Baby hip click are normal
When to Worry About Your Child’s Hip Click
When to Worry About Your Child’s Hip Click | Health Hive Bone and Joint Sometimes parents notice a clicking or popping sound with the movement of their baby’s legs. We spoke to a pediatric orthopaedic surgeon for advice on what to do if this is the case.Jan. 27, 2022 • 4 min read
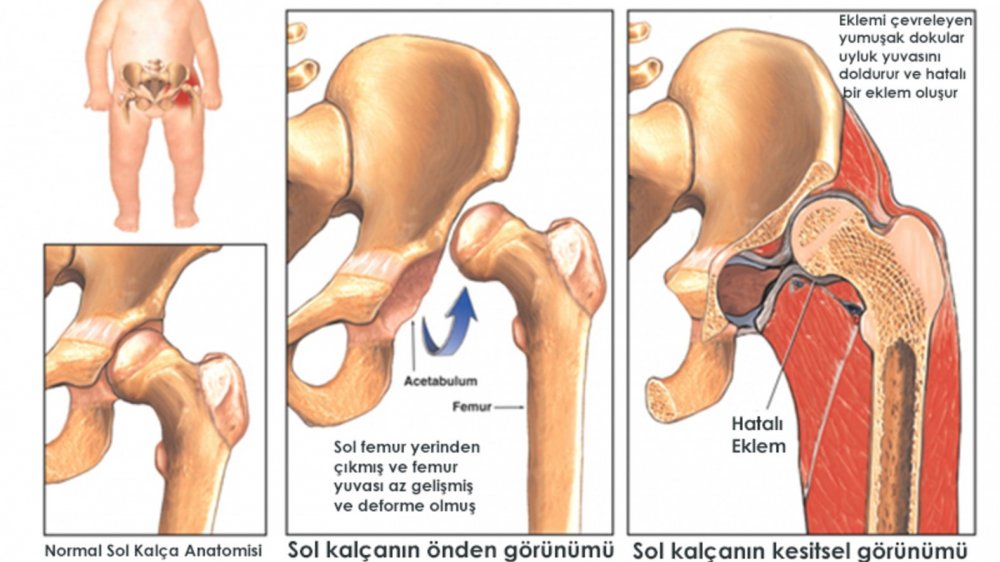
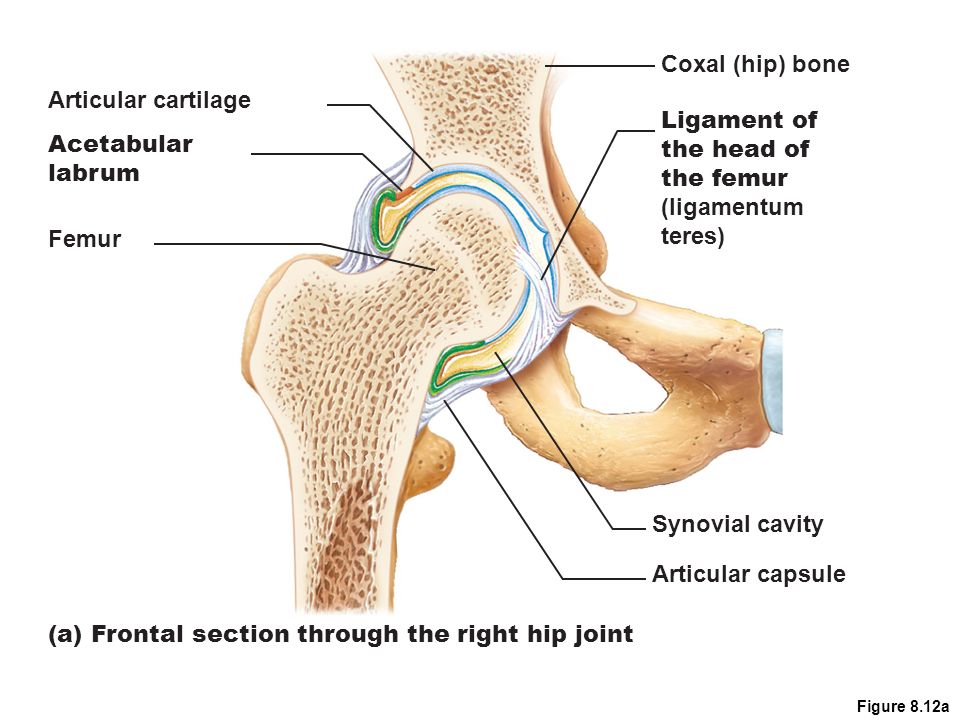
The hip is a ball-and-socket joint, meaning that the femoral head (the top of the femur) is shaped like a ball and sits within the cup-like socket in the pelvis. In some cases, parents may notice abnormalities when an infant or young child’s legs are moved, such as a clicking sound or the feeling of looseness or displacement of the hip.
James Engels, MD, a pediatric orthopaedic surgeon with Rochester Regional Health, advises parents on what to do if their child has a hip click and provides need-to-know information on hip dysplasia.
What is a hip click?
A “hip click” refers to an audible clicking or popping sound that occurs when a baby’s hips are being examined or moved around. Most clicks are not problematic.
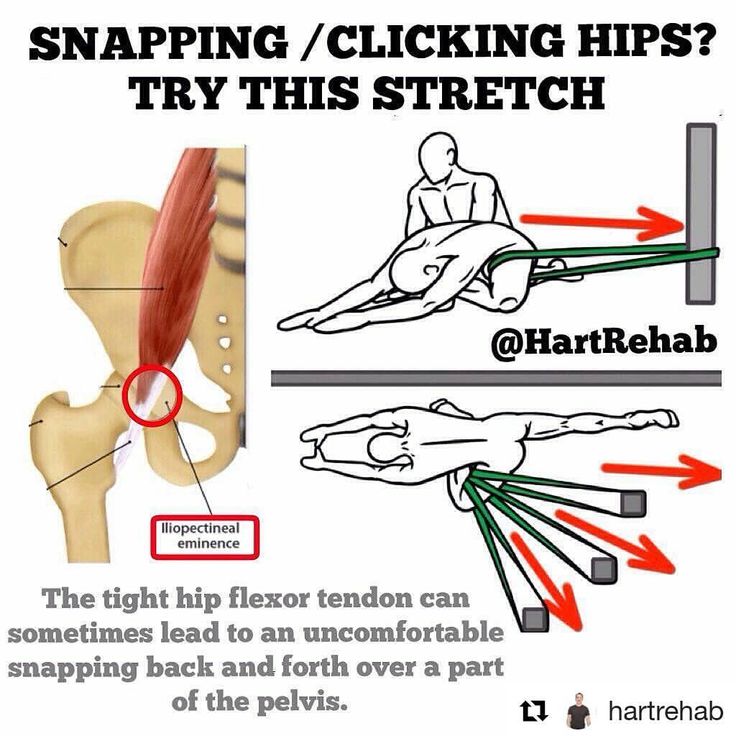
There are tendons or ligaments associated with an infant’s hip joint that can make a snapping or popping sound for a variety of reasons. A hip click could be a sign of abnormalities in hip development, but further examination and possible testing are required to reach a diagnosis. More importantly, instability or displacement of the hip is a significant concern for hip dysplasia.
“A child that has a hip click or hip instability should be monitored for hip dysplasia or other developmental abnormalities. This is something that is usually caught early on by physicians during well-child visits. ”
”
Should my newborn receive a hip exam?
After a child is born at the hospital, pediatric specialists perform a newborn examination. During this thorough physical exam, a specialist will check the baby's hips and legs for abnormalities to assess for hip dysplasia. They do this by gently pushing and pulling the baby’s thigh bones to see how they move in the hip socket.
“If we notice an abnormality in a newborn’s hips, we may order an ultrasound to get a more in-depth look. Once we perform further examinations and testing, we can determine the best way to treat the problem,” said Dr. Engels.
Are there risk factors for hip dysplasia?Some factors may lead to a greater likelihood that a child will have hip dysplasia, such as:
- if a primary relative of the child had hip dysplasia (a parent or sibling)
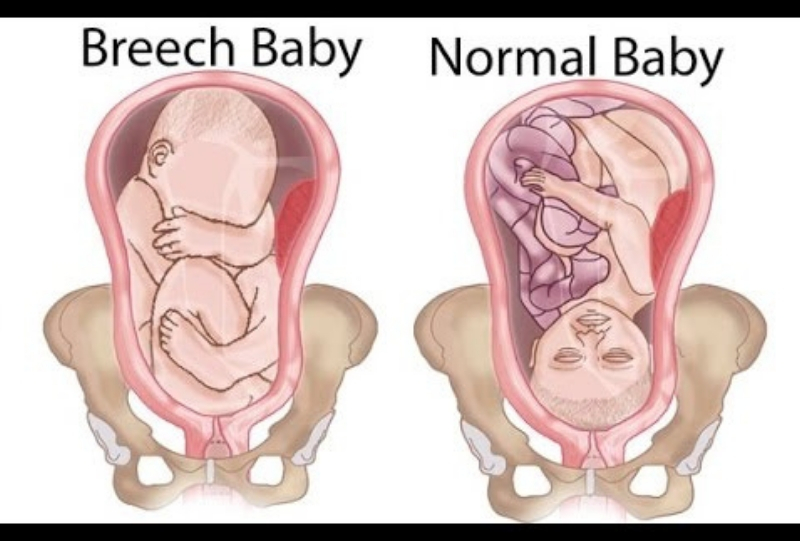
- if there was an extended breech position while the baby was in the womb
- a specialist detects laxity during the newborn hip screening exam
If any of the above are present, the patient should receive further testing to check for hip dysplasia.
Should my child see a doctor for their hip click?
Parents may notice clicking or popping sounds when their child walks or moves their hips or legs. In this case, they should schedule an appointment with their child’s pediatrician for an examination. After the exam, the pediatrician can determine whether further evaluation from a pediatric orthopaedic surgeon is necessary.
Children should have routine well-child visits from the moment they are born up through age 21. For children under 2, these exams occur 2-3 months. At these early visits, a physician will check their hips and legs for signs of hip dysplasia or other abnormalities.
If there is no detection of hip dysplasia or other abnormalities and your child is experiencing a hip click after three or more years of age, schedule an exam with their pediatrician to check for any undetected orthopaedic abnormalities.
“Abnormalities or signs of problems in the hip joints can often be identified at the child’s routine well-exams, especially during the first few years of life.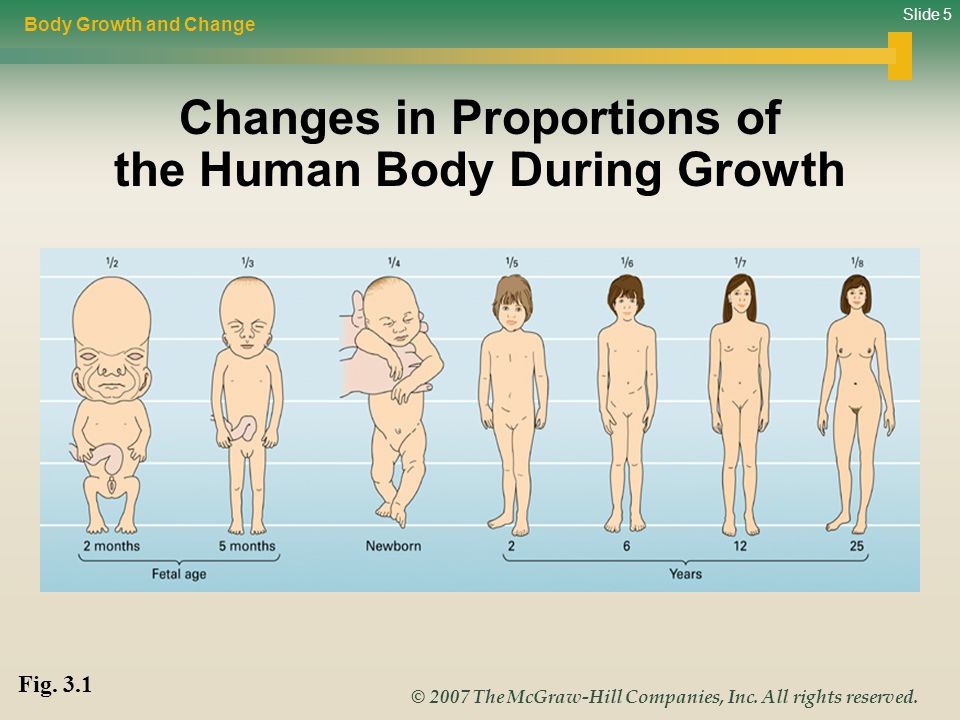 However, if a parent notices clicking, popping, abnormal walking pattern, they should schedule an additional exam with their pediatrician.”
However, if a parent notices clicking, popping, abnormal walking pattern, they should schedule an additional exam with their pediatrician.”
What is hip dysplasia?
Hip dysplasia is a condition in which the hip socket does not fully cover the ball of the upper thighbone, allowing the hip joint to become partially or completely dislocated.
Hip dysplasia can damage the cartilage lining in the hip joint, and in some cases, can lead to loss of the soft cartilage that lines the socket portion of the hip joint, resulting in a painful arthritic hip. That’s why early detection and treatment of hip dysplasia is so important.
Hip dysplasia symptoms
Signs and symptoms of hip dysplasia vary based on age and severity. A hip click may be a sign of hip dysplasia, but it does not guarantee the condition.
Symptoms of hip dysplasia may include:
- Pain in the hip
- Loose or unstable hip joint
- Limping or abnormal walking patterns
- Unequal leg lengths
- Loss of motion
“Many of the signs of hip dysplasia go unnoticed in everyday life, which is why it’s so important for infants to have routine well-child exams that include hip screen examination right from the moment they’re born. This way, we are more likely to detect any abnormalities early on and begin treatment as needed,” said Dr. Engels.
This way, we are more likely to detect any abnormalities early on and begin treatment as needed,” said Dr. Engels.
Hip dysplasia treatments
Pavlik harness
The most common treatment for hip dysplasia in infants is a Pavlik harness. The Pavlik harness is a soft splint that helps keep the infant’s hips and knees bent and the thighs apart. An infant treated with a Pavlik harness stays in the harness at all times of day and night.
In most cases, the infant will wear the harness for 3-4 months and will be monitored as they grow.
“The Pavlik harness is very comfortable for baby. It’s soft and easy to clean. Most importantly, it is extremely effective in treating and curing hip dysplasia,” said Dr. Engels.
Semi-rigid orthosis
If an infant’s hips do not stabilize with the Pavlik harness, or if hip dysplasia is diagnosed later than 6-8 months of age, an orthopaedic physician may prescribe a semi-rigid orthosis.
Instead of a harness, this is more like a brace that keeps the infant’s legs and hips in a more stable and secure position.
Surgery
In severe cases, an infant may need surgery to correct the development of their hips. There are two types of surgical options: closed reduction surgery and open reduction surgery.
Closed reduction surgery occurs under general anesthesia and the infant's hip is placed back into the socket. To help with this process, a tendon in the groin is usually lengthened through a small incision. The infant is then put into a body cast, bracing the pelvis area to hold their hips in position.
In open reduction surgery, under general anesthesia, an incision is made to put the hip back into place. This option is for severe cases in which bones may also need to be cut to help keep the hip in place.
“After any surgical option, we follow-up with the patient routinely until they’re at least 5-7 years of age. We continue to check on their development to ensure everything is healthy."
NEXT STEPS Personalized Bone & Joint Care
At any age, orthopedic conditions can keep us from the basic tasks that mean so much. Using advanced and proven techniques, and drawing on the resources and talents of our full regional network, our team will provide you with personalized care – and the freedom of a happy, active life.
Using advanced and proven techniques, and drawing on the resources and talents of our full regional network, our team will provide you with personalized care – and the freedom of a happy, active life.
Learn More
Recent ArticlesClicky hip alone is not a true risk factor for developmental dysplasia of the hip
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Atypon
Full text links
Observational Study
. 2017 Nov;99-B(11):1533-1536.
2017 Nov;99-B(11):1533-1536.
doi: 10.1302/0301-620X.99B11.BJJ-2017-0416.R1.
K Nie 1 , S Rymaruk 1 , R W Paton 2
Affiliations
Affiliations
- 1 Royal Blackburn Teaching Hospital, East Lancashire Hospitals NHS Trust, Haslingden Road, Blackburn BB2 3HH, UK.
- 2 University of Central Lancashire (UCLAN), Fylde Road, Preston PR1 2HE, UK.
- PMID: 29092995
- DOI: 10.1302/0301-620X.
 99B11.BJJ-2017-0416.R1
99B11.BJJ-2017-0416.R1
Observational Study
K Nie et al. Bone Joint J. 2017 Nov.
. 2017 Nov;99-B(11):1533-1536.
doi: 10.1302/0301-620X.99B11.BJJ-2017-0416.R1.
Authors
K Nie 1 , S Rymaruk 1 , R W Paton 2
Affiliations
- 1 Royal Blackburn Teaching Hospital, East Lancashire Hospitals NHS Trust, Haslingden Road, Blackburn BB2 3HH, UK.
- 2 University of Central Lancashire (UCLAN), Fylde Road, Preston PR1 2HE, UK.
- PMID: 29092995
- DOI: 10.1302/0301-620X.99B11.BJJ-2017-0416.R1
Abstract
Aims: A clicky hip is a common referral for clinical and sonographic screening for developmental dysplasia of the hip (DDH). There is controversy regarding whether it represents a true risk factor for pathological DDH. Therefore a 20-year prospective, longitudinal, observational study was undertaken to assess the relationship between the presence of a neonatal clicky hip and pathological DDH.
Patients and methods: A total of 362 infants from 1997 to 2016 were referred with clicky hips to our 'one-stop' paediatric hip screening clinic.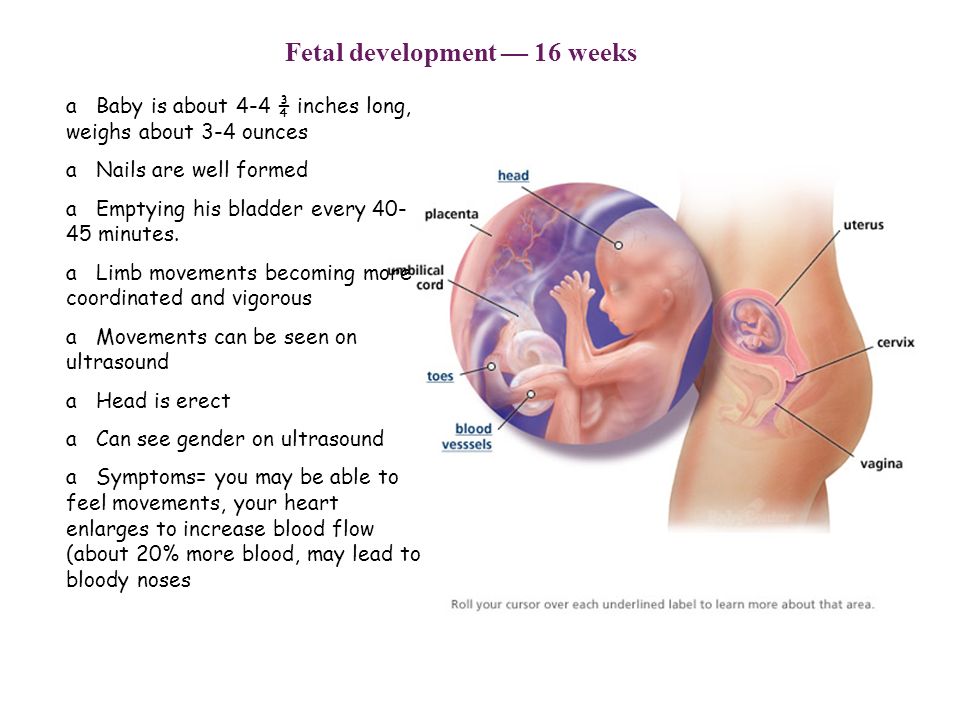 Hips were assessed clinically for instability and by ultrasound imaging using a simplified Graf/Harcke classification. Dislocated or dislocatable hips were classified as Graf Type IV hips.
Hips were assessed clinically for instability and by ultrasound imaging using a simplified Graf/Harcke classification. Dislocated or dislocatable hips were classified as Graf Type IV hips.
Results: The mean age at presentation was 13.8 weeks (12.8 to 14.7). In all 351 out of 362 children (97.0%) had Graf Type I hips (normal) that required no treatment. Nine children (2.5%) had Graf Type II hips but all resolved to Graf Type I hips on follow-up scans. One child (0.3%) had Graf Type III hip dysplasia and one child (0.3%) had an irreducible hip dislocation. The two pathological hips were associated with unilateral limited hip abduction. Mean referrals increased from 12.9 to 23.3 each year (p = 0.002) from the first decade of the study to the second, driven by increasing primary care referrals (5.5 versus 16.7 per year, p < 0.001).
Conclusion: Most clicky hips required no treatment other than reassurance to parents.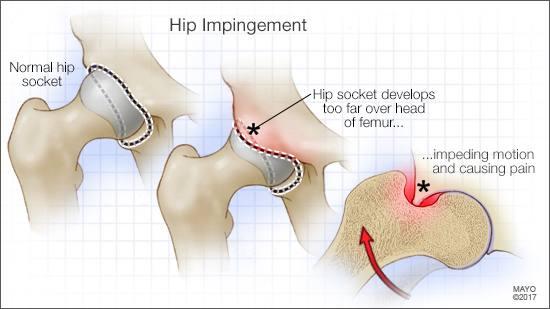 Clicky hips with a normal hip examination should be considered a variant of normal childhood and not a risk factor for DDH. However, an abnormal hip examination including unilateral limited hip abduction should prompt urgent further investigations. Cite this article: Bone Joint J 2017;99-B:1533-6.
Clicky hips with a normal hip examination should be considered a variant of normal childhood and not a risk factor for DDH. However, an abnormal hip examination including unilateral limited hip abduction should prompt urgent further investigations. Cite this article: Bone Joint J 2017;99-B:1533-6.
Keywords: Clicky hip; Developmental dysplasia of the hip; Neonatal hip screening; Ultrasound imaging.
©2017 The British Editorial Society of Bone & Joint Surgery.
Similar articles
-
The 'clicky hip': to refer or not to refer?
Humphry S, Thompson D, Price N, Williams PR. Humphry S, et al. Bone Joint J. 2018 Sep;100-B(9):1249-1252. doi: 10.1302/0301-620X.100B9.BJJ-2018-0184.R1. Bone Joint J. 2018. PMID: 30168765
-
Value of the 'clicky hip' in selective screening for developmental dysplasia of the hip.
Marson BA, Hunter JB, Price KR. Marson BA, et al. Bone Joint J. 2019 Jun;101-B(6):635-638. doi: 10.1302/0301-620X.101B6.BJJ-2018-1238.R3. Bone Joint J. 2019. PMID: 31154832
-
Is 'clicky hip' a risk factor in developmental dysplasia of the hip?
Kamath S, Bramley D. Kamath S, et al. Scott Med J. 2005 May;50(2):56-8. doi: 10.1177/003693300505000205. Scott Med J. 2005. PMID: 15977515
-
Cochrane Review: Screening programmes for developmental dysplasia of the hip in newborn infants.
Shorter D, Hong T, Osborn DA. Shorter D, et al. Evid Based Child Health. 2013 Jan;8(1):11-54. doi: 10.1002/ebch.1891. Evid Based Child Health. 2013. PMID: 23878122 Review.
-
Screening in Developmental Dysplasia of the Hip (DDH).

Paton RW. Paton RW. Surgeon. 2017 Oct;15(5):290-296. doi: 10.1016/j.surge.2017.05.002. Epub 2017 Jun 12. Surgeon. 2017. PMID: 28619546 Review.
See all similar articles
Cited by
-
Examining the Short-Term Natural History of Developmental Dysplasia of the Hip in Infancy: A Systematic Review.
Zomar BO, Mulpuri K, Schaeffer EK. Zomar BO, et al. Indian J Orthop. 2021 Sep 13;55(6):1372-1387. doi: 10.1007/s43465-021-00510-6. eCollection 2020 Dec. Indian J Orthop. 2021. PMID: 34987723 Free PMC article. Review.
-
Effect of acetabular morphological parameters applied in proximal femoral varus osteotomy on the treatment of developmental dysplasia of the hip in children.
Qiu S, Lin H, Xu M, Liu C, Wang H, Cao Q, Liu J. Qiu S, et al. Transl Pediatr. 2021 May;10(5):1361-1368. doi: 10.21037/tp-21-200. Transl Pediatr. 2021. PMID: 34189095 Free PMC article.
Publication types
MeSH terms
Full text links
Atypon
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
Cracking in the joints in adolescents
Cracking in the joints in adolescents.
In adolescence, there is a frequent occurrence when joints crackle in a teenager. Often this is due to uneven growth of bones and internal organs, physical inactivity or, conversely, increased physical exertion. In the absence of pain and discomfort, crunching in the joints goes away thanks to foods rich in vitamins and calcium, moderate sports and a healthy lifestyle.
Why do joints crackle? nine0007 Congenital malformations
During adolescence, some children may present with joint hypermobility accompanied by cracking. This phenomenon is associated with uneven growth of tissues and organs during the transition period. If a person is healthy, the joints work without noise and discomfort. Clicks when moving - a sign of a violation of the structure. In adolescents, the joints crackle for the following reasons:
Hypermobility of the joint
An abnormal congenital structural feature that allows the joint to assume a position that is different from the norm. The reason for this phenomenon is the weakness of the connective tissue. Hypermobility is painless, but when the joint returns to its original position, the teenager hears a crunch. A similar phenomenon acquires the character of a pathology with soreness and frequent dislocations. nine0003
The reason for this phenomenon is the weakness of the connective tissue. Hypermobility is painless, but when the joint returns to its original position, the teenager hears a crunch. A similar phenomenon acquires the character of a pathology with soreness and frequent dislocations. nine0003
Specific structure
Congenital defects of the epiphyses and tendons can cause misalignment of the articular surfaces in a teenager. This is manifested by a crunch and a click - biomechanical disturbances. With small deviations in adolescence, there will be no serious failures: it will be limited to noise and discomfort. But in the future, such a birth defect becomes the cause of diseases of the musculoskeletal system, which are especially pronounced during hard work or physical exertion in training. nine0003
Lifestyle features
Teenagers sit in one position for a long time at school. This leads to an increased load on certain parts of the body - the neck, limbs, etc. Muscles become numb, tense, adjacent joints and cartilage overwork, sometimes even become inflamed. This contributes to the appearance of a crunch, which most often occurs with a sharp change in body position. There will be no particular harm, since the young body quickly restores the condition of cartilage and muscles. But with a tendency to articular diseases, their overload can provoke the development of an undesirable disease. nine0003
This contributes to the appearance of a crunch, which most often occurs with a sharp change in body position. There will be no particular harm, since the young body quickly restores the condition of cartilage and muscles. But with a tendency to articular diseases, their overload can provoke the development of an undesirable disease. nine0003
Result of injury
Tears or fractures can cause inflammation that causes deforming growths. If the bone is curved, the accuracy of the fit is reduced, the bones crunch when walking or running. In adolescents, there is a high probability of restoring the smoothness of the epiphyses, but sometimes the crunch persists after treatment.
How to treat bone crunch in a teenager?
Based on the results of the tests, the doctor decides on the need for treatment. Primary recommendations are often limited to enhanced nutrition rich in calcium and vitamins, as well as drinking plenty of fluids to increase the volume of fluid in the articular junction.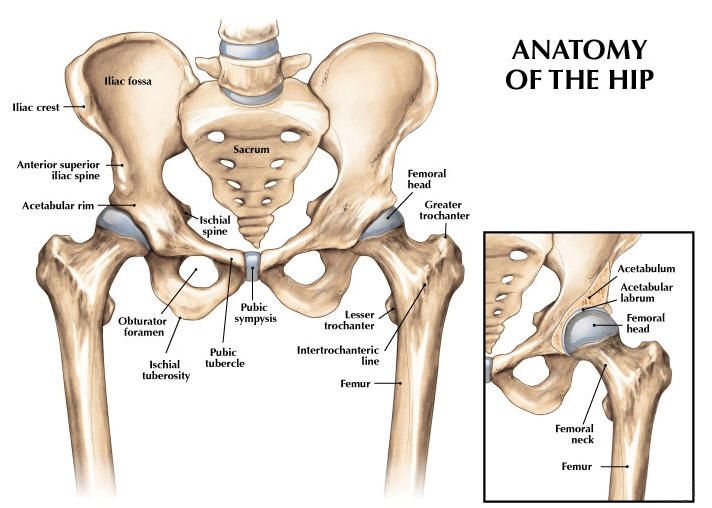 Physiotherapy exercises are useful, but increased loads will have to be postponed for a while. If a teenager complains of pain, it is possible to use medicines prescribed by a doctor. nine0003
Physiotherapy exercises are useful, but increased loads will have to be postponed for a while. If a teenager complains of pain, it is possible to use medicines prescribed by a doctor. nine0003
Snapping hip syndrome: treatment, causes, symptoms
Snapping hip syndrome: treatment, causes, symptomsAbout Portal
AND AND AND
- Diseases
- sports injuries nine0033
- Video
- Good to know
- News nine0033
- I'm worried about
- Preparations
- First aid nine0033
- About the portal
- Contacts
What is it
Main types and causes of occurrence
Symptoms
Examination and diagnosis
Treatment
Exercise
Prognosis
Snapping Hip Syndrome or Coxa Saltans is a condition where a person feels clicks or hears characteristic sounds in the hip joint.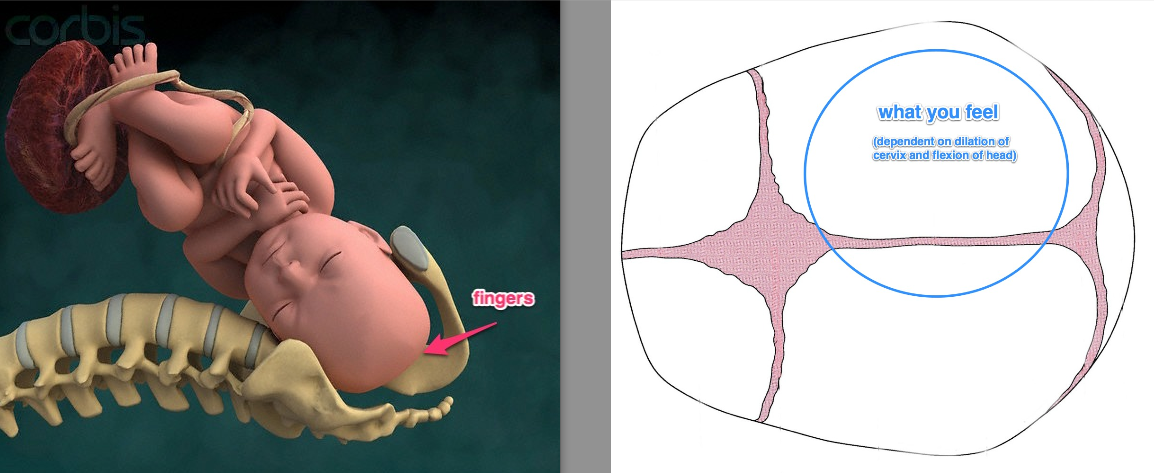 nine0003
nine0003
The syndrome occurs in people involved in professional sports, choreography, gymnastics and other active physical activities. Some patients feel weakness or pain when extending or flexing the hip. Sometimes there is a feeling of dislocation of the hip. This affects activity and the overall quality of life.
The main types and causes of occurrence
External
The cause of pain is constant contact of the ilio-tibial tract with the trochanter. The outdoor type is considered the most common. nine0007 People have clicks when running or climbing stairs. Often there is pain on the outside of the thigh. During the night period, pain intensifies if a person lies on the problem side. Symptoms are most often accompanied by trochanteritis - inflammation of the upper point of the femur.
Special tests
- Aubert's test: the patient lies on his side with the injured thigh up. The upper leg is straight, the lower leg is bent at the knee.
 The doctor bends the upper leg at a right angle. After unbends and abducts the thigh, slowly lowering the limb. If the leg falls below the horizontal line without pain, the test is negative. nine0033
The doctor bends the upper leg at a right angle. After unbends and abducts the thigh, slowly lowering the limb. If the leg falls below the horizontal line without pain, the test is negative. nine0033 - Feeling the area of the greater trochanter during flexion, external and internal rotation of the thigh and checking the condition with circular rotations.
- FABER test: check for clicks during passive hip flexion.
Inner (in front of the thigh)
In this case, the problems are related to the tendon of the muscle. The click occurs when the thigh muscles slide over the protruding bony structures of the joint, or the quadriceps moves over the ball and socket. Symptoms come on gradually, worsen over time: crackling while running, pain in the groin area, when bending the hip. nine0003
Special tests
- Stanchfield test: the person lies on his back, hip flexion 30°. The doctor asks to bend the thigh completely, at the same time resisting it.
 If there is pain in the groin, the test is positive.
If there is pain in the groin, the test is positive. - Thomas test: carried out in the supine position. The patient bends and grasps the knees so that the lower back touches the surface. After lowering one leg, keeping the hip and knee in a bent state. The test result is negative if the lower back does not come off the surface. nine0033
The intra-articular type is caused by impact injuries to the joint. For example, during a fall on a large skewer. The head of the femur strongly collides with the bottom of the acetabulum - as a result, the articular cartilage dies. With this type of syndrome, pain appears during movements: flexion, rotation of the extended hip.
Intra-articular type
Syndrome occurs due to problems inside the joint or cartilage damage. There is a change in the inner part of the capsules: ruptures of the acetabular lip and free joint muscles, osteoarthritis, chondromatosis of the hip joint. nine0003
Main symptoms
The condition is accompanied by a characteristic click in the inner or outer part of the hip joint. In addition to clicking, other symptoms occur.
In addition to clicking, other symptoms occur.
- pain and swelling;
- inflammatory processes;
- weakness in the legs when trying to lift a limb;
- problems with physical activity;
- sensation as if the thigh were failing.
Examination and diagnostics
During the examination, the doctor analyzes the patient's condition, collects an anamnesis: the location of the click, the period of onset of symptoms, the duration of symptoms, the presence of pain, the effect of clicks on physical activity.
The specialist uses a visual analogue scale to measure the intensity of pain. Clinical examination, in addition to palpation, includes special tests. To make an accurate diagnosis, the patient is sent for an ultrasound or MRI. nine0003
Treatment
Most often, snapping hip syndrome does not require intervention to recover.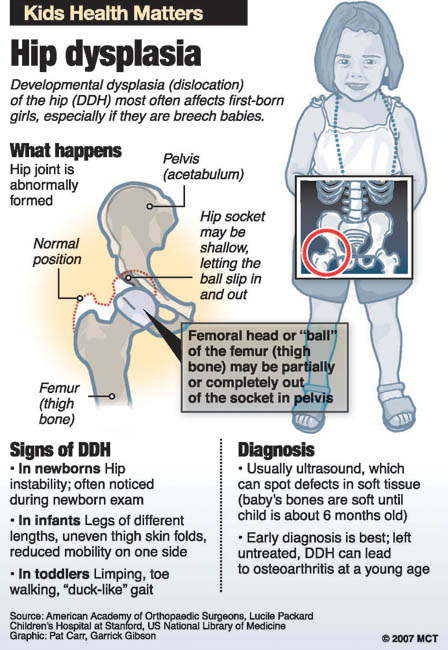 Only when a person is in pain or there are problems in movements, the doctor develops a therapeutic program.
Only when a person is in pain or there are problems in movements, the doctor develops a therapeutic program.
Conservative treatment and physiotherapy
Therapy is based on the exclusion of movements that cause unpleasant symptoms and on simple methods: taking anti-inflammatory drugs, rest, pain injections. For example, the Elox-SOLOpharm drug has analgesic, anti-inflammatory and antipyretic effects: it will help to cope with pain. Additionally, the patient is referred to a physiotherapist. Exercises to strengthen the muscles around the hip joint and stretching are recommended. nine0003
Surgical treatment
Surgery is rarely used when there is no result from conservative therapy. The goal of treatment is to relieve tension in the iliopsoas tendon. The type of operation depends on the reason for the click. For example, arthroscopy is used to remove or repair fragments of a torn upper lip. The surgeon inserts a small camera into the hip joint that displays a real picture to control the instruments.
nine0027
Snapping Hip Syndrome
Try our set of exercises, developed in collaboration with specialists: this is a workout that takes into account the specifics of sports injuries.
Attention! If you've recently been injured, check with your doctor before you start exercising to see if it's right for your body.
Watch video
Exercises
PBT (Iliotibial Tract) Stretch
- Stand with your right side against a wall and cross your lower limbs, placing your right foot behind your left.
- Drive the hips towards the support until there is tension on the outside of the right leg.
- Hold the position for thirty seconds and repeat on the left side.
- Do 4 reps in 2-3 sets.
Piriformis Stretch
- Lie on your back with knees bent and feet flat on the floor. nine0033
- Put your right foot on your left knee, grab your left thigh with your hands.