Babies born with low birth weight
Low Birthweight in Newborns | Boston Children's Hospital
What is low birthweight?
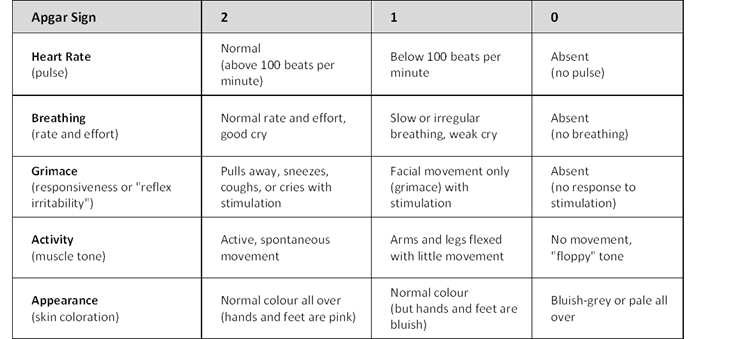
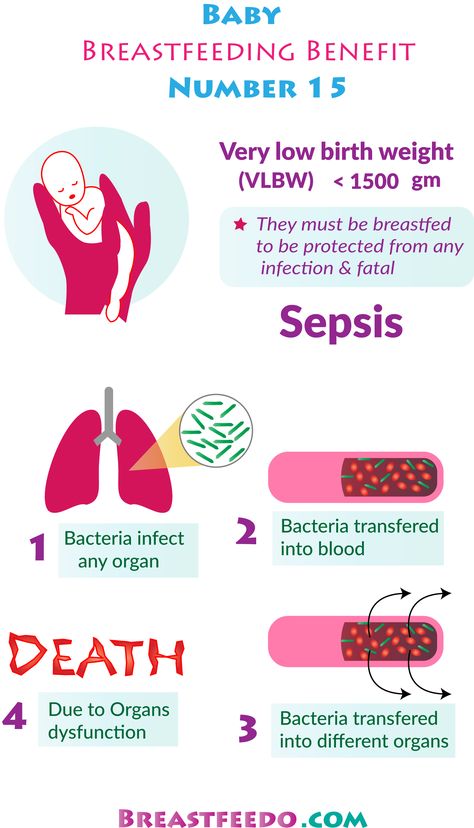
Babies are weighed within the first few hours after birth. The weight is compared with the baby's gestational age and recorded in the medical record. A birthweight less than 5 pounds, 8 ounces, is diagnosed as low birthweight. Babies weighing less than 3 pounds, 5 ounces, at birth are considered very low birthweight.
The average newborn weighs about 7.6 pounds, and about 7.6 percent of all newborns in the U.S. have low birthweight. The overall rate of these very small babies is increasing, primarily because of the increase in multiple birth babies, who tend to be born earlier and weigh less. More than half of multiple birth babies have low birthweight.
Why is low birthweight a concern?
If your baby has a low birthweight, she may be at increased risk for complications. Her tiny body is not as strong, and she may have a harder time eating, gaining weight, and fighting infections. Because she has so little body fat, she may have a hard time staying warm in normal temperatures.
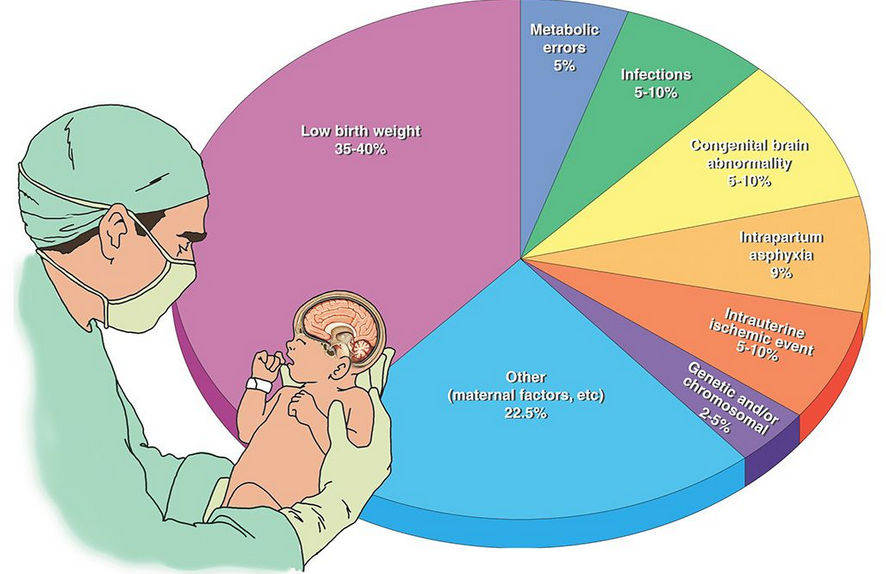
Because many babies with low birthweight are also premature, it is can be difficult to separate the problems due to the prematurity from the problems of just being so tiny. In general, the lower a baby's birthweight, the greater the risks for complications. The following are some of the common problems of low birthweight babies:
- low oxygen levels at birth
- inability to maintain body temperature
- difficulty feeding and gaining weight
- infection
- breathing problems, such as respiratory distress syndrome (a respiratory disease of prematurity caused by immature lungs)
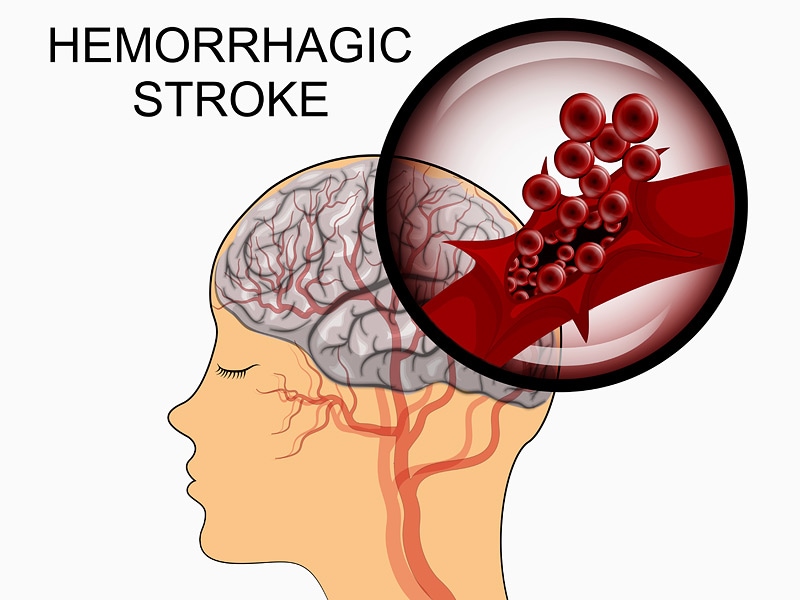
- neurologic problems, such as intraventricular hemorrhage (bleeding inside the brain)
- gastrointestinal problems such as necrotizing enterocolitis (a serious disease of the intestine common in premature babies)
- sudden infant death syndrome (SIDS)
What causes low birthweight?
The primary cause is premature birth, being born before 37 weeks gestation; a baby born early has less time in the mother's uterus to grow and gain weight, and much of a fetus' weight is gained during the latter part of the mother's pregnancy.
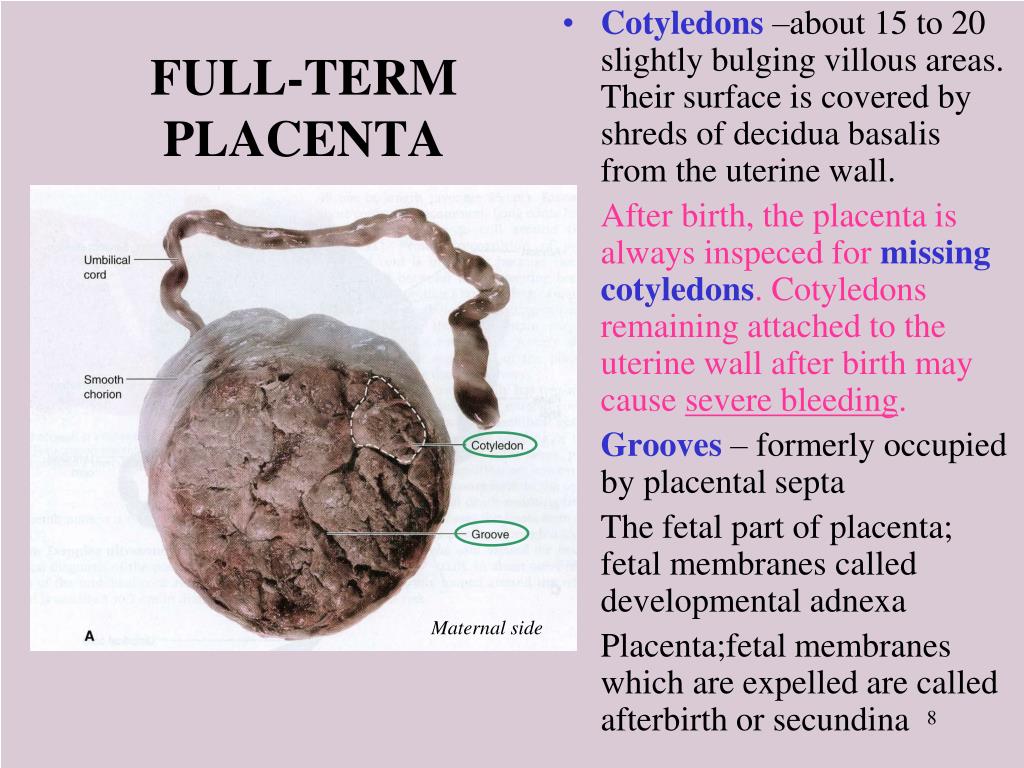
Another cause of low birthweight is intrauterine growth restriction. This occurs when a baby does not grow well in utero because of problems with the placenta, the mother's health, or birth defects. Babies with Intrauterine growth restriction (IUGR) may be born early or full-term; premature babies with IUGR may be very small and physically immature, and full-term babies with IUGR may be physically mature but weak.
Any baby born prematurely is more likely to be small. However, there are other factors that can also contribute to the risk of low birthweight. These include:
- Race: African-American babies are twice as likely as Caucasian babies to have low birthweight.
- Mother's age: Teen mothers (especially those younger than 15) have a much higher risk of having a baby with low birthweight.
- Multiple birth: Multiple birth babies are at increased risk of low birthweight because they often are premature.
- Mother's health: Babies of mothers who are exposed to illicit drugs, alcohol, and cigarettes are more likely to have low birthweight.
 Mothers of lower socioeconomic status are also more likely to have poorer pregnancy nutrition, inadequate prenatal care, and pregnancy complications — all factors that can contribute to low birthweight.
Mothers of lower socioeconomic status are also more likely to have poorer pregnancy nutrition, inadequate prenatal care, and pregnancy complications — all factors that can contribute to low birthweight.
Nearly all low birthweight babies need specialized care in the Neonatal Intensive Care Unit (NICU) until they gain weight and are well enough to go home. Fortunately, there is a 95 percent chance of survival for babies weighing between 3 pounds, 5 ounces, and 5 pounds, 8 ounces.
Can low birthweight be prevented?
Prevention of preterm births is one of the best ways to prevent babies born with low birthweight. Prenatal care is a key factor in preventing preterm births and low birthweight babies.
At prenatal visits, the health of both mother and fetus can be checked. Because maternal nutrition and weight gain are linked with fetal weight gain and birthweight, eating a healthy diet and gaining the proper amount of weight in pregnancy are essential. Mothers should avoid alcohol, cigarettes, and illicit drugs, which can contribute to poor fetal growth, among other complications.
How is a low birthweight diagnosed during pregnancy?
During pregnancy, a baby's birthweight can be estimated in different ways:
- The height of the fundus (the top of a mother's uterus) can be measured from the pubic bone. This measurement in centimeters usually corresponds with the number of weeks of pregnancy after the 20th week. If the measurement is low for the number of weeks, the baby may be smaller than expected.
- An ultrasound is a more accurate method of estimating fetal size. Measurements can be taken of the fetus' head and abdomen, and compared with a growth chart to estimate fetal weight.
Babies are weighed within the first few hours after birth. The weight is compared with the baby's gestational age and recorded in the medical record. A birthweight less than 5 pounds, 8 ounces, is diagnosed as low birthweight. Babies weighing less than 3 pounds, 5 ounces, at birth are considered very low birthweight.
What are the treatment options for low birthweight newborns?
Care for low birthweight babies may include:
- care in the NICU
- temperature-controlled beds
- special feedings, sometimes with a tube into the stomach if a baby cannot suck
- other treatments for complications
Low birthweight babies typically "catch up" in physical growth if there are no other complications. Babies may be referred to special follow-up healthcare programs.
Babies may be referred to special follow-up healthcare programs.
How we care for low birthweight newborns
The Boston Children's Hospital Infant Follow-Up Program is designed for infants born very prematurely, who weigh less than 3.3 pounds and are at high risk for development and motor delays and other problems resulting from prematurity. Our program follows children from the time of discharge until they reach age 3 to 4.
The multi-disciplinary team includes pediatricians, neonatologists, pediatric psychologists, physical therapists, social workers, and if needed, pediatric neurologists.
Low birthweight | March of Dimes
Low birthweight is when a baby is born weighing less than 5 pounds, 8 ounces.
Some low-birthweight babies are healthy, but others have serious health problems that need treatment.
Premature birth (before 37 weeks of pregnancy) and fetal growth restriction are the most common causes of low birthweight.
Being a person of color is not a cause for having a low birthweight baby.
 However, communities of color are disproportionately affected by racism. This affects their health and well-being and increases the risk of pregnancy complications.
However, communities of color are disproportionately affected by racism. This affects their health and well-being and increases the risk of pregnancy complications.Go to all your prenatal care checkups during pregnancy. Your health care provider tracks your baby’s growth and development at each visit.
Talk with your provider about what you can do to help reduce your risk for having a baby with low birthweight.
What is low birthweight?
Low birthweight is when a baby is born weighing less than 5 pounds, 8 ounces. Some babies with low birthweight are healthy, even though they’re small. But having a low weight at birth can cause serious health problems for some babies. A baby who is very small at birth may have trouble eating, gaining weight and fighting off infections. Some may have long-term health problems, too. About 1 in 12 babies (about 8 percent) in the United States is born with low birthweight.
What causes a baby to have a low birthweight?
There are two main reasons:
- Preterm birth.
- Fetal growth restriction (also called intrauterine growth restriction or small for gestational age). This means a baby doesn’t gain the weight they should before birth. Some babies may have low birthweight simply because their parents are small. Others may have low birthweight because something slowed or stopped their growth during pregnancy. Your health care provider measures your belly and uses ultrasound to help track your baby’s growth during pregnancy. Ultrasound uses sound waves and a computer screen to show a picture of your baby while you’re pregnant.
If your provider thinks your baby’s growth is being restricted, you may have ultrasounds more often (every 2 to 4 weeks) to track your baby’s growth. Your provider also may do other tests such as heart rate monitoring and tests to check for infections or birth defects. Babies who have birth defects are more likely to be born too early.
Are you at risk of having a low-birthweight baby?
Some things may make you more likely than others to have a low-birthweight baby. These are called risk factors. Having a risk factor doesn’t mean you’ll definitely have a low-birthweight baby, but it may increase your chances. Talk with your health care provider about what you can do to reduce your risk.
These are called risk factors. Having a risk factor doesn’t mean you’ll definitely have a low-birthweight baby, but it may increase your chances. Talk with your health care provider about what you can do to reduce your risk.
Medical risk factors for having a low-birthweight baby
- Preterm labor. This is labor that starts too soon, before 37 weeks of pregnancy.
- Chronic health conditions. These are health conditions that last for a long time or that happen again and again over a long period of time. Chronic health conditions need to be treated by a health care provider. Chronic health conditions that may lead to having a baby with low birthweight include high blood pressure, diabetes and heart, lung and kidney problems.
- Taking certain medicines to treat health conditions, such as high blood pressure, epilepsy and blood clots. Tell your provider about any prescription medicine you take.
 You may need to stop taking a medicine or switch to one that’s safer during pregnancy.
You may need to stop taking a medicine or switch to one that’s safer during pregnancy. - Infections. Certain infections, especially infections of the internal reproductive organs during pregnancy, can slow a baby’s growth in the womb. These include cytomegalovirus, rubella, chickenpox, toxoplasmosis and certain sexually transmitted infections.
- Problems with the placenta. The placenta grows in the uterus and supplies the baby with food and oxygen through the umbilical cord. Some problems in the placenta can reduce the flow of oxygen and nutrients to the baby, which can limit the baby’s growth.
- Not gaining enough weight during pregnancy. Pregnant people who don’t gain enough weight during pregnancy are more likely to have a low-birthweight baby than those who gain the right amount of weight. If you have an eating disorder or have been treated for an eating disorder, tell your provider.
 Your provider can check on you and your baby carefully throughout pregnancy to help prevent complications and make sure you’re both healthy.
Your provider can check on you and your baby carefully throughout pregnancy to help prevent complications and make sure you’re both healthy. - Having a baby who was born too early or who had low birthweight in the past.
- Being pregnant with multiples (twins, triplets or more). More than half of multiple birth babies have low birthweight.
- Smoking, drinking alcohol, using street drugs and abusing prescription drugs. Pregnant people who smoke are more than 3 times as likely to have a baby who weighs too little at birth than people who don’t smoke. Smoking, drinking alcohol, using street drugs, and abusing prescription drugs during pregnancy can slow the baby’s growth in the womb and increase the risk for preterm birth and birth defects.
- Exposure to air pollution or lead
- Being a member of a group that experiences the effects of racism and health disparities.
- Domestic violence. This is when your partner hurts or abuses you. It includes physical, sexual and emotional abuse.
- Age. Being a teen (especially younger than 15) or being older than 35 makes you more likely than other parents to have a low-birthweight baby.
Rates of low birthweight in the United States
Black babies are more likely than others to weigh less than they should at birth. The rates of low birthweight among different ethnic groups are:
- About 1 in 7 Black babies (about 13 percent)
- About 1 in 12 Asian babies (about 8 percent)
- About 1 in 13 Native American or Alaska Native babies (about 8 percent)
- About 1 in 14 Latinx babies (about 7 percent)
- About 1 in 14 White babies (about 7 percent)
March of Dimes recognizes that racism and its effects are factors in the health disparities in pregnancy outcomes and babies’ health. We must work together to bring fair, just and full access to health care for all moms and babies.
Does a low birth weight cause problems for the baby?
Yes. Babies who weigh less than they should at birth are more likely than babies whose weight is normal to have health problems. Some need special care in a hospital’s newborn intensive care unit (also called NICU) to treat medical problems. These include:
- Breathing problems, such as respiratory distress syndrome (also called RDS). Babies with RDS don’t have a protein called surfactant that keeps small air sacs in a baby’s lungs from collapsing. Treatment with surfactant helps these babies breathe more easily. Babies who have RDS also may need oxygen and other breathing help to make their lungs work.
- Bleeding in the brain (also called intraventricular hemorrhage or IVH). Most brain bleeds are mild and go away on their own. More severe bleeds can cause pressure on the brain that can cause fluid to build up in the brain. This can cause brain damage. In some cases, a surgeon may insert a tube into the baby’s brain to drain the fluid.
- Patent ductus arteriosus. Patent ductus arteriosus is when an opening between 2 major blood vessels leading from the heart does not close properly. This can cause extra blood to flow to the lungs. In many babies who have patent ductus arteriosus, the opening closes on its own within a few days after birth. Some babies need medicine or surgery to close the opening.
- Necrotizing enterocolitis. This is a problem in a baby’s intestines. The intestines are long tubes that are part of the digestive system. The digestive system helps the body break down food. Necrotizing enterocolitis can be dangerous for a baby and can cause feeding problems, swelling in the belly, and other complications. Babies who have necrotizing enterocolitis are treated with antibiotics and fed through an intravenous, or IV, tube. Some babies need surgery to remove damaged parts of intestine.
- Retinopathy of prematurity. This eye disease is what happens when a baby’s retinas don’t fully develop in the weeks after birth.

- Jaundice. This is a condition that makes a baby’s eyes and skin look yellow. It’s caused when there’s too much of a substance called bilirubin in the blood.
- Infections. The immune system protects the body from infection. In a baby who is born too early, the immune system may not be fully developed and may not be able to fight off infection.
Does a low weight at birth cause problems later in life?
Babies who are born weighing too little may be more likely than others to have certain health conditions later in life, including:
- Diabetes
- Heart disease
- High blood pressure
- Intellectual and developmental disabilities
- Metabolic syndrome
- Obesity
If you’ve had a baby who weighed less than they should have at birth, talk with their health care provider about what you can do to help your baby be healthy. As your child grows, make sure they eat healthy food, stay active and go to all their health care checkups. Regular checkups can help your baby’s provider spot health conditions that may cause problems as your baby grows older. These checkups also help make sure that your child gets all the vaccinations they need to stay protected from certain harmful diseases.
Regular checkups can help your baby’s provider spot health conditions that may cause problems as your baby grows older. These checkups also help make sure that your child gets all the vaccinations they need to stay protected from certain harmful diseases.
If my baby has developmental delays, do they need early intervention services?
Yes. If your baby has developmental delays, it’s important to get early intervention services as soon as possible. Developmental delays are when your child doesn’t reach developmental milestones when expected. Early intervention services can help improve your child’s development. They can help children from birth through 3 years old learn important skills. Services include therapy to help a child talk, walk, learn self-help skills and interact with others.
The CDC program Learn the signs. Act early offers tools and information for parents who think their child may have developmental delays. You can find your state’s contact information for early intervention services. You don’t need a doctor’s referral or a medical diagnosis to ask for a free screening.
You don’t need a doctor’s referral or a medical diagnosis to ask for a free screening.
Last reviewed: June, 2021
PREMATURE AND LOW BIRTH WEIGHT AS RISK FACTORS FOR NEURO-MENTAL DEVELOPMENT DISORDERS IN CHILDREN | Zavadenko
1. Zavadenko N.N. Delays in early neuropsychic development: approaches to diagnosis. Roswest Perinatol and Pediatrician 2015; 60(5):6–13.
2. Born too soon. Report on global action on preterm birth. World Health Organization 2014; 126.
3. A.B. Neurology of premature babies. M: MEDpress-inform 2010; 342.
4. Sakharova E.S., Keshishyan E.S. Principles of care for premature babies in the postneonatal period. Rosvestn perinatol and pediatrician 2014; 59(1): 40–45.
5. Stephens B.E., Vohr B.R. Neurodevelopmental Outcome of the Premature Infant. Pediatric Clin North Am 2009; 56(3): 631–646. DOI: 10.1016/j.pcl.2009.03.005
6. Glass H.C., Costarino A.T., Stayer S.A., Brett C., Cladis F., Davis P.J. Outcomes for Extremely Premature Infants. Anesth Analg 2015; 120(6): 1337–1351. DOI: 10.1213/ ANE.0000000000000705
Anesth Analg 2015; 120(6): 1337–1351. DOI: 10.1213/ ANE.0000000000000705
7. Zavadenko N.N. Hyperactivity and attention deficit in childhood. 2nd ed., revised. and additional M: Yurayt Publishing House 2018; 274.
8. Achenbach T.M. Manual for the Child Behavior Checklist. Burlington, University of Vermont Department of Psychiatry 1991; 191.
9. Kornilova T.V., Grigorenko E.L., Smirnov S.D. Adolescents at risk. St. Petersburg, "Peter" 2005; 336.
10. ICD-10 - International Classification of Diseases (10th revision). Classification of mental and behavioral disorders. Research diagnostic criteria. St. Petersburg 1994; 208.
11. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V). American Psychiatric Association. Washington 2013, 947.
12. Zavadenko N.N., Nemkova S.A. Developmental disorders and cognitive dysfunctions in children with diseases of the nervous system. Scientific and practical guide. M: MK 2016; 360.
13. Aarnoudse-Moens C.S., Weisglas-Kuperus N., van Goudoever J.B., Oosterlaan J. Metaanalysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 2009; 124(2): 717–728. DOI: 10.1542/peds.2008-2816
Aarnoudse-Moens C.S., Weisglas-Kuperus N., van Goudoever J.B., Oosterlaan J. Metaanalysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 2009; 124(2): 717–728. DOI: 10.1542/peds.2008-2816
14. Bhutta A.T., Cleves M.A., Casey P.H., Cradock M.M., Anand K.J. Cognitive and behavioral outcomes of schooled children who were born preterm: a meta-analysis. JAMA 2002; 288(6): 728–737.
15. Class Q.A., Rickert M.E., Larsson H., Lichtenstein P., D’Onofrio B.M. Fetal growth and psychiatric and socioeconomic problems: population based sibling comparison. BrJ Psychiatry 2014; 205(5): 355–361. DOI: 10.1192/bjp. bp.113.143693
16. De Jong M., Verhoeven M., van Baar A.L. School outcome, cognitive functioning, and behavior problems in moderate and late preterm children and adults: a review. Semin Fetal Neonatal Med 2012; 17(3): 163–169.
17. Sucksdorff M., Lehtonen L., Chudal R., Suominen A., Joelsson P., Gissler M., Sourander A. Preterm Birth and Poor Fetal Growth as Risk Factors of Attention-Deficit/Hyperactivity Disorder. Pediatrics 2015: 136(3): e599–t608. DOI: 10.1542/peds.2015-1043
Preterm Birth and Poor Fetal Growth as Risk Factors of Attention-Deficit/Hyperactivity Disorder. Pediatrics 2015: 136(3): e599–t608. DOI: 10.1542/peds.2015-1043
18. Lampi K.M., Lehtonen L., Tran P.L., Suominen A., Lehti V., Banerjee P.N. et al. Risk of autism spectrum disorders in low birth weight and small for gestational age infants. J Pediatr 2012; 161:830–836. DOI: 10.1016/j.jpeds.2012.04.058
19. Gardener H., Spiegelman D., Buka S.L. Perinatal and neonatal risk factors for autism: A comprehensive meta-analysis. Pediatrics 2011; 128:344–355. DOI: 10.1542/peds.2010-1036
20. Guinchat V., Thorsen P., Laurent C., Cans C., Bodeau N., Cohen D. Pre-, peri- and neonatal risk factors for autism. Acta Obstet Gynecol Scand 2012; 91:287–300.
21. Kuzniewicz M.W., Wi S., Qian Y., Walsh E.M., Armstrong M.A., Croen L.A. Prevalence and neonatal factors associated with autism spectrum disorders in preterm infants. J Pediatr 2014; 164:20–25. DOI: 10.1016/j.jpeds.2013. 09.021.
09.021.
22. Fezer G.F., de Matos M.B., Nau A.L., Zeigelboim B.S., Marques J.M., Liberalesso P.B.N. Perinatal features of children with autism spectrum disorder. Rev Paul Pediatrician 2017; 35(2): 130–135. DOI: 10.1590/1984-0462/;2017;35;2;00003
23. Toulmina H., Beckman C.F., O’Muircheartaigh J., Gareth B., Nongena P., Makropoulos A., Ederies A. et al. Specialization and integration of functional thalamocortical connectivity in the human infant. PNAS 2015; 112(20): 6485–6490. www. pnas.org/cgi/doi/10.1073/pnas.1422638112
24. Kallankari H., Kaukola T., Olsén P., Ojaniemi M., Hallman M. Very preterm birth and foetal growth restriction are associated with specific cognitive deficits in children attending mainstream school. Acta Paediatr 2015; 104(1): 84–90. DOI: 10.1111/apa.12811
25. Meldrum S.J., Strunk T., Currie A., Prescott S.L., Simmer K., Whitehouse A.J. Autism spectrum disorder in children born preterm-role of exposure to perinatal inflammation. Front Neurosci 2013; 7:1–10. DOI: 10.3389/fnins.2013.00123
DOI: 10.3389/fnins.2013.00123
26. Angelidou A., Asadi S., Alysandratos K.D., Karagkouni A., Kourembanas S., Theoharides T.C. Perinatal stress, brain inflammation and risk of autism – review and proposal. BMC Pediatr 2012; 12:89–101. DOI: 10.1186/1471-2431-12-89
27. Namazova-Baranova L.S. Scientific research and infrastructure of the Pediatrics platform. Pediatric Pharmacology 2012; 9(4): 15–24.
28. Federal Guide to Child Neurology. Ed. IN AND. Guzeva. M: Special publishing house of medical books 2016; 656.
Premature babies. What are Premature Babies?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Premature babies are babies born before the due date, functionally immature, with a weight below 2500 g and a body length of less than 45 cm. underdevelopment of the genital organs, weakness or absence of reflexes, weak cry, intense and prolonged jaundice, etc. Nursing premature babies involves the organization of special care - temperature, humidity, oxygenation level, feeding, and, if necessary, intensive care.
underdevelopment of the genital organs, weakness or absence of reflexes, weak cry, intense and prolonged jaundice, etc. Nursing premature babies involves the organization of special care - temperature, humidity, oxygenation level, feeding, and, if necessary, intensive care.
- Causes of prematurity
- Classification of prematurity
- External signs of prematurity
- Anatomical and physiological features of premature babies
- Special care for premature babies
- Medical examination of premature babies
- Prices for treatment
General
Premature children are those born between the 28th and 37th weeks of pregnancy, having a body weight of 1000-2500 g and a body length of 35-45 cm. The gestational age is considered the most stable criterion; anthropometric indicators, due to their significant variability, are conditional criteria for prematurity. Every year, as a result of spontaneous premature birth or artificially induced termination of pregnancy in the later stages, 5-10% of children from the total number of newborns are born prematurely.
According to the WHO definition (1974), a fetus is considered viable with a gestational age of more than 22 weeks, a body weight of 500 g, a body length of 25 cm. length less than 35 cm is regarded as a late miscarriage. However, if such a child was born alive and lived after birth for at least 7 days, he is registered as premature. The level of neonatal mortality among premature babies is much higher than that among full-term babies, and largely depends on the quality of medical care in the first minutes and days of a child's life.
premature babies
Causes of prematurity
All the reasons leading to the birth of premature babies can be grouped into several groups. The first group includes socio-biological factors, including too young or old age of parents (under 18 and over 40), bad habits of a pregnant woman, malnutrition and unsatisfactory living conditions, occupational hazards, unfavorable psycho-emotional background, etc. Risk of premature delivery and birth premature babies are higher in women who did not plan a pregnancy and neglect medical support for pregnancy.
Risk of premature delivery and birth premature babies are higher in women who did not plan a pregnancy and neglect medical support for pregnancy.
The second group of reasons is burdened obstetric and gynecological history and the pathological course of this pregnancy in the expectant mother. Here, a history of abortion, multiple pregnancy, gestosis, hemolytic disease of the fetus, and premature detachment of the placenta are of the greatest importance. The reason for the birth of premature babies can be short (less than 2 years) intervals between births. Premature babies are often born to women who resort to in vitro fertilization, but this is not due to the very fact of using ART, but rather to the “female” factor that prevents natural fertilization. Gynecological diseases and malformations of the genitals adversely affect pregnancy: cervicitis, endometritis, oophoritis, fibroma, endometriosis, bicornuate saddle uterus, uterine hypoplasia, etc.
The third group of causes that disrupt the normal maturation of the fetus and cause an increased likelihood of the birth of premature babies include various extragenital diseases of the mother: diabetes mellitus, hypertension, heart defects, pyelonephritis, rheumatism, etc. Often, premature births are provoked by acute infectious diseases suffered by a woman in late gestation periods.
Often, premature births are provoked by acute infectious diseases suffered by a woman in late gestation periods.
Finally, the birth of premature babies may be associated with pathology and abnormal development of the fetus itself: chromosomal and genetic diseases, intrauterine infections, severe malformations.
Classification of prematurity
Taking into account the indicated criteria (gestational age, body weight and length), 4 degrees of prematurity are distinguished:
I degree of prematurity - delivery occurs at a period of 36-37 weeks of gestation; the body weight of the child at birth is 2500-2001 g, length - 45-41 cm.
II degree of prematurity - delivery occurs at a period of 32-35 weeks of gestation; the body weight of the child at birth is 2001-2500 g, length - 40-36 cm.
III degree of prematurity - delivery occurs at a period of 31-28 weeks of gestation; the body weight of a child at birth is 1500-1001 g, length - 35-30 cm.
IV degree of prematurity - delivery occurs before 28 weeks of gestation; the birth weight of the child is less than 1000 g, the length is less than 30 cm. The term "premature with extremely low body weight" is used in relation to such children.
External signs of prematurity
Premature babies are characterized by a number of clinical signs, the severity of which correlates with the degree of prematurity.
Severely preterm infants weighing <1500 are born with thin wrinkled skin richly covered with cheesy grease and vellus hair (lanugo). The skin has a bright red color (the so-called simple erythema), which turns pale by 2-3 weeks of age. The subcutaneous fat layer is absent (hypotrophy II-II degree), the child's physique is disproportionate (the head is large and is approximately 1/3 of the body length, the limbs are relatively short). The abdomen is large, flattened with a clearly visible divergence of the rectus muscles, the navel is located in the lower abdomen.
In very premature babies, all fontanelles and sutures of the skull are open, the cranial bones are supple, the brain skull prevails over the facial one. Characterized by underdevelopment of the auricles, poor development of the nails (nail plates do not reach the fingertips), weak pigmentation of the nipples and areola. The genital organs in premature babies are underdeveloped: in girls there is a gaping of the genital slit, in boys - undescended testicles into the scrotum (cryptorchidism).
Premature babies born at 33-34 weeks of gestation and later are characterized by greater maturity. Their appearance is distinguished by the pink color of the skin, the absence of fluff on the face and torso, a more proportional physique (smaller head, higher navel, etc.). In premature babies of I-II degree, the bends of the auricles are formed, the pigmentation of the nipples and areola circles is expressed. In girls, the large labia almost completely cover the genital gap; in boys, the testicles are located at the entrance to the scrotum.
Anatomical and physiological features of premature babies
Prematurity is determined not so much by anthropometric indicators as by morphological and functional immaturity of vital organs and body systems.
Characteristic features of the respiratory organs in premature infants are the narrowness of the upper respiratory tract, the high position of the diaphragm, the compliance of the chest, and the perpendicular arrangement of the ribs relative to the sternum. These morphological features of premature babies cause superficial, frequent, weakened breathing (40-70 per minute), a tendency to apnea lasting 5-10 seconds (apnea of prematurity). Due to the underdevelopment of the elastic tissue of the lungs, the immaturity of the alveoli, and the reduced content of surfactant in premature babies, a syndrome of respiratory disorders easily occurs (congestive pneumonia, respiratory distress syndrome).
The immaturity of the cardiovascular system is characterized by pulse lability, tachycardia 120-180 per minute, muffled heart tones, arterial hypotension (55-65/20-30 mm Hg). In the presence of congenital heart defects (open ductus arteriosus, open foramen ovale), murmurs may be heard. Due to the increased fragility and permeability of the vascular walls, hemorrhages easily occur (subcutaneous, into internal organs, into the brain).
In the presence of congenital heart defects (open ductus arteriosus, open foramen ovale), murmurs may be heard. Due to the increased fragility and permeability of the vascular walls, hemorrhages easily occur (subcutaneous, into internal organs, into the brain).
Morphological signs of CNS immaturity in premature infants are weak differentiation of gray and white matter, smoothness of the brain sulci, incomplete myelination of nerve fibers, and poor vascularization of the subcortical zones. Muscle tone in premature babies is weak, physiological reflexes and motor activity are reduced, the reaction to stimuli is slowed down, thermoregulation is impaired, and there is a tendency to both hypo- and hyperthermia. In the first 2-3 weeks, a premature baby may experience transient nystagmus and strabismus, tremors, shudders, stop clonus.
In premature babies, functional immaturity of all parts of the gastrointestinal tract and low enzyme-excretory activity are noted. In this regard, premature babies are prone to regurgitation, the development of flatulence, dysbacteriosis. Jaundice in premature babies is more intense and lasts longer than in full-term newborns. Due to the immaturity of the liver enzyme systems, the increased permeability of the blood-brain barrier, and the rapid breakdown of red blood cells, premature infants can easily develop bilirubin encephalopathy.
In this regard, premature babies are prone to regurgitation, the development of flatulence, dysbacteriosis. Jaundice in premature babies is more intense and lasts longer than in full-term newborns. Due to the immaturity of the liver enzyme systems, the increased permeability of the blood-brain barrier, and the rapid breakdown of red blood cells, premature infants can easily develop bilirubin encephalopathy.
Functional immaturity of the kidneys in premature infants leads to changes in the electrolyte balance (hypocalcemia, hypomagnesemia, hypernatremia, hyperkalemia), decompensated metabolic acidosis, a tendency to edema and rapid dehydration with inadequate care.
The activity of the endocrine system is characterized by a delay in the formation of the circadian rhythm of hormone release, rapid depletion of the glands. In premature babies, there is a low synthesis of catecholamines, transient hypothyroidism often develops, and a sexual crisis rarely occurs in the first days of life (physiological mastitis, physiological vulvovaginitis in girls).
In premature babies, early anemia develops more rapidly than in full-term babies, there is an increased risk of developing septicemia (sepsis) and septicopyemia (purulent meningitis, osteomyelitis, ulcerative necrotic enterocolitis).
During the first year of life, the increase in body weight and length in premature babies occurs very intensively. However, according to anthropometric indicators, premature babies catch up with their peers born at term only by 2-3 years (sometimes by 5-6 years). The lag in psychomotor and speech development in premature babies depends on the degree of prematurity and comorbidity. In a favorable scenario for the development of a premature baby, alignment occurs in the 2nd year of life.
Further physical and psychomotor development of premature babies may be on par with their peers or be delayed.
Among premature babies, neurological disorders are more common than among full-term peers: astheno-vegetative syndrome, hydrocephalus, convulsive syndrome, vegetative-vascular dystonia, cerebral palsy, hyperactivity, functional dyslalia or dysarthria. Almost a third of premature babies have a pathology of the organ of vision - myopia and astigmatism of varying severity, glaucoma, strabismus, retinal detachment, optic nerve atrophy. Premature babies are prone to frequent repeated SARS, otitis media, against which hearing loss may develop.
Almost a third of premature babies have a pathology of the organ of vision - myopia and astigmatism of varying severity, glaucoma, strabismus, retinal detachment, optic nerve atrophy. Premature babies are prone to frequent repeated SARS, otitis media, against which hearing loss may develop.
Women born prematurely in adulthood often suffer from menstrual irregularities, signs of sexual infantilism; they may be at risk of spontaneous abortion and premature birth.
Specific care for premature babies
Babies born prematurely need special care. Their phased nursing is carried out by neonatologists and pediatricians, first in the maternity hospital, then in the children's hospital and polyclinic. The main components of caring for premature babies are: ensuring optimal temperature and humidity conditions, rational oxygen therapy and metered feeding. In premature babies, constant monitoring of the electrolyte composition and CBS of the blood, monitoring of the gas composition of the blood, pulse and blood pressure is carried out.
Very premature babies are placed immediately after birth in incubators, where, taking into account the condition of the child, a constant temperature (32-35 ° C), humidity (in the first days about 90%, then 60-50%), oxygenation level (about 30%) are maintained. Premature babies of I-II degree are usually placed in heated beds or in ordinary beds in special boxes, where the air temperature is maintained at 24-25°C.
Premature babies who are able to independently maintain normal body temperature, who have reached a body weight of 2000 g, with good epithelization of the umbilical wound, can be discharged home. The second stage of nursing in specialized departments of children's hospitals is indicated for premature infants who have not reached 2000 g in the first 2 weeks, and for children with perinatal pathology.
Feeding premature babies should begin in the first hours of life. Children with absent sucking and swallowing reflexes are fed through a gastric tube; if the sucking reflex is sufficiently pronounced, but the body weight is less than 1800 g, the child is fed through the nipple; children weighing over 1800 g may be breastfed. The frequency of feeding premature babies I-II degree 7-8 times a day; III and IV degree - 10 times a day. Calculation of food is made according to special formulas.
The frequency of feeding premature babies I-II degree 7-8 times a day; III and IV degree - 10 times a day. Calculation of food is made according to special formulas.
Premature babies with physiological jaundice should receive phototherapy (general UV). As part of the rehabilitation of premature babies at the second stage, communication between the child and the mother, skin-to-skin contact, is useful.
Medical examination of premature babies
After discharge, children born prematurely need constant monitoring by a pediatrician during the first year of life. Examinations and anthropometry are carried out weekly in the first month, once every two weeks - in the first half of the year, once a month - in the second half of the year. In the first month of life, premature babies should be examined by a pediatric surgeon, pediatric neurologist, pediatric orthopedic traumatologist, pediatric cardiologist, pediatric ophthalmologist. At the age of 1 year, children need to consult a speech therapist and a child psychiatrist.