There are objective reasons that cannot be overcome with a swoop.
In our country as a whole, infant mortality has significantly decreased over ten years. However, in the last two years the rate of decline has slowed down. Our government says it's bad. From the point of view of doctors, this is not entirely true. There are objective reasons that cannot be overcome with a swoop.
The primary decrease in mortality occurred due to the high-quality saturation of hospitals with equipment, due to the construction of perinatal centers. This gave immediate results. And now these figures have reached a plateau. Another thing is that a plateau, for example, in Kaliningrad, St. Petersburg, is one thing. There mortality rates are at the European level. That is very low. And there are regions where mortality is high - the Altai Territory, the Jewish Autonomous Region, Magadan. There is a lack of doctors, a lack of equipment, very long distances, routing difficulties. And it's very difficult to do anything about it. nine0003
We are not compact Switzerland. We have a huge country with difficult geographical conditions. There are regions where we cannot even deliver a woman by helicopter. At one time I spent a lot of time in Chukotka, watching the obstetric service. Often, if a premature baby is born there, you will not help him in any way.
We have a huge country with difficult geographical conditions. There are regions where we cannot even deliver a woman by helicopter. At one time I spent a lot of time in Chukotka, watching the obstetric service. Often, if a premature baby is born there, you will not help him in any way.
There are no good hospitals there?
Everything is there, but in one city - in Anadyr. And if a woman gave birth in another place, then often she can be cut off from the world. There are periods when even planes do not fly: a snowstorm, something else. And with routing too you will not guess. Because when you are expecting your first child, you are not going to give birth at 24 weeks. This is if the situation with childbirth repeats, then you can plan something, come closer to specialized care at the “dangerous” time ...
Is it true that there have been more premature births lately?
No, their number is stable. This is approximately 7-10 percent of all newborns. Significantly increased their survival rate.
One of the most "inciting" topics on parenting Internet forums is that children who are "culled out" by nature have a bad effect on the quality of the gene pool. Is there any reason to think so?
In order for "survivors" to be able to influence the population, there must be a lot of them in percentage terms. For example, there are very few 26-week-olds - no more than two percent of all births. It can't affect anything in any way. nine0003
I know that at one time they discussed: what will happen if my child marries in the future someone who was once premature, will the gene pool suffer? Firstly, I can say that, as for children born after the 30th week, they are completely healthy, adapted and no different from others. They themselves give birth to beautiful healthy children, we have already seen many generations. The risk of preterm birth is not inherited. And usually premature babies are shaken, they are a lot of work. So in terms of development, these children can give odds to others. nine0003
nine0003
As for children born at 5-6 months old, when they catch up with their peers, it is important that parents continue their active life with them, and not engage in a protective regime. We need songs, dances, sports. These children have behavioral patterns. But now there are centers that supervise such families. If you take care of children, everything will be fine. I look at these kids regularly. And I have a much more optimistic outlook. For example, the frequency of chronic diseases among them is approaching the norm. That is, it is not higher than in the population. Everyone has a chance for a full life, even the most hopeless, at first glance, child. nine0003
Why big babies are born
Just 100 grams did not reach the round number - 5 kg - a girl born to Elena Stelmakh from Minsk. Yes, and the growth turned out to be model - 60 cm. Usually, babies reach such parameters in 2 - 3 months of the first year of life, and here - a newborn. In the maternity hospital, the doctors joked: "Well, you can already give to kindergarten. " This is the third child for the 34-year-old record holder mother. The two eldest sons were also born large - 4 and 4.5 kg.
" This is the third child for the 34-year-old record holder mother. The two eldest sons were also born large - 4 and 4.5 kg.
Physicians remember that “heavyweights” with a body weight of 5.4-5.6 kg were born in our country. Of course, this is not a world record, and in general, small heroes are not such a big rarity. Last year, a baby weighing 6.280 was born in Melitopol, and 29-year-old Chinese woman Wang Yujun - and does weigh 7.4 kg. His father was overjoyed: he had the largest child in the world and, moreover, in the year of the Dragon! And the newly-made mother was only surprised: she ate little during pregnancy, and did not feel at all that she was carrying such a giant under her heart. And really, why are big babies born all of a sudden? Can this be predicted? Do they threaten to become Dobrynya Nikitichs in the future?
Heroic character
— At birth, I myself weighed about 3 kg, fragile and small, and in general I never had large forms. And the husband was born on 3.200. So the children, as you can see, did not grow up to be broad-shouldered heroes in the end, they are thin and far from the tallest, - Elena Stelmakh laughs. When do they gain weight? They, on the contrary, lose it, because they do not sit still for a minute. nine0003
And the husband was born on 3.200. So the children, as you can see, did not grow up to be broad-shouldered heroes in the end, they are thin and far from the tallest, - Elena Stelmakh laughs. When do they gain weight? They, on the contrary, lose it, because they do not sit still for a minute. nine0003
Elena says that the eldest, 11-year-old Dima, began to walk at 9 months, 5-year-old Matvey - at 7 months and 4 days. The doctors at the polyclinic, when they saw that he himself entered the office, threw up their hands: they say, what are you doing, mommy, the spine is still weak, God forbid that ... But can you stop Matvey?
“Now the kindergarten teachers walk hand in hand with him, so they are calmer,” says Elena. - After all, he needs an eye and an eye. Either he smears cream on his eyes, then he breaks his forehead, then the dog bites - you need to kiss her. Yes, and Dima is just as restless. Teachers say: “I could have studied better, but in the classroom he constantly indulges. It seems that he does not listen, he distracts others, but he answers. I say: he probably has a third ear. nine0003
It seems that he does not listen, he distracts others, but he answers. I say: he probably has a third ear. nine0003
Newborn Masha is also growing up to be a restless and strong man. You can’t wrap it in a diaper, you immediately get your hands. She is not yet a month old, but she already holds her head confidently, and reaches for toys, takes the pacifier out of her mouth and studies it with interest, recognizes her brothers. In general, he behaves like a three-month-old baby.
— Just as fast! - Elena hugs her "baby" to herself. - When they chose a name for her, Matvey suggested calling Masha, but only so that she would not be as restless as in the cartoon. But you see how ...
Yes, large children surprise not only with their body weight and height at birth, but also with the pace of development. Experts note: a doubling of the weight, which is usually observed in infants at 5-6 months of age, occurs in accelerating children as early as 4 months. By this moment, their chest circumference becomes larger than their head circumference, which also overtakes all deadlines. The fontanels of little heroes grow faster, teeth erupt earlier...
The fontanels of little heroes grow faster, teeth erupt earlier...
For Elena Mitrodorova, a resident of the village of Machulishchi, the birth of her son Timofey, weighing 4.520 and 60 cm tall, was also a surprise. Who is this? Elena herself is thin and short - 1.62 meters. And the husband is small. The eldest daughters were born with the usual weight - 3.200 and 3.500. But the guy succeeded at least where. Moreover, Elena gave birth to him easily and without complications. nine0003
At first, Timofey grew by leaps and bounds. New clothes became small in a week. For 4 months I grew by 10 cm and added more than 5 kg. At six months he began to crawl, by 10 months he was walking. By the year 12 teeth erupted. But the growth rate has slowed down. When he was a year old, he weighed 12 kg with a height of 76 cm. “Besides, we don’t really indulge him in food because of allergies. And he is not capricious: what you give, he eats everything. It's very easy with him. When I was born, I slept like an adult: from 11 pm until morning! nine0003
Weight paradoxes
Many people think that the birth of a large child is a real gift of fate. "The hero is born!" - hears the mother of the newborn. But doctors are stingy with emotions. They say that it’s harder to give birth to them, they often get birth injuries: collarbone fractures, dislocations, hematomas ... According to the international classification of diseases, if a baby has a mass of more than 4 kg, this is already large, and if 4.5 kg or more is an excessively large child .
"The hero is born!" - hears the mother of the newborn. But doctors are stingy with emotions. They say that it’s harder to give birth to them, they often get birth injuries: collarbone fractures, dislocations, hematomas ... According to the international classification of diseases, if a baby has a mass of more than 4 kg, this is already large, and if 4.5 kg or more is an excessively large child .
“It's wrong to talk about records in the birth of large children,” says Natalya Litvinovich, head of the maternity and physiological department of the Republican Scientific and Practical Center “Mother and Child”. - Babies should fit the size of the mother's pelvis. In my practice, there was a child of 5.1 kg, who was born on her own, through the natural birth canal. Mom was 18 years old, of average height, did not overwear. Therefore, for us, such a large weight was a surprise, we expected 4 kg with a little. Yes, the estimated mass of the child is determined on ultrasound, but . .. with a large error. Fortunately, there were no complications. It was just luck. Because a large fetus is always a risk of trauma during childbirth. If the baby is more than 4 kg, doctors begin to discuss the need for a caesarean section. nine0003
.. with a large error. Fortunately, there were no complications. It was just luck. Because a large fetus is always a risk of trauma during childbirth. If the baby is more than 4 kg, doctors begin to discuss the need for a caesarean section. nine0003
Natalya Georgievna and the mother of two “heroes” herself. The first son was born on 3800, the second on 4400. And if she gave birth to the eldest easily, then the second “heavyweight” baby made both the mother and the obstetricians nervous: he got stuck with his shoulder, dislocated his neck, had to undergo rehabilitation for 1.5 months ... Up to six months, this broad-shouldered “giant”, according to Natalia, was ahead of all tabular data on weight gain, then leveled off with all peers, and when he went to school, he became one of the smallest. “I stood last in the line, because of which I suffered terribly and worried,” Natalya recalls. - His teenage growth began later than the rest of the boys, everyone was already growing up, and he was still small. And then at one fine moment stretched out. He is now medium-sized, thin-boned, thin, 182 height. Doesn't look big. He eats a lot, but he doesn't get fat." nine0003
And then at one fine moment stretched out. He is now medium-sized, thin-boned, thin, 182 height. Doesn't look big. He eats a lot, but he doesn't get fat." nine0003
According to statistics, every tenth baby is born with us over 4 kg. The reasons for this "fatness" can be different. It's one thing when mom and dad have a heroic build. But, as the head of the department of neonatology and medical genetics of BelMAPO Georgy Shishko notes, this is rather an exception, more often small children are born to large parents, and only then they grow up as heroes. But "weightiness" at birth in some cases may indicate a mother's ill health: a violation of carbohydrate metabolism, diabetes mellitus, overt or hidden - often this disease makes itself felt during pregnancy:
— It happens that a baby is born prematurely, and his body weight is like that of a full-term baby. He is large not due to muscles, but as a result of swelling, obesity. In addition, excess insulin in the child's body negatively affects the lungs. And therefore, these children often develop a syndrome associated with impaired breathing, or hyaline membrane disease. There are enlarged internal organs - heart, liver. Against this background, heart failure, heart defects, deficiency of blood coagulation factors, jaundice can develop ... Therefore, it is so important to detect diabetes mellitus during pregnancy and regulate glucose metabolism so that the child does not suffer in utero. And in the future, the newborn "giant" must be examined by an endocrinologist. Because heroic weight is not a sign of heroic health. nine0003
And therefore, these children often develop a syndrome associated with impaired breathing, or hyaline membrane disease. There are enlarged internal organs - heart, liver. Against this background, heart failure, heart defects, deficiency of blood coagulation factors, jaundice can develop ... Therefore, it is so important to detect diabetes mellitus during pregnancy and regulate glucose metabolism so that the child does not suffer in utero. And in the future, the newborn "giant" must be examined by an endocrinologist. Because heroic weight is not a sign of heroic health. nine0003
Tall and "weighty" babies are traditionally considered more vulnerable than their average peers. It is understandable: the norm is always preferable, and any deviations from it to the smaller (less than 3 kg) or larger (more than 4 kg) side are alarming. However, it cannot be said that the cause-and-effect relationship “big baby - big problems” is an indisputable truth. The main thing is not the starting size, but the further development of the child.