Baby projectile vomit formula
Baby Vomiting After Feeding Formula: Causes and Treatment
Your little one is happily gulping their formula while cooing at you. They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
There are several reasons why your baby might be vomiting after a formula feeding, but it’s important to remember that it can be — and often is — very normal.
It’s common for babies to throw up sometimes after feeding on formula or breast milk. Their shiny new digestive systems are still learning what to do with all the yummy milk coming down into their tummy.
However, if your baby often has a hard time keeping their formula down on a regular and frequent basis, let your pediatrician know.
Having a baby around means getting used to soft mushy stuff coming out fairly often. This includes spit-up and vomit.
Spit-up and vomit might seem pretty much the same — and require similar amounts of cleaning to get them off of your sweater and the sofa — but they’re very different. Spitting up is an easy, gentle dribble of milk. Baby may even smile at you as the curd-like spit-up flows from their mouth.
Spit-up is normal in healthy babies, especially if they’re under the age of 1.
On the other hand, vomit takes more effort, as it comes from deeper in your little one’s stomach. It’s a sign that your baby’s stomach is saying nope, not now, please. You might see your baby strain and recoil just before they projectile vomit. This force happens because vomit is squeezed out by the stomach muscles.
Your baby might also look more uncomfortable during and after vomiting. And vomit looks and smells different. This is because it’s usually formula, breast milk, or food (if your baby is eating solids) mixed with stomach juices.
If you’re not sure whether your baby is vomiting or spitting up, look for other vomiting symptoms, like:
- crying
- gagging
- retching
- turning red
- arching their back
That said, there doesn’t seem to be agreed-upon definitions of these two terms among healthcare providers, caregivers, and others. Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Overfeeding
It’s easier for your baby to overfeed when they’re drinking from a bottle than when they’re breastfeeding. They can also gulp down milk faster from a bottle and rubber nipple. What’s more, because formula is always available, it’s easier for you to give them more milk than they need by accident.
Babies have tiny stomachs. A 4- to 5-week-old infant can only hold about 3 to 4 ounces in their tummy at a time. This is why they need lots of smaller feedings. Drinking too much formula (or breast milk) in one feeding can overfill your baby’s stomach, and it can only come out one way — vomit.
Not burping properly
Some babies need to be burped after every feeding because they swallow lots of air as they gulp down milk. Bottle feeding your baby breast milk or formula may lead to more air-swallowing, as they can gulp even faster.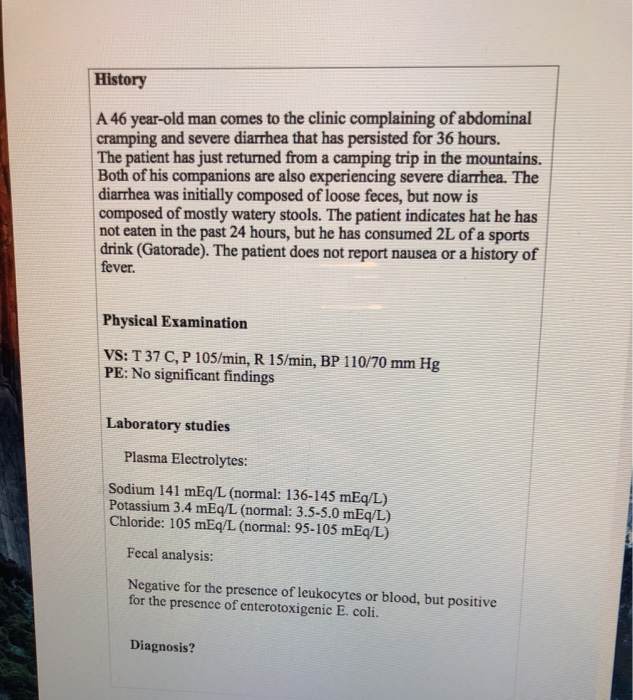
Too much air in the stomach can make your baby uncomfortable or bloated and trigger vomiting. Burping your baby right after feeding them formula may help prevent this.
To help prevent your baby from swallowing too much air and vomiting after formula feeding, check your baby’s bottle. Make sure you’re using a smaller bottle that’s just big enough to hold a few ounces of milk. Also, check to make sure the nipple hole is not too big, and don’t let your baby continue gulping when the bottle is empty.
Baby or infant reflux
Baby can have acid reflux, indigestion, or occasionally gastroesophageal reflux disease (GERD just like grown-ups! This happens because their stomach and food tubes are still getting used to holding down milk.
Baby reflux happens when milk travels back up toward your baby’s throat and mouth. This usually just causes some painless spitting up, but it can irritate your baby’s throat and trigger gagging and vomiting.
Sometimes, smaller feedings can help prevent baby reflux. If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
Constipation
While simple constipation would be an uncommon cause of vomiting in an otherwise healthy infant, sometimes baby vomiting happens because of what isn’t happening at the other end.
Most babies who are formula-fed need to poop at least once a day. Anything less than your baby’s typical pattern, though, might indicate they’re constipated.
If your baby is vomiting after a formula feeding, they might be constipated if they have other symptoms, including:
- gassiness
- not pooping for longer than 3–4 days
- a swollen or bloated stomach
- a firm or hard stomach
- crying bouts or irritableness
- straining very hard but not pooping or pooping only a little
- small, hard pellet-like poop
- dry, dark poop
Stomach bug
If your baby doesn’t usually vomit after having formula, they might have a stomach bug. Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Other symptoms of a stomach bug include:
- crying
- stomach cramps
- stomach rumbling
- bloating
- diarrhea or watery poop
- mild fever (or none at all in babies)
Allergy
In rare cases, the cause of your baby’s vomiting might be in the formula. Although it’s uncommon for babies to be allergic to cow’s milk, it may happen to up to 7 percent of babies under the age of 1.
Most children outgrow a milk allergy by the time they’re 5 years old, but it can cause vomiting and other symptoms in babies. A cow’s milk allergy might cause vomiting right after your baby eats. It can also cause vomiting and other symptoms hours or rarely days later.
If your baby has an allergy to milk or something else, they might have other symptoms of an allergic reaction, like:
- skin rash (eczema)
- diarrhea
- cough
- hives
- difficulty breathing
- wheezing
Lactose intolerance
An allergy to milk is different than being lactose intolerant. Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Your baby might get temporary lactose intolerance after getting a tummy bug or gastroenteritis, although this is uncommon.
Other symptoms include:
- diarrhea or watery poops
- constipation
- bloating
- gassiness
- stomach pain
- stomach rumbling
Note that lactose intolerance is rare in babies under the age of 1.
Other causes
Some common health conditions can cause vomiting at any time, including after breastfeeding or formula feeding. Some rare genetic conditions can also cause vomiting in babies.
Other causes of vomiting in babies include:
- colds and the flu
- ear infections
- some medications
- overheating
- motion sickness
- galactosemia
- pyloric stenosis
- intussusception
In most cases, minor tweaks can help stop your baby’s vomiting. Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
- feed your baby smaller amounts of formula more often
- feed your baby slowly
- burp your baby after the feeding
- hold your baby’s head and chest up while feeding
- hold your baby upright after a feeding
- make sure your baby doesn’t move around or play too much right after a feeding
- try a smaller bottle and smaller-hole nipple to feed
- check the ingredient list on your baby’s formula
- ask your baby’s doctor if you should try a different kind of formula
- talk to your baby’s doctor about a possible allergic reaction
- dress your baby in looser clothing
- make sure their diaper isn’t on too tightly
If your baby has the stomach flu, you’ll both usually just have to ride it out for a day or two. Most babies and children with a stomach bug don’t need treatment.
If your baby is vomiting, see your doctor or pediatrician right away if they:
- are vomiting often
- are vomiting forcefully
- aren’t gaining weight
- are losing weight
- have a skin rash
- are unusually sleepy or weak
- have blood in their vomit
- have green bile in their vomit
Also, see your doctor urgently if your baby has any sign of dehydration from all the vomiting:
- dry mouth
- crying without shedding tears
- a weak or quiet cry
- floppiness when picked up
- no wet diapers for 8 to 12 hours
It’s pretty common for babies to vomit, especially after feeding. This happens for many reasons, including that these little people are still just getting used to keeping down their milk.
Check with your doctor about what you can do. See your doctor urgently if your baby vomits often for any reason.
Baby Vomiting After Feeding Formula: Causes and Treatment
Your little one is happily gulping their formula while cooing at you. They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
There are several reasons why your baby might be vomiting after a formula feeding, but it’s important to remember that it can be — and often is — very normal.
It’s common for babies to throw up sometimes after feeding on formula or breast milk. Their shiny new digestive systems are still learning what to do with all the yummy milk coming down into their tummy.
However, if your baby often has a hard time keeping their formula down on a regular and frequent basis, let your pediatrician know.
Having a baby around means getting used to soft mushy stuff coming out fairly often. This includes spit-up and vomit.
Spit-up and vomit might seem pretty much the same — and require similar amounts of cleaning to get them off of your sweater and the sofa — but they’re very different. Spitting up is an easy, gentle dribble of milk. Baby may even smile at you as the curd-like spit-up flows from their mouth.
Spit-up is normal in healthy babies, especially if they’re under the age of 1.
On the other hand, vomit takes more effort, as it comes from deeper in your little one’s stomach. It’s a sign that your baby’s stomach is saying nope, not now, please. You might see your baby strain and recoil just before they projectile vomit. This force happens because vomit is squeezed out by the stomach muscles.
Your baby might also look more uncomfortable during and after vomiting. And vomit looks and smells different. This is because it’s usually formula, breast milk, or food (if your baby is eating solids) mixed with stomach juices.
If you’re not sure whether your baby is vomiting or spitting up, look for other vomiting symptoms, like:
- crying
- gagging
- retching
- turning red
- arching their back
That said, there doesn’t seem to be agreed-upon definitions of these two terms among healthcare providers, caregivers, and others. Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Overfeeding
It’s easier for your baby to overfeed when they’re drinking from a bottle than when they’re breastfeeding. They can also gulp down milk faster from a bottle and rubber nipple. What’s more, because formula is always available, it’s easier for you to give them more milk than they need by accident.
Babies have tiny stomachs. A 4- to 5-week-old infant can only hold about 3 to 4 ounces in their tummy at a time. This is why they need lots of smaller feedings. Drinking too much formula (or breast milk) in one feeding can overfill your baby’s stomach, and it can only come out one way — vomit.
Not burping properly
Some babies need to be burped after every feeding because they swallow lots of air as they gulp down milk. Bottle feeding your baby breast milk or formula may lead to more air-swallowing, as they can gulp even faster.
Too much air in the stomach can make your baby uncomfortable or bloated and trigger vomiting. Burping your baby right after feeding them formula may help prevent this.
To help prevent your baby from swallowing too much air and vomiting after formula feeding, check your baby’s bottle. Make sure you’re using a smaller bottle that’s just big enough to hold a few ounces of milk. Also, check to make sure the nipple hole is not too big, and don’t let your baby continue gulping when the bottle is empty.
Baby or infant reflux
Baby can have acid reflux, indigestion, or occasionally gastroesophageal reflux disease (GERD just like grown-ups! This happens because their stomach and food tubes are still getting used to holding down milk.
Baby reflux happens when milk travels back up toward your baby’s throat and mouth. This usually just causes some painless spitting up, but it can irritate your baby’s throat and trigger gagging and vomiting.
Sometimes, smaller feedings can help prevent baby reflux. If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
Constipation
While simple constipation would be an uncommon cause of vomiting in an otherwise healthy infant, sometimes baby vomiting happens because of what isn’t happening at the other end.
Most babies who are formula-fed need to poop at least once a day. Anything less than your baby’s typical pattern, though, might indicate they’re constipated.
If your baby is vomiting after a formula feeding, they might be constipated if they have other symptoms, including:
- gassiness
- not pooping for longer than 3–4 days
- a swollen or bloated stomach
- a firm or hard stomach
- crying bouts or irritableness
- straining very hard but not pooping or pooping only a little
- small, hard pellet-like poop
- dry, dark poop
Stomach bug
If your baby doesn’t usually vomit after having formula, they might have a stomach bug. Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Other symptoms of a stomach bug include:
- crying
- stomach cramps
- stomach rumbling
- bloating
- diarrhea or watery poop
- mild fever (or none at all in babies)
Allergy
In rare cases, the cause of your baby’s vomiting might be in the formula. Although it’s uncommon for babies to be allergic to cow’s milk, it may happen to up to 7 percent of babies under the age of 1.
Most children outgrow a milk allergy by the time they’re 5 years old, but it can cause vomiting and other symptoms in babies. A cow’s milk allergy might cause vomiting right after your baby eats. It can also cause vomiting and other symptoms hours or rarely days later.
If your baby has an allergy to milk or something else, they might have other symptoms of an allergic reaction, like:
- skin rash (eczema)
- diarrhea
- cough
- hives
- difficulty breathing
- wheezing
Lactose intolerance
An allergy to milk is different than being lactose intolerant. Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Your baby might get temporary lactose intolerance after getting a tummy bug or gastroenteritis, although this is uncommon.
Other symptoms include:
- diarrhea or watery poops
- constipation
- bloating
- gassiness
- stomach pain
- stomach rumbling
Note that lactose intolerance is rare in babies under the age of 1.
Other causes
Some common health conditions can cause vomiting at any time, including after breastfeeding or formula feeding. Some rare genetic conditions can also cause vomiting in babies.
Other causes of vomiting in babies include:
- colds and the flu
- ear infections
- some medications
- overheating
- motion sickness
- galactosemia
- pyloric stenosis
- intussusception
In most cases, minor tweaks can help stop your baby’s vomiting. Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
- feed your baby smaller amounts of formula more often
- feed your baby slowly
- burp your baby after the feeding
- hold your baby’s head and chest up while feeding
- hold your baby upright after a feeding
- make sure your baby doesn’t move around or play too much right after a feeding
- try a smaller bottle and smaller-hole nipple to feed
- check the ingredient list on your baby’s formula
- ask your baby’s doctor if you should try a different kind of formula
- talk to your baby’s doctor about a possible allergic reaction
- dress your baby in looser clothing
- make sure their diaper isn’t on too tightly
If your baby has the stomach flu, you’ll both usually just have to ride it out for a day or two. Most babies and children with a stomach bug don’t need treatment.
If your baby is vomiting, see your doctor or pediatrician right away if they:
- are vomiting often
- are vomiting forcefully
- aren’t gaining weight
- are losing weight
- have a skin rash
- are unusually sleepy or weak
- have blood in their vomit
- have green bile in their vomit
Also, see your doctor urgently if your baby has any sign of dehydration from all the vomiting:
- dry mouth
- crying without shedding tears
- a weak or quiet cry
- floppiness when picked up
- no wet diapers for 8 to 12 hours
It’s pretty common for babies to vomit, especially after feeding. This happens for many reasons, including that these little people are still just getting used to keeping down their milk.
Check with your doctor about what you can do. See your doctor urgently if your baby vomits often for any reason.
Rotavirus - treatment and prevention
Rotavirus - treatment and preventionRemote consultations with a doctor are available in our center! Read more
8 812 380 02 38 St. Petersburg
Petersburg
Sign up for an appointment
Moiseeva Tatyana Sergeevna
Pediatrician, infectious disease specialist
Cutting infections Early or late, almost every person. After acute respiratory viral infections (ARVI and influenza), this is the most common reason for visiting a doctor in childhood. They are a problem not only for the child, but for the whole family. Perhaps the most common intestinal infection at the moment is rotavirus or, as its parents often call it, "intestinal flu." nine0003
Regardless of the social status of the family and the sanitary and hygienic situation in the house, from birth to 5 years, almost all children suffer from rotavirus gastroenteritis . According to statistics, more than 137 million people worldwide carry this infection every year, about a quarter of whom are hospitalized. Unfortunately, there are cases with a fatal outcome, including in children. Rotavirus gastroenteritis is most severe in children when they first encounter the virus, which usually occurs between the ages of 6 and 18 months. In formula-fed babies, the risk of infection and a more severe course is slightly higher. nine0003
Unfortunately, there are cases with a fatal outcome, including in children. Rotavirus gastroenteritis is most severe in children when they first encounter the virus, which usually occurs between the ages of 6 and 18 months. In formula-fed babies, the risk of infection and a more severe course is slightly higher. nine0003
Adults are also susceptible to this infection. During life, you can become infected repeatedly, since natural immunity to the virus is type-specific (protects only against a specific type of rotavirus and does not protect against others). With repeated exposure to the virus, as a rule, the disease is less pronounced, but the person is contagious and can spread the infection.
So, what is rotavirus? There is an opinion that the rotavirus got its name because it enters the human body through the mouth, this is not true, the virus is called that because it looks like a wheel in its structure (from lat. - rota), hence the name. There are several types that differ slightly from each other in structure, but cause the same clinical picture of the disease. nine0003
nine0003
The route of transmission of this infection is fecal-oral, that is, to put it simply, it is a “disease of dirty hands”. The virus is highly contagious, only 10 particles of the virus are enough to get sick. Rotavirus persists for a long time on any surface, even with thorough cleaning. Therefore, very often this infection affects several family members at the same time, including adults, there are outbreaks in children's groups. It is worth noting that you can get infected only from a sick person, pets do not get sick with “human” rotaviruses. nine0003
The incubation period for rotavirus infection ranges from several hours to 5-7 days. It is characterized by general malaise, weakness, refusal to eat, fever and symptoms of damage to the gastrointestinal tract (frequent watery loose stools, vomiting, abdominal pain). At the first sign of illness, seek medical attention! After examining the child, the doctor will assess his condition, the need for hospitalization, prescribe an examination and treatment. nine0003
nine0003
To diagnose infection, stool testing for rotavirus by PCR (polymerase chain reaction) and ELISA (enzymatic immunoassay) is used, the result is usually ready in 1-2 days. But treatment must be started at the first symptoms of the disease, without waiting for the results. Therapy is carried out according to the symptoms, and practically does not depend on the results of the tests. Tests are prescribed to make sure that it is a rotavirus infection and in case of complications, so that doctors understand what exactly they are dealing with. nine0003
For the treatment of children who do not need hospitalization and stay at home under the supervision of a pediatrician, the so-called pathogenetic therapy is used, aimed at compensating for fluid losses that the child loses during illness with loose stools and vomit.
The most important rule for a mother with rotavirus is to solder the child, several sips every 5-10 minutes. If the child refuses, then drink it from a spoon or from a syringe (after removing the needle). Do not let your child drink large amounts of liquid at one time, even if he is very thirsty, as this may cause him to vomit. It is necessary to be patient and constantly, despite the protests, drink-drink-drink. It is soldering that helps to avoid dehydration and hospitalization. nine0003
If the child refuses, then drink it from a spoon or from a syringe (after removing the needle). Do not let your child drink large amounts of liquid at one time, even if he is very thirsty, as this may cause him to vomit. It is necessary to be patient and constantly, despite the protests, drink-drink-drink. It is soldering that helps to avoid dehydration and hospitalization. nine0003
In addition to water, special saline solutions from a pharmacy are used to solder a child, containing salts that are lost by the body during illness (Hydrovit, Humana, Electrolyte, Gastrolit, Regidron, etc.). In the absence of special preparations, until the moment of their purchase, you can use a home-made solution. You can prepare it by taking a liter of boiled water, adding 1-2 tablespoons of sugar (without a slide), half a teaspoon of table salt and one third of a teaspoon of baking soda. The finished solution can be stored for no more than a day. It is impossible to solder children with milk, juices, fruit drinks, vegetable broths, carbonated drinks. nine0003
nine0003
The second important component of the treatment of rotavirus infection is diet therapy . For the duration of an acute illness and 2-3 weeks after it, the child is prescribed a sparing diet, with the exception of dairy products, juices, raw fruits and vegetables. The child should eat more often than usual, in small portions. Food should be as gentle as possible for the stomach - not spicy, not greasy, not hot, not fried.
For infants who are breastfed or artificially fed, the issue of further feeding is decided on an individual basis with a pediatrician. With continued frequent liquid stools, in artificially fed children, a temporary transition to a mixture with a low lactose content (lactose-free, low-lactose, etc.) is possible. In infants, the issue of partial replacement of breast milk with a mixture with a low lactose content or the addition of special enzymes to breast milk that help milk to be absorbed in the intestines of the child (lactase enzyme preparations) is being resolved. nine0003
nine0003
Also used in therapy are such groups of drugs as: enterosorbents (Smecta, Filtrum-sti, Enterosgel, etc.), probiotics (Enterol, Linex, Bifiform, Acipol, etc.), prebiotics (Hilak-forte, Duphalac et al), enzymes (Creon 10000, Mezim-forte, Pancreatin). You should not give these drugs to your child on your own, you need to consult a doctor, as you need to understand the advisability of taking them at different periods of the disease.
Antiviral and immunomodulatory therapy may be administered if indicated . The decision to prescribe drugs in this group is made only by a doctor.
antibiotic therapy is worth mentioning separately. Antibacterial therapy for uncomplicated rotavirus infection is not carried out. But in some cases, doctors still prescribe antibiotics. And it's not just habit. This is due to the fact that acute intestinal infections are not only viral, but also bacterial in nature (E. coli, Salmonella, Yersinia, and some more). And it is not always possible to determine with 100% accuracy by the symptoms what caused the symptoms: a viral infection, a toxic infection or a bacterial one. There are also mixed causes and an atypical course of the disease, so the question of prescribing antibacterial drugs is at the discretion of the attending physician. nine0003
coli, Salmonella, Yersinia, and some more). And it is not always possible to determine with 100% accuracy by the symptoms what caused the symptoms: a viral infection, a toxic infection or a bacterial one. There are also mixed causes and an atypical course of the disease, so the question of prescribing antibacterial drugs is at the discretion of the attending physician. nine0003
Very important! If the soldering of the child turned out to be ineffective and the child continues to vomit, weakness increases, he urinates less than usual (the interval is 3-4 hours), then there are direct indications for the hospitalization of the baby in a hospital, where he will be prescribed infusion therapy (intravenous fluid).
Now there is a unique opportunity to protect your baby from rotavirus infection. The Rotatek® vaccine has been certified in Russia and has been successfully used abroad for several years. The vaccine protects against the five most common types of rotavirus and prevents severe forms of the other types of the virus.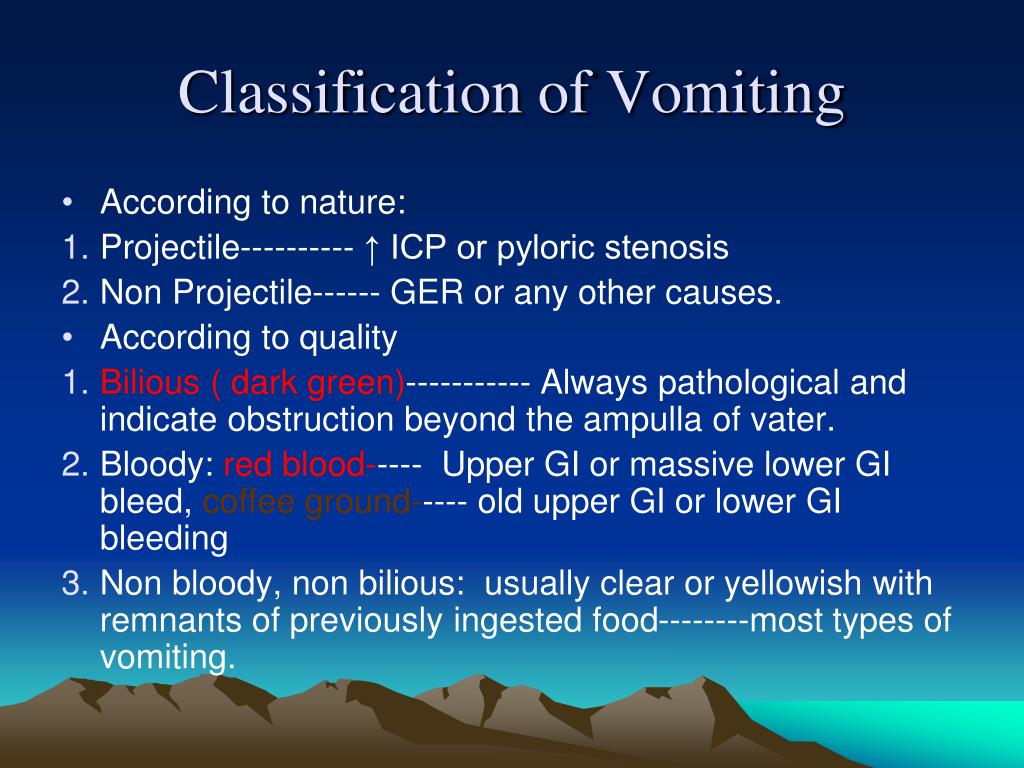 For a full course of vaccination, 3 vaccines must be administered, the convenience of using the vaccine lies in the fact that it is presented in the form of drops for oral administration, and not in the form of a syringe for intramuscular injections. First dose of vaccine at 6-12 weeks of age, then 2 more at least 4 weeks apart. Revaccinations, that is, repeated injections of the vaccine after a full course of vaccination of 3 stages, are not required. nine0003
For a full course of vaccination, 3 vaccines must be administered, the convenience of using the vaccine lies in the fact that it is presented in the form of drops for oral administration, and not in the form of a syringe for intramuscular injections. First dose of vaccine at 6-12 weeks of age, then 2 more at least 4 weeks apart. Revaccinations, that is, repeated injections of the vaccine after a full course of vaccination of 3 stages, are not required. nine0003
The vaccine is intended for children 6 weeks to 32 weeks , not for adults. This is due to the fact that the first encounter with the virus and the most severe course of the disease occurs during this period. In the future, after the immune system has "acquainted" with the virus, the likelihood of developing a serious illness decreases and immunoprophylaxis with a vaccine is no longer so relevant.
Request a call from the call center
Thank you, your request has been accepted and is being processed
Thank you for contacting us!
Our specialist will contact you during the day to clarify the details and make an appointment. Please keep in touch. If you feel uncomfortable waiting or need an urgent appointment, please call 8 812 380 02 38.
Please keep in touch. If you feel uncomfortable waiting or need an urgent appointment, please call 8 812 380 02 38.
Error message
Thank you for helping to make our site better!
Acute intestinal infections in babies
The baby fell ill suddenly: body temperature increased, vomiting appeared. The chair became frequent, liquid, plentiful, watery. It contained inclusions of undigested food, sometimes an admixture of mucus, greenery, less often - streaks or an admixture of blood. All bases to assume, what is it an intestinal infection. nine0003
Due to repeated vomiting and frequent liquid stools in young children, severe, life-threatening dehydration can occur as early as 6-8 hours. And a high temperature, sometimes rising to 40-41 0 , can "lead" convulsions.
Call a doctor immediately and start acting energetically without missing a beat: in such a situation, you yourself must become an "ambulance"! Now it doesn’t matter what has overtaken the baby: dysentery, salmonellosis, rotavirus or other intestinal infection (more than 40 pathogens are known) - all of them at first manifest themselves very similarly, and first aid, both with high body temperature and with dehydration of the body as a result of vomiting and frequent loose stools are the same. nine0003
nine0003
To prevent dehydration of the baby's body, from the first hours, start giving the child boiled water - "drink" him. But since not only water is lost with loose stools and vomit, but also salts of sodium, potassium, chlorine and other electrolytes, which are essential for the normal functioning of the heart, kidneys, brain and other organs, water alone is not enough, saline solutions are required.
For more than 30 years all over the world for oral rehydration (compensation of pathological losses of water and electrolytes through the mouth - "drinking" in case of intestinal infections) glucose-salt solutions specially developed by WHO have been used. In our country, Regidron, which is produced in powders and freely sold in pharmacies, has been widely used both in hospitals and in the treatment of intestinal infections at home. Before use, the contents of the sachet are diluted in a liter of warm boiled water and given to the child to drink. The drug effectively compensates for the existing losses of water and electrolytes, prevents further dehydration of the child's body and aggravation of his condition, but does not have a pronounced therapeutic effect. nine0003
nine0003
In recent years, in accordance with the recommendations of the European Society for Pediatric Gastroenterology and Nutrition (ESPGAN), for better absorption of water and electrolytes in the intestine, the electrolyte composition of solutions has been slightly changed, namely, their osmolarity and sodium-glucose ratio have been reduced. In many pharmacies, the Gastrolit glucose-saline solution, which meets the new standard, has already appeared on sale. Unlike rehydron, gastrolith also contains chamomile extract, which additionally has an anti-inflammatory, antiseptic and antispasmodic effect on the intestines, that is, "Gastrolit" also has a therapeutic effect. nine0003
Which glucose-saline solution is best for drinking ?
There are no significant differences in their effectiveness, but when a child is "drinked" with a solution of "Gastrolit", abdominal pain, vomiting, flatulence phenomena (bloating, rumbling, etc.) disappear 1-2 days faster, the frequency and watery nature of the stool decrease . Before use, the content of 1 sachet of gastrolith is diluted in 200 ml of necessarily hot boiled water to obtain chamomile infusion and cooled to room temperature. nine0003
Before use, the content of 1 sachet of gastrolith is diluted in 200 ml of necessarily hot boiled water to obtain chamomile infusion and cooled to room temperature. nine0003
If these solutions are not available at home, prepare a decoction - for 1 liter of water, either 100 g of raisins or 500 g of carrots (cut into pieces and boil). Add a teaspoon of table salt (without top), ½ teaspoon of baking soda, 4 teaspoons of granulated sugar to it, bring to a boil and cool - the “homemade rehydron” is ready. It is even easier to prepare a sugar-salt solution - for 1 liter of boiled water you need a teaspoon of salt, ½ teaspoon of baking soda and 8 teaspoons of granulated sugar. nine0003
When "drinking" an infant with these solutions, drink from a spoon every 5-7-10 minutes. But little by little! For example, 1-3 teaspoons or 2-3 "sips" through the nipple. It is impossible to give a lot of liquid at once, even if he drinks with greed - this can provoke a new attack of vomiting. For a child 2-3 years old and older, a single dose of solutions can be increased to 2-3 tablespoons, and intervals - up to 10-15 minutes.
For a child 2-3 years old and older, a single dose of solutions can be increased to 2-3 tablespoons, and intervals - up to 10-15 minutes.
What is the total volume of fluid needed to compensate for the pathological loss of water and electrolytes with stool and vomiting ?
WHO experts recommend that in the presence of vomiting and "watery" stools, a young child loses about 10 ml per 1 kg of body weight for each bowel movement. For example, a child weighing 10 kg with each liquid stool will lose 100 ml of liquid, which must be “drinked” between bowel movements and feeding the child. To avoid dehydration, the child should receive a total of about as much fluid per day, including nutrition, as a healthy baby of the same age needs, plus the amount lost with vomiting and loose stools. If he eats less than he should (and during illness this is almost inevitable), then the missing amount of food must be compensated by liquid. nine0003
When gastrolith is used, the solution must not be sweetened and can only be “drained” with gastrolith alone. Age dosages of the required volume of the prepared gastrolith solution for children are detailed in the attached instructions. While the solution of rehydron should be only half the required daily amount of liquid. In this case, the intake of rehydron should be alternated with the intake of the same volume, either weakly brewed unsweetened tea, or boiled water or 5% glucose solution, which can be bought at a pharmacy. nine0003
Age dosages of the required volume of the prepared gastrolith solution for children are detailed in the attached instructions. While the solution of rehydron should be only half the required daily amount of liquid. In this case, the intake of rehydron should be alternated with the intake of the same volume, either weakly brewed unsweetened tea, or boiled water or 5% glucose solution, which can be bought at a pharmacy. nine0003
It is widely believed that a solution of potassium permanganate (potassium permanganate) helps to stop vomiting and diarrhea. I often give it to drink, make enemas with it. Vomiting and diarrhea in most cases really stop, but only for a few hours. Moreover, the chair is absent from the fact that under the influence of potassium permanganate, a fecal plug is often formed, which prevents the exit of intestinal contents. And it's far from safe! With loose stools, the body is freed from a huge amount of pathogenic microbes and viruses, pathogens of intestinal infections, their toxins, gases and other toxic substances formed in the intestines as a result of inflammatory or fermentation processes. With a fecal plug, all of them, lingering in the intestines, begin to be absorbed into the blood, and the child’s condition worsens sharply after a few hours of “relative” well-being - bloating, shortness of breath and uncontrollable vomiting appear. In such cases, immediate hospitalization is required. nine0003
With a fecal plug, all of them, lingering in the intestines, begin to be absorbed into the blood, and the child’s condition worsens sharply after a few hours of “relative” well-being - bloating, shortness of breath and uncontrollable vomiting appear. In such cases, immediate hospitalization is required. nine0003
There are even worse situations with potassium permanganate. A sick baby is given a concentrated solution, believing that it will work more efficiently or a solution containing undissolved crystals. And the ending is tragic: burns of the mucosa of the gastrointestinal tract, intestinal bleeding, intestinal perforation with the development of peritonitis, requiring urgent surgical intervention, and even the death of a child.
Please do not give potassium permanganate by mouth to children under any circumstances !
Vomiting and diarrhea in intestinal infections are initially protective in nature - the body tries to "throw out" microbes and toxic products with vomit and frequent loose stools. It is more expedient to help the body in this - to wash the stomach and even make a cleansing enema. At home, let the child drink as much boiled water as possible and the vomiting that has begun will “wash out” microbes and toxins from the stomach. If it is not there, call it yourself by pressing on the root of the tongue with the handle of a clean spoon, in extreme cases, with a finger wrapped in a sterile gauze or bandage. This should be repeated 2-3 times, and then let the child drink an enterosorbent (smecta, filtrum, enterosgel, etc.), strictly observing the age dosages indicated in the instructions. Enterosorbents "bind" microbes, viruses and their poisons in the gastrointestinal tract, then remove them with feces, which greatly facilitates the course of the disease, quickly reduces the frequency and improves the consistency of the stool. It is not rational to use activated carbon for this purpose - its effectiveness in normal dosages is very low. nine0003
It is more expedient to help the body in this - to wash the stomach and even make a cleansing enema. At home, let the child drink as much boiled water as possible and the vomiting that has begun will “wash out” microbes and toxins from the stomach. If it is not there, call it yourself by pressing on the root of the tongue with the handle of a clean spoon, in extreme cases, with a finger wrapped in a sterile gauze or bandage. This should be repeated 2-3 times, and then let the child drink an enterosorbent (smecta, filtrum, enterosgel, etc.), strictly observing the age dosages indicated in the instructions. Enterosorbents "bind" microbes, viruses and their poisons in the gastrointestinal tract, then remove them with feces, which greatly facilitates the course of the disease, quickly reduces the frequency and improves the consistency of the stool. It is not rational to use activated carbon for this purpose - its effectiveness in normal dosages is very low. nine0003
After gastric lavage and enterosorbent intake, vomiting in intestinal infections usually stops. If this does not happen, then vomiting and diarrhea, especially in infants, may be one of the manifestations of diseases such as appendicitis, influenza, otitis media, pneumonia, meningitis, etc. In these cases, it is necessary to call a doctor at home or an ambulance » for the hospitalization of the child in the appropriate hospital. It is better to stop therapeutic measures before the doctor arrives, with the exception of antipyretics, and the volume of liquid for “drinking” should not exceed pathological losses with loose stools. nine0003
If this does not happen, then vomiting and diarrhea, especially in infants, may be one of the manifestations of diseases such as appendicitis, influenza, otitis media, pneumonia, meningitis, etc. In these cases, it is necessary to call a doctor at home or an ambulance » for the hospitalization of the child in the appropriate hospital. It is better to stop therapeutic measures before the doctor arrives, with the exception of antipyretics, and the volume of liquid for “drinking” should not exceed pathological losses with loose stools. nine0003
To feed or not to feed ?
The general rule is this: it is necessary to give food, reducing the daily amount of food, but not more than half. However, it all depends on the frequency of vomiting and the condition of the child, and this is what you need to focus on. Ideal: feed "according to appetite", but more often and in small portions, so as not to overfill the stomach and not provoke vomiting. If the baby is breastfed, continue breastfeeding. But with frequent vomiting (or regurgitation), it is better to switch to “metered” feeding with expressed breast milk in small portions at regular intervals (after 2-2.5-3 hours with a night break). A baby who is bottle-fed, as well as a 2-3-year-old child and older, on the first day of the disease can be fed with normal food (kefir, cottage cheese, adapted infant formula, cereals with half milk, etc.), but preference should be given to medical - prophylactic food products enriched with bifido- or lactobacilli (children's kefir "Bifidok", mixture "Agusha", acidophilic mixture "Baby", "Kroshechka", etc.). nine0003
But with frequent vomiting (or regurgitation), it is better to switch to “metered” feeding with expressed breast milk in small portions at regular intervals (after 2-2.5-3 hours with a night break). A baby who is bottle-fed, as well as a 2-3-year-old child and older, on the first day of the disease can be fed with normal food (kefir, cottage cheese, adapted infant formula, cereals with half milk, etc.), but preference should be given to medical - prophylactic food products enriched with bifido- or lactobacilli (children's kefir "Bifidok", mixture "Agusha", acidophilic mixture "Baby", "Kroshechka", etc.). nine0003
In case of a pronounced fermentation process (increased gas formation, bloating and rumbling in the abdomen, foamy stools, etc.), it is better to replace the child’s usual food for several days with commercially available and age-adapted low-lactose or lactose-free baby foods. It is also recommended to introduce cereals on water or vegetable broths into the diet, an earlier appointment of meat gosha is shown.
Older children in the acute period of intestinal infection should be completely excluded from the diet of foods that cause fermentation in the intestines and increased gas formation, containing coarse fiber: whole milk and cereals with whole milk, fermented baked milk, cream, black bread, meat, chicken and fish broths, dishes from beans, peas, beets, cabbage, grapes, citrus fruits, as well as all fatty, fried, canned food (except canned food for baby food), limit sweets. Carbonated drinks (fanta, etc.) are also prohibited. nine0003
Emergency treatment for high body temperature.
The temperature is not higher than 38 0 (if the child tolerates it well and provided that such rises were not accompanied by convulsions before), you can not “knock down”. But if the mercury column rises above 38-38.5 0 or the so-called "convulsive readiness" appears - trembling of the fingertips and chin, proceed to intense antipyretic measures.
Attention! If the hands and feet are hot , like the rest of the body - start with physical methods of cooling. Undress the baby and fan it vigorously (option: put a fan nearby). Put a napkin moistened with cold water and wrung out on your forehead, and plastic bags with ice or bottles of cold water wrapped in a thin cloth in the armpits and inguinal cavities. Let's drink cool water or a glucose-salt solution (rehydron or gastrolith) as often as possible.
Undress the baby and fan it vigorously (option: put a fan nearby). Put a napkin moistened with cold water and wrung out on your forehead, and plastic bags with ice or bottles of cold water wrapped in a thin cloth in the armpits and inguinal cavities. Let's drink cool water or a glucose-salt solution (rehydron or gastrolith) as often as possible.
If the temperature has risen to 40 0 and above, wiping the body with 3% vinegar or a special mixture is required: equal amounts of water, table vinegar (not essence) and alcohol. Pour the prepared mixture into the palm of your hand and rub the baby’s chest, stomach, back, arms and legs quite intensively, but very carefully - everything except the face. It is very useful to wear stockings or socks moistened with this liquid.
The temperature should drop after 10-15 minutes. If there is no effect, give the child antipyretics: children's panadol, efferalgan, etc. As soon as the temperature drops to at least 38 0 , stop physical cooling. If after some time it rises again, then repeat the cooling measures until the doctor or ambulance arrives.
If after some time it rises again, then repeat the cooling measures until the doctor or ambulance arrives.
Attention! If the hands and feet are cold - doctors call this condition “white hyperthermia”: it indicates a violation of heat transfer due to spasm (contraction) of skin vessels and then physical methods of cooling are contraindicated! They can increase the spasm, the heat transfer will decrease, the temperature will rise even more and the child's condition will worsen before our eyes. You can only gently rub the body with a water-vinegar-alcohol mixture, if possible, to a slight reddening - this procedure expands the blood vessels of the skin and heat transfer increases. nine0003
The main thing to reduce the temperature in such cases is antipyretics for children, as well as vasodilators - papaverine, dibazol, etc.
If convulsive readiness or convulsions appear, in addition to antipyretics, give the child any of the antihistamines: pipolfen (it also has an antiemetic effect), suprastin, etc. But this is not enough. If there are convulsions, you can’t hesitate and wait for the local pediatrician - call an ambulance! nine0003
But this is not enough. If there are convulsions, you can’t hesitate and wait for the local pediatrician - call an ambulance! nine0003
Open a window for fresh air - oxygen is vital for a child;
Don't leave your baby alone, he might fall out of bed. If he is lying on his back, turn his head to one side so that he does not choke on vomit. Even better, the position on his side - this will facilitate their discharge;
Wipe your mouth with a damp gauze pad around your finger to remove vomit and mucus;
· Be careful not to sink the tongue - this threatens to suffocate; nine0003
Try not to pick it up so as not to cause pain, but hold it upright when you pick it up.
As the temperature decreases, convulsions usually disappear.
And finally, one more recommendation-caution: all medicines should be only in the age dose. Grind the tablets, dilute in boiled water and give from a spoon. No other drugs (especially antibiotics) - without a doctor's prescription! Do not rush to give enzyme preparations, especially proteolytic (abomin, etc. ) and pancreatin with bovine bile components (festal, etc.) - they can only increase diarrhea, especially with intestinal infections of viral etiology, which in young children are up to 70 -80% of the total. The appointment of antibiotics or other antibacterial drugs (furazolidone, etc.) in these cases only aggravates the course of the disease and contributes to the development of dysbacteriosis. nine0003
) and pancreatin with bovine bile components (festal, etc.) - they can only increase diarrhea, especially with intestinal infections of viral etiology, which in young children are up to 70 -80% of the total. The appointment of antibiotics or other antibacterial drugs (furazolidone, etc.) in these cases only aggravates the course of the disease and contributes to the development of dysbacteriosis. nine0003
Acute intestinal infections, except for severe forms, can be treated at home. The main directions of treatment tactics and during the hospitalization of the child are the same: a rational diet, "drinking", enzyme preparations (pancreatin, mezim forte, etc.), symptomatic therapy (antiemetic, antipyretic, analgesic drugs, etc.). In severe dehydration, a drip is prescribed.
In recent years, highly effective methods have been developed for the treatment of intestinal infections without antibiotics, including severe forms, using probiotics, enterosorbents, and specific immunoglobulin preparations.