Abnormal 10 week ultrasound
10 Week Ultrasound: Procedure, Abnormalities and More
If you are reading this, we take it that you are 10 weeks pregnant. Congratulations! Now that you are 10 weeks pregnant, you can stop worrying when you’ll start looking pregnant because you have reached that phase where your pregnancy bump will start showing. Your doctor may suggest an ultrasound scan around this time to make sure that your baby is healthy and is developing normally. An ultrasound, also called a sonogram, will help create a picture of your baby on a monitor with the help of sound waves. Read on to know why you need an ultrasound scan at 10 weeks of your pregnancy and how it is performed.
Why Should You Have an Ultrasound at 10 Weeks?
Following are the reasons for performing an ultrasound scan at 10 weeks of pregnancy.
1. To check the baby’s growth.
Your doctor may suggest an ultrasound scan at 10 weeks of your pregnancy to check the progress or growth of your baby. By conducting a scan, she will be able to identify whether or not your baby is developing normally. At 10 weeks of pregnancy, the foetus weighs about 4gm and measures around 3.1cm from crown to rump. An ultrasound will make it clear how your baby is developing. She will also calculate the baby’s gestational age based on these measurements and predict a due date.
2. To check for any abnormalities.
Between 10 and 14 weeks of your pregnancy, nuchal translucency scan (NTS) will be performed to test the foetus for the risk of Down syndrome and other chromosomal abnormalities. In this, the unborn baby’s nuchal fold, which is the transparent back of the neck, will be measured to test for any abnormalities. This test is usually conducted in the 12th week of pregnancy.
3. To hear the baby’s heartbeat.
You must have heard your baby’s heartbeat through an ultrasound scan at around 8 weeks of your pregnancy itself. But you can hear it during the 10th week as well. Your doctor will perform this test to ensure that your baby’s heart functions normally.
4. To ensure that the baby’s organs are functioning normally.
In the 10th week of pregnancy, the skin of the foetus is translucent. This means that all the internal organs will be visible on the ultrasound scan. Thus your doctor will be able to gauge whether all the organs are developing normally and functioning properly or not.
5. To see how the spine is developing.
The spine should be visible by the 10th week of pregnancy. The doctor will conduct an ultrasound to check if the spine is developing normally.
6. To determine the position of the baby.
If this is your first ultrasound, then the doctor will tell you about the location of the pregnancy, i.e., the position of your baby. An ultrasound will help rule out an ectopic pregnancy.
How to Prepare for Your 10th Week Pregnancy Scan
To prepare for your 10-week ultrasound scan, you will need to have a full bladder. Going for the scan with a full bladder will help the ultrasound technician to get a clear image of the baby, the placenta, uterus, ovaries, and cervix. You will need to drink 3 glasses of water an hour before you have the ultrasound so that your bladder is full.
You will need to drink 3 glasses of water an hour before you have the ultrasound so that your bladder is full.
How Long Does It Take to Perform an Ultrasound Scan?
A typical ultrasound scan can take between 15 to 30 minutes to perform. The sonographer has to get a good image of the baby and also examine your uterus, placenta, and ovaries. If the baby is very active and moves around or is in an awkward position, the sonographer might take longer to capture clear images. And if clear images are not obtained, the scan may have to be rescheduled for some other time.
How Is an Ultrasound Scan Performed?
In order to perform an ultrasound, the sonographer will ask you to lie down on the examination table and expose your belly and abdomen. She will then apply some gel over your belly and press a wand called a transducer on the skin. This wand will send ultrasound waves that will form an image of your baby on the monitor. The technician will apply some pressure on your belly with the wand to get a clear view of the baby. The scan is not painful and is non-invasive. In some cases, the scan may be done vaginally if the abdominal scan fails to produce clear images. But you don’t have to worry – the vaginal probe is also not painful.
The scan is not painful and is non-invasive. In some cases, the scan may be done vaginally if the abdominal scan fails to produce clear images. But you don’t have to worry – the vaginal probe is also not painful.
What Will You See on the Scan at the Tenth Week of Your Pregnancy?
Here is what you can expect to see in your 10-week ultrasound scan.
- You might see your baby moving at the 10-week ultrasound. You can also expect to see your baby’s hands, feet, and head clearly.
- As your little one’s skin will be transparent, you may also see the internal organs.
- On the monitor, you will also see your baby’s heart beating and you will be able to hear it too.
- You might see your baby’s forehead bulged. It is usually bulged to accommodate the growing brain. However, the forehead will flatten gradually.
- You might also see your baby’s fingers and toes. You can also expect to see his nose and ears. You will see your baby’s eyelids but they will be closed.

- Baby’s skeleton is complete, and the framework of the spine can be seen.
No Movement at the 10th-week Ultrasound – Is this Normal?
If you do not see your baby moving at the 10th-week of your ultrasound, don’t worry. Chances are your little one might be sleeping in the womb. As long as your sonographer assures you that the baby’s growth, development, and heartbeat are normal, you need not worry.
What If Some Abnormalities Are Discovered in the Scan?
If any abnormalities are spotted in the 10-week ultrasound pictures, your sonographer or doctor will inform you about it. In such cases, the doctor may recommend further testing such as Chorionic Villi Sampling, blood tests, and amniocentesis to be certain. Based on the findings, the doctor will speak to you about the further course of action to be taken and may even refer you to a specialist.
The 10-week ultrasound scan is also called a dating scan, as it is used to determine the gestational age of the baby and predict the due date.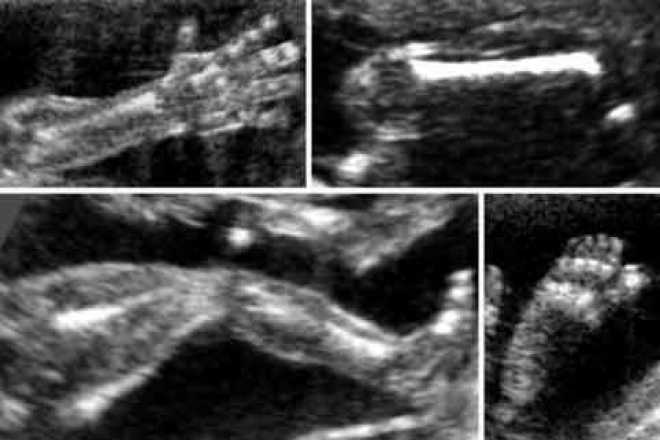 The nuchal translucency test is part of this scan. Some parents may choose to get a printed picture of the scan to preserve as a memento. In some countries, the technician may be able to determine the gender of the baby. However, sex determination is illegal in India. The 10-week ultrasound is done to ensure that the foetal development is normal and the baby is healthy. So don’t miss this ultrasound if your doctor has suggested it. Go for regular tests and have a healthy pregnancy!
The nuchal translucency test is part of this scan. Some parents may choose to get a printed picture of the scan to preserve as a memento. In some countries, the technician may be able to determine the gender of the baby. However, sex determination is illegal in India. The 10-week ultrasound is done to ensure that the foetal development is normal and the baby is healthy. So don’t miss this ultrasound if your doctor has suggested it. Go for regular tests and have a healthy pregnancy!
Previous Week: 9 Weeks Pregnant Ultrasound
Next Week: 11 Weeks Pregnant Ultrasound
Helping you understand scary (but often harmless) pregnancy ultrasound findings | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
October 24, 2017
Your Pregnancy Matters
Robyn Horsager-Boehrer, M.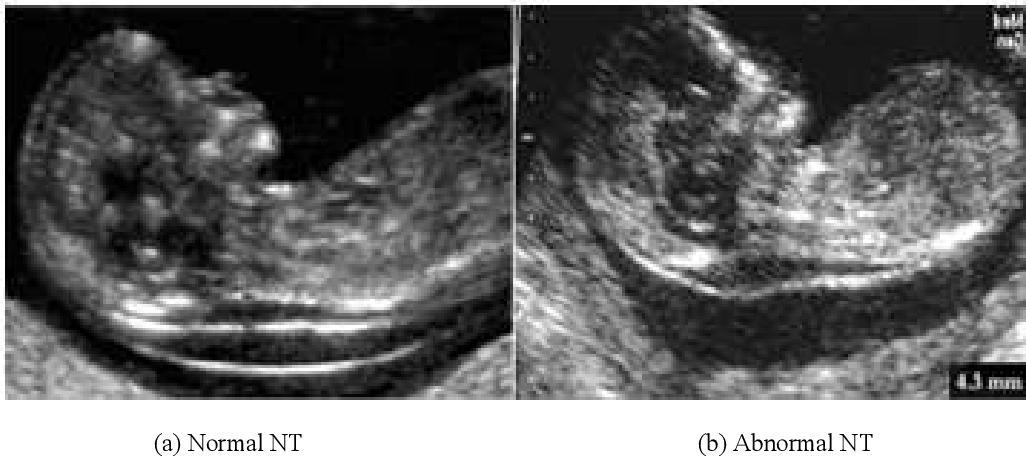 D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
Expecting parents encounter an abundance of medical terms during pregnancy. Some of these can be quite scary, particularly when the patient sees them in electronic medical records or imaging reports without context from a doctor.
Below are three fairly common ultrasound findings that you might come across. The first is a physical abnormality that, when seen by itself, almost never causes problems before or after delivery. The second and third findings are markers, which means they’re loosely associated with (but not causes of) chromosomal conditions such as trisomy 21, or Down syndrome. Alone, markers almost always are harmless. Combined with another marker or a screening test that suggests a high risk of chromosome concerns, the marker might indicate a higher risk for that condition.
Alone, markers almost always are harmless. Combined with another marker or a screening test that suggests a high risk of chromosome concerns, the marker might indicate a higher risk for that condition.
These terms can sound scary. But once we have a little more information about your background and risk for congenital problems in the fetus, they rarely are cause for concern. Your doctor will probably refer you to a maternal-fetal medicine doctor for advanced imaging of the findings, just to be safe.
Single umbilical artery (SUA) appears as one small circle.Single umbilical artery
This one really freaks people out because the umbilical cord is seen as the baby’s lifeline, but this defect is common and occurs in as many as 1 percent of single-baby pregnancies and almost 5 percent of multiple pregnancies. The umbilical cord typically has three blood vessels: one umbilical vein that delivers nutrients and oxygen-rich blood to the baby and two arteries that drain blood back to the placenta.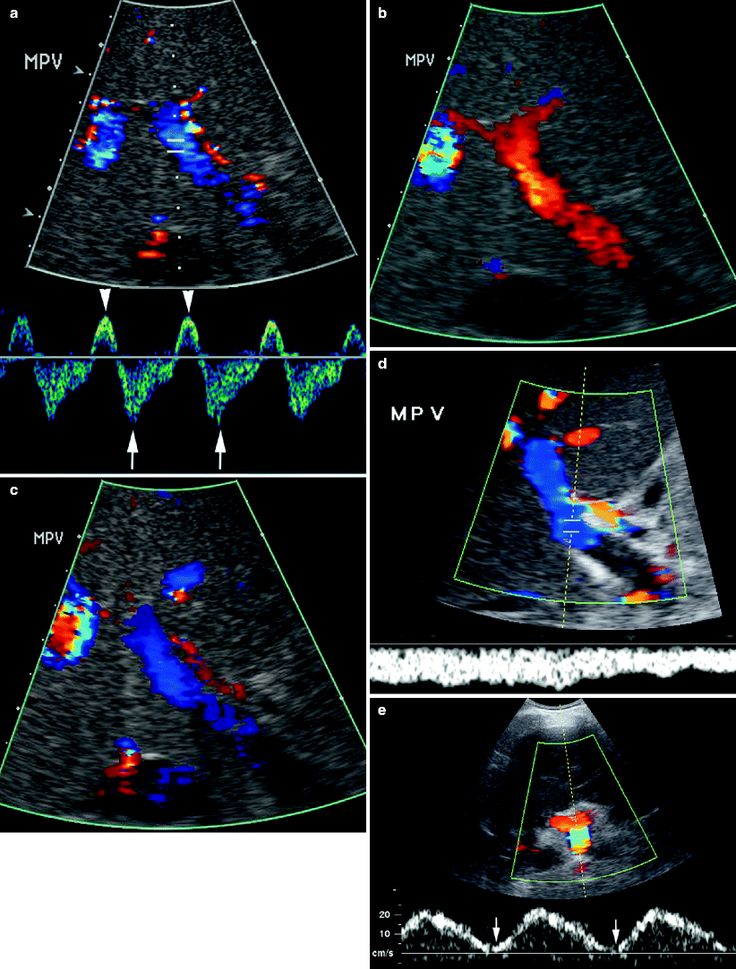 This pregnancy defect occurs when just one artery develops or one of the two arteries that did develop becomes blocked and withers away. An umbilical cord with a single umbilical artery is also called a “two vessel cord” since it contains just one artery and one vein.
This pregnancy defect occurs when just one artery develops or one of the two arteries that did develop becomes blocked and withers away. An umbilical cord with a single umbilical artery is also called a “two vessel cord” since it contains just one artery and one vein.
Some researchers think single umbilical artery (SUA) might be associated with slightly smaller babies or delivering a few days early. But on average, these babies weigh 6.5 pounds and arrive after 38 weeks of pregnancy – not very small or very early. Though typically harmless, the defect also carries a slightly higher risk for chromosomal conditions such as Down syndrome.
If we see this defect on an ultrasound, we’ll thoroughly examine the baby to make sure everything else is developing as expected. A single umbilical artery is associated with a higher risk that the baby might have a problem with other organ systems such as the heart and kidneys. We’ll also check the mother’s risk for chromosomal abnormalities through blood tests or other screenings. At the end of this evaluation, if a SUA is the only red flag, there’s almost never cause for concern for the baby’s health. We might do extra ultrasounds in the third trimester just to check on the baby’s growth, but nothing else needs to be done – there are no long-term complications. After delivery, there is no use for these arteries. They simply shrivel up and waste away.
At the end of this evaluation, if a SUA is the only red flag, there’s almost never cause for concern for the baby’s health. We might do extra ultrasounds in the third trimester just to check on the baby’s growth, but nothing else needs to be done – there are no long-term complications. After delivery, there is no use for these arteries. They simply shrivel up and waste away.
Choroid plexus cyst
As many as 2 percent of pregnancies will show choroid plexus cysts. The choroid plexus is the part of the brain that makes spinal fluid, which is released by fingerlike projections in the brain. Sometimes these get stuck together and fluid collects between them, which appears as a cyst on ultrasound.
The word “cyst” implies something that shouldn’t be there, and a cyst that has formed in the brain really sounds scary. People ask, “Is it taking up space so normal brain tissue can’t develop? Will it continue to get bigger?” But it’s really just a little fluid buildup that is seen in the middle of the pregnancy and is usually gone by about 6 months of gestation. Choroid plexus cysts on their own are not harmful. If the mother has screened positive for higher risk of the chromosome abnormality trisomy 18 in pregnancy, we would talk about additional testing. But otherwise, virtually all of these cysts go away on their own with no long-term risk and no need for follow-up testing during or after pregnancy.
People ask, “Is it taking up space so normal brain tissue can’t develop? Will it continue to get bigger?” But it’s really just a little fluid buildup that is seen in the middle of the pregnancy and is usually gone by about 6 months of gestation. Choroid plexus cysts on their own are not harmful. If the mother has screened positive for higher risk of the chromosome abnormality trisomy 18 in pregnancy, we would talk about additional testing. But otherwise, virtually all of these cysts go away on their own with no long-term risk and no need for follow-up testing during or after pregnancy.
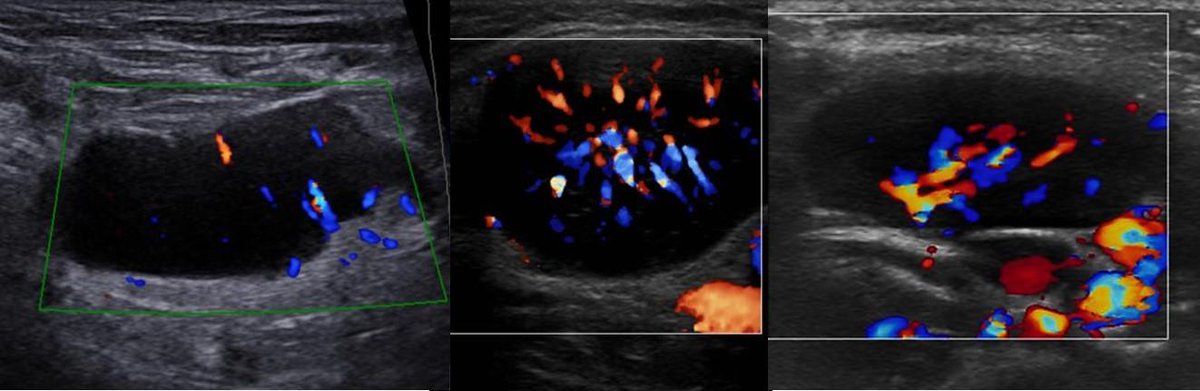
Echogenic intracardiac focus
Heart problems are the most common congenital birth defects, and it’s easy to panic when something unusual is detected on ultrasound. But echogenic intracardiac focus (EIF) is almost never something to worry about. It shows up as a bright spot on the heart in imaging, and it’s thought to be a microcalcification on the heart muscle.
It shows up as a bright spot on the heart in imaging, and it’s thought to be a microcalcification on the heart muscle.
EIF occurs in as many as 5 percent of all pregnancies. It is so common in babies with Asian ethnicity that it can’t even be used as a marker. So our first question when we detect a bright spot is about the parents’ ethnic backgrounds. Similar to choroid plexus cysts, this marker might indicate a chromosomal condition if paired with other worries on the ultrasound or an increased risk for Down syndrome or trisomy 13 on a prenatal screen. Again, if it’s an isolated finding, we don’t worry about it. EIF has no impact on heart function before or after birth and almost never requires follow-up testing.
If a patient has already had an amniocentesis or chorionic villus sampling (CVS), or even a cell-free fetal DNA screen, then all of these findings are even less important.
Balancing transparency with necessity
A lot of the time, doctors don’t even mention these isolated findings if we know there’s nothing else going on with the baby and the mom is at low risk for chromosomal problems.
For most women, I mention that the finding will appear on the final ultrasound report since patients can see all of their results in our electronic medical record. I explain what it means and why they shouldn’t worry. For others, I don’t say anything at all. My patients’ emotional health is just as important as their physical health, and I don’t want them to worry unnecessarily. While I tend toward transparency, I do take it case by case. We do as much as we can to make sure you worry as little as possible, but if you do run across a term that concerns you, please ask. We’ll always give you an honest answer.
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
November 15, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 7, 2022
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.
 D.
D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.D.
August 23, 2022
More Articles
Prenatal ultrasonography of fetal craniofacial anomalies
Authors: Annisa Shui Lam Mak, Kwok Yin Leung
Introduction
other, more subtle anomalies, syndromes, chromosomal mutations, or even rarer conditions such as infections or metabolic disorders.
It remains a difficult process, especially in the first trimester. The frequency of detection of craniofacial anomalies (PCA) varies depending on the type of anomaly, its severity, gestational age, associated anomalies, as well as methods and technologies of ultrasound examinations. So the prevalence of cheiloschisis and craniosynostosis is about 0.15% and 0.05%, respectively.
Various professional societies, including the International Society for Ultrasound in Obstetrics and Gynecology (ISUOG), the American Institute of Ultrasound in Medicine, and the Asian Oceania Federation of Obstetrics and Gynecology, have issued recommendations for facial and skull examinations in the second trimester of pregnancy. The main purpose of this article is to provide updated information on the prenatal detection of PPA in order to improve the accuracy of diagnosis.
Changes in the brain region of the skull
The size, shape, integrity and density of the skull bone can be assessed when head size is measured and when brain structures are examined.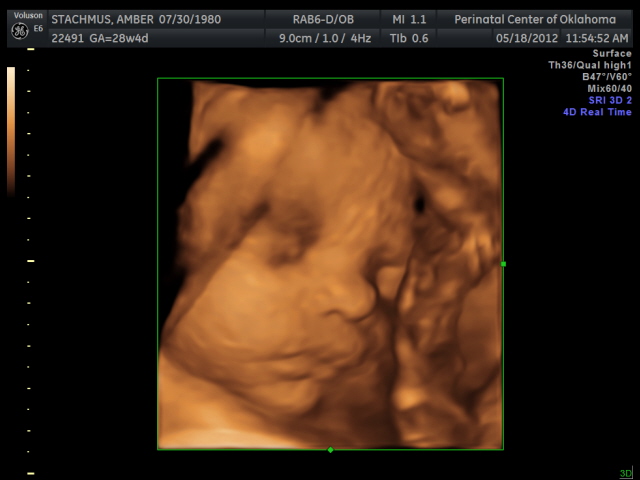 The skull is oval in shape and has a continuous echogenic structure interrupted only by narrow echolucentric sutures. Abnormal features (Fig. 1-3) and associated anomalies are shown in Table 1.
The skull is oval in shape and has a continuous echogenic structure interrupted only by narrow echolucentric sutures. Abnormal features (Fig. 1-3) and associated anomalies are shown in Table 1.
Figure 1: Second trimester fetus with trigonocephaly.
Axial view of the fetal head (H) shows a triangular forehead (arrow).
Figure 2: Second trimester fetus with brachycephaly. Axial view of the fetal head (H) shows that the skull shape is shorter than typical (arrow).
Figure 3: Second trimester fetus with scaphocephaly.
Axial view of the fetal head (H) showing a long (pointer) and narrow fetal head (arrows).
Table 1.
| Criteria | Index | Anomaly |
| Size | Small | Microcephaly |
| Large | Macrocephaly | |
| Form | Not oval, lemon-shaped | Spina bifida, trisomy 18 or skeletal dysplasia |
| Integrity | Defect in the skull bone with protrusion of brain tissue | Encephalocele |
| Density | No echogenicity, skull easily compressed | Weak mineralization, osteogenesis imperfecta or hypophosphatasia |
Diagnosis of craniosynostosis is expressed in the loss of hypoechogenicity in the segment of the main sutures of the skull, along with the expansion of other orthogonal sutures. Indirect signs, including abnormal cephalic index (CI), skull shape (Table 2), and/or facial morphology such as hypotelorism or hypertelorism, may precede suture closure by weeks 4-16. CIs below 70% or above 85% indicate dolichocephaly and brachycephaly, respectively.
Indirect signs, including abnormal cephalic index (CI), skull shape (Table 2), and/or facial morphology such as hypotelorism or hypertelorism, may precede suture closure by weeks 4-16. CIs below 70% or above 85% indicate dolichocephaly and brachycephaly, respectively.
Table 2.
| Shape anomaly | Seam | Associated anomalies |
| Scaphocephaly / Dolichocephaly (long) | Sagittal | – |
| Brachycephaly (short, wide) | Bilateral coronal | Down syndrome Pfeiffer syndrome |
| Plagiocephaly (ipsilateral frontal or occipital flattening) | Single-ended coronal or lambdoid | – |
| Trigonocephaly (forward direction) | Metopic | Jacobsen syndrome or Smith-Lemli-Opitza syndrome |
| Clover (trilobite) | Sagittal, coronal and lambdoid | Thanatophoric dysplasia, Apert syndrome, Crouzon syndrome Carpenter's syndrome |
| Oxycephaly (pointed or conical) | Sagittal and lambdoid | – |
The circumference measurement also has a role.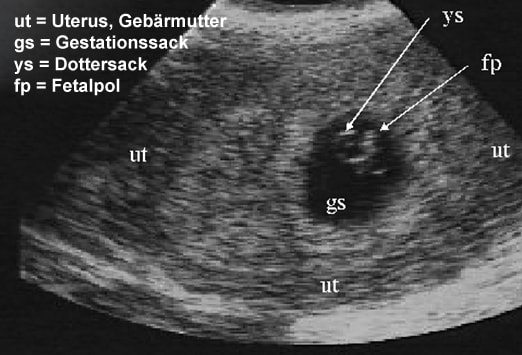 Since a head circumference deviation of more than 3 standard units below or 2 standard units above the mean, depending on gestational age, is a clue to a possible diagnosis of microcephaly or macrocephaly, respectively.
Since a head circumference deviation of more than 3 standard units below or 2 standard units above the mean, depending on gestational age, is a clue to a possible diagnosis of microcephaly or macrocephaly, respectively.
However, the use of these reference values may lead to an overdiagnosis of microcephaly. Other supporting signs should be looked out for, which include forehead deformity, a flat occiput, or intracranial contents that are abnormal or invisible.
DO YOU CARE THE ULTRASONIC MACHINE CORRECTLY?
Download the care guide now
Facial changes
The facial examination should be performed in three planes to assess different facial structures as this facilitates the detection of anomalies (Table 3). According to the ISUOG guidelines, the minimum assessment of the fetal face includes the presence of both orbits, the assessment of the nose/nostrils, the presence of the mouth and, preferably, the assessment of the profile of the face and lips.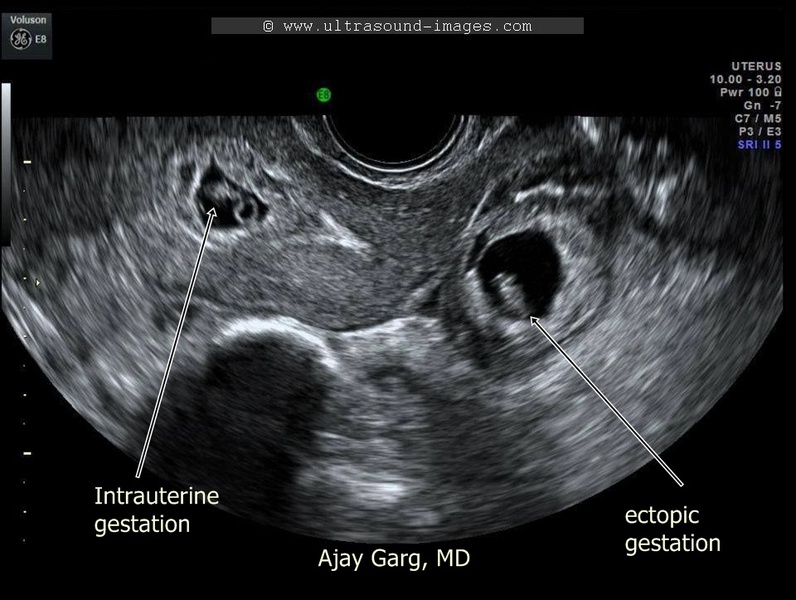
Table 3.
| Flat | Structure | Index | Anomaly |
| Crown | Lips | Integrity violation | Cheiloschisis |
| Roth | Small or continuous, open | Microstomia or syndromes | |
| Nose | Tapered or one nostril available | Hypoplasia or single nostril syndrome | |
| Palpebral groove | Tilt up or down | ||
| Cross | Orbits | Small, absent, abnormal interocular diameter | Microphthalmia / anophthalmia, hypotelorism / hypertelorism |
| Medial cyst | Lacrimal sac cyst | ||
| Crystal lens | Echogenic | Cataract | |
| Dental buds | Cracks, abnormal number | Cleft palate, oligodontia / anodontia | |
| Lower jaw | Small | Micrognathia | |
| Tongue | Missing or double equal sign | Cleft uvula | |
| Ears | Wrong size, shape, location or deployed | Anomaly of ear development | |
| Sagittal | Lob | Convex | Skeletal dysplasia |
| Flattened | Microcephaly | ||
| Hanging | Extension nose | ||
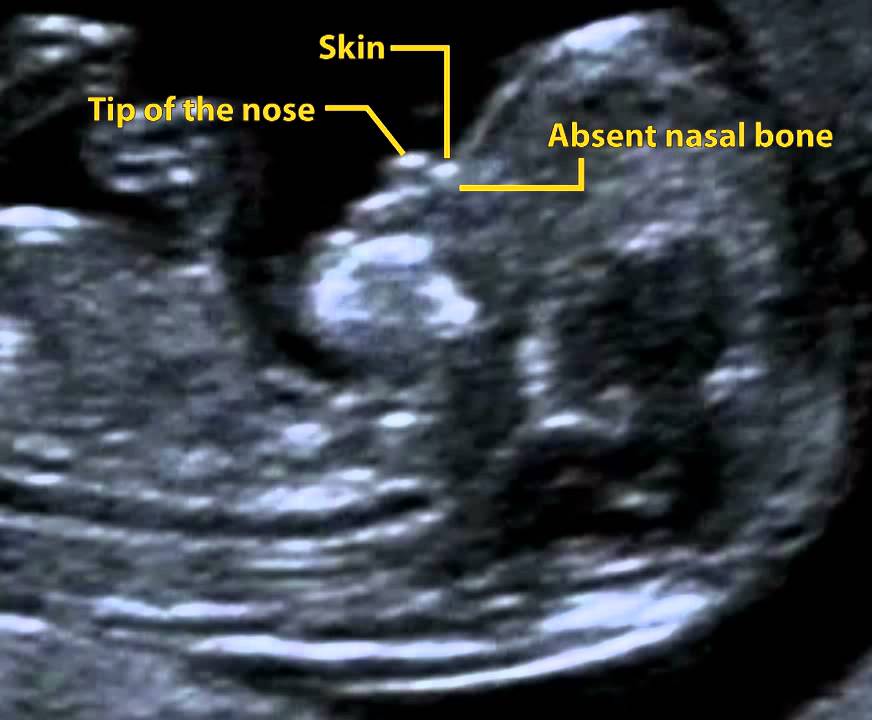
| Nose | Flattened | Syndromes | |
| Absence or shortening of the nasal bone | Aneuploidy | ||
| Upper jaw | Premaxillary protrusion | Bilateral Cleft Facial | |
| Soft sky | No soft palate or "equal sign" | Cleft palate, accessory uvula | |
| philtrum | Long or short | Syndromes | |
| Lower jaw | Small | Micrognathia | |
| Symmetry | Facial asymmetry | ||
| Language | Large, protruding, massively displaced backwards | Macroglossia, tumor glossoptosis | |
| Ears | Abnormal size, shape or location or deployed | Anomaly of ear development |
A cleft is diagnosed when the integrity of the lip is lost on one or both sides on the coronal view (Fig.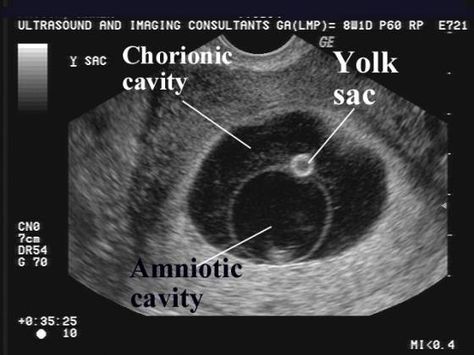 4, 5). Bilateral cleft lip suggests a premaxillary bulge in sagittal view (Fig. 6). It is difficult to diagnose an incomplete cleft lip (Fig. 7), often only a cleft palate is visible. Using color Doppler, one can see the flow of amniotic fluid normally passing through the nostrils during breathing activity, in case of an anomaly through the palate when it has a cleft.
4, 5). Bilateral cleft lip suggests a premaxillary bulge in sagittal view (Fig. 6). It is difficult to diagnose an incomplete cleft lip (Fig. 7), often only a cleft palate is visible. Using color Doppler, one can see the flow of amniotic fluid normally passing through the nostrils during breathing activity, in case of an anomaly through the palate when it has a cleft.
Figure 4: Second trimester fetus with unilateral cleft lip.
Coronal view of the fetal face showing loss of integrity (arrow) of the upper lip (L).
Figure 5: Second trimester fetus with bilateral cleft lip.
Coronal view of the fetal face showing loss of integrity (arrows) of the upper lip (L) on both sides (1 and 2).
Figure 6: Second trimester fetus with premaxillary bulge.
Sagittal view of the fetal face showing a soft tissue mass (arrow) projecting forward under the nose (N).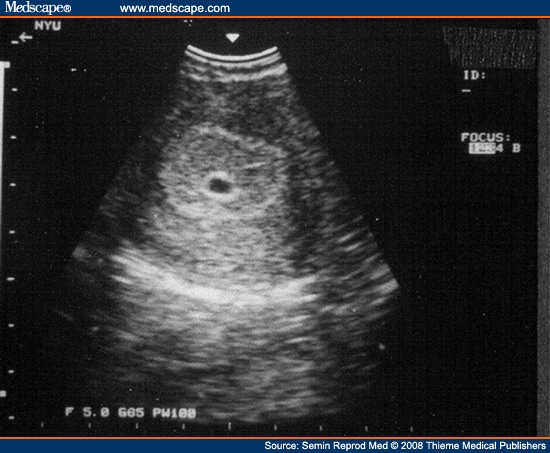
Figure 7: Second trimester fetus with partial unilateral cleft lip. The coronal plane of the fetal face shows partial loss of integrity (arrows) of the upper lip (L).
The face profile can be assessed from the mid-sagittal projection. In particular, frontal bulges (Fig. 8), micrognathia (Fig. 9), or a flat nose (Fig. 10) may be found. From the lateral side, ear anomalies can be assessed (Fig. 11). Both eyes and their anomalies can be assessed in the axial plane (Fig. 12-14).
Figure 8: Second trimester fetus with prominent forehead.
Mid-sagittal view showing a straight bulge (arrow) of the forehead (FH).
Figure 9: Second trimester fetus with micrognathia.
Mid-sagittal view showing a small and receding (arrow) chin (C).
Figure 10: Second trimester fetus with flat nose.
Mid-sagittal view showing a flat (arrow) nose (N).
Figure 11: Second trimester fetus with ear anomaly.
Lateral sagittal view showing a small (arrows) right (R) ear (E) with loss of normal structure.
Figure 12: Second trimester fetus with hypotelorism.
The axial view shows the anomalously reduced distance (arrows) between the two orbits (circle).
Figure 13: Second trimester fetus with bilateral cataract.
Axial view showing echogenicity (arrows) in the lens (L) of both eyes.
Figure 14: Second trimester fetus with protrusion between two orbits. The axial view shows a soft tissue mass (arrows) protruding between two orbits (circles).
It is worth distinguishing between micrognathia (small lower jaw) and retrognathia - displacement of the jaw to the rear. It is differentiated by determining the lower angle of the face in relation to the width of the lower jaw to the width of the upper jaw. With a confounded family history or if an anomaly is suspected, measurements of fetal structures such as nasal bone length, ear length, maxillary length, and eye and interocular space diameters may be performed.
With a confounded family history or if an anomaly is suspected, measurements of fetal structures such as nasal bone length, ear length, maxillary length, and eye and interocular space diameters may be performed.
3D/4D 3D Imaging
The use of 3D ultrasound, including surface imaging, multiplanar and multilayer imaging, allows accurate assessment of various craniofacial structures and their anomalies, including cleft palate (Figs. 15, 16) and craniosynostosis. Images may be useful for counseling (Figures 17, 18). The use of 3D (Fig. 19) can help differentiate closed and open sutures. The use of 4D can be used to evaluate facial expressions.
Figure 15: Second trimester fetus with bilateral cleft lip and palate. 3D axial view showing loss of integrity (arrows) of the lip (L) and palate (P) on both sides.
Figure 16: Second trimester fetus with midline cleft lip and palate. 3D axial view showing midline loss of integrity (arrows) of the lip (L) and palate (P). The colored boxes on the right show the orientation of the active images on the left: axial view (1), sagittal view (2), and coronal view (3).
The colored boxes on the right show the orientation of the active images on the left: axial view (1), sagittal view (2), and coronal view (3).
Figure 17: Second trimester fetus with unilateral cleft lip.
3D surface view of the fetal face showing a cleft (arrow) on the upper lip (L).
Figure 18: Second trimester fetus with midline cleft.
3D superficial image of the fetal face shows a cleft (arrow) in the midline of the upper lip (L).
Figure 19: Second trimester fetus with craniosynostosis.
3D skeletal superficial, axial view of the skull showing constriction (arrows) of the coronal suture (CS) and part of the anterior fontanelle (AF).
First trimester ultrasound
Between 11 and 13 weeks, during the 6 days of pregnancy, ISUOG guidelines suggest measuring biparietal diameter and head circumference, as well as assessing the integrity and echogenicity of the skull. You can try to assess the orbits, interorbital distances, facial profile, ears, and the integrity of the mouth and lips. In the first trimester, a flattening of the profile can be detected (Fig. 20). However, some craniofacial anomalies, such as craniosynostosis, cannot be diagnosed in the first trimester, and thus a second trimester scan of the anomaly remains the standard for fetal anatomic evaluation.
You can try to assess the orbits, interorbital distances, facial profile, ears, and the integrity of the mouth and lips. In the first trimester, a flattening of the profile can be detected (Fig. 20). However, some craniofacial anomalies, such as craniosynostosis, cannot be diagnosed in the first trimester, and thus a second trimester scan of the anomaly remains the standard for fetal anatomic evaluation.
Figure 20: First trimester fetus with flat facial profile.
Sagittal view showing flat forehead (FH) (arrow), nose (N) (arrow) and drooping chin (C) (curved arrow).
Lateral investigations
When a cleft palate is found, it is important to determine whether it is unilateral, bilateral, or median, and whether there is any cleft plate or amniotic streak, because this varies the prognosis and associated conditions . Combined cleft lip and palate is more common than cleft lip itself, and the associated problems are more serious.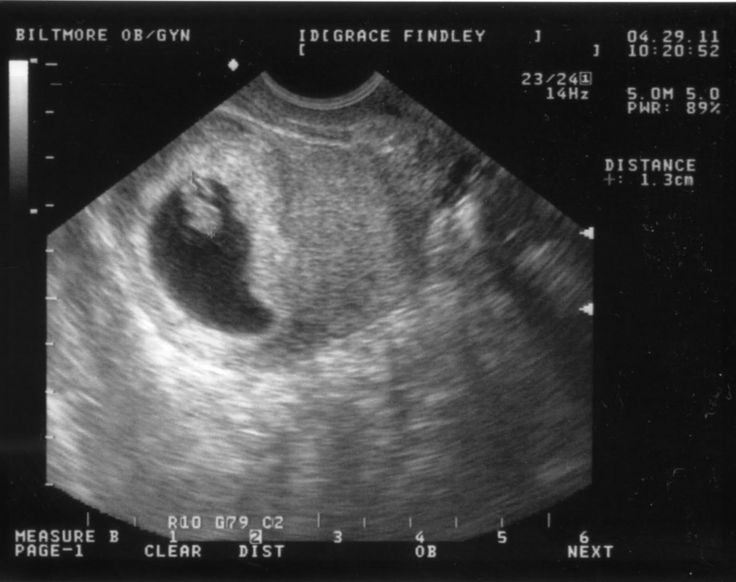 Unilateral/bilateral and median cleft lip are considered different conditions as they have different embryological origins.
Unilateral/bilateral and median cleft lip are considered different conditions as they have different embryological origins.
Whenever a craniofacial anomaly is detected, it is important to perform a detailed scan to look for additional anomalies, especially other potentially subtle malformations of the face, central nervous system, heart, or extremities. Many craniofacial anomalies, including facial clefts, micrognathia, craniosynostosis, hypertelorism/hypothalmia, microphthalmia/anophthalmia, cataracts, and anotia/microtia, are associated with various syndromes and conditions (Table 4).
Overall, 10% of clefts were accompanied by a chromosomal abnormality and 27% had an associated abnormality. Approximately 15% of cases of craniosynostosis are syndromic. Protrusion of the tongue can be a sign of Beckwith-Wiedemann syndrome or Down syndrome.
Table 4.
| Anomaly | Associated defects | Syndromes |
| Cleft face | Upper limbs | Ectrodactyly, ectodermal dysplasia, splitting syndrome, oral-facial syndrome type I |
| Cleft face | Other anomalies of the facial skull and heart | CHARGE syndrome (coloboma, cardiac anomaly, choanal atresia, mental retardation, genital and ear anomalies) |
| Micrognathia | Ears | Goldenhar syndrome |
| Micrognathia | Limbs | Hypogenesis mouth-mandible-limb syndrome, Nager syndrome, splitting syndrome, Roberts syndrome |
| Micrognathia | Other anomalies of the facial skull | Robin Syndrome, Treacher Collins Syndrome |
| Craniosynostosis | Other anomalies of the facial skull and limbs | Apert syndrome, Crouzon syndrome, Carpenter syndrome, thanatophoric dysplasia, Pfeiffer syndrome, Saetre-Chotzen syndrome, Muencke syndrome, Jackson-Weiss syndrome, Antley-Bixtler syndrome, Wolff-Hirshhorn syndrome (4p) |
Prognosis
Prognosis and management depend on the type and severity of craniofacial anomalies, the underlying condition, or chromosomal mutations. If the prognosis is poor, such as in the case of multiple anomalies or associated aneuploidies, the option of terminating the pregnancy may be offered, depending on gestational age and local norms. Alternatively, continuation of pregnancy with prenatal counseling is appropriate for mild and isolated disorders such as cleft lip.
If the prognosis is poor, such as in the case of multiple anomalies or associated aneuploidies, the option of terminating the pregnancy may be offered, depending on gestational age and local norms. Alternatively, continuation of pregnancy with prenatal counseling is appropriate for mild and isolated disorders such as cleft lip.
Isolated macrocephaly (with a head circumference that is 2-3 standard deviations above the mean for gestational age), dolichocephaly, and brachycephaly usually have a favorable outcome.
In our catalog you can choose devices for examinations in the field of obstetrics and gynecology from leading manufacturers of ultrasound equipment. Contact our manager to clarify the details and choose the model that is best for you.
prices for tests for pregnant women
During fetal development, ultrasound is one of the key methods of examination. There is no exact schedule for ultrasound, so the doctor focuses primarily on the condition of the patient, the condition of the fetus, the presence of somatic pathology. If we take a physiologically occurring pregnancy, then ultrasound is performed in each of the trimesters.
If we take a physiologically occurring pregnancy, then ultrasound is performed in each of the trimesters.
Ultrasound at 8 weeks is the first time this study is recommended. The eighth week is the first critical period, therefore, it is most rational to carry out diagnostics during this period.
Since it is the 8th week of pregnancy, a transvaginal examination is performed more often, which is more reliable. At this time, transabdominal ultrasound is used less and less. The transvaginal method does not pose any threat to either the mother or the fetus.
Ultrasound at 8 weeks can confirm
- Normal uterine pregnancy;
- Dimensions of the gestational sac;
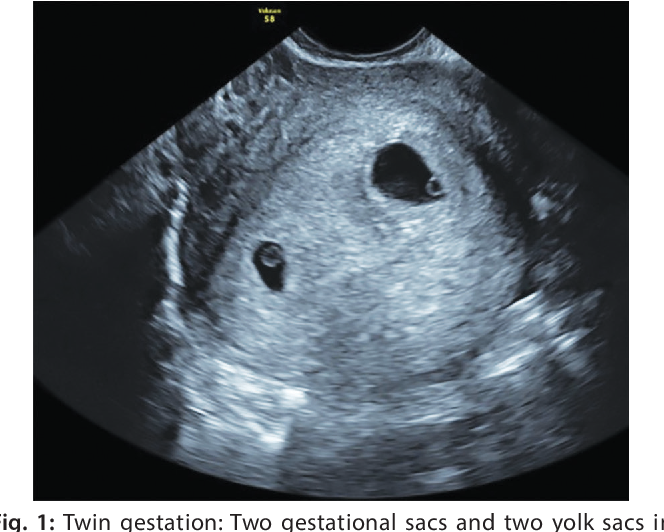
- Whether the pregnancy is multiple;
- Fetal attachment site;
- Rule out malformations;
- Exclude various obstetric complications.
If the doctor confirms a physiologically proceeding pregnancy on ultrasound, does not reveal complications, the fetus develops according to age norms, then the next ultrasound is prescribed at 12 weeks. This period is another critical period when it is necessary to assess the condition of the woman and the unborn baby.
This period is another critical period when it is necessary to assess the condition of the woman and the unborn baby.
If the first two critical periods are mainly related to hormonal changes, then the next period - 22 weeks, is most often associated with sexual infections. Therefore, we also perform an ultrasound at 22 weeks. Pregnancy can provoke the development of latent infections, which, in turn, can lead to certain complications.
Tests at 8 weeks of pregnancy
There are no exact recommendations for registering pregnant women, but doctors recommend starting monitoring at the antenatal clinic before 12 weeks. There is a mandatory list of tests in accordance with the order of the Ministry of Health of the Russian Federation, and an additional one, which is appointed by the gynecologist individually.
Tests at 8 weeks of gestation:
- CBC;
- OAM;
- Swab;
- Determination of blood group and Rh factor;
- Tests for major venereal diseases.

In addition, the 8th week of pregnancy is the period of visiting the following doctors:
- Therapist;
- Optometrist;
- ENT;
- Dentist.
Accordingly, if any pathology is detected, any of these specialists has the right to prescribe an additional analysis in their direction. If this pregnancy proceeds with complications, or if there are previous complications in the anamnesis, then the laboratory and instrumental complex may expand.
You will have to take tests regularly, so you should prepare in advance for the next tests at week 12.
Ultrasound at 12 weeks pregnant
As we mentioned earlier, the next critical period is the 12th week of pregnancy. Therefore, the next ultrasound is performed at this time. Here we are not talking about a simple study, but about screening, which allows you to identify intrauterine malformations of the fetus.
In contrast to the ultrasound at 8 weeks, this is predominantly a transabdominal examination. Transvaginal ultrasound is performed only for certain indications:
Transvaginal ultrasound is performed only for certain indications:
- Low insertion of the placenta;
- Presence of isthmic-cervical insufficiency;
- Pelvic inflammation;
- Atypical location of myomatous nodes;
- Incorrect position of the fetus, in which transabdominal ultrasound at 12 weeks of gestation is of little information.
So, what information does ultrasound give a gynecologist?
- Detection of deviations in the growth and development of the fetus;
- Possibility to suspect congenital anomalies;
- Exact gestational age;
- Palpitation;
- Cord entanglement;
- Characteristics of amniotic fluid;
- Condition of the placenta.
It must be clearly understood that ultrasound during pregnancy is only one of the methods of examination, therefore, if there are any deviations in the indicators, you should not panic, you should get a specialist consultation. The doctor, interpreting the results, always relies on many factors, which allows him to adequately assess the true state of the future mother and fetus.
The doctor, interpreting the results, always relies on many factors, which allows him to adequately assess the true state of the future mother and fetus.
Even if the deviations in some indicators have been confirmed, doctors still talk only about a certain probability of developing a particular pathology. In this case, a second screening may be prescribed, or a similar study is carried out at a later date. In any case, the final decision regarding the continuation of the pregnancy is made exclusively by a specialist.
Tests at 12 weeks of pregnancy
As we have already said, 12 weeks is the time for screening. For this, an ultrasound examination is prescribed, the external indicators of the woman are evaluated, and a blood test is performed.
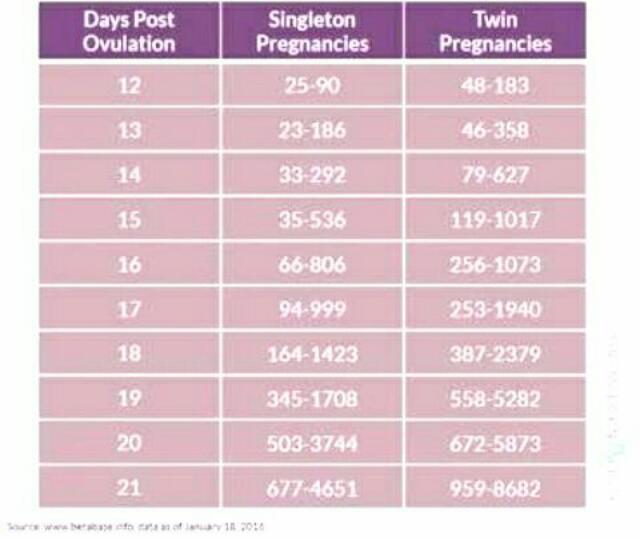
Particular attention is paid to two coefficients: β-hCG and PAPP-A. It is believed that in the presence of deviations according to these parameters, one can judge the presence of fetal pathologies. According to the level of hCG, doctors predict the further management of pregnancy and the possibility of miscarriage or premature birth.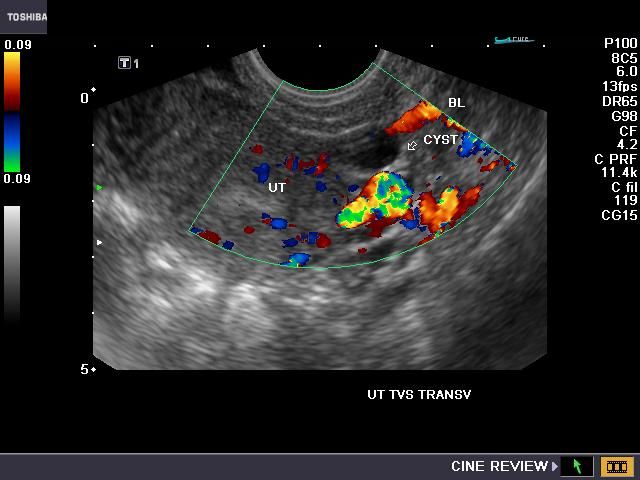
Accordingly, according to the results of screening, it is possible to identify:
- The baby has Down's syndrome;
- Multiple pregnancy;
- Specify term;
- Detect toxicosis;
- Determine the risk of miscarriage;
- Check for other chromosomal abnormalities.
Thus, tests at the 12th week of pregnancy are decisive for solving a number of issues related to the further development of the fetus. It should be clearly understood that screening is not 100% reliable, therefore, if you receive any deviations from normal results, you should immediately contact a specialist who can correctly assess such changes in indicators.
Ultrasound at 22 weeks gestation
The next scheduled ultrasound is performed at 22 weeks of gestation. Here, for the doctor, it is not the condition of the mother or the size of the fetus that is important, but the assessment of the formation of various organs and systems, as well as bones.
So, the 22nd week - the fetus has already formed all the main organs and systems, and on the monitor screen the child acquires the outlines familiar to future parents. Accordingly, the following indicators come to the fore:
- All internal organs should form. During an ultrasound, the doctor evaluates their location, how they function;
- The spine is also studied, the presence of bones and their sizes are determined;
- Assesses the brain and its activity;
- Assess the condition of the placenta, umbilical cord vessels;
- Composition of amniotic fluid;
- Condition of the cervix.
In contrast to the ultrasound at 8 weeks, at this time the ultrasound is performed transabdominally. 22 weeks is already the second trimester, and right now the question is being decided whether there are serious deviations in the development of the fetus, and further actions of obstetricians. The question of whether to continue a further pregnancy is decided not by one doctor, but by a whole council, based on numerous research results.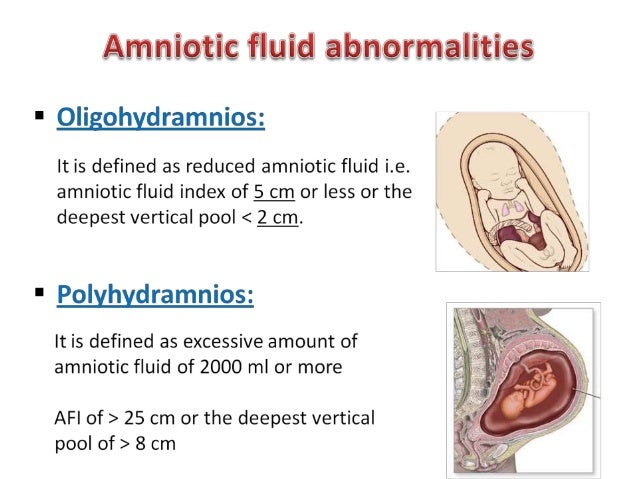
Tests at 22 weeks pregnant
Week 22 is when the second screening is more common. This analysis is prescribed in the period from 18 to 24 weeks, but this time is considered optimal. Accordingly, during repeated screening, the doctor already makes final conclusions about the condition and development of the fetus, the presence of deviations.
In addition to ultrasound, the doctor prescribes mandatory tests to monitor the woman's health. The expectant mother again takes a general blood and urine test, where the most important are a number of indicators: hemoglobin, erythrocytes, leukocytes, ESR, protein in the urine.
During the examination, the gynecologist must measure the woman's height, weight, blood pressure, and measure the abdomen. Tests at 22 weeks of gestation are designed to assess the likelihood of developing preeclampsia. Here, the role is played not by hormonal changes, but by the exacerbation of chronic pathology. Therefore, timely screening and assessment of the woman's condition allows you to plan further tactics for managing pregnancy.