Baby coming out from mother
Your baby in the birth canal Information | Mount Sinai
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Childbirth is really a series of four stages that culminate in the actual birth and short period thereafter. For more specific information regarding emergency delivery see the information on childbirth, emergency delivery.
Emergency measures are indicated when childbirth is imminent and no health care professional is present. Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Emergency measures are indicated when childbirth is imminent and no health care professional is present. Indications of late labor include rupturing of the amniotic sac, dilation of the cervix, and appearance of the baby's head at the vaginal opening.
Cephalic (head first) presentation is considered normal, but a breech (feet or buttocks first) delivery can be very difficult, even dangerous for the mother and the baby.
In a normal pregnancy, the baby is positioned head down in the uterus.
The term fetal presentation refers to the part of your baby's body that is closest to the birth canal. In most full-term pregnancies, the baby is positioned head down, or cephalic, in the uterus.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
FETAL LIE
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between his head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
Engagement
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
Descent
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
Flexion
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
Extension
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
Expulsion
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Last reviewed on: 12/3/2020
Reviewed by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Childbirth Options, Differences & Benefits
Overview
What are the types of delivery methods?
It’s hard to know exactly what will happen when you give birth. Most people have a plan in mind for how they hope their labor and delivery goes. When it comes to delivering your baby, it’s good to know there are many methods pregnancy care providers use. Types of delivery include:
- Vaginal delivery.
- Assisted vaginal delivery (vacuum or forceps).
- C-section (Cesarean birth).
- VBAC (vaginal birth after cesarean).
What type of delivery is best?
A vaginal delivery is the safest and most common type of childbirth. Vaginal deliveries account for about 68% of all births in the United States. Most medical organizations and obstetricians recommend a vaginal delivery unless there is a medical reason for a C-section.
Vaginal delivery
What is a vaginal delivery?
In a vaginal birth, your baby is born through your vagina or birth canal. It’s the most preferred and most common way to deliver a baby because it carries the lowest risk (in most cases). A vaginal delivery occurs most often between weeks 37 and 42 of pregnancy. A vaginal delivery has three stages: labor, birth and delivering the placenta.
Some benefits of a vaginal delivery include:
- Faster recovery.
- Safest for the pregnant person and the baby.
- Lower rates of infection.
- Babies are at lower risk for respiratory problems and have a stronger immune system.
- Lactation and breastfeeding are usually easier.
A vaginal delivery can be spontaneous or induced:
- Spontaneous vaginal delivery: A vaginal delivery that happens on its own and without labor-inducing drugs. Going into labor naturally at 40 weeks of pregnancy is ideal.
- Induced vaginal delivery: Drugs or other techniques start labor and soften or open your cervix for delivery. Pregnancy care providers often recommend inducing labor when a pregnant person has a medical condition or is past due. Labor is usually induced with Pitocin®, a synthetic form of the drug oxytocin.
What happens if you don’t push during a vaginal delivery?
In most cases, once your cervix is fully dilated and your healthcare team is in place, your provider will ask you to push during a contraction. Pregnancy care providers have differing opinions on when to push, how long to push, delayed pushing or waiting until you feel the urge to push.
It’s hard to say what will happen if you don’t or can’t push during a vaginal delivery, because your birthing experience is so unique. However, studies show that resisting the urge to push or delaying pushing (laboring down) can cause complications like infection, bleeding or damage to your pelvis.
It’s best to discuss pushing with your pregnancy care provider ahead of time so you know what to expect during labor.
Assisted vaginal delivery
What is an assisted vaginal delivery?
An assisted vaginal delivery is when your obstetrician uses forceps or a vacuum device to get your baby out of your vagina. Assisted deliveries often happen when:
- You’ve been in labor a long time.
- Your labor isn’t progressing.
- You become too fatigued to continue pushing.
- You or your baby are showing signs of distress.
Assisted deliveries only occur when certain conditions are met.
What are examples of assisted deliveries?
The procedure your obstetrician recommends will depend on the conditions that arise while you’re in labor. Assisted delivery procedures can include the following:
- Forceps delivery: Forceps are a tong-like surgical tool obstetricians use to grasp your baby’s head in order to guide them out of the birth canal.
- Vacuum extraction delivery: In a vacuum extraction, your obstetrician places a small suction cup on your baby’s head. The cup is attached to a pump that pulls on your baby while you push.
Vacuum extraction and forceps delivery are similar in their advantages and disadvantages, and often the choice between them comes down to the experience of your obstetrician.
C-section
What is a C-section?
During a C-section birth, your obstetrician delivers your baby through surgical incisions made in your abdomen and uterus. A C-section delivery might be planned in advance if a medical reason calls for it, or it might be unplanned and take place during your labor if certain problems arise. There are about 1.2 million C-section deliveries in the United States each year.
Your provider may recommend a planned cesarean delivery if you:
- Had a previous C-section delivery.
- Are expecting multiples.
- Have placenta previa.
- Have a breech baby.
- Have a baby with fetal macrosomia or a large baby.
- Have a uterine fibroid or other obstruction.
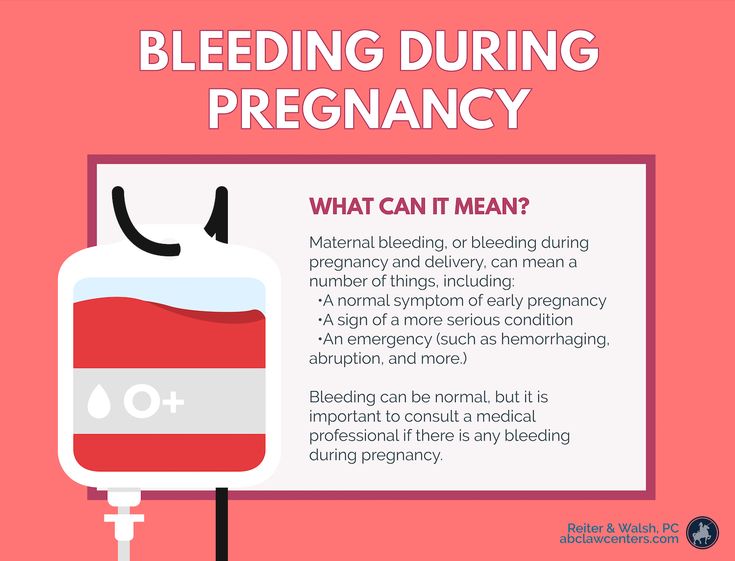
Sometimes, your labor and delivery changes, and a cesarean birth becomes necessary for the health and safety of you or your baby. An unplanned C-section might be needed if any of the following conditions arise during your labor:
- Fetal distress (your baby isn’t tolerating labor).
- Labor isn’t progressing.
- Umbilical cord prolapse.
- Placental abruption.
- Hemorrhage or excessive bleeding.
Risks of C-section deliveries
Like any surgery, a cesarean birth involves some risks. In general, there is more risk associated with a C-section than with a vaginal delivery.
These might include:
- Infection.
- Loss of blood or need for a blood transfusion.
- A blood clot that may break off and enter the bloodstream (embolism).
- Injury to the bowel or bladder.
- Longer recovery and longer hospital stay.
- Abdominal adhesions.
Benefits of C-section deliveries
Some people prefer a C-section birth because it gives them more control on choosing a due date. This is called an elective C-section. Some providers may allow elective C-sections for nonmedical reasons, however, this is usually discouraged. In most cases, a C-section birth occurs because it’s medically necessary. The American Congress of Obstetrics and Gynecologists (ACOG) recommends that scheduled cesareans not be performed before 39 weeks gestation, unless medically indicated.
Some benefits of a C-section as compared to a vaginal delivery are:
- Lower risk of your baby having trauma from passing through your vagina.
- Less risk of your baby being oxygen-deprived during delivery.
- Possible lower risk of incontinence or sexual dysfunction.
VBAC (vaginal birth after cesarean)
What is a VBAC?
If you’ve already had a cesarean birth, you may be able to have your next baby vaginally. This is a VBAC, or vaginal birth after cesarean. Because a surgical cut results in a scar on your uterus, the concern is that the pressure of labor in a vaginal delivery could cause your uterus to open (rupture) along the previous C-section scar. For this reason, certain criteria must be met in order for your obstetrician to attempt a vaginal birth after C-section.
Can I have a baby vaginally after a C-section?
People who have had a cesarean delivery might be able to deliver vaginally in a future pregnancy. If you meet the following criteria, your chances of a successful vaginal birth after cesarean (VBAC) are high:
- Your obstetrician made a low transverse incision during your cesarean.
This is the typical way to perform a C-section, unless they need to deliver your baby in a hurry.
- You don’t have other uterine scars or abnormalities.
- You had a prior vaginal delivery.
- You haven’t had a previous uterine rupture.
What else should I know about delivery?
There are several other terms you should be familiar with in case your pregnancy care provider discusses them during labor and delivery.
Episiotomy
An episiotomy is a surgical incision that widens the opening of your vagina. This allows your baby’s head to pass through more easily. Most people will not need an episiotomy.
There are two types of episiotomy incisions: the midline, made directly back toward your anus, and the mediolateral, which slants away from your anus.
Amniotomy (breaking your bag of waters)
An amniotomy is the artificial rupture of the amniotic membranes, or sac, which contains the fluid surrounding your baby. Your pregnancy care provider may artificially rupture your membranes (AROM) to:
- Induce or progress labor.
- Place an internal monitor to assess your contractions.
- Place an internal monitor on your baby’s scalp to assess their well-being.
- Check for meconium (a greenish-brown substance, which is your baby’s first poop).
Your provider will use an amniohook, which looks like a crochet hook, to rupture the sac. Once the procedure is complete, delivery should take place within 24 hours to prevent infection.
Fetal monitoring
Fetal monitoring is the process of watching your baby’s heart rate during labor. This can be external or internal. Knowing how your baby is handling labor helps your pregnancy care provider decide if labor can continue or if delivery is necessary.
- In external fetal monitoring, an ultrasound device is placed on your abdomen to record information about your baby’s heart rate, and the frequency and duration of your contractions.
- Internal monitoring involves the use of a small electrode to record your baby’s heart rate.
Your membranes must be ruptured before the electrodes can be attached to your baby’s scalp. A pressure sensor can also be placed near your baby to measure the strength of contractions.
Frequently Asked Questions
Which type of delivery is most painful?
This may come down to personal opinion. There are many factors involved — for example, using pain medication, the type of pain medication or your pain tolerance. You should discuss pain relief with your pregnancy care provider before labor so you know the risks and benefits of each type.
There are two general options: no medication (drug-free or natural delivery) or using pain medications.
A drug-free delivery means you intend to give birth vaginally without any pain medication. You can’t have a C-section without medication.
Your options for pain relief during childbirth could consist of:
- Analgesics: Analgesics relieve pain without causing complete loss of feeling or muscle movement.
The most common example of an analgesic used during childbirth is an epidural. You can receive an epidural for a vaginal or a cesarean delivery.
- Anesthetics: Anesthetics (or anesthesia) keep you from feeling pain by blocking signals from your brain. These drugs are given as a shot or through an intravenous (IV) line. During a C-section, you may receive general anesthesia, which puts you to sleep. Another option during childbirth could be local anesthesia, which involves a shot of medication in a specific area of your body, like the nerves in your vagina and vulva.
Another factor in deciding what type of delivery is most painful is the recovery. Generally, a vaginal delivery is easier to recover from than a C-section delivery.
A note from Cleveland Clinic
Your labor and delivery experience will be unique to you. During pregnancy, it’s a good idea to familiarize yourself with the different types of delivery and other terms associated with childbirth. Your pregnancy care provider will recommend the safest delivery method based on your medical history and pregnancy.
How your baby is born: the whole process step by step - Parents.ru
- Photo
- Mustafagull/Getty Images/E+
neonatologist
It is up to the baby to decide when to be born. It is his endocrine system that triggers the birth mechanism, stimulating the production of the main birth hormone, oxytocin, in the mother. Normally, this happens when all the systems and organs of the child are already fully prepared for independent life - usually at the 38-40th week of pregnancy.
In order for the birth of a baby to go smoothly, the process must be gradual, and therefore preparation for it begins in advance, about 2 weeks before the decisive day. Under the influence of the hormones of the child's body, in particular, those produced by the adrenal cortex, more and more oxytocin is produced in the mother's body, which causes contractions of the muscles of the uterus, estrogen (they increase uterine tone) and relaxin (it softens the muscles and ligaments). At the 38th week, the baby's head moves closer to the exit from the uterus, and the expectant mother notices that the stomach has dropped a little. The uterus is increasingly contracting - but so far these irregular preparatory contractions do not cause discomfort to either the child or the mother and usually go unnoticed by them.
- Photo
- kieferpix/Getty Images/iStockphoto
The first stage
Birth is stressful and hard work for a little man. The walls of the native dwelling, where the baby spent 9 months, suddenly begin to put pressure on their inhabitant, he is irresistibly drawn somewhere down, where he has to squeeze through a narrow winding labyrinth, and besides, in the process of childbirth, the supply of oxygen and nutrition stops every now and then. As in an adult in moments of physical and mental stress, a child during childbirth sharply increases the level of "stress hormones" catecholamines (adrenaline, norepinephrine and dopamine). Fortunately, wise nature has provided a number of protective measures that make it easier for the baby to be born. So, along with catecholamines, endorphins and enkephalins are intensively produced in the child's body - substances that create an analgesic effect and help the body mobilize forces.
During the first stage of labor, when the cervix opens under the action of contractions, the baby is busy gradually descending from the uterine cavity to the entrance to the small pelvis. Moving head forward and pushing it like a battering ram, the child covers a distance of only a few centimeters, but this journey takes as much as 6-12 hours. Such slowness is very important, because if the process happens too quickly, it threatens the child with birth injuries.
With each contraction, the baby feels pressure from the muscles of the uterus and abdominals. But, due to the fact that the baby is surrounded by amniotic fluid, this pressure is softened. When the uterus contracts, the placenta contracts, and the blood flow to the baby for the duration of the contraction (and in the midst of childbirth, it lasts up to 1 minute) stops. To compensate for the lack of oxygen, the baby's heart begins to beat faster - up to 180 beats per minute instead of 140 at rest. At the moment of tension of the uterus, the baby freezes, in order to then take the next “step” forward.
- Photo
- Robert Lang Photography/Getty Images
Steep route
The baby's direct entry into the world occurs during the period of pushing, which occurs after the cervix is fully dilated. This stage of childbirth is considered the most time-consuming for both the child and the mother. The woman is actively pushing, straining the abdominal muscles, and the baby's head, under the influence of contractions, passes through the small pelvis and enters the genital gap. As the child moves through the narrow space of the small pelvis, the bones of his skull are on top of each other, adapting to the winding route. The torso of the baby, first of all, the chest, is also “compacted”.
Edema of subcutaneous adipose tissue forms on the crown and back of the head - a birth tumor that protects the baby's brain from pressure. In the most common development of events, the back of the baby's head is shown first, then the crown, forehead and face facing down towards the floor. After the birth of the entire head, the baby turns 90 °, facing the mother's thigh, and the upper and lower shoulders come out in turn. Now we can assume that the main work has already been done: after the birth of the head (the largest part of the child's body) and shoulders, the torso and legs come out without problems.
During childbirth, mother and baby work in sync. So, at the initial stage of labor, contractions force the child to move towards the exit from the uterus, and he, in turn, presses his head on the cervix, opening it from the inside. During the period of exile, the mother pushes, straining the abdominal muscles, and the baby pushes the back of the head against the pelvic floor more and more, due to which the attempts become more frequent and intense.
Cardiotocography helps doctors judge how the baby feels during childbirth. It allows you to evaluate the heart rate of the baby, as well as the tone of the uterus of his mother. The rhythm of the baby's heartbeat changes every now and then during childbirth. But doctors, knowing what changes should occur in the norm, can immediately respond if violations occur. For example, during the period of attempts, the pulse becomes less frequent when the baby's head passes the narrowest part of the mother's small pelvis. Movement in this area normally takes only a few minutes, but if the baby is delayed and the heart rate remains slow for too long, then the child needs urgent help: a caesarean section or the imposition of obstetric instruments.
- Photo
- Handemandaci/Getty Images
Welcome!
A baby greets his birth with a loud cry — this is a reflex reaction to a change in environmental conditions (temperature, lighting, etc. ) and the first supply of oxygen to the lungs. Thanks to this, they straighten out, and the fetal fluid that filled them before birth comes out of them. The deeper the first breath, the more the newborn cries. It is no coincidence that the loud crying of a baby is considered one of the important indicators of his health. If there is no scream or it is barely audible, then the baby has breathing problems and needs emergency help. A healthy newborn breathes frequently, actively moves his arms and legs, his heart beats quickly (more than 100 beats per minute). He screams indignantly if his heels are tickled to test his reflexes; sneezes and coughs when clearing the nose and mouth.
As soon as the baby is born, a whole flurry of new sensations falls upon him. These are the touches of human hands (before, the baby only felt the splash of amniotic fluid), bright light and loud sounds, too harsh after darkness and silence in the uterus. And yet ... cold - after all, in the uterine cavity the temperature is 37-38 ° C, and in the birth block - "only" 23-24 ° C.
As soon as the baby is born, it is immediately placed on the mother's breast and a few drops of colostrum are dripped into the mouth. It’s great if dad is next to the newborn at this moment. The closeness of parents (of course, primarily mothers) in the first minutes of life is very important, because on a subconscious level, the whole situation of birth is stored in the memory of the child. The atmosphere, emotions, sensations with which a little man crosses the threshold of a new world may affect his psychological health in the future. It is no coincidence that psychologists and biologists consider imprinting - the perception of the first life impressions (tactile, auditory, visual, etc.) - fundamental for proper development. It is thanks to these first minutes that a newborn baby remembers his mother and from now on unmistakably recognizes her, immediately calming down as soon as she takes him in her arms.
More useful materials for expectant mothers - in our channel on Yandex. Zen.
Irina Bezrukova
The process of childbirth
This event must be approached with self-confidence, one's strengths, capabilities and reliability of information received about childbirth during pregnancy. Tuning in the right way and doing everything right, knowledge helps. It is incomparably easier for pregnant women who have a good idea of all the stages of the birth process and are psychologically prepared for the upcoming event than for those expectant mothers who are poorly aware of what will happen to them.
Childbirth is divided into three periods:
- Disclosure period . As a result of regular contractions (involuntary contraction of the muscles of the uterus), the cervix opens.
- The period of expulsion of the fetus from the uterine cavity. Attempts are added to the contractions - arbitrary (that is, controlled by the woman in labor) contractions of the abdominal muscles.
The baby moves through the birth canal and is born.
- Follow-up period . The placenta and membranes are born.
First stage of labor
The fact that labor has already begun or is about to begin is indicated by the appearance of regular contractions and / or the outflow of amniotic fluid. Contractions are involuntary periodic contractions of the muscles of the uterus, aimed at shortening and opening the cervix. Normally, the length of the cervix is 3-5 cm, and the diameter is only a few millimeters. And for the birth of a child, it is necessary that the cervix completely shorten and open up to 9-10 cm.
The period of dilation is the longest in the process of childbirth. In the natural course of childbirth, this period lasts 10-11 hours for primiparas, 6-7 hours for multiparous ones.
At the beginning of this period there are regular contractions that last 15-20 seconds with an interval of about 15 minutes. As the cervix dilates, the contractions intensify, become longer, and the intervals between them shorten. When the break between contractions is 10 minutes, you need to go to the maternity hospital.
During the opening period, it is recommended to walk, move, breathe properly, take a warm shower or bath. These measures contribute to a faster opening of the cervix, while reducing pain. You can ask your husband or midwife to massage the lumbar region - this will reduce the discomfort from contractions.
Second stage of labor
Most women agree that the end of the dilation phase, before the onset of the second stage of labor, is the most difficult. Contractions become frequent and painful, anesthesia by this moment usually ceases to act, fatigue accumulates, it is still impossible to push. The state of many women at this moment is described by one single phrase: “That's it! I can not anymore!". The only consolation is that it doesn't last long.
After the cervix is fully dilated, the doctor allows the mother to push. A woman usually herself feels strong urges to "push" the child out of the birth canal. These urges are called pushes.
For pushing to be effective, you need to push properly and breathe properly. Before pushing, you need to get more air into the lungs, hold your breath and try to push effectively. It is important not to strain your face and legs during attempts, but on the contrary - to relax as much as possible. Between attempts, you also need to relax and rest.
The second stage of labor lasts from 15 minutes to two hours, and in multiparous this stage is shorter than in primiparas. During this period, doctors especially carefully monitor the condition of the mother and fetus (they regularly listen to heartbeats, etc.).
Meanwhile, the baby is moving along the genital tract. At the height of one of the attempts from the genital slit, the lower pole of the head (or buttocks - in breech presentation) is shown, after the end of the attempt, the head is hidden in the genital slit. This process - cutting the head - continues for some time. At a certain moment, the pole of the head remains in the genital gap and in between attempts. Under the influence of continuing attempts, the eruption of the head begins, which continues until its full birth. There is very little left. A few more attempts - and the whole child is born.
The newborn is placed on the mother's stomach (ideally), and they get to know each other for a while, rest after the birth. The midwife or doctor then cuts the umbilical cord and takes the baby away for proper treatment, bathing, weighing and examination by a pediatrician.
Can be applied to the breast 10-15 minutes after birth. This promotes uterine contraction and milk production.
Third stage of labor
The last stage of labor - the birth of the placenta - is the shortest. Usually, the afterbirth is born 10-20 minutes after the birth of the baby. Mom might need to push a little for this.
If the placenta does not separate for more than 30 minutes, doctors diagnose the retention of the placenta in the uterus and begin to take emergency measures.
The delivered placenta is carefully examined for its integrity. If everything is fine, that is, the placenta has separated completely, the woman is sewn up with tears or incisions (if any). After that, a heating pad with ice is placed on her stomach and observed for some time in the delivery room (1.5-2 hours).
This is where the birth process ends and a new life begins for mother and baby.
References
- Florian S., Ichou M., Panico L. Parental migrant status and health inequalities at birth: The role of immigrant educational selectivity. // Soc Sci Med - 2021 - Vol278 - NNULL - p.113915; PMID:33905985
- Naja S., Al Kubaisi N., Singh R., Abdalla H., Bougmiza I. Screening for antenatal depression and its determinants among pregnant women in Qatar: revisiting the biopsychosocial model. // BMC Pregnancy Childbirth - 2021 - Vol21 - N1 - p.330; PMID:33902481
- Shchepin VO., Khabriev RU. [The characteristics of population mortality of the Russian Federation, the Central Federal Okrug and City of Moscow in 2020].
// Probl Sotsialnoi Gig Zdravookhranenniiai Istor Med - 2021 - Vol29 - N2 - p.189-193; PMID:33
- 2
- Saavedra LPJ., Prates KV., Gonçalves GD., Piovan S., Matafome P., Mathias PCF. COVID-19 During Development: A Matter of Concern. // Front Cell Dev Biol - 2021 - Vol9 - NNULL - p.659032; PMID:33898461
- Caparros-Gonzalez RA., Romero-Gonzalez B., Puertas-Gonzalez JA., Quirós-Fernandez S., Coca-Guzman B., Peralta-Ramirez MI. [Midwives and psychologists as professionals to screen and prevent pregnancy-specific stress.] // Rev Esp Salud Publica - 2021 - Vol95 - NNULL - p.; PMID:33896933
- Burakowska K., Gorka P., Penner GB. Effects of canola meal inclusion rate in starter mixtures for Holstein heifer calves on dry matter intake, average daily gain, ruminal fermentation, plasma metabolites, and total-tract digestibility. // J Dairy Sci - 2021 - Vol - NNULL - p.; PMID:33896627
- Toker E., Aktaş S. The childbirth experiences of Syrian refugee mothers living in Turkey: a qualitative study.